Abstract
The U.S. public health response to coronavirus disease 2019 (COVID-19) has been widely criticized as having downplayed the potential implications COVID-19 could have on one's personal health. Despite the unprecedented threat of COVID-19, many individuals still believed that it was not at all likely that they would become infected. We sought to investigate trends in adults’ perceived susceptibility to COVID-19 over the first year of the pandemic, whether distinct trajectories emerged, and if these trajectories differed by participant socio-demographic characteristics.
This was a longitudinal cohort study with 5 time points of data collection (March 13, 2020–March 3, 2021). Subjects included 627 adults living with ≥1 chronic conditions, who completed a baseline interview and at least one follow-up interview. In addition to collecting relevant socio-demographic characteristics, participants’ perceived susceptibility to COVID-19 across time was assessed and classified into distinct trajectories.
Nearly two-thirds (62.2%) of participants perceived themselves to be highly susceptible to COVID-19 from the onset of the pandemic (“early responders”) and sustained this over a year, a third (29.0%) eventually perceived themselves to be highly susceptible (“late responders”), and 8.8% maintained a low likelihood of susceptibility throughout the pandemic (“non-responders”). In multivariable analyses, compared to White participants, Latinx participants were significantly more likely to be non-responders and report low likelihood of perceived susceptibility (Risk Ratio [RR]: 3.46; 95% confidence interval: 1.19, 10.1), as were Black participants (RR: 5.49; 95% confidence interval: 2.19, 13.8).
A year into the COVID-19 pandemic, 1 out of 11 participants persistently did not think they might be susceptible and potentially infected. Future studies are needed to understand reasons why certain individuals, particularly those of racial/ethnic minorities, did not perceive themselves at risk for infection.
Keywords: Chicago, comorbidity, coronavirus disease 2019, coronavirus disease 2019 perceived susceptibility, socio-demographic health disparities, trajectories
1. Introduction
The severe acute respiratory syndrome coronavirus 2 and resultant coronavirus disease 2019 (COVID-19) have evolved into an unprecedented pandemic, requiring communities to mobilize quickly to realize the threat and take action to prevent infection and spread.[1] However, due to a public health response in the United States that has been widely recognized as misguided and fraught with misinformation, many adults may have been slow to realize the potential implications this coronavirus could have on their or a loved one's personal health.[2]
At the earliest onset of COVID-19's presence throughout the U.S., the COVID-19 & chronic conditions (C3) study was launched to investigate the knowledge, attitudes and actions related to COVID-19 among a cohort of middle age and older adults with one or more chronic conditions. We previously reported that in early March 2020, despite cases rapidly accelerating, a quarter of C3 participants reported believing that it was not at all likely that they would eventually get sick with the illness.[3]
As a follow-up, we sought to longitudinally examine the yearlong trend of adults’ perceived susceptibility to COVID-19, and determine whether some individuals followed similar progressions and could thereby be classified into distinct trajectories. Furthermore, we explored whether the trajectories differed by participant socio-demographic characteristics.
2. Methods
2.1. Study design
The C3 study is an on-going longitudinal, telephone-based survey that began at the onset of the COVID-19 pandemic. The initial survey was conducted from March 13 to 20, 2020 during the very first week of the outbreak in Chicago, Illinois. Over the course of a year, four subsequent study interviews, referred to as waves, occurred (Wave 2: March 27–April 3, Wave 3: May 1–May 20, Wave 4: July 15–August 18, Wave 5: November 30–March 3, 2021). The Illinois stay-at-home order began on March 20th, immediately after Wave 1 was completed. Chicago experienced a peak in COVID-19 cases in May, which resulted in an extension of the order through May 29, 2020. Waves 2 and 3 occurred during this period. Starting June 4, Chicago reached a plateau phase with the first surge, where the 7 days rolling average positivity rate was <10% and remained through Wave 4 data collection. Finally, during Wave 5, Chicago once again reached a peak in COVID-19 cases, where the positivity rate topped 13% during mid-November.[4] The Northwestern Institutional review board approved all study procedures.
2.2. Study participants
Eligibility criteria included participants actively enrolled in one of five ongoing, National Institutes of Health (NIH)-funded research studies managed by our research team. All parent studies excluded individuals with severe hearing, vision and cognitive impairments due to concerns regarding the informed consent process. Four of the five research studies included only English-speaking subjects, while one study included Spanish-speaking subjects as well. The five parent studies have been previously described in our earlier publications, including full inclusion and exclusion criteria. These studies are comprised of mostly older adults with multiple chronic conditions. All participants have received medical care at one of five academic internal medicine practices or two federally qualified health centers throughout the greater Chicago metropolitan area.[3,5,6]
Trained research coordinators recruited participants from their parent studies to participate in a brief phone questionnaire pertaining to COVID-19. Survey data was collected using Research Election Data Capture (REDCap). Each survey averaged 20 to 40 minutes, and participants were compensated with a $10 to $15 gift card for their time, depending on the wave. A total of 673 participants were enrolled in the study and completed a Wave 1 interview. Of those enrolled, 626 participants completed a Wave 2 interview (93.3% cooperation rate), 601 completed a Wave 3 interview (89.7%), 558 completed a Wave 4 interview (82.9%), and 544 completed a Wave 5 interview (80.8%). For the purposes of this analysis, we included 627 participants who completed both their baseline survey, in addition to at least one follow-up survey.
2.3. Covariates and study outcomes
At all five waves, participants were surveyed about their perceived susceptibility to COVID-19, asking if they thought they would get sick from coronavirus (not at all, it's possible, I probably will, I definitely will). This outcome measure was dichotomized (not at all vs. it's possible, I probably will, I definitely will) to distinguish between participants who had any level of perceived susceptibly versus no susceptibility (yes/no).
Across all five NIH parent studies there was uniform data collection of participant demographics (age, sex, race/ethnicity, and language proficiency), socio-economic status (income and employment status), and self-reported number of chronic conditions. A single item captured participant self-reported overall health (excellent, very good, good, fair, and poor). All studies measured health literacy: four used the newest vital sign, and one used the validated brief health literacy screen single-item question, “How confident are you filling out medical forms by yourself?”’ Research has shown that the classifications from these instruments are highly correlated.[7]
2.4. Statistical methods
Descriptive statistics (means with standard deviations and percent frequencies) were calculated for all participant characteristics and survey responses. We then identified groups of individuals following similar progressions of perceived susceptibility to COVID-19 over multiple waves and classified them into trajectory groups using the traj command in Stata/SE, version 15 (StataCorp, College Station, TX, US).[8] This method estimates discrete mixture models on longitudinal data, in our case assuming a Bernoulli distribution (logistic model) for the dichotomous perceived susceptibility variable. We used the Bayesian information criterion to determine the number of discrete trajectories in the data. Participants were assigned to a trajectory based on posterior probabilities of belonging to each group.[9] Associations between participant characteristics and their assigned trajectory group were examined in bivariate analyses using chi-square tests. A multivariable Poisson model was used to estimate relative risks (with 95% confidence intervals (CIs)) of following a certain trajectory.[10] Models adjusted for potential confounders (age, gender, race, income, health literacy, employment status, and primary care setting), as well as parent study. All statistical analyses were performed using Stata/SE, version 15 (StataCorp).
3. Results
Table 1 provides a summary of participant characteristics. The average age of participants was 63 years (mean: 62.8 standard deviation: 10.9). The majority were female (60.8%), 21.5% identified as Latinx, and 30.7% identified as Black. Nearly a third were living below the federal poverty level (28.8%) and 26.5% were working for pay. The majority of participants had three or more chronic conditions (63.0%) and a total of 22.3% and 22.8% had low or marginal health literacy, respectively.
Table 1.
Participant characteristics.
| Variable | Summary valueN = 627 |
| Age, M (SD) | 62.8 (10.9) |
| Age group, % | |
| <60 | 34.8 |
| 60–69 | 37.2 |
| ≥70 | 28.1 |
| Female, % | 60.8 |
| Race, % | |
| Latinx | 21.5 |
| White | 47.8 |
| Black | 30.7 |
| Limited English proficiency, % | 10.9 |
| Living below poverty level, % | 28.8 |
| Employment status, % | |
| Working for pay | 26.5 |
| Not working (retired/unemployed) | 73.5 |
| Health literacy, % | |
| Low | 22.3 |
| Marginal | 22.8 |
| Adequate | 54.9 |
| Number of chronic conditions, % | |
| 1 | 21.1 |
| 2 | 16.0 |
| 3 or more | 63.0 |
| Self-reported overall health, % | |
| Excellent | 8.3 |
| Very good | 28.7 |
| Good | 39.7 |
| Fair | 19.8 |
| Poor | 3.5 |
| Primary care setting, % | |
| AMC | 70.2 |
| FQHC | 29.8 |
| Parent study, % | |
| Study 1 | 18.8 |
| Study 2 | 22.8 |
| Study 3 | 32.1 |
| Study 4 | 6.1 |
| Study 5 | 20.3 |
AMC = Academic Medical Center, FQHC = Federally Qualified Health Center
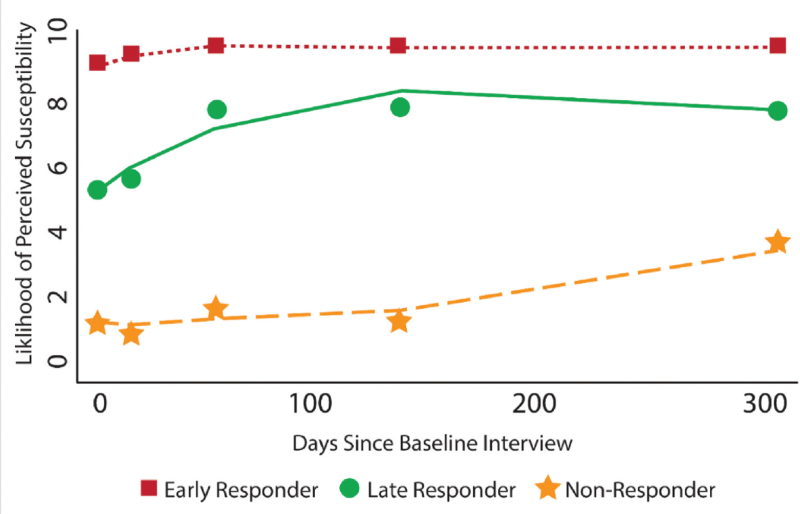
Participant responses varied across waves when asked if they thought they would get sick from coronavirus. Table S1, Supplemental Digital Content shows the full set of categorical responses. When dichotomized, 24.9% of participants had no perceived susceptibility to COVID-19 at Wave 1. This number continued to decline across the next four waves (22.5%, 13.8%, 13.5%, and 11.5%, respectively). When modeling the trajectory of perceived susceptibility to COVID-19, three distinct groups emerged, as shown in Figure 1. The first group (“early responders”) made up 62.2% of the sample and included participants who perceived themselves to be highly susceptible to COVID-19 from the onset of the pandemic. The second group (“late responders”) made up 29.0% of the sample and included participants who eventually perceived themselves to be highly susceptible. Finally, the third group (“non-responders”) made up 8.8% of the sample and included participants maintained a low likelihood of susceptibility throughout the pandemic.
Figure 1.
Trajectories of perceived susceptibility to COVID-19.
In bivariate analyses, trajectory group was associated with several participant characteristics (Table 2). A greater proportion of early responders were White (57.5%) compared to Latinx (20.2%) or Black adults (22.3%), whereas non-responders were more likely to be Black (58.5%) than Latinx (28.3%) or White (13.2%) (P < .001). Additionally, non-responders were more likely than early or late responders to live below the poverty level (41.8% vs. 22.0% and 39.4%; P < .001), to receive medical care at federally qualified health centers (45.5% vs. 26.4% and 32.4%; P = .01), to be unemployed or retired (79.6% vs. 69.8% and 79.5%; P = .03), and to have limited health literacy (47.3% vs. 17.2% and 25.8%; P < .001).
Table 2.
Bivariate analysis by trajectory group (N = 627).
| Variable | Early responder(n = 390) | Late responder(n = 182) | Non-responder(n = 55) | P |
| Age group, % | ||||
| <60 | 36.2 | 33.0 | 30.9 | |
| 60–69 | 36.9 | 35.7 | 43.6 | .67 |
| ≥70 | 26.9 | 31.3 | 25.5 | |
| Gender, % | ||||
| Female | 57.7 | 67.0 | 61.8 | .10 |
| Male | 42.3 | 33.0 | 38.2 | |
| Race, % | ||||
| Latinx | 20.2 | 22.2 | 28.3 | |
| White | 57.5 | 37.4 | 13.2 | <.001 |
| Black | 22.3 | 40.4 | 58.5 | |
| Limited English proficiency, % | ||||
| Yes | 9.5 | 12.1 | 16.4 | .25 |
| No | 90.5 | 87.9 | 83.6 | |
| Living below poverty level, % | ||||
| Yes | 22.0 | 39.4 | 41.8 | <.001 |
| No | 78.0 | 60.6 | 58.2 | |
| Employment status, % | ||||
| Working for pay | 30.2 | 20.5 | 20.4 | .03 |
| Not working | 69.8 | 79.5 | 79.6 | |
| Health literacy, % | ||||
| Low | 17.2 | 25.8 | 47.3 | |
| Marginal | 19.0 | 31.3 | 21.8 | <.001 |
| Adequate | 63.8 | 42.9 | 30.9 | |
| Number of chronic conditions, % | ||||
| 1–2 | 37.2 | 38.5 | 30.9 | .59 |
| 3 or more | 62.8 | 61.5 | 69.1 | |
| Self-reported health, % | ||||
| Good – excellent | 77.7 | 73.6 | 80.0 | .47 |
| Fair – poor | 22.3 | 26.4 | 20.0 | |
| Primary care setting, % | ||||
| AMC | 73.6 | 67.6 | 54.6 | .01 |
| FQHC | 26.4 | 32.4 | 45.4 | |
| Parent study, % | ||||
| Study 1 | 20.5 | 15.4 | 18.2 | |
| Study 2 | 23.3 | 22.0 | 21.8 | |
| Study 3 | 30.0 | 36.3 | 32.7 | .88 |
| Study 4 | 6.2 | 5.5 | 7.3 | |
| Study 5 | 20.0 | 20.9 | 20.0 |
AMC = Academic Medical Center, FQHC = Federally Qualified Health Center
Bolded values are significant at the P < 0.05 level.
In order to better understand those participants who maintained a low likelihood of susceptibility to COVID-19 throughout the pandemic, the early responders and late responders were combined and compared to the non-responders. In multivariable analyses adjusting for age, gender, race, income, health literacy, employment status, primary care setting, and parent study (Table 3), compared to White participants, Latinx participants were significantly more likely to be non-responders (Risk Ratio [RR]: 3.46; 95% CI: 1.19, 10.1), as were Black participants (RR: 5.49; 95% CI: 2.19, 13.8).
Table 3.
Multivariable analysis modeling non-responders (N = 627).
| Non-responder | ||
| Variable | RR (95% CI) | P |
| Age group, % | ||
| <60 | REF | – |
| 60–69 | 1.49 (0.74, 2.99) | .27 |
| ≥70 | 1.49 (0.62, 3.59) | .38 |
| Gender, % | ||
| Male | REF | – |
| Female | 0.93 (0.50, 1.71) | .80 |
| Race, % | ||
| Latinx | 3.46 (1.19, 10.1) | .02 |
| White | REF | – |
| Black | 5.49 (2.19, 13.8) | <.001 |
| Living below poverty level, % | ||
| No | REF | – |
| Yes | 1.01 (0.53, 1.96) | .97 |
| Health literacy, % | ||
| Low | 1.95 (0.90, 4.21) | .09 |
| Marginal | 1.18 (0.52, 2.66) | .69 |
| Adequate | REF | – |
| Employment status | ||
| Not working | REF | |
| Working for pay | 0.96 (0.47, 1.95) | .91 |
| Primary care setting, % | ||
| AMC | REF | – |
| FQHC | 2.33 (0.72, 7.58) | .16 |
| Parent study, % | ||
| Study 1 | REF | – |
| Study 2 | 0.26 (0.07, 1.00) | .05 |
| Study 3 | 0.31 (0.08, 1.18) | .09 |
| Study 4 | 1.17 (0.27, 5.05) | .83 |
| Study 5 | 0.52 (0.20, 1.35) | .18 |
Bolded values are significant at the P < 0.05 level.
4. Discussion
Among this sample of middle age and older adults with at least one chronic condition, we identified three distinct groups related to perceived susceptibility to COVID-19 over the first year of the pandemic. These trajectories included those who always felt they were vulnerable to the virus, those who developed a belief of susceptibility over time, and those who have not felt vulnerable throughout the pandemic. While the majority of individuals recognized their potential to become infected by COVID-19, 1 out of 11 participants persistently did not recognize the threat. Given the entire C3 sample is considered at highest risk for adverse outcomes if infected, this is a concerning prevalence. Nonetheless, these findings are understandable, given the inconsistent messaging and the amount of misinformation surrounding the pandemic.
Our finding of disparities by race and ethnicity with regard to perceived susceptibility is in line with findings from a previous study by Scarinci et al,[11] One possible explanation could be that Black and Latinx adults in our sample did not believe they were going to become infected with COVID-19 because they were taking the necessary public health actions to protect themselves and others. This includes social distancing, wearing a mask, and towards the latter end of data collection, even vaccination. All of these actions might have given confidence to individuals that they could avoid infection. Another explanation, presented by Plough et al, suggested inadequate knowledge of perceived risk of COVID-19 might drive these inequities.[12] However, our team has previously published findings from this cohort that did not find evidence of racial or ethnic disparities in COVID-related knowledge.[3]
Prior research also has posited that cultural and/or spiritual differences, not assessed in our investigation, might explain differences in how one perceives an imminent health threat and an ability to influence the outcome. Similarly, Scarinci et al suggested that disparities in perceived vulnerability to COVID-19 might be driven by a sense of fatalism caused by longstanding mistrust in the government.[11] It is possible that longstanding inequalities in socioeconomic status and life circumstances, racism, and mistrust in government might lead to a lost sense of ability to protect oneself from the coronavirus. Given that communities of color have been disproportionately affected by the pandemic in terms of both rates of infection and deaths, especially in Chicago, this could in part explain our findings.[13,14] Additional qualitative studies are warranted to better understand these results.
There are certain limitations that should be noted. This study was comprised of participants from NIH-funded research that took place in one large U.S. city. Therefore, these findings may have limited generalizability, specifically for younger adults with no pre-existing conditions or those in rural settings. However, our sample was well characterized in terms of demographic and psychosocial factors. Additionally, one of the parent studies (chronic obstructive pulmonary disease) measured health literacy using the validated brief health literacy screen single item, rather than the Newest Vital Sign. However, sensitivity analyses excluding them from the analysis indicated that results were similar (results not reported). Finally, this analysis studied perceived susceptibility to COVID-19 using a single survey item that may or may not have had implications on any pandemic-related behaviors or outcomes.
Future qualitative studies might better elucidate the reasons why certain individuals, in particular those of racial/ethnic minorities, did not perceive themselves to be susceptible to the global threat of COVID-19, even as the pandemic progressed and racial disparities in infection and morbidity/mortality emerged. The pandemic has occurred during parallel, historical political and social movements in the U.S. that might have also influenced how one might perceive a public health threat in lieu of other threats of equal or even greater perceived significance. The link between beliefs about the coronavirus and public health actions and health outcomes should also be examined to further understand the ramifications of not acknowledging the personal risk of COVID-19.
Author contributions
Conceptualization: Guisselle Wismer, Michael Wolf, Rebecca Lovett, Stacy Bailey
Data curation: Laura Curtis, Rebecca Lovett
Formal analysis: Laura Curtis, Lauren Opsasnick, Mary Kwasny, Rachel O’Conor
Funding acquisition: Michael Wolf, Stacy Bailey
Investigation: Laura Curtis, Michael Wolf, Stacy Bailey
Methodology: Guisselle Wismer, Laura Curtis, Lauren Opsasnick, Michael Wolf, Rachel O’Conor, Stacy Bailey
Project administration: Andrea Zuleta, Guisselle Wismer, Julia Benavente, Michael Wolf, Morgan Eifler, Rachel O’Conor, Stacy Bailey
Resources: Guisselle Wismer, Julia Benavente, Michael Wolf
Software: Lauren Opsasnick
Supervision: Laura Curtis, Lauren Opsasnick
Visualization: Guisselle Wismer, Julia Benavente, Stacy Bailey
Writing – original draft: Lauren Opsasnick
Writing – review & editing: Andrea Zuleta, Guisselle Wismer, Julia Benavente, Laura Curtis, Lauren Opsasnick, Mary Kwasny, Michael Wolf, Morgan Eifler, Rachel O’Conor, Rebecca Lovett, Stacy Bailey
Supplementary Material
Footnotes
Abbreviations: C3 = COVID-19 & chronic conditions study, CI = confidence interval, COVID-19 = coronavirus disease 2019, NIH = National Institute of Health, REDCap = Research Election Data Capture, RR = Risk Ratio.
How to cite this article: Opsasnick LA, Curtis LM, Kwasny MJ, O’Conor R, Wismer GA, Benavente JY, Lovett RM, Eifler MR, Zuleta AM, Bailey SC, Wolf MS. Trajectories of perceived susceptibility to COVID-19 over a year: the COVID-19 & chronic conditions (C3) cohort study. Medicine. 2022;101:24(e29376).
Data is supported from the following National Institute of Health-sponsored studies: “Health Literacy and Cognitive Function Among Older Adults” (R01 AG030611), “Self-Management Behaviors among COPD patients with Multimorbitidy” (R01 HL126508), “A Universal Medication Schedule to Promote Adherence to Complex Drug Regimens” (R01 AG046352), “Transplant Regimen Adherence for Kidney Recipients by Engaging Information Technologies” (R01 DK110172), “EHR-Based Universal Medication Schedule to Improve Adherence to Complex Regimens” (R01 NR015444), and “COVID-19 Supplement to LitCog IV: Health Literacy and Cognitive Function Among Older Adults” (3R01 AG030611-13S1). This work is also supported by The Claude D. Pepper Older Americans Independence Center at Northwestern University (P30 AG059988). Data used with permission from the PIs.
MSW reports grants from the NIH during the conduct of the study; grants from Merck, the Gordon and Betty Moore Foundation, the NIH, and Eli Lilly outside the submitted work; and personal fees from Sanofi, Pfizer, and Luto outside the submitted work. SCB reports grants from the NIH during the conduct of the study; grants from Merck, the NIH, and Eli Lilly outside the submitted work; grants and personal fees from the Gordon and Betty Moore Foundation outside the submitted work; and personal fees from Sanofi, Pfizer, and Luto outside the submitted work. LAO, LMC, MJK, RO, GAW, JYB, RML, MRE, and AMZ have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
References
- [1].World Health Organization. Responding to community spread of COVID-19: interim guidance, 7 March 2020. 2020. [Google Scholar]
- [2].Agley J, Xiao Y. Misinformation about COVID-19: evidence for differential latent profiles and a strong association with trust in science. BMC Public Health 2021;21:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wolf MS, Serper M, Opsasnick L, et al. Awareness attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the U.S. outbreak: a cross-sectional survey. Ann Intern Med 2020;173:100–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].City of Chicago. COVID-19: Latest, data. 2020. [Google Scholar]
- [5].Bailey SC, Serper M, Opsasnick L, et al. Changes in COVID-19 knowledge, beliefs behaviors, and preparedness among high-risk adults from the onset to the acceleration phase of the US outbreak. J Gen Internal Med 2020;35:3285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].O’Conor R, Opsasnick L, Benavente JY, et al. Knowledge and behaviors of adults with underlying health conditions during the onset of the COVID-19 U.S outbreak: the Chicago COVID-19 comorbidities survey. J Community Health 2020;45:1149–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Stagliano V, Wallace LA. Brief health literacy screening items predict newest vital sign scores. J Am Board Fam Med 2013;26:558–65. [DOI] [PubMed] [Google Scholar]
- [8].Jones B, Nagin D. A note on a Stata plugin for estimating group-based trajectory models. Sociol Methods Res 2013;42:608–13. [Google Scholar]
- [9].Jones B, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 2001;29:374–93. [Google Scholar]
- [10].Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–6. [DOI] [PubMed] [Google Scholar]
- [11].Scarinci IC, Pandya VN, Kim YI, et al. Factors associated with perceived susceptibility to COVID-19 among urban and rural adults in Alabama. J Community Health 2021;46:932–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Plough A, Bristow B, Fielding J, Caldwell S, Khan S. Pandemics and health equity: lessons learned from the H1N1 response in Los Angeles County. J Public Health Manag Pract 2011;17:20–7. [DOI] [PubMed] [Google Scholar]
- [13].Jimenez T, Restar A, Helm PJ, Cross RI, Barath D, Arndt J. Fatalism in the context of COVID-19: perceiving coronavirus as a death sentence predicts reluctance to perform recommended preventive behaviors. SSM Popul Health 2020;11:100615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Akesson J, Ashworth-Hayes S, Hahn R, et al. Fatalism, beliefs, and behaviors during the COVID-19 pandemic 2020;27245.NBER Working Papers. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.