Abstract
Objective
The financial effects of the coronavirus disease 2019 (COVID-19) pandemic have fundamentally changed the healthcare environment, with hospitals expected to have lost billions in 2021. A preexisting nationwide nursing shortage became drastically worse during the pandemic amid dramatically increasing labor costs. We examined the evolution and financial effects of these changes during repeated pandemic surges within a vascular surgery division at a tertiary medical center.
Methods
Operating room, inpatient unit, and outpatient clinic financial data were examined retrospectively. The monthly averages for a 14-month control cohort before COVID-19 (January 2019 to February 2020) were compared to the averages for seven interval groups of sequential, 3-month cohorts from March 2020 through November 2021 (groups 1-7).
Results
The monthly relative value unit (RVU) generation had returned to the mean before the COVID-19 pandemic (2520 RVUs) after an isolated decrease early in the pandemic (group 1; 1734 RVUs). The RVUs ranged from 2540 to 2863 per month for groups 2 to 5, with a slight decline in groups 6 and 7. The average monthly RVUs in the COVID-19 period (2437 RVUs) were nearly equivalent (P = .93) to those for the pre–COVID-19 cohort. An analysis of payor mix demonstrated an increase in commercial and Medicaid payors, with a respective decrease in Medicare payors, during COVID-19. The contribution to indirect, or profit, from inpatient hospital and outpatient clinical revenue showed a drastic decrease in group 1, followed by a swift rebound when the government restrictions were eased (group 2). The total monthly vascular nursing unit expense demonstrated a marked increase with each sequential group during COVID-19, with an average monthly upsurge of +$82,171 (+47%; P < .001). An increase in the nursing labor expenses of +$884 per vascular case (from $1630 to $2514; +54%; P < .001) was observed in the COVID-19 era. The nursing labor costs per patient day had increased from $580 to $852 (+$272; +53%; P < .001). The nursing labor cost per RVU had increased from $69.5 to $107.7 (+$38.2; +55%; P < .001). On a system-wide level, the agency-related nursing costs had increased from $4.9 million to $13.6 million per month (+178%; P < .001) in 2021 compared with 2020.
Conclusions
The COVID-19 pandemic has had severe, nationwide effects on healthcare delivery, exacerbating the deleterious effects of an existing, critical nursing shortage. To the best of our knowledge, the present study is the first detailed analysis of this phenomenon and its effects on a surgical division. Our results have demonstrated a progressive, drastic increase in nursing labor costs during the pandemic, with a resultant sustained erosion of financial margins despite a level of clinical productivity, as measured in RVUs, equal to the prepandemic standards. This precarious trend is not sustainable and will require increased, targeted government funding.
Keywords: Cost, COVID-19, Margin, Medicare, Nursing labor, Pandemic, Profit
Article Highlights.
-
•
Type of Research: A single-center, retrospective, observational study
-
•
Key Findings: During the first 21 months of the pandemic, our nursing labor costs had increased ≤67% each month (P < .001) with a resultant, progressive decline in the department financial margin of ≤50% (P < .001).
-
•
Take Home Message: Nursing workforce shortages have led to skyrocketing hospital labor costs and decreased vascular surgery financial margins during the pandemic.
The coronavirus disease 2019 (COVID-19) pandemic, with >80 million total cases and >975,000 deaths in the United States, has fundamentally and permanently changed the national healthcare landscape. America’s hospitals face significant, ongoing financial instability as the pandemic continues to evolve. With cases and hospitalizations at high levels owing to the rapid spread of the Delta variant and the abrupt advent of the Omicron variant, the community of U.S. physicians, nurses, and other hospital personnel has been strained and pushed beyond the existing structural capacity to deliver reliable care. At the same time, hospitals have been experiencing profound net income losses that likely will continue through 2022.
The financial challenges present before the pandemic have been grossly exposed and augmented during the past 2 years. Before 2020, about one quarter of hospitals were operating with negative margins. However, by the beginning of 2021, after almost 1 year of COVID-19, more than one half of U.S. hospitals had reported negative margins.1 According to the American Hospital Association, hospitals nationwide will have lost an estimated $54 billion in net income during 2021, even after the distribution of $176 billion in federal Coronavirus Aid, Relief, and Economic Security (CARES) Act funding from 2020.2 The uncertain trajectory of the continuing Delta and Omicron variants, and the possible emergence of new variants in the United States, will likely exacerbate these trends, further straining American healthcare infrastructure. In New Orleans, a severe Delta surge in December 2021 and January 2022 led to recurrent limits on some elective cases because of nursing staff COVID-19 infections, compounding the existing shortages in available nursing labor that have continued through to the present day.
In addition, additional hospital staffing costs were not addressed as a part of the CARES Act, and reports from across the United States have been emerging with increasing frequency regarding the desperate shortages experienced by small, rural hospitals and the largest healthcare systems alike.3 In particular, the longstanding shortage of qualified nurses in the United States has intensified to critical and untenable levels. In September 2021, the American Nurses Association urged the U.S. Department of Health and Human Services (HHS) to declare the nurse staffing shortage a national crisis. In a public letter to the HHS, the American Nurses Association called for the current administration to acknowledge this emergency and to take concrete and aggressive action to address a “crisis-level nurse staffing shortage that puts nurses’ ability to care for patients in jeopardy.”4
Despite the seemingly ubiquitous and severe effects of the nursing shortage, a paucity of reports has investigated the tangible effects of this crisis on the economic stability of individual hospitals. Also, to the best of our knowledge, no studies have detailed the effects of the increased labor costs on surgical department financial margins. We examined, not only the overall effects of the pandemic on the fiscal health of an academic vascular surgery division, but also the effects of increasing labor costs on departmental margins.
Methods
The operating room, inpatient unit, and outpatient clinic financial data were examined retrospectively. The monthly averages from a 14-month control cohort before COVID-19 (January 2019 to February 2020) were compared to the averages for seven interval groups of sequential, 3-month cohorts from March 2020 through November 2021 (groups 1-7). The fiscal effect was analyzed from real revenue and cost data derived from actual hospital accounting records, not Medicare estimates or hospital administration projections. The calculation of nursing expenses, including salaries and benefits, used a cost accounting method, similar to a cost to charge model, but using actual data, not estimates or projections, specific to each unit. Operating room expenses were analyzed similarly but were based more heavily on the numbers of the specific staff used and the level of their respective expertise for each specific case.
Financial data were extracted from the hospital accounting records by an in-house financial analyst using StrataJazz software (Strata, Chicago, IL), a comprehensive financial analytics and performance platform used by Ochsner Health for financial planning, decision support, and fiscal inquiries. In the analysis, the professional financial and statistical data were extracted from the vascular surgery section’s detailed financial income statements. Hospital data were extracted from Strata's product line analysis and patient-encounter reporting platform. Nursing expenses for the vascular surgery units were defined as salary paid to established and additional, agency-based nurses hired during the COVID-19 pandemic to adequately staff inpatient hospital and outpatient clinical positions. The costs of nursing for vascular cases were determined solely from direct cost accounting values from encounters with a vascular surgeon listed as the “primary surgeon” for a given encounter. Regardless of the admitting service, if a vascular surgeon were listed as the “primary surgeon” for the encounter, vascular surgery was assigned the respective pre-, intra-, and postoperative nursing expenses. The nursing costs specific to vascular surgery patients were tracked on a daily basis and a per unit level and were deciphered according to the total number of beds per respective unit occupied by vascular surgery patients. The institutional and agency nurses were tracked using unique identifiers, and the data were recorded after each respective, daily unit census at our institution. Based on the respective unit’s summary financial statement, the nursing labor expenses were reported as values separate and distinct from other direct costs such as imaging, equipment, devices, and operating room anesthesia.
The financial end points analyzed included the monthly and group relative value unit (RVU) generation, overall payor/insurance mix, vascular surgery hospital and outpatient clinic margins, total vascular contribution to indirect or profit margin (CTI) from inpatient and outpatient revenue, vascular surgery nursing unit costs per month, and vascular surgery nursing unit expenses per case and per patient day. To eliminate the insurance payor mix as a variable and standardize labor expenditure data, the vascular nursing costs per RVU were calculated and compared among the groups. The average patient length of stay and U.S. Centers for Medicare & Medicaid Services (CMS) case mix indexes (CMIs) for vascular surgery cases were reviewed and compared to further standardize the trends over time. The CMI is defined as the average diagnosis-related group relative weight per case and is calculated by summing the diagnosis-related group weights for all Medicare discharges and dividing them by the number of discharges, providing a standardized estimate of case severity.
The former “clinic”-based model of the current Ochsner Health System was phased out during the past decade and replaced by a more universally used accounting system. In our financial analyses, we approached everything at the service line level. The hospital and outpatient clinic revenue and respective costs were maintained separately, and all financial data were allocated to each specific specialty using distinct inpatient and outpatient accounts, which were then combined for the total CTI or profit and total expenses for subsequent analysis when required. In the financial model for our healthcare system, the overall profit for vascular surgery includes both the professional revenue generated in vascular surgery and the hospital (facility) revenue generated from vascular surgery cases when a vascular surgeon was listed as the primary surgeon for a specific encounter.
In the analysis of costs and revenue, we examined all the direct costs, including all expenses within the vascular surgery clinic, which included administrative assistants and managers. Any salaries paid directly from the vascular surgery financial statement were included. However, >90% of these expenses were incurred by the institution as a whole and, therefore, had little effect on the specific vascular financial bottom line and were excluded. On the hospital side, any labor expenses from the care units for vascular surgery patients were included. Back-office areas and corporate areas, such as accounting, finance, business development, human resources, and security, were not included in the expenses, as reported. These expenses were considered indirect because they did not affect vascular patient care.
The CARES Act funding was allocated to the healthcare system, then to each facility, and then to each respective service line at the discretion of the administration. As was likely the case in nearly all healthcare systems, this type of granular and everchanging. month-to-month, and sometimes week-to-week, financial data were not available on a service line basis and were dependent on innumerable internal and external forces. Institutional review board approval was formally obtained. Statistical analysis was performed using the standard Student two-sample t test and the Anderson-Darling normality test.
Results
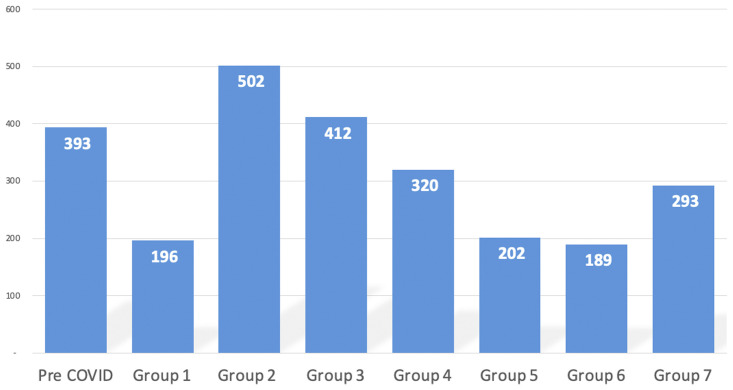
The monthly RVU generation had rebounded to and exceeded the pre–COVID-19 pandemic mean of 2520 RVUs after an isolated decrease early in the pandemic (group 1; 1734 RVUs), with values ranging from 2540 to 2863 per month for groups 2 to 5. Group 6 (2251 RVUs/mo) and group 7 (2292 RVUs/mo) demonstrated slightly decreased monthly RVUs compared with the pre–COVID-19 cohort. The average monthly RVUs in the COVID-19 period (2437 RVUs) was nearly equivalent (P = .93) to the monthly RVUs in the pre–COVID-19 cohort (2520 RVUs; Fig 1 ). Other traditional benchmarks of clinical production and revenue generation, such as monthly case volume, length of stay, and CMS CMI, did not change significantly when the two cohorts were compared. The subtle CMI change did not affect the respective physician payout. An analysis of payor mix trends demonstrated an increase in commercial (from 16% to 21%; +5%) and Medicaid (from 7% to 12%; +5%) payors, with a respective decrease in Medicare payors (from 77% to 66%; −11%), in the COVID-19 era. Perhaps the after effects of the population shift after the devastation of Hurricane Ida in August 2021 had contributed to these shifts in payor mix.
Fig 1.

Traditional determinants of surgical net revenue, monthly case volume, relative value unit (RVU), length of stay, and U.S. Centers for Medicare & Medicaid Services (CMS) case mix index (CMI) did not change significantly when the two major cohorts were compared. COVID, Coronavirus disease 2019.
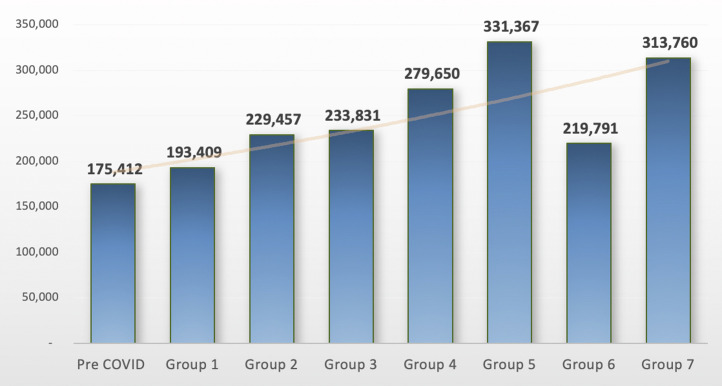
Despite the observed consistency in these parameters, which largely determine the financial outcomes, a progressive erosion occurred in the total combined vascular surgery hospital and outpatient clinic margin. The CTI, or profit margin, from inpatient hospital and outpatient clinical revenue showed an initial, drastic decrease in group 1, which had resulted from the wide scale elective case restrictions in the initial stages of the COVID-19 pandemic, followed by a swift rebound when the government restrictions were eased (group 2). A severe decline was found in the vascular inpatient margins as the pandemic progressed (groups 4-7; Fig 2 ). This decrease in revenue was accompanied by a concurrent and drastic increase in nursing labor expenses, which were quantified and analyzed using several methods. The total monthly vascular nursing unit expenses demonstrated a steady and marked increase with each sequential group in the COVID-19 cohort, with an average monthly increase of +$82,171 (+47%; P < .001; Fig 3 ). When the data for groups 5, 6, and 7 (March through November 2021) were analyzed, the average monthly costs had increased to +$113,667 (+67%; P < .001).
Fig 2.
Vascular surgery total operating (hospital and outpatient clinic) profit margin (contribution to indirect [CTI]). Data in thousands of dollars. Significant decreases in hospital margin were observed after an initial rebound increase in groups 2 and 3 after the removal of national and regional restrictions on elective cases in the first months of the coronavirus disease 2019 (COVID) pandemic (group 1).
Fig 3.
Total vascular surgery nursing unit expenses ($). A nearly continuous and severe escalation in nursing labor costs occurred seen during the coronavirus disease 2019 (COVID) pandemic.
A detailed analysis of these costs as related to three standardized metrics—labor expense per case, labor expense per patient day, and labor expense per RVU— revealed similarly severe escalations. An increase in nursing labor expenses of +$884 per vascular case (from $1630 to $2514; +54%; P < .001) was observed in the COVID-19 era, which had increased to +$1222 per case (+75%; P < .001) in groups 5 to 7 as the pandemic evolved. The nursing labor costs per patient day had increased from $580 to $852 (+$272; +53%; P < .001) during COVID-19, similarly worsening to $925 (+$345/day; +59%; P < .001) in groups 5, 6, and 7 (Fig 4 ).
Fig 4.
Total vascular surgery nursing unit expenses ($) standardized as a function of admitted patient day. Escalating nursing labor expenditures were analyzed against the control of admitted patient day (length of stay), demonstrating sustained and significant increases as the coronavirus disease 2019 (COVID) pandemic has continued.
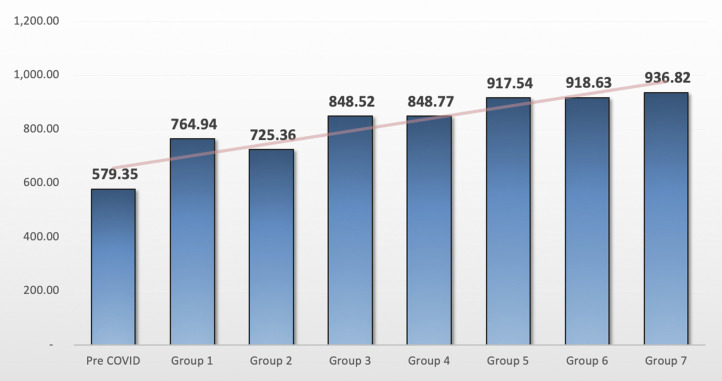
The cost of nursing and agency labor was then analyzed against a control value, the RVU, which is standardized, established, and applied uniformly by Medicare. During the COVID-19 era, the nursing labor costs per RVU had increased from $69.50 to $107.70 (+$38.20; +55%; P < .001; Fig 5 ). Ongoing RVU conversion factor implementation has been delayed to 2022, although preliminary analyses demonstrated a likely change in the CTI of ∼0.3%. On a system-wide level, agency-related nursing costs increased from $4.9 to $13.6 million/mo (+178%; P < .001) in 2021 compared with 2020. The evolution and comparison of the total vascular nursing expense, RVU production, and vascular surgery CTI during the COVID-19 pandemic are shown in Fig 6 . The increasing nursing expenses reliably, directly, and proportionally followed the repeated COVID-19 surges in New Orleans, leading to a decreased profit margin (CTI), despite sustained RVU production. Also, our preliminary data did not suggest a significant increase in non-labor expenses, although the analysis is ongoing.
Fig 5.
Total nursing expense as a function of relative value unit (RVU; $/RVU). To eliminate the potential effect of shifting payor mix on the calculated total margin, total nursing expenses were analyzed on a per RVU basis, demonstrating a dramatic conglomerate increase during the coronavirus disease 2019 (COVID) era.
Fig 6.
Total vascular nursing expense, vascular (Vasc) relative value unit (RVU), and vascular surgery margin during coronavirus disease 2019 (COVID-19) surges in a repeat pandemic epicenter. Increasing total nursing expenses (solid red bar) directly and proportionally followed repeated COVID-19 surges (blue spikes) in New Orleans, leading to a decreased profit margin (solid green bar) despite sustained RVU production (green line).
Discussion
The COVID-19 pandemic has had severe, nationwide effects on healthcare delivery, exacerbating the deleterious effects of an existing, critical, healthcare workforce shortage. In our series from the largest healthcare system in the Gulf South, an extreme increase in nursing labor expenses during the COVID-19 pandemic produced a consistent erosion in vascular surgery profit, evidenced by consistent RVU and net revenue generation with a concomitant, counterintuitive, drastic decline in the profit margin. In addition to stable monthly RVU generation throughout the COVID-19 pandemic, other traditional benchmarks that affect the financial bottom line of a surgical division, such as patient length of stay, total monthly procedure volume, and the CMS CMI did not change significantly during the pandemic, and, therefore, did not reduce the profit margin. The net revenue, margins, and total costs, as reported in our cohorts, represent a real payor mix distribution and actual cost values derived from hospital accounting data, not from Medicare estimates or hospital administration projections, increasing the accuracy and generalizability of the reported data.
Although our analysis of the two major cohorts revealed some shifts in the payor mix distribution, a variable that directly affects the reimbursement and profit margins, a concurrent and relatively equivalent increase in commercial payors during the pandemic likely offset this effect (more profitable commercial payors increased by +5% and more costly Medicaid payors had increased by +5% during the pandemic). However, to obviate the potential effects of a shifting payor mix on the calculated total margin, ultimately confirm the accuracy of the estimated effects of labor expenditures, and also to extend the generalizability of our data, the nursing expenses were analyzed on a per RVU basis, which again showed a dramatic (+55%) increase in the COVID-19 era. An analysis of the cost per RVU is perhaps the most accurate standard by which to measure variations in clinical expenses over time, because Medicare-established RVUs are not susceptible to even modest subjectivity that could subtly affect the final margin.
Our healthcare system is the largest in the Gulf South, with satellite hospitals throughout the extended regions, with many vascular surgery cases referred to our main hospital and our division, specifically. Although many healthcare centers have seen continuing decreases in RVUs, we have not experienced this trend, perhaps because of our unique presence in the region.1, 2, 3, 4, 5, 6, 7 To the best of our knowledge, significant regional and national changes in nursing labor costs were not observed during the 14-month pre–COVID-19 interval. The increase in nursing labor cost observed since March 2020 were wholly attributable to the increased turnover in our respective healthcare system’s nursing staff and the consequently required increase in the usage of extremely expensive agency nurses to staff those positions. This phenomenon, in turn, initiated an increase in salaries and bonuses for established healthcare system nurses who were retained. A comparison of the expense of nursing labor in the New Orleans area to other regional areas or a national average would be quite difficult to quantify with confidence given the lack of reliable, transparent, generalizable data from other regions. Healthcare systems in general are extremely careful with their respective granular financial data, especially in the current era of fiscal loss.
Our analysis was designed and executed to examine a specific and serious issue—the wildly increasing costs of nursing labor and the relationship of these labor costs to the clinic profit and hospital profit (CTI). The co-linear, most powerful relationship we observed during the pandemic was that of increasing nursing expenses per case, RVU, and encounter. We have also been examining other areas of direct costs and supply chain variables with financial impact during the COVID-19 pandemic.
Although, to the best of knowledge, our report is the first to demonstrate a direct relationship between nursing labor expenses and declining surgical margins, nationwide reports detailing the crippling effects of pandemic-induced labor costs on healthcare finance have emerged. According to data from a nearly 3000-hospital Medicare Cost Report, the average annual hospital contract labor expense increased >20% to $4.59 million as a result of increased expenditures in 2021. This average contract labor cost more than doubled in <10 years from $2.23 million in 2011. Using these Medicare data, care analytics firm Kaufman Hall showed that the total expenses per discharge in 2021 had increased 24% and the labor expenses per adjusted discharge had increased by 26% compared with the prepandemic trends.5 Although less severe, these data parallel our own experience of nursing expenses per patient day and per vascular surgery case with increases of 53% and 54%, respectively. The clinical labor costs have increased by an average of 8% per patient day compared with the prepandemic data reported in the 2019 Medicare Cost Report. Thus, for the average 500-bed hospital, this would translate into an annual increase of $17 million in labor expenses alone since the pandemic began. Our results have demonstrated an even more drastic increase, from $4.9 million per month in 2020 to $13.6 million per month in 2021, annualizing to an additional $104.4 million spent in 2021 for nursing labor expenses.
Since the onset of the COVID-19 pandemic, national healthcare employment has decrease by 524,000, with the nursing workforce and residential care facilities accounting for approximately four fifths of the loss according to the U.S. Bureau of Labor and Statistics.6 In addition, ∼24% of the 5000 U.S. hospitals reporting staff status to the HHS have reported a critical staffing shortage according to data released in a January 8, 2022 report, with another 100 hospitals (+5%) anticipating shortages within 1 week of the HHS evaluation.7 These values represent the largest share of hospital shortages since the HHS began releasing such categorized data in November 2020. This type of acute labor shortage has added to hospitals' already precarious financial status by inducing costly and intensive recruitment and retention packages, which, in turn, have resulted in widespread increases in labor costs. The same U.S. Bureau of Labor and Statistics summary reported that healthcare systems nationally are paying $24 billion more per year for qualified clinical labor than required before the pandemic.6 In addition, data from that report showed that overtime hours had increased 52% as of September 2022, and the use of agency and temporary labor had increased 132% for full-time and 131% for part-time laborers, again mirroring our departmental experience. The use of contingency labor, or positions created to complete a temporary project or specific function, had increased by nearly 126%. Overtime and the use of agency staff are the most expensive labor choices for hospitals—usually adding ≥50% to a typical employee's hourly rate according to the HHS.8 This amalgam of drastic increases in labor expenditure has been evolving into a perfect storm of potential financial catastrophe in the United States.
An additional complicating factor contributing to the current workforce crisis is the proportionally high COVID-19 exposure risk that nurses incur, with subsequent quarantines and recoveries requiring the use of mandatory sick time. Data from the HHS and the U.S. Bureau of Labor and Statistics have shown that the use of sick time, especially among full-time employees in intensive care units, has increased 50% for full-time clinical staff and >60% for part-time employees compared with the prepandemic baseline.6 , 7 This stereotypical sequence of exposure, infection, and mandatory time off has serious financial repercussions for the previously stated reasons. This phenomenon was clearly observed in our own experience. The highest proportional spikes in labor expenses occurred after the highest peaks in citywide COVID-19 positivity (Fig 6).
The exodus of experienced nurses from the current workforce and the increasing turnover rate among early career nurses has led to a widening nursing skills gap, with major repercussions for U.S. healthcare systems. Experts in healthcare labor had highlighted the critical shortage of highly skilled nurses for years before the pandemic. In October 2010, the Institute of Medicine released a landmark report titled “The Future of Nursing,” in collaboration with the Robert Wood Johnson Foundation, which called for an increase in the number of baccalaureate-level nurses in the workforce to 80% and a doubling of the number of nurses with doctoral degrees.9 The current nursing workforce falls far short of these recommendations—only 64.2% of registered nurses are currently prepared at the baccalaureate or graduate level according to the latest workforce survey released by the National Council of State Boards of Nursing.10
Graduate nursing education and the additional professional training of established nurses present their own unique consequences for the overall nursing workforce. Between 2010 and 2017, the number of nurse practitioners in the United States more than doubled, from ∼91,000 to ∼190,000. This growth occurred in every U.S. region and was driven by the rapid expansion of doctoral and professional educational programs that disproportionally attracted nurses from the millennial generation. This marked growth in the number of nurse practitioners has reduced the size of the registered nurse workforce by ∼80,000 nationwide. Additionally, a report in Nursing Economics estimated that between 2010 and 2030, >1 million registered nurses would retire from the workforce—taking decades of skills and knowledge with them.11
Under the CARES Act passed in March 2020, Congress attempted to stem the tide of overwhelming financial loss in healthcare by establishing a provider relief fund that has been replenished several times, now standing at $178 billion. However, no funding was specifically dedicated to address workforce and, in particular, nursing labor shortages and the resultant costs. Given these current critical and unsustainable related trends, the CMS has been moving to update its clinical labor pricing data.12 The 2022 Medicare Physician Fee Schedule will support physician practices, in particular, primary care practices, that rely heavily on nurses, medical assistants, and other clinical staff to provide patient care. The rates for registered nurses will increase 67%, and the rate for medical assistants will increase 50%. Additionally, in November 2021, the current administration announced a $1.5 billion investment to specifically address healthcare workforce shortages and improve clinical care in underserved communities disproportionately affected by the COVID-19 pandemic. A critical obstacle preventing nursing workforce expansion is health education student debt, which is at an average of >$200,000 per student. With this investment by the U.S. government, the educational debt of >22,700 doctors, dentists, nurses, and behavioral health providers will be absolved in exchange for a commitment averaging 4 years of working in critically understaffed areas affected by the pandemic.13 Given the immense scope, chronicity, and severity of the nursing shortage in the national healthcare system, it remains to be seen whether government intervention beyond these recently announced programs will alleviate this potentially catastrophic trend.
Our study had several limitations. The data collection period was limited to a prepandemic interval of 14 months, perhaps reducing the power of the control cohort data because financial trends might evolve over the course of years. Previous reports of the financial effects of the pandemic on surgical revenue had analyzed just 2-month control periods in 2019 vs 2020.14 Although the accuracy and baseline generalizability of the data were strengthened by the use of financial margins and costs representing real payor mix and cost values derived from hospital accounting data, rather than the more commonly reported Medicare estimates and hospital administration projection, our results reflect trends from one healthcare system in a repeat epicenter of the pandemic. As such, broad-based conclusions from this data set might not be uniformly applicable to healthcare systems around the United States. Different hospitals could have variable income losses depending on the volume and type of elective procedures performed, hospital staffing, hospital financial reserves, and other factors specific to each hospital. In addition, inherent to a retrospective review in an observational study, confirmation and observation bias are possible. Finally, although the increase in nursing labor costs certainly correlated with the decreased margins in our study, direct and complete causality would be challenging to prove as an absolute in this situation, owing to the unintentional potential omission of variables such as supply costs and other infrastructure expenditures.
Conclusions
The financial effects of the COVID-19 pandemic has fundamentally changed the healthcare environment in the United States. The overall nursing shortage has fiercely intensified under a multitude of de novo stressors during the pandemic, which has exposed and aggravated long-term issues that have hamstrung the nursing workforce for decades. The results from the present series have demonstrated severe erosion of vascular surgery profit margin with dramatically escalating nursing labor costs and consistent clinical revenue generation. Although this institutional trend will continue to evolve, the pandemic is also continuing to evolve, with no definite end in sight. Clearly, this situation is not tenable, and dedicated institutional, state, and national programs to assuage the workforce and financial crises are required. Although some relief targeted to the nursing shortage has been dedicated by the U.S. government, the immense financial loss from COVID-19 suggests a fundamental rethinking of government’s role in pandemic-related workforce preparation is required. At present, the United States has prioritized spending on acute COVID-19 treatment, with far less spent on staffing, public health services, and infrastructure. The current trend is wholly unsustainable and potentially catastrophic. As the United States struggles to recover from the ongoing pandemic, current investments in nursing education, training, and recruitment should likely be established permanently.
Author Contributions
Conception and design: CB, SM
Analysis and interpretation: CB, GE, WS, SM
Data collection: CB, GE, PR
Writing the article: CB
Critical revision of the article: CB, GE, PR, WS, SM
Final approval of the article: CB, GE, PR, WS, SM
Statistical analysis: CB
Obtained funding: Not applicable
Overall responsibility: CB
From the Southern Association for Vascular Surgery
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Swanson S. National Hospital Flash Report: December 2021. Kaufman, Hall and Associates. https://www.kaufmanhall.com/sites/default/files/2021-12/Dec2021-National-Hospital-Flash-Report.pdf Available at:
- 2.Financial Effects of COVID-19: Hospital Outlook for the Remainder of 2021. https://www.aha.org/guidesreports/2021-09-21-financial-effects-covid-19-hospital-outlook-remainder-2021 Available at:
- 3.Boyle P. Hospitals innovate amid dire nursing shortages. American Association of Medical Colleges. September 2021. https://www.aamc.org/news-insights/hospitals-innovate-amid-dire-nursing-shortages Available at:
- 4.Grant E. Official American Nurses Association Communication. https://www.nursingworld.org/news/news-releases/2021/ana-urges-us-department-of-health-and-human-services-to-declare-nurse-staffing-shortage-a-national-crisis/https://www.nursingworld.org/∼4a49e2/globalassets/rss-assets/analettertohhs_staffingconcerns_final-2021-09-01.pdf Available at:
- 5.Becker’s Hospital CFO Report: January 9, 2022. https://www.beckershospitalreview.com/e-weeklies/beckers-hospital-cfo-report-e-weekly.html Available at:
- 6.U.S. Bureau of Labor and Statistics News Release. January 7, 2022. https://www.bls.gov/news.release/pdf/empsit.pdf Available at:
- 7.HHS Protect Public Data Hub. January 12, 2022. https://protect-public.hhs.gov/pages/hospital-reporting Available at:
- 8.U.S. Department of Health and human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. The future of the nursing work-force: national- and state-level projections, 2012-2025. https://www.njccn.org/wp-content/uploads/2015/07/The-Future-of-the-Nursing-Workforce-Nationa-and-State-Level-Projections-2012-2025.pdf Available at:
- 9.Institute of Medicine The Future of Nursing: Leading Change, Advancing Health. The National Academies Press. 2011. Available at: [DOI] [PubMed]
- 10.National Council of State Boards of Nursing: National Nursing Workforce Study. https://www.ncsbn.org/workforce.htm Available at:
- 11.Buerhaus P.I., Skinner L.E., Auerbach D.I., Staiger D.O. State of the registered nurse workforce as a new era of health reform emerges. Nurs Econ. 2017;35:229–237. [Google Scholar]
- 12.U.S. Centers for Medicare & Medicaid Services Physician Fee Schedule. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched Available at:
- 13.The White House. Vice President Harris Announces Historic Funding to Bolster Equitable Health Care During Pandemic, and Beyond: November 2021. https://www.whitehouse.gov/briefing-room/statements-releases/2021/11/22/vice-president-harris-announces-historic-funding-to-bolster-equitable-health-care-during-pandemic-and-beyond Available at:
- 14.Fang Z.B., Simons J., Judelson M.D., Arous E.J., Jones D.W., Steppacher R.C., et al. Financial implications of coronavirus disease 2019 on a tertiary academic vascular surgery practice. J Vasc Surg. 2021;73:1869–1875. doi: 10.1016/j.jvs.2021.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]