Abstract
Objective/Background
To examine the impact of prostate cancer (PCa) on sleep health for patients and caregivers. We hypothesized that sleep disturbances and poor sleep quality would be prevalent among patients with PCa and their caregivers.
Patients/Methods
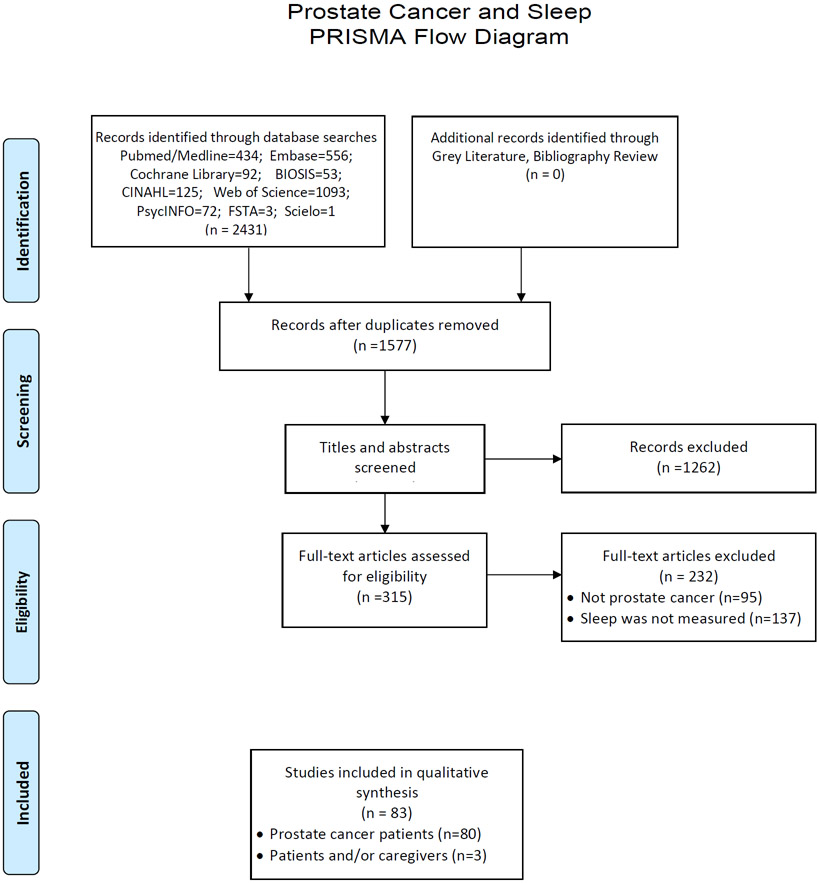
A systematic literature search was conducted according to the Preferred Reporting Items for a Systematic Review and Meta-analysis guidelines. To be eligible for this systematic review, studies had to include: (1) patients diagnosed with PCa and/or their caregivers; and (2) objective or subjective data on sleep. 2,431 articles were identified from the search. After duplicates were removed, 1,577 abstracts were screened for eligibility, and 315 underwent full-text review.
Results and Conclusions
Overall, 83 articles met inclusion criteria and were included in the qualitative synthesis. The majority of papers included patients with PCa (98%), who varied widely in their treatment stage. Only 3 studies reported on sleep among caregivers of patients with PCa. Most studies were designed to address a different issue and examined sleep as a secondary endpoint. Commonly used instruments included the Insomnia Severity Index and European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaires (EORTC-QLQ). Overall, patients with PCa reported a variety of sleep issues, including insomnia and general sleep difficulties. Both physical and psychological barriers to sleep are reported in this population. There was common use of hypnotic medications, yet few studies of behavioral interventions to improve sleep for patients with PCa or their caregivers. Many different sleep issues are reported by patients with PCa and caregivers with diverse sleep measurement methods and surveys. Future research may develop consensus on validated sleep assessment tools for use in PCa clinical care and research to promote facilitate comparison of sleep across PCa treatment stages. Also, future research is needed on behavioral interventions to improve sleep among this population.
Keywords: caregivers, quality of life, Prostate cancer, sleep, sleep health, caregiver, urology, individualized patient profile, improved individual outcomes, primary, secondary, tertiary care
INTRODUCTION
Sleep problems are extremely common in the population and result in substantial morbidity. 35.5% of US male adults have short sleep duration (<7 hours),1 and it is associated with multiple chronic health conditions and greater health utilization.
Another major issue is sleep apnea, involving abnormal breathing during sleep, with an estimated global prevalence of 711-961 million.2 Sleep apnea is associated with multiple cardiovascular sequelae. Sleep apnea has also been associated with urinary and sexual problems in men, including nocturia3 and erectile dysfunction.4
Previous studies have examined the relationship between sleep disorders and cancer risk. Liu et al. reported pooled results showing that neither short sleep nor long sleep was associated with the risk of prostate cancer (PCa).5 Similarly, a systematic review by Stone et al. reported no significant relationships between short or long sleep duration and PCa-specific mortality.6 By contrast, shift work was associated with an increased risk of PCa.7
Another important consideration is survivorship and maximizing quality of life for cancer survivors. For patients who are recently diagnosed or treated for cancer, previous research has reported high rates of sleep disturbances of up to 75%, substantially higher than the general population.1 That notwithstanding, most studies have focused on breast cancer.8 Less is known about the prevalence of sleep health problems among patients diagnosed with PCa, or their family caregivers. However, research in other chronic conditions has shown that caregivers experience sleep disruption which in turn impinge upon their quality of life and caregiving capacity.9 Our objective was to examine the impact of PCa on sleep health, including the type and frequency of sleep problems, association of sleep health with quality of life, and interventions to improve sleep health in patients with PCa and caregivers. We hypothesize that sleep disturbances and poor sleep quality are prevalent among patients with PCa and caregivers..
METHODS
We conducted a systematic review of research on sleep among patients with PCa and/or caregivers. To do so, we identified published studies that administered sleep monitoring devices and/or sleep-related questionnaires or survey items to patients with PCa and/or their caregivers.
Eligibility Criteria
To be eligible for this systematic review, studies had to include: (1) patients diagnosed with PCa and/or caregivers of patients with PCa; and (2) measurement of sleep. Studies were excluded if they did not collect sleep data specifically for patients with PCa or their caregivers (e.g., aggregate responses among patients with a variety of cancer diagnoses), if only fatigue was measured instead of sleep, non-English, or only published as an abstract. Figure 1 displays the PRISMA flow diagram.
Figure 1.
PRISMA Flow Diagram
Search Strategy
A systematic literature search was according to the PRISMA guidelines on January 21, 2020, including PubMed/Medline, Embase, the Cochrane Library, Biosis Citation Index (BCI), Cumulative Index to Nursing and Allied Health (CINAHL), Web of Science, Food Science & Technology Abstracts, and APA PsycINFO. No date or language limits were applied. Bibliographies of included studies were reviewed for additional references (see Appendix for search strategy).
Data Screening and Extraction
Two reviewers independently screened titles and abstracts using Covidence, with disagreements resolved by consensus discussion. The full texts of potentially eligible articles were retrieved and reviewed for inclusion. Bibliographies of these selected articles was analyzed for further eligible articles. The studies that met inclusion criteria were assessed by ≥2 independent reviewers using a standardized data extraction form to ensure they satisfied the inclusion criteria. Extracted data included the sample size, cancer-related data, study design, subjective and/or objective measures of sleep, and analysis of the links between sleep health with other outcomes (e.g., quality of life). Disagreements were resolved through consensus. Eligible studies were assessed for quality utilizing the Hawker et al. quality assessment checklist, with scores ranging from 9-36.10
RESULTS
We identified 80 studies reporting on sleep among patients with PCa (Table 1) and 3 studies that included caregivers or both patients and caregivers (Table 2). The results are grouped by the sleep measure applied (see Appendix for a description of the measures).
Table 1.
Summary of the studies that included prostate cancer patients (N=80).
| Question(s) or Scale(s) Administered |
First Author | Year | Main Objective of the Study | Country | Sample Size (Total) |
Sample Size (Prostate Patients) |
Quality Scores † |
|---|---|---|---|---|---|---|---|
| Actigraphy | Holliday12 | 2016 | This prospective, longitudinal, phase II study assessed fatigue, sleep, and serum cytokine levels during radiotherapy for early-stage prostate cancer. | US | 28 | 28 | 30 |
| Actigraphy, Epworth Sleepiness Scale | Hanisch11 | 2011 | The aims of this study were to conduct a more detailed analysis of sleep patterns and to assess the effects of poor sleep on daily functioning among patients with prostate cancer undergoing androgen deprivation therapy. | US | 60 | 60 | 24 |
| Athens Insomnia Scale | Navarro-Martinez13 | 2019 | To evaluate the role of peripheral inflammation in frailty syndrome in patients with prostate cancer undergoing antiandrogen therapy. | Spain | 46 | 46 | 33 |
| BPI | Khan14 | 2011 | The aim of this study was to examine the reported rates and predictive factors of sleep disturbance in patients with bone metastases. | Canada | 400 | 96 | 34 |
| Cancer Problems in Living Scale | Baker94 | 2005 | This study identified the psychosocial problems that patients from 3 states who had been diagnosed with 1 of the 10 most commonly occurring cancers indicated concerned them the most. | US | 752 | 97 | 32 |
| Edmonton Symptom Assessment System | Yennurajalingam95 | 2012 | The aim of this study was to describe the impact of an outpatient palliative care consultation on symptoms in patients with advanced prostate cancer. | US | 55 | 55 | 31 |
| EORTC QLQ-C15 PAL Questionnaire | Jasinska21 | 2010 | The objective of this study was to assess the change of quality of life of hospitalized terminally ill palliative oncological patients, using the newly developed EORTC Core Quality of Life Questionnaire (QLQ-C15-PAL). | Poland | 41 | 4 | 31 |
| EORTC QLQ-C30 | van Andel23 | 2003 | This study compared the effects on health-related quality of life of epirubicin administered on a 4-weekly versus a weekly intravenous regimen. | The Netherlands | 79 | 79 | 34 |
| EORTC QLQ-C30 | Collette20 | 2004 | The aim of this study was to examine whether baseline health-related quality of life parameters assessed by the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire C30 (EORTC QLQ-C30) were independent prognostic factors of survival. | Multi-center several countries in Europe | 391 | 391 | 33 |
| EORTC QLQ-C30 | Jonler18 | 2005 | The first objective of this study was to describe quality of life in a group of patients diagnosed with metastatic prostate cancer and skeletal metastases. At the time of evaluation, the patients had not received any treatment but were evaluated before entering a study of androgen-modulating therapy (the Scandinavian Prostate Cancer Group study 5). The second objective was to identify demographic and disease-related factors affecting quality of life. | Denmark, Finland, Iceland, Iceland, Norway and Sweden | 917 | 917 | 33 |
| EORTC QLQ-C30 | Lintz96 | 2003 | This study investigated the support and psychological care needs of men with prostate cancer. | UK | 210 | 210 | 36 |
| EORTC QLQ-C30 | Mols22 | 2009 | This study describes the differences in short-term effects of health-related quality of life in prostate brachytherapy patients who were treated with and without volume-reducing hormone therapy. | the Netherlands | 312 | 312 | 33 |
| EORTC QLQ-C30 | Roeloffzen25 | 2010 | The aim of this study was to prospectively assess long-term health-related quality of life 6 years after prostate brachytherapy. | the Netherlands | 127 | 127 | 32 |
| EORTC QLQ-C30 | Vordermark24 | 2006 | The study compares the effects of two modalities of dose-escalated radiotherapy on health-related quality of life. | Germany | 84 | 84 | 28 |
| EORTC QLQ-C30 | Zenger17 | 2010 | The aim of this study is two-fold. The first part compares quality of life data of patients with prostate cancer with those of a representative and age-specific sample of the general population and the influence of cancer related as well as socio-demographic parameters on quality of life. | Germany | 444 | 265 | 26 |
| EORTC QLQ-C30, FACT-G | Sullivan97 | 2007 | The aim of this study was to assess health-related quality of life for patients with hormone-refractory prostate cancer. | UK, Australia, Canada, France, Italy, US | 280 | 280 | 28 |
| Epworth Sleepiness Scale | Monga27 | 1999 | The objectives of this study were to (1) prospectively evaluate fatigue utilizing validated instruments in patients with localized prostate cancer, and (2) examine the relationships between fatigue, depression, quality of life, and sleep disturbance. | US | 36 | 36 | 31 |
| Epworth Sleepiness Scale | Sharma28 | 2009 | This study evaluated the effects of high dose isoflavones on the consequences of androgen deprivation therapy. | US | 33 | 33 | 27 |
| Epworth Sleepiness Scale, PSQI | Koskderelioglu26 | 2017 | This study evaluated the appearance of sleep disturbances in patients on androgen deprivation therapy. | Turkey | 106 | 106 | 34 |
| EQ Visual Analogue Scale | Jefford98 | 2017 | This study assessed the quality of life of survivors of breast, colorectal, or prostate cancer, non-Hodgkin lymphoma or melanoma at 1-, 3- and 5-years post-diagnosis. | Australia | 4,674 | 1,066 | 25 |
| Functional Assessment of Cancer Therapy-General (FACT-G) | Ukoli30 | 2006 | This study assessed the quality of life of African American men who have had radical prostatectomy. | US | 100 | 100 | 34 |
| Functional Assessment of Cancer Therapy-Prostate (FACT-P) | Stephens31 | 2007 | This study explored patients’ quality of life during neoadjuvant hormone therapy. | UK, New Zealand, Australia | 316 | 316 | 29 |
| General Sleep Disturbance Scale | Rich32 | 2017 | This study examined the utility of auricular electroacupuncture for a small cohort of men with androgen deprivation therapy induced vasomotor symptoms while the men underwent radiotherapy | US | 10 | 10 | 27 |
| General Sleep Disturbance Scale (GSDS) | Merriman34 | 2011 | This study aimed to determine if self-reported attentional fatigue differed in patients with breast cancer and prostate cancer before radiation therapy, and to determine the relationships between attentional fatigue and other symptoms in these two groups. | US | 155 | 82 | 34 |
| Generalized Anxiety Disorder-10 | Sharpley35 | 2014 | The aim of this study was to explore the associations between hormone treatment variables and depression, and the nature of depression in prostate cancer patients by comparing the severity and symptom profile of anxiety and depression in men who were currently receiving hormone therapy versus those who were not. | Australia | 156 | 156 | 33 |
| Insomnia Severity Index | Cessna41 | 2016 | This study assessed fatigue in two samples of cancer patients. | US | 257 | 121 | 33 |
| Insomnia Severity Index | Dirksen39 | 2016 | The purpose of this study was to identify and describe symptom cluster subgroups pre-and post-radiation therapy in men with prostate cancer. | US | 84 | 84 | 26 |
| Insomnia Severity Index | Dirksen38 | 2014 | The study purpose was to explore the association between prostate cancer symptoms and cytokine levels at pretreatment and posttreatment. | US | 29 | 29 | 29 |
| Insomnia Severity Index | Dirksen37 | 2009 | The purpose of this study was to describe insomnia in veteran men with prostate cancer and to examine relationships among insomnia, depression, and distress. | US | 51 | 51 | 29 |
| Insomnia Severity Index | Fillion40 | 2003 | This study assessed the validity of an adapted fatigue scale among women and men undergoing therapy for breast or prostate cancer, respectively. | Canada | 604 | 327 | 33 |
| Insomnia Severity Index | Hervouet42 | 2005 | This study compared the prevalence of psychological difficulties (i.e., anxiety and depression), psychophysiological problems (i.e., insomnia and fatigue), and sexual difficulties across three modalities of treatment for prostate cancer (radiotherapy, brachytherapy, and radical prostatectomy) | Canada | 861 | 861 | 33 |
| Insomnia Severity Index | Savard99 | 2015 | The goal of the current study was to assess, separately in patients with breast and prostate cancer, the effect of adjuvant treatments on the evolution of insomnia symptoms and the mediating role of somatic symptoms. | Canada | 728 | 263 | 30 |
| Insomnia Severity Index | Savard45 | 2013 | The aim of this study was to compare the evolution of insomnia symptoms and somatic symptoms in patients receiving combined androgen deprivation therapy and radiation therapy. | Canada | 60 | 60 | 34 |
| Insomnia Severity Index | Savard100 | 2011 | This study aimed to assess the prevalence and natural course (incidence, persistence, remission, and relapse) of insomnia comorbid with cancer during an 18-month period. | Canada | 784 | 235 | 34 |
| Insomnia Severity Index | Savard36 | 2005 | This study assessed the prevalence, clinical characteristics, and risk factors for insomnia in patients treated with radical prostatectomy for prostate cancer. | Canada | 327 | 327 | 32 |
| Insomnia Interview Schedule | Savard44 | 2009 | This study aimed to assess the prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. | Canada | 991 | 269 | 33 |
| Insomnia Severity Index | Trudel-Fitzgerald43 | 2013 | This prospective study investigated longitudinal changes of five symptoms (i.e., depression, anxiety, insomnia, fatigue, and pain) in patients scheduled to undergo surgery for cancer. | Canada | 828 | 234 | 32 |
| International RLS severity scale | Desax46 | 2015 | To present 2 patients with prostate cancer who developed severe restless legs syndrome after starting enzalutamide. | Switzerland | 2 | 2 | 26 |
| MD Anderson Symptom Assessment Inventory (MDASI) | Basch101 | 2015 | The objective of this study was to prospectively evaluate the effect of cabozantanib on pain and narcotic use in metastatic castration-resistant prostate cancer. | US | 144 | 144 | 30 |
| MD Anderson Symptom Assessment Inventory (MDASI) | Cleeland102 | 2013 | This study assessed effects of disease site and stage on the percentages of patients rating symptoms as moderate to severe. | US | 3,106 | 320 | 30 |
| MD Anderson Symptom Assessment Inventory (MDASI) | Gonzalez49 | 2017 | The purpose of this exploratory study was to examine the prevalence of symptoms experienced by Puerto Rican men who were scheduled to receive external beam radiation therapy. | US | 54 | 54 | 29 |
| Medical outcomes Survey (MOS) Sleep scale | Thomas50 | 2010 | This study examined changes in sleep in 33 patients with breast cancer and 23 patients with prostate cancer during radiation therapy and over a 6-month follow-up. | US | 56 | 23 | 30 |
| Memorial Anxiety Scale for Prostate Cancer (MAX-PC) | Mehnert54 | 2007 | This study examines the frequency and character of cancer- and treatment-related problems and its association with symptom distress and prostate cancer-related anxiety in patients at the beginning of an oncological rehabilitation program. | Germany | 197 | 197 | 34 |
| Memorial Anxiety Scale for Prostate Cancer (MAX-PC) | Roth53 | 2003 | In this study, the authors developed and tested the Memorial Anxiety Scale for Prostate Cancer (MAX-PC) to facilitate the identification and assessment of men with prostate cancer-related anxiety. | US | 385 | 385 | 31 |
| Memorial Symptom Assessment Scale (MSAS) | Knapp52 | 2012 | The purposes of this study were to evaluate the trajectories of occurrence, severity, and distress for the six most prevalent symptoms reported by patients with prostate cancer undergoing radiation therapy | US | 82 | 82 | 34 |
| Memorial Symptom Assessment Scale (MSAS) | Portenoy51 | 1994 | The purpose of this study was to explore symptom characteristics and quality of life among a heterogeneous population of cancer patients. | US | 243 | 63 | 27 |
| OSA | Gozal55 | 2016 | The aim of this study was to determine whether cancer incidence for major cancer types and risk of metastases or mortality from cancer are increased in the presence of obstructive sleep apnea. | US | 5,596,888 | 168,154 | 32 |
| Pittsburgh Sleep Quality Index | Elkins56 | 2014 | The purpose of the present article is to describe the use of hypnotic relaxation therapy in the treatment of a patient with prostate cancer suffering from hot flashes | US | 1 | 1 | 21 |
| Pittsburgh Sleep Quality Index | Hoyt60 | 2016 | The purpose of this study was to examine the relationships of sleep disturbance, depressive symptoms, and diurnal cortisol patterns in men treated for prostate cancer. | US | 66 | 66 | 32 |
| Pittsburgh Sleep Quality Index | Humpel62 | 2009 | The aim of this study was to explore if there was also a relationship of physical activity with sleep difficulties and fatigue, common effects of cancer and its treatments. | Australia | 91 | 59 | 33 |
| Pittsburgh Sleep Quality Index | McQuade58 | 2017 | The aim of this study was to examine the efficacy of tai chi/qigong in men with prostate cancer undergoing radiotherapy. | 90 | 90 | 36 | |
| Pittsburgh Sleep Quality Index | Penedo103 | 2006 | To examine the quality of life (QOL) in a sample of men recently treated for localized prostate cancer to determine whether minority men are at greater risk of decrements in QOL and to identify factors that might explain disparities in QOL outcomes. | US | 204 | 204 | 32 |
| Pittsburgh Sleep Quality Index | Golshani57 | 2019 | The present study aimed to comparing the effectiveness of mindfulness-based cognitive therapy with acceptance and commitment therapy on severity of fatigue, sleep quality and the resiliency in a patient with prostate cancer. | Iran | 1 | 1 | 27 |
| Pittsburgh Sleep Quality Index | Saini59 | 2013 | The aim of this study was to compare the occurrence of depression, anxiety, self-body image perception, sleep disturbances, and diminished quality of life in patients with prostate cancer undergoing adjuvant androgen-deprivation therapy as opposed to patients in observation. | Italy | 103 | 103 | 31 |
| Pittsburgh Sleep Quality Index, GSDS | Miaskowski33 | 2011 | The aim of this study was to examine how self-reported ratings of sleep disturbance changed from the time of the simulation visit to four months after the completion of radiation therapy. | US | 82 | 82 | 32 |
| PROMIS-Sleep Disturbance | Dickinson65 | 2019 | The purpose of this study was to describe the multidimensional fatigue experience of men with prostate cancer enrolled in an ongoing descriptive longitudinal study involving men diagnosed with nonmetastatic prostate cancer scheduled to receive external beam radiation therapy | US | 57 | 57 | 35 |
| PROMIS-Sleep Disturbance | Feng68 | 2019 | This study aimed to investigate co-occurring symptoms associated with persistent fatigue in men receiving external beam radiation therapy for nonmetastatic prostate cancer. | US | 47 | 47 | 34 |
| PROMIS-Sleep Disturbance | Jensen67 | 2017 | The aim of this study was to estimate cancer population-based reference values in the United States for the PROMIS domains by age and stage of disease. | US | 5,284 | 1,140 | 32 |
| PROMIS-Sleep Disturbance | Lashbrook66 | 2018 | To identify factors associated with psychosocial, physical, and practical difficulties of daily living and distress among cancer survivors from a regional area in Australia. | Australia | 134 | 34 | 33 |
| PROMIS-Sleep Disturbance | Quach63 | 2016 | To evaluate the reliability and validity of six PROMIS measures (anxiety, depression, fatigue, pain interference, physical function, and sleep disturbance) telephone-administered to a diverse, population-based cohort of patients with localized prostate cancer | US | 778 | 778 | 34 |
| PROMIS-Sleep Disturbance | Reeve64 | 2018 | This study explored symptom burden and functional status among men with prostate cancer to identify patient characteristics associated with health-related quality of life. | US | 373 | 373 | 35 |
| Qualitative methods | Flynn104 | 2010 | The goal of this focus group study was to develop a qualitative summary of the unique and broad spectrum of effects that cancer and cancer treatments can have on patients' sleep-wake functioning | US | 67 | 18 | 28 |
| Qualitative methods | Grunfeld87 | 2012 | This study explored the experience and impact of androgen deprivation therapy symptoms, particularly hot flashes, among men with metastatic prostate cancer, using focus groups. | England | 21 | 21 | 25 |
| Qualitative methods | Holmstrom86 | 2019 | The aim of this study was to use a patient centerd approach to develop a conceptual model describing the salient symptoms and impacts of metastatic castration-resistant prostate cancer in chemotherapy-naive patients. | US | 19 | 19 | 34 |
| Self-reported | Bill-Axelson77 | 2013 | To compare patterns of symptom burden and distress in men with localized prostate cancer randomized to radical prostatectomy or watchful waiting and followed up longitudinally. | Sweden | 272 | 272 | 31 |
| Self-reported | Challapalli78 | 2018 | To assess the prevalence of vasomotor symptoms in men receiving ADT for their prostate cancer. | UK | 250 | 250 | 28 |
| Self-reported | Greenberg80 | 1993 | This study aimed to define changes in sleep and subjective fatigue associated with radiation treatment over a 15-week period. | US | 15 | 15 | 27 |
| Self-reported | Jan79 | 2016 | This study evaluated the association between perceived stress, social support, disease progression and mortality after diagnosis of prostate cancer using a larger cohort | Sweden | 4,105 | 4,105 | 31 |
| Self-reported | LeMasters76 | 2013 | Objectives were to compare health-related quality of life between survivors of breast cancer, prostate cancer, and colorectal cancer to matched controls. | US | 11,964 | 3,636 | 28 |
| Self-reported | Msaouel74 | 2017 | The primary aim of this study was to inform providers on patient-expressed issues while enhancing the content validity of instruments assessing quality of life and patient reported outcomes in prostate cancer. | US | 2,128 | 2,128 | 33 |
| Self-reported | Pacheco73 | 2016 | This study aimed to examine whether any of the behaviors and risk factors for prostate cancer were found in men with other cancers, compared with control subjects. | Argentina | 1,349 | 326 | 23 |
| Self-reported | Tewari75 | 2008 | This pilot study aimed to assess feasibility of avoiding a urethral catheter after robotic radical prostatectomy by using suprapubic diversion with a urethral splint. | US | 30 | 30 | 32 |
| Self-reported nighttime awakenings | Alban69 | 2008 | To report the use of acupuncture to treat frequent urination and nocturia following radical prostatectomy. | US | 1 | 1 | 22 |
| Self-reported sleep problems | Cindolo72 | 2009 | The aims were to study the acceptability rate of and overall patient satisfaction with an automatic sequential leg compression system. | Italy | 184 | 184 | 29 |
| Self-reported sleep problems | Kim70 | 2002 | This study examined the relation between patients' self-reported severity of side effects and their levels of negative affect, and the efficacy of an informational intervention in ameliorating or preventing symptom development. | US | 152 | 152 | 25 |
| Self-reported sleep quality and duration | Carlson71 | 2004 | This paper reports the results of pre- post-intervention study of an eight-week mindfulness-based stress reduction intervention provided to patients with breast and prostate cancer. | Canada | 105 | 10 | 24 |
| Sleep Disturbance Index (SDI) | Gustafsson82 | 1995 | The aim of this study was to investigate the psychological reactions associated with screening for prostate cancer with special focus on the impact of false positive and true positive test results | Sweden | 2,400 | 33 | 25 |
| Surgical Outcomes Measurement System (SOMS) | Kundu83 | 2018 | The aim of this study was to prospectively evaluate physical and psychosocial functioning after diagnosis of prostate cancer and factors associated with treatment satisfaction. | US | 54 | 54 | 35 |
| Symptom Related Daily Interference Scale | de Valois81 | 2015 | The aim of this research was to evaluate the feasibility of using a 5-point ear acupuncture protocol to improve the well-being of men diagnosed with prostate cancer. | UK | 20 | 20 | 32 |
| You, Your Family, and the City of of Hope are a Team screening instrument | Zhou84 | 2018 | This study explored the prevalence of sleep problems and its correlates in a large sample of cancer patients prior to initiating treatment. | US | 5,702 | 469 | 32 |
Notes.
Quality scores are tabulated according to the Hawker et al. quality assessment checklist, with scores ranging from 9 to 36.
Table 2.
Summary of the studies that included caregivers of patients with prostate cancer (N=3).
| Question(s) or Scale(s) Administered |
First Author | Year | Main Objective of the Study | Country | Sample Size |
Quality Scores† |
|---|---|---|---|---|---|---|
| Self-report | Robbins85 | 2016 | The aim of this study was to analyze sleep barriers reported by patients with prostate cancer and caregivers posted to a large online health community. | Worldwide | 685 | 26 |
| General Sleep Disturbance Scale | Fletcher86 | 2008 | The purpose of this study was to determine the prevalence and severity of depression, anxiety, pain, sleep disturbance, and fatigue in a sample of family caregivers of patients with prostate cancer who were to begin radiation therapy. | US | 60 | 33 |
| General Sleep Disturbance Scale | Fletcher87 | 2009 | This study examined predictors of and trajectories for evening and morning fatigue were evaluated in family caregivers of oncology patients. | US | 60 | 32 |
Notes.
Quality scores are tabulated according to the Hawker et al. quality assessment checklist, with scores ranging from 9 to 36.
Studies of Sleep in Patients with Prostate Cancer (Table 1; N=80)
Actigraphy
Two studies were identified that measured sleep with actigraphy. Hanisch et al.11 examined patients with PCa undergoing androgen deprivation therapy (ADT). Total sleep time was 5.9 hours, and sleep efficiency was 75%. Holliday et al.12 recruited early-stage PCa patients undergoing radiotherapy. Over the course of therapy, there was a trend of decreased sleep onset latency (rate change: 0.86), indicating that patients fell asleep faster as therapy continued, but no significant difference in sleep efficiency or sleep duration across the weeks of therapy. In summary, these studies using objective sleep parameters found insufficient sleep duration in patients on ADT, and no change in sleep duration during radiation therapy.
Athens Insomnia Index (AII)
One study, conducted by Navarro-Martínez et al., administered the Athens Insomnia Index (AII). They examined peripheral inflammation among patients with PCa undergoing antiandrogen therapy, finding sub-threshold insomnia symptoms among the men according to the AII (2.3).13
Brief Pain Inventory (BPI)
One study in this review measured sleep using the Brief Pain Inventory (BPI). Specifically, in a mixed population of cancer patients (25% PCa) with symptomatic bone metastases treated with palliative radiation therapy, Khan and colleague found PCa was not significantly associated with sleep disturbance, as captured on the BPI, compared to other primary cancer sites.14
Cancer Problems in Living Scale (CPILS)
One study in this review used the CPILS to measure sleep. Specifically, Baker et al. administered the CPILS to PCa patients 1 year post-diagnosis and found 37% reported sleep difficulties were a top concern among patients.15
Edmonton Symptom Assessment System
One study in this review examined sleep using the Edmonton Symptom Assessment System. Specifically, Yennurajalingam and colleagues surveyed patients with advanced PCa and found that 40% had clinically relevant problems with sleep.16
The European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire (EORTC-QLQ)
Ten studies administered the EORTC-QLQ, which includes a question assessing sleep difficulties. Approximately half of these studies assessed prevalence of sleep difficulties in specific populations and/or the relationship between sleep difficulties and outcomes, such as survival. For instance, Zenger found that 39% of a sample of PCa patients at various treatment stages reported sleep difficulties, noting that this was higher than the general population (29%).17 Jonler and colleagues found that 25% of patients with metastatic PCa reported sleep difficulties,18 yet Lintz and colleagues found that sleep difficulties were more common among patients with advanced versus localized PCa.19 In a prospective analysis of patients with metastatic PCa, Collette and colleagues found that sleep difficulty, paradoxically, was an independent predictor of survival.20
The remaining studies made use of the EORTC-QLQ to examine change in symptoms. For instance, Jasinska and colleagues found that 42% of hospitalized terminally ill patients with PCa reported sleep difficulties, which remained unchanged between the beginning and end of their hospital stay.21 Mols et al. recruited patients with PCa to complete questionnaires before treatment and 6 weeks and 3 months post-treatment, finding patients with PCa reported significant decreased sleep difficulty post-treatment.22 van Andel et al., conducted a prospective randomized trial of patients randomized to either receive epirubicin 25 mg/m2 weekly or 100 mg/m2 every 4-weeks. After 8 weeks, patients treated with 100 mg of epirubicin reported less sleep difficulty compared to before starting the medication.23 Vordermark et al., conducted a cross-sectional survey of men treated with either 3-D conformal boost to 74Gy or two high dose rate brachytherapy boost after 46 Gy 3-D conformal treatment.24 Sleep difficulty had the highest mean score among the other EORTC QLQ-C30 symptoms. Roeloffzen et al., 2010 investigated quality of life in PCa post-brachytherapy, finding a statistically significant reduction in insomnia at 6 years post-treatment compared to the baseline.25 In summary, the EORTC-QLQ-C30 was used in numerous studies, including patients with both localized and advanced disease, with variable results as to the extent of sleep problems compared to other quality of life issues, and in one study suggesting a link between sleep difficulty with survival.
Epworth Sleepiness Scale (ESS)
Several studies administered the ESS. Hanisch et al. found that patients undergoing ADT reported mild levels of sleepiness.11 Another study found that sleepiness was higher among patients with PCA undergoing ADT than those not undergoing ADT.26 Monga et al. evaluated sleep in patients with localized PCa throughout different stages of radiotherapy, finding an increase in ESS score from pre-radiotherapy to completion of treatment.27 Sharma et al. reported results of a randomized controlled trial comparing the effect of high dose isoflavones versus taste-matched control in patients with PCa undergoing androgen deprivation therapy, finding no significant difference in sleepiness between baseline scores and scores at 6- or 12 months post-treatment.28
EQ Visual Analogue Scale
Jefford et al. measured patient-reported quality of life among cancer survivors several years post-diagnosis using the EQ Visual Analogue Scale.29 At 1-year post-diagnosis, 29.6% of patients with PCa said agree or strongly agree to “I always feel tired,” while 35.0% agreed with this statement 5-years post-diagnosis.
Functional Assessment of Cancer Therapy (Prostate: FACT-P and General: FACT-G)
Two studies administered the FACT. Ukoli and colleagues performed a cross-sectional survey to assess quality of life after radical prostatectomy in African American men, finding that 53% reported fatigue and 39% reported sleep probems.30 Stephens and colelagues examined changes in quality of life during neoadjuvant hormonal therapy in a subset of patients with PCa in a trial of standard and high-dose radiotherapy.31 Compared to the baseline, patients reported that they were sleeping less well than usual, with an increase in fatigue. In summary, these two studies demonstrated that fatigue and sleep problems among patients treated by radical prostatectomy worsened after hormonal therapy.
General Sleep Disturbance Scale (GSDS)
Several studies administered the GSDS. Rich and colleagues found that auricular electroacupuncture among patients with PCa undergoing ADT was associated with a decline in sleep disturbance (mean 57 to 37).32Miaskowski and colleagues measured longitudinal changes in sleep disturbance using the GSDS in patients with PCa undergoing primary or adjuvant radiation therapy.33 Sleep disturbance increased over the course of radiation therapy, then declined after treatment. Merriman et al. examined the relationship between attentional fatigue with sleep quality in patients with breast and PCa prior to radiation therapy. Among patients with PCa, sleep disturbance was inversely associated with fatigue.34 In summary, studies using the GSDS highlight specific patient factors associated with sleep disturbances, the relationship between attentional fatigue with sleep disturbances, and a possible benefit from auricular electroacupuncture.
Generalized Anxiety Disorder-10 (GAD-10)
Sharpley et al. measured anxiety scores in patients with PCa using the “GAD-10” (GAD-7 supplemented by 3 additional items).35 Among patients not using ADT, the mean GAD-10 score for trouble sleeping was 1.5 versus 1.9 with ADT(p=0.004).
Insomnia Severity Index (ISI)
Twelve studies administered the ISI. Savard et al., 2005 surveyed patients with PCa an average of 4 years after treatment.36 Overall, 31.5% reported non-specific sleep difficulties with 18% meeting insomnia criteria. Among men meeting criteria for insomnia, 47.5% reported that onset followed the cancer diagnosis. Among patients with insomnia prior to diagnosis, 68% reported that the cancer diagnosis and/or treatment aggravated their sleep difficulties.
Savard et al., 2013 recruited patients with PCa receiving radiation therapy with or without ADT to complete questionnaires regarding insomnia over 16 months. Insomnia was present in 14.3% of the radiation therapy group and 22.0% of the radiation therapy/ADT group at baseline. Rates remained relatively stable during follow-up in the radiation group (range 13.5 to 21.6%), whereas they increased progressively in the radiation therapy/ADT group to 41.9% at 4 months and remained around 40% thereafter. Hot flashes and night sweats were significant mediators of the relationship between ADT and insomnia. Urinary frequency was a significant mediator of the relationship between radiation therapy with insomnia.
Savard et al., 2015 conducted a longitudinal study of the effect of adjuvant treatments for patients with breast and PCa over 18-months. Hormone therapy exposure was associated with significantly increased ISI scores overall (mean of 5.4 vs 7.3), which was mediated by night sweats (48.6% of total effect).
Dirksen et al., 2009 recruited veterans with PCa undergoing various treatments for a survey study, 51% of whom had metastatic disease.37 Mean ISI score among the sample was 9.9, and 53% had clinically significant insomnia, with 45% experiencing “difficulty initiating sleep” and 55% experiencing “problems maintaining their sleep.” When men complained about sleep problems to their healthcare provider, almost all were prescribed sleeping medication. There was a significant positive relationship between insomnia severity with depression.
Dirksen et al., 2014. conducted a longitudinal study of patients with nonmetastatic PCa.38 There were significant differences between pre- and post-radiation ISI scores (5.4 versus 7.4). Dirksen et al., 2016 conducted a longitudinal study of symptoms in patients with PCa receiving radiation therapy.39 Insomnia was found to significantly worsen post-treatment (pretreatment mean: 5.5, post treatment mean: 6.5).
Fillion et al. recruited patients with breast and PCa (at surgical follow-up) to perform a French-Canadian adaptation of the Multidimensional Fatigue Inventory,40 and the ISI. The mean ISI score among the prostate sample was 6.1. Higher fatigue was associated with greater insomnia.
Cessna et al. recruited patients with hematologic cancer and PCa, including men starting ADT and men previously treated with surgery without ADT.41 They found that greater fatigue was significantly correlated with insomnia in the subset with PCa.
Hervouet et al. conducted a cross-sectional study of patients with PCa treated with various methods (radiotherapy, brachytherapy, and radical prostatectomy),42 and 31.9% reported insomnia. There were no significant differences in insomnia between treatment types.
Trudel-Fitzgerald et al. conducted a prospective longitudinal study of patients with cancer receiving different treatments.43 Patients with PCa reported less insomnia and fatigue compared to breast, gynecological and other cancer types. In summary, many studies have examined insomnia using the ISI in patients undergoing multiple forms of treatment for PCa, generally showing higher rates of insomnia after treatment, particularly hormonal therapy.
Insomnia Interview Schedule (IIS)
Savard et al. (2009) conducted a prospective longitudinal study measuring the prevalence of insomnia across patients with various cancer sites.44 Among participants with various cancers, 28.5% and 26.2% met diagnostic criteria for insomnia disorder at baseline and at 2 months, respectively. Patients with PCa presented with the lowest rates of insomnia across other cancer sites with rates of 15.8% at baseline and 15.9% at 2 months. Combining insomnia disorder and insomnia symptoms, prevalence rates were 37.8% at baseline which significantly decreased to 27.8% at 2 months.
Savard et al. (2011) assessed the prevalence of insomnia in patients with PCa across 18 months.45 Prevalence of insomnia was the lowest for patients with PCa (25% to 39%) throughout the study duration, compared to other forms of cancer. In summary, studies using the ISS suggest lower rates of insomnia in PCa compared to other cancer types.
International Restless Legs Syndrome (RLS) Severity Scale
Desax et al. published a case report of two patients with metastatic castration-resistant PCa.46 Both patients reported RLS with enzalutamide, with scores of 27 and 28 out of 40 on the RLS Severity Scale.
MD Anderson Symptom Inventory (MDASI)
Three studies administered the MDASI. Basch et al., examining cabozantanib and pain, found that PCa patients who experienced a reduction in pain also reported a reduction (approximately 50%) in sleep disturbance versus those without a decrease in pain.47 Second, Cleeland et al., conducted a prospective study of symptoms in patients with various cancers, finding disturbed sleep was the second most severe reported symptom among patients with PCa after fatigue.48 Third, Gonzalez and colleagues examined symptom burden among men with PCa undergoing radiation therapy, finding disturbed sleep was the most severe symptom among men who receiving ADT; whereas, participants who did not receive ADT reported no severe symptoms that interfered with daily activities.49 In summary, three studies showed that sleep disturbance is among the most severe symptoms reported in PCa, which is worse with ADT and pain.
Medical Outcomes Survey (MOS) Sleep
Thomas et al. conducted a longitudinal study of patients with breast and PCa cancers undergoing radiation.50 They found a significant downward trend in the number of hours of sleep among men with PCa during treatment and follow-up.
Memorial Symptom Assessment Scale (MSAS)
Difficulty sleeping on the MSAS was reported by more than half of all patients with cancer (52.8% with PCa).51 Knapp et al. evaluated the trajectories of the six most prevalent symptoms reported by patients undergoing radiation therapy for PCa.52 Occurrence of sleep difficulties declined over time, as did severity and distress scales for sleep difficulties over time. In summary, these studies showed that although sleep disturbances are frequent in PCa, they declined over time in men undergoing radiation therapy.
Memorial Anxiety Scale for Prostate Cancer (MAX-PC)
Roth et al. developed the MAX-PC, which includes measures assessing sleep.53 Mehnert and colleagues administered the MAX-PC to patients at the beginning of an oncological rehabilitation program, finding that 32% of patients after prostatectomy reported that cancer-related distress affected sleep.54
Obstructive Sleep Apnea (OSA) Clinical Diagnoses
Gozal et al. conducted a nationwide study to examine the relationship between OSA diagnoses with risk and outcomes for various cancers.55 For PCa, they found no significant difference in the risk of metastasis and mortality between those with and without OSA. In summary, one study looking at clinical diagnoses of sleep apnea did not find an association with lethal PCa.
Pittsburgh Sleep Quality Index (PSQI)
Nine studies administered the PSQI. Among these studies, several administered the PSQI to evaluate change in sleep from pre to post-treatment. In a study examining the use of hypnotic therapy for patients with PCa suffering from hot flashes, Elkins and colleagues found PSQI improved from baseline to follow-up.56 Golshani and colleagues delivered mindfulness-based cognitive therapy to a single patient with PCa whose PSQI scores improved during the study.57 Also, McQuade et al. found, as part of their study to evaluate a tai chi/qi tong intervention during radiation therapy, that those in the intervention group slept longer than the control group.58 In a study of patients with PCa , Saini et al. found those undergoing ADT reported worse sleep quality as measured by the PSQI than those not undergoing ADT.59 In a similar study design, Koskderelioglu et al. found worse sleep quality as measured by the PSQI among those undergoing ADT compared to those not undergoing ADT.26 Hoyt and colleagues, examining patients undergoing radiation therapy or radical prostatectomy for localized PCa, found that worse sleep quality at study entry was predictive of higher levels of depressive symptoms post-treatment.60
On the other hand, several studies administered the PSQI in cross sectional study designs. For instance, Miaskowski et al. administered the PSQI to patients with PCa prior to undergoing radiation therapy, demonstrating that most patients demonstrated poor sleep quality.33 Penedo et al. compared sleep quality between patients from different race/ethnicities and found Hispanic men had the worst (highest) PSQI, followed by African American men, and non-Hispanic white.61 Humpel et al. compared sleep quality between patients with different types of cancer, finding patients with PCa reported fewer sleep disturbances than did patients with breast cancer.62 In summary, both observational and interventional studies suggest racial/ethnic differences in sleep quality among patients with PCa, worse sleep quality with hormonal therapy, and possible short-term improvements in sleep quality with behavioral interventions like mindfulness and tai chi/qi tong.
PROMIS Sleep Disturbance
Six studies administered the PROMIS Sleep Disturbance questionnaire. Quach et al. examined sleep in patients with PCa, finding that the PROMIS score averaged 50, indicating mild sleep disturbance.63 Similarly, among patients with localized PCa, Reeve and colleagues found evidence of mild sleep difficulties in their sample.64
Dickinson et al. examined sleep in patients with localized PCa scheduled for radiation therapy across several time points found sleep disturbance as measured by the PROMIS was highest post-treatment, then declined to their lowest point 12 months post-treatment (43.8).65
Lashbrook and colleague surveyed patients with different cancer diagnoses and found that patients with PCa reported the highest mean scores on the PROMIS sleep disturbance scale.66 On the other hand, Jensen et al. also surveyed patients with different cancer diagnoses and found scores on the PROMIS sleep disturbance survey among patients with PCa were slightly below other cancers.67
Feng et al. recruited patients with PCa following radiation therapy and found sleep disturbance as measured by the PROMIS was associated with lower urinary tract symptoms, pain, and depressive symptoms.68 In summary, multiple studies have examined sleep disturbance using PROMIS, demonstrating links between sleep with physical and mental quality of life.
Other Self-Reported Measures
A variety of self-reported sleep measures have been used in the PCa literature. Alban et al. examined self-reported sleep duration and awakenings in a single patient with PCa who received acupuncture after prostatectomy, finding that the treatment was associated with fewer awakenings.69 Kim et al. examined the efficacy of an informational intervention to ameliorate PCa treatment effects and found that the intervention group reported a fewer self-reported sleep problems than control.70 In a study evaluating an 8-week mindfulness-based stress reduction intervention, Carlson and colleagues found self-reported sleep quality among patients with PCa improved after the intervention.71 In a study examining patients using a compression device after radical prostatectomy, Cindolo and colleagues found 23% self-reported “bothersome insomnia” as a result of the device.72
Pacheco et al. assessed a number of changes among patients after receiving a PCa diagnosis and observed reports of difficulty sleeping, higher consumption of sleep medications, more sleep disruptions, and difficulty falling asleep.73 Msaouel et al. examined quality of life barriers among patients with PCa and found that inability to sleep was the fourth most challenging issue.74 Tewari et al. examined differences in discomfort while sleeping in patients with PCa using a catheter-less technique for radical prostatectomy, finding that this technique was associated with fewer reports of discomfort during sleep.75
LeMasters et al. examined sleep duration in a variety of cancer survivors and non-cancer controls, finding PCa survivors reported more inefficient sleep than non-cancer controls.76 Bill-Axelson et al. examined sleeping problems in men with localized PCa randomized to radical prostatectomy (RP) or watchful waiting and found that sleep problems were consistently reported by between 30 and 40% of men in both groups.77(p)
Challapalli et al. examined sleep disturbance in patients with PCa receiving ADT and found that 25% of patients reported sleep disturbance in some form.78
Jan et al. performed a population-based survey of Swedish men with clinically localized PCa managed with watchful waiting, radical prostatectomy or radiation therapy and found sleep problems were not associated with relapse, PCa, or non-PCa mortality, but were associated with increases in perceived stress.79 Greenberg et al. examined self-reported sleep duration in patients with PCa during radiation therapy. Patients slept the most during the final week of treatment.80 In summary, numerous interventional and observational studies used a heterogeneous grouping of other self-reported measures for sleep.
Symptom Related Daily Interference Scale (SRDIS)
De Valois et al. examined the effect of applying an ear acupuncture protocol among patients with PCa and observed a reduction in sleep-related daytime interference after treatment.81
Sleep Disturbance Index (SDI)
Gustaffson et al. (1995) examined sleep disturbance among men diagnosed with PCa on biopsy found SDI scores increased significantly 4 weeks after diagnosis, then decreased at 14 weeks.82
Surgical Outcomes Measurement System (SOMS)
Kundu et al. performed a prospective longitudinal assessment of patients with clinically localized or locally advanced PCa at baseline and post-treatment.83 For men treated with surgery, the mean score on the SOMS did not change over time, but for men who underwent active surveillance, the mean score on the SOMS worsened at 3 months.
You, Your Family, and the City of Hope are a Team
Zhou et al. conducted a cross-sectional survey of patients with various cancer types and assessed the extent to which sleep was a problem for these groups.84 Patients with PCa were least likely of all cancers to report severe sleep problems (4.3% reported sleep being a “severe” or “very severe” problem).
Qualitative Methods
Several studies utilized qualitative methods to examine sleep in patients with PCa. Flynn et al. used focus groups to discuss sleep issues contributing to sleep-wake functioning in patients with multiple cancers, including PCa. 85 Factors contributing to poor sleep included anxiety, as well as physical factors (e.g., hot flashes, restless legs, bowel control or urination). Consequences of poor sleep included daytime sleepiness/tiredness and fatigue. Prescription sleep aids were discussed for managing sleep problems.
Holmstrom et al. examined sleep using semi-structured interviews of patients with metastatic castration-resistant PCa (mCRPC) who were chemotherapy-naïve at a median of 4.8 years since the diagnosis of metastasis.86 Sleep problems were described as among the greatest impacts of mCRPC on health-related quality of life. Patients reported that sleep problems were not always related to thinking about the disease or pain, but also due to nocturia.
Grunfield et al. examined sleep quality and duration in patients with metastatic PCa undergoing ADT with focus groups.87 Participants reported having nocturia and hot flashes or night sweats that negatively impacted sleep quality and duration. Some participants reported behavioral responses (e.g., changing pillows and room temperature). The resultant fatigue contributes to tiredness and negative moods during the day. In summary, data from qualitative studies identified sleep problems as a significant barrier to quality of life and well-being among patients with PCa, with both urinary and hormonal symptoms as contributing factors.
STUDIES WITH CAREGIVERS (Table 2; N=3)
Studies Including Both Caregivers and Patients with Prostate Cancer
Robbins et al. reported an analysis of sleep-related posts to an online PCa community.88 Most posts were authored by patients (86%), with 16% from caregivers. The most common complaint was general trouble sleeping. Use of prescription sleep aids was reported in 22% of posts. Qualitative analysis revealed the presence of physical (e.g., hot flashes) and psychological (e.g., anxiety) barriers to sleep.
Studies with Caregivers Exclusively
General Sleep Disturbance Scale (GSDS)
Fletcher et al. recruited family caregivers of patients with PCa before radiation therapy, finding that more than one third of caregivers had high scores for sleep disturbance and that greater sleep disturbance was associated with reduced quality of life.89 In a subsequent study, Fletcher and colleagues (2009) reported on longitudinal assessments of caregivers, finding that sleep at baseline was a significant predictor of individual differences in the trajectory of fatigue.90 In summary, two studies of caregivers found that sleep disturbance was prevalent and associated with evening fatigue and quality of life.
Synopsis of Study Quality Ratings
In the case of studies that included patients with PCa, the average quality score was 30.6 (out of 36), ranging from 21 (Elkins)56 to 36 (McQuade).58 In caregiver studies, quality scores were on average 33.3, ranging from 26 (Robbins)88 to 33 (Fletcher).89
DATA INTERPRETATION AND EXPERT RECOMMENDATIONS
This systematic review confirms that PCa has a substantial impact on sleep health as measured by a diverse range of instruments. Sleep was a common problem faced by PCa survivors compared to other survivorship issues, although the proportion of patients reporting clinically significant disturbances varied widely across different populations and treatment types.
Other symptoms were linked with sleep difficulties in patients with PCa, including both physical (e.g., night sweats, urinary symptoms, pain) and psychological symptoms (e.g., cancer-related distress, depression, and anxiety). Some studies also suggested differences in sleep disturbance based on demographic factors, such as age and ethnicity.
A few studies compared sleep disturbances between patients with PCa and other cancers. In some studies, patients with PCa had a similar prevalence of sleep disturbance compared to other cancers; in others, patients with PCa had less subjective sleep disturbance compared to patients with other malignancies.
We identified scant literature on how to improve sleep health, specifically for patients with PCa. The limited available data suggest that interventions such as acupuncture, hypnotic therapy, mindfulness-based cognitive therapy, and educational information may provide short-term benefits. A systematic review by Teleni et al. of the effects of dietary and exercise interventions on quality of life in men with PCa undergoing ADT found no such interventions focused on improving sleep quality and insomnia.91 Overall, the evidence for interventions addressing sleep health specifically was limited, and additional studies are needed to specifically examine interventions to improve sleep health in the PCa population. This area of future research is particularly critical given the potential negative consequences of high rates of sleeping medications reported among PCa survivors. Moreover, evidence-based and effective sleep interventions in PCa may be a response to the call for innovative and personalized tools for PCa care.92
Many of the studies were observational or examined sleep as a secondary endpoint in a study designed to address a different issue. Some studies found changes in sleep health over time among men undergoing different types of treatment. For example, multiple studies of patients undergoing radiation therapy experienced a reduction in sleep disturbances over the course of treatment. By contrast, several studies found worse sleep health during ADT.
It is important to note that our focus was sleep and not fatigue, although this related parameter was addressed in some included studies. Cancer-related fatigue is defined by the National Comprehensive Cancer Network (NCCN) as a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning.93 Fatigue is rarely an isolated symptom and most often occurs with other symptoms such as pain, emotional distress, anemia and sleep disturbances. Fatigue should be systematically assessed, and the NCCN has a dedicated guideline on screening and management of cancer-related fatigue. It recommends evaluation for sleep disturbance as one of many important components in the assessment of potentially treatable contributory factors.
Sleep disturbances are specifically addressed in general cancer survivorship guidelines from the NCCN.93 They recommend that questions about sleep should be asked at regular intervals, especially when there is a change in clinical status or treatment. By contrast, the American Cancer Society Prostate Cancer Survivorship Guidelines do not specifically address sleep. Our results suggest that PCa and its treatment can have many different negative effects on sleep, and in fact, sleep disturbances are among the top concerns of patients with PCa. The relative lack of studies dedicated specifically to improving sleep in patients with PCa highlights an important gap for future research.
In addition, our systematic review identified only three studies that reported on sleep health among caregivers of patients with PCa.88-90 The limited available data suggest that sleep disturbances are common among caregivers, and that they are associated with fatigue and poor quality of life. Further research is needed to identify the barriers to sleep and interventions to improve sleep quality for caregivers.
Conclusion
Sleep health is an important component to PCa survivorship, which is closely linked to quality of life. Both patients and their caregivers report a variety of sleep disturbances, and hypnotic sleep medications are commonly used. More research is needed into behavioral options to improve sleep among patients with PCa and caregivers.
Supplementary Material
Funding:
This study was supported by the NYU Perlmutter Cancer Center Developmental Project Program, which is partially supported by the Cancer Center Support Grant P30CA016087.
ABBREVIATIONS
- ADT
Androgen deprivation therapy
- CPILS
Cancer Problems in Living Scale
- EORTC-QLQ
The European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire
- ESS
Epworth Sleepiness Scale
- FACT-P
Functional Assessment of Cancer Therapy Prostate
- FACT-G
Functional Assessment of Cancer Therapy General
- GSDS
General Sleep Disturbance Scale
- GSDS
General Sleep Disturbance Scale
- GAD-10
Generalized Anxiety Disorder-10
- IIS
Insomnia Interview Schedule
- ISI
Insomnia Severity Index
- RLS
International Restless Legs Syndrome Severity Scale
- MDASI
MD Anderson Symptom Inventory
- MOS
Medical Outcomes Survey Sleep
- MAX-PC
Memorial Anxiety Scale for Prostate Cancer
- MSAS
Memorial Symptom Assessment Scale
- OSA
Obstructive Sleep Apnea
- PSQI
Pittsburgh Sleep Quality Index
- PCa
Prostate Cancer
- SDI
Sleep Disturbance Index
- SOMS
Surgical Outcomes Measurement System
- SRDIS
Symptom Related Daily Interference Scale
Footnotes
Conflict of Interest: Dr. Robbins reports consulting fees from Denihan Hospitality Group LLC, Savoir Beds Ltd, Rituals Cosmetics BV, Sleep Cycle AB, Loóna Inc, Wave Meditation Inc, and With Deep LLC.
Contributor Information
Rebecca Robbins, Harvard Medical School, Boston, MA; Brigham & Women’s Hospital, Boston, MA.
Renee Hanna, Department of Urology, University of Michigan School of Medicine, Ann Arbor, MI.
Chidera Ejikeme, Harvard College, Cambridge, MA.
Stephanie L. Orstad, Division of General Internal Medicine and Clinical Innovation, Department of Medicine, NYU Grossman School of Medicine, New York, NY.
Sima Porten, Department of Urology, University of California, San Francisco.
Carolyn A. Salter, Madigan Army Medical Center.
Tatiana Sanchez-Nolasco, Department of Urology and Population Health, NYU School of Medicine, New York, NY.
Dorice Vieira, NYU Grossman School of Medicine, New York, NY; Department of Population Health, NYU School of Medicine, New York, NY.
Stacy Loeb, Departments of Urology and Population Health, NYU School of Medicine and Manhattan Veterans Affairs, New York, NY.
References
- 1.Centers for Disease Control and Prevention. Short Sleep Duration Among US Adults.; 2017. Accessed February 28, 2021. https://www.cdc.gov/sleep/data_statistics.html
- 2.Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. The Lancet Respiratory Medicine. 2019;7(8):687–698. doi: 10.1016/S2213-2600(19)30198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou J, Xia S, Li T, Liu R. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020;24(4):1293–1298. doi: 10.1007/s11325-019-01981-6 [DOI] [PubMed] [Google Scholar]
- 4.Kellesarian SV, Malignaggi VR, Feng C, Javed F. Association between obstructive sleep apnea and erectile dysfunction: a systematic review and meta-analysis. Int J Impot Res. 2018;30(3):129–140. doi: 10.1038/s41443-018-0017-7 [DOI] [PubMed] [Google Scholar]
- 5.Liu R, Wu S, Zhang B, Guo M, Zhang Y. The association between sleep duration and prostate cancer: A systematic review and meta-analysis. Medicine (Baltimore). 2020;99(28):e21180. doi: 10.1097/MD.0000000000021180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stone CR, Haig TR, Fiest KM, McNeil J, Brenner DR, Friedenreich CM. The association between sleep duration and cancer-specific mortality: a systematic review and meta-analysis. Cancer Causes Control. 2019;30(5):501–525. doi: 10.1007/s10552-019-01156-4 [DOI] [PubMed] [Google Scholar]
- 7.Deng N, Haney NM, Kohn TP, Pastuszak AW, Lipshultz LI. The Effect of Shift Work on Urogenital Disease: a Systematic Review. Curr Urol Rep. 2018;19(8):57. doi: 10.1007/s11934-018-0815-y [DOI] [PubMed] [Google Scholar]
- 8.Liu L, Ancoli-Israel S. Sleep Disturbances in Cancer. Psychiatr Ann. 2008;38(9):627–634. doi: 10.3928/00485713-20080901-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1060. doi: 10.1001/jama.2014.304 [DOI] [PubMed] [Google Scholar]
- 10.Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res. 2002;12(9):1284–1299. doi: 10.1177/1049732302238251 [DOI] [PubMed] [Google Scholar]
- 11.Hanisch LJ, Gooneratne NS, Soin K, Gehrman PR, Vaughn DJ, Coyne JC. Sleep and daily functioning during androgen deprivation therapy for prostate cancer. European Journal of Cancer Care. 2011;20(4):549–554. doi: 10.1111/j.1365-2354.2010.01226.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holliday EB, Dieckmann NF, McDonald TL, Hung AY, Thomas CR, Wood LJ. Relationship between fatigue, sleep quality and inflammatory cytokines during external beam radiation therapy for prostate cancer: A prospective study. Radiother Oncol. 2016;118(1):105–111. doi: 10.1016/j.radonc.2015.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navarro-Martinez R, Serrano-Carrascosa M, Buigues C, et al. Frailty syndrome is associated with changes in peripheral inflammatory markers in prostate cancer patients undergoing androgen deprivation therapy. Urol Oncol. 2019;37(12):976–987. doi: 10.1016/j.urolonc.2019.08.005 [DOI] [PubMed] [Google Scholar]
- 14.Khan L, Uy C, Nguyen J, et al. Self-reported rates of sleep disturbance in patients with symptomatic bone metastases attending an outpatient radiotherapy clinic. J Palliat Med. 2011;14(6):708–714. doi: 10.1089/jpm.2010.0491 [DOI] [PubMed] [Google Scholar]
- 15.Baker F, Denniston M, Zabora JR, Marcellus D. Cancer Problems in Living and Quality of Life After Bone Marrow Transplantation. Journal of Clinical Psychology in Medical Settings. 2003;10(1):27–34. doi: 10.1023/A:1022801713046 [DOI] [PubMed] [Google Scholar]
- 16.Yennurajalingam S, Atkinson B, Masterson J, et al. The impact of an outpatient palliative care consultation on symptom burden in advanced prostate cancer patients. J Palliat Med. 2012;15(1):20–24. doi: 10.1089/jpm.2011.0219 [DOI] [PubMed] [Google Scholar]
- 17.Zenger M, Lehmann-Laue A, Stolzenburg JU, Schwalenberg T, Ried A, Hinz A. The relationship of quality of life and distress in prostate cancer patients compared to the general population. Psychosoc Med. 2010;7:Doc02. doi: 10.3205/psm000064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jonler M, Nielsen OS, Groenvold M, et al. Quality of life in patients with skeletal metastases of prostate cancer and status prior to start of endocrine therapy: results from the Scandinavian Prostate Cancer Group Study 5. Scand J Urol Nephrol. 2005;39(1):42–48. doi: 10.1080/00365590410002528 [DOI] [PubMed] [Google Scholar]
- 19.Lintz K, Moynihan C, Steginga S, et al. Prostate cancer patients’ support and psychological care needs: Survey from a non-surgical oncology clinic. Psychooncology. 2003;12(8):769–783. doi: 10.1002/pon.702 [DOI] [PubMed] [Google Scholar]
- 20.Collette L, van Andel G, Bottomley A, et al. Is baseline quality of life useful for predicting survival with hormone-refractory prostate cancer? A pooled analysis of three studies of the European Organisation for Research and Treatment of Cancer Genitourinary Group. J Clin Oncol. 2004;22(19):3877–3885. doi: 10.1200/jco.2004.07.089 [DOI] [PubMed] [Google Scholar]
- 21.Jasinska M, Tracz M, Kurczewska U, Orszulak-Michalak D. Assessment of change of quality of life in hospitalized terminally ill cancer patients. Wspolczesna Onkologia. 2010;14(5):333–339. [Google Scholar]
- 22.Mols F, Stijns P, Dankaart B, Houterman S, Vingerhoets A, Hendrikx A. Health-related quality of life in I-125 prostate brachytherapy patients treated with and without volume-reducing hormone therapy: results of a short-term prospective study. J Endourol. 2009;23(1):153–159. doi: 10.1089/end.2008.0089 [DOI] [PubMed] [Google Scholar]
- 23.van Andel G, Fernandez de Moral P, Caris CT, et al. A randomized study comparing epirubicin in a 4-weekly versus a weekly intravenous regimen in patients with metastatic, hormone resistant, prostatic carcinoma: effects on health related quality of life. World J Urol. 2003;21(3):177–182. doi: 10.1007/s00345-003-0342-3 [DOI] [PubMed] [Google Scholar]
- 24.Vordermark D, Wulf J, Markert K, et al. 3-D conformal treatment of prostate cancer to 74 Gy vs. high-dose-rate brachytherapy boost: a cross-sectional quality-of-life survey. Acta Oncol. 2006;45(6):708–716. doi: 10.1080/02841860600710913 [DOI] [PubMed] [Google Scholar]
- 25.Roeloffzen EM, Lips IM, van Gellekom MP, et al. Health-related quality of life up to six years after (125)I brachytherapy for early-stage prostate cancer. Int J Radiat Oncol Biol Phys. 2010;76(4):1054–1060. doi: 10.1016/j.ijrobp.2009.03.045 [DOI] [PubMed] [Google Scholar]
- 26.Koskderelioglu A, Gedizlioglu M, Ceylan Y, Gunlusoy B, Kahyaoglu N. Quality of sleep in patients receiving androgen deprivation therapy for prostate cancer. Neurol Sci. 2017;38(8):1445–1451. doi: 10.1007/s10072-017-2989-3 [DOI] [PubMed] [Google Scholar]
- 27.Monga U, Kerrigan AJ, Thornby J, Monga TN. Prospective study of fatigue in localized prostate cancer patients undergoing radiotherapy. Radiat Oncol Investig. 1999;7(3):178–185. doi: [DOI] [PubMed] [Google Scholar]
- 28.Sharma P, Wisniewski A, Braga-Basaria M, et al. Lack of an effect of high dose isoflavones in men with prostate cancer undergoing androgen deprivation therapy. J Urol. 2009;182(5):2265–2272. doi: 10.1016/j.juro.2009.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jefford M, Ward AC, Lisy K, et al. Patient-reported outcomes in cancer survivors: a population-wide cross-sectional study. Support Care Cancer. 2017;25(10):3171–3179. doi: 10.1007/s00520-017-3725-5 [DOI] [PubMed] [Google Scholar]
- 30.Ukoli FA, Lynch BS, Adams-Campbell LL. Radical prostatectomy and quality of life among African Americans. Ethn Dis. 2006;16(4):988–993. [PubMed] [Google Scholar]
- 31.Stephens RJ, Dearnaley DP, Cowan R, Sydes M, Naylor S, Fallowfield L. The quality of life of men with locally advanced prostate cancer during neoadjuvant hormone therapy: data from the Medical Research Council RT01 trial (ISRCTN 47772397). BJU Int. 2007;99(2):301–310. doi: 10.1111/j.1464-410X.2006.06560.x [DOI] [PubMed] [Google Scholar]
- 32.Rich T, Porter GW II, Ricks-Santi L, Milshtein T, Corbin T. Intermittent 96-Hour Auricular Electroacupuncture for Hot Flashes in Patients with Prostate Cancer: A Pilot Study. Medical Acupuncture. 2017;29(5):313–321. doi: 10.1089/acu.2017.1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miaskowski C, Paul SM, Cooper BA, et al. Predictors of the trajectories of self-reported sleep disturbance in men with prostate cancer during and following radiation therapy. Sleep. 2011;34(2):171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Merriman JD, Dodd M, Lee K, et al. Differences in self-reported attentional fatigue between patients with breast and prostate cancer at the initiation of radiation therapy. Cancer Nurs. 2011;34(5):345–353. doi: 10.1097/NCC.0b013e318202520a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharpley CF, Bitsika V, Wootten AC, Christie DRH. Differences in major depressive disorder and generalised anxiety disorder symptomatology between prostate cancer patients receiving hormone therapy and those who are not. Psychooncology. 2014;23(12):1350–1355. doi: 10.1002/pon.3566 [DOI] [PubMed] [Google Scholar]
- 36.Savard J, Simard S, Hervouet S, Ivers H, Lacombe L, Fradet Y. Insomnia in men treated with radical prostatectomy for prostate cancer. Psychooncology. 2005;14(2):147–156. doi: 10.1002/pon.830 [DOI] [PubMed] [Google Scholar]
- 37.Dirksen SR, Epstein DR, Hoyt MA. Insomnia, depression, and distress among outpatients with prostate cancer. Appl Nurs Res. 2009;22(3):154–158. doi: 10.1016/j.apnr.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 38.Dirksen SR, Kirschner KF, Belyea MJ. Association of symptoms and cytokines in prostate cancer patients receiving radiation treatment. Biol Res Nurs. 2014;16(3):250–257. doi: 10.1177/1099800413490228 [DOI] [PubMed] [Google Scholar]
- 39.Dirksen SR, Belyea MJ, Wong W, Epstein DR. Transitions in Symptom Cluster Subgroups Among Men Undergoing Prostate Cancer Radiation Therapy. Cancer Nurs. 2016;39(1):3–11. doi: 10.1097/ncc.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fillion L, Gelinas C, Simard S, Savard J, Gagnon P. Validation evidence for the French Canadian adaptation of the Multidimensional Fatigue Inventory as a measure of cancer-related fatigue. Cancer Nurs. 2003;26(2):143–154. doi: 10.1097/00002820-200304000-00008 [DOI] [PubMed] [Google Scholar]
- 41.Cessna JM, Jim HS, Sutton SK, et al. Evaluation of the psychometric properties of the PROMIS Cancer Fatigue Short Form with cancer patients. J Psychosom Res. 2016;81:9–13. doi: 10.1016/j.jpsychores.2015.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hervouet S, Savard J, Simard S, et al. Psychological functioning associated with prostate cancer: cross-sectional comparison of patients treated with radiotherapy, brachytherapy, or surgery. J Pain Symptom Manage. 2005;30(5):474–484. doi: 10.1016/j.jpainsymman.2005.05.011 [DOI] [PubMed] [Google Scholar]
- 43.Trudel-Fitzgerald C, Savard J, Ivers H. Evolution of Cancer-Related Symptoms Over an 18-Month Period. J Pain Symptom Manage. 2013;45(6):1007–1018. doi: 10.1016/j.jpainsymman.2012.06.009 [DOI] [PubMed] [Google Scholar]
- 44.Savard J, Villa J, Ivers H, Simard S, Morin CM. Prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. J Clin Oncol. 2009;27(31):5233–5239. doi: 10.1200/JCO.2008.21.6333 [DOI] [PubMed] [Google Scholar]
- 45.Savard J, Hervouet S, Ivers H. Prostate cancer treatments and their side effects are associated with increased insomnia. Psychooncology. 2013;22(6):1381–1388. doi: 10.1002/pon.3150 [DOI] [PubMed] [Google Scholar]
- 46.Desax MC, Hundsberger T, Rothermundt C, Omlin A, Gillessen S. Restless Legs Syndrome-An Emerging Potential Side Effect of Enzalutamide: Report of 2 Cases. Clin Genitourin Cancer. 2015;13(5):E385–E386. doi: 10.1016/j.clgc.2015.04.007 [DOI] [PubMed] [Google Scholar]
- 47.Basch E, Autio KA, Smith MR, et al. Effects of cabozantinib on pain and narcotic use in patients with castration-resistant prostate cancer: results from a phase 2 nonrandomized expansion cohort. Eur Urol. 2015;67(2):310–318. doi: 10.1016/j.eururo.2014.02.013 [DOI] [PubMed] [Google Scholar]
- 48.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 49.Gonzalez VJ, McMillan SC, Groer M, Imbert S, Pedro E, Tome J. Symptom Burden: Experiences of Puerto Rican Men With Prostate Cancer Prior to External Beam Radiation Therapy. Clin J Oncol Nurs. 2017;21(1):104–112. doi: 10.1188/17.CJON.104-112 [DOI] [PubMed] [Google Scholar]
- 50.Thomas KS, Bower J, Hoyt MA, Sepah S. Disrupted sleep in breast and prostate cancer patients undergoing radiation therapy: the role of coping processes. Psychooncology. 2010;19(7):767–776. doi: 10.1002/pon.1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Portenoy RK, Thaler HT, Kornblith AB, et al. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994;30A(9):1326–1336. doi: 10.1016/0959-8049(94)90182-1 [DOI] [PubMed] [Google Scholar]
- 52.Knapp K, Cooper B, Koetters T, et al. Trajectories and Predictors of Symptom Occurrence, Severity, and Distress in Prostate Cancer Patients Undergoing Radiation Therapy. J Pain Symptom Manage. 2012;44(4):486–507. doi: 10.1016/j.jpainsymman.2011.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roth AJ, Rosenfeld B, Kornblith AB, et al. The memorial anxiety scale for prostate cancer: validation of a new scale to measure anxiety in men with with prostate cancer. Cancer. 2003;97(11):2910–2918. doi: 10.1002/cncr.11386 [DOI] [PubMed] [Google Scholar]
- 54.Mehnert A, Lehmann C, Schulte T, Koch U. Presence of symptom distress and prostate cancer-related anxiety in patients at the beginning of cancer rehabilitation. Onkologie. 2007;30(11):551–556. doi: 10.1159/000108578 [DOI] [PubMed] [Google Scholar]
- 55.Gozal D, Ham SA, Mokhlesi B. Sleep Apnea and Cancer: Analysis of a Nationwide Population Sample. Sleep. 2016;39(8):1493–1500. doi: 10.5665/sleep.6004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elkins GR, Kendrick C, Koep L. Hypnotic relaxation therapy for treatment of hot flashes following prostate cancer surgery: a case study. Int J Clin Exp Hypn. 2014;62(3):251–259. doi: 10.1080/00207144.2014.901051 [DOI] [PubMed] [Google Scholar]
- 57.Golshani G, Pirnia B. Comparison of mindfulness-based cognitive therapy (MBCT) with acceptance and commitment therapy (ACT) on the severity of fatigue, improvement of sleep quality and resilience in a patient with prostate cancer: A single-case experimental study. International Journal of Cancer Management. 2019;12(2). [Google Scholar]
- 58.McQuade JL, Prinsloo S, Chang DZ, et al. Qigong/tai chi for sleep and fatigue in prostate cancer patients undergoing radiotherapy: a randomized controlled trial. Psychooncology. 2017;26(11):1936–1943. doi: 10.1002/pon.4256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saini A, Berruti A, Cracco C, et al. Psychological distress in men with prostate cancer receiving adjuvant androgen-deprivation therapy. Urologic Oncology: Seminars and Original Investigations. 2013;31(3):352–358. doi: 10.1016/j.urolonc.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 60.Hoyt MA, Bower JE, Irwin MR, Weierich MR, Stanton AL. Sleep quality and depressive symptoms after prostate cancer: The mechanistic role of cortisol. Behav Neurosci. 2016;130(3):351–356. doi: 10.1037/bne0000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Penedo FJ, Dahn JR, Shen BJ, Schneiderman N, Antoni MH. Ethnicity and determinants of quality of life after prostate cancer treatment. Urology. 2006;67(5):1022–1027. doi: 10.1016/j.urology.2005.11.019 [DOI] [PubMed] [Google Scholar]
- 62.Humpel N, Iverson DC. Sleep quality, fatigue and physical activity following a cancer diagnosis. Eur J Cancer Care (Engl). 2010;19(6):761–768. doi: 10.1111/j.1365-2354.2009.01126.x [DOI] [PubMed] [Google Scholar]
- 63.Quach CW, Langer MM, Chen RC, et al. Reliability and validity of PROMIS measures administered by telephone interview in a longitudinal localized prostate cancer study. Qual Life Res. 2016;25(11):2811–2823. doi: 10.1007/s11136-016-1325-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reeve BB, Tan X, Chen RC, Usinger DS, Pinheiro LC. Symptom and function profiles of men with localized prostate cancer. Cancer. 2018;124(13):2832–2840. doi: 10.1002/cncr.31401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dickinson K, Kupzyk K, Saligan L. Evaluating Dimensions of Fatigue in Men With Prostate Cancer Receiving Radiation Therapy. Cancer Nurs. Published online December 28, 2019. doi: 10.1097/ncc.0000000000000782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lashbrook M, Bernardes CM, Kirshbaum MN, Valery PC. Physical functioning and psychological morbidity among regional and rural cancer survivors: A report from a regional cancer centre. Aust J Rural Health. 2018;26(3):211–219. doi: 10.1111/ajr.12419 [DOI] [PubMed] [Google Scholar]
- 67.Jensen RE, Potosky AL, Moinpour CM, et al. United States Population-Based Estimates of Patient-Reported Outcomes Measurement Information System Symptom and Functional Status Reference Values for Individuals With Cancer. J Clin Oncol. 2017;35(17):1913–1920. doi: 10.1200/JCO.2016.71.4410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Feng LR, Fuss T, Dickinson K, Ross A, Saligan LN. Co-Occurring Symptoms Contribute to Persistent Fatigue in Prostate Cancer. Oncology. 2019;96(4):183–191. doi: 10.1159/000494620 [DOI] [PubMed] [Google Scholar]
- 69.Alban J. Acupuncture treatment of frequent urination and nocturia postprostatectomy. Medical Acupuncture. 2008;20(2):119–121. [Google Scholar]
- 70.Kim Y, Roscoe J, Morrow G. The effects of information and negative affect on severity of side effects from radiation therapy for prostate cancer. Supportive Care in Cancer. 2002;10(5):416–421. doi: 10.1007/s00520-002-0359-y [DOI] [PubMed] [Google Scholar]
- 71.Carlson L, Speca M, Patel K, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29(4):448–474. doi: 10.1016/S0306-4530(03)00054-4 [DOI] [PubMed] [Google Scholar]
- 72.Cindolo L, Salzano L, Mirone V, et al. Thromboprophylaxis in Radical Retropubic Prostatectomy: Efficacy and Patient Compliance of a Dual Modality. Urol Int. 2009;83(1):12–18. doi: 10.1159/000224861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pacheco SO, Pacheco FJ, Zapata GM, et al. Food Habits, Lifestyle Factors, and Risk of Prostate Cancer in Central Argentina: A Case Control Study Involving Self-Motivated Health Behavior Modifications after Diagnosis. Nutrients. 2016;8(7). doi: 10.3390/nu8070419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Msaouel P, Gralla RJ, Jones RA, Hollen PJ. Key issues affecting quality of life and patient-reported outcomes in prostate cancer: an analysis conducted in 2128 patients with initial psychometric assessment of the prostate cancer symptom scale (PCSS). BMJ Support Palliat Care. 2017;7(3):308–315. doi: 10.1136/bmjspcare-2016-001146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tewari A, Rao S, Mandhani A. Catheter-less robotic radical prostatectomy using a custom-made synchronous anastomotic splint and vesical urinary diversion device: report of the initial series and perioperative outcomes. BJU Int. 2008;102(8):1000–1004. doi: 10.1111/j.1464-410X.2008.07875.x [DOI] [PubMed] [Google Scholar]
- 76.LeMasters T, Madhavan S, Sambamoorthi U, Kurian S. A population-based study comparing HRQoL among breast, prostate, and colorectal cancer survivors to propensity score matched controls, by cancer type, and gender. Psychooncology. 2013;22(10):2270–2282. doi: 10.1002/pon.3288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bill-Axelson A, Garmo H, Holmberg L, et al. Long-term distress after radical prostatectomy versus watchful waiting in prostate cancer: a longitudinal study from the Scandinavian Prostate Cancer Group-4 randomized clinical trial. Eur Urol. 2013;64(6):920–928. doi: 10.1016/j.eururo.2013.02.025 [DOI] [PubMed] [Google Scholar]
- 78.Challapalli A, Edwards SM, Abel P, Mangar SA. Evaluating the prevalence and predictive factors of vasomotor and psychological symptoms in prostate cancer patients receiving hormonal therapy: Results from a single institution experience. Clin Transl Radiat Oncol. 2018;10:29–35. doi: 10.1016/j.ctro.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jan M, Bonn SE, Sjölander A, et al. The roles of stress and social support in prostate cancer mortality. Scandinavian Journal of Urology. 2016;50(1):47–55. doi: 10.3109/21681805.2015.1079796 [DOI] [PubMed] [Google Scholar]
- 80.Greenberg DB, Gray JL, Mannix CM, Eisenthal S, Carey M. Treatment-related fatigue and serum interleukin-1 levels in patients during external beam irradiation for prostate cancer. J Pain Symptom Manage. 1993;8(4):196–200. doi: 10.1016/0885-3924(93)90127-h [DOI] [PubMed] [Google Scholar]
- 81.De Valois B, Young TE, Thorpe P, Preston J, Degun T. Improving well-being of prostate cancer survivors using the NADA acupuncture protocol: A clinical outcome study. Medical Acupuncture. 2015;27(3):194–205. [Google Scholar]
- 82.Gustafsson O, Theorell T, Norming U, Perski A, Ohstrom M, Nyman CR. Psychological reactions in men screened for prostate cancer. Br J Urol. 1995;75(5):631–636. doi: 10.1111/j.1464-410x.1995.tb07422.x [DOI] [PubMed] [Google Scholar]
- 83.Kundu SD, Victorson D, DeLancey JO, et al. Psychosocial factors and treatment satisfaction after radical prostatectomy. Journal of Community and Supportive Oncology. 2018;16(3):e130–e137. [Google Scholar]
- 84.Zhou ES, Clark K, Recklitis CJ, Obenchain R, Loscalzo M. Sleepless from the Get Go: Sleep Problems Prior to Initiating Cancer Treatment. Int J Behav Med. 2018;25(5):502–516. doi: 10.1007/s12529-018-9715-2 [DOI] [PubMed] [Google Scholar]
- 85.Flynn KE, Shelby RA, Mitchell SA, et al. Sleep-wake functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS((R))). Psychooncology. 2010;19(10):1086–1093. doi: 10.1002/pon.1664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Holmstrom S, Naidoo S, Turnbull J, Hawryluk E, Paty J, Morlock R. Symptoms and Impacts in Metastatic Castration-Resistant Prostate Cancer: Qualitative Findings from Patient and Physician Interviews. Patient. 2019;12(1):57–67. doi: 10.1007/s40271-018-0349-x [DOI] [PubMed] [Google Scholar]
- 87.Grunfeld EA, Halliday A, Martin P, Drudge-Coates L. Andropause Syndrome in Men Treated for Metastatic Prostate Cancer: A Qualitative Study of the Impact of Symptoms. Cancer Nursing. 2012;35(1):63. doi: 10.1097/NCC.0b013e318211fa92 [DOI] [PubMed] [Google Scholar]
- 88.Robbins R, Jean-Louis G, Chanko N, Combs P, Byrne N, Loeb S. Using data from an online health community to examine the impact of prostate cancer on sleep. BJU Int. 2020;125(5):34–635. doi: 10.1111/bju.14986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fletcher BS, Paul SM, Dodd MJ, et al. Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. J Clin Oncol. 2008;26(4):599–605. doi: 10.1200/jco.2007.12.2838 [DOI] [PubMed] [Google Scholar]
- 90.Fletcher BAS, Schumacher KL, Dodd M, et al. Trajectories of fatigue in family caregivers of patients undergoing radiation therapy for prostate cancer. Res Nurs Health. 2009;32(2):125–139. doi: 10.1002/nur.20312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Teleni L, Chan RJ, Chan A, et al. Exercise improves quality of life in androgen deprivation therapy-treated prostate cancer: systematic review of randomised controlled trials. Endocr Relat Cancer. 2016;23(2):101–112. doi: 10.1530/ERC-15-0456 [DOI] [PubMed] [Google Scholar]
- 92.Kucera R, Pecen L, Topolcan O, et al. Prostate cancer management: long-term beliefs, epidemic developments in the early twenty-first century and 3PM dimensional solutions. EPMA J. 2020;11(3):399–418. doi: 10.1007/s13167-020-00214-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.National Comprehensive Cancer Network. Accessed February 28, 2021. https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf
- 94.Baker F, Denniston M, Smith T, West MM. Adult cancer survivors: how are they faring? Cancer. 2005;104(11 Suppl):2565–2576. doi: 10.1002/cncr.21488 [DOI] [PubMed] [Google Scholar]
- 95.Yennurajalingam S, Atkinson B, Masterson J, et al. The Impact of an Outpatient Palliative Care Consultation on Symptom Burden in Advanced Prostate Cancer Patients. JOURNAL OF PALLIATIVE MEDICINE. 2012;15(1):20–24. doi: 10.1089/jpm.2011.0219 [DOI] [PubMed] [Google Scholar]
- 96.Lintz K, Moynihan C, Steginga S, et al. Prostate cancer patients’ support and psychological care needs: Survey from a non-surgical oncology clinic. PSYCHO-ONCOLOGY. 2003;12(8):769–783. doi: 10.1002/pon.702 [DOI] [PubMed] [Google Scholar]
- 97.Sullivan PW, Mulani PM, Fishman M, Sleep D. Quality of life findings from a multicenter, multinational, observational study of patients with metastatic hormone-refractory prostate cancer. Qual Life Res. 2007;16(4):571–575. doi: 10.1007/s11136-006-9156-2 [DOI] [PubMed] [Google Scholar]
- 98.Jefford M, Ward AC, Lisy K, et al. Patient-reported outcomes in cancer survivors: a population-wide cross-sectional study. SUPPORTIVE CARE IN CANCER. 2017;25(10):3171–3179. doi: 10.1007/s00520-017-3725-5 [DOI] [PubMed] [Google Scholar]
- 99.Savard J, Ivers H, Savard MH, Morin CM. Cancer treatments and their side effects are associated with aggravation of insomnia: Results of a longitudinal study. Cancer. 2015;121(10):1703–1711. doi: 10.1002/cncr.29244 [DOI] [PubMed] [Google Scholar]
- 100.Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM. Natural Course of Insomnia Comorbid With Cancer: An 18-Month Longitudinal Study. JOURNAL OF CLINICAL ONCOLOGY. 2011;29(26):3580–3586. doi: 10.1200/JCO.2010.33.2247 [DOI] [PubMed] [Google Scholar]
- 101.Basch E, Autio KA, Smith MR, et al. Effects of Cabozantinib on Pain and Narcotic Use in Patients with Castration-resistant Prostate Cancer: Results from a Phase 2 Nonrandomized Expansion Cohort. EUROPEAN UROLOGY. 2015;67(2):310–318. doi: 10.1016/j.eururo.2014.02.013 [DOI] [PubMed] [Google Scholar]
- 102.Cleeland CS, Zhao F, Chang VT, et al. The symptom burden of cancer: Evidence for a core set of cancer-related and treatment-related symptoms from the Eastern Cooperative Oncology Group Symptom Outcomes and Practice Patterns study. Cancer. 2013;119(24):4333–4340. doi: 10.1002/cncr.28376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Penedo F, Dahn J, Shen B, Schneiderman N, Antoni M. Ethnicity and determinants of quality of life after prostate cancer treatment. Urology. 2006;67(5):1022–1027. doi: 10.1016/j.urology.2005.11.019 [DOI] [PubMed] [Google Scholar]
- 104.Flynn KE, Shelby RA, Mitchell SA, et al. Sleep-wake functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS (R)). PSYCHO-ONCOLOGY. 2010;19(10):1086–1093. doi: 10.1002/pon.1664 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.