Abstract
Purpose:
Within the context of local increases in US heart disease death rates, we estimated when increasing heart disease death rates began by county among adults aged 35–64 years and characterized geographic variation.
Methods:
We applied Bayesian spatiotemporal models to vital statistics data to estimate the timing (i.e., the year) of increasing county-level heart disease death rates during 1999–2019 among adults aged 35–64 years. To examine geographic variation, we stratified results by US Census region and urban-rural classification.
Results:
The onset of increasing heart disease death rates among adults aged 35–64 years spanned the two-decade study period from 1999 to 2019. Overall, 43.5% (95% CI: 41.3, 45.6) of counties began increasing before 2011, with early increases more prevalent outside of the most urban counties and outside of the Northeast. Roughly one-in-five (18.4% [95% CI: 15.6, 20.7]) counties continued to decline throughout the study period.
Conclusions:
This variation suggests that factors associated with these geographic classifications may be critical in establishing the timing of changing trends in heart disease death rates. These results reinforce the importance of spatiotemporal surveillance in the early identification of adverse trends and in informing opportunities for tailored policies and programs.
Keywords: Heart disease, Vital statistics, Geography, Mortality
Introduction
Heart disease is the leading cause of death in the United States [1]. Nationally, death rates declined dramatically from the 1960s through the early 2000s, with marked geographic variation in the timing of the onset of these declines [2–4]. Declines began in the 1950s in large metropolitan areas and in states in the Northeast and Pacific coast before extending to the rest of the country throughout the 1960s and early 1970s [4, 5].
However, since 2011, national declines in heart disease death rates have stagnated, with some demographic groups and many counties experiencing increasing death rates [6–10]. Unlike the historic geographic pattern in which the southern US experienced the greatest concentrations of higher heart disease death rates and weaker declines, [9–12] increases since 2011 have been observed in counties across the country, with a higher prevalence of increasing death rates in smaller cities and rural counties [13]. These increases have been especially prevalent among adults aged 35–64 years [10, 12, 14, 15]. Deaths among this age group are especially concerning as they are largely preventable [9, 15]. Consequently, these working age adults represent a key population for public health programs and clinical interventions geared toward the primary and secondary prevention of heart disease [9].
Prior county-level studies of these recent increases in heart disease death rates have used a fixed initial year for the timing of the increases (i.e., the year 2011) based on the year of onset of national stagnation [10, 12, 14]. Geographic variation in when these recent county-level increases began has not been studied. However, as previously observed with the historic onset of declines, examining the timing of changing trends can reveal geographic and temporal variation that may be masked by national data. Characterizing the timing of these local changes may then provide key data for cardiovascular disease surveillance by better characterizing those places that first experienced adverse trends. These additional data may then inform policies and programs to better respond to these adverse trends within specific communities. Therefore, to describe this geographic variation, this study estimated the timing of onset of increasing heart disease death rates by US county during 1999–2019 among US adults aged 35–64 years and characterized geographic variation in this timing by US Census region and urban-rural classification.
Methods
Data sources
We obtained unsuppressed annual heart disease death counts for ages 35–64 by county of residence for 1999 through 2019 from the National Vital Statistics System of the National Center for Health Statistics (NCHS). Although vital statistics data are available through 2020, we excluded 2020 from this analyses due to increases in heart disease mortality associated with the SARS-CoV-2 pandemic [16]. Heart disease deaths were defined as those with an underlying cause of death listed as ICD-9 codes 390–398, 402, and 404–429, and ICD-10 codes I00–I09, 111, 113, and 120–151. We used NCHS bridged-race estimates for annual county-level populations [17].
The unit of analysis was the county (or county equivalent). Given changes in county definitions during the study period (e.g., the creation of new counties), a single set of 3136 counties based on the most recent county definitions was used for the entire study period.
Estimating heart disease death rates
We estimated annual county-level heart disease death rates for ages 35–64 for the years 1999 through 2019 using a statistical model that produces precise, reliable rates, even in the presence of small numbers of deaths and populations [18, 19]. Specifically, we used a previously published Bayesian conditional autoregressive model that has been used extensively to generate county-level estimates of cardiovascular disease mortality [10–12, 14, 20, 21]. This model is based on the Besag-York-Mollié conditional autoregressive model for spatially-referenced count data and incorporates correlation across space, time, and age group [21, 22]. We fit this model with a Markov chain Monte Carlo (MCMC) algorithm using user-developed code in the R programming language [23]. For each county, we estimated annual death rates as the medians of the posterior distributions defined by the MCMC iterations. Death rates were age-standardized to the 2010 US population using 10-year age groups.
More specifically, we modeled Yikt, the number of deaths in county i and age group k during year t from population nikt using a Poisson distribution of the form Yikt ~ Pois(nikt λikt), where λikt is the death rate. To model λikt, we assume , where βkt is a random intercept for each group for each year with a vague N(0,100) prior, Zikt is a spatiotemporal random effect that incorporates correlation between age groups, and is a variance parameter with a weakly informative gamma prior [24]. Our models accounted for correlation across time, space, and age group by modeling the spatiotemporal random effect (Zikt) using the multivariate space-time conditional autoregressive (MST-CAR) model based on the multivariate CAR model of Gelfand and Vounatsou [25]. Spatial correlation of the random effect for each county is defined by queen contiguity. Similarly, temporal correlation uses an approach similar to a standard autoregressive order 1 (AR[1]) model with a beta prior. Finally, correlations between age groups were estimated via an unstructured covariance matrix with an inverse Wishart prior [24]. We ran the MCMC algorithm with four chains for 6000 iterations, diagnosing convergence via trace plots for many model parameters and discarding the first 3000 iterations as burn-in.
Estimating the timing of the onset of increasing heart disease death rates
To estimate the timing of the onset of increasing heart disease death rates, we first divided the 21-year study period into seven consecutive three-year intervals (1999–2001, 2002–2004, 2005–2007, 2008–2010, 2011–2013, 2014–2016, and 2017–2019). By identifying the timing of the onset of increases using these three-year intervals instead of a single year, we balanced the granularity of the timing with the precision of the estimated interval.
For each county, we then defined the time of onset of increasing death rates as the interval with the highest probability of including the minimum rate. Rates in years before and after the minimum rate must, on average, be decreasing and increasing, respectively. Therefore, the interval that includes the minimum rate represents the transition from a period of declining death rates to a period of increasing or plateauing death rates. We calculated the probability that the interval included the minimum rate using the MCMC samples from the posterior distributions of heart disease death rates. For each county, we calculated the proportion of samples within each of the seven consecutive three-year intervals that included the county’s minimum rate. We then assigned the interval with the highest posterior probability (i.e., most common interval across the MCMC samples) as the interval during which increases began.
Other methods of estimating the timing of changes in trends (e.g., joinpoint regression) are not able to detect changes in trends based on small numbers of events, limiting the ability to make comparison across geographic units with vastly different populations [26]. Our use of the posterior distributions enabled the detection of changes in trends even for counties with small numbers of events or small populations. Additionally, by using the posterior distributions of the death rates, this method accounted for the precision of the underlying rates and was, therefore, more robust than simply selecting the interval that contained the lowest estimated rate.
To verify that the interval containing the minimum rate reflected a transition from decreasing rates to increasing rates, for each county we also calculated the percent change before (from 1999 to the interval midpoint) and after (from the interval midpoint to 2019) the interval of onset of increasing death rates. We calculated percent change as the difference between the later and earlier rate, divided by the earlier rate. Counties with onset of increases in the first interval (n = 134) were excluded from percent change calculations before the interval of onset; those with increases in the last interval (n = 659) were excluded from percent change calculations after the interval of onset. We performed this calculation using MCMC samples from the posterior distributions of death rates. By using the entire distribution of the rate estimate (instead of only using the point estimate), percent change calculations accounted for the precision of the underlying rates.
Onset of increasing heart disease death rates relative to the national change in trend
To examine onset of increasing heart disease death rates relative to the national change in trend in 2011 [6–8], we grouped the three-year intervals into three categories. The first category represented counties with increases that began prior to the national change in trend and included all three-year intervals prior to 2011. The second category included counties with increases that began after 2011 but before the final interval. The third category included counties that did not experience increasing death rates (i.e., those counties with lowest rates in the final interval). We then used the posterior distributions of the assigned categories to calculate the percent of counties and 95% credible intervals (95% CI) within each of these categories. By using this distribution, our percentages account for uncertainty in the underlying assignment of the category.
Geographic variation
To examine geographic variation in the onset of increasing death rates, we first mapped the interval of onset. We also stratified our results on two variables that further describe the geographic patterns: region and urban-rural classification. We defined regions as the four US Census regions (Northeast, Midwest, South, West). For urban-rural classification, we used the 2006 National Center for Health Statistics urban-rural classification scheme for counties [27]. We selected this version of the classification (rather than the 2013 version) because it better represented the classification at the beginning of the study period.
Inclusion criteria
For a county to be included in this analysis, we required that the estimated heart disease death rates were reliable (i.e., the credible interval width was less than the point estimate) and the population was greater than 100 for each year (1999–2019). These requirements ensured that we only reported reliable heart disease death rates in sufficiently large populations and that the same set of counties (n = 3116) was used for all years of the study period.
Results
Distributions of the onset of increasing heart disease death rates
Among 3116 included counties, the onset of increasing heart disease death rates among adults aged 35–64 years spanned the two-decade study period from 1999 through 2019 (Table 1). Overall, 43.5% (95% CI: 41.3, 45.6) of counties began increasing prior to the national change in trend in 2011. Geographically, earlier increases were concentrated in a band of counties from Oklahoma through Iowa and Tennessee (Fig. 1). Later increases were more widely distributed across the country.
Table 1.
Distributions of county-level heart disease death rates and trends by interval of onset of increasing heart disease death rates
| Interval of onset of increasing heart disease death rates* | Number of counties with onset of increases during this interval (%) | Median death rate at interval midpoint (10th, 90th percentiles) | Median total percent change before interval midpoint (10th, 90th percentiles) | Median total percent change after interval midpoint (10th, 90th percentiles) |
|---|---|---|---|---|
| 1999–2001 | 134 (4.3) | 145.3 (89.0, 208.2) | N/A | 14.2 (−1.1, 38.3) |
| 2002–2004 | 70 (2.2) | 127.0 (77.4, 181.5) | −5.1 (−13.6, 0.5) | 12.7 (−2.0, 30.0) |
| 2005–2007 | 373 (12.0) | 118.6 (72.3, 177.8) | −13.2 (−24.6, −3.5) | 16.7 (3.0, 32.7) |
| 2008–2010 | 668 (21.4) | 102.8 (70.8, 160.1) | −21.7 (−32.2, −9.6) | 12.3 (2.7, 26.6) |
| 2011–2013 | 926 (29.7) | 90.9 (58.6, 150.8) | −25.8 (−37.8, −12.9) | 8.6 (1.1, 19.6) |
| 2014–2016 | 286 (9.2) | 81.2 (53.1, 129.9) | −30.1 (−41.0, −17.0) | 5.4 (−0.7, 13.6) |
| No increase† | 659 (21.1) | 94.5 (60.2, 165.8) | −26.3 (−39.9, −10.7) | N/A |
Interval of onset of increasing heart disease death rates defined as the interval with the highest probability of including the lowest death rate during 1999–2019.
Counties in this category had lowest heart disease death rates in the last interval (2017–2019).
Fig. 1.
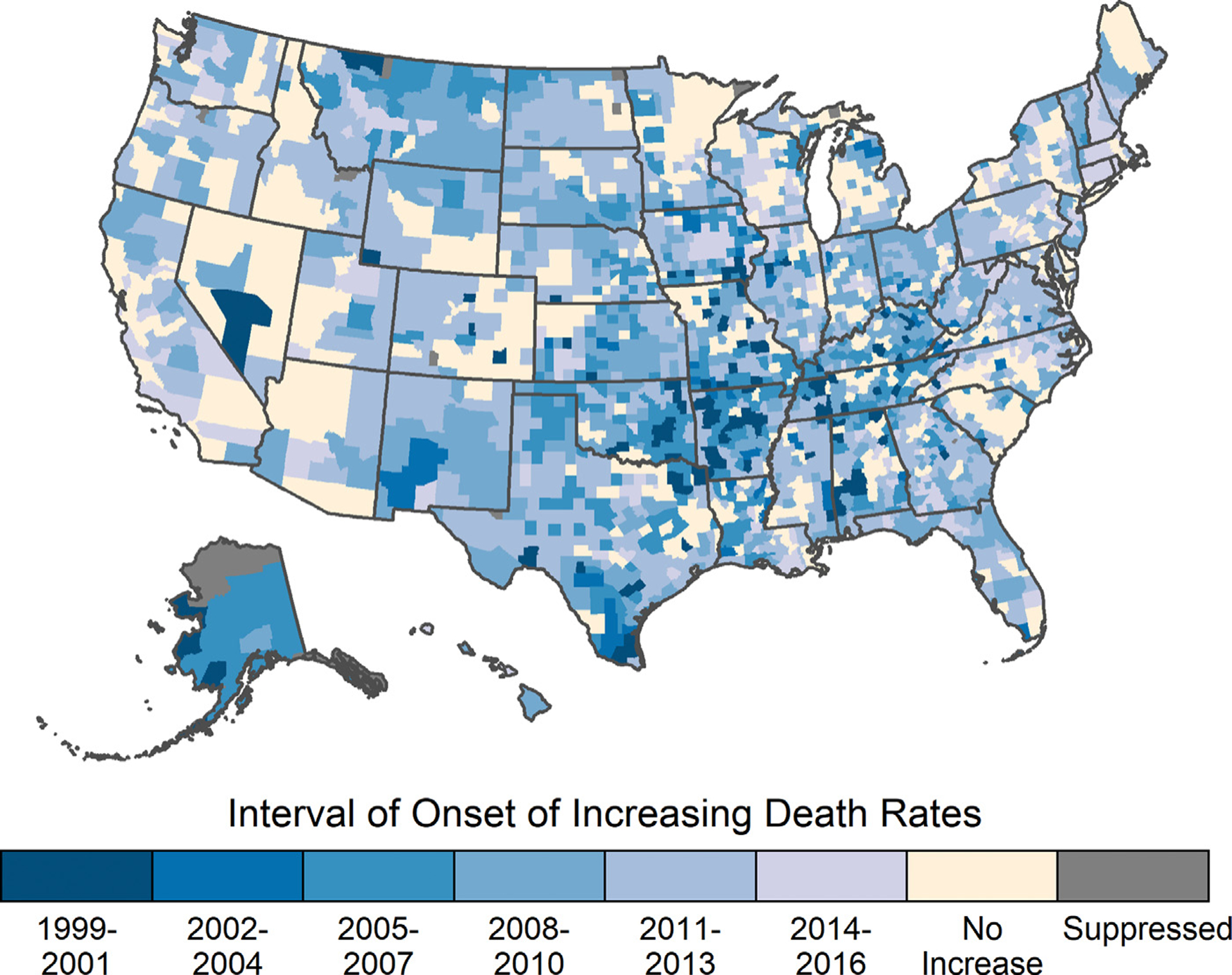
Interval of onset of increasing heart disease death rates in adults ages 35–64, by county, United States, 1999–2019.
One hundred thirty-four counties (4.3% of counties) had lowest rates in the first interval (Table 1). For these counties, trends in heart disease death rates from the first interval through 2019 increased or occasionally plateaued (median 14.2%, [10th, 90th percentiles: −1.1%, 38.3%]). Conversely, 659 counties (21.1% of counties) had lowest heart disease death rates in the last interval. For these counties, the median percent change from 1999 through the last interval was consistently negative (median: −26.3% (10th, 90th percentiles: −39.9%, −10.7%)), indicating that, on average, heart disease death rates in these counties continued to decline and did not increase during the study period.
Onset of increasing heart disease death rates by census region
Increasing heart disease death rates began earlier in counties outside of the Northeast region (Table 2, Fig. 2). Among counties outside of the Northeast, 45.7% (95% CI: 40.8, 48.9), 46.8% (95% CI: 44.1, 49.5), and 35.6% (95% CI: 30.5, 40.0) of counties in the Midwest, South, and West, respectively, began to increase prior to the national change in trend in 2011. Conversely, only 27.2% (95% CI: 21.2, 33.6) of counties in the Northeast were increasing prior to the national change in trend. Compared to the Northeast, the percent of counties with increases prior to the national increase was 1.7 (95% CI: 1.4, 2.1), 1.7 (95% CI: 1.4, 2.2) and 1.3 (95% CI: 1.0, 1.7) times greater in the Midwest, South, and West, respectively (Table 2). Some counties within each region did not experience increases during the entire study period, ranging from 16.1% (95% CI: 13.8, 18.6) of counties in the South to 24.2% (95% CI: 20.2, 29.3) of counties in the West (Table 2, Fig. 3).
Table 2.
Percent of counties experiencing increasing heart disease death rates relative to the national changes in trend in 2011, by US census region and urban-rural classification
| Percent of counties (95% CI) | Ratio of percentages (95% CI) | |||||
|---|---|---|---|---|---|---|
| Onset of increases prior to 2011 | Onset of increases in 2011 or later | No increases | Onset of increases prior to 2011 | Onset of increases in 2011 or later | No increases | |
| Overall | 43.5 (41.3, 45.6) | 38.1 (36.1, 40.9) | 18.4 (15.6, 20.7) | – | – | – |
| Region Northeast (n = 217) |
27.2 (21.2, 33.6) | 51.2 (43.8, 58.1) | 21.7 (15.7, 28.1) | Ref | Ref | Ref |
| Midwest (n = 1051) |
45.7 (40.8, 48.9) | 36.3 (32.5, 40.2) | 18.3 (14, 22.1) | 1.7 (1.4, 2.1) | 0.7 (0.6, 0.9) | 0.8 (0.6, 1.2) |
| South (n = 1418) |
46.8 (44.1, 49.5) | 37.0 (33.7, 40.4) | 16.1 (13.8, 18.6) | 1.7 (1.4, 2.2) | 0.7 (0.6, 0.8) | 0.8 (0.6, 1.0) |
| West (n = 430) |
35.6 (30.5, 40.0) | 40.2 (34.2, 45.8) | 24.2 (20.2, 29.3) | 1.3 (1.0, 1.7) | 0.8 (0.6, 1.0) | 1.1 (0.8, 1.6) |
| Urban-rural classification Large central metro (n = 63) |
17.5 (9.5, 23.8) | 46.0 (36.5, 55.6) | 38.1 (27.0, 46.0) | Ref | Ref | Ref |
| Large fringe metro (n = 354) |
27.7 (23.4, 32.5) | 50.3 (44.4, 55.6) | 22.0 (18.1, 26.3) | 1.6 (1.1, 2.9) | 1.1 (0.9, 1.4) | 0.6 (0.5, 0.8) |
| Medium metro (n = 332) |
38.9 (34.3, 42.8) | 41.0 (36.4, 45.8) | 20.2 (16.9, 23.8) | 2.3 (1.6, 4.1) | 0.9 (0.7, 1.1) | 0.5 (0.4, 0.7) |
| Small metro (n = 340) |
44.1 (39.7, 49.1) | 38.8 (33.5, 43.8) | 16.5 (12.6, 20.6) | 2.6 (1.9, 4.7) | 0.9 (0.7, 1.1) | 0.4 (0.3, 0.6) |
| Micropolitan (n = 691) |
46.2 (42.7, 49.8) | 36.6 (32.6, 40.5) | 17.2 (13.9, 20.3) | 2.8 (1.9, 4.9) | 0.8 (0.6, 1) | 0.5 (0.4, 0.6) |
| Noncore (n = 1336) |
48.4 (45.4, 51.9) | 34.4 (31.6, 38.2) | 17.2 (13.4, 20.0) | 2.9 (2, 5.2) | 0.8 (0.6, 1) | 0.5 (0.3, 0.6) |
Fig. 2.
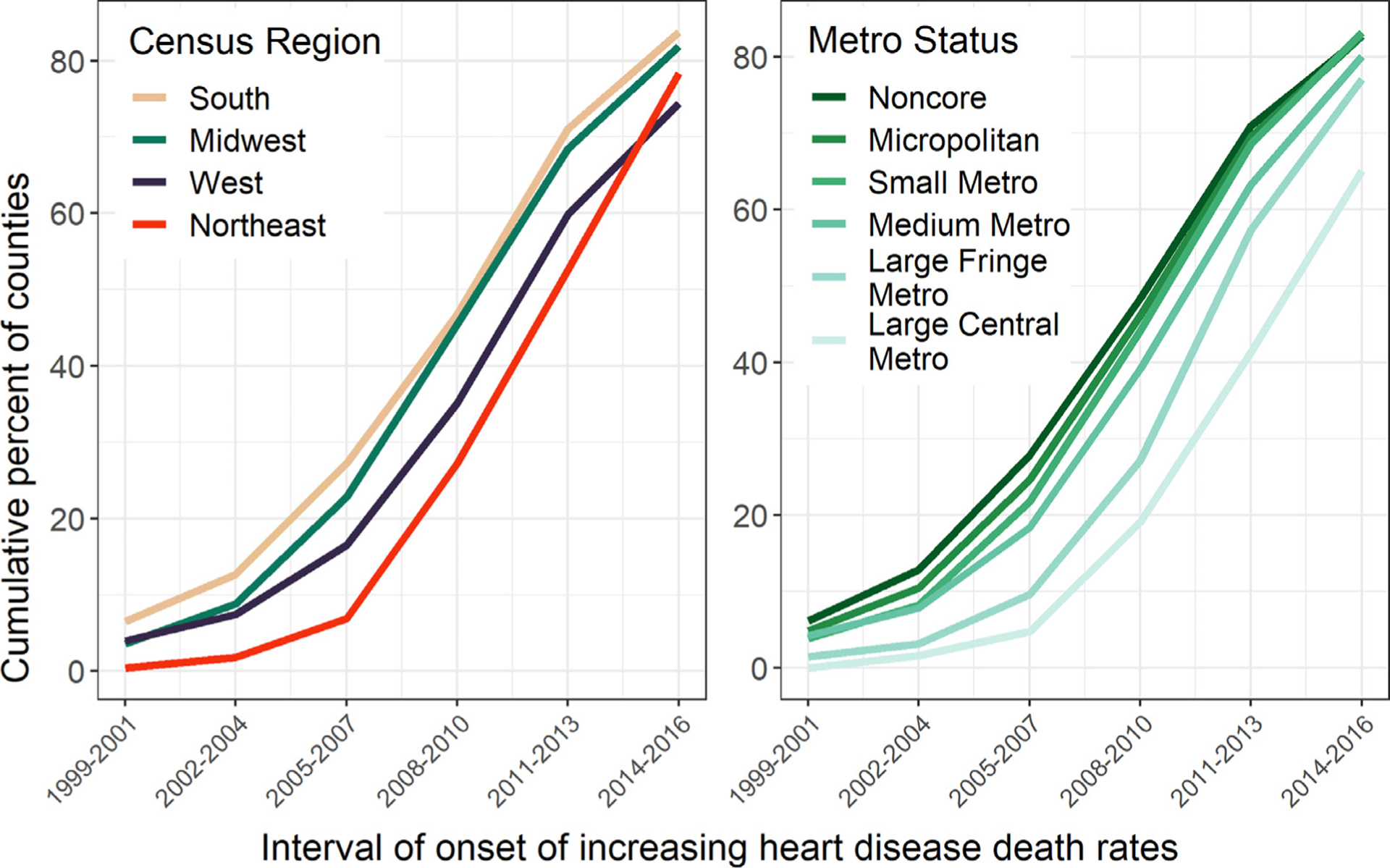
Cumulative percent of counties experiencing increasing heart disease death rates by US census region and urban-rural classification, 1999–2019. Note: Counties included in the earliest interval (1999–2001) may have started to increase prior to 1999.
Fig. 3.
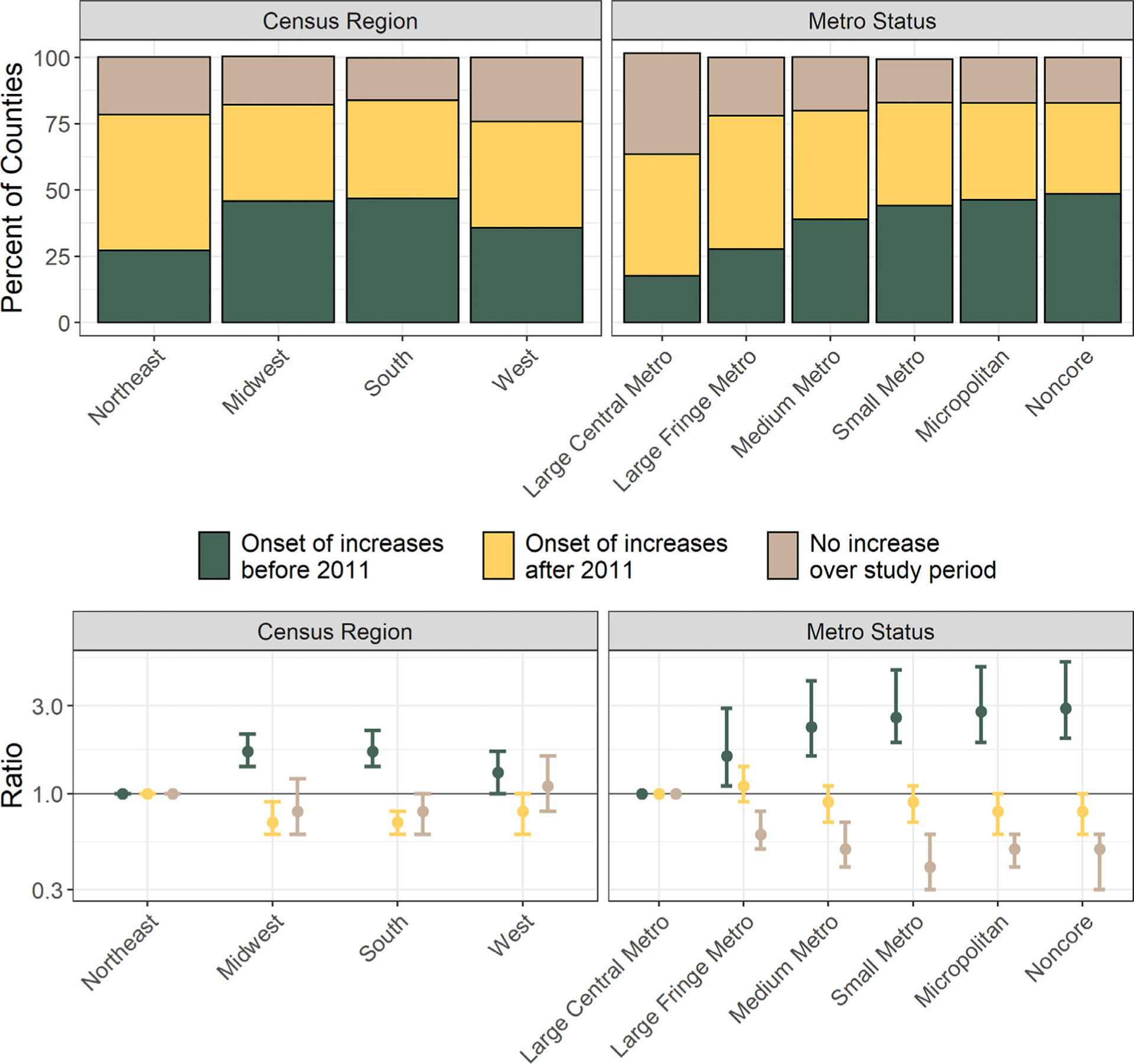
Percent of counties with onset of increasing heart disease death rates before and after the national onset in 2011, by US census region and urban-rural classification.
Onset of increasing heart disease death rates by urban-rural classification
Increasing heart disease death rates began earlier outside of the large central metro counties (Table 2, Fig. 2). Among these counties, 27.7% (95% CI: 23.4, 32.5), 38.9% (95% CI: 34.3, 42.8), 44.1% (95% CI: 39.7, 49.1), 46.2% (95% CI: 42.7, 49.8), and 48.4% (95% CI: 45.4, 51.9) of large fringe metro, medium metro, small metro, micropolitan, and noncore counties, respectively, began to experience increasing heart disease mortality prior to 2011. Conversely, approximately one-fifth (17.5% [95% CIL 9.5, 23.8]) of large central metro counties began to increase before the national change in trend in 2011 (Fig. 2).
Roughly two-in-five (38.1% [95% CI: 27.0, 46.0]) of large central metro counties declined throughout the study period (Table 2). Compared to these large central metro counties, large fringe metro, medium metro, small metro, micropolitan, and noncore counties were roughly 50% less likely to decline for the entire study period (ratios of 0.6 [95% CI: 0.5, 0.8], 0.5 [95% CI: 0.4, 0.7], 0.4 [95% CI: 0.3, 0.6], 0.5 [95% CI: 0.4, 0.6], and 0.5 [95% CI: 0.3, 0.6], respectively) (Table 2, Fig. 3).
Discussion
In this study of the timing of changing county-level trends in heart disease mortality, we found that national data have masked both temporal and geographic variation in the onset of recent increases in heart disease death rates among adults aged 35–64 years. The timing of local increases spanned over two decades, with the earliest increases in the early 2000s concentrated outside of the Northeast and outside of central metro counties. However, some counties in all regions and all urban-rural categories continued to experience declining heart disease death rates during the entire study period.
During the latter half of the 20th century, heart disease mortality experienced strong national declines [2–4]. These national improvements have been equally attributed to advances in prevention and treatment [28]. However, at a more geographically granular level, these historic declines varied markedly in magnitude and began at different times, with the timing differing by urban-rural classification, region, and their corresponding socioeconomic characteristics [2, 3, 13].
Our findings regarding the recent onset of increasing heart disease death rates mirror this variation in the timing of historic declines [2, 3]. The Northeast region fared best in the timing of both declining and increasing death rates, with most communities in the region experiencing the early onset of declining heart disease death rates and the late onset of increasing heart disease death rates. Likewise, the onsets of both declines and increases exhibited a strong urban-rural gradient, with the most urban areas experiencing the earliest onset of declines and the latest onset of increases. Although the study populations and geographic units in the earlier studies documenting onset of declines differed slightly from our study (ages 35–74 vs. 35–64, state economic areas vs. counties, white population vs. all racial and/or ethnic groups, respectively), this symmetry in findings between the timing of historic declines and recent increases reinforces the importance of place-based factors (rather than prevention and treatment alone) in establishing when trends in heart disease death rates change.
Our observed differences by urban-rural classification suggest additional insight into the drivers of the timing of changing trends in heart disease death rates. Since the mid-1990s, rural counties have traditionally experienced excess in all-cause mortality stemming from physician shortages and lower health insurance coverage, which are in turn rooted in socioeconomic factors [29–31]. These same socioeconomic and health systems factors contribute to geographic disparities in cardiovascular disease mortality, especially in the Southern US where heart disease death rates are highest and historic declines in those rates have been slowest [10, 13, 32]. Likewise, limited access to medical settings may compound poor health among working age adults, who are less engaged with the medical system and who are less aware of key cardiovascular disease risk factors (e.g., hypertension) [33–35]. Consequently, the earlier onset of increasing heart disease mortality in counties outside of highly urban centers may reflect a geographic inequity in access to both the medical system and to environments that facilitate the prevention and treatment of heart disease.
However, even within these urban-rural and regional classifications, the timing of recent increases varied such that some counties within each category continued to experience declining heart disease death rates throughout the study period. Future work may continue to explore these associations and to examine the complex interplay between local-level socioeconomic conditions, timing of changes in primary and secondary prevention, and the timing of changing trends, especially within the context of racial and/or ethnic disparities in heart disease mortality. Importantly, these studies may benefit from examining positive characteristics of the roughly 20% of resilient counties that defied national trends and continued to decline.
These results may also directly inform the public health surveillance of cardiovascular disease, which is especially important since deaths among these working age adults are preventable [9]. The geographic and temporal variation observed within our results reinforce the critical nature of collecting, analyzing, and monitoring local chronic disease outcomes [36]. Our results demonstrate that county-level changes in trends may serve as bellwethers for national changes, allowing quicker, more geographically specific implementation of actions to reverse adverse trends long before the trends become apparent at the national level. By the time national trends in heart disease death rates changed in 2011, more than one-in-five (26.3 million) adults aged 35–64 years lived in counties with increasing death rates (Supplemental Table 1, Supplemental Fig. 1). These individuals comprise communities that represent key opportunities for the prevention of cardiovascular health risk factors, treatment of heart disease, and improvement of heart health. Prevention and treatment opportunities may benefit from occurring outside of the typical medical settings, including in communities and at workplaces, given the potential for limited medical access among these working age adults and in communities outside of urban population centers [29–31].
Limitations
This analysis is subject to at least four limitations. First, cause of death listed on death certificates may be misclassified [37, 38]. However, our use of the broad category of “all diseases of the heart” reduces this potential misclassification [39, 40]. Additionally, this outcome represents the most comprehensive measure of heart disease burden that is available at the county-level. Second, small numbers of deaths and small populations may lead to imprecise rates and uncertainty in the assigned interval of onset. Our Bayesian model allowed us to generate more precise rates than would have been possible using non–suppressed NCHS mortality data. However, some rates remained imprecise and these were suppressed. Using this set of precise rate estimates, we then estimated the interval of onset by using MCMC samples from the posterior distributions of heart disease death rates. The resulting posterior probabilities of the estimated intervals were much higher than the probability of selecting an interval by chance, indicating more precision and greater certainty in the estimate (Supplemental Fig. 2). The definition of these intervals represents a third limitation. We chose three-year intervals to balance precision of the estimates and temporal granularity. In a sensitivity analysis, we performed the analysis using 2-year intervals. The observed patterns did not noticeably change using this definition, but the posterior probabilities using this definition were much smaller (Supplemental Table 2, Supplemental Fig. 3). Finally, the potential heterogeneity of health outcomes within counties may mask more geographically granular disparities [29]. However, the county is the smallest geographic level for which national death data are available.
Conclusion
Over the span of two decades, counties across the country began to experience increasing heart disease death rates among working age adults, foreshadowing the national change in trend by a decade. Variation in this timing by region and urban-rural classification suggests that factors associated with these geographic classifications may be critical in establishing the timing of changing trends in heart disease death rates. These results further reinforce the key role of spatiotemporal surveillance in the early identification of adverse trends and in informing subsequent opportunities for tailored policies and programs.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Abbreviations:
- MCMC
Markov chain Monte Carlo
- 95% CI
95% credible interval
- NCHS
National Center for Health Statistics
Footnotes
Declaration of interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- [1].Kochanek KD, Xu JQ, Arias E. Mortality in the United States, 2019. NCHS Data Brief, no 395. Hyattsville, MD: National Center for Health Statistics; 2020 [PubMed] [Google Scholar]
- [2].Wing S, Casper M, Riggan W, Hayes C, Tyroler HA. Socioenvironmental characteristics associated with the onset of decline of ischemic heart disease mortality in the United States. Am J Public Health 1988;78(8):923–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wing S, Barnett E, Casper M, Tyroler HA. Geographic and socioeconomic variation in the onset of decline of coronary heart disease mortality in white women. Am J Public Health 1992;82(2):204–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ragland KE, Selvin S, Merrill DW. The onset of decline in ischemic heart disease mortality in the United States. Am. J. Epidemiol 1988;127(3):516–31. [DOI] [PubMed] [Google Scholar]
- [5].Wing S, Hayes C, Heiss G, John E, Knowles M, Riggan W, et al. Geographic variation in the onset of decline of ischemic heart disease mortality in the United States. Am J Public Health 1986;76(12):1404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O’Flaherty M, et al. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999–2018: observational analysis of vital statistics. BMJ 2020;370:m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Go AS, Rana JS. Heterogeneity in national U.S. mortality trends within heart disease subgroups. 2000–2015. BMC Cardiovasc Disord 2017;17(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH, et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol 2016;1(5):594–9. [DOI] [PubMed] [Google Scholar]
- [9].Ritchey MD, Wall HK, George MG, Wright JS. US trends in premature heart disease mortality over the past 50 years: where do we go from here? Trends Cardiovasc Med 2019;30(6):364–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Vaughan AS, Ritchey MD, Hannan J, Kramer MR, Casper M. Widespread recent increases in county-level heart disease mortality across age groups. Ann Epidemiol 2017;27(12):796–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Vaughan AS, Schieb L, Casper M. Historic and recent trends in county-level coronary heart disease death rates by race, gender, and age group, United States, 1979–2017. PLoS ONE 2020;15(7):e0235839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Vaughan AS, Schieb L, Quick H, Kramer MR, Casper M. Before the here and now: what we can learn from variation in spatiotemporal patterns of changing heart disease mortality by age group, time period, and birth cohort. Soc Sci Med 2018;217:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Casper M, Kramer MR, Quick H, Schieb LJ, Vaughan AS, Greer S. Changes in the geographic patterns of heart disease mortality in the United States: 1973 to 2010. Circulation 2016;133(12):1171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Vaughan AS, Quick H, Pathak EB, Kramer MR, Casper M. Disparities in temporal and geographic patterns of declining heart disease mortality by race and sex in the United States, 1973–2010. J Am Heart Assoc 2015;4(12):e002567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ritchey MD, Loustalot F, Bowman BA, Hong Y. Trends in mortality rates by subtypes of heart disease in the United States, 2000–2010. JAMA 2014;312(19):2037–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].National Center for Health Statistics. Excess deaths associated with COVID-19: provisional death counts for coronavirus disease (COVID-19) 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Accessed Jan 10, 2022.
- [17].National Center for Health Statistics. US Census populations with bridged race categories 2017. Accessed from: www.cdc.gov/nchs/nvss/bridged_race.htm. Accessed Jan 10, 2022.
- [18].Quick H, Casper M, Waller LA. A multivariate space-time model for analysing county level heart disease death rates by race and sex. J. R Stat Soc, C: Appl Stat 2017;67:291–304. [Google Scholar]
- [19].Vaughan AS, Kramer MR, Waller LA, Schieb LJ, Greer S, Casper M. Comparing methods of measuring geographic patterns in temporal trends: an application to county-level heart disease mortality in the United States, 1973 to 2010. Ann Epidemiol 2015;25(5):329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Vaughan AS, Woodruff RC, Shay CM, Loustalot F, Casper M. Progress toward achieving national targets for reducing coronary heart disease and stroke mortality: a county-level perspective. J Am Heart Assoc 2021;10(4):e019562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Quick H, Waller LA, Casper M. A multivariate space–time model for analysing county level heart disease death rates by race and sex. J Roy Stat Soc C 2018;67(1):291–304. [Google Scholar]
- [22].Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math 1991;43(1):1–20. [Google Scholar]
- [23].R Core Team. R: a language and environment for statistical computing Vienna, Austria: R foundation for statistical computing; 2020. Accessed from: https://www.R-project.org/. Accessed Jan 10, 2022.
- [24].Waller LA, Carlin BP, Xia H, Gelfand AE. Hierarchical spatio-temporal mapping of disease rates. J Am Stat Assoc 1997;92(438):607–17 [Google Scholar]
- [25].Gelfand AE, Vounatsou P. Proper multivariate conditional autoregressive models for spatial data analysis. Biostatistics 2003;4(1):11–15 [DOI] [PubMed] [Google Scholar]
- [26].Goovaerts P Analysis of geographical disparities in temporal trends of health outcomes using space-time joinpoint regression. Int J Appl Earth Obs Geoinf 2013;22:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ingram DD, Franco SJ. NCHS urban-rural classification scheme for counties. Vital Health Stat 2 2012(154):1–65. [PubMed] [Google Scholar]
- [28].Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med 2007;356:2388–98. [DOI] [PubMed] [Google Scholar]
- [29].Cosby AG, McDoom-Echebiri MM, James W, Khandekar H, Brown W, Hanna HL. Growth and persistence of place-based mortality in the United States: the rural mortality penalty. Am J Public Health 2019;109(1):155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gong G, Phillips SG, Hudson C, Curti D, Philips BU. Higher US rural mortality rates linked to socioeconomic status, physician shortages, and lack of health insurance. Health Aff (Millwood) 2019;38(12):2003–10 [DOI] [PubMed] [Google Scholar]
- [31].Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, et al. Health-related behaviors by urban-rural county classification - United States, 2013. MMWR Surveill Summ 2017;66(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ahmad K, Chen EW, Nazir U, Cotts W, Andrade A, Trivedi AN, et al. Regional variation in the association of poverty and heart failure mortality in the 3135 counties of the United States. J Am Heart Assoc 2019;8(18):e012422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Centers for Disease Control and Prevention. Hypertension cascade: hypertension prevalence, treatment and control estimates among US adults aged 18 years and older applying the criteria from the American college of cardiology and american heart association’s 2017 hypertension guideline—NHANES 2015–2018 Atlanta, GA: US department of health and human services; 2019. Accessed at: May 13, 2021. Accessed from: https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. [Google Scholar]
- [34].Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, et al. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020;324(12):1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension 2017;70(4):736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Brissette I, Casper M, Huston SL, Jordan M, Karns B, Kippes C, et al. Application of geographic information systems to address chronic disease priorities: experiences in state and local health departments. Prev Chronic Dis 2019;16(E65):180674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Pagidipati NJ, Gaziano TA. Estimating deaths from cardiovascular disease: a review of global methodologies of mortality measurement. Circulation 2013;127(6):749–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Lloyd-Jones DM, Martin D, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann. Intern. Med 1998;129:1020–6 [DOI] [PubMed] [Google Scholar]
- [39].Coady S, Sorlie P, Cooper L, Folsom A, Rosamond W, Conwill D. Validation of death certificate diagnosis for coronary heart disease: the atherosclerosis risk in communities (ARIC) study. J Clin Epidemiol 2001;54(1):40–50. [DOI] [PubMed] [Google Scholar]
- [40].Ives DG, Samuel P, Psaty BM, Kuller LH. Agreement between nosologist and cardiovascular health study review of deaths: implications of coding differences. J Am Geriatr Soc 2009;57(1):133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


