Abstract
Objective:
Sexual and gender minority (SGM) young people may use alcohol or cannabis (A/C) at higher rates that non-SGM peers, but little is known about whether SGM young adults experience poorer health, psychosocial, and other outcomes at similar levels of A/C use.
Methods:
We used longitudinal survey data from a community cohort recruited from California middle schools in 2008 (average age 11.5) and followed across 12 waves through 2020. Participants reported on past-month A/C use at each wave. Individuals also reported SGM status as well as outcomes in multiple domains in wave 12. Sequelae of change models tested differences in intercept and slope for A/C use trajectories from waves 1–12 across SGM groups, and simultaneously examined differences in outcomes by SGM status adjusting separately for A/C trajectories.
Results:
SGM (n=445) and non-SGM (n=2,089) groups did not differ on baseline probability of A/C use. SGM individuals showed steeper increases in probability of cannabis but not alcohol use over time. Adjusting for trajectories of A/C use, SGM individuals had significant disparities relative to non-SGM peers with respect to: employment and economic stability, criminal justice involvement, social functioning, subjective physical health, behavioral health, and perceived unmet mental health treatment need.
Conclusions:
At the same levels of A/C use from middle school through young adulthood, SGM individuals show disparities in multiple domains compared to non-SGM peers. Targeted efforts to reduce substance use in conjunction with other structural disadvantages experienced by SGM youths are needed to address the emergence of disparities in young adulthood.
Keywords: substance use trajectories, disparities, sexual and gender minority, LGBT, young adulthood
Substance use is widely recognized as an important contributor to health and other disparities for lesbian, gay, bisexual, transgender, intersex, non-binary, and other individuals who do not identify as heterosexual and/or cisgender (i.e., sexual and gender minority individuals; hereafter, SGM) (Institute of Medicine, 2011; National Academies of Sciences, Engineering, and Medicine, 2020). SGM adolescents and adults have well-documented disparities in rates of alcohol, cannabis, and other substance use relative to their non-SGM peers (Hatzenbuehler et al., 2008; Hughto et al., 2021; Marshal et al., 2008; Schuler et al., 2019). Prior research has shown that SGM youths begin using substances earlier than their non-SGM peers, substance use escalates more quickly (e.g., more rapid progression to regular use), and these differences may persist over the life course (Fish et al., 2021; National Academies of Sciences, Engineering, and Medicine, 2020). This is concerning because early and escalating substance use is associated with a range of negative health, psychosocial, and other outcomes (e.g., poorer physical and mental health; lower educational attainment) that may manifest as early as young adulthood (Hanson et al., 2011; Scholes-Balog et al., 2016; Thompson et al., 2019; Trim et al., 2007; Tucker et al., 2005). Substance use may also exacerbate challenges with navigating developmental processes inherent to transitioning to adulthood, such as identity development, burgeoning independence, establishing social networks outside of families and regions of origin, and transitions in education and careers (Arnett, 1998, 2000; Schulenberg et al., 2004), which may set the stage for poorer outcomes in later life.
The consequences of substance use are also not equitable across all segments of the population, and may disproportionately affect some groups more than others, even at similar levels of use. Minority stress theory (Meyer, 2003; Goldbach & Gibbs, 2017) posits that minority groups, including SGM individuals, experience higher rates of discrimination, violence, stigma, identity concealment, and/or internalized homophobia/transphobia/biphobia, which can escalate risks for coping-related substance use and may compound or exacerbate negative outcomes associated with substance use. For example, SGM individuals experience high rates of social and structural discrimination and victimization, which may increase risk of alcohol and other drug use and other problems while reducing access to resources that may buffer against such stressors (Institute of Medicine, 2011; Krueger et al., 2020; McCabe et al., 2010; Meyer, 2003; National Academies of Sciences, Engineering, and Medicine, 2020; Russell & Fish, 2016). Such factors may also contribute to poorer substance use-related outcomes for SGM young people compared to non-SGM peers, even at similar levels of use over time. For example, although prior studies have not focused on SGM status, studies of racial/ethnic disparities have found more severe consequences from drinking for racial/ethnic minority-identifying adults compared to adults who identify as non-Hispanic White, even at low levels of heavy drinking (Mulia et al., 2009). Similarly, studies of adolescents show that some racial/ethnic minority groups experience poorer substance use-related outcomes compared to white peers, even at similar trajectories of alcohol or cannabis (A or C) use during adolescence (D’Amico et al., 2016). Such disparities at similar levels of use may be attributable to a range of factors, including differences in access to resources (e.g., behavioral health treatment) and potential interactive or compounding effects of substance use with discrimination and other stressors associated with minority group status (Chartier et al., 2010; Pascoe et al., 2009; Williams et al., 2009).
To date, however, limited research has examined whether SGM young adults experience disproportionately negative effects of substance use on different areas of functioning at similar levels of A/C use. Although recent longitudinal research has characterized trajectories of substance use and behavioral health of SGM youth (Coulter et al., 2018; Dermody, et al., 2019; Fish & Pasley, 2015), these studies have typically not examined how substance use trajectories are associated with distal outcomes in other domains of functioning (e.g., social relationships; educational attainment; employment or economic functioning). This represents a gap in the evidence base on SGM health and well-being in part because it provides an incomplete characterization of the different ways in which early substance use may or may not contribute to contemporary disparities for SGM individuals. For example, key domains examined in NASEM’s (2020) recent update to the Institute of Medicine’s (2011) groundbreaking report on the health of SGM populations included: families and social relationships; education; economic well-being; physical and mental health; and coverage, access, and utilization of evidence-based health care (National Academies of Sciences, Engineering, and Medicine, 2020). SGM individuals also experience disparate problems in other domains that may be linked to substance use, such as risky sexual behavior (Institute of Medicine et al., 2011), poor sleep (Butler et al., 2020), and disciplinary or criminal justice consequences (Poteat et al., 2016). Assessing substance use patterns in relation to these different domains is critical for providing a more comprehensive understanding of SGM individuals’ health and wellbeing and for characterizing the breadth of potential substance use-related disparities that this group may experience relative to non-SGM peers.
A trajectory-based approach to examining longitudinal patterns of substance use and multiple outcomes can shed light on critical timepoints and functional targets for primary, secondary, and tertiary prevention. Adolescence and young adulthood are pivotal developmental “springboards” for onward trajectories and outcomes in later life (Arnett et al., 2014; National Academies of Sciences, Engineering, and Medicine,, 2019). Therefore, greater attention to early substance use trajectories and associated outcomes may highlight points of intervention to remediate disparities in mental and physical health, socioeconomic wellbeing, and incarceration among adult SGM populations. There is a need for a life course approach to SGM health with a focus on substance use trajectories as well as greater attention to a broader range of functional domains to better characterize the experience of SGM individuals as they move from adolescence into adulthood.
To address these gaps, we examined separate trajectories of alcohol and cannabis use in a diverse, contemporary cohort of young people followed from early adolescence into young adulthood and assessed outcomes across eight domains of functioning. We first compared alcohol and cannabis use trajectories between SGM and non-SGM individuals. We focus on alcohol and cannabis use as these are the most commonly used substances among young people, they produce intoxication and correlate with poorer outcomes across multiple domains, and because prior research has shown differences in rates of alcohol and cannabis use across SGM and non-SGM adolescents and young adults (Corliss et al., 2010; Coulter et al., 2018; Hughto et al., 2021; Schuler et al., 2018). We then assessed disparities in outcomes, after adjusting for alcohol and cannabis trajectories, across multiple domains of functioning in young adulthood, including 1) education, 2) employment and economic stability, 3) transition to adult roles, 4) criminal justice involvement, 5) social functioning, 6) physical health, 7) behavioral health, and 8) unmet treatment need.
Method
Dataset
The study analyzed existing data from an ongoing longitudinal survey study of young people based in California, details of which are reported in full elsewhere (D’Amico et al., 2016; D’Amico et al., 2012). We report how we determined our sample size, all data exclusions (if any), all manipulations, and all measures in the study. Briefly, participants (n=6,509) were originally recruited in 2008, when they were in 6th and 7th grade (average age 11.5), from 16 middle schools in Southern California as part of a substance use prevention program evaluation (CHOICE) (D’Amico et al., 2012). Individuals were representative of the broader student bodies within Southern California middle schools in terms of demographic characteristics and future substance use risk. Participants completed survey waves 1 through 5 during middle school classes. After they transitioned from middle school to high school, following wave 5, participants were subsequently re-contacted and re-consented to complete annual web-based surveys. At wave 6 (fielded 2013–2014), 61% of the wave 5 sample participated in the follow-up survey. Across subsequent waves, retention rates have ranged from 80% to 92%. At wave 12, fielded in 2019–2020, 2,534 participants completed the survey. Based on multivariate logistic regression analyses, retention from wave 11 to wave 12 was not predicted by wave 11 substance use similar to all previous waves (i.e., past-month use of alcohol, cannabis, or cigarettes); however, we did find that at this wave that females were more likely to be retained than males (93.41% vs. 90.53%, respectively); those who identified as Hispanic (93.28%) and Asian (92.93%) were more likely to be retained than those identifying as White (90.87%), Black (82.76%), or another racial identity (90.11%); and those retained were slightly younger than those who were not (mean age = 21.57 vs. 21.85 at wave 11, respectively). The present study uses data from wave 1 through 12, corresponding to the period from middle school to young adulthood. The final analytic sample for this study included the 2,534 participants who completed the wave 12 survey, when young adult outcome data were collected. All participants consented to the study, and procedures were approved by the RAND Human Subjects Protection Committee.
Measures
Alcohol and Cannabis Use from Middle School through Young Adulthood
Alcohol and cannabis use at waves 1–12 were assessed using items from Monitoring the Future (Johnston et al., 2016): “During the past month, how many days did you [drink alcohol; use marijuana]?” Responses ranged from 0 to 20–30 days [note: beginning in Wave 11, response options changed to continuous 0 to 30 days]. Due to considerable skew, especially in early waves, and related problems with model convergence using frequency data, responses were dichotomized to indicate any (1) vs. no (0) alcohol use and any (1) vs. no (0) cannabis use at each study wave.
Sexual Orientation and Gender Identity
Sexual and gender minority status was based on items assessing sexual orientation, sexual behavior, transgender identity, gender identity, assigned sex at birth, and non-concordance between sex assigned at birth and current gender identity. Self-reported sexual orientation (“Which of these best describes your sexual orientation?”) included Straight/heterosexual; Gay; Lesbian; Bisexual; Questioning; Asexual. Sexual behavior (“With whom of the following have you had vaginal or anal sex?”) included Only with females; Only with males; With both females and males. Assigned sex at birth was assessed by: “What was your sex assigned at birth?” (Male; Female; Intersex/Other). Current gender identity was assessed by “Do you currently identify as:” (Man, Woman, Gender Neutral [nonbinary], Other). Finally, transgender identity was assessed using a single item: “Are you currently transgender?” (1 = yes; 0 = no).
We created an indicator variable for SGM status based on responses to these items in wave 12. Individuals were categorized in the sexual/gender minority group (SGM = 1) if they met any of the following criteria: reported a sexual orientation of gay, lesbian, bisexual, or questioning (Katz-Wise et al., 2017), reported being transgender, reported same-sex behavior (e.g., men who endorsed having vaginal or anal sex only with males, or with both females and males) (Katz-Wise et al., 2017), reported assigned sex at birth as intersex/other, reported a gender identity other than male or female, or if the respondent’s current gender identity was different from their sex assigned at birth (Tate et al., 2013). We used these indicators and not others (e.g., asexual identity) because they are most likely to reflect lived experience as a sexual and/or gender minority (i.e., outwardly visible behaviors, identities, or other characteristics that would be subject to external minority stressors) (Meyer, 2003; McInroy et al., 2020). All others were categorized as non-SGM (SGM = 0).
Trajectory Model Covariates
Model covariates included self-reported age, assigned sex at birth, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, and multiracial [more than one race/ethnicity] or another race/ethnicity), and mother’s education (as a proxy for socioeconomic status). We also included an indicator variable for CHOICE intervention status at wave 1 (although note: the intervention occurred in 2008–2009, over 10 years ago, and intervention condition was not significantly associated with substance use or other functional outcomes after wave 2).
Outcomes at Wave 12, by Domain
Education.
Post-high school education was assessed as a binary measure (0 = high school diploma or less; 1 = more than a high school diploma).
Employment and economic stability.
Unemployment was assessed as a binary measure (0 = employed part-time or fulltime; 1 = unemployed). Participants also reported whether they had been fired from a job in response to a new item generated by the research team: “In the past year, how often have you… been fired from a job?” (1 = Not at all to 6 = 20 or more times). Response values were re-coded to represent the number of times the event occurred in the past year, with the mid-point taken of any response ranges (e.g., 6–9 times re-coded to 7.5); the range of the re-coded variable was 0–20. Respondents also reported on experiences of homelessness in the past year using the following items: “In the past 12 months, have you slept at a friend’s and/or family member’s home because you had nowhere else to stay (i.e., you did not have a fixed, stable nighttime residence at the time)?” (1 = yes, 0 = no) and “In the past 12 months, did you spend the night in any of these places because you had nowhere else to stay?” (A youth or adult shelter; In a public place, such as a train or bus station, a restaurant, or an office building; In an abandoned building; Outside in a park, on the street, under a bridge or overhang, or on a rooftop; In a subway or other public place underground; With someone you did not know because you needed a place to stay; In a car, truck, or van; response options for each subitem were 0 = no, 1= yes) (Sontag-Padilla et al., 2017). Items were summed and dichotomized to generate a single binary indicator of experiencing homelessness vs. not in the past 12 months. Food insecurity is assessed beginning in wave 12 as how often in the past 12 months individuals experienced concerns with paying for food (e.g., “I worried whether my food would run out before I got money to buy more”; “The food that I bought just didn’t last, and I didn’t have money to get more”) (Sontag-Padilla et al., 2017); response options for these two items ranged from 1 = always true to 4 = never true. We created a dichotomous indicator such that those who endorsed any response other than “never true” to either item were considered as experiencing food insecurity.
Transition to adult roles.
Perceived transition to adulthood was assessed using the IDEA scale (Baggio et al., 2015), a measure of perceived transition to independence/adulthood, which asks respondents to rate how much they agree with the following: “Think of a roughly 5-year period, with the present in the middle, this period of your life is a…Time of many possibilities, Time of exploration, Time of feeling stressed out, Time of high pressure, Time of defining yourself, Time of deciding on your own beliefs and values, Time of feeling adult in some ways but not others, Time of gradually becoming an adult” (response options: 1 = strongly disagree, 2 = somewhat disagree, 3 = somewhat agree, 4 = strongly agree). Total scores were calculated as the mean of all items. Higher scores indicate engagement in a greater number of emerging adult roles and perception of transitioning to adulthood.
Criminal justice involvement.
Criminal justice involvement was assessed using a single item created by the research team: “In the past year, how often have you… Gotten into trouble with the police because of something you did?” (1=Not at all, 6 = 20 or more times, re-coded such that final variable has range 0–20).
Social functioning.
Social functioning was assessed with the PROMIS Peer Relationships Short Form (e.g., “I was able to count on my friends”) (DeWalt et al., 2013) rated on a 5-point scale (0 = never to 4 = always). Items were summed and transformed to a t-score, with higher values indicating better social functioning. Loneliness was assessed using three items from the Three Item Loneliness Scale (Hughes et al., 2004): 1) How often do you feel that you lack companionship? 2) How often do you feel left out? And 3) How often do you feel isolated from others? (response options: 1= hardly ever, 2 = some of the time, 3 = often). Items were summed, with higher values indicating greater loneliness.
Physical health.
Physical health was assessed using a summary score based on the following items: subjective overall health (0 = excellent to 4 = poor), ability to physically engage in activities that one enjoys (1 = with no trouble to 5 = not able to do), and ability to participate in sports/activities similar to their peers (0 = with no trouble to 4 = not able to do) (Schat, Kelloway, & Desmarais, 2005). Items were reverse scored and summed (D’Amico et al., 2016), and higher scores indicated better physical health.
Behavioral health.
Symptoms of common mental health conditions were assessed using the 8-item Patient Health Questionnaire (PHQ-8) (Kroenke et al., 2009) for symptoms of depression, the 7-item Generalized Anxiety Disorder (GAD 7) screen for symptoms of anxiety (Spitzer et al., 2006), and the PCL-5 for symptoms of post-traumatic stress disorder (Blevins et al., 2015). Risky sexual behavior was assessed using two separate items that assessed whether participants had sex with a casual partner after having used alcohol, marijuana, or other drugs in the past 3 months (yes/no) and whether or not they had sexual intercourse with a casual partner without using a condom (yes/no). For descriptive purposes, individuals also reported on the number of casual sexual partners in the past three months; those who reported no casual sexual partners were coded as “no” for the two items. Sleep quality was assessed using a single item: “During the past month, how would you rate your overall sleep quality?” (1 = very good, 2 = fairly good, 3 = fairly bad, 4 = very bad) (Buysse, 2014), with higher scores indicating poorer sleep quality or greater sleep problems.
Unmet treatment need.
Perceived unmet treatment need for 1) alcohol and other drug use and 2) mental health conditions in the past year were assessed using two items from the NSDUH (Center for Behavioral Health Statistics and Quality, 2018): “During the past 12 months, was there any time when you needed alcohol or any drug services or counseling for yourself but didn’t get it?” and “During the past 12 months, was there any time when you needed mental health services or counseling for yourself but didn’t get it?” (1 = yes, 0 = no).
Analyses
We first calculated descriptive statistics (means, frequencies) for demographic and outcome variables overall and by the SGM and non-SGM groups, and conducted unadjusted bivariate tests to compare means/frequencies for all variables of interest by SGM group. Trajectories of alcohol and cannabis use were examined separately using latent growth modeling in a structural equation modeling framework with the weighted least squares with mean and variance adjusted estimator. This method allows for individuals to be included in trajectory modeling with missing data and does not require complete data across all waves and ultimately provides unbiased and consistent estimates (Asparouhov, 2010). In this framework, model intercepts can be interpreted as the average probability of alcohol or cannabis use at baseline (survey wave 1). Model slopes represents the change in probability of A or C use over time (waves 1–12). All models were implemented in Mplus v8 (Muthén & Muthén, 2017).
To assess differences in trajectories by SGM status, we first examined SGM (dummy coded, with non-SGM as the reference category) as a predictor of the slope and intercept of A or C use, controlling for age at wave 1, sex assigned at birth, race/ethnicity, mother’s education, and intervention group. We then examined SGM differences in outcomes in young adulthood (wave 12) by estimating models that assessed the direct effect from SGM status to each outcome, controlling for intercept and slope of A or C use predicting outcomes. We used a sequelae of change model (Duncan et al., 1999), which allows the random effect of the rate of change of A or C use to function as both an outcome (as it is conventionally modeled), as well as a predictor of subsequent outcomes. This approach also allows multiple outcomes to be estimated simultaneously within the same model, rather than requiring separate models for each dependent variable of interest, which is preferred as there are substantially fewer models being estimated, yields better estimates of standard errors, and provides a more accurate characterization of how predictors, like A or C use and SGM status, affect various outcomes that may or may not be interrelated. The model examining direct effects of SGM status, adjusting for A or C use intercept and slope, can be interpreted as a test of disparities in multiple outcomes at wave 12 for SGM individuals (relative to non-SGM peers) after accounting for trajectories of A or C use from waves 1–12; that is, disparities in outcomes after setting both groups to the same “level” of A or C use over time. Because the focus of this investigation was on SGM disparities in outcomes we focus on direct effects of SGM status on outcomes rather than effects of alcohol and cannabis use on health, psychosocial, and other functional outcomes, which are well-documented in the literature. Full model results showing direct effects of A or C use intercept and slope on outcomes of interest are presented in supplement Table S1. All models adjusted for age, sex assigned at birth, race/ethnicity mother’s education, and intervention group. In order to account for multiple statistical tests, we implemented a Benjamini-Hochberg False Discovery Rate procedure to adjust for multiple comparisons (Benjamini & Hochberg, 1995). In text, we report only on significant tests with p-values lower than the corresponding Benjamini-Hochberg adjusted critical p-value. Analysis code for this study is available upon reasonable request by emailing the corresponding author. Data are not yet available as the parent study is still in progress.
Post-hoc sensitivity analyses.
Trajectories of A or C use from waves 1–12 are based on binary indicators of any versus no past-month use. We explored the possibility of modeling trajectories based on frequency of use but were unable to do so due to extremely low rates of any use during early study waves (corresponding to middle school and early high school) and subsequent model convergence issues. We also explored the use of binary indicators of heavy use (e.g., any binge drinking [defined as “five or more drinks of alcohol in a row, that is, within a couple of hours”] in the past month; use on 20+ days in the past month) as an alternative. However, we encountered similar problems with respect to model convergence using this approach due to very low prevalence in early study waves. For example, in study wave 1, only nine participants in the full analytic sample endorsed past-month binge drinking; no participants endorsed drinking and only 2 participants endorsed using cannabis on 20 or more days in the past month. Acknowledging that frequency of use may be a more developmentally appropriate metric for assessing substance use-related risks in young adulthood, we conducted cross-sectional sensitivity analyses using linear and logistic regression wave 12 data to assess whether SGM and non-SGM groups differed with respect to outcomes of interest after adjusting for frequency of past-month A or C use. As with trajectory analyses, all sensitivity analyses controlled for age, assigned sex at birth, race/ethnicity, and mother’s education, and CHOICE intervention status at wave 1.
Results
Sample Characteristics
Participant characteristics overall, and by SGM status, are shown in Table 1. Briefly, in the full sample (n = 2,534), racial/ethnic identity was as follows: 47% Hispanic, 23% non-Hispanic White, 23% Asian, 5% multi-racial or another racial identity, and 2% non-Hispanic Black. Almost 18% of respondents (n = 445) were classified in the SGM group. SGM and non-SGM groups differed significantly with respect to race/ethnicity and sex assigned at birth (see Table 1). Within the SGM group, 68% identified as female, 32% male, and 4% identified as transgender.
Table 1.
Sample characteristics
| Full Sample (n = 2,534) |
SGM group (n = 445) |
Non-SGM group (n = 2,089) |
Group Difference |
|
|---|---|---|---|---|
| % (n)/ Mean (SD) |
% (n) / Mean (SD) |
% (n) / Mean (SD) |
p | |
| Age (wave 12) | 22.6 (0.8) | 22.5 (0.8) | 22.6 (0.8) | .65 |
| Race | .01 | |||
| Non-Hispanic White | 23.1% (585) | 26.7% (119) | 22.3% (466) | |
| Non-Hispanic Asian | 23.4% (592) | 16.9% (75) | 24.8% (517) | |
| Non-Hispanic Black | 1.8% (45) | 2.0% (9) | 1.7% (36) | |
| Hispanic | 46.8% (1185) | 49.0% (218) | 46.3% (967) | |
| Multi-racial/another race/ethnicity | 5.0% (127) | 5.4% (24) | 4.9% (103) | |
| Assigned Sex at Birth | < .0001 | |||
| Male | 45.0% (1140) | 31.9% (142) | 47.8% (998) | |
| Female | 55.0% (1392) | 67.9% (302) | 52.2% (1090) | |
| Intersex/other | 0.04% (1) | 0.2% (1) | 0.0% (0) | |
| Mother’s Education | .69 | |||
| < High school | 18.0% (433) | 17.5% (74) | 18.1% (359) | |
| High school | 16.1% (389) | 14.5% (61) | 16.5% (328) | |
| Some college | 19.8% (476) | 20.4% (86) | 19.6% (390) | |
| Associate’s degree | 6.8% (164) | 6.9% (29) | 6.8% (135) | |
| College degree or higher | 34.8% (838) | 37.2% (157) | 34.3% (681) | |
| SGM characteristics* | ||||
| Sexual orientation | ||||
| Straight/heterosexual | -- | 10.59% (47) | -- | -- |
| Gay | -- | 13.06% (58) | -- | -- |
| Lesbian | -- | 9.01% (40) | -- | -- |
| Bisexual | -- | 55.41% (246) | -- | -- |
| Questioning | -- | 10.81% (48) | -- | -- |
| Asexual | -- | 1.13% (5) | -- | -- |
| Same-sex vaginal/anal sex | -- | 46.28% (205) | -- | -- |
| Differing gender identity and sex assigned at birth | -- | 10.34% (46) | -- | -- |
| Gender neutral or other gender identity | -- | 6.96% (31) | -- | -- |
| Transgender identity | -- | 4.04% (18) | -- | -- |
| Intersex/other | 0.04% (1) | 0.2% (1) | 0.0% (0) | |
| Past-month alcohol use (wave 12) | 64.2% (1620) | 69.4% (308) | 63.1% (1312) | .01 |
| Past-month number of days using alcohol, among those who used (wave 12) | 6.4 (6.1) | 6.6 (6.3) | 6.4 (6.0) | .51 |
| Past-month cannabis use (wave 12) | 31.0% (783) | 45.6% (202) | 27.9% (581) | < .0001 |
| Past-month number of days using cannabis, among those who used (wave 12) | 11.7 (11.4) | 13.1 (11.6) | 11.2 (11.2) | .05 |
Note. SGM = sexual/gender minority. Group differences assessed by unadjusted bivariate t-test (age) and omnibus chi-square tests (all other variables).
SGM characteristics are not mutually exclusive.
SGM group status was based on multiple criteria (sexual identity, same-sex sexual behavior, transgender identity, and concordance between birth sex and current gender identity) which were not mutually exclusive. In the SGM group, 55% identified as bisexual, with smaller portions identifying as gay (13%), straight/heterosexual (11%), questioning (11%), or lesbian (9%). About half (46%) had engaged in same-sex sexual behavior. More participants had differing birth sex and current gender identity (10%) than identified as a minority gender identity (7%) or as transgender (4%).
Table 1 also shows alcohol and cannabis use in wave 12. SGMs differed with respect to non-SGM individuals on rates of past-month alcohol and cannabis use in wave 12, such that those in the SGM group reported higher rates of alcohol use (69% vs 63%, p = .01) and cannabis use (46% vs 28%, p < .0001) in the past month relative to non-SGM individuals. Among those reporting any current use, compared to the non-SGM group, there was a trend such that SGM young adults also indicated using cannabis on slightly more days in the past month (M = 13.1 vs. M = 11.2 days; p = .05); groups did not differ on frequency of alcohol use.
Table 2 shows descriptive statistics and group differences in outcomes across SGM and non-SGM individuals based on unadjusted bivariate tests. As shown in the table, comparisons showed SGM and non-SGM groups differed on nearly all outcomes.
Table 2.
Means and frequencies of wave 12 outcomes by sexual/gender minority group status
| Domain | Outcome variable | Full sample (n = 2,534) |
SGM (n = 445) |
Non-SGM (n = 2,089) |
Group difference |
|---|---|---|---|---|---|
| % (n)/ M (SD) | % (n) /M (SD) | % (n) /M (SD) | p | ||
| Education | Educational attainment post-high school (% yes) | 58.9% (1491) | 54.8% (244) | 59.8% (1247) | .05 |
| Employment and economic stability | Currently employed full- or part-time (% yes) | 74.0% (1868) | 67.9% (302) | 75.3% (1566) | .001 |
| Number of times fired from job in past year (range 0–20) | 0.1 (1.3) | 0.4 (2.5) | 0.1 (0.8) | .004 | |
| Homelessness in past year (% yes) | 8.1% (204) | 14.2% (63) | 6.8% (141) | < .0001 | |
| Food insecurity in past year (% yes) | 31.1% (781) | 45.1% (200) | 28.1% (581) | < .0001 | |
| Transition to adult roles |
IDEA scale score (range 1–4) | 3.3 (0.6) | 3.4 (0.6) | 3.3 (0.6) | .006 |
| Criminal justice involvement | Instances of being in trouble with police in past year (range 0–20) | 0.2 (1.4) | 0.4 (2.6) | 0.1 (1.0) | .006 |
| Social functioning | PROMIS Social Functioning (range 19.3–69.8) | 50.0 (10.0) | 48.4 (10.3) | 50.4 (9.9) | .0001 |
| Loneliness score (range 2–9) | 5.0 (2.0) | 5.8 (2.1) | 4.9 (1.9) | < .0001 | |
| Physical health | Physical health score (range 0–12) | 9.2 (2.3) | 8.6 (2.6) | 9.4 (2.2) | < .0001 |
| Behavioral health | Anxiety - GAD-7 score (range 0–21) | 5.2 (5.6) | 7.4 (6.1) | 4.7 (5.3) | < .0001 |
| Depression - PHQ 8 score (range 0–24) | 5.6 (5.6) | 8.0 (6.3) | 5.1 (5.3) | < .0001 | |
| PTSD - PCL-5 score (range 0–5) | 1.9 (1.8) | 2.4 (1.9) | 1.7 (1.8) | < .0001 | |
| Sex with casual partner after using alcohol, marijuana, or other drugs (% yes) | 10.5% (259) | 15.8% (69) | 9.4% (190) | < .0001 | |
| Sex with casual partner without condom (% yes) | 11.2% (275) | 14.5% (63) | 10.5% (212) | .02 | |
| Sleep problems (range 1–4) | 2.2 (0.8) | 2.4 (0.8) | 2.2 (0.7) | < .0001 | |
| Unmet treatment need | Unmet treatment need - alcohol/drug use (% yes) | 4.2% (105) | 6.1% (27) | 3.8% (78) | .03 |
| Unmet treatment need - mental health (% yes) | 16.6% (418) | 31.5% (140) | 13.4% (278) | < .0001 |
Note. SGM = sexual/gender minority. PTSD = Post-traumatic stress disorder. Group differences assessed using unadjusted bivariate t-tests (for continuous variables) or chi-squares (for categorical variables).
Alcohol Models
Predictors of intercept and slope of alcohol use
Figure 1 (panel a) shows percentages of past-month alcohol use across waves by SGM group. The first model examined SGM differences in the intercept and slope for alcohol use across waves 1–12, adjusting for age, sex, race/ethnicity, mother’s education, and intervention group. The intercept represents average probability of alcohol use at baseline (wave 1) and slope represents change in probability of use over time. Overall model fit was good: χ2 (163) = 570.25, RMSEA = 0.03, CFI = 0.95, SRMR = 0.08. Adjusting for covariates, there were no differences by SGM status on baseline probability of alcohol use (β = 0.15, p = .12) or rate of change in alcohol use over time (β = - 0.01, p = .89). Youths reporting Asian (vs. non-Hispanic White) race were less likely to use alcohol at baseline (β = - 0.67, p < .001) and older youth were more likely than younger ones to use alcohol at baseline (β = 0.18, p < .001). With regard to change over time, Asian (vs. non-Hispanic White) identifying youth had a steeper increase in use over time (β = 0.26, p = .03), while young people identifying as Hispanic (vs. non-Hispanic White) (β = −0.34, p = .002) and another race/ethnicity (β = −0.42, p = .01) had a less steep increase over time. Lastly, older youth had a less steep increase in alcohol use over time than younger ones (β = −0.13, p < .001).
Figure 1.
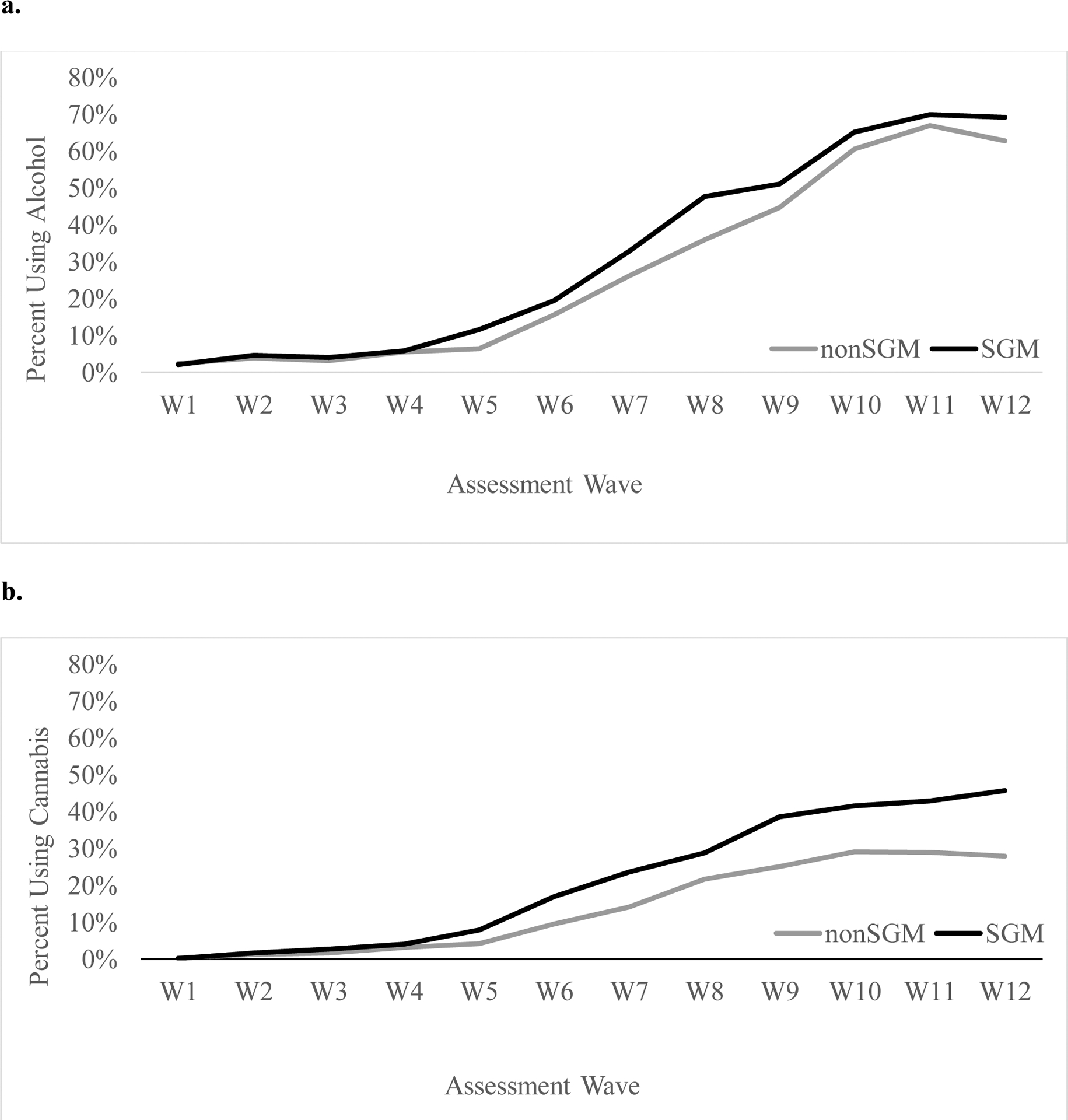
Rates of past-month alcohol and cannabis use from middle school through young adulthood by sexual and gender minority status
Note. This figure shows the percentage of individuals endorsing past-month alcohol (panel a.) and cannabis use (panel b.) by sexual/gender minority group at each assessment wave, from middle school (W1) through young adulthood (W12). W=wave. SGM = sexual/gender minority.
SGM differences for wave 12 outcomes controlling for alcohol use trajectories
The next model examined direct effects from SGM status to wave 12 outcomes, controlling for both the average (intercept) and rate of change (slope) of probability of alcohol use across waves 1– 12. Models also controlled for age, sex at birth, race/ethnicity, mother’s education, and CHOICE intervention condition at wave 1. This model can be interpreted as a test of the association between SGM status and outcomes at wave 12, assuming both groups demonstrated the same trajectories (i.e., fixed intercept and slope) in probability of alcohol use over time (waves 1–12). The overall model fit well (χ2 (352) = 1114.09, RMSEA = 0.03, CFI = 0.95, SRMR = 0.10). Results for direct effects of SGM status on outcomes, controlling for effects of alcohol use intercept and slope, are shown in Table 3. Full model results showing effects of use trajectory covariates (intercept; slope) on young adult outcomes are shown in supplemental Table S1. Briefly, higher average baseline probability of alcohol use (intercept) was associated with poorer outcomes across multiple domains, whereas rate of increase across waves (slope) showed inconsistent associations with outcomes in wave 12 (see Table S1).
Table 3.
Parameter estimates of sexual/gender minority status predicting wave 12 outcomes, controlling for alcohol/cannabis use trajectories
| Effect of SGM status, controlling for alcohol use (reference is non-SGM) |
Effect of SGM status, controlling for cannabis use (reference is non-SGM) |
||
|---|---|---|---|
| Domain | Outcome variable | β (95% CI [LL, UL]) p-value |
β (95% CI [LL, UL]) p-value |
| Education | Educational attainment post-high school (yes) | −0.106 (−0.412, 0.200) p = .497 |
−0.254 (−0.499, −0.009) p = .042* |
| Employment and economic stability | Currently unemployed (yes) |
0.252 (0.097, 0.407)
p = .001 ** |
0.301 (0.136, 0.466)
p < .001 ** |
| Number of times fired from job in past year |
0.337 (0.174, 0.501)
p < .001 ** |
0.317 (0.157, 0.476)
p <.001 ** |
|
| Experienced homelessness (yes) |
0.426 (0.174, 0.678)
p = .001 ** |
0.466 (0.236, 0.696)
p = .001 ** |
|
| Experienced food insecurity (yes) | 0.355 (0.037, 0.673) p = .029* |
0.519 (0.234, 0.804)
p = .001 ** |
|
| Transition to adult roles | IDEA scale | 0.114 (−0.079, 0.307) p = .246 |
0.068 (−0.051, 0.188) p = .261 |
| Criminal justice involvement | Instances of being in trouble with police in past year |
0.273 (0.135, 0.411)
p < .001 ** |
0.257 (0.139, 0.375) p < .001** |
| Social functioning | PROMIS Social Functioning score |
−0.226 (−0.363, −0.088)
p = .001 ** |
−0.257 (−0.371, −0.143)
p = .001 ** |
| Loneliness score |
0.503 (0.399, 0.607)
p < .001 ** |
0.553 (0.383, 0.723) p < .001** |
|
| Physical health | Physical health score |
−0.305 (−0.438, −0.171)
p < .001 ** |
−0.376 (−0.538, −0.214)
p < .001 ** |
| Behavioral health | Anxiety - GAD-7 score |
0.455 (0.355, 0.555)
p < .001 ** |
0.427 (0.320, 0.535)
p < .001 ** |
| Depression - PHQ 8 score |
0.544 (0.442, 0.646)
p < .001 ** |
0.514 (0.408, 0.621)
p < .001 ** |
|
| PTSD - PCL-5 score |
0.337 (0.158, 0.516)
p < .001 ** |
0.380 (0.178, 0.582)
p < .001 ** |
|
| Sex with casual partner after using alcohol, marijuana, or other drugs (yes) | 0.282 (0.036, 0.528) p = .025* |
0.085 (−0.131, 0.301) p = .439 |
|
| Sex with casual partner without condom (yes) | 0.201 (−0.010, 0.413) p = .062 |
0.081 (−0.119, 0.281) p = .428 |
|
| Sleep problems |
0.326 (0.217, 0.436)
p < .001 ** |
0.349 (0.220, 0.477)
p < .001 * |
|
| Unmet treatment need | Unmet treatment need for alcohol or other drug use (yes) | 0.192 (−0.101, 0.484) p = .199 |
0.302 (−0.009, 0.614) p = .057 |
| Unmet treatment need for mental health (yes) |
0.594 (0.434, 0.754)
p < .001 ** |
0.531 (0.375, 0.688)
p < .001 ** |
Note. Values are standardized estimates of the direct effect of sexual/gender minority group status on each outcome from sequelae of change models, adjusting for effects of alcohol or cannabis use intercept and slope from waves 1 to 12. Models also controlled for age, assigned sex at birth, race/ethnicity, mother’s education, and intervention group at wave 1. β = standardized model effect estimate. CI = confidence interval; LL = lower limit; UL = upper limit. SGM = sexual/gender minority. PTSD = Post-traumatic stress disorder. To account for alpha inflation due to multiple tests, we applied Benjamini-Hochberg False Discovery Rate correction for all estimates.
< .05;
and bolded text indicate statistically significant after correction for multiple tests.
At the same levels of use, compared to non-SGM respondents, SGM individuals were more likely to be currently unemployed (p < .001), reported more instances of being fired from a job (p < .001), and more instances of being in trouble with police (p < .001), and were more likely to experience homelessness (p < .001) in the past year. Additionally, compared to non-SGM peers, SGM individuals reported lower social functioning scores (p = .001) and higher loneliness scores (p < .001). SGM status was also associated with poorer subjective physical health (p < .001), higher ratings of anxiety (p < .001), depression (p < .001) and PTSD (p < .001) symptoms, poorer sleep quality (p < .001), and greater likelihood of unmet mental health treatment need in the past year (p < .001). SGM and non-SGM groups did not significantly differ with respect to post-high school education, IDEA scale scores, sexual risk behaviors, or perceived unmet treatment need for alcohol or other drug use.
Cannabis Models
Predictors of intercept and slope of cannabis use
Figure 1 (panel b) shows rates of current cannabis use at each wave, by SGM group. The first model examined SGM differences in the intercept and slope for cannabis use across waves 1–12, adjusting for age, sex, race/ethnicity, mother’s education, and intervention condition. Model fit was χ2 (163) = 739.28, RMSEA = 0.04, CFI = 0.94, SRMR = 0.11. The SGM and non-SGM groups did not significantly differ on initial probability of cannabis use. However, SGM status was significantly associated with change in probability of use over time (β = 0.27, p = 0.01). Specifically, those who identified at SGM had a steeper increase in cannabis use probability over time compared to non-SGM youths. In addition, older youths were more likely than younger ones to use cannabis at baseline (β = 0.17, p < .001) and had a less steep increase (slope) in cannabis use over time than younger individuals (β = −0.15, p < .001).
SGM differences for wave 12 outcomes controlling for cannabis use trajectories
We next examined direct effects from SGM status to wave 12 outcomes, controlling for both the intercept and slope of probability of cannabis use across waves 1– 12 along with age, sex at birth, race/ethnicity, mother’s education, and intervention condition. These models can be interpreted as a test of the association between SGM status and outcomes at wave 12, assuming all groups demonstrated the same trajectories (i.e., fixed intercept and slope) of probability of cannabis use over time (waves 1–12). The overall model fit well (χ2 (331) = 1252.03, p < .01, RMSEA = 0.03, CFI = 0.95, SRMR = 0.095). Effects of cannabis use trajectory covariates (intercept; slope) on young adult outcomes are shown in supplemental Table S1. Briefly, similar to the alcohol models, higher baseline probability of cannabis use (intercept) was consistently associated with poorer outcomes across multiple domains in wave 12 (see Table S1).
Differences in outcomes for SGM compared to non-SGM respondents at the same levels of cannabis use (i.e., effects of SGM status adjusting for cannabis trajectory intercept and slope) are shown in Table 3. The pattern of findings was virtually identical to that observed for the comparable alcohol models (see above), albeit with differences in magnitude of effects of SGM status on outcomes (based on standardized betas), such that SGM individuals showed consistent disparities across nearly all domains at the same level of cannabis use. In addition, as with the alcohol models, SGM status was not significantly associated with likelihood of post-high school education, IDEA scale scores, sexual risk behaviors, or perceived unmet treatment need for alcohol/drug use.
Sensitivity Analyses
Cross-sectional sensitivity analyses assessing differences between SGM and non-SGM groups adjusting for frequency of A or C use and demographic covariates at wave 12 showed nearly identical patterns to those observed in the sequelae of change models. That is, the SGM group showed consistently poorer functioning across nearly all domains (see Table S2).
Discussion
This study examined the emergence of health, psychosocial, and other disparities for SGM young adults compared to non-SGM peers after controlling for trajectories of alcohol and cannabis use. We extend the existing literature on disparities in functioning for SGM individuals by showing that functional disparities manifest as early as young adulthood, are evident even after accounting for trajectories of alcohol or cannabis use, and appear across multiple different domains (e.g., economic stability, including homelessness and food insecurity; police involvement; behavioral health; social functioning; physical health; unmet need for mental health treatment). Overall, findings indicate that SGM young people may experience disproportionately negative outcomes relative to non-SGM peers – even at the same levels (i.e., fixed trajectories) of alcohol and cannabis use during early life.
In contrast to other studies examining trajectories of alcohol use across SGM and non-SGM groups (e.g., Corliss et al., 2008; Coulter et al., 2008; Dermody et al., 2019; Fish & Pasley, 2015; Hatzenbuehler et al., 2008; Marshal et al., 2009), we did not observe differences between groups in alcohol use trajectories. Several explanations, which are not mutually exclusive, may help explain this contrasting finding. First, there are potential differences across samples. For example, a substantial portion of the previous longitudinal research has been conducted with data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), which represents a significantly older cohort. Although those analyses have used data from a similar age span, most Add Health participants are now in their late 30s and 40s (Harris et al., 2019), and their adolescence and young adulthood reflects a different historical context and likely a different lived experience. While there is still significant room for improvement, there have been dramatic social changes in acceptance of SGM persons over the past two decades (Poushter & Kent, 2020; McCarthy, 2019). Other SGM alcohol trajectory research has drawn from samples such as the Growing Up Today Study (e.g., Coulter et al., 2018) or the Pittsburgh Girls Study (e.g., Dermody et al., 2019). Each of these samples has its own limitations to generalizability; the former is a cohort of children of Nurse’s Health Study II participants, and the latter is a sample of youth who were female at enrollment and also recruited from a limited geographic area. Further, differences may be explained by different statistical methods and age ranges used to model trajectories across studies. For example, in contrast to this study, Coulter and colleagues used longitudinal latent class analysis to examine alcohol trajectory classes in emerging adulthood (ages 18 to 25) (Coulter et al., 2018). A related explanation for our null finding related to alcohol trajectories is our focus on any versus no current use. Due to low rates of use in early waves, we were unable to model trajectories based on more nuanced patterns of use (e.g., frequency of use; although note: cross-sectional comparisons at wave 12 also revealed no difference across SGM and non-SGM groups on frequency of past-month alcohol use). Still, given the preponderance of youths identifying as bisexual in this sample, we might have expected alcohol trajectory disparities to emerge. Bisexual youth (e.g., Fish & Baams, 2018) and adults (e.g., Hughes et al., 2020), particularly female-identified persons, tend to have greater alcohol-related disparities relative to other sexual minority subgroups or heterosexual peers. However, much of this emerges from cross-sectional studies and samples that have limitations similar to those already mentioned. Although we were unable to disaggregate the SGM group due to relatively small cell sizes, this consideration is relevant to future longitudinal research. Given the growing attention to SGM health disparities over the past decade and accompanying interest and calls to measure SGM status in health research (Institute of Medicine, 2011; National Academies of Sciences, Engineering, and Medicine, 2020), future longitudinal studies with larger, more representative samples may be better able to shed light on contemporary comparisons and within-SGM subgroup differences.
We did, however, observe differences between SGM and non-SGM young people with respect to increases in cannabis use probability from middle school through young adulthood, such that SGM young people showed significantly steeper increases compared to their non-SGM peers. In addition, at wave 12, rates of past-month cannabis use were 1.6 times greater in the SGM group compared to the non-SGM group. This is consistent with other studies, which have documented significantly higher rates of cannabis use among SGM young adults compared to cisgender/heterosexual peers (Schuler et al., 2018). Prevention efforts in early/middle adolescence may be needed to address cannabis use before SGM youths progress to more established use. This may be particularly important in areas where cannabis is legally accessible for adults ages 21 and over, such as California.
There are few empirically supported substance use prevention and treatment programs that are specifically tailored to SGM adolescents (Coulter et al., 2019). However, prior work suggests potentially promising avenues for future prevention/intervention development. For example, the greater prevalence of cannabis and other substance use within networks of SGM youth may be perpetuated in part through more permissive norms and greater exposure to peer use (National Academies of Sciences, Engineering, and Medicine, 2020; Pollard et al., 2010), which may in turn increase risks of problem use and use-related negative consequences. Efforts to explicitly integrate tailored norm-related content along with peer refusal strategies into prevention programming for SGM adolescents may help decrease the likelihood of progression to problematic use as these young people mature into young adults. This is especially relevant in the contemporary context, where cannabis legalization may make its use increasingly normative (Koval et al., 2019). Future studies should also examine the motivations and contexts of cannabis use among SGM adolescents, and whether these differ from those of non-SGM adolescents. Such research can also shed light on both risk and protective factors, which could identify potential leverage points for reducing harms.
We observed significant disparities for SGM young adults compared to non-SGM peers across multiple domains after accounting for A or C use from middle school through young adulthood, including: unemployment and economic stability (e.g., being fired from a job; experiencing homelessness), social functioning (e.g., loneliness), behavioral health (e.g., anxiety and depression symptoms; sleep quality; unmet mental health treatment need), and subjective physical health. We also found that, compared to non-SGM peers, SGM young people experienced more instances of being in trouble with the police. This pattern is consistent with prior reports of disparities for SGM individuals across different domains (Institute of Medicine, 2011). However, the current findings significantly extend the existing literature by showing the emergence of this breadth of disparities within a single community-based cohort of young adults and after accounting for longitudinal patterns of two of the most commonly used substances, which have been identified as important contributors to SGM health and other disparities.
Collectively, our findings further support the notion that other factors beyond substance use, namely social and structural stressors, drive the emergence of SGM disparities for young adults. Social and structural stressors experienced by SGM youths include familial rejection and perceived or experienced lack of school or community supports (National Academies of Sciences, Engineering, and Medicine, 2020; Russell & Fish, 2016). SGM young people also experience disproportionately high rates of bullying, discrimination, and victimization during middle and high school that may increase risk of substance use along with a host of other negative outcomes (Poteat et al., 2014; Russell & Fish, 2016). Such stressful experiences help to account for the disparities in substance use disorders evident for SGM individuals (Krueger et al., 2020). Therefore, it may be more prudent to view substance use as part of a syndemic rather than as a primary driver of poorer outcomes for SGM young people (Anderson et al., 2020; Coulter et al., 2015; Stall et al., 2008). A syndemic involves the intersections and interactions between multiple co-occurring biopsychosocial problems and unmet needs in a population (Singer & Clair, 2003). Prior research, particularly regarding HIV disparities, has demonstrated the role of marginalization, including violence and discrimination, as a key syndemic risk factor (Herrick et al., 2014; Meyer et al., 2011; Poteat et al., 2016). Although preventing and reducing early substance use may be necessary to help improve well-being for SGM young people, it is likely insufficient to address the full range of disparities experienced by SGM young adults. Interventions seeking to address SGM substance use must also account for social and structural factors that increase substance use risk. In addition, efforts to improve SGM outcomes across a range of functional domains also need to shift upstream and beyond more proximal symptoms of marginalization, including substance use.
Limitations
Our findings should be considered in the context of several limitations. First, although a considerable strength of the study is its examination of substance use trajectories from middle school through young adulthood, this approach imposed some analytic limitations. Specifically, due to low rates of use in earlier study waves when youth were in middle school, models of alcohol and cannabis use were based on dichotomous indicators of any vs no use at each time point rather than frequency of use. Furthermore, the purpose of the study was to assess SGM and non-SGM differences in functioning in young adulthood after accounting for longitudinal patterns of substance use in early life. However, associations between substance use and many of the outcomes of interest in this study are likely reciprocal, and we did not assess bidirectional associations between substance use and functioning over time. Additional work is needed to understand how SGM and non-SGM youths may differ with respect to the way in which patterns of substance use and functional problems jointly manifest over the course of early development. In addition, although we used multiple identity and behavior items to characterize SGM status, items were based on self-report at a single time point, coinciding with data collection of our outcome variables. It is possible that SGM status may change over time. However, studies examining identity transitions have found that the majority of those indicating shifts in sexual orientation and gender identity are likely to remain within the overall SGM umbrella (Ott et al., 2011; Saewyc et al., 2012). We were also unable to assess differences by specific sexual orientation or gender identity subgroups due to small cell sizes, which is an important limitation as past work has documented differences in rates of alcohol and cannabis use by sexual orientation and gender subgroups (Coulter et al., 2019; Mereish, 2018; Schuler et al., 2018). Moreover, we did not assess disparities in relation to intersecting identities (e.g., SGM young people who are also racial or ethnic minorities) (Crenshaw, 2017; Balsam et al., 2011). Future work is needed to better understand the emergence of alcohol and cannabis-related disparities across subgroups of SGM individuals.
Conclusion
Overall, our findings highlight that, compared to non-SGM peers, SGM young adults experience disproportionate hardships spanning numerous domains, even at similar levels of alcohol and cannabis use. Although it is important to address substance use during early life, prevention programs are unlikely to fully resolve these disparities for SGM young people. Additional efforts to address the specific hardships experienced by SGM youths as they enter young adulthood, including the numerous chronic stressors and systemic challenges that they face on a daily basis are needed to help addresses the causes and disproportionate consequences of alcohol and cannabis use among SGM young adults.
Supplementary Material
Public Significance Statement.
This study finds that disparities in multiple domains of functioning experienced by sexual and gender minority young adults are substantial compared to heterosexual and cisgender peers, even at similar levels of alcohol or cannabis use during early life.
In addition to substance use interventions, there is a parallel need to address the unique hardships, stressors, and systemic challenges experienced by sexual and gender diverse youths that may increase substance use and disparities in multiple domains as they enter young adulthood.
Acknowledgments
This work was supported by grants from the National Institute of Alcohol Abuse and Alcoholism at the National Institutes of Health (R01AA016577; R01AA020883, R01AA025848; R01AA025848-04S1: D’Amico). The authors have no conflicts of interest to disclose. Analysis code for this study is available upon reasonable request by emailing the corresponding author. Data are not yet available as the parent study is still in progress.
References
- Anderson JC, Chugani CD, Jones KA, Coulter RWS, Chung T, & Miller E (2020). Characteristics of precollege sexual violence victimization and associations with sexual violence revictimization during college. Journal of American College Health, 68(5), 509–517. doi: 10.1080/07448481.2019.1583237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ (1998). Learning to stand alone: the contemporary American transition to adulthood in cultural and historical context. Human Development, 41, 295–315. [Google Scholar]
- Arnett JJ (2000). Emerging adulthood - A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. doi: 10.1037//0003-066x.55.5.469 [DOI] [PubMed] [Google Scholar]
- Arnett JJ, Žukauskienė R, & Sugimura K (2014). The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. The Lancet Psychiatry, 1(7), 569–576. doi: 10.1016/s2215-0366(14)00080-7 [DOI] [PubMed] [Google Scholar]
- Asparouhov TMB (2010). Weighted least squares estimation with missing data. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Baggio S, Iglesias K, Studer J, & Gmel G (2015). An 8-item short form of the Inventory of Dimensions of Emerging Adulthood (IDEA) among young Swiss men. Evaluation & the Health Professions, 38(2), 246–254. doi: 10.1177/0163278714540681 [DOI] [PubMed] [Google Scholar]
- Balsam KF, Molina Y, Beadnell B, Simoni J, & Walters K (2011). Measuring multiple minority stress: the LGBT People of Color Microaggressions Scale. Cultural Diversity and Ethnic Minority Psychology, 17(2), 162–174. doi: 10.1037/a0023244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, & Hochber Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B (Methodological), 57(1), 289–300. [Google Scholar]
- Blevins CA, Weathers F, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. Journal of Trauma and Stress, 28(6), 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Butler ES, McGlinchey E, & Juster RP (2020). Sexual and gender minority sleep: a narrative review and suggestions for future research. Journal of Sleep Research, 29(1), e12928. doi: 10.1111/jsr.12928 [DOI] [PubMed] [Google Scholar]
- Buysse DJ (2014). Sleep health: can we define it? Does it matter? Sleep, 37(1), 9–17. doi: 10.5665/sleep.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2018). 2019 National Survey on Drug Use and Health (NSDUH): CAI Specifications for Programming (English Version). Retrieved from https://www.samhsa.gov/data/
- Chartier K, & Caetano R (2010). Ethnicity and health disparities in alcohol research. Alcohol Research and Health 33(1–2), 152–160. [PMC free article] [PubMed] [Google Scholar]
- Corliss HL, Rosario M, & Wypij D (2008). Sexual orientation disparities in longitudinal alcohol use patterns among adolescents. Archives of Pediatric and Adolescent Medicine, 162(11), 1071–1078. doi: 10.1001/archpedi.162.11.1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corliss HL, Rosario M, Wypij D, Wylie SA, Frazier AL, & Austin SB (2010). Sexual orientation and drug use in a longitudinal cohort study of U.S. adolescents. Addictive Behaviors, 35(5), 517–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter RW, Kinsky SM, Herrick AL, Stall RD, & Bauermeister JA (2015). Evidence of syndemics and sexuality-related discrimination among young sexual-minority women. LGBT Health, 2(3), 250–257. doi: 10.1089/lgbt.2014.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter RWS, Egan JE, Kinsky S, Friedman MR, Eckstrand KL, Frankeberger J, … & Miller E. (2019). Mental health, drug, and violence interventions for sexual/gender minorities: a systematic review. Pediatrics, 144(3), e2018336. doi: 10.1542/peds.2018-3367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter RWS, Jun H, Calzo JP, Truong NL, Mair C, Markovic N, … & Corliss HL. (2018). Sexual-orientation differences in alcohol use trajectories and disorders in emerging adulthood: results from a longitudinal cohort study in the United States. Addiction, 113, 1619–1632. doi: 10.1111/add.14251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter RWS, Ware D, Fish JN, & Plankey MW (2019). Latent classes of polysubstance use among adolescents in the United States: intersections of sexual identity with sex, age, and race/ethnicity. LGBT Health, 6(3), 1–6. doi: 10.1089/lgbt.2018.0149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw KW (2017). On intersectionality: Essential writings. New York, NY: The New Press. [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, & Pedersen ER (2016). Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: examining use patterns from age 11 to 17 years. Addiction, 111(10), 1825–1835. doi: 10.1111/add.13442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, & Green HD (2012). Preventing alcohol use with a voluntary after-school program for middle school students: results from a cluster randomized controlled trial of CHOICE. Prevention Science, 13(4), 415–425. doi: 10.1007/s11121-011-0269-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dermody SS, McGinley J, Eckstrand K, & Marshal MP (2019). Sexual minority female youth and substance use disparities across development. Journal of LGBT Youth, 17(2), 214–229. doi: 10.1080/19361653.2019.1598313 [DOI] [Google Scholar]
- DeWalt DA, Thissen D, Stucky BD, Langer M, Morgan DE, Irwin D, … Varni J. (2013). PROMIS pediatric peer relationships scale: development of a peer relationships item bank as part of social health measurement. Health Psychology 32(10), 1093–1103. doi: 10.1037/a0032670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, & Strycker LA (1999). An introduction to latent variable growth curve modeling: Concepts, issues, and applications. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Fish JN, & Baams L (2018). Trends in alcohol-related disparities between heterosexual and sexual minority youth from 2007 to 2015: Findings from the Youth Risk Behavior Survey. LGBT Health, 5(6), 359–367. doi: 10.1089/lgbt.2017.0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, Bishop MD, & Russell ST (2021). Developmental differences in sexual orientation and gender identity-related substance use disparities: findings from population-based data. Journal of Adolescent Health, 68(6), 1162–1169. doi: 10.1016/j.jadohealth.2020.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, & Pasley K (2015). Sexual (minority) trajectories, mental health, and alcohol use: a longitudinal study of youth as they transition to adulthood. Journal of Youth and Adolescence, 44(8), 1508–1527. doi: 10.1007/s10964-015-0280-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbach JT, & Gibbs JJ (2017). A developmentally informed adaptation of minority stress for sexual minority adolescents. Journal of Adolescence, 55, 36–50. doi: 10.1016/j.adolescence.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson KL, Medina KL, Padula CB, Tapert SF, & Brown SA (2011). Impact of adolescent alcohol and drug use on neuropsychological functioning in young adulthood: 10-year outcomes. Journal of Child & Adolescent Substance Abuse, 20(2), 135–154. doi: 10.1080/1067828X.2011.555272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel EA, Hussey JM, Killeya-Jones LA, Tabor J, & Dean SC (2019). Cohort profile: The national longitudinal study of adolescent to adult health (Add health). International Journal of Epidemiology, 48(5), 1415–1415k. doi: 10.1093/ije/dyz115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, & Fromme K (2008). Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: results from a prospective study. Developmental Psychology, 44(1), 81–90. doi: 10.1037/0012-1649.44.1.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick A, Stall R, Egan J, Schrager S, & Kipke M (2014). Pathways towards risk: syndemic conditions mediate the effect of adversity on HIV risk behaviors among young men who have sex with men (YMSM). Journal of Urban Health, 91(5), 969–982. doi: 10.1007/s11524-014-9896-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: results from two population-based studies. Research on Aging, 26(6), 655–672. doi: 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Veldhuis CB, Drabble LA, & Wilsnack SC (2020). Research on alcohol and other drug (AOD) use among sexual minority women: A global scoping review. PLoS one, 15(3), e0229869. doi: 10.1371/journal.pone.0229869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughto JMW, Quinn E, Dunbar MS, Rose AJ, Shireman TI, & Jasuja GK (2021). Prevalence and Co-occurrence of Alcohol, Nicotine, and Other Substance Use Disorder Diagnoses Among US Transgender and Cisgender Adults. JAMA Network Open, 4(2), e2036512. doi: 10.1001/jamanetworkopen.2020.36512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, Committee on Lesbian, Gay, & Bisexual and Transgender Health Issues and Research Gaps and Opportunities. (2011). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies. [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, & Schulenberg JE (2016). Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor, MI: University of Michigan, Institute for Social Research. [Google Scholar]
- Katz-Wise SL, Rosario M, Calzo JP, Scherer EA, Sarda V, & Austin SB (2017). Endorsement and Timing of Sexual Orientation Developmental Milestones Among Sexual Minority Young Adults in the Growing Up Today Study. Journal of sex research, 54(2), 172–185. doi: 10.1080/00224499.2016.1170757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koval AL, Kerr DCR, & Bae H (2019). Perceived prevalence of peer marijuana use: changes among college students before and after Oregon recreational marijuana legalization. The American Journal of Drug and Alcohol Abuse, 45(4), 392–399. doi: 10.1080/00952990.2019.1599381 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. [DOI] [PubMed] [Google Scholar]
- Krueger EA, Fish J, & Upchurch DM (2020). Sexual orientation disparities in substance use: investigating social stress mechanisms in a national sample. American Journal of Preventive Medicine, 58(1), 59–68. doi: 10.1016/j.amepre.2019.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, … & Morse JQ. (2008). Sexual orientation and adolescent substance use: a meta-analysis and methodological review. Addiction, 103(4), 546–556. doi: 10.1111/j.1360-0443.2008.02149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, & Thompson AL (2009). Individual trajectories of substance use in lesbian, gay and bisexual youth and heterosexual youth. Addiction, 104(6), 974–981. doi: 10.1111/j.1360-0443.2009.02531.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, & Boyd CJ (2010). The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 100, 1946–1952. doi: 10.2105/AJPH.2009.163147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy J (2019). Gallup first polled on gay issues in ‘77. What has changed? Gallup Poll Social Series. Gallup. Washington, D.C. Access date: September 14, 2021. https://news.gallup.com/poll/258065/gallup-first-polled-gay-issues-changed.aspx [Google Scholar]
- McInroy LB, Beaujolais B, Leung VW, Craig SL, Eaton AD, & Austin A (2020). Comparing asexual and non-asexual sexual minority adolescents and young adults: stressors, suicidality and mental and behavioural health risk outcomes. Psychology & Sexuality. doi: 10.1080/19419899.2020.1806103 [DOI] [Google Scholar]
- Mereish EH (2018). Addressing research gaps in sexual and gender minority adolescents’ substance use and misuse. Journal of Adolescent Health, 62(6), 645–646. doi: 10.1016/j.jadohealth.2018.03.011 [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JP, Springer SA, & Altice FL (2011). Substance abuse, violence, and HIV in women: a literature review of the syndemic. Journal of Women’s Health, 20(7), 991–1006. doi: 10.1089/jwh.2010.2328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Yu Y, Greenfield TK, & Zemore SE (2009). Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcoholism, Clinical and Experimental Research, 33(4), 654–662. doi: 10.1111/j.1530-0277.2008.00880.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus User’s Guide (Eighth Edition ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2019). The Promise of Adolescence: Realizing Opportunity for All Youth. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2020). Understanding the Well-Being of LGBTQI+ Populations. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Ott MQ, Corliss HL, Wypij D, Rosario M, & Austin SB (2011). Stability and change in self-reported sexual orientation identity in young people: application of mobility metrics. Archives of Sexual Behavior, 40(3), 519–532. doi: 10.1007/s10508-010-9691-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, & Richman LS (2009). Perceived discrimination and health: a meta-analytic review. Psychological Bulletin, 135(4), 531–554. doi: 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard MS, Tucker JS, Green HD, Kennedy D, & Go MH (2010). Friendship networks and trajectories of adolescent tobacco use. Addictive Behaviors, 35(7), 678–685. doi: 10.1016/j.addbeh.2010.02.013 [DOI] [PubMed] [Google Scholar]
- Poteat T, Scheim A, Xavier J, Reisner S, & Baral S (2016). Global Epidemiology of HIV Infection and Related Syndemics Affecting Transgender People. Journal of Acquired Immune Deficiency Syndromes, 72 Suppl 3, S210–219. doi: 10.1097/QAI.0000000000001087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat VP, Scheer JR, & Chong ESK (2016). Sexual orientation-based disparities in school and juvenile justice discipline: A multiple group comparison of contributing factors. Journal of Educational Psychology, 108(2), 229–241. doi: 10.1037/edu0000058 [DOI] [Google Scholar]
- Poteat VP, Scheer JR, & Mereish EH (2014). Factors affecting academic achievement among sexual minority and gender-variant youth. Advances in Child Development and Behavior, 47, 261–300. doi: 10.1016/bs.acdb.2014.04.005 [DOI] [PubMed] [Google Scholar]
- Poushter J, & Kent N (2020). The global divide on homosexuality persists. Pew Research Center. Washington, DC. Access date: September 14, 2021. https://www.pewresearch.org/global/2020/06/25/global-divide-on-homosexuality-persists/ [Google Scholar]
- Russell ST, & Fish JN (2016). Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annual Review of Clinical Psychology, 12, 465–487. doi: 10.1146/annurev-clinpsy-021815-093153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saewyc EM (2011). Research on adolescent sexual orientation: Development, health disparities, stigma and resilience. Jouranl of Research on Adolescence, 21(1), 256–272. doi: 10.1111/j.1532-7795.2010.00727.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schat ACH, Kelloway EK, & Desmarais S (2005). The Physical Health Questionnaire (PHQ): construct validation of a self-report scale of somatic symptoms. Journal of Occupational Health Psychology, 10(4), 363–381. doi: 10.1037/1076-8998.10.4.363 [DOI] [PubMed] [Google Scholar]
- Scholes-Balog KE, Hemphill SA, Evans-Whipp TJ, Toumbourou JW, & Patton GC (2016). Developmental trajectories of adolescent cannabis use and their relationship to young adult social and behavioural adjustment: A longitudinal study of Australian youth. Addictive Behaviors, 53, 11–18. doi: 10.1016/j.addbeh.2015.09.008 [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Sameroff AJ, & Cicchetti D (2004). The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology, 16(4), 799–806. doi: 10.1017/S0954579404040015 [DOI] [PubMed] [Google Scholar]
- Schuler MS, Rice CE, Evans-Polce RJ, & Collins RL (2018). Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug & Alcohol Dependence, 189, 139–146. doi: 10.1016/j.drugalcdep.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Stein BD, & Collins RL (2019). Differences in substance use disparities across age groups in a natinoal cross-sectional survey of lesbian, gay, and bisexual adults. LGBT Health, 6(2), 1–9. doi: 10.1089/lgbt.2018.0125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M, & Clair S (2003). Syndemics and public health: Reconceptualizing Disease in Bio-Social Context. Medical Anthropology Quarterly, 17(4), 423–441. doi: 10.1525/maq.2003.17.4.423 [DOI] [PubMed] [Google Scholar]
- Sontag-Padilla L, Dunbar MS, Seelam R, Kase CA, Setodji CM, & Stein BD (2017). California Community College Faculty and Staff Help Address Student Mental Health Issues. Retrieved from Santa Monica, CA: https://www.rand.org/pubs/research_reports/RR2248.html [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Lowe B (2006). A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine, 166, 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stall R, Friedman M, & Catania JA (2008). Interacting Epidemics and Gay Men’s Health: A Theory of Syndemic Production among Urban Gay Men. In Wolitski RJ, Stall R, & Valdiserri RO (Eds.), Unequal Opportunity: Health Disparities Affecting Gay and Bisexual Men in the United States (pp. 251–274). New York, NY: Oxford University Press. [Google Scholar]
- Tate CC, Ledbetter JN, & Youssef CP (2013). A two-question method for assessing gender categories in the social and medical sciences. Journal of Sex Research, 50(8), 767–776. doi: 10.1080/00224499.2012.690110 [DOI] [PubMed] [Google Scholar]
- Thompson K, Leadbeater B, Ames M, & Merrin GJ (2019). Associations between marijuana use trajectories and educational and occupational success in young adulthood. Prevention Science, 20(2), 257–269. doi: 10.1007/s11121-018-0904-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trim RS, Meehan BT, King KM, & Chassin L (2007). The relation between adolescent substance use and young adult internalizing symptoms: findings from a high-risk longitudinal sample. Psychology of Addictive Behaviors, 21(1), 97–107. doi: 10.1037/0893-164X.21.1.97 [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, Orlando M, Martino SC, & Klein DJ (2005). Substance use trajectories from early adolescence to young adulthood: A comparison of smoking, binge drinking, and marijuana use. Journal of Drug Issues, 35(2), 307–332. doi: 10.1177/002204260503500205 [DOI] [Google Scholar]
- Williams DR, & Mohammed SA (2009). Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine, 32(1), 20–47. doi: 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


