Abstract
Background
COVID-19 vaccines have shown success in protecting people worldwide, although serious adverse effects have been reported in very rare cases.
Case summary
A 32-year-old male with a prior medical history of mild COVID-19 infection developed fulminant myocarditis five days after mRNA-1273 vaccination (first dose), which was confirmed using endomyocardial biopsy. He acutely developed respiratory failure and cardiogenic shock with ventricular tachycardia, but recovered completely with short-term high-dose steroid therapy and mechanical cardiac support, which is the recommended treatment for fulminant lymphocytic myocarditis.
Discussion
COVID-19 vaccine-induced myocarditis varies from mild to severe. In the present case, the patient was treated as for fulminant lymphocytic myocarditis and recovered relatively quickly. The mechanism of COVID-19 vaccine-associated myocarditis needs to be urgently investigated.
Keywords: mRNA-1273 vaccine, Myocarditis, COVID-19, Previous infection, Case report
Learning points.
This report helps to understand the clinical presentation, diagnostic investigations, and clinical course of fulminant myocarditis after COVID-19 vaccination.
Patients with fulminant myocarditis after COVID-19 vaccination might recover completely with short-term high-dose steroid therapy and mechanical cardiac support, as with fulminant lymphocytic myocarditis.
Introduction
COVID-19 vaccines have shown great success in protecting people worldwide, and the mRNA-1273 vaccine (Moderna, Cambridge, MA, USA) is one of the most widely used of these vaccines. Although there have been some reports of myocarditis after COVID-19 vaccination,1–5 it is rarely fulminant. Here, we report a case of fulminant myocarditis after mRNA-1273 vaccination in a young male with a previous COVID-19 infection.
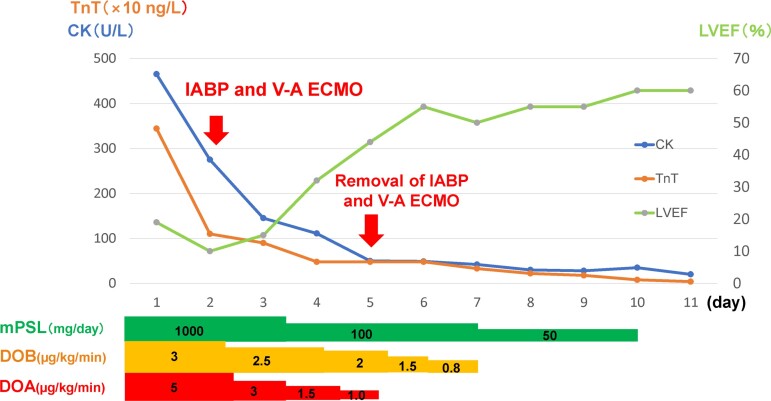
Clinical timeline. The patient’s clinical course and management during the acute phase of myocarditis. After starting mechanical cardiac support (MCS) and intravenous drugs, including methylprednisolone (mPSL), dopamine (DOA), and dobutamine (DOB), levels of creatine kinase (CK) and troponin T (TnT) decreased quickly, and the patient was weaned from MCS on day 5. Left ventricular ejection fraction (LVEF) improved on day 6 from 10 to 55%. IABP = intra-aortic balloon pump, VA-ECMO = venoarterial extracorporeal membrane oxygenation.
Timeline
Case presentation
A 32-year-old male was admitted for persistent fever (37.3°C) and upper abdominal pain 5 days after mRNA-1273 vaccination (first dose). Vital signs evaluation showed a blood pressure of 88/60 mmHg, heart rate of 133 beats/min, tachypnoea (37 breaths/min), and oxygen saturation of 99% on room air. He had a prior medical history of COVID-19 infection 9 months earlier.
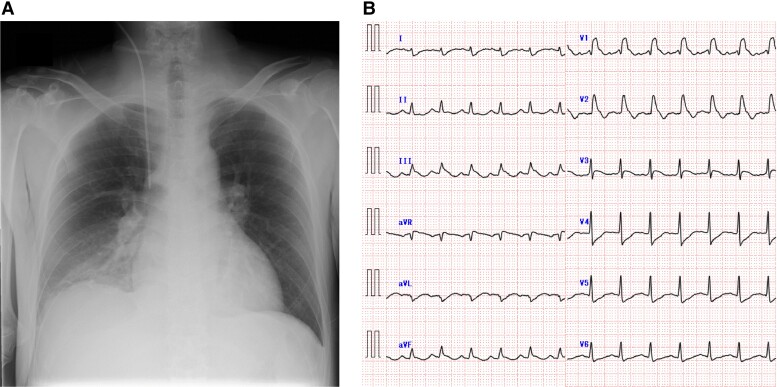
On arrival at the hospital, laboratory blood tests showed elevated levels of inflammatory markers like white blood cells at 9400/μL (normal range, 3300–8600/µL) and C-reactive protein at 1.35 mg/dL (normal range, <0.14 mg/dL) and cardiac biomarkers like creatine kinase at 465 U/L (normal range, 41 to 153 U/L) and troponin T at 3444 ng/L (normal range, <14 ng/L). Chest X-ray showed cardiomegaly without obvious pulmonary congestion or pleural effusion (Figure 1A). Electrocardiogram showed sinus tachycardia with ST-segment elevation in leads II, aVF, and V1 to V3 (Figure 1B). Echocardiography showed diffuse hypokinesis of the left ventricle and a left ventricular ejection fraction (LVEF) of 20% (see Supplementary material online, Video S1). Emergency coronary angiography which was performed to exclude acute coronary syndrome showed normal coronary arteries, and endomyocardial biopsy was performed.
Figure 1.
Chest X-ray and electrocardiogram on admission. (A) Chest X-ray showed cardiomegaly without obvious pulmonary congestion or pleural effusion, and (B) electrocardiogram showed sinus tachycardia with ST-segment elevation in leads II, aVF, and V1 to V3.
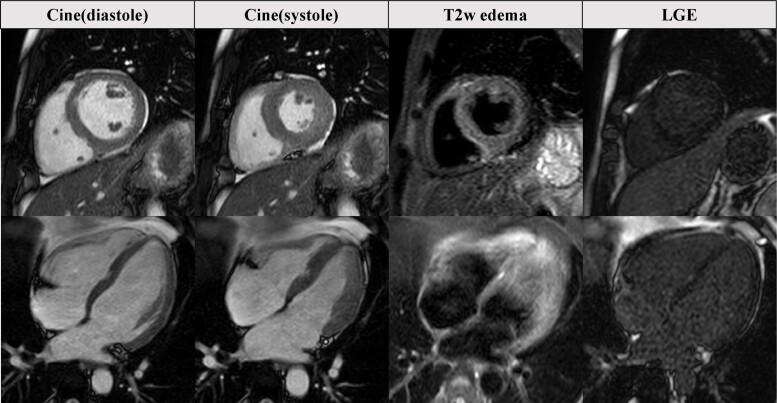
Several hours later, in the intensive care unit, the patient acutely developed respiratory failure and cardiogenic shock with ventricular tachycardia. Hence, he was intubated and given mechanical cardiac support with venoarterial extracorporeal membrane oxygenation (VA-ECMO) and intra-aortic balloon pump (IABP). He received intravenous infusions of dopamine 5 μg/kg/min and dobutamine 3 μg/kg/min, and intravenous furosemide 40 mg/day and steroid pulses of 1000 mg/day for 3 days. Echocardiography on day 4 showed improved left ventricular function (LVEF 32%), and he was weaned from VA-ECMO and IABP on day 5. The patient was extubated on day 8 and discharged from the intensive care unit on day 12. Echocardiography on day 15 showed recovery of left ventricular function (LVEF 65%) (see Supplementary material online, Video S2). Cardiac magnetic resonance imaging on day 16 showed recovery of LVEF to 49% without focal myocardial oedema and no significant late gadolinium enhancement lesions in the myocardium (Figure 2). The patient recovered completely and was discharged on Day 22.
Figure 2.
Magnetic resonance imaging. Cardiac magnetic resonance imaging on day 16 showed preserved left ventricular ejection fraction without focal myocardial oedema and no significant late gadolinium enhancement lesions in the myocardium.
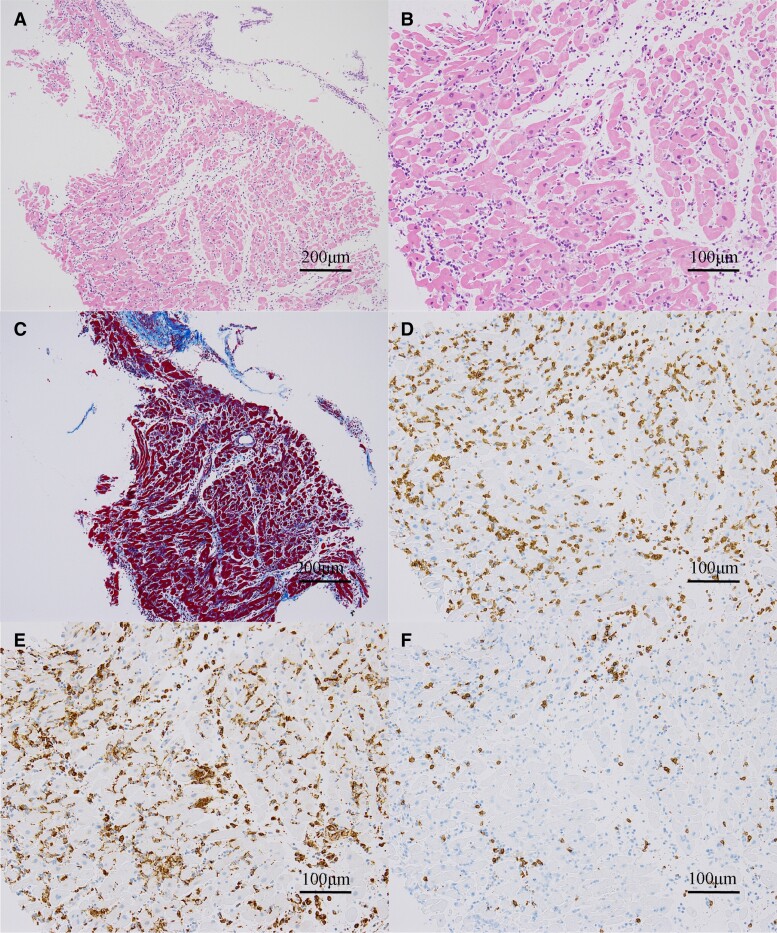
Endomyocardial biopsy results were as follows: There was a high degree of inflammatory cell infiltration with a predominance of CD3-positive T lymphocytes mixed with histiocytes and eosinophils in the myocardial interstitium, together with partial myocyte damage. There was also mild fibrosis in the interstitium. There were no epithelioid cell granulomas or giant cells, consistent with the findings of lymphocytic myocarditis (Figure 3). A real-time polymerase chain reaction (PCR) test did not detect any viral genomes in the tissue specimens.
Figure 3.
Endomyocardial biopsy. Inflammatory cell infiltration and fibrosis were observed with haematoxylin-eosin staining (A, B) and Masson-trichrome staining (C). Although CD3+ T cells and CD68 + macrophages were observed in the myocardial interstitium (D, E), not many CD20+ B cells were observed (F).
Discussion
COVID-19 vaccine-associated myocarditis is rare; among the previous reports of myocarditis caused by BNT162b2, only one case was fulminant.1 The condition has been epidemiologically reported to be more common in young males, more frequent with mRNA-1273 than BNT162b2, and more common following the second dose than the first dose of vaccination, although the mechanism is unfortunately unknown at present.2,3
In our patient, a PCR test was negative for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Serum serologic tests showed no evidence of active parvovirus, echovirus, adenovirus, Epstein Barr virus, influenza A and B viruses, cytomegalovirus, and coxsackievirus. Endomyocardial biopsy did not reveal any viral genomes using a multivirus real-time PCR system, which has the potential to detect 163 human viruses.6 In this case, the results of a PCR test for SARS-CoV-2, serum serologic test, coronary angiography, findings of endomyocardial biopsy, and the patient’s clinical course suggested a diagnosis of vaccine-associated fulminant myocarditis.
Regarding the management of this case, the patient was treated with high-dose intravenous corticosteroids for 3 days, with subsequent rapid tapering of the dose over 7 days, in consideration of the fact that it was vaccine-associated myocarditis based on the medical history, which resulted in a good outcome. The high intravenous pulse doses of corticosteroids might have been effective as immunosuppressive therapy in this case.7
The relationship between previous COVID-19 infection and vaccine-associated myocarditis is an interesting point of discussion. A previous case report of post-vaccine myocarditis in a patient previously infected with COVID-19 highlighted a potential relationship between the second dose of COVID-19 vaccination and acute myocarditis in otherwise healthy patients with previous exposure to COVID-19 infection.4 In a case series report, three of the 23 patients developed myocarditis after the first vaccination, and all three had a history of COVID-19 infection.5 It has also been reported that vaccinating people with a history of COVID-19 infection results in higher titres and more adverse reactions than those without a history of COVID-19 infection.8 Although the mechanism of COVID-19 vaccine-associated myocarditis has not been clarified, immune cross-reaction based on structural homology between the viral antigen and myocardial proteins, that is, molecular mimicry theory, and immune-inflammatory response has been proposed.9,10 Based on these reports, it is possible that in this case, although 9 months had passed since the COVID-19 infection, the first vaccine dose produced the same level of antibodies as would be expected with a second vaccine dose, resulting in a stronger reaction.
In this case of fulminant myocarditis after COVID-19 vaccination, endomyocardial biopsy results showed many CD3- and CD68-positive inflammatory cell infiltrates in the myocardial interstitium, which was consistent with lymphocytic myocarditis.
In conclusion, we described a case of fulminant myocarditis that developed soon after mRNA-1273 vaccination in a young male with a prior history of COVID-19 infection. Although endomyocardial biopsy revealed numerous lymphocytic infiltrates, the mechanism of fulminant myocarditis after mRNA-1273 vaccination is still unclear and remains to be elucidated.
Lead author biography
 Dr. Kohei Horiuchi graduated from Iwate Medical University, Japan. He currently works as a clinical resident in the Cardiovascular Division at National Hospital Organization Osaka National Hospital, Osaka, Japan.
Dr. Kohei Horiuchi graduated from Iwate Medical University, Japan. He currently works as a clinical resident in the Cardiovascular Division at National Hospital Organization Osaka National Hospital, Osaka, Japan.
Supplementary material
Supplementary material is available at the European Heart Journal – Case Reports online.
Supplementary Material
Acknowledgements
We thank Dr. Harutaka Katano (Department of Pathology, National Institute of Infectious Diseases) for viral genome analysis using a multivirus real-time PCR system, Dr. Masahiro Higashi (Department of Radiology, National Hospital Organization Osaka National Hospital) for reading the cardiac MRI, Dr. Tomoko Uehira (Department of Infection Control and Prevention, National Hospital Organization Osaka National Hospital) for helpful discussions and comments, and Dr. Kiyoshi Mori (Department of Central Laboratory and Surgical Pathology, National Hospital Organization Osaka National Hospital) for preparation and interpretation of the pathology specimens.
Consent: The authors confirm that written consent for submission and publication of this case report, including the images and associated text, was obtained from the patient in line with COPE guidelines.
Conflict of interest: H.A. has received grants from Nippon Boehringer Ingelheim. Y.U. has received research grants from Abbott Vascular, Pfizer, Bayer, Daiichi-Sankyo, Astellas, Shionogi, Sanofi, Ono, Nihon Kohden, Amgen Astellas, Actelion, Bristol-Myers Squibb, Medtronic, AstraZeneca, Otsuka and Novartis, and lecture fees from Daiichi-Sankyo, MSD, Goodman, Sanofi, Mochida, Takeda, Kowa, Teijin, Astellas, Actelion, Bristol-Myers Squibb, AstraZeneca, Boston Scientific, Sumitomo Dainippon Pharma, Eisai and Amgen Astellas.
Funding: None declared.
Contributor Information
Kohei Horiuchi, Cardiovascular Division, National Hospital Organization Osaka National Hospital, 2-1-14 Hoenzaka, Chuo-ku, Osaka 540-0006, Japan.
Shumpei Kosugi, Cardiovascular Division, National Hospital Organization Osaka National Hospital, 2-1-14 Hoenzaka, Chuo-ku, Osaka 540-0006, Japan.
Haruhiko Abe, Cardiovascular Division, National Hospital Organization Osaka National Hospital, 2-1-14 Hoenzaka, Chuo-ku, Osaka 540-0006, Japan.
Yasunori Ueda, Cardiovascular Division, National Hospital Organization Osaka National Hospital, 2-1-14 Hoenzaka, Chuo-ku, Osaka 540-0006, Japan.
References
- 1. Mevorach D, Anis E, Cedar N, Bromberg M, Haas EJ, Nadir E, Olsha-Castell S, Arad D, Hasin TLevi N, Asleh R, Amir O, Meir K, Cohen D, Dichtiar R, Novick D, Hershkovitz Y, Dagan R, Leitersdorf I, Ben-Ami R, Miskin I, Saliba W, Muhsen K, Levi Y, Green MS, Keinan-Boker L, Alroy-Preis S. Myocarditis after BNT162b2 mRNA vaccine against COVID-19 in Israel. N Engl J Med 2021;385:2140–2149. doi: 10.1056/NEJMoa2109730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gargano JW, Wallace M, Hadler SC, Langley G, Su JR, Oster ME, Broder KR, Gee J, Weintraub E, Shimabukuro T, Scobie HM, Moulia D, Markowitz LE, Wharton M, McNally VV, Romero JR, Talbot HK, Lee GM, Daley MF, Oliver SE. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the advisory committee on immunization practices — United States, June 2021. MMWR Morb Mortal Wkly Rep 2021;70:977–982. doi: 10.15585/mmwr.mm7027e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circulation 2021;144:471–484. doi: 10.1161/CIRCULATIONAHA.121.056135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ammirati E, Cavalotti C, Milazzo A, Pedrotti P, Soriano F, Schroeder JW, Morici N, Giannattasio C, Frigerio M, Metra M, Camici PG, Oliva F. Temporal relation between second dose BNT162b2 mRNA COVID-19 vaccine and cardiac involvement in a patient with previous SARS-COV-2 infection. Int J Cardiol Heart Vasc 2021;34:100774. doi: 10.1016/j.ijcha.2021.100774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, Loran D, Hrncir D, Herring K, Platzer M, Adams N, Sanou A, Cooper LT. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol 2021;6:1202–1206. doi: 10.1001/jamacardio.2021.2833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Katano H, Kano M, Nakamura T, Kanno T, Asanuma H, Sata T. A novel real-time PCR system for simultaneous detection of human viruses in clinical samples from patients with uncertain diagnoses. J Med Virol 2011;83:322–330. doi: 10.1002/jmv.21962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, Friedrich MG, Klingel K, Lehtonen J, Moslehi JJ, Pedrotti Pa, Rimoldi OE, Schultheiss HP, Tschöpe C, Cooper LT, Camici PG. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail 2020;13:e007405. doi: 10.1161/CIRCHEARTFAILURE.120.007405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krammer F, Srivastava K, Alshammary H, Amoako AA, Awawda MH, Beach KF, Bermúdez-González MC, Bielak DA, Carreño JM, Chernet RL, Eaker LQ, Ferreri ED, Floda DL, Gleason CR, Hamburger JZ, Jiang K, Kleiner G, Jurczyszak D, Matthews JC, Mendez WA, Nabeel I, Mulder LCF, Raskin AJ, Russo KT, Salimbangon ABT, Saksena M, Shin AS, Singh G, Sominsky LA, Stadlbauer D, Wajnberg A, Simon V. Antibody responses in seropositive persons after a single dose of SARS-CoV-2 mRNA vaccine. N Engl J Med 2021;384:1372–1374. doi: 10.1056/NEJMc2101667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lee ASY, Balakrishnan IDD, Khoo CY, Ng CT, Loh JKX, Chan LL, Teo LLY, Sim DKL. Myocarditis following COVID-19 vaccination: a systematic review (October 2020-October 2021). Heart Lung Circ 2022;31:757–765. doi: 10.1016/j.hlc.2022.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sulemankhil I, Abdelrahman M, Negi SI. Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: a case report and literature review. Cardiovasc Revasc Med 2021;38:117–123. doi: 10.1016/j.carrev.2021.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.