Abstract
Objectives
Appendicectomy remains of the most common emergency operations in the United Kingdom. The exact etiologies of appendicitis remain unclear with only potential causes suggested in the literature. Social deprivation and ethnicity have both been demonstrated to influence outcomes following many operations. There are currently no studies evaluating their roles with regards to severity and outcomes following appendicectomy.
Material and Methods
Demographic data were retrieved from health records for adult patients who underwent appendicectomy between 2010-2016 within a single NHS trust. To measure social deprivation, Indices of Multiple Deprivation (IMD) rankings were used. Histology reports were reviewed and diagnosis classified into predefined categories: non-inflamed appendix, uncomplicated appendicitis, complicated appendicitis and gangrenous appendicitis.
Results
Three thousand four hundred and forty-four patients were identified. Mean age was 37.8 years (range 73 years). Using a generalized linear model, South Asian ethnicity specifically was found to be independently predictive of increased length of stay following appendicectomy (p <0.001). Amongst South Asian patients, social deprivation was found to be further predictive of longer hospital stay (p= 0.005). Deprivation was found to be a predictor of complicated appendicitis but not of gangrenous appendicitis (p= 0.01). Male gender and age were also independent predictors of positive histology for appendicitis (p <0.001 and p= 0.021 respectively).
Conclusion
This study is the first to report an independent association between South Asian ethnicity and increased length of stay for patients undergoing appendicectomy in a single NHS trust. The associations reported in this study may be a result of differences in the pathophysiology of acute appendicitis or represent inequalities in healthcare provision across ethnic and socioeconomic groups.
Keywords: Appendicitis, general surgery, deprivation, ethnicity
Introduction
Appendicitis is one of the most common but also one of the most challenging acute surgical diagnoses (1). Despite an ongoing debate of conservative versus surgical management, appendicectomy remains one of the most frequently performed emergency surgical procedures in the world.
The wide differential diagnosis of acute lower abdominal pain often results in equivocal diagnosis of acute appendicitis. Whilst risk scoring systems have been developed that utilize a mixture of clinical and biochemical parameters (2-4), these are poorly implemented particularly in the United Kingdom. Due to a lack of validation of these scoring systems, a strong belief remains among practitioners that the decision to investigate invasively and consider operative management is best left to the judgement of the surgeon (5). The difficulties in clinical diagnosis of appendicitis, which are not purely investigation related, can therefore result in variability in the delivery of treatment and a potential subsequent variation in outcome.
Socioeconomic deprivation has been shown to be associated with increased length of stay in a variety of admissions, such as for coronary artery bypass and hip surgery (6,7). This is also supported by various national economic studies that suggest that lower income groups utilize more healthcare facilities, potentially due to later presentation to health professionals and as a result being more acutely unwell at first healthcare contact (8). This association has been reported to hold across primary care services, emergency departments and tertiary care centers (9-11).
The continued refinement of modern acute surgical services and the ongoing uptake of laparoscopic surgery for even severe appendicitis has led to shortened length of stay in hospital (12). These improvements in care should apply to patients of all ages and ethnicities and across all socioeconomic classes. However, evidence from centers around the world exists for differences between socioeconomic groups in both postoperative recovery and length of stay. An 11-year national analysis carried out in Taiwan demonstrated longer length of stay and increased costs in patients undergoing appendicectomy who belonged to lower socioeconomic groups (13). Despite ongoing debate on the etiology of appendicitis with many studies published on appendicitis pathology (14), there remains a paucity of research investigating the impact of social deprivation on outcomes following surgery for acute appendicitis.
Although differential incidence rates of appendicitis based on ethnic origin have been previously suggested, no direct associations have been proven definitively (15). Investigating the influence of ethnicity on the risk of developing acute appendicitis remains challenging as many other factors may be confounding such as social deprivation, cultural attitudes and biological factors that have yet to be elucidated.
The aim of our study was to investigate the relationship between demographic factors (including ethnicity and social deprivation) and length of stay in hospital and the final histological diagnosis in patients who had undergone appendicectomy in a single NHS trust.
Patients and Methods
Data Source
All patients aged 17 years or older who underwent appendicectomy between 2010 and 2016 at any of the three hospitals within a single UK NHS Foundation trust in the West Midlands were included. The study was registered with the relevant NHS organisation’s governance department as a clinical audit, therefore an NHS Research Ethics Committee review was not required. Data were extracted from electronic health records. Variables collected included date of birth, gender, ethnicity, residential postcode, admission date, discharge date and histological diagnosis.
Variables Used
Due to significant heterogeneity in the clinical coding of ethnicity, patients were reclassified into one of a set of nine ethnic categories: African, Asian (east/south/other), Caribbean, Caucasian, mixed, other or unknown.
Residential postcodes were used to obtain each patient’s corresponding ranking score based on the 2015 Indices of Multiple Deprivation. This is a multi-domain score generally regarded as the best measure of social deprivation available in the UK (16). As an indication, Birmingham ranked as the 6th most deprived Core City Local Authority at the time the indices were derived. Furthermore, areas within both the top and bottom deciles of deprivation were present within the catchment area of the NHS trust investigated in this study.
Admission and discharge dates were used to calculate each patient’s length of stay; this was rounded up and measured in whole calendar days.
Histology reports were reviewed for any macroscopic or microscopic confirmation of inflammation within the appendix. A modified version of the classification system for appendicitis previously described by Carr was used (17). Diagnoses were categorized into one of four groups: (i) normal or non-inflamed appendix, (ii) ‘uncomplicated appendicitis’ - inflamed appendix with or without suppuration, (iii) ‘complicated appendicitis’ - evidence of perforation, necrosis or both arising from the appendix, (iv) ‘gangrenous appendicitis’ - evidence of gangrene within the appendix with or without perforation. Where histological analysis gave an alternative diagnosis such as a neuroendocrine tumor or inflammatory bowel disease, these were categorized as a non-inflamed appendix. This enabled us to correlate demographic variables against histological evidence of appendicitis and not other diseases, as well as ensure maximal inclusion of patients in the analysis.
Statistical Analyses
The predictive potential of the demographic variables collected against length of stay in hospital was investigated using a generalized linear model. For histological diagnosis, a nominal variable, multinomial logistic regression was used. Statistical analysis was performed using R version 3.5.1 ‘Feather Spray’ (18).
Results
3444 patients were included in the study (Table 1). There were 1675 female patients (48.76%) and 1769 male patients (51.24%). There was no significant difference in the sexual distribution (Chi-squared test, p= 0.2573). The average age for the whole cohort of patients was 37.8 years (range 73 years), however as expected there were a higher number of younger patients amongst both genders.
Table 1. Summary table of sex, mean length of stay in days (LOS) and ethnic distribution by age group Sex, n (%).
| Sex, n (%) | Ethnic Category, n (%) | ||||||||||||
| Mean LOS | Asian | Asian | Asian | ||||||||||
| Age Group (y) | Female | Male | (range) | African | (East) | (Other) | (South) | Caribbean | Caucasian | Mixed | Other | Unknown | Total |
| 17-27 | 628 (50.00) | 628 (50.00) | 2.97 (0-93) | 16 (1.27) | 5 (0.40) | 13 (1.04) | 189 (15.05) | 18 (1.43) | 909 (72.37) | 9 (0.72) | 41 (3.26) | 56 (4.46) | 1256 |
| 28-37 | 353 (47.70) | 387 (52.30) | 3.04 (0-26) | 11 (1.49) | 5 (0.68) | 8 (1.08) | 128 (17.30) | 16 (2.16) | 471 (63.65) | 5 (0.68) | 50 (6.76) | 46 (6.22) | 740 |
| 38-47 | 236 (45.30) | 285 (54.70) | 3.57 (0-24) | 9 (1.73) | 3 (0.58) | 4 (0.77) | 71 (13.63) | 15 (2.88) | 355 (68.14) | 1 (0.19) | 21 (4.03) | 42 (8.06) | 521 |
| 48-57 | 195 (50.39) | 192 (49.61) | 4.48 (0-47) | 5 (1.29) | 1 (0.26) | 0 (0.00) | 24 (6.20) | 10 (2.58) | 303 (78.29) | 1 (0.26) | 10 (2.58) | 33 (8.53) | 387 |
| 58-67 | 130 (49.43) | 133 (50.57) | 6.81 (0-74) | 2 (0.76) | 1 (0.38) | 2 (0.76) | 13 (4.94) | 2 (0.76) | 221 (84.03) | 0 (0.00) | 2 (0.76) | 20 (7.60) | 263 |
| 68-77 | 96 (49.48) | 98 (50.52) | 9.07 (0-85) | 3 (1.53) | 0 (0.00) | 0 (0.00) | 9 (4.64) | 2 (1.03) | 172 (88.66) | 0 (0.00) | 0 (0.00) | 8 (4.12) | 194 |
| 77-87 | 33 (42.31) | 45 (57.69) | 10.94 (0-65) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (2.56) | 1 (1.28) | 70 (89.74) | 0 (0.00) | 1 (1.28) | 4 (5.13) | 78 |
| 88+ | 4 (80.00) | 1 (20.00) | 22.80 (2-69) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 5 (100) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 5 |
| Total | 1675 (48.64) | 1769 (51.36) | 4.09 (0-93) | 46 (1.34) | 15 (0.44) | 27 (0.78) | 436 (12.66) | 64 (1.86) | 2506 (72.76) | 16 (0.46) | 125 (3.63) | 209 (6.07) | 3444 |
Distribution of the included patients across the defined ethnic categories used in this study can be found in Table 1. The two most prevalent categories were Caucasian (72.82%) and South Asian (12.70%). The ethnic categories with the highest mean IMD rankings and therefore the most socioeconomically deprived was African and South Asian, whereas the least deprived ethnic categories were East Asian and Caucasian (Table 2).
Table 2. Summary of indices of multiple deprivation rankings (IMD Rank) for all ethnic categories.
| Ethnicity | Mean IMD Rank (Range) |
| African | 5800.4 (105-31937) |
| Asian (East) | 16537.6 (705-31936) |
| Asian (Other) | 8059.7 (30-32555) |
| Asian (South) | 6434.7 (105-32037) |
| Caribbean | 8712.5 (181-31267) |
| Caucasian | 14351.2 (52-32829) |
| Mixed | 7915.0 (105-27446) |
| Other | 8400.0 (105-32693) |
| Unknown | 12825.3 (105-32718) |
| Total | 12751.7 (30-32829) |
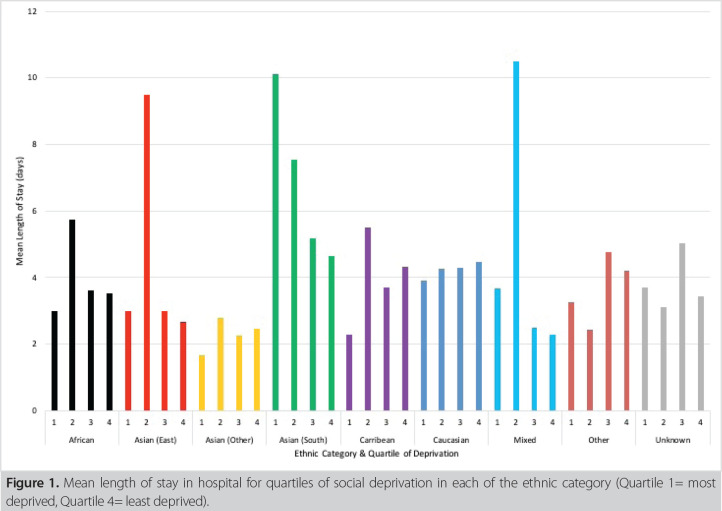
The total mean length of stay in hospital for all included patients was 4.33 days (SD 5.9 days); however, amongst older patients, length of stay in general was greater than this (Table 1). Figure 1 illustrates mean length of stay in hospital for quartiles of social deprivation in each of the ethnic categories. Amongst most ethnic categories, length of stay was variable amongst quartiles of deprivation. Notably however, length of stay was similar across deprivation quartiles amongst Caucasian patients and interestingly shows an increasing trend in South Asian pa - tients. This suggests that deprivation influenced length of stay on South Asian patients specifically, with more deprived South Asian patients having a greater length of stay than more afflu - ent patients.
Figure 1. Mean length of stay in hospital for quartiles of social deprivation in each of the ethnic category (Quartile 1= most deprived, Quartile 4= least deprived).
The percentage of appendixes that were histologically report - ed as normal or non-inflamed across all included patients was 28.37% (Table 3). 54.38% of reports were of uncomplicated ap - pendicitis, with 17.25% of histology reports containing one or more of necrosis, perforation or gangrene.
Table 3. Distribution of histological diagnostic categories by age group.
| Age Range (y) | 1 - non-inflamed Appendix | 2 - uncomplicated Appendicitis | 3 - Complicated Appendicitis | 4 - Gangrenous Appendicitis | Total | ||||
| n | % | n | % | n | % | n | % | ||
| 17-27 | 387 | 30.81% | 688 | 54.78% | 113 | 9.00% | 68 | 5.41% | 1256 |
| 28-37 | 192 | 25.95% | 448 | 60.54% | 62 | 8.38% | 38 | 5.14% | 740 |
| 38-47 | 146 | 28.02% | 276 | 52.98% | 65 | 12.48% | 34 | 6.53% | 521 |
| 48-57 | 82 | 21.19% | 209 | 54.01% | 62 | 16.02% | 34 | 8.79% | 387 |
| 58-67 | 61 | 23.19% | 135 | 51.33% | 45 | 17.11% | 22 | 8.37% | 263 |
| 68-77 | 77 | 39.69% | 82 | 42.27% | 22 | 11.34% | 13 | 6.70% | 194 |
| 77-87 | 31 | 39.74% | 34 | 43.59% | 8 | 10.26% | 5 | 6.41% | 78 |
| 88+ | 1 | 20.00% | 1 | 20.00% | 3 | 60.00% | 0 | 0.00% | 5 |
| Total | 977 | 28.37% | 1873 | 54.38% | 380 | 11.03% | 214 | 6.21% | 3444 |
Length of Stay
A generalized linear model was created to test the associations of age, gender, ethnicity and deprivation against length of stay (Table 4). Due to a potential confounding association between ethnicity and deprivation, an interaction term was included for these two variables.
Table 4. Generalized linear model coefficients of index of multiple deprivation ranking (IMD Rank), ethnic category, age and interaction terms of deprivation ranking and ethnic category with length of stay as the dependent variable.
| Coefficient | Standard Error | Z-value | p | |
| (Intercept) | 4.203 x 10-1 | 9.684 x 10-2 | 4.34 | <0.001 |
| IMD Rank | -4.168 x 10-6 | 9.467 x 10-6 | -0.44 | 0.660 |
| Ethnicity-Asian (East) | 1.899 x 10-1 | 2.599 x 10-1 | 0.731 | 0.465 |
| Ethnicity-Asian (Other) | -2.797 x 10-1 | 1.871 x 10-1 | -1.495 | 0.135 |
| Ethnicity-Asian (South) | 3.431 x 10-1 | 9.867 x 10-2 | 3.478 | <0.001 |
| Ethnicity-Caribbean | 1.007 x 10-1 | 1.272 x 10-1 | 0.791 | 0.429 |
| Ethnicity-Caucasian | 1.709 x 10-1 | 9.615 x 10-2 | 1.778 | 0.075 |
| Ethnicity-Mixed | -1.471 x 10-1 | 2.141 x 10-1 | -0.687 | 0.492 |
| Ethnicity-Other | 3.472 x 10-1 | 1.133 x 10-1 | 3.064 | 0.002 |
| Ethnicity-Unknown | 7.501 x 10-2 | 1.088 x 10-1 | 0.689 | 0.491 |
| Sex (Male) | -3.605 x 10-2 | 1.651 x 10-2 | -2.183 | 0.029 |
| Age | 2.329 x 10-2 | 4.441 x 10-4 | 52.448 | <0.001 |
| IMD Rank x Asian (East) | -2.139 x 10-6 | 1.48 x 10-5 | -0.144 | 0.885 |
| IMD Rank x Asian (Other) | 4.891 x 10-6 | 1.633 x 10-5 | 0.3 | 0.765 |
| IMD Rank x Asian (South) | 2.751 x 10-6 | 9.682 x 10-6 | 2.841 | 0.005 |
| IMD Rank x Caribbean | -8.689 x 10-8 | 1.209 x 10-6 | -0.007 | 0.994 |
| IMD Rank x Caucasian | -5.77 x 10-6 | 9.512 x 10-6 | -0.607 | 0.544 |
| IMD Rank x Mixed | 4.06 x 10-5 | 1.563 x 10-5 | 2.597 | 0.009 |
| IMD Rank x Other | -1.775 x 10-5 | 1.116 x 10-5 | -1.591 | 0.112 |
| IMD Rank x Unknown | -5.962 x 10-6 | 9.999 x 10-6 | -0.596 | 0.551 |
| (Note: coefficients and standard errors are very small as length of stay is a numerically low value). | ||||
Age was found to be the most significant predictor of increased length of stay in hospital (Z-value= 52.448, p <0.001). This asso - ciation was to be expected.
South Asian ethnicity was found to be independently associat - ed with an increased length of stay in hospital (Z-value= 3.478, p <0.001). Sex and social deprivation were not statistically sig - nificant independent predictors of increased length of stay.
However, when interaction terms between deprivation and each of the ethnicities were considered, it was found that amongst South Asian patients only, social deprivation was as - T sociated with an increased length of stay in hospital (Z-value 2.841, p= 0.005). This suggests that although social deprivation is not a predictor of longer hospital stay in all patients, it may influence the admission duration of South Asian patients specifically.
Histological Diagnosis
The histological diagnoses found in each ethnic category are shown in Table 5. From a multinomial logistic regression analysis with histological diagnostic category as the dependent variable and a non-inflamed appendix as the reference outcome, it was found that IMD rank was independently predictive of having specifically ‘complicated’ appendicitis following appendicectomy (p= 0.01), but was not associated with having any evidence of gangrene on histology (p= 0.68). Therefore, the results of this study suggest that being more socioeconomically deprived results in a greater likelihood of having necrosis with or without perforation reported on histology but not gangrene.
Table 5. Distribution of histological diagnostic categories by ethnic category.
| Ethnic Category | 1 - non-inflamed Appendix | 2 - uncomplicated Appendicitis | 3 - Complicated Appendicitis | 4 - Gangrenous Appendicitis | Total | ||||
| n | % | n | % | n | % | n | % | ||
| African | 11 | 23.91% | 26 | 56.52% | 4 | 8.70% | 5 | 10.87% | 46 |
| Asian (East) | 4 | 26.67% | 7 | 46.67% | 3 | 20.00% | 1 | 6.67% | 15 |
| Asian (Other) | 6 | 22.22% | 14 | 51.85% | 7 | 25.93% | 0.00% | 27 | |
| Asian (South) | 117 | 26.83% | 251 | 57.57% | 48 | 11.01% | 20 | 4.59% | 436 |
| Caribbean | 19 | 29.69% | 30 | 46.88% | 9 | 14.06% | 6 | 9.38% | 64 |
| Caucasian | 738 | 29.45% | 1340 | 53.47% | 264 | 10.53% | 164 | 6.54% | 2506 |
| Mixed | 6 | 37.50% | 9 | 56.25% | 1 | 6.25% | 0.00% | 16 | |
| Other | 32 | 25.60% | 67 | 53.60% | 17 | 13.60% | 9 | 7.20% | 125 |
| Unknown | 44 | 21.05% | 129 | 61.72% | 27 | 12.92% | 9 | 4.31% | 209 |
| Total | 977 | 28.37% | 1873 | 54.38% | 380 | 11.03% | 214 | 6.21% | 3444 |
Age was found to be a significant predictor of having confirmed appendicitis compared to having a histologically non-inflamed appendix (p= 0.021), but no apparent difference in odds ratios was found in the prediction of complicated or gangrenous appendicitis based on age. Similarly, male sex was found to be significantly associated with having confirmed appendicitis (p <0.001 in all 3 categories) compared to a histologically non-inflamed appendix, but much like age did not appear to predict complicated or gangrenous appendicitis. Any associations between any of the ethnic categories with any category of appendicitis did not hold when interacted with IMD ranking-these associations were therefore deemed not independent and so their statistical significance was ignored.
Discussion
This study is the first analysis to suggest that South Asian ethnicity appears to be independently associated with increased length of stay in admissions for operative management of acute appendicitis. In addition, amongst South Asian patients, social deprivation was found to be associated with increased length of stay. This study is the first to investigate possible associations between demographic variables and histological evaluation post-appendicectomy. Social deprivation was found to be associated with a greater likelihood of observing necrosis with or without perforation on histological analysis, but did not predict the presence of gangrene. In keeping with previously published datasets, male gender and age remain strong independent predictors of positive histology for appendicitis following appendicectomy. Finally, we report a negative appendicectomy rate of 27.8% over 7 years in this single center analysis, marginally higher than the historically acceptable rate of 15-25% (19).
Role of Ethnicity
The catchment area of the NHS trust investigated in this study included significant areas with large non-Caucasian communities with and without social deprivation. Also included were municipalities with largely Caucasian populations, again with varying levels of deprivation. The sample of patients obtained overall therefore was felt to be sufficiently representative of the UK population.
Diagnostic delay may lead to either or both of increased length of stay in hospital and prolonged postoperative recovery. Cultural differences between ethnicities may affect presentation behaviors and pathways to secondary care and attitudes to emergency surgery (20). Where language barriers exist between patients and healthcare professionals, the reporting of symptoms may be affected sufficiently to lead to delays in action being taken or misunderstandings regarding severity of symptoms leading to potential overtreatment. As these factors can either prolong or shorten admission duration, the data collected and analyses performed in this study are unable to differentiate whether any of them are independently important factors.
Nonetheless, the specific associations between South Asian ethnicity both alone and in combination with deprivation are surprising, particularly given that the center studied is known to have a significant South Asian population. This ethnic category in particular may have certain perioperative risk factors that may affect recovery from appendicectomy such as diabetes, obesity and cardiovascular disease. However, this may not explain the observations from this study fully given the major proportion of younger patients included, who would be expected to have minimal co-morbidities. Although not fully elucidated, the etiology of acute appendicitis may have a more severe etiology in South Asian patients-the exact reasons for this are unclear. However, no significant association was found between South Asian ethnicity and a histological diagnosis of more complicated appendicitis.
Overall, whilst an association between South Asian ethnicity and prolonged length of stay for admissions with appendicectomy has been observed in this study, no definitive conclusions can be made as to reasons why this is the case. Some of these reasons, to name a few, may be a disparity in health-related knowledge between South Asians and other ethnicities, increased prevalence of certain co-morbidities (e.g., type 2 diabetes), cultural differences in attitudes to healthcare in the perioperative period (21), differences in the pharmacokinetics of antibiotics and analgesics (22), measurement of symptoms using methods that are less appropriate for certain ethnicities (e.g., pain scales not being entirely holistic). Furthermore, the causes for South Asians having increased length of stay may be different geographically and vary by local health economy.
Role of Social Deprivation
Associations between social deprivation and longer admission duration have been observed elsewhere in the literature and in different clinical settings (6,7). With a relationship only seen in South Asian patients, this study is the first to suggest an increased length of stay due to deprivation amongst a relatively specific demographic group in a single acute NHS trust. In addition, this study is the first in general to be able to provide potential insights into the influence of social deprivation on length of stay across different ethnic categories following emergency surgery.
There may be numerous reasons for longer stays in hospital amongst the more deprived population. These may include different thresholds for patients to present themselves acutely, differences in routes of presentation either via primary or directly to secondary care and differences in health education and awareness regarding the nature of acute medical issues. Different attitudes to surgery could lead to differences between socioeconomic groups in potential attempts at non-operative management-for example there may be preferences amongst certain groups not to have surgery and therefore trial antibiotics first. Finally, there may be ethnic or cultural barriers to timely discharge from hospital following surgery, such as availability of care at home or in social care (23).
The observation that increased social deprivation raises the likelihood of normal histology following appendicectomy may be due to a vast array of factors. A key factor influencing histology will be the preferences of operating surgeons regarding the removal of the macroscopically normal ‘lily-white’ appendix. If there is a preference to perform an appendicectomy even when laparoscopy is negative for acute appendicitis, the proportion of histopathology results reporting a non-inflamed appendix will be increased independent of any patient factors. For the three hospitals investigated in this study, the departmental policy was that if acute appendicitis was deemed the most likely diagnosis preoperatively and no other pathology to explain the patient’s symptoms was identified on laparoscopy, appendicectomy was justifiable. No data regarding the macroscopic appearance of the appendix at the time of surgery was collected in this study, which precluded any investigation into surgeon-based influences on the study results. However, the data obtained in this study allowed a pragmatic investigation into histological outcomes following appendicectomy.
Despite the lack of high-level evidence in the form of randomized trials or meta-analyses, there appears to be a growing international consensus that during surgery for suspected acute appendicitis, a macroscopically normal appendix should be removed (24). Nevertheless, heterogeneity in management of the normal appendix means that patient factors affecting histological diagnosis will always remain difficult to investigate from observational studies in particular. Data from this study suggest an increased likelihood of negative histology amongst patients who are more socioeconomically deprived. Any further studies investigating demographic factors and histological outcomes following appendicectomy will need to remain pragmatic in order to accommodate differences in operative management of acute appendicitis.
Finally, many of the possible reasons for the observed influence of social deprivation and histological outcome overlap with previously mentioned factors affecting length of stay such as pathways to the operating theatre, health behaviors and attitudes affecting time to presentation from onset of symptoms and availability of healthcare resources, both perioperatively and outside of hospital.
Hospitals should ideally adapt their services according to local health needs. Where certain socioeconomic groups are more populous and with specific healthcare requirements, appropriate services should be established amongst healthcare providers to ensure patients receive the best possible care.
Role of Age & Sex
Despite the increased incidence of appendicitis in younger male patients, it has previously been reported that female patients undergo twice as many appendicectomies (25). Our analysis reported a higher rate of positive histology for appendicitis in male patients. The differential diagnosis of right-sided lower abdominal pain is much wider in the young female patient, with consideration required towards potential gynecological causes of abdominal pain. Furthermore in younger patients, there may be a greater likelihood for the operating surgeon to perform a ‘prophylactic appendicectomy’ in which a normal appendix is removed in order to minimize the risk of appendicitis at a later time (26).
In addition, the uptake of laparoscopy particularly for both the investigation and management of acute right sided abdominal pain continues to increase and is now becoming the standard of care for the operative management of appendicitis. Combined with pressures to increase the throughput of emergency surgical services in the NHS, the threshold for laparoscopy may be decreasing and therefore partially explain higher negative appendicectomy rates seen in some centers such as the setting of this study. However, continuing variations in practice amongst surgeons makes this a difficult conclusion to make definitively.
Also of importance is the common practice in the UK of confirming acute appendicitis radiologically in older patients before proceeding to surgery, irrespective of gender. Although not stipulated in any published UK guidelines, most patients of more advanced age undergo cross sectional imaging in order to rule out cecal pathologies such as right sided colonic malignancy before deciding on operative management. This results in a significantly lower negative appendicectomy rate within the elderly cohort.
The role of age and gender in the management of undifferentiated right lower quadrant pain was investigated as part of the UK Right Iliac Fossa Treatment (RIFT) audit (27). This cross-sectional snapshot audit took place more recently than the period of this observational study and across a more generalizable population. Prior to moving forward with further research into the age and sex associations suggested by this study, there would be utility in establishing whether a more national investigation such as the RIFT study corroborates the findings of this single center longitudinal analysis.
Study Limitations
A key limitation of this study was that data were only collected from patients who underwent appendicectomy. Patients who were successfully treated non-operatively or who presented to a healthcare professional with symptoms suggestive of appendicitis, but never reached the care of an acute surgical team, were not included.
Length of stay was measured in whole calendar days between the admission and discharge date, rounded up where required. There is potential therefore for the artifactual increase in length of stay by one day for patients who underwent surgery overnight. Nonetheless, whilst this may affect the applicability of length of stay as an absolute measure when comparing this study’s dataset with that of another study, the associations observed should be unaffected as this potential systematic error would apply to all of the study population.
The reclassification of patients into one of nine predetermined ethnic categories due to such a significant heterogeneity in initial ethnicity coding resulted in a loss of more detailed information about patient’s nationalities. Younger patients in particular are more likely to have been born in the UK and therefore potentially not have the same risk factors as those from their family’s country of origin.
Although the study period was seven years, only the Index of Multiple Deprivation 2015 was used. New indices of multiple deprivation are not released annually however and although social deprivation is evidently difficult to quantify, the Index of Multiple Deprivation scores are considered the best method available in the UK (16). Nonetheless, measuring socioeconomic deprivation in younger patients is more difficult as some of the variables used in determining their IMD score are either not applicable to them or may not pertain to their primary residence. A typical example of this would apply to a university student who should not necessarily be classed as unemployed with no income and in addition may not normally reside in the catchment area of the studied hospital.
In this study, a negative appendicectomy was regarded as the absence of inflammation of the appendix as stated on the histopathology report, irrespective of the final diagnosis. Non-inflammatory but nonetheless pathological findings on histology were therefore regarded as normal. These included diagnoses such as neuroendocrine tumors, Meckel’s diverticulitis with a non-inflamed appendix and parasitic infection without inflammation. The effects of these pathologies on length of stay in hospital and their different incidences across demographic groups may affect the results of this study. However, these pathologies are all rare and would likely not affect a sufficiently large sample size significantly.
Conclusion
Overall, this retrospective longitudinal analysis is the first to highlight South Asian patients as a particular demographic group at risk of increased length of stay for an admission with appendicectomy. The differential effect of social deprivation across ethnicities observed in this study has not been reported in other studies investigating the patient pathway for acute appendicitis.
Further population-based research is required in order to investigate possible causative factors that cannot be proven conclusively from observational data, both locally to establish potential region-specific inequalities and in other areas to ascertain whether similar associations are seen.
Finally, we report a higher negative appendicectomy rate amongst young female patients compared to their male counterparts, most likely due to differences in diagnostic difficulty between these two groups and surgeon specific preferences on the operative management of a normal appearing appendix.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
Peer Review: Externally peer-reviewed.
Ethics Committee Approval: According to the results of the decision tool of NHS Health Research Authority and UK RI Medical Research Council, it is no need to have NHS REC review for this study.
Author Contributions: Concept - RS; Design - SB, QA; Supervision - RS; Materials - RS; Data Collection and/or Processing - SB, QA, IS; Analysis and/or Interpretation - SB; Literature Search - SB, QA; Writing Manuscript - SB, QA; Critical Reviews -SB, QA, VS, MD, RN, MR, RS.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Stewart B, Khanduri P, McCord C, Ohene-Yeboah M, Uranues S, Vega Rivera F, et al. Global disease burden of conditions requiring emergency surgery. e9-22Br J Surg. 2014;101(1) doi: 10.1002/bjs.9329. [DOI] [PubMed] [Google Scholar]
- 2.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557–564. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 3.Chong CF, Adi MI, Thien A, Suyoi A, Mackie AJ, Tin AS, et al. Development of the RIPASA score: a new appendicitis scoring system for the diagnosis of acute appendicitis. Singapore Med J. 2010;51(3):220–225. [PubMed] [Google Scholar]
- 4.de Castro SM, Ünlü C, Steller EP, van Wagensveld BA, Vrouenraets BC. Evaluation of the appendicitis inflammatory response score for patients with acute appendicitis. World J Surg. 2012;36(7):1540–1545. doi: 10.1007/s00268-012-1521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Musunuru S, Chen H, Rikkers LF, Weber SM. Computed tomography in the diagnosis of acute appendicitis: definitive or detrimental? . J Gastrointest Surg. 2007;11(11):1417–1421. doi: 10.1007/s11605-007-0268-y. discussion 1421-2. [DOI] [PubMed] [Google Scholar]
- 6.Barnard J, Grant SW, Hickey GL, Bridgewater B. Is social deprivation an independent predictor of outcomes following cardiac surgery. An analysis of 240,221 patients from a national registry. e008287BMJ Open. 2015;5(6) doi: 10.1136/bmjopen-2015-008287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dy CJ, Lane JM, Pan TJ, Parks ML, Lyman S. Racial and socioeconomic disparities in hip fracture care. J Bone Joint Surg Am. 2016;98(10):858–865. doi: 10.2106/JBJS.15.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Askari A, Nachiappan S, Currie A, Latchford A, Stebbing J, Bottle A, et al. The relationship between ethnicity, social deprivation and late presentation of colorectal cancer. Cancer Epidemiol. 2017;47:88–93. doi: 10.1016/j.canep.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Mukhtar TK, Bankhead C, Stevens S, Perera R, Holt TA, Salisbury C, et al. Factors associated with consultation rates in general practice in England, 2013-2014: a cross-sectional study. e370-e377Br J Gen Pract. 2018;68(670) doi: 10.3399/bjgp18X695981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scantlebury R, Rowlands G, Durbaba S, Schofield P, Sidhu K, Ashworth M. Socioeconomic deprivation and accident and emergency attendances: cross-sectional analysis of general practices in England. e649-54Br J Gen Pract. 2015;65(639) doi: 10.3399/bjgp15X686893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones AP, Haynes R, Sauerzapf V, Crawford SM, Forman D. Geographical access to healthcare in Northern England and post-mortem diagnosis of cancer. J Public Health (Oxf ) 2010;32(4):532–537. doi: 10.1093/pubmed/fdq017. [DOI] [PubMed] [Google Scholar]
- 12.Sartelli M, Baiocchi GL, Di Saverio S, Ferrara F, Labricciosa FM, Ansaloni L, et al. Prospective observational study on acute appendicitis worldwide (POSAW) World J Emerg Surg. 2018;13:19–19. doi: 10.1186/s13017-018-0179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin KB, Lai KR, Yang NP, Chan CL, Liu YH, Pan RH, et al. Epidemiology and socioeconomic features of appendicitis in Taiwan: a 12-year population-based study. World J Emerg Surg. 2015;10:42–42. doi: 10.1186/s13017-015-0036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 15.Terlinder J, Andersson RE. Incidence of appendicitis according to region of origin in first- and second-generation immigrants and adoptees in Sweden. A cohort follow-up study. Scand J Gastroenterol. 2016;51(1):111–120. doi: 10.3109/00365521.2015.1030688. [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Housing, Communities & Local Government. English indices of deprivation 2015. Available on: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015. (Accessed date: 18 August 2018).
- 17.Carr NJ. The pathology of acute appendicitis. Ann Diagn Pathol. 2000;4(1):46–58. doi: 10.1016/s1092-9134(00)90011-x. [DOI] [PubMed] [Google Scholar]
- 18.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available on: https://www.R-project.org/ (Accessed date: 8 March 2018)
- 19.Detmer DE, Nevers LE, Sikes ED. Regional results of acute appendicitis care. JAMA. 1981;246(12):1318–1320. [PubMed] [Google Scholar]
- 20.Swami V, Hendrikse S. Attitudes to cosmetic surgery among ethnic minority groups in Britain: cultural mistrust, adherence to traditional cultural values, and ethnic identity salience as protective factors. Int J Psychol. 2013;48(3):300–307. doi: 10.1080/00207594.2011.645480. [DOI] [PubMed] [Google Scholar]
- 21.Khosla N, Washington KT, Regunath H. Perspectives of health care providers on US South Asians’ attitudes toward pain management at end of life. Am J Hosp Palliat Care. 2016;33(9):849–857. doi: 10.1177/1049909115593063. [DOI] [PubMed] [Google Scholar]
- 22.Wyatt R. Pain and ethnicity. Virtual Mentor. 2013;15(5):449–454. doi: 10.1001/virtualmentor.2013.15.5.pfor1-1305. [DOI] [PubMed] [Google Scholar]
- 23.Burke RE, Ibrahim SA. Discharge destination and disparities in oostoperative care. JAMA. 2018;319(16):1653–1654. doi: 10.1001/jama.2017.21884. [DOI] [PubMed] [Google Scholar]
- 24.Jaunoo SS, Hale AL, Masters JP, Jaunoo SR. An international survey of opinion regarding investigation of possible appendicitis and laparoscopic management of a macroscopically normal appendix. Ann R Coll Surg Engl. 2012;94(7):476–480. doi: 10.1308/003588412X13373405385377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Körner H, Söndenaa K, Söreide JA, Andersen E, Nysted A, Lende TH, et al. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg. 1997;21(3):313–317. doi: 10.1007/s002689900235. [DOI] [PubMed] [Google Scholar]
- 26.Newhall K, Albright B, Tosteson A, Ozanne E, Trus T, Goodney PP. Cost-effectiveness of prophylactic appendectomy: a Markov model. Surg Endosc. 2017;31(9):3596–3604. doi: 10.1007/s00464-016-5391-y. [DOI] [PubMed] [Google Scholar]
- 27.RIFT Study Group On behalf of the West Midlands Research Collaborative. Right Iliac Fossa Pain Treatment (RIFT) Study: protocol for an international, multicentre, prospective observational study. e017574BMJ Open. 2018;8(1) doi: 10.1136/bmjopen-2017-017574. [DOI] [PMC free article] [PubMed] [Google Scholar]