Abstract
Background
The mortality from COVID-19 alone cannot account for the impact of the pandemic. Cardiovascular disease (CVD) mortality has increased disproportionately in specific racial/ethnic populations.
Objective
This study aimed to characterize how the COVID-19 pandemic impacted the association between CVD mortality and social and demographic factors as characterized by the Social Vulnerability Index (SVI).
Methods
Medical Examiner Case Archive of Cook County, Illinois was utilized to identify CVD deaths in 2019 (pre-pandemic) and 2020 (pandemic). Rate ratios (RRs) were used to compare age-adjusted mortality rates (AAMRs). Addresses of deaths were geocoded to Chicago Community Areas. The Spearman's rank correlation coefficient (ρ) test was used to identify the association between SVI and CVD mortality.
Results
AAMRs of CVD deaths significantly increased among non-Hispanic Black individuals (AAMRR, 1.1; 95 % CI, 1.1–1.2) and Hispanic individuals (AAMRR, 1.8; 95 % CI, 1.5–2.1) from 2019 to 2020. Among non-Hispanic White individuals, the AAMR did not significantly increase (AAMRR, 1.0; 95 % CI, 0.9–1.1). A significant positive association was observed between SVI and the percentage of non-Hispanic Black residents (ρ = 0.45; P < 0.05), while the inverse was observed with the percentage of non-Hispanic White residents (ρ = −0.77; P < 0.05). A significant positive association between SVI and CVD mortality rate increased (ρ = 0.24 and 0.28; P < 0.05).
Conclusions
Significant association between SVI and CVD mortality was strengthened from 2019 to 2020, and CVD mortality increased among non-Hispanic Black and Hispanic populations. These findings demonstrate that the COVID-19 pandemic has led to an exacerbation of health inequities among different racial/ethnic populations resulting in increased CVD mortality.
Keywords: Cardiovascular disease mortality, COVID-19 pandemic, Health disparity, Social vulnerability index
1. Introduction
The Coronavirus Disease 2019 (COVID-19) has resulted in >1 million deaths in the United States since being declared a global pandemic by the World Health Organization [1]. However, the mortality from COVID-19 alone does not account for the impact of the pandemic. Studies have reported that during the pandemic a proportion of excess all-cause deaths, ranging from 28 % to 50 %, were secondary to causes other than COVID-19 [2], [3]. Cardiovascular disease was a significant cause of the excess deaths, and the number of deaths secondary to ischemic heart disease and hypertension notably increased during the beginning of the COVID-19 pandemic. During March 2020 to May 2020, the number of hospitalizations due to cardiovascular disease decreased while out-of-hospital cardiac arrests increased, which inform the pandemic's impact on CVD management and mortality [4], [5], [6], [7], [8], [9], [10].
Different racial/ethnic populations have been disproportionately affected by COVID-19. A prior study reported that non-Hispanic Black, Hispanic, and non-Hispanic Asian populations experienced a significantly greater increase in heart and cerebrovascular disease deaths during the COVID-19 pandemic compared with the non-Hispanic White population [10]. Furthermore, a study reported a reversal of the Latino mortality paradox in 2020, with Latino individuals experiencing greater mortality than non-Hispanic Whites during the COVID-19 pandemic [11], [12], [13]. The disproportionate increase of cardiovascular deaths among specific racial/ethnic populations suggests that the COVID-19 pandemic has exacerbated preexisting social barriers to care that have disproportionately affected these populations [14], [15], [16], [17], [18], [19]. Non-Hispanic Black populations have been at increased risk for CVD and mortality, and the higher burden of clinical risk factors for CVD (e.g., hypertension and hyperlipidemia) alone has not accounted for this increased risk [20].
Prior to the COVID-19 pandemic, structural and social factors, such as housing and job insecurity or high poverty rates, have affected racial/ethnic minority populations and contributed to the greater CVD burden observed in these communities. Effects of the COVID-19 pandemic have likely exacerbated these social disadvantages, resulting in increased CVD mortality among specific racial/ethnic populations. This study aimed to characterize the association between social and demographic factors and CVD mortality before and during the COVID-19 pandemic.
2. Methods
2.1. Data
Data on deaths in Cook County, Illinois (including the City of Chicago), were collected from the Medical Examiner Case Archive [13]. The Medical Examiner Case Archive includes deaths that occur in Cook County and are under the jurisdiction of the Medical Examiner. The Medical Examiner Case Archive has been utilized in prior studies to identify cardiovascular disease deaths and includes data on the causes and manners of deaths as classified by the International Classification of Diseases, 10th Revision, and Clinical Modification (ICD-10) codes [21], [22], [23], [24]. Demographic information, including age, sex, race, and ethnicity, were obtained from death certificates of the Medical Examiner Case Archive. Deaths related to COVID-19 have been recorded in the archive dataset since March 16, 2020.
Deaths of persons identified as non-Hispanic White, non-Hispanic Black, and Hispanic from death certificates were included. Deaths of persons identified as Other were excluded from analysis. Deaths secondary to cardiovascular disease were identified using ICD-10 codes recognizing diseases of the circulatory system: I00-I02 (acute rheumatic fever), I05-I09 (chronic rheumatic heart diseases), I10-I15 (hypertensive diseases), I20-I25 (ischemic heart diseases), I26-I28 (pulmonary heart disease and diseases of pulmonary circulation), I30-I52 (other forms of heart diseases), I60-I69 (cerebrovascular diseases), and I70-I79, I80-I89, I95-I99 (other disorders of the circulatory system). Cardiovascular disease deaths associated with COVID-19 were excluded from analysis. To compare cardiovascular disease deaths that occurred before and during the COVID-19 pandemic, deaths that occurred during January 1, 2019, to December 31, 2019, and January 1, 2020, to December 31, 2020, were identified and compared.
The City of Chicago is the third most populous city in the United States by 2020 US Census Bureau data with 33.3 % of the population identified as non-Hispanic White, 29.6 % of the population identified as non-Hispanic Black, and 28.8 % identified as Hispanic. The City of Chicago is comprised of 77 Chicago Community Areas (CCA) defined by the geographic boundaries of about 800 census tracts [25]. Incident addresses for all CVD deaths were geocoded using ArcMap geographic information system (GIS) software program.
The Chicago Health Atlas was utilized to identify the burden of CVD mortality risk in each CCA [26]. The Chicago Health Atlas is a collection of health data that is gathered and published by the Chicago Department of Public Health. Sources that contribute to the development of the Chicago Health Atlas include the American Community Survey, the Centers for Disease Control and Prevention (CDC), Healthy Chicago Survey, and the Cook County Medical Examiner. The following variables were utilized to characterize CVD mortality risk: adult hypertension rates, adult diabetes rates, adult smoking rates, adult obesity rates, and percentage of residents in families that are in poverty (below the Federal Poverty Level) [26].
We also utilized the Centers for Disease and Control and Prevention/Agency for Toxic Substances and Disease Registry (CDC/ATSDR) Social Vulnerability Index (SVI) [27], [28]. Social vulnerability refers to the sum of economic, demographic, and social factors that affect a community's risk exposure and ability to respond to hazardous events such as natural disasters. Four themes of vulnerability, comprised of fifteen variables from the American Community Survey data from 2014 to 2018, are used to report the social vulnerability index [1]: socioeconomic status [2], household composition & disability [3], minority status and language, and [4] housing type and transportation. Each of the fifteen variables is ranked, and the fifteen variable rankings are summed to calculate the SVI which is reported as a percentile rank ranging from 0 to 1 where a higher value indicates greater vulnerability.
Only de-identified and publicly available data were used in this study, and thus institutional review board approval of the University of Illinois at Chicago was not needed.
2.2. Analysis
To calculate the age-adjusted mortality rates (AAMRs) (per 100,000 population), age-specific death rates were directly standardized using the 2019 non-Hispanic White, Cook County, Illinois population as reported by the United Census Bureau [29]. Rate ratios and 95 % CIs were calculated using a Poisson distribution to compare AAMRs between 2019 (pre-pandemic year) and 2020 (pandemic year). Statistical analysis was performed using RStudio (Version 1.4.1717, RStudio).
The SVI of the CCAs was aggregated from the mean SVI of the census tracts in each CCA. ArcMap was utilized to map CVD mortality risk factors, SVI, and CVD mortality rates to each CCA. We used the Spearman's rank correlation coefficient (ρ) test to identify associations among the three groups of indicators. Statistical analyses were performed using ArcMAP and STATA/IC (Version 15.1, Statacorp).
3. Results
In 2020, a total of 13,899 deaths were documented by the Medical Examiner in Cook County, Illinois, and 5777 deaths were documented in 2019. In 2019, the AAMR of all-cause deaths (per 100,000 population) was greatest among the non-Hispanic Black population compared to the non-Hispanic White or Hispanic populations (233.0 deaths, 115.8 deaths, and 60.0 deaths per 100,000, respectively). Hispanic individuals had a lower AAMR compared to non-Hispanic White individuals in 2019 (60.0 deaths vs. 115.8 deaths per 100,000, respectively). However, in 2020 the AAMR of Hispanic individuals was greater than non-Hispanic White individuals (328.8 deaths vs. 267.8 deaths per 100,000, respectively). From 2019 to 2020, the AAMR significantly increased among non-Hispanic Black individuals (AAMR ratio, 2.3; 95 % CI, 2.2–2.4), non-Hispanic White individuals (AAMR ratio, 2.3; 95 % CI, 2.2–2.4), and Hispanic individuals (AAMR ratio, 5.5; 95 % CI 5.2–5.8) (Table 1).
Table 1.
All-cause deaths and age-adjusted mortality rates by race and ethnicity in 2019 and 2020.
| Race and ethnicity of residents | 2019 |
2020 |
2020–2019 AAMR ratio | 95 % CI | ||
|---|---|---|---|---|---|---|
| Deaths | AAMRa | Deaths | AAMRa | |||
| Non-Hispanic Black | 2564 | 233.0 | 5567 | 536.8 | 2.3 | (2.2, 2.4) |
| Non-Hispanic White | 2504 | 115.8 | 5791 | 267.8 | 2.3 | (2.2, 2.4) |
| Hispanic | 709 | 60.0 | 2541 | 328.8 | 5.5 | (5.2, 5.8) |
Abbreviations: AAMR, age-adjusted mortality rate. CI, confidence interval.
AAMR is reported per 100,000 population.
The number of deaths from CVD increased from 2019 to 2020 (1793 deaths vs. 1974 deaths, respectively). The AAMR of CVD deaths was greatest among the non-Hispanic Black population in 2019 and 2020 (76.8 deaths and 88.0 deaths per 100,000, respectively). From 2019 to 2020, the AAMR of CVD deaths significantly increased among non-Hispanic Black individuals (AAMR ratio, 1.1; 95 % CI, 1.1–1.2) and Hispanic individuals (AAMR ratio, 1.8; 95 % CI 1.5–2.1). However, among White individuals, the AAMR of CVD deaths did not significantly increase from 2019 to 2020 (AAMR ratio, 1.0; 95 % CI 0.9–1.1) (Table 2).
Table 2.
Cardiovascular disease deaths and age-adjusted mortality rates by race and ethnicity in 2019 and 2020.
| Race and ethnicity of residents | 2019 |
2020 |
2020–2019 AAMR ratio | 95 % CI | ||
|---|---|---|---|---|---|---|
| Deaths | AAMRa | Deaths | AAMRa | |||
| Non-Hispanic Black | 783 | 76.8 | 891 | 88.0 | 1.1 | (1.1, 1.2) |
| Non-Hispanic White | 888 | 41.1 | 921 | 42.6 | 1.0 | (0.9, 1.1) |
| Hispanic | 122 | 11.9 | 162 | 21.2 | 1.8 | (1.5, 2.1) |
Abbreviation: AAMR, age-adjusted mortality rate. CI, confidence interval.
AAMR is reported per 100,000 population.
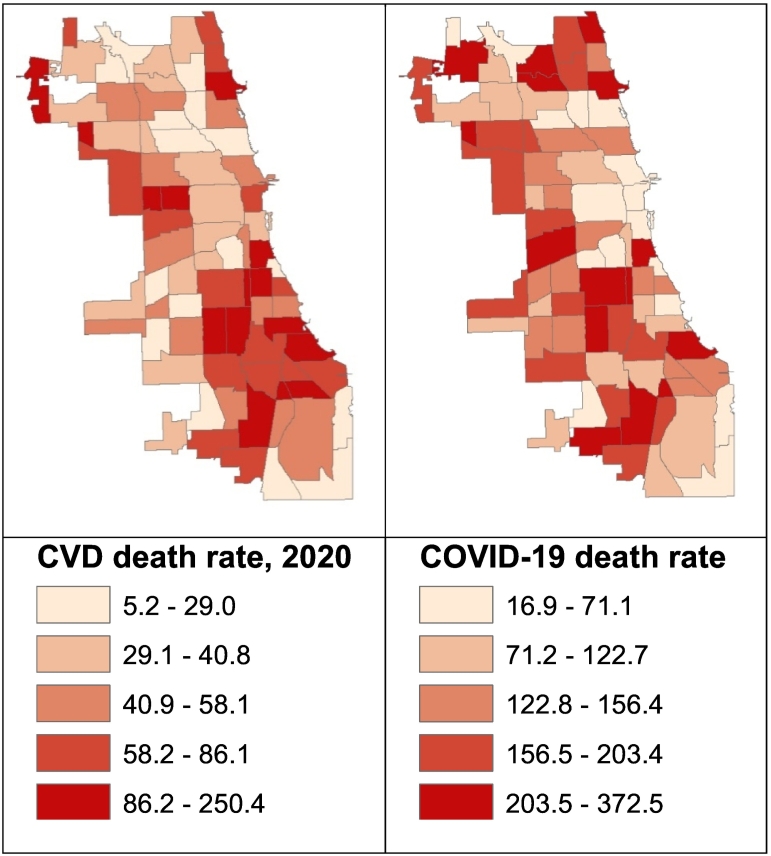
Fig. 1 depicts the 2020 CVD and COVID-19 mortality rate of 77 Chicago Community Areas, and areas with greater CVD mortality coincided with areas of greater COVID-19 mortality.
Fig. 1.
The spatial distribution of mortality rates secondary to COVID-19 and cardiovascular disease by Chicago community areas.
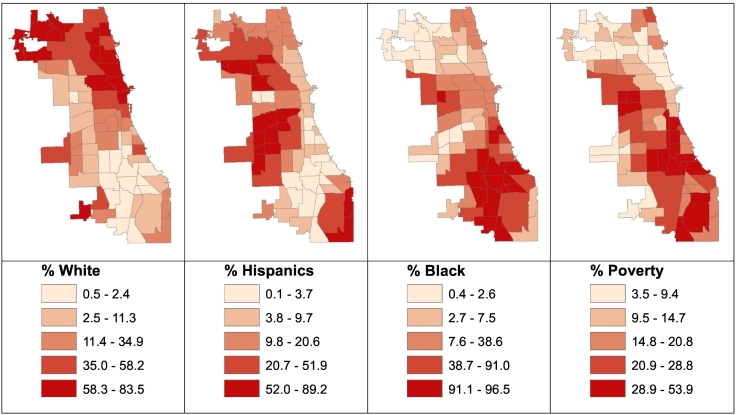
The percentage of non-Hispanic Black, Hispanic, or non-Hispanic White residents at the CCA level is shown in Fig. 2. Chicago's Southern and Western areas coincided with CCAs with predominantly non-Hispanic Black residents. The Western areas of Chicago coincided with CCAs with predominantly Hispanic residents indicating high residential segregation. In addition, the percentage of residents in families living in poverty was mapped at the CCA level, and areas with higher poverty rates coincided with predominantly non-Hispanic Black communities. Furthermore, CCAs with increased CVD mortality rates in 2020 largely overlapped with CCAs with predominantly non-Hispanic Black communities.
Fig. 2.
The spatial distribution of the percentage of non-Hispanic, African American/Black, Hispanic, and white residents as well as the percentage of residents who live under the National Poverty Line in Chicago Community.
In both 2019 and 2020, traditional risk factors associated with cardiovascular disease such as hypertension (ρ = 0.38 and 0.33; P < 0.05) and smoking (ρ = 0.32 and 0.38; P < 0.05) were positively associated with cardiovascular disease mortality rates (Table 3). Both the percentage of non-Hispanic Black residents (ρ = 0.55 and 0.57; P < 0.05) and the percentage of residents living in poverty (ρ = 0.47 and 0.51; P < 0.05) were significantly associated with CVD mortality rates in 2019 and 2020. Notably, these positive associations strengthened from 2019 to 2020. Significant negative associations were observed between cardiovascular disease mortality rate and percentage of non-Hispanic White (ρ = −0.38 and −0.46; P < 0.05) and Hispanic residents (ρ = −0.52 and −0.49; P < 0.05). Interestingly, while the negative association between CVD mortality and the percentage of non-Hispanic White residents strengthened, the negative association between CVD mortality and the percentage of Hispanic residents weakened from 2019 to 2020.
Table 3.
Association of risk for CVD mortality, social vulnerability, and CVD mortality rates at the community level in 2019 and 2020.
| Correlation coefficient (ρ)⁎ |
|||
|---|---|---|---|
| CVD mortality rate |
SVI | ||
| 2019 | 2020 | ||
| Percent of non-Hispanic Black residents | 0.55 | 0.57 | 0.45 |
| Percent of non-Hispanic White residents | −0.38 | −0.46 | −0.77 |
| Percent of Hispanic residents | −0.52 | −0.49 | 0.02 |
| Hypertension rate | 0.38 | 0.33 | 0.23 |
| Diabetes rate | 0.12 | 0.18 | 0.40 |
| Smoking rate | 0.32 | 0.38 | 0.44 |
| Obesity rate | 0.15 | 0.21 | 0.62 |
| Poverty rate | 0.47 | 0.51 | 0.73 |
| Social vulnerability index | 0.24 | 0.28 | Not applicable |
Abbreviations: CVD, cardiovascular disease. SVI, social vulnerability index.
Significant association (P < 0.05) are marked in bold.
The social vulnerability index of the 77 CCAs ranged from 0.13 to 0.95, with a median SVI of 0.71. SVI was significantly positively associated with rates of known CVD risk factors such as hypertension (ρ = 0.23; P < 0.05), obesity (ρ = 0.62; P < 0.05), diabetes (ρ = 0.40; P < 0.05), and smoking (ρ = 0.44; P < 0.05) within the CCAs (Table 3). SVI was also significantly positively associated with the percentage of non-Hispanic Black residents (ρ = 0.45; P < 0.05), while the inverse association was observed with the percentage of non-Hispanic White residents (ρ = −0.77; P < 0.05). The significant positive association between SVI and CVD mortality rate strengthened from 2019 and 2020 (ρ = 0.24, 0.28; P < 0.05).
4. Discussion
A significant increase in CVD mortality was observed among non-Hispanic Black and Hispanic individuals from 2019 to 2020. The percentage of non-Hispanic Black residents in the CCAs was positively associated with CVD mortality. In contrast, the percentage of non-Hispanic White or Hispanic residents was negatively associated with CVD mortality. The significant positive association between social vulnerability and CVD mortality strengthened from 2019 to 2020.
The mortality from COVID-19 infection alone cannot account for the impact of the COVID-19 pandemic. The pandemic limited access to health care, resulted in job losses and exacerbated housing and food insecurities for many, and the downstream consequences of this health crisis may have disrupted cardiovascular disease management. The association between social vulnerability and CVD mortality strengthened from 2019 to 2020, suggesting that preexisting health disparities may have been exacerbated for those already at high-risk for cardiovascular disease mortality. Furthermore, we observed a significant increase in the number of CVD deaths in Cook County, Illinois; findings that have also been noted on a national scale. A prior study demonstrated that nationally the CVD mortality rate significantly increased from 2019 (pre-pandemic) to 2020 (pandemic), and the increase in CVD mortality was observed again when trends from prior to the pandemic (2011–2019) was compared with the pandemic period (2020) [9], [10], [30].
Racial and ethnic residential segregation has been pervasive in Chicago, and 90 % non-Hispanic Black residents reside in the south and west sides of Chicago (17 of 77 CCAs) [25], [26], [31], [32]. Residential segregation results in the concentration of poverty, discrimination, environmental pollution, or housing insecurity. CCAs with a high percentage of non-Hispanic Black residents coincided with areas with a high percentage of residents in poverty and greater social vulnerability (Fig. 2). We observed that not only was the percentage of non-Hispanic Black residents significantly associated with CVD mortality, but the association also strengthened from 2019 to 2020 during the COVID-19 pandemic, while a significant negative association between CVD mortality and the percentage of non-Hispanic White residents strengthened from 2019 to 2020. These findings demonstrate that exposure to social and health risks concentrated in segregated neighborhoods results in health inequities and CVD mortality, which were exacerbated during the COVID-19 pandemic.
Prior to the COVID-19 pandemic, the mortality rate among Hispanic individuals was less than that of non-Hispanic White individuals despite an increased rate of poverty among Hispanic individuals. A recent study demonstrated that the “Latino mortality paradox” was reversed during the COVID-19 pandemic [13]. In this study, we also observed a reversal of the Latino mortality paradox. However, we did not observe a significant association between SVI and the percentage of Hispanic residents. SVI incorporates factors related to not only socioeconomic status but also social support, such as household composition. The results of this study suggest that although the Hispanic population has disproportionately experienced poverty in comparison to the non-Hispanic White population, cultural and social factors may lead to protective, improved health behaviors as has been suggested in prior studies addressing the “Latino mortality paradox” [11], [12].
4.1. Limitations
This study has limitations. First, the results reflect analysis of a single metropolitan area and may be limited in external validity or generalizability. However, Chicago and Cook County, Illinois have a diverse population that may serve as a representative cohort to further examine the burden of CVD mortality. Second, we analyzed deaths secondary to CVD as identified by the Medical Examiner, and undiagnosed COVID-19 cases may have contributed to the number of CVD deaths identified during the pandemic. Third, the pre-pandemic and pandemic time periods were defined as January 1, 2019, to December 31, 2019, and January 1, 2020, to December 31, 2020, respectively. As the Medical Examiner Case Archive recorded deaths secondary to COVID-19 from March 16, 2020, the defined study periods may have underestimated the number of deaths secondary to COVID-19 during the pandemic.
5. Conclusions
There was an increase in cardiovascular disease mortality observed from 2019 to 2020 during the COVID-19 pandemic in Chicago and larger Cook County, Illinois. Cardiovascular disease mortality significantly increased among the non-Hispanic Black and Hispanic population, whereas the mortality rate did not significantly increase among the non-Hispanic White population. Furthermore, the significant association between social vulnerability and cardiovascular disease mortality increased from 2019 to 2020. These findings suggest that the COVID-19 pandemic has exacerbated preexisting health inequities leading to increased cardiovascular disease mortality among specific racial/ethnic populations. The results of this study inform the continued need for public health strategies to both recognize and address health inequities that continue to result in racial and ethnic inequality in cardiovascular disease mortality.
Sources of funding
There are no sources of funding to report.
CRediT authorship contribution statement
YJK – formal analysis, writing original/review and editing SK – formal analysis, conceptualization, methodology JA – formal analysis, software ASV - supervision NTN - concept, methods, data curation, writing original/review and editing, supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Centers for Disease and Control and Prevention COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#datatracker-home [Internet]. [cited 2022 May 31]. Available from.
- 2.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinberger D.M., Chen J., Cohen T., Crawford F.W., Mostashari F., Olson D., et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern. Med. 2020;180(10):1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatt A.S., Moscone A., McElrath E.E., Varshney A.S., Claggett B.L., Bhatt D.L., et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020;76(3):280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uy-Evanado A., Chugh H.S., Sargsyan A., Nakamura K., Mariani R., Hadduck K., et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin. Electrophysiol. 2021;7(1):6–11. doi: 10.1016/j.jacep.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mountantonakis S.E., Saleh M., Coleman K., Kuvin J., Singh V., Jauhar R., et al. Out-of-hospital cardiac arrest and acute coronary syndrome hospitalizations during the COVID-19 surge. J. Am. Coll. Cardiol. 2020;76(10):1271–1273. doi: 10.1016/j.jacc.2020.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baum A., Schwartz M.D. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai P.H., Lancet E.A., Weiden M.D., Webber M.P., Zeig-Owens R., Hall C.B., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5(10):1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wadhera R.K., Shen C., Gondi S., Chen S., Kazi D.S., Yeh R.W. Cardiovascular deaths during the COVID-19 pandemic in the United States. J. Am. Coll. Cardiol. 2021;77(2):159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wadhera R., Figueroa J.F., Rodriguez F., Liu M., Tian W., Kazi D.S., et al. Racial and ethnic disparities in heart and cerebrovascular disease deaths during the COVID-19 pandemic in the United States. Circulation. 2021;143(24):2346–2354. doi: 10.1161/CIRCULATIONAHA.121.054378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruiz J.M., Steffen P., Smith T.B. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am. J. Public Health. 2013;103(3):e52–e60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abraído-Lanza A.F., Dohrenwend B.P., Ng-Mak D.S., Turner J.B. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am. J. Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon P., Ho A., Shah M.D., Shetgiri R. Trends in mortality from COVID-19 and other leading causes of death among Latino vs White individuals in Los Angeles County, 2011–2020. JAMA. 2021;326(10):973–974. doi: 10.1001/jama.2021.11945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chowkwanyun M., Reed A.L., Jr. Racial health disparities and COVID-19 — caution and context. N. Engl. J. Med. 2020;383(3):201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 16.van Dorn A., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim S.J., Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ. Behav. 2020;47(4):509–513. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diaz C.L., Watson K.E. Racial/ethnic health disparities in cardiovascular disease during the COVID-19 pandemic: revisiting a long-lasting problem. Cardiovasc. Res. 2021;118(1):8–10. doi: 10.1093/cvr/cvab318. [DOI] [PubMed] [Google Scholar]
- 19.Hill J.A., Albert M.A., Carnethon M.R., Watson K.E. Disparities in cardiovascular medicine: circulation's response. Circulation. 2020;142(12):1127–1128. doi: 10.1161/CIRCULATIONAHA.120.050670. [DOI] [PubMed] [Google Scholar]
- 20.Golomb M., Redfors B., Crowley A., Smits P.C., Serruys P.W., von Birgelen C., et al. Prognostic impact of race in patients undergoing PCI analysis from 10 randomized coronary stent trials. JACC Cardiovasc. Interv. 2020;13(13):1586–1595. doi: 10.1016/j.jcin.2020.04.020. [DOI] [PubMed] [Google Scholar]
- 21.Tang Y., Sampson B., Pack S., Shah K., Um S.Y., Wang D., et al. Ethnic differences in out-of-hospital fatal pulmonary embolism. Circulation. 2011;123(20):2219–2225. doi: 10.1161/CIRCULATIONAHA.110.976134. [DOI] [PubMed] [Google Scholar]
- 22.Tester D.J., Ackerman M.J. Postmortem long QT syndrome genetic testing for sudden unexplained death in the young. J. Am. Coll. Cardiol. 2007;49(2):240–246. doi: 10.1016/j.jacc.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 23.Tseng Z.H., Olgin J.E., Vittinghoff E., Ursell P.C., Kim A.S., Sporer K., et al. Prospective countywide surveillance and autopsy characterization of sudden cardiac death. Circulation. 2018;137(25):2689–2700. doi: 10.1161/CIRCULATIONAHA.117.033427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kramer M.C.A., Rittersma S.Z.H., de Winter R.J., Ladich E.R., Fowler D.R., Liang Y.H., et al. Relationship of thrombus healing to underlying plaque morphology in sudden coronary death. J. Am. Coll. Cardiol. 2010;55(2):122–132. doi: 10.1016/j.jacc.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 25.City of Chicago Chicago Ward, community area and neighborhood maps. https://www.chicago.gov/city/en/depts/dgs/supp_info/citywide_maps.html [Internet]. [cited 2021 Nov 14]. Available from.
- 26.City of Chicago Chicago Health Atlas. https://chicagohealthatlas.org/indicators [Internet]. [cited 2021 Nov 14]. Available from.
- 27.Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry CDC/ATSDR Social Vulnerability Index. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html [Internet]. [cited 2021 Dec 5]. Available from.
- 28.Flanagan B.E., Gregory E.W., Hallisey E.J., Heitgerd J.L., Lewis B. A social vulnerability index for disaster management. J. Homel. Secur. Emerg.Manag. 2011;8(1) [Google Scholar]
- 29.United States Census Bureau County population by characteristics: 2010-2019. https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-detail.html [Internet]. [cited 2021 Dec 5]. Available from.
- 30.Sidney S., Lee C., Liu J., Khan S.S., Lloyd-Jones D.M., Rana J.S. Age-adjusted mortality rates and age and risk-associated contributions to change in heart disease and stroke mortality, 2011–2019 and 2019–2020. JAMA Netw. Open. 2022;5(3) doi: 10.1001/jamanetworkopen.2022.3872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orsi J.M., Margellos-Anast H., Whitman S. Black-White health disparities in the United States and Chicago: a 15-year progress analysis. Am. J. Public Health. 2011;100(2):349–356. doi: 10.2105/AJPH.2009.165407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Margellos H., Silva A., Whitman S. Comparison of health status indicators in Chicago: are Black-White disparities worsening? Am. J. Public Health. 2004;94(1):116–121. doi: 10.2105/ajph.94.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]