Abstract
Objective
To assess the potential bidirectional relationship between food insecurity and HIV infection in sub-Saharan Africa.
Design
Nationally representative HIV impact assessment household-based surveys.
Setting
Zambia, Eswatini, Lesotho, Uganda and Tanzania and Namibia.
Participants
112 955 survey participants aged 15–59 years with HIV and recency test results.
Measures
Recent HIV infection (within 6 months) classified using the HIV-1 limited antigen avidity assay, in participants with an unsuppressed viral load (>1000 copies/mL) and no detectable antiretrovirals; severe food insecurity (SFI) defined as having no food in the house ≥three times in the past month.
Results
Overall, 10.3% of participants lived in households reporting SFI. SFI was most common in urban, woman-headed households, and in people with chronic HIV infection. Among women, SFI was associated with a twofold increase in risk of recent HIV infection (adjusted relative risk (aRR) 2.08, 95% CI 1.09 to 3.97). SFI was also associated with transactional sex (aRR 1.28, 95% CI 1.17 to 1.41), a history of forced sex (aRR 1.36, 95% CI 1.11 to 1.66) and condom-less sex with a partner of unknown or positive HIV status (aRR 1.08, 95% CI 1.02 to 1.14) in all women, and intergenerational sex (partner ≥10 years older) in women aged 15–24 years (aRR 1.23, 95% CI 1.03 to 1.46). Recent receipt of food support was protective against HIV acquisition (aRR 0.36, 95% CI 0.14 to 0.88).
Conclusion
SFI increased risk for HIV acquisition in women by twofold. Heightened food insecurity during climactic extremes could imperil HIV epidemic control, and food support to women with SFI during these events could reduce HIV transmission.
Keywords: epidemiology, HIV & AIDS, nutrition
Strengths and limitations of this study.
This study of 112 955 adults across six countries in sub-Saharan Africa is a large multinational sample surveyed across multiple different economic and environmental contexts.
The large number of participants allowed the analysis of potential behavioural and biological mediators between food insecurity and HIV acquisition.
The response rates were consistently higher than 80%, but there is always the potential for bias towards self-selection of lower risk respondents in any survey.
The cross-sectional nature of the study did not allow us to determine the direction of the relationship between food shortages and HIV acquisition with certainty.
The limited antigen avidity assay has limitations in estimation of HIV incidence as the algorithm used to classify someone as recently infected excludes anyone who might have started antiretroviral drugs within the first 6 months of infection.
Introduction
Climate change and its consequences are having a profound and escalating impact on global health. Acute events such as cyclones and flooding are predicted to become more frequent and severe, as are slower-onset changes such as drought and temperature extremes. These changes impact all domains of food security, including availability, access and utilisation.1–3 Trends in world hunger have slowly reverted from a steady decline to a yearly increase, with a particular rise in sub-Saharan Africa (SSA), where almost 20% of the population is undernourished.4 5 Even predating the COVID-19 pandemic, models predicted that the risk of hunger and malnutrition globally could increase by 20% by 2050, generating humanitarian need in 200 million people per year,6 with the problem currently exacerbated by the economic impacts of the pandemic and the war in Ukraine.7–9 Urbanisation in Africa is also driving environmental degradation and climate emissions, with the potential for rapidly worsening agricultural outputs.10 11 Food insecurity impacts every facet of society, including political stability, economic productivity and population displacement.
Food insecurity can be either acute or chronic.12 The primary drivers of transitory food insecurity relate to prices and availability, which are sensitive to environmental stressors, whereas chronic food insecurity is driven more by poverty.13 Acute food insecurity is a sensitive measure of economic shock and can capture changes in wealth that might prompt changes in health-related behaviours or trigger coping strategies, such as exchanging sex for food.14–16
The HIV pandemic has had a bidirectional link to food insecurity,17 as the associated health consequences can drive lower productivity and decreased labour mobility, whereas food insecurity can increase HIV risk behaviours, disruptions in care and higher mortality.15–19 The impact has been assumed to be gendered in that women are particularly vulnerable to income shocks and to disruption to access to health resources.20 Food insecurity has also been associated with lower efficacy of antiretroviral treatment (ART) due to drug malabsorption or decreased adherence, with virological failure.21–23 As countries pursue the new UNAIDS 95-95-95 goals, weather extremes disrupting food production and supplies could jeopardise epidemic control, both in terms of increased risk behaviours, as well as disruption of treatment due to displacement or poverty, impacting access to testing and ART services.24 This results in increasing community-level infectiousness, driving the synergistic relationship between land degradation, vulnerability to drought, food insecurity and HIV transmission.25 26
The Population-Based HIV Impact Assessments (PHIAs), a series of national household-based surveys which collected data on the prevalence of HIV, recent HIV infection and viral load suppression (VLS), were conducted in several countries in SSA beginning in 2015. These surveys provide a unique opportunity to assess the relationship between food insecurity and HIV incidence in a large representative cohort of individuals. We used a theoretical framework to explore the relationships between food shortages, HIV and behavioural and biological mediators (online supplemental figure 1, appendix p 2).
bmjopen-2021-058704supp001.pdf (2.3MB, pdf)
Methods
Survey design
We used data from all PHIA surveys collecting data on household food availability between 2015 and 2018 (Eswatini, Lesotho, Namibia, Tanzania, Uganda and Zambia).27–32 Surveys employed a two-stage sampling design to select a nationally representative sample of people aged 0–59 years or greater in each country, which have previously been described.33 34 The first-stage sampling units were enumeration areas (EAs) selected with probabilities proportionate to the number of households in the EA, with allocation to subnational areas designed to achieve 30% precision around a national estimate of incidence and 95% CIs of ±0.10 for regional estimates of VLS in individuals aged 15–49 years. The survey sample weights were adjusted to compensate for the variable probabilities of selection for the complex sample design, differential non-response rates within relevant subgroups of the sample and undercoverage of certain populations. Further details on sampling are provided in the online supplemental appendix (p. 6), and in country final reports.33
Consenting heads of households provided a roster of household members, who separately consented to interviews and household-based HIV testing.
The period during which the surveys were conducted spanned different climate contexts, ranging from intense drought to overly wet conditions and flooding, described in the appendix (online supplemental figures 2–5, appendix pp 3–5).
Patient and public involvement
Patients were not involved directly in the formation of this study, although representatives from organisations representing people living with HIV were consulted as part of the questionnaire design, and as part of dissemination activities.
Procedures
Interviewers administered the household questionnaire, which captured data from the household head on household assets, receipt of social support in the past 3 months, and access to food as measured by the Household Food Insecurity Access Scale Indicator Guide.35 Further variable descriptions, including the questions used and the construction of our exposure, are provided in the online supplemental appendix p 6. The adult questionnaire was administered to all eligible participants aged 15 years and older during face-to-face interviews using Google Nexus 9 tablets. The questionnaire included questions on lifetime (excluding Tanzania) and recent sexual behaviours (past 12 months), and on characteristics of the three most recent sexual partners. Sampling design and questionnaire specifics are included in the online supplemental appendix pp 6,7.
Survey staff tested participants for HIV using the national algorithm. HIV RNA in plasma and dried blood spots (DBS) was measured using real-time PCR. Laboratory staff at the University of Cape Town conducted qualitative screening for detection of the most commonly used antiretrovirals (ARVs) with long half-lives on DBS specimens from all HIV-infected adults. Staff used the HIV-1 limited antigen (LAg) avidity immunoassay to classify recent infection in HIV-positive samples, where samples with a normalised optical density below 1.5 which did not have VLS (defined as HIV RNA <1000 copies/mL) and without detectable ARVs, were considered indicative of recent infection, with a mean duration of infection of 130 days (95% CI 118 to 142) in all countries aside from Uganda (153 days, 95% CI 127 to 178).36 We calculated annualised incidence estimates using the WHO incidence formula.37
Statistical analysis
We restricted our analysis to participants aged 15–59 years who had been tested for HIV. All analyses were conducted in Stata V.15.1, with the country-specific sampling weights allowing each country in the pooled data analysis to be self-representing for its population size. Taylor series weights were used for variance estimation. All presented percentages and estimates are weighted whereas numbers are crude.
We defined severe food insecurity as a household having no food in the house at least three times in the past 4 weeks. Receipt of food support was defined as having received food regardless of receipt of other support. The dependency ratio was calculated by dividing the number of children on the household roster by the number of adults, multiplied by 100, and then divided into quartiles. Household wealth quintiles were constructed at the country level using Principal Component Analysis based on household assets and infrastructure.38 Transactional sex was defined as having exchanged sex for material support or having sold sex in the past 12 months. Early sexual debut was sex occurring before age 15 years, and intergenerational sex as partnering with someone at least 10 years older. High-risk sex was defined as having sex without a condom with someone with an unknown or positive HIV status.
We estimated community-level viraemia as the weighted proportion of all adults in the sampled EA with a viral load ≥1000 copies/mL, regardless of serostatus and excluding those recently infected to avoid biasing our analysis by including those with the outcome in the exposure variable.26
We ran two main analyses: (1) severe food insecurity as the outcome and (2) recent HIV as the outcome and severe food insecurity as the exposure, using similar methodology. We used logistic regression for model 1, retaining in our multivariable model all variables with a p<0.20 in the univariable analysis, then retaining significant variables (p<0.10) in the final model. Goodness of fit of our final model was tested using Hosmer-Lemeshow test. We included urbanicity, sex, household wealth quintile, country and age as categorical variables in all models a priori, based on our theoretical framework.25 39 40 For model 2, we used Poisson regression due to the rarity of recent HIV as an outcome with stratified analyses by sex, due to evidence of inequity in impact of severe food insecurity.16 We also analysed mediating behaviours identified in our framework using Poisson regression in a similar fashion to model 2, restricted to those reporting ever having sexual activity, aside from the analysis of early sexual debut. We restricted our analysis of intergenerational sex to young women aged 15–24 years as these partnerships are particularly risky in this age group.41 42 We excluded data from Tanzania in the analysis of forced sex due to the questions on forced sex being asked of a non-representative sample in that country (for details see online supplemental appendix p 7).
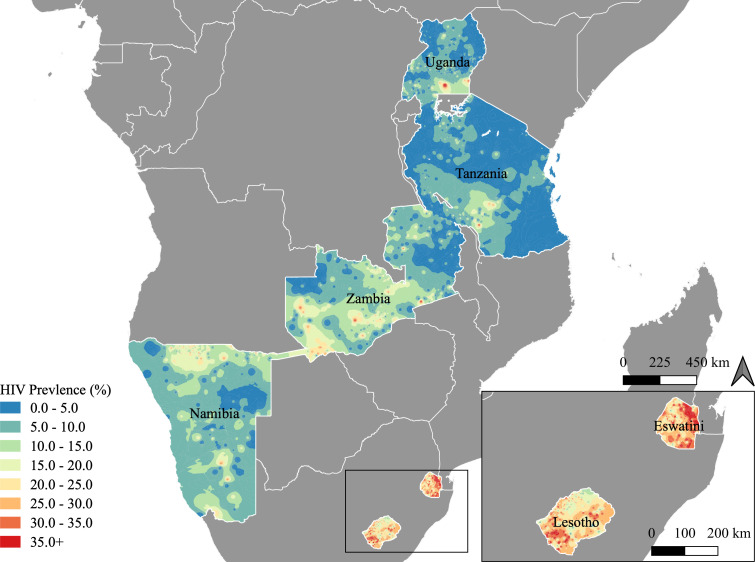
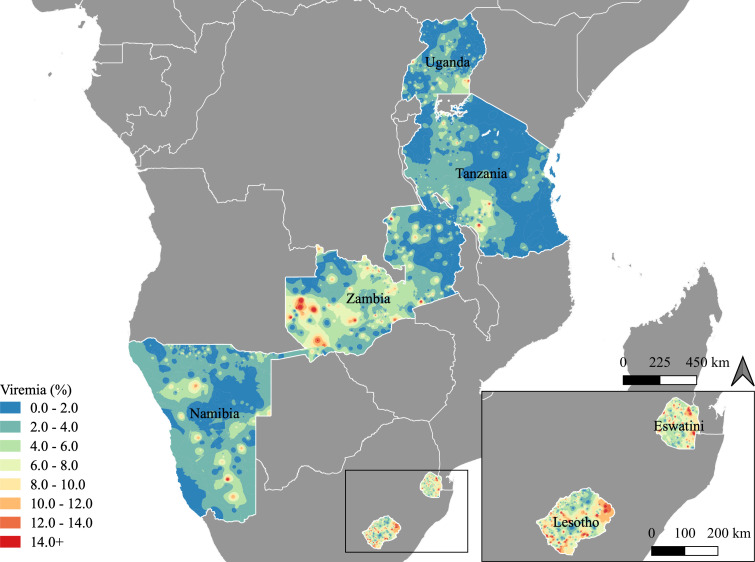
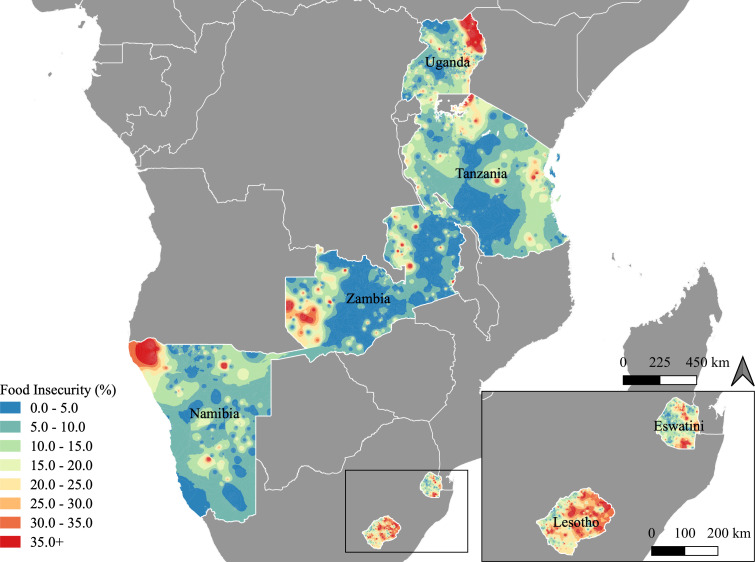
We generated maps of the prevalence of HIV infection, viraemia and any food insecurity with SAGA in QGIS V.3.4. We used georeferenced weighted averages at the EA level, with all cases linked to the centroid of the EA, and kernel density smoothing and interpolation over 200 adult participants for each smoothing circle.
Results
We enrolled 54 033 households, with 112 955 adults aged 15–59 years with HIV test results and data on food insecurity. The majority of heads of households were men, although more women were heads of households in Lesotho (50.9%, n=3621/7502), Eswatini (54.7%, n=2549/4652) and Namibia (51.2%, n=4041/8002, table 1). Most participants were rural (63.5%, n=73 501/54 033), with the highest rural proportions in Uganda and Eswatini, and the lowest in Namibia. The largest age group was 15–24 years old, comprising 40.2% (n=42 112/112 995) of the weighted population. The proportion of participants who had a secondary or greater education was highest in Eswatini (70.6%, n=6477/9553) and Namibia (70.0%, n=9979/16 267), and lowest in Tanzania (25.6%, n=6490/28 340). Less than half of participants (45.8%, 47 357/112 995) had been formally employed in the past 12 months. HIV prevalence was highest in women in Eswatini (34.2%, n=1913/5525, figure 1), and lowest in men in Tanzania (3.5%, n=521/12 297). More HIV-positive men (47.5%, n=1727/4473) than women (37.9%, n=2963/9736) had unsuppressed viral load, which was highest in men in Tanzania (58.7%, n=301/521), and community viraemia was highest in Lesotho, although highly heterogeneous across countries (figure 2).
Table 1.
Characteristics of participating households and adults aged 15–59 years, by country
| Characteristic household level | Eswatini N=4652 % (n) |
Lesotho N=7052 % (n) |
Tanzania N=13 328 % (n) |
Uganda N=11 717 % (n) |
Namibia N=8002 % (n) |
Zambia N=9282 % (n) |
Total N=54 033 % (n) |
| Households reporting any food insecurity | 31.3 (1531) | 31.1 (2273) | 21.4 (2818) | 27.8 (3599) | 22.9 (2015) | 17.8 (1628) | 23.5 (13 864) |
| Median youth dependency ratio (IQR)* | 40 (0–55) | 33 (0–50) | 50 (33–64) | 50 (33–67) | 33 (0–50) | 100 (40–200) | 100 (50–150) |
| Female head of household | 54.7 (2549) | 50.9 (3621) | 26.8 (3417) | 31.0 (3714) | 51.2 (4041) | 23.7 (2196) | 29.2 (19 530) |
| Receipt of economic support† | |||||||
| None | 63.9 (2904) | 79.7 (5560) | 94.2 (12 521) | 93.7 (10 961) | 71.7 (5404) | 96.1 (8923) | 93.1 (46 273) |
| Economic only | 19.1 (914) | 13.6 (981) | 5.2 (736) | 5.0 (593) | 19.7 (1842) | 3.0 (271) | 5.5 (6729) |
| Food support | 17.0 (834) | 6.7 (511) | 0.6 (71) | 1.2 (163) | 8.6 (756) | 0.9 (88) | 1.3 (2423) |
| Individual level | N=9553 % (n) | N=11 655 % (n) | N=28 340 % (n) | N=28 030 % (n) | N=16 267 % (n) | N=19 110 % (n) | N=112 955 % (n) |
| Geography, % (n) | |||||||
| Urban | 28.0 (2131) | 48.8 (5208) | 37.5 (9348) | 28.8 (7663) | 58.4 (6765) | 45.7 (8339) | 36.5 (39 454) |
| Rural | 72.0 (7422) | 51.2 (6447) | 62.5 (18 992) | 71.2 (20 367) | 41.6 (9502) | 54.3 (10 771) | 63.5 (73 501) |
| Sex, % (n) | |||||||
| Women | 54.4 (5525) | 49.7 (6870) | 50.8 (16 043) | 52.5 (16 094) | 51.5 (9220) | 51.1 (10 981) | 51.4 (64 726) |
| Men | 45.6 (4028) | 50.3 (4785) | 49.2 (12 297) | 47.5 (11 945) | 48.5 (7047) | 48.9 (8129) | 48.6 (48 229) |
| Median age (IQR) | 28 (21–38) | 30 (22–40) | 28 (20–39) | 27 (20–37) | 29 (21–40) | 27 (20–38) | 28 (20–38) |
| Age group (years) | |||||||
| 15–24 | 37.2 (3599) | 34.1 (4037) | 38.5 (10 359) | 43.3 (11,241) | 35.2 (5557) | 41.1 (7319) | 40.2 (42 112) |
| 25–34 | 29.0 (2600) | 29.8 (3223) | 27.3 (7704) | 26.9 (7613) | 28.6 (4302) | 27.3 (5130) | 27.3 (30 572) |
| 35–44 | 18.7 (1698) | 19.0 (2148) | 18.8 (5603) | 16.4 (4879) | 19.4 (3310) | 18.1 (3736) | 18.0 (21 374) |
| 45–59 | 15.1 (1656) | 17.1 (2247) | 15.4 (4674) | 13.4 (4297) | 16.8 (3098) | 13.5 (2925) | 14.5 (18 897) |
| No food in house in past 4 weeks | |||||||
| Never | 66.4 (6089) | 69.0 (7820) | 79.3 (22 479) | 72.1 (19 441) | 75.6 (11 788) | 83.1 (15 896) | 77.1 (83 513) |
| Rarely (1–2x) | 18.6 (1900) | 13.1 (1569) | 11.3 (3299) | 15.8 (4767) | 11.1 (1944) | 10.2 (1954) | 12.7 (15 433) |
| Sometimes (3–10x) | 12.3 (1280) | 13.4 (1678) | 7.2 (2010) | 10.7 (3433) | 10.9 (2104) | 5.8 (1089) | 8.4 (11 594) |
| Often (>10x) | 2.8 (284) | 4.5 (588) | 2.2 (552) | 1.4 (389) | 2.4 (431) | 0.9 (171) | 1.8 (2415) |
| Educational level | |||||||
| None | 3.5 (372) | 5.0 (572) | 12.4 (4135) | 7.1 (2451) | 6.7 (1490) | 5.0 (961) | 9.3 (9981) |
| Primary | 25.9 (2722) | 39.7 (4912) | 62.0 (17 703) | 55.6 (15 882) | 23.3 (4757) | 41.9 (8322) | 55.5 (54 298) |
| Secondary or greater | 70.6 (6447) | 55.3 (6164) | 25.6 (6490) | 37.3 (9538) | 70.0 (9979) | 53.1 (9814) | 35.2 (48 432) |
| Marital status | |||||||
| Never married | 55.3 (5178) | 38.6 (4267) | 32.1 (7914) | 33.1 (8263) | 60.4 (9228) | 37.2 (6355) | 34.2 (41 205) |
| Married | 36.8 (3519) | 48.1 (5624) | 57.0 (17 086) | 53.6 (15 790) | 32.1 (5583) | 53.6 (10 648) | 54.5 (58 250) |
| Separated/Divorced/Widowed | 7.9 (800) | 13.3 (1743) | 10.9 (3285) | 13.3 (3910) | 7.5 (1310) | 9.3 (1965) | 11.4 (13 013) |
| Employed in past 12 months | 43.3 (3853) | 39.2 (4099) | 44.7 (12 155) | 53.2 (14 346) | 45.9 (6756) | 33.8 (6148) | 45.8 (47 357) |
| Recent migrant‡ | 10.9 (947) | 6.3 (675) | 14.6 (4005) | 24.5 (6556) | 29.2 (4383) | 14.3 (2683) | 17.9 (19 249) |
| HIV-positive | |||||||
| Women | 34.2 (1913) | 30.3 (2161) | 6.5 (1187) | 7.7 (1163) | 15.6 (1623) | 14.6 (1689) | 9.0 (9736) |
| Men | 20.5 (875) | 20.9 (1032) | 3.5 (521) | 4.7 (545) | 9.2 (722) | 9.3 (778) | 5.3 (4473) |
| Viral load >1000 copies/mL§ | |||||||
| Women | 24.6 (461) | 29.5 (617) | 42.5 (513) | 37.7 (432) | 18.5 (313) | 39.8 (627) | 37.9 (2963) |
| Men | 33.8 (274) | 36.4 (364) | 58.7 (301) | 46.1 (247) | 31.1 (220) | 42.5 (321) | 47.5 (1727) |
Some totals maybe ≥100% due to rounding. Data are survey weighted using Taylor series weights for estimates of variance.
*Dependency ratio was calculated as the number of rostered usual residents aged 0–14 years/(rostered 15 and older)×100.
†Measured over the past 3 months.
‡Migrant defined as being away from home for at least 1 month in the past 12 months, except for Namibia, where it was during the past 3 years.
§Among HIV-positive.
Figure 1.
Weighted map of HIV Prevalence in adults aged 15-59. Maps were generated with SAGA in QGIS V.3.4. We used georeferenced weighted averages at the enumeration area (EA) level, with all cases linked to the centroid of the EA, and kernel density smoothing and interpolation over 200 adult participants for each smoothing circle.
Figure 2.
Weighted map of community HIV viraemia. (A) Maps were generated with SAGA in QGIS V.3.4. We used georeferenced weighted averages at the enumeration area (EA) level, with all cases linked to the centroid of the EA, and kernel density smoothing and interpolation over 200 adult participants for each smoothing circle. Community HIV viraemia (%) was defined as a viral load >1000 copies/mL, in the total sampled population regardless of HIV serostatus.
Correlates of severe food insecurity
Across all countries, 23.5% (n=13 864/54 033) of households reported having experienced any lack of food in the past 4 weeks, with 10.2% (n=14 009/112 955) of participants reporting severe food insecurity. All countries had regions with high burdens of food insecurity, but the distribution was highly heterogeneous, with frequency of any food insecurity ranging from 0% to 80% of an EA’s population (figure 3). The highest prevalence of severe food insecurity was seen in Lesotho (17.9%, 2266/11 655, table 2). Adjusted results from the multivariable analysis were similar to univariable results: male-headed households were less likely to suffer from severe food insecurity (adjusted OR (aOR) 0.71, 95% CI 0.63 to 0.80), as were wealthier households (aOR 0.68, 95% CI 0.64 to 0.71 for each quintile increase in wealth). At the individual level, secondary or greater education (aOR 0.75, 95% CI 0.68 to 0.82), formal employment in the past year (aOR 0.90, 95% CI 0.84 to 0.97) and being married (aOR 0.81, 95% CI 0.71 to 0.91 compared with never married) were all protective against severe food insecurity. Living in a household with many young dependents (aOR 1.12, 95% CI 1.08 to 1.17 per quartile increase), being aged 35–44 or 45–59 years compared with 15–24 years, being separated/divorced or widowed (aOR 1.17, 95% CI 1.02 to 1.33), having recently migrated (aOR 1.14, 95% CI 1.05 to 1.24) and being HIV-positive were all associated with severe food insecurity (aOR 1.23, 95% CI 1.10 to 1.38). Excluding those who were recently HIV-infected did not change the association between HIV infection and severe food insecurity. After adjustment, sex, receipt of social support and HIV status of the head of household were no longer significant, and rural residence became protective.
Figure 3.
Weighted map of any food insecurity in adults aged 15–59 years. Maps were generated with SAGA in QGIS V.3.4. We used georeferenced weighted averages at the enumeration area (EA) level, with all cases linked to the centroid of the EA, and kernel density smoothing and interpolation over 200 adult participants for each smoothing circle;. Any food insecurity was defined as no food in the house at least once in the past 4 weeks.
Table 2.
Analysis of factors associated with increased odds of severe food insecurity among adults aged 15–59 years
| Characteristic (n=112 955) | Proportion of participants with severe food insecurity % (n/N) | OR 95% CI | Adjusted OR (aOR) 95% CI |
P value |
| Country | ||||
| Zambia | 6.7% (1260/19 110) | 1.0 | 1.0 | |
| Tanzania | 9.5% (2562/28 340) | 1.45 (1.23 to 1.72) | 1.34 (1.12 to 1.61) | 0.001 |
| Uganda | 12.1% (3822/28 030) | 1.91 (1.65 to 2.22) | 1.72 (1.47 to 2.00) | <0.001 |
| Namibia | 13.3% (2535/16 267) | 2.13 (1.82 to 2.50) | 1.84 (1.53 to 2.20) | <0.001 |
| Eswatini | 15.0% (1564/9553) | 2.46 (2.05 to 2.94) | 2.19 (1.81 to 2.65) | <0.001 |
| Lesotho | 17.9% (2266/11 655) | 3.03 (2.61 to 3.51) | 2.88 (2.47 to 3.36) | <0.001 |
| Location of residence | ||||
| Urban | 7.8% (10 228/73 501) | 1.0 | 1.0 | <0.001 |
| Rural | 11.7% (3781/39 454) | 1.58 (1.39 to 1.78) | 0.72 (0.61 to 0.84) | |
| Sex of head of household | ||||
| Female | 14.1% (5993/36 264) | 1.0 | 1.0 | <0.001 |
| Male | 9.0% (7684/73 575) | 0.60 (0.54 to 0.67) | 0.71 (0.63 to 0.80) | |
| HIV-positive head of household | NS | |||
| No | 10.2% (8833/75 463) | 1.0 | ||
| Yes | 12.2% (2447/14 589) | 1.23 (1.08 to 1.40) | ||
| Not tested | 9.6% (2397/19 786) | 0.94 (0.83 to 1.06) | ||
| Household wealth quintile | ||||
| Per quintile increase | - | 0.70 (0.67 to 0.72) | 0.68 (0.64 to 0.71) | <0.001 |
| Dependent ratio quartile | ||||
| Per quartile increase | - | 1.22 (1.17 to 1.27) | 1.12 (1.08 to 1.17) | <0.001 |
| Receipt of economic support | NS | |||
| None | 9.9% (10 586/93 311) | 1.0 | ||
| Economic only | 12.6% (2414/14 513) | 1.31 (1.12 to 1.53) | ||
| Food support | 16.3% (1009/5131) | 1.76 (1.37 to 2.26) | ||
| Sex of participant | 0.523 | |||
| Women | 10.7% (8330/64 726) | 1.0 | 1.0 | |
| Men | 9.8% (5679/48 229) | 0.90 (0.85 to 0.95) | 1.02 (0.96 to 1.08) | |
| Age group (years) | ||||
| 15–24 | 10.1% (5132/42 112) | 1.0 | 1.0 | |
| 25–34 | 9.2% (3460/30 572) | 0.90 (0.84 to 0.98) | 1.02 (0.92 to 1.13) | 0.746 |
| 35–44 | 11.1% (2721/21 374) | 1.11 (1.02 to 1.20) | 1.13 (1.00 to 1.27) | 0.042 |
| 45–59 | 11.5% (2696/18 897) | 1.16 (1.07 to 1.26) | 1.12 (0.99 to 1.26) | 0.061 |
| Educational attainment | <0.001 | |||
| None/Primary | 12.0% (9539/64 235) | 1.0 | 1.0 | |
| Secondary and above | 7.0% (4446/48 476) | 0.55 (0.51 to 0.60) | 0.75 (0.68 to 0.82) | |
| Marital status | ||||
| Never married | 10.1% (5115/41 205) | 1.0 | 1.0 | |
| Married | 9.4% (6544/58 250) | 0.92 (0.85 to 1.00) | 0.81 (0.71 to 0.91) | 0.001 |
| Separated/Divorced/Widowed | 15.0% (2295/13 013) | 1.58 (1.45 to 1.71) | 1.17 (1.02 to 1.33) | 0.023 |
| Employed in past 12 months | 0.004 | |||
| No | 10.9% (9014/65 511) | 1.0 | 1.0 | |
| Yes | 9.4% (4982/47 357) | 0.84 (0.79 to 0.89) | 0.90 (0.84 to 0.97) | |
| Recent migrant* | 0.001 | |||
| No | 10.1% (11321/91851) | 1.0 | 1.0 | |
| Yes | 10.9% (2421/19 249) | 1.09 (1.01 to 1.17) | 1.14 (1.05 to 1.24) | |
| HIV infection† | 0.001 | |||
| Negative | 10.0% (11 516/98 250) | 1.0 | 1.0 | |
| Positive | 12.8% (2201/13 256) | 1.32 (1.19 to 1.46) | 1.23 (1.10 to 1.38) |
All proportions are weighted and numerator and denominators are crude values. ORs calculated using logistic regression of weighted values and Taylor estimates of variance. P values determined by Wald test. All variables p<0.20 in univariable analysis were tested in the final model, with those with a p value<0.10 retained. Age, country, urbanicity, sex and wealth quintile were included a priori.
*Migrant defined as away from home for >1 month in the past 12 months, except for Namibia, where it was the past 3 years.
†The model was also run restricting HIV infection to those diagnosed >1 year prior to survey, which did not change the results.
NS, not significant.
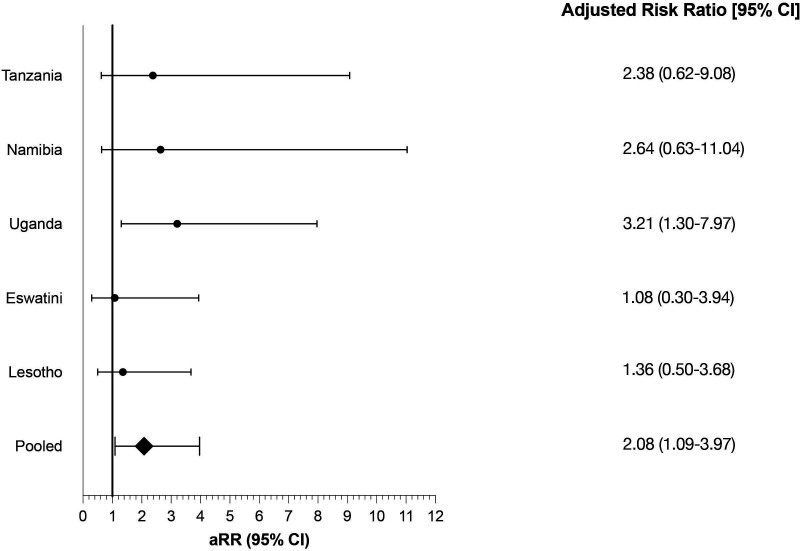
Association between severe food insecurity, food and economic support and recent HIV infection
Of the 14 208 HIV-positive participants, 1.9% (n=200) were classified as having recent HIV infection, of which 140 were women and 60 were men. Incidence was highest in women aged 15–49 years in Eswatini (1.73%, 95% CI 0.96 to 2.50, online supplemental figure 6), and lowest in men aged 15–24 years in Tanzania (0%, 95% CI 0 to 0.23). Among those without chronic HIV infection, there were 27 recent cases in 6699 women with severe food insecurity, and 113 cases in the other 48 431 women; there were 13 recent cases in 4974 men with severe food insecurity, and 47 in the other 38 842 men. In univariable analysis of predictors of recent HIV infection, the relative risk of new infection was highest in women aged 25–34 years and in men aged 35–44 and 45–59 years, compared with participants aged 15–24 years (table 3). Results from our multivariable model demonstrated that severe food insecurity was associated with a twofold increase in risk of recent infection in women (adjusted relative risk (aRR) 2.08, 95% CI 1.09 to 3.97), with the effect relatively homogeneous across countries, although a lower risk was seen in Lesotho and Eswatini (figure 4). There was no significant risk noted in men. Both sexes were at higher risk of HIV acquisition if previously married, compared with never married, but currently married men were also at significantly higher risk of recent HIV infection (aRR 8.96, 95% CI 1.77 to 45.35). Receipt of food support was associated with a pronounced lower risk of recent HIV in women (aRR 0.36, 95% CI 0.14 to 0.88), whereas receipt of other types of support was not, and neither were protective in men. The use of a scale measure of food insecurity incorporating the three questions on food availability and access did not produce substantively different results than our measure (online supplemental table 1), although fewer people were classified as severely food insufficient. This is further discussed in the online supplemental appendix (p 9).
Table 3.
Analysis of factors associated with the relative risk of recent HIV infection among adults aged 15–59 years, by sex
| Characteristic | Women (n=54 834) | Men (n=43 827) | ||||||
| RR (95% CI) | P value | aRR (95% CI) | P value | RR (95% CI) | P Value | aRR (95% CI) | P value | |
| Severe food insecurity | 2.11 (1.11 to 4.03) | 0.023 | 2.08 (1.09 to 3.97) | 0.026 | 1.85 (0.82 to 4.20) | 0.140 | 1.77 (0.84 to 3.74) | 0.134 |
| Age group (years) | ||||||||
| 15–24 | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| 25–34 | 1.72 (0.97 to 3.05) | 0.064 | 1.20 (0.61 to 2.35) | 0.594 | 2.62 (0.93 to 7.36) | 0.067 | 0.81 (0.22 to 3.05) | 0.760 |
| 35–44 | 1.14 (0.59 to 2.21) | 0.698 | 0.77 (0.35 to 1.67) | 0.500 | 5.40 (1.92 to 15.21) | 0.001 | 1.45 (0.35 to 5.99) | 0.605 |
| 45–59 | 0.61 (0.21 to 1.76) | 0.355 | 0.34 (0.11 to 1.12) | 0.077 | 4.75 (1.49 to 15.13) | 0.009 | 1.27 (0.30 to 5.54) | 0.747 |
| Country | ||||||||
| Zambia | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Tanzania | 0.38 (0.22 to 0.66) | 0.001 | 0.46 (0.26 to 0.82) | 0.009 | 0.60 (0.24 to 1.50) | 0.272 | 0.58 (0.22 to 1.52) | 0.263 |
| Uganda | 0.59 (0.36 to 0.97) | 0.036 | 0.68 (0.41 to 1.14) | 0.140 | 1.45 (0.58 to 3.61) | 0.421 | 1.31 (0.50 to 3.42) | 0.583 |
| Namibia | 0.67 (0.34 to 1.30) | 0.233 | 0.89 (0.43 to 1.83) | 0.749 | 0.47 (0.13 to 1.67) | 0.243 | 0.72 (0.19 to 2.73) | 0.631 |
| Eswatini | 1.60 (0.91 to 2.81) | 0.102 | 1.64 (0.89 to 3.02) | 0.115 | 3.07 (1.18 to 8.00) | 0.022 | 2.84 (1.04 to 7.79) | 0.042 |
| Lesotho | 1.32 (0.75 to 2.30) | 0.331 | 0.86 (0.47 to 1.56) | 0.614 | 3.46 (1.42 to 8.47) | 0.007 | 2.60 (0.99 to 6.85) | 0.053 |
| Location of residence | ||||||||
| Urban | 1.0 | 1.0 | 1.0 | |||||
| Rural | 0.72 (0.46 to 1.13) | 0.154 | 2.44 (1.14 to 5.25) | 0.022 | 2.47 (1.14 to 5.35) | 0.022 | ||
| Wealth quintile | ||||||||
| (per quintile increase) | 0.99 (0.84 to 1.16) | 0.886 | 0.81 (0.66 to 0.98) | 0.033 | ||||
| Community viraemia | ||||||||
| (per 1% increase) | 1.12 (1.09 to 1.16) | <0.001 | 1.10 (1.05 to 1.15) | <0.001 | 1.10 (1.05 to 1.16) | <0.001 | 1.10 (1.02 to 1.18) | 0.015 |
| Receipt of economic support | ||||||||
| None | 1.0 | 1.0 | 1.0 | |||||
| Economic only | 1.14 (0.58 to 2.21) | 0.709 | 1.06 (0.54 to 2.07) | 0.864 | 1.48 (0.55 to 3.99) | 0.436 | ||
| Food support | 0.51 (0.20 to 1.32) | 0.162 | 0.36 (0.14 to 0.88) | 0.025 | 4.10 (0.74 to 22.76) | 0.106 | ||
| Migration | ||||||||
| None | 1.0 | 1.0 | ||||||
| Away for >1 month | 1.11 (0.57 to 2.17) | 0.751 | 0.79 (0.32 to 1.92) | 0.597 | ||||
| Employment status | ||||||||
| No formal employment | 1.0 | 1.0 | 1.0 | |||||
| Worked in past year | 1.48 (0.93 to 2.36) | 0.097 | 2.33 (1.11 to 4.91) | 0.026 | 1.95 (0.95 to 4.02) | 0.070 | ||
| Marital status | ||||||||
| Never married | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Married | 1.51 (0.86 to 2.65) | 0.148 | 1.86 (0.94 to 3.68) | 0.074 | 10.83 (3.86 to 30.38) | <0.001 | 8.96 (1.77 to 45.35) | 0.008 |
| Separated/Divorced/ Widowed | 3.10 (1.69 to 5.71) | <0.001 | 4.25 (1.89 to 9.57) | 0.001 | 11.19 (2.21 to 56.73) | 0.004 | 8.23 (1.15 to 59.02) | 0.036 |
| Male circumcised | 0.60 (0.30 to 1.19) | 0.144 | NS | NS | ||||
RR determined by Poisson regression using weighted values and Taylor estimates of variance. All variables p<0.20 in univariable analysis were tested in the final model, with those with a p value<0.10 retained. Age group and country were included a priori. Results indicated in bold are significant at p<0.05.
aRR, adjusted relative risk; RR, relative risk.
Figure 4.
Country-specific adjusted relative risk (aRR) of HIV acquisition by severe food insecurity in women aged 15–59 years. Zambia results are not included as the model did not converge.
The frequency of different potential mediating behaviours is described in online supplemental table 2. Women in Uganda reported the highest frequency of transactional sex (19.5%, n=2353/11 824), early sexual debut (12.1%, n=2009/15 813) and forced sex (16.2%, n=384/2898), whereas women in Tanzania reported more high-risk sex (45.8%, n=5038/11 246) and intergenerational sex in young women (18.2%, n=616/3556). There was a statistically significant association between severe food insecurity and transactional sex (aRR 1.28, 95% CI 1.17 to 1.41, table 4). Women with severe food insecurity also reported more frequent early sexual debut (aRR 1.18, 95% CI 1.06 to 1.31), more forced sex (aRR 1.36, 95% CI 1.11 to 1.66) and more high-risk sex (aRR 1.08, 95% CI 1.02 to 1.14). Economic (aRR 0.89, 95% CI 0.84 to 0.95) and food support (aRR 0.81, 95% CI 0.69 to 0.97) were both associated with significantly lower risks of high-risk sex. Severe food insecurity was also associated with an elevated risk (aRR 1.23, 95% 1.03 to 1.46) of intergenerational sex, reported by 16.5% of young women. None of the behaviours were associated with urbanicity after adjusting for other demographic factors. There was heterogeneity between countries for the increased risk of forced and intergenerational sex in women with food insecurity (online supplemental figure 7).
Table 4.
Multivariable analysis of the relative risk of several high-risk sexual behaviours among women aged 15–59 years
| Characteristic | Behavioural outcome | ||||
| Transactional sex | Early sexual debut | History of forced sex† | High-risk sex‡ | Intergenerational sex in AGYW§ | |
| aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | |
| Severe food insecurity | 1.28 (1.17 to 1.41)*** | 1.18 (1.06 to 1.31)** | 1.36 (1.11 to 1.66)** | 1.08 (1.02 to 1.14)** | 1.23 (1.03 to 1.46)** |
| Country | |||||
| Zambia | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Tanzania | 0.71 (0.64 to 0.80)*** | 0.73 (0.67 to 0.81)*** | - | 1.39 (1.31 to 1.46)*** | 1.37 (1.17 to 1.60)*** |
| Uganda | 1.11 (1.00 to 1.22)* | 1.08 (0.99 to 1.18) | 1.59 (1.30 to 1.95)*** | 1.19 (1.13 to 1.26)*** | 1.18 (1.02 to 1.37)* |
| Namibia | 0.44 (0.38 to 0.50)*** | 0.87 (0.77 to 0.99)* | 0.59 (0.48 to 0.72)*** | 0.71 (0.66 to 0.78)*** | 1.43 (1.14 to 1.80)** |
| Eswatini | 0.24 (0.19 to 0.30)*** | 0.62 (0.53 to 0.72)*** | 0.52 (0.40 to 0.67)*** | 0.70 (0.64 to 0.76)*** | 2.06 (1.67 to 2.55)*** |
| Lesotho | 0.34 (0.29 to 0.39)*** | 0.56 (0.49 to 0.64)*** | 1.46 (1.27 to 1.68)*** | 0.88 (0.82 to 0.94)*** | 1.02 (0.84 to 1.23) |
| Location of residence | |||||
| Urban | NS | NS | 1.0 | NS | 1.0 |
| Rural | 0.93 (0.75 to 1.17) | 1.14 (0.98 to 1.32) | |||
| Age group (years)¶ | |||||
| 15–24 | 1.0 | 1.0 | 1.0 | 1.0 | Per year increase |
| 25–34 | 0.85 (0.79 to 0.91)*** | 0.78 (0.71 to 0.85)*** | 0.87 (0.73 to 1.03) | 1.01 (0.97 to 1.06) | 1.04 (1.02 to 1.07)*** |
| 35–44 | 0.89 (0.83 to 0.97)** | 0.77 (0.70 to 0.86)*** | 0.82 (0.66 to 1.02)** | 1.21 (1.15 to 1.28)*** | -- |
| 45–59 | 0.70 (0.61 to 0.80)*** | 0.68 (0.60 to 0.76)*** | 0.57 (0.44 to 0.75)*** | 1.44 (1.38 to 1.51)*** | -- |
| Wealth quintile | |||||
| Per quintile increase | 0.92 (0.89 to 0.94)*** | 0.91 (0.88 to 0.93)*** | 1.09 (1.01 to 1.18) | 0.93 (0.92 to 0.95)*** | 1.09 (1.04 to 1.14)*** |
| Education | |||||
| None/Primary | 1.0 | 1.0 | |||
| Secondary or more education | 0.81 (0.74 to 0.88)*** | 0.39 (0.35 to 0.43)*** | NS | NS | 0.71 (0.62 to 0.82)*** |
| Marital status | |||||
| Single | 1.0 | 1.0 | 1.0 | 1.0 | |
| Married | 0.34 (0.31 to 0.37)*** | 1.51 (1.36 to 1.68)*** | 0.92 (0.87 to 0.98)** | 2.75 (2.27 to 3.34)*** | |
| Separated/Divorced/ Widowed | 1.19 (1.08 to 1.31)*** | 1.71 (1.51 to 1.93)*** | NS | 1.12 (1.04 to 1.20)*** | 2.63 (2.09 to 3.31)*** |
| Receipt of economic support†† | |||||
| None | 1.0 | ||||
| Economic only | NS | NS | NS | 0.89 (0.84 to 0.95)*** | NS |
| Food support | 0.81 (0.69 to 0.97)* | ||||
RR determined by Poisson regression using weighted values and Taylor estimates of variance. All variables p<0.20 in univariable analysis were tested in the final model, with those with a p value<0.10 retained. Age group and country were included a priori.
*P≤0.05; **p≤0.01; ***p≤0.001.
†Violence questions were asked to a subset of participants in each household. The results exclude Tanzania due to a non-representative sample. In Uganda, sexual violence questions were only asked to those aged 15–24 years.
‡Defined as having sex without a condom with someone of unknown or positive HIV status in the past 12 months.
§Defined as having a sexual partner at least 10 years older in the past 12 months.
¶Age included as a continuous variable in the analysis restricted to the 15–24 year age band.
††Measured over the past 3 months.
AGYW aged 15–24 years. Analysis restricted to those who report a history of sexual activity aside from sexual debut.
AGYW, adolescent girls and young women; NS, not significant.
Discussion
To our knowledge, this is the first study to directly link acute food insecurity with HIV incidence in women in SSA, supporting prior studies which have shown associations between hunger, sexual risk-taking and prevalent HIV infection.15 16 39 The robustness and representativeness of the PHIA data, spanning multiple countries and contexts with highly variable community HIV burden, is particularly valuable for substantiating the likely pathways for this association.16 43 Our data also suggest that some of the communities with the highest levels of any food insecurity, such as areas in Lesotho, tend to have the highest HIV prevalence. Given the likelihood of future periods of drought, and related food insecurity, these findings have serious implications for efforts to achieve or maintain epidemic control.
There was substantial variation in the spatial distribution of households reporting any food insecurity, both across countries and subnationally. Across all contexts, poorer households headed by women or those with many children consistently had much higher odds of severe food shortages. These findings have been shown in multiple other studies, attributed to the fact that women often have little control over resources such as land and employment, leading to a disproportionate susceptibility to poverty and income shocks.44 Being female in itself is not a predictor of severe food insecurity, as marriage is protective, suggesting that women in male-headed households are protected by their husband’s income-earning potential. The bidirectionality of the relationship between food insecurity and HIV infection is also seen here, where infection was strongly associated with severe food insecurity even when we restricted our analysis to those infected for >1 year.25
The twofold increase in risk of recent HIV infection seen in women who reported severe food insecurity reinforces other studies showing increases in risk behaviour and higher HIV prevalence in women with food insecurity,20 45 46 but the detailed analyses of sexual risk behaviours among women experiencing severe food insecurity allows us to better understand the direction of the association. The increased risk of HIV acquisition may be attributed to the constellation of risk factors impacting these women, including a 28% increase in risk of engaging in transactional sex. This behaviour declined with age, wealth and education. These findings build on previous studies which found that food insecurity and poverty is commonly associated with sex in exchange for goods.16 39 43 44 Young food-insecure women were also more likely to report significantly older partners, possibly because they confer some financial benefit. These older partners are often more infectious than same-aged partners as a result of higher rates of viraemia due to having recently acquired HIV, being undiagnosed or not taking ART.41 42 47 It is also noteworthy that women of all ages compounded their risk by not using condoms with men who might be HIV positive, a risk factor implicated as a key driver of HIV acquisition.48 Finally, the fact that food-insecure women reported both more forced sex over their lifetimes, as well as more frequent early sexual debut suggests that some of the risk behaviours are a result of compounded vulnerabilities, and that exposure to multiple adverse events might precede or predispose women to food insecurity. These findings also support that food security has a significant gender dimension, where women are both more at risk of severe hunger, and suffer more consequences due to limited coping strategies, which include different forms of sexual activity in exchange for material support.20 The intercountry heterogeneity of the association between severe food insecurity and certain risk behaviours suggests that there might be multiple different pathways between food insecurity and HIV acquisition, and these are likely to be highly contextual.
Another key finding is that, while most forms of social support were not associated with a protective effect, receipt of food support was associated with a 64% lower risk of recent HIV infection in women. This suggests that hunger alleviation interrupts the cycle of vulnerability, possibly because food support generally goes directly to women who are responsible for intrahousehold consumption needs, and is unlikely to be used by men for other purchases.49 Our results suggest that food support addresses women’s immediate food shortage, alleviating the pressure to engage in forms of high-risk behaviours to obtain food. Further analysis of our data, disaggregated by sex, age and risk group, and epidemiological context, is currently being conducted to understand how different forms of social support impact behaviours and HIV risk; this should enable the comparison of our data with other studies which have shown benefits of social or financial support, both in terms of short-term assistance and long-term coping strategies.50 51 This research supports the need to address structural constraints underlying poverty, as well as behavioural change and gender equity, and underscores the importance of including women as active agents who can assist in understanding how best to use social assistance.
Study limitations
Limitations of this study include the single-point estimate of HIV infection and associated behaviours, where the cross-sectional nature of the data means that the direction of effect is difficult to determine with certainty. The LAg avidity assay has limitations in estimation of HIV incidence and the algorithm excludes anyone who might have started ARV drugs within the first 6 months of infection.37 We also had relatively small numbers of people classified as recently infected across the surveys, particularly men, which prohibited an in-depth analysis of factors driving HIV infection in this group. However, in women, our findings are supported by our theoretical framework, suggesting that the findings are robust. The attenuation of any effect seen in the multivariable model of recent HIV infection in men also suggests that the patterns of risk for this sex are more context dependent, and therefore a pooled analysis across several different countries is less appropriate. Furthermore, as hazardous drinking data were not collected in all PHIA countries, it prohibited its inclusion in our models, which might have obscured its importance as a driver of both food shortages as well as HIV acquisition.52 Further research incorporating more community-level variables, as well as other factors which might be more predictive of infection in males, are critical to the identification of high-risk men.
Conclusions
In this time of global economic disruption and stark increases in food insecurity,9 53 it is critical to track the emergence of food shortages in communities that are most vulnerable to the devastating effects of climate change. Our study suggests that in addition to population-level emergency food assistance, women, particularly those heading their own households, need to be specifically targeted with food assistance. At the same time, these women can be linked to support services that will help them reduce their risk of HIV infection. Beyond these acute responses, programmes need to follow-up with support for economic empowerment of unmarried women, so that they can support themselves and their children without relying on high-risk sexual activity in their times of greatest need. Investments in community resilience need to ensure that these women are fully integrated into the programmes, whether in the agricultural sector or in the market or service economy.
Future research should further evaluate how current biomedical prevention modalities such as pre-exposure prophylaxis, and structural interventions such as educational support targeted towards young women, might disrupt this pathway. In light of evidence suggesting that the age at acquisition is shifting upwards,54 re-evaluation of prevention programmatic age targets is recommended in order to support women throughout their life span. Understanding that food insecurity has both short-term and long-term consequences, including HIV transmission, should spur further investments in preparedness, including in crop resilience, and environmental justice. Addressing the root causes of climate change by encouraging the use of renewable energy resources in SSA could also offset the impacts of worsening emissions and environmental degradation.10
Supplementary Material
Acknowledgments
The authors would also like to acknowledge all PHIA participants and survey staff, and the Ministries of Health of Zambia, Lesotho, Eswatini, Namibia, Tanzania and Uganda, and colleagues from the PHIA research group for their contributions to this study.
Footnotes
Contributors: AL, EG, AS, NM, JJ, CG, HP, AJH, WK, KJ, SF and JW designed the study. AL, EG, AS, NM, JJ, CG, SB, KS, AJH, DB, JM, WK, NP, LM, JW and SF designed the data collection tools. AL and EG did the statistical analysis. AL took primary responsibility for writing the manuscript, and is responsible for the overall content as the guarantor. All coauthors contributed to data analysis and interpretation, and to the writing and review of the manuscript.
Funding: This project has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) under the terms of cooperative agreement #U2GGH001226. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the funding agencies. Coauthors from the CDC participated in study design, data collection, analysis, and interpretation, and in the writing of the report. The corresponding author had final responsibility for the decision to submit for publication.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All data are publicly available for download from the PHIA website.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The PHIA protocol and data collection tools were approved by national ethics committees for each country, and the institutional review boards at Columbia University Irving Medical Center, the US Centers for Disease Control and Prevention (CDC) and the University of California, San Francisco in the case of Namibia. Due to the inclusion of six countries and the multiple ethical boards involved, we are only providing the protocol numbers for Columbia University IRB (AAAQ0753, AAAQ7860, AAAQ8408, AAAQ8537, AAAR2051, AAAQ889). A guardian or parent provided permission for adolescent minors who were then asked for assent for all procedures. Written or verbal (Tanzania and Uganda) informed consent/assent was documented via electronic signature, with witnesses verifying consent for illiterate individuals.
References
- 1.Misselhorn A, Hendriks SL. A systematic review of sub-national food insecurity research in South Africa: missed opportunities for policy insights. PLoS One 2017;12:e0182399. 10.1371/journal.pone.0182399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS . Climate change and AIDS: a joint working paper Geneva, 2008. Available: http://data.unaids.org/pub/basedocument/2008/20081223_unep_unaids_joint_working_paper_on_cca_en.pdf
- 3.Watts N, Amann M, Ayeb-Karlsson S, et al. The Lancet countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet 2018;391:581–630. 10.1016/S0140-6736(17)32464-9 [DOI] [PubMed] [Google Scholar]
- 4.FAO, IFAD, UNICEF . The state of food security and nutrition in the world 2020. transforming food systems for affordable healthy diets. Rome: FAO, 2019. [Google Scholar]
- 5.Onyenakie CC, Nnakwe RU, Dear N, et al. Prevalence and predictors of food insecurity among people living with and without HIV in the African cohort study. Public Health Nutr 2022;25:1–14. 10.1017/S136898002100361X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.International Federation of Red Cross and Red Crescent Societies . The cost of doing nothing. The humanitarian price of climate change and how it can be avoided. Geneva, 2020. Available: https://media.ifrc.org/ifrc/wp-content/uploads/sites/5/2019/09/2019-IFRC-CODN-EN.pdf [Accessed 30 Jun 2020].
- 7.FSIN and Global Network against Food Crises . Global report on food crises 2020 September update: in times of COVID-19. Rome, 2020. [Google Scholar]
- 8.Watts N, Amann M, Arnell N, et al. The 2020 report of the Lancet countdown on health and climate change: responding to converging crises. Lancet 2021;397:129–70. 10.1016/S0140-6736(20)32290-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gummerson E, Cardona C, Anglewicz P, et al. The wealth gradient and the effect of COVID-19 restrictions on income loss, food insecurity and health care access in four sub-Saharan African geographies. PLoS One 2021;16:e0260823. 10.1371/journal.pone.0260823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erdogan S, Onifade ST, Altuntas M. Synthesizing urbanization and carbon emissions in Africa: how viable is environmental sustainability amid the quest for economic growth in a globalized world? Environ Sci Pollut Res Int 2022. [DOI] [PubMed] [Google Scholar]
- 11.Adedoyin FF, Alola AA, Bekun FV. The nexus of environmental sustainability and agro-economic performance of Sub-Saharan African countries. Heliyon 2020;6:e04878. 10.1016/j.heliyon.2020.e04878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones AD, Ngure FM, Pelto G, et al. What are we assessing when we measure food security? A compendium and review of current metrics. Adv Nutr 2013;4:481–505. 10.3945/an.113.004119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Misselhorn AA. What drives food insecurity in southern Africa? A meta-analysis of household economy studies. Global Environmental Change 2005;15:33–43. 10.1016/j.gloenvcha.2004.11.003 [DOI] [Google Scholar]
- 14.Chop E, Duggaraju A, Malley A, et al. Food insecurity, sexual risk behavior, and adherence to antiretroviral therapy among women living with HIV: a systematic review. Health Care Women Int 2017;38:927–44. 10.1080/07399332.2017.1337774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dinkelman T, Lam D, Leibbrandt M. Linking poverty and income shocks to risky sexual behaviour: evidence from a panel study of young adults in Cape Town. S Afr J Econ 2008;76:S52–74. 10.1111/j.1813-6982.2008.00170.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weiser SD, Leiter K, Bangsberg DR, et al. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med 2007;4:e260–97. 10.1371/journal.pmed.0040260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Lancet HIV The syndemic threat of food insecurity and HIV. Lancet HIV 2020;7:e75. 10.1016/S2352-3018(20)30004-7 [DOI] [PubMed] [Google Scholar]
- 18.Ojo T, Ruan C, Hameed T, et al. HIV, tuberculosis, and food insecurity in Africa-A Syndemics-Based scoping review. Int J Environ Res Public Health 2022;19:19031101. 10.3390/ijerph19031101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onono MA, Odhiambo G, Sheira L, et al. The role of food security in increasing adolescent girls' agency towards sexual risk taking: qualitative findings from an income generating agricultural intervention in southwestern Kenya. BMC Public Health 2021;21:2028. 10.1186/s12889-021-12051-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Austin KF, Noble MD, Berndt VK. Drying climates and gendered suffering: links between drought, food insecurity, and women's HIV in less-developed countries. Soc Indic Res 2021;154:313–34. 10.1007/s11205-020-02562-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aibibula W, Cox J, Hamelin A-M, et al. Association between food insecurity and HIV viral suppression: a systematic review and meta-analysis. AIDS Behav 2017;21:754–65. 10.1007/s10461-016-1605-5 [DOI] [PubMed] [Google Scholar]
- 22.Tsikhutsu I, Bii M, Dear N, et al. Prevalence and correlates of viral load suppression and HIV drug resistance among children and adolescents in South Rift Valley and Kisumu, Kenya. Clin Infect Dis 2022:ciac059. 10.1093/cid/ciac059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Becker N, Poudel KC, Cordeiro LS, et al. A quantitative analysis of food insecurity and other barriers associated with ART nonadherence among women in rural communities of Eswatini. PLoS One 2021;16:e0256277. 10.1371/journal.pone.0256277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bekun FV, Akadin SS. Poverty and agriculture in Southern Africa revisited: a panel causality perspective. SAGE Open 2019;9. [Google Scholar]
- 25.Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr 2011;94:1729S–39. 10.3945/ajcn.111.012070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanser F, Vandormael A, Cuadros D, et al. Effect of population viral load on prospective HIV incidence in a hyperendemic rural African community. Sci Transl Med 2017;9:aam8012. 10.1126/scitranslmed.aam8012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.LePHIA 2016-2017 Collaborating Institutions . LePHIA 2016-2017 interview and biological datasets v1.0 (DTA), 2017. [Google Scholar]
- 28.SHIMS2 2016-2017 Collaborating Institutions . SHIMS2 2016-2017 interview and biological datasets v1.0 (DTA), 2017. [Google Scholar]
- 29.THIS 2016-2017 Collaborating Institutions . THIS 2016-2017 interview and biological datasets v1.0 (DTA), 2017. [Google Scholar]
- 30.NAMPHIA 2017 Collaborating Institutions . NAMPHIA 2017 interview and biological datasets v1.0 (DTA), 2017. [Google Scholar]
- 31.UPHIA 2016-2017 Collaborating Institutions . UPHIA 2016-2017 interview and biological datasets v1.0 (DTA, 2017. [Google Scholar]
- 32.ZAMPHIA 2016 Collaborating Institutions . ZAMPHIA 2016 interview and biological datasets v1.0 (DTA, 2017. [Google Scholar]
- 33.ICAP at Columbia . PHIA project: a drop that counts New York, NY, 2016. Available: https://phia.icap.columbia.edu/ [Accessed 1 May 2020].
- 34.Sachathep K, Radin E, Hladik W, et al. Population-based HIV impact assessments survey methods, response, and quality in Zimbabwe, Malawi, and Zambia. J Acquir Immune Defic Syndr 2021;87:S6–16. 10.1097/QAI.0000000000002710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ballard T, Coates J, Swindale A. Household hunger scale: indicator definition and measurement guide. in: food and nutrition technical assistance II project, ed. Washington, DC, 2011. [Google Scholar]
- 36.Duong YT, Qiu M, De AK, et al. Detection of recent HIV-1 infection using a new limiting-antigen avidity assay: potential for HIV-1 incidence estimates and avidity maturation studies. PLoS One 2012;7:e33328. 10.1371/journal.pone.0033328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization . WHO Working Group on HIV incidence measurement and data use Geneva, 2018. Available: https://apps.who.int/iris/bitstream/handle/10665/272940/WHO-CDS-HIV-18.9-eng.pdf
- 38.Rutstein S. Steps to constructing the new DHS wealth index, 2015. [Google Scholar]
- 39.Pascoe SJS, Langhaug LF, Mavhu W, et al. Poverty, food insufficiency and HIV infection and sexual behaviour among young rural Zimbabwean women. PLoS One 2015;10:e0115290. 10.1371/journal.pone.0115290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loevinsohn M. The 2001-03 famine and the dynamics of HIV in Malawi: a natural experiment. PLoS One 2015;10:e0135108. 10.1371/journal.pone.0135108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Akullian A, Bershteyn A, Klein D, et al. Sexual partnership age pairings and risk of HIV acquisition in rural South Africa. AIDS 2017;31:1755–64. 10.1097/QAD.0000000000001553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Male partner age and HIV infection among young women in cohabitating partnerships in five countries in southern Africa. 10th International AIDS Society Conference on HIV Science; Mexico City, Mexico 2019.
- 43.Miller CL, Bangsberg DR, Tuller DM, et al. Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS Behav 2011;15:1512–9. 10.1007/s10461-010-9693-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ivers LC, Cullen KA. Food insecurity: special considerations for women. Am J Clin Nutr 2011;94:1740S–4. 10.3945/ajcn.111.012617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gillespie S, Greener R, Whiteside A, et al. Investigating the empirical evidence for understanding vulnerability and the associations between poverty, HIV infection and AIDS impact. AIDS 2007;21:S1–4. 10.1097/01.aids.0000300530.67107.45 [DOI] [PubMed] [Google Scholar]
- 46.Tsai AC, Hung KJ, Weiser SD. Is food insecurity associated with HIV risk? Cross-sectional evidence from sexually active women in Brazil. PLoS Med 2012;9:e1001203. 10.1371/journal.pmed.1001203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schaefer R, Gregson S, Eaton JW, et al. Age-disparate relationships and HIV incidence in adolescent girls and young women: evidence from Zimbabwe. AIDS 2017;31:1461–70. 10.1097/QAD.0000000000001506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Justman J, Reed JB, Bicego G, et al. Swaziland HIV incidence measurement survey (SHIMS): a prospective national cohort study. Lancet HIV 2017;4:e83–92. 10.1016/S2352-3018(16)30190-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Field Exchange . Is targeting of food aid directly to women based on gender roles and appropriate response? Lessons from Southern Sudan, 1999, 2020. Available: https://www.ennonline.net/fex/6/directly [Accessed 22 Feb 2020].
- 50.Qiao S, Li X, Stanton B. Social support and HIV-related risk behaviors: a systematic review of the global literature. AIDS Behav 2014;18:419–41. 10.1007/s10461-013-0561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bertozzi SM, Gutiérrez J-P. Poverty, cash transfers, and risk behaviours. Lancet Glob Health 2013;1:e315–6. 10.1016/S2214-109X(13)70111-6 [DOI] [PubMed] [Google Scholar]
- 52.Gottert A, Pulerwitz J, Heck CJ, et al. Creating HIV risk profiles for men in South Africa: a latent class approach using cross-sectional survey data. J Int AIDS Soc 2020;23:e25518. 10.1002/jia2.25518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McLinden T, Stover S, Hogg RS. HIV and food insecurity: a syndemic amid the COVID-19 pandemic. AIDS Behav 2020;24:2766–9. 10.1007/s10461-020-02904-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Akullian A, Vandormael A, Miller JC, et al. Large age shifts in HIV-1 incidence patterns in KwaZulu-Natal, South Africa. Proc Natl Acad Sci U S A 2021;118:2013164118. 10.1073/pnas.2013164118 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058704supp001.pdf (2.3MB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All data are publicly available for download from the PHIA website.