Abstract
As countries continue the third year of the pandemic, we believe that there has been unfair attention to COVID-19 vaccine efficacy and safety, while tacitly ignoring serious challenges with vaccine uptake, without which vaccination may not be effective against the spread of COVID-19. While several studies have been published on COVID-19 vaccine hesitancy, there remains a need to conduct a comprehensive global analysis of vaccine hesitancy. We conducted a scoping review of 60 studies published globally on vaccine hesitancy and acceptance. We conducted a qualitative analysis to identify motivators and barriers to vaccination across several cultural and demographic contexts. We found the following factors to be relevant in any discussion about addressing or minimizing vaccine hesitancy: risk perceptions, trust in health care systems, solidarity, previous experiences with vaccines, misinformation, concerns about vaccine side effects and political ideology. We combine our insights from this comprehensive review of global literature to offer an important and practical discussion about two strategies that have been used to improve vaccine uptake: (i) communication and education and (ii) vaccine rollout and logistics.
Keywords: COVID-19, SARS-CoV-2, pandemic planning, scoping review, vaccine hesitancy
BACKGROUND
The COVID-19 pandemic has caused major changes to systems, practices, policies and routines. As countries continue the third year of the pandemic, nationwide prevention efforts have considered the inclusion of vaccination as a part of a multipronged approach to curb the spread of COVID-19 for at least 1 year. The increased attention toward vaccination as a prevention method has been promoted by studies showing the high effectiveness of at least 14 vaccine candidates, all of which are being used to inoculate populations in nations around the world today (Anand et al., 2021).
While vaccine development is a considerable feat, only recently has there been considerable attention to COVID-19 vaccine hesitancy. We know that vaccine hesitancy rates are increasing worldwide over time (Dubé et al., 2021), and several research studies have attempted to delineate the factors that promote vaccine hesitancy, rejection and delay (Majid and Ahmad, 2020). In a previously published essay, we recommended the consideration of vaccine hesitancy in policy planning alongside the development and approval of vaccine candidates (Ahmad et al., 2020). We predicted that vaccine hesitancy would prove to be a hurdle in optimizing the uptake and acceptance of COVID-19 vaccines. We have also conducted a comprehensive synthesis of vaccine hesitancy from past pandemics and global outbreaks (Truong et al., 2021), and found unfair attention on vaccine efficacy and safety, while tacitly ignoring vaccine uptake, without which vaccination may not be effective against the spread of COVID-19. Today, we see the real-world outcomes of vaccine hesitancy and rejection. For example, at the end of January 2021, protestors caused the temporary closure of the largest vaccination site in California (The Associated Press Staff, 2021).
An increasing number of studies have looked at vaccine hesitancy in a variety of populations, contexts and countries. It is more imperative than ever before to synthesize this evidence with a specific lens on how vaccine hesitancy differs across contexts. We conducted this scoping review to examine the various factors that promote COVID-19 vaccine hesitancy and acceptance. We provide an overall picture of the literature as well as key differences across a range of characteristics (i.e. age, education level and countries). Finally, we use this opportunity to outline the implications of our research for ongoing vaccine administration programs. Our review both examines vaccine hesitancy in the current climate and highlights important topics that we believe might arise as countries shift to postpandemic recovery and mass vaccination.
METHODS
Approach
We conducted a scoping review using Arksey and O’Malley’s (Arksey and O’Malley, 2005) methodological framework that comprises of six steps: scoping, searching, screening, data extraction, data analysis and optional stakeholder consultation. Due to the rapid need for this research, we did not conduct an optional stakeholder consultation, however, we included two physicians on our research team and researchers who have published empirical studies on vaccine hesitancy.
Search and screening
We executed a database search on 4 January 2021, on MEDLINE, PsychINFO, Embase, Global Health, CINAHL and the Web of Science. We used the systematic search strategy from a previously published systematic review but repurposed it to specify vaccine hesitancy toward COVID-19 vaccines (Majid and Ahmad, 2020). Our search strategy can be found in Additional File 1. We conducted title and abstract and full-text screening in pairs with verification. We were most interested in articles of any empirical study design (i.e. quantitative, qualitative or mixed methods) on vaccine hesitancy and acceptance. Our full list of eligibility criteria can be found in Table 1.
Table 1:
Eligibility criteria
| Inclusion | Exclusion |
|---|---|
| • Primary quantitative, qualitative and mixed-methods studies • The primary aim of studies may include measuring the prevalence of COVID-19 vaccine hesitancy or attitudes to vaccines willingness to participate in vaccine trials or examining the motivations to reject or delay vaccination • Studies on general perceptions, attitudes or behaviors toward COVID-19 vaccines |
• Commentaries, editorials, abstracts and evidence syntheses • Any articles (of any design) on vaccine hesitancy pertaining to non-COVID-19 vaccines including vaccines for other coronaviruses • Any articles pertaining to the cost, accessibility and convenience of COVID-19 vaccines • Articles on how COVID-19 affects routine vaccination rates |
Data extraction and analysis
We retrieved the study and participant characteristics of all included studies. We retrieved the following: author (year of publication), the title of study, research objectives, country of publication, vaccine name, study design, data collection methods, number and type of participants, eligibility criteria, the age range of participants, ethnicity of participants, education level of participants and the proportion of males. We conducted descriptive statistics of these characteristics to provide a holistic view of the study types and participant populations. This information was used to determine how vaccine hesitancy differed across several countries and contexts. We then conducted thematic analysis on the findings of included studies (Clarke and Braun, 2014). We adopted a staged open coding process that involved a pilot coding phase of 10 articles to create a coding schema. We used this schema to develop a set of coding templates that represented the themes and subthemes of included studies. We used the following templates to organize data from the remaining studies: overall proportions and demographic factors, motivators to vaccination, barriers to vaccination and strategies or recommendations. We then reviewed all remaining studies in pairs to find any data relevant to the themes mentioned previously. Once complete, one member of the research team reviewed each theme and developed a narrative summary that was critically reviewed by the rest of the research team. The primary author then reviewed all summaries and integrated them into one findings section, which was reviewed by the research team.
RESULTS
Search results
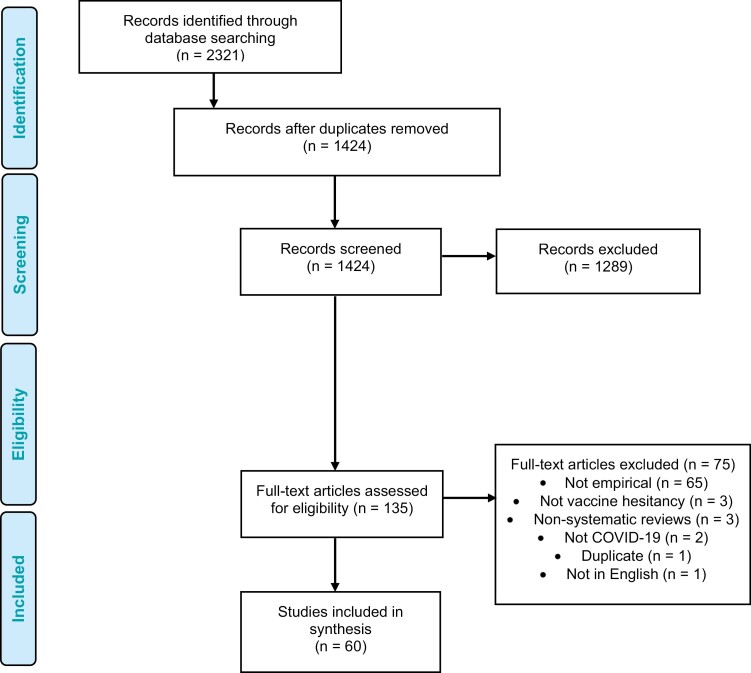
We screened the title and abstracts of 1424 studies after the removal of 897 duplicates. We excluded 1289 studies because they were not eligible for inclusion. We conducted full-text screening on 135 studies, of which we excluded 75 for various reasons shown in Figure 1. In this review, we analyzed 60 studies.
Fig. 1:
Screening and selection process.
Motivators of vaccination
We found several motivators that encouraged the acceptance of COVID-19 vaccines among study participants. These factors included the following: higher risk perception toward COVID-19; trust in the health care system; solidarity (i.e. a prosocial concern for others driven by the desire for a return to ‘normal life’) and a ‘left-leaning’ or ‘liberal’ political ideology.
Higher risk perception toward COVID-19
Thirteen included studies demonstrated a positive correlation between higher risk perceptions toward COVID-19 and vaccine acceptance (Detoc et al., 2020; Dror et al., 2020; Graffigna et al., 2020; Prati, 2020; Reiter et al., 2020; Salali and Uysal, 2020; Wang et al., 2020; Ward et al., 2020; Williams et al., 2020; Wong et al., 2020; Gagneux-Brunon et al., 2021; Guidry et al., 2021; Leng et al., 2021). We found that participants’ risk perception was influenced by the following three specific factors: being in contact with someone who had experienced COVID-19, having preexisting medical conditions and belonging to an older age group. Interactions with individuals who contracted COVID-19 strengthened participants’ risk perception of COVID-19 being a severe and extremely infectious disease (Kreps et al., 2020). In their interactions, participants may have been exposed to the immediate and long-term effects of the virus firsthand. By appreciating the severity of COVID-19, participants developed an increased perceived risk of COVID-19 and, in turn, were more likely to accept a potential vaccine and other health interventions aimed at combatting COVID-19 such as physical distancing and mask-wearing (Miao et al., 2020).
Additionally, participants in included studies with preexisting medical illnesses and older individuals were more likely to accept vaccines (Sarasty et al., 2020; Williams et al., 2020). For example, participants who had chronic lung diseases showed an increased risk perception because of their higher mortality risk from COVID-19 (Williams et al., 2020). This cross-sectional survey of UK adults found an increased perceived risk perception to COVID-19 motivated individuals to vaccinate due to a fear of fatal complications and mortality (Williams et al., 2020).
Trust in the health care system
Another significant motivator of vaccine acceptance was trust in the health care system and allopathic health care providers. In seven studies, trusting allopathic providers and the health care system was the primary factor that encouraged vaccine acceptance (Abu-Farha et al., 2020; Al-Mohaithef and Padhi, 2020; Bell et al., 2020; Kreps et al., 2020; Lazarus et al., 2021; Malik et al., 2020; Prati, 2020; Reiter et al., 2020; Wang et al., 2020). Multiple factors determined participants’ trust in the health care system, including positive interactions with health care providers, previous acceptance of vaccines and a belief in the natural origin of SARS-CoV-2.
Positive interactions with health care providers promoted trust between participants and the health care system. In Freeman’s study, adults from the UK described positive interactions as experiencing a nonjudgmental and supportive environment (Freeman et al., 2020). This environment was created through health care providers going ‘out of their way’ to ensure that they recognized and addressed patients’ concerns (Freeman et al., 2020). These interactions contributed to a strong and trusting patient–provider relationship, which bolstered trust in COVID-19 vaccine recommendations (Freeman et al., 2020; Prati, 2020).
Additionally, acceptance of the COVID-19 vaccine was found to be associated with the acceptance of vaccines for other diseases in the past (Bell et al., 2020; Dong et al., 2020; Palamenghi et al., 2020; Leng et al., 2021). This association was particularly evident in individuals who were previously vaccinated against influenza (Dror et al., 2020; Grech et al., 2020a, 2020b; Gagneux-Brunon et al., 2021; Kose et al., 2021). Previous vaccine acceptance also demonstrated an established trust in the health care system and allopathic providers. High levels of preexisting trust in vaccines and those that manufactured them increased participants’ confidence in the vaccine development process (Goldman et al., 2020b, 2020c; Gagneux-Brunon et al., 2021; Kose et al., 2021).
Participants in one study that surveyed English and Turkish adults found that participants’ trust in the health care system was due to their belief that COVID-19 originated ‘naturally’ (Salali and Uysal, 2020). These participants were less likely to believe in conspiracy theories concerning the artificial manufacturing of COVID-19 (Salali and Uysal, 2020). They were also more likely to feel that the government had their best interests in mind and was not part of a larger conspiracy (Salali and Uysal, 2020). In Salali et al.’s study, the vaccine acceptance rate was 26% higher in Turkey and 63% higher in the UK among participants who believed in the natural origin of COVID-19 compared with those who believed that it was manufactured artificially.
Solidarity
A sense of solidarity and social responsibility to help end the COVID-19 pandemic was a significant driver of vaccine acceptance in 11 studies (Barello et al., 2020; Bell et al., 2020; Goldman et al., 2020a, 2020c; Pogue et al., 2020; Reiter et al., 2020; Sherman et al., 2020; Williams et al., 2020; Leng et al., 2021; Jung and Albarracín 2021). This sense of solidarity stemmed from the following three motivators: protecting family members and other community members from COVID-19, achieving a sense of normality in everyday life and the influence of social groups and personal beliefs toward vaccines. Participants in seven studies stated that community and family members’ protection was the primary motivator for vaccinating against COVID-19 (Barello et al., 2020; Bell et al., 2020; Goldman et al., 2020c; Pogue et al., 2020; Reiter et al., 2020; Sherman et al., 2020; Williams et al., 2020). Included studies mentioned three significant factors that fostered prosocial concern: having children, regularly interacting with populations with high susceptibility to COVID-19 and living in lower population-dense areas.
Participants in included studies who had children were more likely to vaccinate their children and accept changes in vaccine manufacturing regulations to accelerate the development of COVID-19 vaccines (Goldman et al., 2020a, 2020c). In one study, surveying caregivers in the USA, Canada, Israel, Japan, Spain and Switzerland, 86% of caregivers stated protection as the primary reason to vaccinating their children (Goldman et al., 2020c). Individuals with children may feel that their children have an increased susceptibility to severe disease and as a result may be more accepting of vaccinating themselves and/or their children.
Similarly, individuals who interacted with populations with high susceptibility to COVID-19 were more likely to vaccinate (Bell et al., 2020). These included essential workers, individuals who interacted with children and older individuals regularly, and health care workers who managed at-risk patients (Bell et al., 2020). These individuals felt that it was their responsibility to protect those they interacted with through vaccination. Campaigns aimed at increasing individual awareness of potentially spreading COVID-19 to disease-susceptible acquaintances may foster prosocial concern in the general population (Bell et al., 2020).
Another factor that determined participants’ prosocial concern for community members was their neighbourhood’s population density (Jung and Albarracín 2021). In Jung’s study, a nationally representative longitudinal survey of participants from the USA demonstrated that people living in low-dense areas were more concerned with spreading disease in their communities, which increased the likelihood of vaccine acceptance (Jung and Albarracín 2021). Individuals in lower population-dense areas felt that their decision to vaccinate had a significant impact on the community’s overall health compared with participants in areas with higher density (Jung and Albarracín 2021).
Achieving a sense of normality in everyday life was another factor that contributed to a sense of solidarity among participants to vaccinate (Bell et al., 2020; Goldman et al., 2020c). Participants mentioned the importance of helping their children resume their regular social lives in school as a motivator to vaccinate (Bell et al., 2020; Goldman et al., 2020c). Strategies aimed at encouraging individuals to vaccinate to return to a more ‘normal’ lifestyle may increase COVID-19 vaccine acceptance (Bell et al., 2020).
Belonging to certain social groups also played a significant role in influencing COVID-19 vaccine acceptance (Leng et al., 2021). In one survey of Chinese adults, COVID-19 vaccination acceptance rates were notably higher in participants with vaccine-accepting acquaintances (Leng et al., 2021). Vaccination acceptance rates increased by 12.8% when the proportion of participants’ vaccinated acquaintances rose from 30 to 90% (Leng et al., 2021). Vaccine-accepting social groups may promote positive messages of herd immunity and solidarity to participants through peer influence. Strategies that promote the dissemination of positive COVID-19 vaccine among these social groups through community leaders and members may increase vaccine acceptance at the community level.
‘Left-leaning’ or ‘liberal’ political ideology
When it came to political ideology and its influence on vaccine acceptance, five studies demonstrated an increased acceptance of COVID-19 vaccination among participants with a ‘left-leaning’ political ideology (Kreps et al., 2020; Largent et al., 2020; Reiter et al., 2020; Ward et al., 2020).
Barriers to vaccination
We found several barriers that overlapped with motivators to vaccinate. We discuss the following barriers: lower risk perception, previous experiences with vaccines, misinformation and misconceptions, side effects and vaccine efficacy and ‘right-leaning’ or ‘conservative’ political ideology.
Lower risk perceptions
Lower risk perceptions were identified as a barrier to vaccination in seven studies (Bell et al., 2020; Fisher et al., 2020; Reiter et al., 2020; Salali and Uysal, 2020; Sherman et al., 2020; Smith and Reiss, 2020; Kose et al., 2021) Participants in included studies stated how they viewed the harms associated with vaccines outweighed the potential complications of contracting COVID-19 (Fisher et al., 2020; Reiter et al., 2020). This decreased perception of disease severity was linked to a lower likelihood of vaccine acceptance (Fisher et al., 2020; Sherman et al., 2020; Smith and Reiss, 2020). In Fisher’s study, participants from the USA were more likely to be unsure about vaccinating, and less likely to believe that they will acquire COVID-19 (Fisher et al., 2020). This decreased risk perception toward COVID-19 among participants stemmed primarily from the following two beliefs: a belief that they were healthy and that their natural immunity would effectively combat COVID-19, and mistrust in information from governments and other health authorities on the severity of COVID-19.
Three studies reported that being in good health was a barrier to vaccination (Bell et al., 2020; Sherman et al., 2020; Kose et al., 2021). In Sherman et al.’s study, vaccination intention was lower in participants who believed that COVID-19 vaccines were only necessary for those at risk of serious illness; these participants did not believe that they were a part of this group (Sherman et al., 2020). Furthermore, vaccine skeptics may not believe in the need to vaccinate because of a belief that their natural immunity would protect them (Bell et al., 2020; Kose et al., 2021).
Another factor that decreased participants’ risk perception of COVID-19 was lower trust in information provided to them regarding its effects. Participants felt that the disease was not as severe as governments and pharmaceutical companies proclaimed, which decreased perceptions of risk (Smith and Reiss, 2020). A potential reason for mistrust in COVID-19 information from health authorities was explored in Salali’s study, which demonstrated that individuals in countries with lower life expectancy and higher mortality risk showed increased risk perception and mistrust of social groups (Salali and Uysal, 2020).
Past experiences with vaccines
Data on how past experiences encouraged vaccine rejection or delay were mentioned in four studies (Bell et al., 2020; Fisher et al., 2020; Goldman et al., 2020c; Grech and Gauci, 2020). Up to 6% of survey respondents in one study stated that they would refuse a COVID-19 vaccine because they or their child had previously been infected with COVID-19 (Bell et al., 2020). Moreover, participants who had not received an influenza vaccine in the previous year were nearly 100% less likely to accept a potential COVID-19 vaccine (Fisher et al., 2020). Caregivers in two studies were hesitant toward the COVID-19 vaccine because they generally held an antivaccine stance toward all vaccines (Goldman et al., 2020c; Grech and Gauci, 2020).
Misinformation and misconceptions
Twenty-one studies found that conspiracy theories encouraged vaccine hesitancy (Basch et al., 2020; Bell et al., 2020; Čavojová et al., 2020; Earnshaw et al., 2020; Freeman et al., 2020; Mouchtouri et al., 2020; Neumann-Böhme et al., 2020; Palamenghi et al., 2020; Pogue et al., 2020; Prati, 2020; Romer and Jamieson, 2020; Salali and Uysal, 2020; Sarasty et al., 2020; Sherman et al., 2020; Smith and Reiss, 2020; Taylor et al., 2020; Williams et al., 2020; Bogart et al., 2021; Guidry et al., 2021; Marcec et al., 2021; Teovanović et al., 2021). Belief in the dangers of the measles–mumps–rubella vaccine was a strong mediator of the relationship between conspiracy beliefs and vaccine intention (Romer and Jamieson, 2020). Moreover, 17% of survey respondents cited low trust in vaccines, science or the medical profession as a reason for vaccine refusal (Bell et al., 2020; Sarasty et al., 2020).
The following conspiracy theories were found among participants (Freeman et al., 2020; Palamenghi et al., 2020; Pogue et al., 2020; Romer and Jamieson, 2020; Bogart et al., 2021): the virus was a ‘hoax’; the government was deliberately withholding information from the public; the virus was spread deliberately to reduce population size; the virus was a ploy to increase control over the public; the spread of virus was meant to increase the wealth of wealthy individuals; the virus spread was intended to destabilize a specific country or economy (i.e. the virus was created by China to ‘destroy’ the West); the virus was created by the USA and WHO to be used as a bioweapon; the elite and billionaires such as Bill Gates created the virus to implement a ‘one-world’ government; the virus was meant to be used by a government to create a police state; the virus was created by the 5G network; the virus was created to ensure that everyone was vaccinated; the WHO already has a vaccine but is withholding it from the general population; and antibody testing will harvest DNA. The most popular theory, held by 15.1% of participants in one study, was that the virus was created by humans (Freeman et al., 2020).
One study indicated that while mass media generally framed COVID-19 vaccination in a positive light, as more information—and misinformation—about the vaccine became available, positive sentiment toward vaccines eroded, raising vaccine fear and hesitancy (Sherman et al., 2020). Interestingly, studies on social media consumption and vaccine attitudes found that a small amount of exposure to antivaccination attitudes on social media influenced vaccination attitudes (Salali and Uysal, 2020; Smith and Reiss, 2020). Moreover, a lack of up-to-date information on vaccines was cited by participants’ who refused to accept the vaccine for their children and themselves (Bell et al., 2020; Mouchtouri et al., 2020; Sarasty et al., 2020; Teovanović et al., 2021).
Through network analysis, a study found that the belief that COVID-19 was exaggerated by officials and the government was associated with a disregard for physical distancing, poor hand hygiene and antivaccination attitudes (Taylor et al., 2020; Teovanović et al., 2021). One study indicated that misinformation was associated with decreased trust in scientific research (Palamenghi et al., 2020). Reliance on mainstream television was a positive predictor of vaccination (Romer and Jamieson, 2020), and notably, the belief that the media exaggerated the risks of contracting COVID-19 was negatively associated with willingness to receive a COVID-19 vaccination (Williams et al., 2020). Moreover, the unfortunate global success of the antivaccination movement was heavily reliant on social media, which provided a convenient and inexpensive means of spreading misinformation (Marcec et al., 2021). For instance, in one study several conspiracy videos on the vaccine received a total of 647 746 views (Basch et al., 2020).
Younger people, people of color, people of other ethnicities and people from the American Southwest and West were more likely to believe in conspiracies in one study from the USA (Earnshaw et al., 2020). Black participants were more hesitant to accept COVID-19 vaccines than White or Hispanic participants in another study from the USA (Guidry et al., 2021). This disparity could be attributed to the Black community’s increased distrust of the health care system because of historical and ongoing systemic racism (Bogart et al., 2021; Guidry et al., 2021).
Side effects and vaccine efficacy
Eighteen studies discussed side effects and vaccine efficacy (Bell et al., 2020; Dror et al., 2020; Fisher et al., 2020; Goldman et al., 2020c; Grech et al., 2020a, 2020b; Kreps et al., 2020; Neumann-Böhme et al., 2020; Pogue et al., 2020; Wang et al., 2020; Ward et al., 2020; Williams et al., 2020; Wong et al., 2020; Akarsu et al., 2021; Guidry et al., 2021; Kose et al., 2021; Leng et al., 2021; Marcec et al., 2021). In Russia, 19% of participants said there was no need for a COVID-19 vaccine, 18% were concerned about vaccine effectiveness, 11% were not fully informed about the new vaccine, 9% believed that the vaccine was dangerous, and 9% cited the negative impact of vaccines on the immune system as a reason to not vaccinate (Marcec et al., 2021). Moreover, concerns about vaccine safety and its side effects were a major impediment to vaccination decision-making, particularly for newly introduced, rapidly developed vaccines that may not have been thoroughly tested in the real world (Bell et al., 2020; Dror et al., 2020; Fisher et al., 2020; Goldman et al., 2020c; Grech et al., 2020a; Kreps et al., 2020; Pogue et al., 2020; Wang et al., 2020; Williams et al., 2020; Wong et al., 2020; Akarsu et al., 2021; Kose et al., 2021). A common concern in included studies appeared to be that a COVID-19 vaccine was experimental, with no studies on long-term side effects, and that the vaccine may not be safe for certain groups, such as pregnant women, people with preexisting conditions such as multiple sclerosis, and people with several allergies (Neumann-Böhme et al., 2020). Perceptions of vaccine ineffectiveness and side effects were also influenced by participants’ understanding of the limited duration of vaccine protection, and the proportion of their acquaintances who were vaccinated (Neumann-Böhme et al., 2020; Guidry et al., 2021; Leng et al., 2021). For instance, decreased vaccine uptake occurred when vaccines were perceived to be less effective, had a high risk of adverse side effects, was mandatory, not free, required multiple doses, and protected people for short durations (Leng et al., 2021).
Having doubts regarding vaccine efficacy, influenced by the idea that the virus mutated quickly, or by making comparisons with the influenza vaccine was another barrier to vaccine uptake (Ward et al., 2020). In one study, more than half of participants were concerned about potential vaccine side effects, with women (36%) being more concerned than men (19%) (Neumann-Böhme et al., 2020). Additionally, participants were more concerned about the long-term compared to the short-term side effects (Grech et al., 2020b). Some participants believed that the public was duped into believing that vaccines were effective since they believed that vaccine safety data were fabricated (Freeman et al., 2020). Furthermore, some participants believed that vaccines were harmful to children and that this information was withheld from the public (Freeman et al., 2020).
‘Right-leaning’ or ‘conservative’ political ideology
‘Right-leaning’ political ideology was mentioned by six studies (Freeman et al., 2020; Kreps et al., 2020; Largent et al., 2020; Pogue et al., 2020; Reiter et al., 2020; Ward et al., 2020). The location where vaccines were developed affected individuals’ attitudes toward vaccination (Pogue et al., 2020). For instance, people in the USA were less likely to vaccinate if they were developed outside of the USA (Kreps et al., 2020). Those with conservative/traditional beliefs viewed themselves to be at a lower risk of COVID-19, reducing their perceived need to vaccinate (Reiter et al., 2020). Individuals who identified themselves as Republicans or Independents were significantly less likely to vaccinate than participants who described themselves as Democrats (Largent et al., 2020). Furthermore, ‘right-leaning’ participants were more likely to believe in COVID-19 conspiracies, and refuse a COVID-19 vaccine if provided (Freeman et al., 2020; Ward et al., 2020).
DISCUSSION
In this paper, we analyzed 60 studies from a variety of countries to identify the motivators and barriers to COVID-19 vaccine acceptance. We were able to draw several factors that promote vaccine acceptance or rejection, including risk perceptions, trust in health care systems, solidarity, previous experiences with vaccines, misinformation, concerns about vaccine side effects and political ideology. We switch gears in the discussion section to discuss the implications of these findings for developing strategies to combat vaccine rejection and delay. We discuss two strategies that can aid in improving vaccine uptake: (i) communication and education and (ii) vaccine rollout and logistics.
Communication and education
Communicating with and educating the general public about vaccination is integral for achieving high COVID-19 vaccine uptake (Barello et al., 2020; Basch et al., 2020; Bell et al., 2020; Čavojová et al., 2020; Dror et al., 2020; Earnshaw et al., 2020; Fisher et al., 2020; Freeman et al., 2020; Goldman et al., 2020b, 2020c; Graffigna et al., 2020; Grech et al., 2020a; Kreps et al., 2020; Malik et al., 2020; Neumann-Böhme et al., 2020; Palamenghi et al., 2020; Peretti-Watel et al., 2020; Pogue et al., 2020; Prati, 2020; Reiter et al., 2020; Romer and Jamieson, 2020; Schoch-Spana et al., 2020; Wang et al., 2020; Wong et al., 2020; Bogart et al., 2021; Guidry et al., 2021; Jung and Albarracín 2021; Lazarus et al., 2021; Marcec et al., 2021). In a UK study conducted by Bell et al. (Bell et al., 2020), authors suggested that it was incumbent upon the government and public health officials to reassure the public about vaccine safety in a timely and transparent manner should any safety concerns about the vaccine arise. Moreover, early communication was key in understanding the factors that may impede vaccine acceptability and strategizing how to stem these factors (Bell et al., 2020). Reassuring the public was especially important when a vaccine was to become quickly available, predicting greater hesitancy in the event information provision lagged vaccine availability (Neumann-Böhme et al., 2020). Based on their findings from a multicountry European survey, they also stated the need to emphasize the social benefits of vaccines so that the public can ‘weigh the public health dimension more heavily in their decision whether to vaccinate’ (Neumann-Böhme et al., 2020). As our findings indicate, bolstering prosocial concern, particularly among individuals residing in dense populations, may prove to be crucial in increasing global vaccination rates (Jung and Albarracín 2021).
Fisher et al. (Fisher et al., 2020) emphasized the importance of ‘transparent reporting’ of vaccine safety as it was found in their study that concerns surrounding safety and efficacy were common reasons that explained vaccine hesitancy. The call for communication transparency regarding vaccine safety was similarly sounded by Lazarus et al. (Lazarus et al., 2021), who after a survey spanning nineteen countries concluded that ‘clear and consistent’ communication was needed when explaining how vaccines work as well as their safety and efficacy to bolster public confidence. Lazarus et al. (Lazarus et al., 2021) also emphasized the importance of ‘instilling public confidence’ in regulatory agency reviews on vaccine safety. However, Palamenghi et al. (Palamenghi et al., 2020) stressed the importance of encouraging public debates that allowed concerns surrounding safety to be expressed, and at the same time provide scientists and decision-makers the opportunity and space to directly address concerns. These debates may be possible with webinars to foster discussion, as was done recently by the Registered Nurses Association of Ontario in Canada. This webinar informed nurses about currently available information regarding COVID-19 vaccines and addressed common public misconceptions regarding vaccination (https://rnao.ca/covid19/vaccine). Importantly, this forum also gave nurses the chance to ask questions in a nonjudgmental environment that encouraged discussion (https://rnao.ca/covid19/vaccine). Leveraging social media channels, maintaining an online presence, using diverse experts and scientists, and having health care providers model recommended behaviors are among the many strategies that have worked to communicate COVID-19 vaccination information to the public (Siegrist and Zingg, 2014; Abrams and Greenhawt, 2020). However, social media can be used to spread misinformation and counternarratives; governments and health officials may use these social media platforms to recognize these narratives early and create individualized strategies to address them before dissemination (Pollett and Rivers, 2020). Social media platforms have also implemented fact-checking algorithms to fight the spread of information (Meta Business Help Center, 2022).
Similar to calls for clear and important messaging about vaccine safety and efficacy, studies also noted that educational campaigns and initiatives were imperative for increasing the uptake of COVID-19 vaccines. The study by Barello et al. (Barello et al., 2020) described how effective a multidisciplinary educational curriculum about vaccine preventative behaviors can be for communities. Furthermore, the same authors emphasized teaching complex health issues in a culturally affirmative manner to students about the barriers to vaccination (Barello et al., 2020). Countries have introduced various campaigns to improve the acceptance and uptake of vaccines; for example, a campaign by the Government of Canada used the ripple effect idea to emphasize how vaccination can influence the health and well-being of everyone (Public Health Agency of Canada, 2021); and the United States Department of Health and Human Services has a website dedicated to a COVID-19 Public Education Campaign (United States Department of Health and Human Services, 2022).
Studies have also advocated for educating health care providers to prevent and reduce vaccine hesitancy. A Greek study on the attitudes of health care workers during the pandemic suggested the need for a ‘national strategy and health education program’ to enhance the immunization of health care providers against COVID-19 (Papagiannis et al., 2020). Educating health care providers, particularly on safety and efficacy, may optimize vaccination rates (Grech et al., 2020a). Studies have also stressed the importance of educating the public with evidence-based information to prevent vaccine-hesitant beliefs and behaviors. According to Čavojová et al. (Čavojová et al., 2020), scientific reasoning reduced ‘suspect beliefs’ surrounding COVID-19 vaccination in the public. Goldman et al. (Goldman et al., 2020b) also advocated for strategies that educate parents about the severity of COVID-19 to prevent low uptake rates for a potential COVID-19 vaccine for children. However, one study noted the need for a ‘careful balance’ between public education surrounding vaccination and coercion (Lazarus et al., 2021). Additionally, some studies posited that educational efforts could increase their effectiveness by being careful with the disseminating source and tailoring the message to the needs and preferences of diverse communities. This perspective was displayed in Malik et al. (Malik et al., 2020) where the study observed that participants held the highest levels of trust in COVID-19 information that came from health care professionals. Malik et al. (Malik et al., 2020) also adopted a culturally affirmative view by stating that educational efforts should particularly focus on communities of color and low-income groups, as these demographics are at ‘high risk’ of low vaccine uptake. As our findings indicate, low vaccine uptake already exists among communities of color in the UK and USA, and that concerted action is needed to increase vaccine uptake in those communities (Bell et al., 2020; Fisher et al., 2020).
Vaccine rollout and logistics
Included studies also emphasized the importance of vaccine development, rollout and logistics (Barello et al., 2020; Bell et al., 2020; Dong et al., 2020; Fisher et al., 2020; Goldman et al., 2020b; Graffigna et al., 2020; Grech et al., 2020b; Jazieh et al., 2020; Largent et al., 2020; Neumann-Böhme et al., 2020; Pogue et al., 2020; Sherman et al., 2020; Williams et al., 2020; Wong et al., 2020; Bogart et al., 2021; Borriello et al., 2021; Detoc et al., 2020; Guidry et al., 2021; Jung and Albarracín 2021; Kose et al., 2021). Studies included in this review highlighted the importance of developing strategies tailored to low-income groups and communities of color, especially since many have faced a greater number of challenges during the pandemic compared to other communities (Abdelhafiz et al., 2020; Pogue et al., 2020). These communities have experienced systemic racism for decades, and therefore, require interventions that empower and enable community members (Bogart et al., 2021).
Certain studies have also provided suggestions on ways to ease access to a COVID-19 vaccine to reduce vaccine hesitancy. Neumann-Böhme et al. (Neumann-Böhme et al., 2020) stressed that vaccines should be easily accessible and distributed equitably, and Borriello et al. (Borriello et al., 2021) mooted the idea that vaccines should be readily accessible at pharmacies, hospitals and physician clinics. Jean-Jacques and Bauchner (Jean-Jacques and Bauchner, 2021) identified the following four strategies to ensure equitable distribution of vaccines: prioritize vaccine distribution to zip codes most severely affected; partner with local health care institutions and community organizations; prioritize vaccine distribution to those who face mobility or other transportation barriers and simplify registration procedures. Some of these strategies have been implemented, for example, in Ontario, Canada (and other countries) where a greater number of vaccines are being allocated to the most populated and affected areas. Furthermore, the COVID-19 Vaccines Global Alliance (COVAX) co-led by the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi and the WHO and delivered by UNICEF aims for equitable accessing of vaccines to low- and middle-income countries (WHO, 2022). The WHO Strategy to Achieve Global COVID-19 Vaccination aims to vaccinate at least 40% of each country’s population by the end of 2022 and 70% by the middle of 2023 (WHO, 2021). This will be accomplished by prioritizing the delivery of vaccines to older adults and high-risk populations, followed by all adults and then adolescents (WHO, 2021).
Geographical factors are also essential to consider when improving vaccine accessibility; Jung et al. (Jung and Albarracín 2021) advocated for refining and improving rural health system infrastructure to achieve optimal vaccination rates in those areas. Interestingly, in a Chinese study conducted by Dong et al. (Dong et al., 2020), researchers found that vaccines with a longer duration of efficacy may increase vaccine acceptance among rural patients. This preference was due to a perceived lack of access to high-quality health care in rural and remote areas, further highlighting geographical discrepancies in the allocation of health care resources (Dong et al., 2020). There may be other strategies that improve vaccine uptake in rural communities; a regional analysis is necessary to formulate highly targeted approaches (Goldman et al., 2020c).
Studies also offered a wide range of other solutions in designing public vaccination programs. Neumann-Böhme et al. (Neumann-Böhme et al., 2020) stressed the need for a targeted approach aimed at women a gender-specific approach was advocated by these authors. Modi et al. (Modi et al., 2021) indicated how the initial exclusion of pregnant and lactating women from vaccination deployment strategies was ‘a throwback to a paternalistic era’ (Modi et al., 2021). There is still uncertainty whether there is sufficient justification for the continued exclusion of this group from public vaccination programs. Modi et al. (Modi et al., 2021) recommended a ‘presumption of inclusion’ of pregnant women and lactating women, especially because of the historical exclusion of this group from vaccination programs.
Directions for further research
Studies examined in this paper also raised some areas of possible research in order to mitigate vaccine-hesitant behaviors during this pandemic (Dong et al., 2020; Dror et al., 2020; Earnshaw et al., 2020). Some researchers supported the idea of monitoring the changing attitudes of people (Dong et al., 2020). Earnshaw et al. (Earnshaw et al., 2020) also advocated for research on the association between conspiracy theories and individual policy support. Dror et al. (Dror et al., 2020) recommended the need for research on the association between parenthood and vaccine hesitancy. Such a line of research can support the development of novel strategies that increase vaccine uptake.
Limitations of this review
This study conducted a comprehensive global review of 60 studies on COVID-19 vaccine hesitancy. However, the body of literature on this topic is growing will require an update to ensure that our understanding of COVID-19 vaccine hesitancy is accurate and consistent. Furthermore, included studies did not discuss access to COVID-19 vaccines, which previous research has hypothesized might influence COVID-19 vaccine hesitancy (Truong et al., 2021). Future research might consider examining the relationship between COVID-19 vaccine hesitancy and vaccine access.
Supplementary Material
Contributor Information
Umair Majid, Institute of Health Policy, Management, and Evaluation, University of Toronto, Toronto, ON, Canada.
Mobeen Ahmad, Department of Internal Medicine, Abington Memorial Hospital, Abington Jefferson Health, Abington, PA, USA.
Shahzadi Zain, Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON, Canada.
Adebisi Akande, Department of Biological Sciences, University of Toronto, Toronto, ON, Canada.
Fahham Ikhlaq, Department of Health and Society, University of Toronto, Toronto, ON, Canada.
Conflict of Interest
Umair Majid receives financial support from the Canadian Institutes of Health Research and the Government of Ontario, Canada. Neither party was involved in the design and conduct of this research.
REFERENCES
- Abdelhafiz, A. S., Mohammed, Z., Ibrahim, M. E., Ziady, H. H., Alorabi, M., Ayyad, M.et al. (2020) Knowledge, perceptions, and attitude of Egyptians towards the novel coronavirus disease (COVID-19). Journal of Community Health, 45, 881–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrams, E. M. and Greenhawt, M. (2020) Risk communication during COVID-19. The Journal of Allergy and Clinical Immunology: In Practice, 8, 1791–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Farha, R. K., Alzoubi, K. H. and Khabour, O. F. (2020) Public willingness to participate in COVID-19 vaccine clinical trials: a study from Jordan. Patient Preference and Adherence, 14, 2451–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad, M., Truong, J. and Majid, U. (2020) Let’s talk COVID-19 vaccine hesitancy. Longwoods. https://www.longwoods.com/content/26286//let-s-talk-covid-19-vaccine-hesitancy (last accessed 20 February 2021). [Google Scholar]
- Akarsu, B., Canbay Özdemir, D., Ayhan Baser, D., Aksoy, H., Fidancı, I. and Cankurtaran, M. (2021) While studies on COVID-19 vaccine are ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. International Journal of Clinical Practice, 75, e13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali, K. F., Whitebridge, S., Jamal, M. H., Alsafy, M. and Atkin, S. L. (2020) Perceptions, knowledge, and behaviors related to COVID-19 among social media users: cross-sectional study. Journal of Medical Internet Research, 22, e19913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Mohaithef, M. and Padhi, B. K. (2020) Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. Journal of Multidisciplinary Healthcare, 13, 1657–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand, U., Jakhmola, S., Indari, O., Chandra Jha, H., Chen, Z. S., Tripathi, V.et al. (2021) Potential therapeutic targets and vaccine development for COVID-19 management: a review on the recent update. Frontiers in Immunology, 12, 2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey, H. and O’Malley, L. (2005) Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32. [Google Scholar]
- Barello, S., Nania, T., Dellafiore, F., Graffigna, G. and Caruso, R. (2020) ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. European Journal of Epidemiology, 35, 781–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basch, C. H., Hillyer, G. C., Zagnit, E. A. and Basch, C. E. (2020) YouTube coverage of COVID-19 vaccine development: implications for awareness and uptake. Human Vaccines & Immunotherapeutics, 16, 2582–2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell, S., Clarke, R., Mounier-Jack, S., Walker, J. L. and Paterson, P. (2020) Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine, 38, 7789–7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biasio, L. R., Bonaccorsi, G., Lorini, C. and Pecorelli, S. (2021) Assessing COVID-19 vaccine literacy: a preliminary online survey. Human Vaccines & Immunotherapeutics, 17, 1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart, L. M., Ojikutu, B. O., Tyagi, K., Klein, D. J., Mutchler, M. G., Dong, L.et al. (2021) COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among Black Americans living with HIV. Journal of Acquired Immune Deficiency Syndromes (1999), 86, 200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borriello, A., Master, D., Pellegrini, A. and Rose, J. M. (2021) Preferences for a COVID-19 vaccine in Australia. Vaccine, 39, 473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Čavojová, V., Šrol, J. and Ballová Mikušková, E. (2020) How scientific reasoning correlates with health-related beliefs and behaviors during the COVID-19 pandemic? Journal of Health Psychology, 27, 534–547. [DOI] [PubMed] [Google Scholar]
- Clarke, V. and Braun, V. (2014) Thematic analysis. In Teo, T. (ed), Encyclopedia of Critical Psychology. Springer, New York, NY, pp. 1947–1952. [Google Scholar]
- Detoc, M., Bruel, S., Frappe, P., Tardy, B., Botelho-Nevers, E. and Gagneux-Brunon, A. (2020) Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine, 38, 7002–7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, D., Xu, R. H., Wong, E. L. Y., Hung, C. T., Feng, D., Feng, Z.et al. (2020) Public preference for COVID-19 vaccines in China: a discrete choice experiment. Health Expectations, 23, 1543–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A.et al. (2020) Vaccine hesitancy: the next challenge in the fight against COVID-19. European Journal of Epidemiology, 35, 775–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé, E., Ward, J. K., Verger, P. and MacDonald, N. E. (2021) Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annual Review of Public Health, 42, 175–191. [DOI] [PubMed] [Google Scholar]
- Earnshaw, V. A., Eaton, L. A., Kalichman, S. C., Brousseau, N. M., Hill, E. C. and Fox, A. B. (2020) COVID-19 conspiracy beliefs, health behaviors, and policy support. Translational Behavioral Medicine, 10, 850–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehoche, E. E., Adejoh, J., Idoko, J. and Madu, C. (2020) Preliminary survey on knowledge, attitudes, and practices about the COVID-19 pandemic among residents in North Central Nigeria. Borneo Journal of Pharmacy, 3, 121–129. [Google Scholar]
- Fisher, K. A., Bloomstone, S. J., Walder, J., Crawford, S., Fouayzi, H. and Mazor, K. M. (2020) Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Annals of Internal Medicine, 173, 964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman, D., Loe, B. S., Chadwick, A., Vaccari, C., Waite, F., Rosebrock, L.et al. (2020) COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychological Medicine, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagneux-Brunon, A., Detoc, M., Bruel, S., Tardy, B., Rozaire, O., Frappe, P.et al. (2021) Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. Journal of Hospital Infection, 108, 168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. D., Marneni, S. R., Seiler, M., Brown, J. C., Klein, E. J., Cotanda, C. P.et al. (2020a) Caregivers’ willingness to accept expedited vaccine research during the COVID-19 pandemic: a cross-sectional survey. Clinical Therapeutics, 42, 2124–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. D., Staubli, G., Cotanda, C. P., Brown, J. C., Hoeffe, J., Seiler, M.et al. (2020b) Factors associated with parents’ willingness to enroll their children in trials for COVID-19 vaccination. Human Vaccines & Immunotherapeutics, 17, 1607–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. D., Yan, T. D., Seiler, M., Cotanda, C. P., Brown, J. C., Klein, E. J.et al. (2020c) Caregiver Goldman willingness to vaccinate their children against COVID-19: cross sectional survey. Vaccine, 38, 7668–7673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graffigna, G., Palamenghi, L., Boccia, S. and Barello, S. (2020) Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: a mediation analysis. Vaccines, 8, 576–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grech, V., Bonnici, J. and Zammit, D. (2020a) Vaccine hesitancy in Maltese family physicians and their trainees vis-a-vis influenza and novel COVID-19 vaccination. Early Human Development, 105259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grech, V. and Gauci, C. (2020) Vaccine hesitancy in the University of Malta Faculties of Health Sciences, Dentistry and Medicine vis-a-vis influenza and novel COVID-19 vaccination. Early Human Development, 105258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grech, V., Gauci, C. and Agius, S. (2020b) Vaccine hesitancy among Maltese healthcare workers toward influenza and novel COVID-19 vaccination. Early Human Development, 105213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidry, J. P., Laestadius, L. I., Vraga, E. K., Miller, C. A., Perrin, P. B., Burton, C. W.et al. (2021) Willingness to get the COVID-19 vaccine with and without emergency use authorization. American Journal of Infection Control, 49, 137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jazieh, A. R., Coutinho, A. K., Bensalem, A., Alsharm, A. A., Errihani, H., Mula-Hussain, L. Y. I.et al. (2020) 1687P Oncologists knowledge, attitude and practice in COVID-19 pandemic and its negative impact on them: an international study. Annals of Oncology, 31, S998. [Google Scholar]
- Jean-Jacques, M. and Bauchner, H. (2021) Vaccine distribution—equity left behind? JAMA, 325, 829–830. [DOI] [PubMed] [Google Scholar]
- Jung, H. and Albarracín, D. (2021) Concerns for others increases the likelihood of vaccination against influenza and COVID-19 more in sparsely rather than densely populated areas. Proceedings of the National Academy of Sciences of the United States of America, 118, e2007538118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kose, S., Mandiracioglu, A., Sahin, S., Kaynar, T., Karbus, O. and Ozbel, Y. (2021) Vaccine hesitancy of the COVID-19 by health care personnel. International Journal of Clinical Practice, 75, e13917. [Google Scholar]
- Kovács, A., Oláh, A., Pakai, A., Inhoff, E., Far, G., Wirthné-Gyergyák, K.et al. (2020) PSU20 attitude of Hungarian adults towards emergency plans before COVID-19 outbreak in Hungary. Value in Health, 23, S741. [Google Scholar]
- Kreps, S., Prasad, S., Brownstein, J. S., Hswen, Y., Garibaldi, B. T., Zhang, B.et al. (2020) Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Network Open, 3, e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Vecchia, C., Negri, E., Alicandro, G. and Scarpino, V. (2020) Attitudes towards influenza vaccine and a potential COVID-19 vaccine in Italy and differences across occupational groups, September 2020. La Medicina del lavoro, 111, 445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Largent, E. A., Persad, G., Sangenito, S., Glickman, A., Boyle, C. and Emanuel, E. J. (2020) US public attitudes toward COVID-19 vaccine mandates. JAMA Network Open, 3, e2033324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, J. V., Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K.et al. (2021) A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27, 225–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng, A., Maitland, E., Wang, S., Nicholas, S., Liu, R. and Wang, J. (2021) Individual preferences for COVID-19 vaccination in China. Vaccine, 39, 247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majid, U. and Ahmad, M. (2020) The factors that promote vaccine hesitancy, rejection, or delay in parents. Qualitative Health Research, 30, 1762–1776. [DOI] [PubMed] [Google Scholar]
- Malik, A. A., McFadden, S. M., Elharake, J. and Omer, S. B. (2020) Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine, 26, 100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcec, R., Majta, M. and Likic, R. (2021) Will vaccination refusal prolong the war on SARS-CoV-2? Postgraduate Medical Journal, 97, 143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meta Business Help Center. (2022) About fact-checking on Facebook. https://www.facebook.com/business/help/2593586717571940?id=673052479947730 (last accessed 20 February 2021).
- Miao, F., Li, L., Li, R., Liu, S. and Du, X. (2020) PIN33 public health behaviour changes during the Covid-19 outbreak in China: a comparison in different risk groups. Value in Health Regional Issues, 22, S54. [Google Scholar]
- Modi, N., Ayres-de-Campos, D., Bancalari, E., Benders, M., Briana, D., Di Renzo, G. C.et al. (2021) Equity in coronavirus disease 2019 vaccine development and deployment. American Journal of Obstetrics and Gynecology, 224, 423–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouchtouri, V. A., Agathagelidou, E., Kofonikolas, K., Rousou, X., Dadouli, K., Pinaka, O.et al. (2020) Nationwide survey in Greece about knowledge, risk perceptions, and preventive behaviors for COVID-19 during the general lockdown in April 2020. International Journal of Environmental Research and Public Health, 17, 8854–8866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann-Böhme, S., Varghese, N. E., Sabat, I., Barros, P. P., Brouwer, W., van Exel, J.et al. (2020) Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. The European Journal of Health Economics, 21, 977–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamenghi, L., Barello, S., Boccia, S. and Graffigna, G. (2020) Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. European Journal of Epidemiology, 35, 785–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papagiannis, D., Malli, F., Raptis, D. G., Papathanasiou, I. V., Fradelos, E. C., Daniil, Z.et al. (2020) Assessment of knowledge, attitudes, and practices towards new coronavirus (SARS-CoV-2) of health care professionals in Greece before the outbreak period. International Journal of Environmental Research and Public Health, 17, 4925–4939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peretti-Watel, P., Seror, V., Cortaredona, S., Launay, O., Raude, J., Verger, P.et al. (2020) A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. The Lancet Infectious Diseases, 20, 769–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierantoni, L., Lenzi, J., Lanari, M., De Rose, C., Morello, R., Di Mauro, A.et al. (2021) Nationwide COVID-19 survey of Italian parents reveals useful information on attitudes to school attendance, medical support, vaccines and drug trials. Acta Paediatrica, 110, 942–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pogue, K., Jensen, J. L., Stancil, C. K., Ferguson, D. G., Hughes, S. J., Mello, E. J.et al. (2020) Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines, 8, 582–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollett, S. and Rivers, C. (2020) Social media and the new world of scientific communication during the COVID-19 pandemic. Clinical Infectious Diseases, 71, 2184–2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati, G. (2020) Intention to receive a vaccine against SARS-CoV-2 in Italy and its association with trust, worry and beliefs about the origin of the virus. Health Education Research, 35, 505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada. (2021) Government of Canada launches new “Ripple Effect” advertising campaign to encourage COVID-19 vaccination. Government of Canada. https://www.canada.ca/en/public-health/news/2021/05/government-of-canada-launches-new-ripple-effect-advertising-campaign-to-encourage-covid-19-vaccination.html (last accessed 20 February 2021). [Google Scholar]
- Reiter, P. L., Pennell, M. L. and Katz, M. L. (2020) Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine, 38, 6500–6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer, D. and Jamieson, K. H. (2020) Conspiracy theories as barriers to controlling the spread of COVID-19 in the US. Social Science & Medicine, 263, 113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salali, G. D. and Uysal, M. S. (2020) COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychological Medicine, 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarasty, O., Carpio, C. E., Hudson, D., Guerrero-Ochoa, P. A. and Borja, I. (2020) The demand for a COVID-19 vaccine in Ecuador. Vaccine, 38, 8090–8098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoch-Spana, M., Brunson, E. K., Long, R., Ruth, A., Ravi, S. J., Trotochaud, M.et al. (2020) The public’s role in COVID-19 vaccination: human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine, 39, 6004–6012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman, S. M., Smith, L. E., Sim, J., Amlôt, R., Cutts, M., Dasch, H.et al. (2020) COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Human Vaccines & Immunotherapeutics, 17, 1612–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist, M. and Zingg, A. (2014) The role of public trust during pandemics: implications for crisis communication. European Psychologist, 19, 23–32. [Google Scholar]
- Smith, T. C. and Reiss, D. R. (2020) Digging the rabbit hole, COVID-19 edition: anti-vaccine themes and the discourse around COVID-19. Microbes and Infection, 22, 608–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S., Landry, C. A., Paluszek, M. M., Rachor, G. S. and Asmundson, G. J. (2020) Worry, avoidance, and coping during the COVID-19 pandemic: a comprehensive network analysis. Journal of Anxiety Disorders, 76, 102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teovanović, P., Lukić, P., Zupan, Z., Lazić, A., Ninković, M. and Žeželj, I. (2021) Irrational beliefs differentially predict adherence to guidelines and pseudoscientific practices during the COVID-19 pandemic. Applied Cognitive Psychology, 35, 486–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Associated Press Staff. (2021) Anti-vaccine protesters temporarily shut down California vaccine site. CTV News. https://www.ctvnews.ca/health/coronavirus/anti-vaccine-protesters-temporarily-shut-down-california-vaccine-site-1.5289599 (last accessed 20 February 2021). [Google Scholar]
- Truong, J., Bakshi, S., Wasim, A., Ahmad, M. and Majid, U. (2021) What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promotion International, 37, daab105. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. (2022) COVID-19 Public Education Campaign: an initiative to increase confidence in COVID-19 vaccines and reinforce basic prevention measures. https://wecandothis.hhs.gov (last accessed 20 February 2021).
- Wang, J., Jing, R., Lai, X., Zhang, H., Lyu, Y., Knoll, M. D.et al. (2020) Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines, 8, 482–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, J. K., Alleaume, C., Peretti-Watel, P., Seror, V., Cortaredona, S., Launay, O.et al. (2020) The French public’s attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Social Science & Medicine, 265, 113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, L., Gallant, A. J., Rasmussen, S., Brown Nicholls, L. A., Cogan, N., Deakin, K.et al. (2020) Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. British Journal of Health Psychology, 25, 1039–1054. [DOI] [PubMed] [Google Scholar]
- Wong, L. P., Alias, H., Wong, P. F., Lee, H. Y. and AbuBakar, S. (2020) The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines & Immunotherapeutics, 16, 2204–2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021) Strategy to achieve global COVID-19 vaccination by mid-2022. COVID-19: Scientific Briefs. https://www.who.int/publications/m/item/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022 (last accessed 20 February 2021).
- World Health Organization. (2022) COVAX: working for global equitable access to COVID-19 vaccines. https://www.who.int/initiatives/act-accelerator/covax (last accessed 20 February 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.