Abstract
Objective
The impact of oral diseases on children cannot be overemphasized because their effects may go beyond the individual to the household and the community at large. This study aimed to determine the prevalence of common oral conditions in children between the ages of 9 and 16 years in Accra.
Methods
A cross-sectional study was carried out among participants from 16 selected junior high schools in Accra. Their caries experience was assessed using the decayed, missing, and filled teeth (DMFT) index. Other variables recorded were age, sex, previous history of a dental visit, and the presence of other common oral conditions (ie, periodontal disease, traumatised teeth, oral mucosal lesions, neoplasia, cysts, and malocclusion). Summaries and descriptive statistics were generated and reported. The DMFT was compared between subgroups, and the χ2 test was used to compare outcomes of categorical variables.
Results
A total of 1118 students participated in the study. This consisted of 37.8% males and 62.2% females. The mean age was 12.8 (standard deviation = 1.7) years. Common oral conditions were found in 49.7% of the participants and the prevalence of caries, periodontal disease, and malocclusion were found to be 13.3%, 30.4%, and 11.3%, respectively. The population's mean DMFT was found to be 0.27 (standard deviation = 0.76).
Conclusions
The prevalence of caries and periodontal disease calls for additionaleffort to reduce the burden of common oral conditions in Ghanaian children.
Key words: Prevalence, Observational study, Dental caries, Periodontal disease, Malocclusion, Ghana
Introduction
Oral diseases have been described by the World Health Organization (WHO) as the most prevalent noncommunicable disease worldwide, affecting some 3.58 billion people.1 Oral conditions do not only have functional and psychosocial repercussions on affected persons, but they are also indicators of overall well-being.2 The impact of oral diseases in children cannot be overemphasized because their effects may go beyond the individual to the household and the community at large.1
Dental caries in both primary and permanent teeth is considered to be the most common disease in childhood.3 Although distribution and response to the condition may vary according to the geographical location, it has been suggested that more than 51 million school hours are lost each year to dental-related illnesses by school-going children.4 Excluding the indirect and intangible costs, dental caries has also been reported to incur some US$298 billion in direct treatment alone to the global economy, making up a proportionate 4.6% of worldwide health expenditures.5 Current worldwide prevalence rates indicate that 60%-90% of schoolchildren have dental caries,6 but percentages seem to vary across different populations, with some reporting lower figures.7,8 The disease burden in low- and middle-income countries (LMICs), however, is said to be increasing.6 Periodontal disease, including gingivitis in children, has gained prominence,9 with some reports indicating a very high disease burden.10
Other oral conditions prevalent in children can include malocclusion, trauma, halitosis, swellings, and congenital and epithelial lesions of the mouth and maxillofacial region.11,12 The young, school-going age range of 9-16 is of importance because there is a new awareness of the self from adolescence, and this stage also presents a period when there is considerable development of health behaviours, attitudes, and practices.13
The oral health care system in Ghana is still evolving, with more emphasis on oral disease prevention. For a country such as Ghana, it is imperative that children are specifically considered in policies and planning regarding oral health. Understanding the current burden of common oral conditions is therefore necessary to drive and inform national and institutional policy directions. However, there is a paucity of data in the literature in this regard. Though some studies have previously investigated the caries experience in similar populations,8,14 they did not together explore the burden of other common oral conditions. The objective of this study was, therefore, to provide a current picture of the prevalence of common oral conditions in children between the ages of 9 and 16 years.
Methods
Ghana is an emerging economy in West Africa, currently with an estimated population of about 30 million. It is geopolitically divided into 16 regions, with Accra, the capital city in the Greater Accra region, being 1 of the most populous cities in the country. Children 10-16 years of age in Greater Accra were estimated to account for 9.6% of the region's population at the last census.15
This study was a cross-sectional survey among selected Ghanaian public school students between the ages of 9 and 16 years. The study was conducted as part of a screening program carried out in Accra to commemorate the World Oral Health Day in Ghana, in March 2018, an event organized by the Ghana Dental Association and the Health Ministry of the government of Ghana. Sixteen (16) peri-urban public schools across Accra, out of 20 randomly selected public schools, responded to the invitation to participate in the study. Three schools attributed their decline to conflict with their academic calendar, and 1 school reported technical challenges with their means of transport. The sample size of 348 was obtained with the formula: S = (z2 × σ2)/d2, where z is the z value (1.96 for 95% confidence level); d = distance on either side of mean in confidence interval (0.05); and σ = standard deviation (0.476 from an estimated decayed, missing, and filled teeth [DMFT] evaluation of a Ghanaian population).14 Students from all the schools were consecutively selected to participate in the exercise and randomly assigned to the investigators.
Individuals included in the study were current students, aged between 9–16 years, who, on the day of the oral examination, were willing to participate and had consent from their parents or guardians. Nineteen students declined to participate for various reasons.
Background information and medical history data was collected using a pretested semistructured questionnaire with personal interviews. This was followed by a thorough oral examination, using direct visual screening with tongue blades in broad daylight. Examiners, being a team of 8 qualified and certified dental surgeons, were calibrated through a series of intensive training before the study. Interexaminer errors, after the training were within the range of ±1.0 for DMFT measures of randomly selected patients, and the interexaminer correlation was greater than 0.7. During the training and calibration, the examiners were also trained to record data directly onto the entry sheets designed for the study to minimise errors. Patients for calibration were selected from and examined at the University of Ghana Dental School Clinic, Accra. Variables recorded included age (9-12 yrs/13-16 yrs), sex (male/female), and previous dental visit (yes/no). Evidence of the presence of periodontal disease (present/absent), traumatised teeth, oral lesions, neoplasia, cysts, and malocclusion were also recorded for each patient, as well as the DMFT resulting from dental caries.
Only definite teeth cavitations were recorded as dental caries.16 Conditions classified as malocclusion were Class I, II, and III malocclusions, with or without severe crowding, and an anterior open bite. Periodontal disease was defined as the presence of at least 1 of the following: bleeding on brushing (determined by a positive history), inflamed gingiva with or without visible supragingival plaque or calculi, swollen gingiva, receded gingiva, and appreciably mobile permanent teeth.17 All cases of malocclusion, periodontal disease, and neoplasms were verified by on-site orthodontists, periodontists and a maxillofacial surgeon. Anterior tooth traumatic injury was captured as teeth with clinical signs, including fracture, discolouration, and tooth displacement, confirmed by a positive history. Dental caries was considered present through component ‘D’ other than 0 in the DMFT index. Likewise, malocclusion, periodontal disease, neoplasms, and epithelial lesions were considered present with their clinical manifestations and positive history confirmed by the respective specialists.
All variables were entered in Microsoft Excel 2007 and analysed using Stata 14 statistical software (StataCorp.). Analysis included all children who were examined. Background characteristics for all respondents were described, and proportions for variables reported. A Wilcoxon rank-sum test (Mann-Whitney U test) was used to compare the DMFT between subgroups, and binary logistic regression was used to determine the factors associated with the presence of periodontal disease and malocclusion. A χ2 test was also used to compare categorical variables with consequent test of significance assuming a confidence of 95% and an alpha level of 0.05. Fisher exact test was used where applicable for smaller subgroups.
Appropriate referrals were sent to parents of children in need of dental care. Oral hygiene education was also given to all participants. The study was approved by the Ethical Review Board of the College of Health Sciences, University of Ghana, ensuring ethical standards of the Institutional Research Committee and the Helsinki Declaration of 1964 and its later amendments. Consent and assent were obtained from parents and study participants, respectively.
Results
A total of 1137 children met the inclusion criteria. However, 11 students complained of ill health, and an additional 8 were dropped due to inconsistencies with the consent. Finally, 1118 students participated in the study, representing a response rate of 98.3%. This consisted of 37.8% males and 62.2% females (Table 1). With a range of 9 to 16 years, the mean and median ages were 12.8 years (standard deviation = 1.7) and 13 years, respectively.
Table 1.
Background characteristics of respondents.
| Variable | Number (N) | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 423 | 37.8 |
| Female | 695 | 62.2 |
| Age | ||
| 9-12 years | 460 | 41.1 |
| 13-16 years | 658 | 58.9 |
| Previous dental visits | ||
| Yes | 75 | 6.7 |
| No | 1043 | 93.3 |
| Occlusion | ||
| Normal | 992 | 88.7 |
| Malocclusion | 126 | 11.3 |
| Periodontal disease | ||
| Present | 340 | 30.4 |
| Absent | 778 | 69.6 |
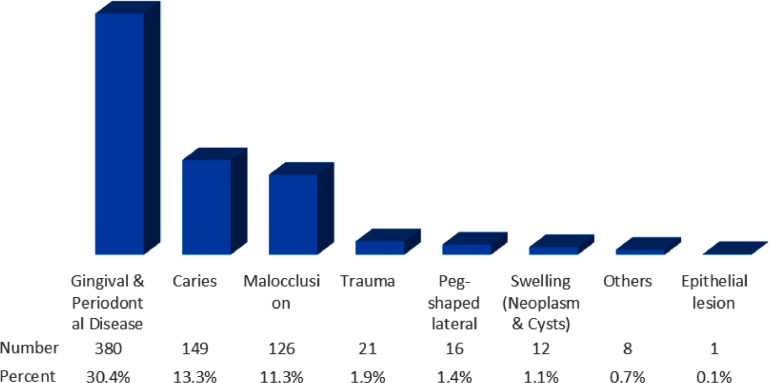
Diseases of the periodontium accounted for the highest number of conditions seen in the mouth. Individuals with gingival and periodontal diseases were more than 2 times the proportion of students with caries (Figure 1). Although 50.3% of the population were clinically free of any oral disease, 21 (1.9%) had evidence of trauma to the anterior teeth, of which only 1 (4.8% of the subpopulation) had undergone treatment. Twelve students were identified with swellings of the maxillofacial region. One hyperpigmented lesion on the labial mucosa was found. Only 1 (8.3%) out of the 12 individuals found to have maxillofacial swellings had previously sought medical consultation or management.
Fig. 1.
Prevalence of common oral conditions.
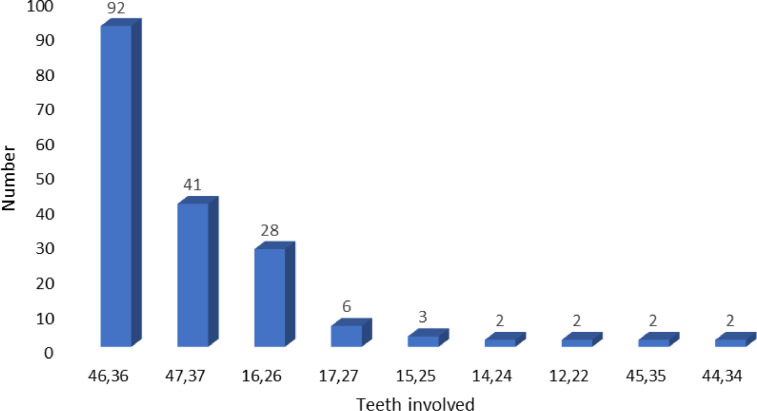
The prevalence of caries was 13.3% and that of periodontal disease was 30.4% (Figure 1). Among all carious permanent teeth, the lower first molars were the most affected. This was followed by the mandibular second molars and maxillary first and second molars, respectively (Figure 2). No anterior teeth were affected by caries.
Fig. 2.
Pattern of carious permanent teeth among adolescents.
In all, common oral conditions were found in 556 participants (49.7%), thus requiring some needed professional care at the time of the examination. Of these, 61.9% were males, and 38.1% were females.
The mean DMFT of the entire population was 0.27 (standard deviation = 0.76), with no observable differences between the subgroups (Table 2). The presence of caries in this study did not change significantly with sex, age variation, periodontal disease, or the presence of malocclusion.
Table 2.
Caries and associated factors among Ghanaian children.
| Variable | Caries, N (%) | X2 (P value) |
Mean DMFT | Mann-Whitney test for DMFT (P value) | OR | CI |
|---|---|---|---|---|---|---|
| Sex | .634 | .994 | ||||
| Female | 90 (13.0) | 0.28 | Ref | |||
| Male | 59 (14.0) | 0.26 | 1.09 | 0.77-1.55 | ||
| Age | .231 | .918 | ||||
| 13-16 years | 81 (12.3) | 0.28 | Ref | |||
| 9-12 years | 68 (14.8) | 0.25 | 1.24 | 0.87-1.75 | ||
| Previous dental visits | .292 | .444 | ||||
| Yes | 7 (9.3) | 0.23 | Ref | |||
| No | 142 (13.6) | 0.28 | 1.43 | 0.64-3.19 | ||
| Occlusion | .291 | .331 | ||||
| Normal | 136 (13.7) | 0.23 | Ref | |||
| Malocclusion | 13 (10.3) | 0.28 | 0.72 | 0.40-1.32 | ||
| Periodontal disease | .747 | .743 | ||||
| Absent | 102 (13.1) | 0.26 | Ref | |||
| Present | 47 (13.8) | 0.28 | 0.94 | 0.65-1.36 |
DMFT = decayed, missing, or filled teeth; OR = odds ratio.
!Fisher exact test used where applicable
Cross-tabulation between periodontal disease and other variables (Table 3) showed that age category and previous dental visits varied significantly for the presence of periodontal disease (respective P- values of .001 and .011). Sex and malocclusion did not, however, show any significant variation with the occurrence of periodontal disease among the study population. The odds of having periodontal disease if one was a child who had never visited the dentist were 2.24 times that of a child who visited the dentist (Table 3).
Table 3.
Periodontal disease and associated factors among Ghanaian children.
| Variable | Number, N (%) | X2 value* | P value | OR | CI |
|---|---|---|---|---|---|
| Sex | 1.342 | .247 | |||
| Female | 120 (17.3) | Ref | |||
| Male | 220 (52.0) | 1.17 | 0.89-1.52 | ||
| Age | 8.883 | .001 | |||
| 13-16 years | 107 (16.3) | Ref | |||
| 9-12 years | 233 (50.6) | 1.81 | 1.38-2.37 | ||
| Previous dental visits | 6.539 | .011 | |||
| No | 328 (31.4) | Ref | |||
| Yes | 12 (16.0) | 2.24 | 1.19-4.22 | ||
| Occlusion | 0.119 | .730 | |||
| Normal | 300 (30.2) | Ref | |||
| Malocclusion | 40 (31.7) | 0.93 | 0.63-1.39 |
OR = odds ratio.
Fisher exact test used where applicable
Again, females were more likely to have a malocclusion compared to males (odds ratio = 1.53; Table 4), while the number of males involved in an anterior traumatic event were 3 times the number of females.
Table 4.
Malocclusion and associated factors among Ghanaian children.
| Variable | Number, N (%) | X2 value* | P value | Crude OR | CI |
|---|---|---|---|---|---|
| Sex | 4.88 | .027 | |||
| Male | 67 (9.6) | Ref | |||
| Female | 59 (14.0) | 1.53 | 1.05-2.21 | ||
| Age | 0.299 | .585 | |||
| 9-12 years | 49 (10.7) | Ref | |||
| 13-16 years | 77 (11.7) | 1.11 | 0.76-1.63 | ||
| Dental visits | 1.799 | .180 | |||
| Previous visit | 12 (16.0) | Ref | |||
| First visit | 114 (10.9) | 1.66 | 0.87-3.19 |
OR = odds ratio.
Fisher exact test used where applicable
Discussion
The aim of this study was to determine the prevalence of common oral conditions among a children 9 to 16 years of age in Accra, Ghana. With a population mean DMFT of 0.27, the prevalence of caries was determined to be 13.4% and that for periodontal disease was 30.4%.
The Sustainable Development Goals (SDG) advocate for ensuring healthy lives and promoting well-being for all, at all ages, with a specific goal to achieve universal health coverage and access to quality essential health care services.18 The oral health of any community, therefore, plays a significant role in the pursuit of this goal. The disease burden of several oral conditions have been widely reported, with variation in percentages, suggesting that it differs among different populations. The WHO published a worldwide caries prevalence of 60%-90% but has been reported that to be 32.6% among a similar age group to what is reported here in India,19 4%-40% in Nigeria,20 and 13% in other studies in sub-Saharan Africa.21 A study done to determine the prevalence of dental caries among 12-year-old schoolchildren in Ghana 30 years ago (1991) established a 13% prevalence.22 Similar to a study 11 years later,8 this survey shows a disease burden of 13.3% among school-going children. Not only do these figures indicate that our population possibly has a comparatively lower prevalence of caries but that the disease burden has remained fairly constant over the past 3 decades. Both conclusions are at variance with a report from a global epidemiological study that suggests higher prevalence and worsening disease burden in LMICs.23 The findings reported here, however favourably compares with studies in Benin and Nigeria.20,21 The mean DMFT of the entire population was 0.27. It was found to be 0.62 among 12-year-olds in India,19 and 0.25 among 12- to 15-year-olds in Nigeria.20 Our observation, however, differed slightly among the different variables. With the assumptions of this study, caries was not found to be associated with sex, age variation, or the presence of malocclusion among the children. Further exploration into specific risk factors is required, while biological and anatomical differences in cariogenesis among different ethnicities and population groups may still be a fertile area for investigation. Though not significant for previous dental visits or periodontal disease, a slightly higher proportion of children with periodontal disease had dental caries in this study.
The term ‘periodontal disease’ refers to a spectrum of pathologies affecting the surrounding structures of the teeth: the gums, periodontal ligament, cementum, and alveolar bone. As was included in our case definition, periodontal disease, depending on the extent, may present as reddening of the gum, bleeding on brushing, recession of the gums loss of bone, tooth mobility’ and tooth loss.24,25 Periodontal disease was reported to have a prevalence of 30% and 90% across different populations in Nigeria.21,25 We, however, found a periodontal disease prevalence of 30.4% among our peri-urban population in Accra, with its presence being associated with the age category and the history of dental visits.
Without measuring the orthodontic treatment need, our study found 11.3% of the population to have a malocclusion. This finding is at variance with results of 34.8%, 47.2%, and 59.4% in Iran, Turkey, and Saudi Arabia, respectively.26, 27, 28 Malocclusion generally describes an abnormal occlusion in which teeth are not in a normal position in relation to adjacent teeth in the same jaw or the opposing teeth when the jaws are closed. Orthodontists, however define it as an appreciable deviation from ideal occlusion,29 therebyreducing subjectivity in determining what is a malocclusion.
There was a 1.9% prevalence of anterior tooth traumatic injury, for which a proportionate number were males. Traumatic dental injury was found to have occurred in 11.4% of a school population in Nigeria,30 18.5% in a 3- to 5-year-old Sudanese population,31 and 9.3% in a 12-year-old Indian population.32 This study, however, reports the prevalence of individuals with evidence of anterior traumatic injury, thus excluding individuals who might have had a traumatic dental injury without necessarily having any sign or symptom, as demonstrated in other studies. Using the methodology reported here, our findings were comparable to a community-based survey in Brazil that reported the prevalence of anterior trauma to permanent teeth as 0.15%.33
The findings reported here highlight an unmet need for oral health care among children in Ghana. For example, the 6.7% of our participants who had previously seen a dentist is disproportionate to the nearly 50% who were found to have at least, one oral condition, and needing professional care. The prevalence rate of caries and periodontal disease also calls for diversification in reducing the burden of oral conditions in Ghanaian children. Although the current dentist-to-population ratio of about 1:70,000 will influence any proposed solution, oral hygiene education needs to be intensified to empower individuals and to improve community health behaviours regarding oral health. Ghana has yet to see a robust oral health policy that would direct the provision of oral health services and its development. Areas of oral health education, promotion, disease prevention, and control require a critical appraisal and input into the national agenda. This also underscores the call by WHO to promote oral health in Africa, addressing the 7 priority oral diseases (dental caries, periodontal diseases, oral cancers, noma, oral manifestations of HIV and AIDS, orofacial trauma, and cleft lip and palate) by packaging and integrating oral health care into primary health care, targeting schools and communities.34
This study investigated only a few risk factors and variables, which is a notable limitation, as is the use of crude clinical parameters and the inclusion of only children who attend public schools. Although the study design itself might limit inference of findings to the general population, this survey provides valuable estimates and information for further studies in this particular setting across several areas within the country and subregion.
Conclusions
The burden of dental caries among children in Accra has not changed in the past 30 years. With dental caries and periodontal disease being common problems among school-going children 9 to 16 years of age in peri-urban Accra, there is need for expansion of efforts to improve access to dental visits, while reducing the burden of common oral conditions in Ghanaian children.
Conflict of interest
None disclosed.
Acknowledgments
Acknowledgements
The authors appreciate the collaboration of the Ghana Dental Association, the Government of Ghana, through Ministry of Health and the Ghana Health Service, as well as the many schoolchildren who participated in the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.World Health Organization (WHO). Oral health. Available from:http://www.who.int/oral_health/en/. Accessed March 24, 2021.
- 2.Kassebaum NJ, Smith AGC, Bernabé E, et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 2017;96(4):380–387. doi: 10.1177/0022034517693566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anil S, Anand PS. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr. 2017;5:157. doi: 10.3389/fped.2017.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson SL, Vann WF, Kotch JB, Pahel BT, Lee JY, Lee JY. Impact of poor oral health on children's school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Listl S, Galloway J, Mossey PA, Marcenes W. Global economic impact of dental diseases. J Dent Res. 2015;94(10):1355–1361. doi: 10.1177/0022034515602879. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO). International statistical classification of diseases and related health problems. Available from:https://books.google.com/books?hl=en&lr=&id=Tw5eAtsatiUC&oi=fnd&pg=PA1&dq=World+Health+Organization.+(2004)+Global+Oral+Health+Data+Bank.+WHO.+Geneva:+WHO.&ots=o3bZfYlJmM&sig=DAZo5zsV2c3qN6nHE4KaVbkinIo. Accessed November 12, 2018.
- 7.Hussaini S, Bendigiri N, Swati I. A study on the dental problems of school children. Int J Community Med Public Health. 2016;3(5):1090–1093. doi: 10.18203/2394-6040.ijcmph20161363. [DOI] [Google Scholar]
- 8.Bruce I, Addo ME, Ndanu T. Oral health status of peri-urban schoolchildren in Accra, Ghana. Int Dent J. 2002;52(4):278–282. doi: 10.1111/j.1875-595x.2002.tb00631.x. http://www.ncbi.nlm.nih.gov/pubmed/12212816 Available from: Accessed April 2, 2017. [DOI] [PubMed] [Google Scholar]
- 9.Al-Ghutaimel H, Riba H, Al-Kahtani S, Al-Duhaimi S. Common periodontal diseases of children and adolescents. Int J Dent. 2014;2014 doi: 10.1155/2014/850674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albandar JM, Brown LJ, Brunelle JA, Löe H. Gingival state and dental calculus in early-onset periodontitis. J Periodontol. 1996;67(10):953–959. doi: 10.1902/jop.1996.67.10.953. [DOI] [PubMed] [Google Scholar]
- 11.Oredugba FA, Akindayomi Y. Oral health status and treatment needs of children and young adults attending a day centre for individuals with special health care needs. BMC Oral Health. 2008;8(1):30. doi: 10.1186/1472-6831-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taiwo AO, Braimah RO, Ibikunle AA, et al. Oral and maxillofacial tumours in children and adolescents: clinicopathologic audit of 75 cases in an academic medical centre, Sokoto, Northwest Nigeria. African J Paediatr Surg. 2017;14(3):37–42. doi: 10.4103/ajps.AJPS_81_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wargo J. The physical school environment: an essential component of a health-promoting school. Available from: https://apps.who.int/iris/bitstream/handle/10665/42683/9241590645.pdf?sequence=1&isAllowed=y&ua=1. Accessed March 24, 2021.
- 14.Ndanu TA, Aryeetey R, Sackeyfio J, Otoo G, Lartey A. Oral hygiene practices and caries prevalence among 9-15 years old Ghanaian school children. J Nutr Heal Sci J Nutr Heal Sci. 2015;2(1) doi: 10.15744/2393-9060.1.404. [DOI] [Google Scholar]
- 15.Ghana Statistical Service. 2010 population and housing census (PHC). Available from: http://www.statsghana.gov.gh/docfiles/2010phc/2010. Accessed 24 March 2021.
- 16.Parasuraman G, Krishna YG, Kaviya M, Jain NA, Rajendran P, Dutta R. A study on the prevalence of dental caries among the school-going children in Tamil Nadu. Int J Community Med Public Health. 2017;4(10):3582–3589. doi: 10.18203/2394-6040.ijcmph20174122. [DOI] [Google Scholar]
- 17.Aranza OT, Talavera Peña I. Prevalence of gingivitis in preschool-age children living on the east side of Mexico City. Bol Med Hosp Infant Mex 2011;68(1):19–23. Available from:https://pdfs.semanticscholar.org/cf80/d2b07f6283879badb0c3ac8be8924c3b65d6.pdf. Accessed March 24, 2021.
- 18.United Nations. Sustainable development goals. Available from:http://www.un.org/sustainabledevelopment/sustainable-development-goals/. Accessed March 24, 2021.
- 19.Shailee F, Sogi G, Sharma K, Nidhi P. Dental caries prevalence and treatment needs among 12- and 15- year old schoolchildren in Shimla city, Himachal Pradesh, India. Indian J Dent Res. 2012;23(5):579. doi: 10.4103/0970-9290.107330. [DOI] [PubMed] [Google Scholar]
- 20.Braimoh OB, Umanah AU, Ilochonwu NA. Caries distribution, prevalence, and treatment needs among 12–15-year-old secondary school students in Port Harcourt, Rivers State, Nigeria. J Dent Surg. 2014;2014:1–6. doi: 10.1155/2014/483760. [DOI] [Google Scholar]
- 21.Tobin AO, Ajayi IO. Common oral conditions and correlates: an oral health survey in Kwara State Nigeria. BMC Res Notes. 2017;10(1):568. doi: 10.1186/s13104-017-2894-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Addo-Yobo C, Williams SA, Curzon MEJ. Dental caries experience in Ghana among 12-year-old urban and rural schoolchildren. Caries Res. 1991;25(4):311–314. doi: 10.1159/000261382. [DOI] [PubMed] [Google Scholar]
- 23.Global DT, Frencken JE, Sharma P, et al. Global epidemiology of dental caries and severe periodontitis – a comprehensive review. J Clin Periodontol. 2017;44:94–105. doi: 10.1111/jcpe.12677. [DOI] [PubMed] [Google Scholar]
- 24.Natto ZS, Aladmawy M, Alasqah M, Papas A. Factors contributing to tooth loss among the elderly: a cross sectional study. Singapore Dent J. 2014;35:17–22. doi: 10.1016/J.SDJ.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Popoola BO, Dosumu EB, Ifesanya JU, Popoola BO, Dosumu EB, Ifesanya JU. Periodontal status and treatment need among adolescents in Ibadan, Southwestern Nigeria. Brazilian J Oral Sci. 2015;14(2):117–121. doi: 10.1590/1677-3225v14n2a04. [DOI] [Google Scholar]
- 26.Gudipaneni RK, Aldahmeshi RF, Patil SR, Alam MK. The prevalence of malocclusion and the need for orthodontic treatment among adolescents in the northern border region of Saudi Arabia: an epidemiological study. BMC Oral Health. 2018;18(1):16. doi: 10.1186/s12903-018-0476-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Int Sch Res Not. 2014;2014:1–5. doi: 10.1155/2014/349793. [DOI] [Google Scholar]
- 28.Laganà G, Masucci C, Fabi F, Bollero P, Cozza P. Prevalence of malocclusions, oral habits and orthodontic treatment need in a 7- to 15-year-old schoolchildren population in Tirana. Prog Orthod. 2013;14(1):12. doi: 10.1186/2196-1042-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davies SJ. Malocclusion – a term in need of dropping or redefinition? Br Dent J. 2007;202(9):519–520. doi: 10.1038/bdj.2007.372. [DOI] [PubMed] [Google Scholar]
- 30.Ogordi PU, Ize-Iyamu IN, Adeniyi EO. Prevalence of traumatic dental injury to the anterior teeth in children attending paramilitary and nonparamilitary schools in Nigeria. Ann Afr Med. 2019;18(2):80–85. doi: 10.4103/aam.aam_27_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sulieman AG, Awooda EM. Prevalence of anterior dental trauma and its associated factors among preschool children aged 3–5 years in Khartoum city, Sudan. Int J Dent. 2018;2018:1–5. doi: 10.1155/2018/2135381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ain TS, Lingesha Telgi R, Sultan S, et al. Prevalence of traumatic dental injuries to anterior teeth of 12-year-old school children in Kashmir, India. Arch Trauma Res. 2016;5(1):e24596. doi: 10.5812/atr.24596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heimer M, Vieira S, Colares V. Prevalence of dental trauma among 6-7-year-old children in the city of Recife, PE, Brazil. Braz J Oral Sci. 2012;11:72–75. [Google Scholar]
- 34.World Health Organization (WHO). Promoting oral health in Africa. Prevention and control of oral diseases and noma as part of essential noncommunicable disease interventions. Available from:https://www.afro.who.int/publications/promoting-oral-health-africa-prevention-and-control-oral-diseases-and-noma-part. Accessed March 24, 2021.