Abstract
Objectives
The length and the attachment of the mesoappendix is important in the degree of inflammation, spread of tumor and during surgical resection of the appendix. The presence of accessory appendicular artery along with varied origin of appendicular artery may cause intra- as well as post-operative complications. Hence, the study of length of mesoappendix and the origin and branching pattern of arterial supply to the appendix was undertaken.
Material and Methods
Sixty formalin fixed appendix specimens were resected along with the intact mesopappendix and were dissected to analyze the extent of attachment, origin of appendicular arteries and the accessory branches as well.
Results
The whole length mesoappendix was seen in 76% and the half length mesoappendix was not found. The main appendicular artery originated from the ileocolic artery in 80%, and accessory appendicular artery was seen in 13% of the study specimens.
Conclusion
The mesoappendix and the branching pattern of the appendicular artery varies from person to person, and this awareness will be of use during surgeries on appendix.
Keywords: Appendix, mesoappendix, appendectomy, appendicular artery
Introduction
The vermiform appendix is located in the right lower quadrant of the abdomen and is one of the important differential diagnosis in case of pain (1,2). Its length varies from 2-20 cm, with an average length of 9 cm (2,3). The attachment of the base of the appendix to the caecum remains constant, whereas the tip can be found in a para-colic/para-caecal (11 o’clock), retrocaecal (12 o’clock), splenic (2 o’clock) position, promontoric (3 o’clock), pelvic (4 o’clock), midinguinal/subcaecal (6 o’clock) position, pre-ileal and post-ileal positions (1,2,4).
Vermiform appendix is connected by a short mesoappendix to the lower part of the mesentery of the ileum enclosing the appendicular artery and the inferior ileocaecal recess (2). The terminal part of the artery lies on the wall of the appendix and hence may be thrombosed in appendicitis, resulting in distal gangrene and necrosis. In about 50% of the cases an accessory artery of Dr. Sheshachalam (5), a branch of posterior caecal artery is present and needs separate ligation during appendectomy. Thrombosis of this artery, in acute appendicitis, inevitably results in gangrene and subsequent perforation. Appendicitis is the most common cause of acute abdomen (4,6). Identification of the normal position of the appendix is important because in appendicitis, variable positions may produce symptoms and signs related to their position, and hence can mimic other diseases (7,8). According to Lohar et al. (9), the age group of the incidence of appendicitis is 11-20 years constituting 44.6%, 21-30 years constituting 36.1%, 31-40 years constituting 11.5% while between 0 and 10 years age group, it was 3%, and between 41-50 years and 51-75 years of age group, it was 2.3% each in India in 2021. Hence, the rate of appendectomy is higher, and intra-operative and post-operative complication of hemorrhage in cases of accessory appendicular artery is more common. Short mesoappendix can cause the appendix to necrose in case of inflammation, as appendicular artery, which is as such an end artery, to be more nearer to the wall. This study aimed at studying the length of mesoappendix and the arterial pattern of the appendix in detail.
Patients and Methods
The present study was performed on 60 specimens of human vermiform appendices. The study was done in situ in the cadavers before the appendix was displaced by manipulation and dissection from the right iliac fossa. The abdomen was opened by a long midline incision and the flaps were reflected to give a good view of the abdominal cavity along with its contents. The appendix was studied along with its relation to the ileum and caecum. All taeniae of the caecum converge to the base and acts as the best guide for the vermiform appendix. The extent of the mesoappendix was studied. Specimens fixed with 10% formalin were initially washed with free-flowing tap water to wash away the formalin so as to avoid irritation to the eyes and nasal mucosa. It also caused softening of the fixed tissue. After clearing the mesoappendix, the appendicular artery was visualized. The number of arteries present in it was noted down. To find the branches of the artery, the tracing was done proximally, carefully observing if it was a single artery or a double artery. Then, the parental arteries were identified and recorded. When dissecting and clearing the arteries closer to the appendix, the branching pattern, anastomotic pattern and the end arteries were noted. Some arteries after supplying the tip of the appendix passed posterior to the appendix and supplied that aspect separately. All the arteries were accompanied by their respective veins and nerves.
Results
The following results were obtained by observing the extent of the mesoappendix and arterial pattern of appendix in 60 vermiform appendices:
• Extension up to whole length of the appendix in 46 specimens,
• Extension up to 2/3 of length of the appendix in 14 specimens,
• Extension up to half of the length of the appendix in none of the specimens.
Vermiform appendix was supplied by single appendicular artery in majority of the cases (52), but accessory appendicular artery (8) was also found to be present in mesoappendix ( Table 1).
Table 1. Incidence of the number of appendicular artery suppling appendix.
| S. No | Number of artery | Number of specimens |
| 1 | Single artery | 52 |
| 2 | Double arteries | 8 |
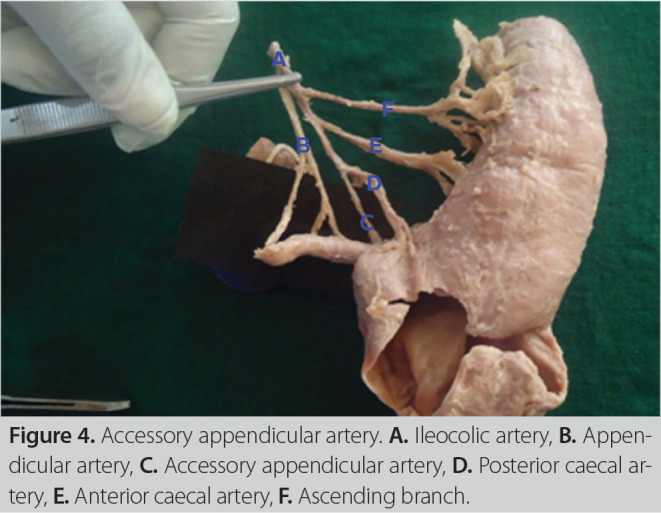
The main appendicular artery arose from the ileocolic artery in 48 cases (Figures 1,2), ileal artery in 8 cases and posterior caecal artery in 4 cases (Table 2). The accessory appendicular artery was seen to originate in contrast from the main branch, predominantly from posterior caecal artery than the ileocolic artery (Table 3) (Figures 3,4).
Figure 1. Accessory appendicular artery. A. Ileocolic artery, B. Appendicular artery, C. accessory appendicular artery.
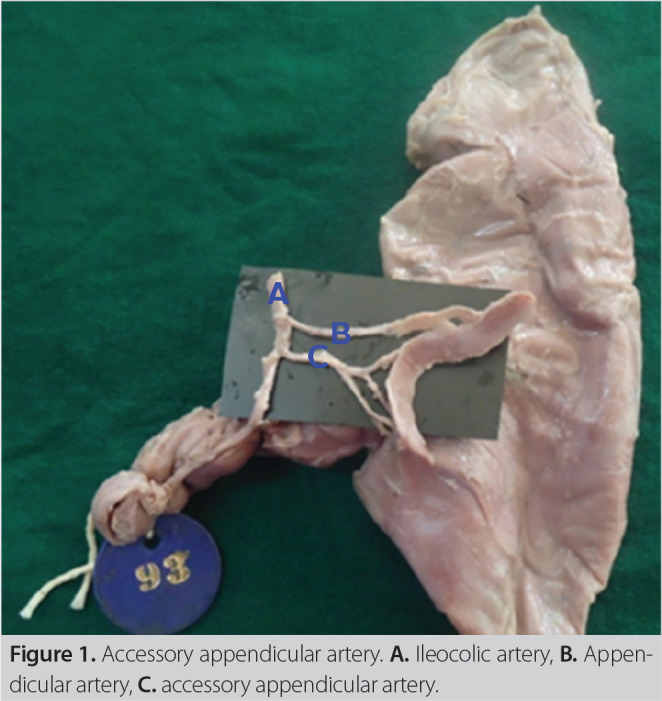
Figure 2. Accessory appendicular artery. A. Ileocolic artery, B. Appendicular artery, C. Accessory appendicular artery.
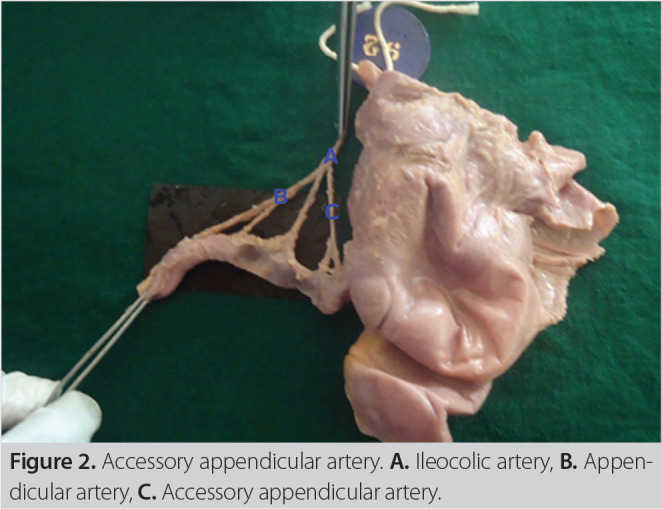
Table 2. Source of origin of main appendicular artery from the pa- rental artery.
| S. No | Parental artery | Number of specimens | Percentage |
| 1 | Ileocolic artery | 48 | 80% |
| 2 | Ileal artery | 8 | 13.33% |
| 3 | Posterior caecal artery | 4 | 6.67% |
| 4 | Anterior caecal artery | NIL | NIL |
Table 3. Origin of accessory appendicular artery.
| S. No | Parental artery | Number of specimens |
| 1 | Ileocolic artery | 2 |
| 2 | Ileal artery | NIL |
| Posterior caecal artery | 6 | |
| Anterior caecal artery | NIL |
Figure 3. Accessory appendicular artery. A. Ileocolic artery, B. Appendicular artery, C. Accessory appendicular artery, D. Posterior caecal artery, E. Anterior caecal artery, F. Ascending branch.
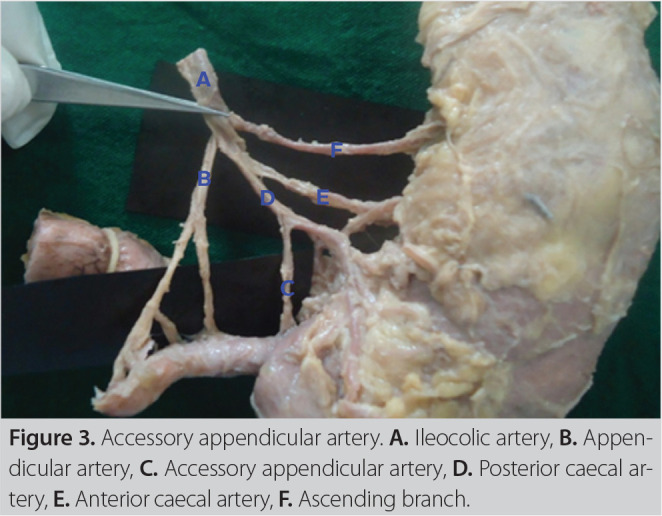
Figure 4. Accessory appendicular artery. A. Ileocolic artery, B. Appendicular artery, C. Accessory appendicular artery, D. Posterior caecal artery, E. Anterior caecal artery, F. Ascending branch.
Discussion
The extension of the mesoappendix is responsible for the vascularization of the vermiform appendix and severity during inflammation, as its failure to reach the tip of the appendix may lead to gangrene and hence early perforation during inflammation (10). The latest inclusion of the spread of appendiceal tumour in the mesoappendix and elective removal of mesoappendix during appendectomy, adds to the significance of our study (11). The same mesoappendix acts as a pathway where a window is created and the stump of appendix is clamped once or twice (depending on the thickness of mesoappendix) (12).
This study aimed exclusively to get an in depth insight on the attachment of mesoappendix and the origin and branching pattern of arteries supplying the appendix. In this study, the extent of mesoappendix till the tip was found to be 76.6%. On reviewing the literature, the study done by Geethanjali in 2011 had the nearest incidence of 69.23% (13). According to the study by Anderson et.al., the mesoappendix reached the tip of the appendix in 80% of the cases (10). According to Tahir Iqbal in 2012, there was a long mesoappendix frequently extending up to the tip of the appendix and often an ileo-caecal fold (14).
In the present study, the mesoappendix extended up to 2/3rd of the length of the appendix in 23.3%. The study done by Geethanjali has had an incidence of 30.77%, which is the nearest to the present study, where the mesoappendix failed to reach the tip (13). This present study does not coincide with the study of Rahman MM in 2005, where the extension of mesoappendix was 2/3rd of the appendix in 45% cases, half and whole extension of mesoappendix were found in 31% and 24% cases, respectively (15).
Surgical interest in the appendix has been aroused since 1886 by the recognition of its inflammation by Reginald Herbeit Fitz. The different anatomical studies performed on appendix concern its localization and its vascularization with the objective of improving the techniques of its ablation. In 1980, Mitroffanof successfully used an appendix for the treatment of an incontinent bladder (Appendiculovesicostomy). Since then, vascularized appendix has been used on its pedicle, and subsequently in free transplant, with success, to rebuild ureters, urethras, the uterine tubes and extra hepatic biliary tract. According to Djibril Ouattaraa knowledge of its vascularization is indispensable to guarantee the survival of the whole of the transplant (16).
The appendicular artery is an end artery from its midpoint and as it very close to the wall, it gets easily thrombosed during acute inflammation. The distal appendix is easily necrosed and hence, perforation is common. There is no unanimity in the literature about the origin of the main appendicular artery. Some authors claim that it arises solely from the ileocolic, while others claim that it comes off from one of the branches of the ileocolic artery (17). The majority of those authors who have noted the presence of accessory appendicular arteries claim that these arteries invariably arise from the anterior or posterior caecal artery and cause significant intra-op as well as post-op bleeding (18). The systematization of the vascularization of the appendix differs according to the number and the type of arteries supplying it. The main appendicular artery is defined as one which runs in the crescentic fold of the mesoappendix to the tip of the appendix; and the accessory appendicular artery (from ileocolic artery or its branches) as one which supplies other parts of the appendix except the tip. In this study, the main artery was invariably the branch of ileocolic artery (80%), ileal artery (13.3%) and posterior caecal artery (6.6%). We did not come across even a single artery that originated from anterior caecal artery. The main appendicular artery arises from inferior division of superior mesenteric artery in 46.88%, ileal branch 28.13%, ileocolic artery 18.75% and from arterial arcade in 6.25% of cases. 21.87% of cases showed additional appendicular artery in a study by Hosmani (19).
In this study, appendix was supplied by a single appendicular artery in 87% of the cases, but accessory appendicular artery was also found to be present in the mesoappendix, and it was seen arising from various closely related arteries. In the African population (20), the incidence is totally in contrast, as there were 80% of cases showing the presence of an accessory appendicular artery, and in 20% of cases supplied only by single appendicular artery. In this present study, the incidence of double appendicular arteries supplying the appendix was about 13%. The same has been observed by Nirmaladevi as 10% (21) and Toriola as 9% (20) but not by Ashwini Balasaheb, which has been found as 40% (22). The accessory appendicular artery was seen to originate in contrast from the main branch, predominantly from posterior caecal artery than the ileocolic artery in our study as in concordance with Ajmani et.al (23), though we differ in that, there were no accessory arteries arising from anterior caecal artery. Solanke et al. (24) have cited that there were extensive arterial anastomoses between the arteries supplying the appendix. We differ and contradict this statement, as there were nil arterial anastomoses observed in the current study, confirming that each individual branch was its own end artery, confounding the risk of gangrene. The anastomotic pattern can really be studied by injecting a suitable dye and the pattern of distribution seen by radiological examination in the living, which is the further scope of this study.
Conclusion
Study of the mesoappendix gives a guide to the surgeons during appendectomy. The shorter the extent of the mesoappendix, the more risk of gangrenous complications. The main appendicular artery arose from ileocolic, posterior caecal and ileal arteries but not at all from the anterior caecal artery. Knowledge of the presence of accessory appendicular artery is of utmost importance to prevent hemorrhage during surgery, and 13% of the specimens had an accessory artery. The most common origin of the accessory appendicular artery was from the posterior caecal artery, followed by the ileocolic artery. This study, hence, gives more insight to the anatomical aspects of the mesoappendix and appendicular arterial pattern for surgeons.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
Peer Review: Externally peer-reviewed.
Ethics Committee Approval: For this study, it is not necessary to have the ethical approval because this is a cadaveric surgery.
Author Contributions: Concept - H.R.; Design - T.B.; Supervision - S.P., H.R.; Data Collection and/or Processing - S.P.; Analysis and/or Interpretation - S.P.; Literature Search - V.G.; Writing Manuscript - H.R.; Critical Reviews - V.G.
Financial Disclosure: The authors are not related to any support and financial participation (eg employment, consultancy, honorary, stock ownership and options, expert statement, patents received or pending, copyrights) in the past three years. They also declare that they are not involved in nonfinancial relationships (personal, political or professional) that may affect the writing of the article.
References
- 1.Sabiston DC, Townsend RD, Courtney M. Sabiston’s textbook of surgery, the biological basis of modern surgical practice. In: Appendix 16th ed (vol 2): 918. Philadelphia: W.B. Saunders Company; 2001. [Google Scholar]
- 2.Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE and et al. Alimentary system. 38th ed. Churchill Livingstone; New York: 1995. Gray’s anatomy; pp. 1775–1776. [Google Scholar]
- 3.Buschard K, Kjaeldguard A. Investigation and analysis of the position. Length and embryology of the vermiform appendix. Acta Chirugica Scandinavica. 1973;139(3):293–298. [PubMed] [Google Scholar]
- 4.Schwartz SJ, Shires GT, Spencer FC, Daly JM, Fischer JE, Galloway AC. Principles of surgery Schwartz. In: The Appendix. 7th ed (vol 3) 1383-5 Philadelphia: MC Graw-Hill; 1999. [Google Scholar]
- 5.Seshachalam T, Gorur SR. The arterial supply of the appendix: from the department of anatomy, University Medical College. Mysore Ind Med Gaz. 1930;65(12):693–694. [PMC free article] [PubMed] [Google Scholar]
- 6.Addiss DG, Shaffer N, Fowler BSF, Tauxe RV. The epidemiology of appendicitis and appendicectomy in the United States. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 7.Sabiston DC, Townsend Courtney M. Sabiston’s textbook of surgery, the biological basis of modern surgical practice. In: Appendix. 16th ed (vol 2): 918. Philadelphia: W.B. Saunders Company; 2001. [Google Scholar]
- 8.Bakheit MA, Warille AA. Anomalies of the vermiform appendix and prevalance of acute appendicitis in Khartom. East Afr Med J. 1999;16(6):338–340. [PubMed] [Google Scholar]
- 9.Lohar HP, Asger Calcuttawala MA, Nirhale DS, Athavale VS, Malhotra M, Priyadarshi N. Epidemiological aspects of appendicitis in a rural setup. Med J DY Patil Univ. 2014;7:753–757. [Google Scholar]
- 10.Anderson RE, Houganer A, Thalin AJD. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patients and with appendicectomy rate. Eur J Surg. 1992;158:37–41. [PubMed] [Google Scholar]
- 11.Rait JS, McGillicuddy J, Ajzajian J. Appendiceal neoplasms and histological involvement of the mesoappendix: a case series. Ann Med Surg. 2020;56:64–67. doi: 10.1016/j.amsu.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naguib N. Simple technique for laparoscopic appendicectomy to ensure safe division of the mesoappendix. Scandinavian J Surg. 2014;103:73–74. doi: 10.1177/1457496913519527. [DOI] [PubMed] [Google Scholar]
- 13.Geethanjali HT, Subhash LP. A study of variations in the position of vermiform appendix. Anatomica Karnataka. 2011;5(2):17–23. [Google Scholar]
- 14.Iqbal T, Amanullah A, Nawaz R. Pattern and positions of vermiform appendix in people of bannu district. Gomal J Med Sci. 2012;10:100–103. [Google Scholar]
- 15.Rahman MM, Khalil M, Sultana SZ, Mannan S, Nessa A, Ahamed MS. Extent of meso appendix in Bangladeshi people. J Bangladesh Soc Physiol. 2009;4(1):20–23. [Google Scholar]
- 16.Ouattara D, Kipré YZ, Broalet E, Séri FG, Angaté HY, Bi N’Guessan GG, et al. Classification of the terminal arterial vascularization of the appendix with a view to its use in reconstructive microsurgery. Surg Radiol Anat. 2007;29(8):635–641. doi: 10.1007/s00276-007-0265-6. [DOI] [PubMed] [Google Scholar]
- 17.Davis L. Christopher’s Textbook of Surgery. 8th ed. Philadelphia and London: W. B. Saunders; 1964. pp. 679–679. [Google Scholar]
- 18.Surya Kumari N, Srinivas CH. Study of vermiform appendix with its arterial supply in guntur district, andhra pradesh-a fetal specimen study. J Evol Med Dent Sci. 2015;4(72):12548–12556. [Google Scholar]
- 19.Veeresh H. A study of arterial supply of vermiform appendix in humans. J Evol Med Dent Sci. 2012;1(5):807–807. [Google Scholar]
- 20.Solanke TF. The position, length, and content of the vermiform appendix in nigerians. Brit J Surg. 1970;57(2):100–102. doi: 10.1002/bjs.1800570205. [DOI] [PubMed] [Google Scholar]
- 21.Nirmaladevi M, Seshayyan S. Cadaveric study on the origin of the appendicular artery. Int J Anat Res. 2016;4(1):1769–1771. [Google Scholar]
- 22.Nuchhi AB, Yatagiri SV, Patil BG, Bannur BM. Study of arterial supply of caecum and appendix: a cadaveric study. Int J Anat Res. 2017;5(3.1):4158–4162. doi: 10.16965/ijar.2017.272. [DOI] [Google Scholar]
- 23.Ajmani ML, Ajmani K. The position, length and arterial supply of vermiform appendix. Anatomischeranzeiger. 1983;153(4):369–374. [PubMed] [Google Scholar]
- 24.Solanke TF. The blood supply of vermiform appendix in Nigerians. J Anat. 1968;102:353–361. [PMC free article] [PubMed] [Google Scholar]


