Abstract
The ability to generate microglia from human induced pluripotent stem cells (iPSCs) provides new tools and avenues for investigating the role of microglia in health and disease. Furthermore, iPSC-derived microglia can be maintained in co-culture with iPSC-derived cortical neurons, which enable investigations of microglia-neuron interactions that are hypothesized to be dysregulated in a number of neuropsychiatric disorders. Human iPSCs were differentiated to generate microglia using an adapted version of a protocol developed by the Fossati group and the iPSC-derived microglia were validated with marker analysis and real-time PCR. Human microglia generated using this protocol were positive for the markers CD11C, IBA1, P2RY12, and TMEM119, and expressed the microglial-related genes AIF1, CX3CR1, ITGAM, ITGAX, P2RY12, and TMEM119. Human iPSC-derived cortical neurons that had been differentiated for 30 days were plated with microglia and maintained in co-culture until day 60, when experiments were undertaken. The density of dendritic spines in cortical neurons in co-culture with microglia was quantified under baseline conditions and in the presence of pro-inflammatory cytokines. In order to examine how microglia modulate neuronal function, calcium imaging experiments of the cortical neurons were undertaken using the calcium indicator Fluo-4 AM. Live calcium activity of cortical neurons was obtained using a confocal microscope and fluorescence intensity was quantified using ImageJ. This report describes how co-culturing human iPSC-derived microglia and cortical neurons provides new approaches to interrogate effects of microglia on cortical neurons.
SUMMARY:
This protocol describes a methodology to differentiate microglia from human iPSCs and maintain them in co-culture with iPSC-derived cortical neurons in order to study mechanistic underpinnings of neuroimmune interactions using human neurons and microglia.
INTRODUCTION:
Microglia function in the brain
In the human brain, microglia are the primary innate immune cells1. Brain development is regulated by microglia via two routes: release of diffusible factors and phagocytosis1. Microglia-derived diffusible factors help support myelination, neurogenesis, synaptic formation, maturation, cell death, and cell survival1. Microglia also phagocytize various elements in brain synapses, axons and in both living and dead cells2–8. Receptors on microglia recognize tags such as calreticulin, ATP and sialic acid and regulate cellular phagocytosis9,10. In the hippocampus, microglia maintain the homeostasis of neurogenesis through its phagocytic role11.
Synaptic phagocytosis in the dorsolateral geniculate nucleus (dLGN) of the rodent brain has been shown to be regulated by microglia1. In rodents, it has been shown that there are two periods during development when intense microglial synaptic phagocytosis is observed. The first period occurs during initial synapse formation and the second period occurs when connections are being fine-tuned and pruned12. Other factors that are involved in synaptic pruning are inflammatory proteins and the Class I major histocompatibility complex (MHC1, H2-Kb and Db)13,14. It has been suggested that C1q (complement component 1q) on the microglia colocalizes with MHC1 which triggers synaptic pruning15. Furthermore, mouse studies show that interleukin-33 (IL-33) secreted by astrocytes regulates synapse homeostasis in the thalamus and the spinal cord through its effects on microglia, though this has yet to be investigated in humans 13. Microglia secrete a variety of cytokines that help maintain neuronal health, such as tumor necrosis factor α (TNFα), IL-1β, IL-6, IL-10 and interferon-γ (IFN-γ) and these cytokines can modulate dendritic spine and synapse formation16–18.There are significant gaps in our knowledge of neuron-microglia interactions during human brain development. Most of our knowledge comes from studies from rodent models while there is a paucity of information on the temporal and mechanistic aspects of synaptic pruning in the human cortex. Microglia support neuronal survival in the neo-cortex and other cell types contribute as well1. It is not clear how microglia contribute to this preservation and what the interplay between microglia and the other cell types are. Microglia release several cytokines that affect neuronal and synaptic development but the mechanistic basis of their effects of these cytokines in neurons are largely unknown19,20. In order to develop a more complete understanding of the function of microglia in the human brain, it is critical to explore its interactions with different cell types found in the human brain. This report describes a method to co-culture human iPSC-derived neurons and microglia generated from the same individual. Establishing this methodology will enable well-defined investigations to interrogate the nature of microglia-neuronal interactions and to develop robust ex vivo cellular models to study neuroimmune dysfunction in the context of different neurodevelopmental and neuropsychiatric disorders.
The role of microglia in schizophrenia
Synaptic pruning is a major neurodevelopmental process that takes place in the adolescent brain21,22. Multiple lines of evidence suggest that synaptic pruning during this critical period is abnormal in schizophrenia (SCZ)23–26. SCZ is a chronic, debilitating psychiatric disorder characterized by hallucinations, delusions, disordered thought processes and cognitive deficits23,24. Microglia, the resident macrophages in the brain, play a central role in synaptic pruning25,26. Postmortem and positron emission tomography (PET) studies show evidence for dysfunctional microglial activity in SCZ25–32. Postmortem SCZ brains show well-replicated but subtle differences in the brain – pyramidal neurons in cortical layer III show decreased dendritic spine density and fewer synapses33–35. Synaptic pruning is a process by which superfluous excitatory synaptic connections are eliminated by microglia during adolescence, when SCZ patients usually have their first psychotic break22,36. Postmortem studies show an association between SCZ and microglial activation, with increased density of microglia in SCZ brains, as well as increased expression of proinflammatory genes27. In addition, PET studies of human brains using radioligands for microglial activation show increased levels of activated microglia in the cortex25–28. Recent genome wide association studies (GWAS) show that the strongest genetic association for SCZ resides in the major histocompatibility complex (MHC) locus and this association results from alleles of the complement component 4 (C4) genes that are involved in mediating postnatal synaptic pruning in rodents37. This association has provided additional support for the hypothesis that aberrant pruning by microglia may result in the decreased dendritic spine density seen in SCZ postmortem brains. Investigations of microglial involvement in synaptic pruning in SCZ have so far been limited to indirect studies with PET imaging or inferences from investigations of postmortem brains.
Generating human microglia in the laboratory
Cultured primary mouse microglia have been frequently used in studying microglia, though there are several indications that rodent microglia may not be representative of human microglial anatomy and gene expression38. Several studies have also differentiated microglia directly from blood monocytes through transdifferentiation39–42. Blood monocyte-derived microglia-like cells exhibit major differences from human microglia in gene and protein expression profile pro-inflammatory responses and they appear to be more macrophage-like in their biology43. Recent methodological advances now enable generation of microglia from human iPSCs which provide opportunities to study live microglia that more accurately resemble the biology of microglia found in the human brain. These iPSC-derived microglial cells have been shown to recapitulate the phenotype, gene expression profiles and functional properties of primary human microglia44–48. This paper provides a method to co-culture human iPSC-derived neurons and microglia generated from the same individual in order to develop personalized ex vivo models of neuron-microglia interactions. For this ex vivo co-culture model, a microglial differentiation protocol from the Fossati group was adapted and combined with an adapted version of a cortical neuronal generation protocol from the Livesey group 49,50.
PROTOCOL:
The human iPSCs used in this study were reprogrammed from fibroblasts that had been obtained through informed consent from healthy control subjects, with approval form the institutional review board (IRB). The reprogramming and characterization of iPSCs used in this study (ML15, ML27, ML40, ML56, ML141, ML 250, ML292) were described in a prior study51.
1. Maintenance of iPSCs
-
1.1
Prepare a 1:50 dilution of LDEV-free reduced growth factor basement membrane matrix in DMEM/F12 without phenol red and pre-coat a 6-well plate with 1mL diluted solution for at least 2 h at 37°C prior to thawing cell stocks.
-
1.2
Thaw cryopreserved iPSC stocks in a 37°C water bath for 2 min. Add the cells to a 15mL centrifuge tube containing 5mL DMEM/F12. Spin the cells down at 300 x g for 5 min. Remove coating solution from the pre-coated LDEV-free reduced growth factor basement membrane matrix plate and add 1mL of stem cell medium (SCM) with 10μM Rock inhibitor (Y-27632). Resuspend the cell pellet in SCM with 10μM Y-27632 and add to the pre-coated plate, for a final volume of 2mL of SCM plus Y-27632. Maintain iPSC cell cultures in this medium for 24 h in a 37°C incubator.
-
1.3
Replace medium with 2mL of fresh SCM without Y-27632 24 h after thawing.
-
1.4
After iPSCs reach 80–90% confluence, passage them onto 75mL flasks coated with LDEV-free reduced growth factor basement membrane matrix. Passage cells by first rinsing cells with HBSS and remove after letting sit for 30 s. Add 1mL non-enzymatic cell dissociation reagent and incubate for 4 min at 37°C. Prepare plate with SCM containing 10μM Y-27632. Aspirate non-enzymatic cell dissociation reagent and add 1mL SCM + 10μM Y-27632 to each well. Gently scrape well with cell lifter and obtain cells with a 1000μL pipette. Deposit cells onto LDEV-free reduced growth factor basement membrane matrix-coated 75mm flask in a total volume of 8mL of SCM + Y-27632.
2. Microglia Differentiation
-
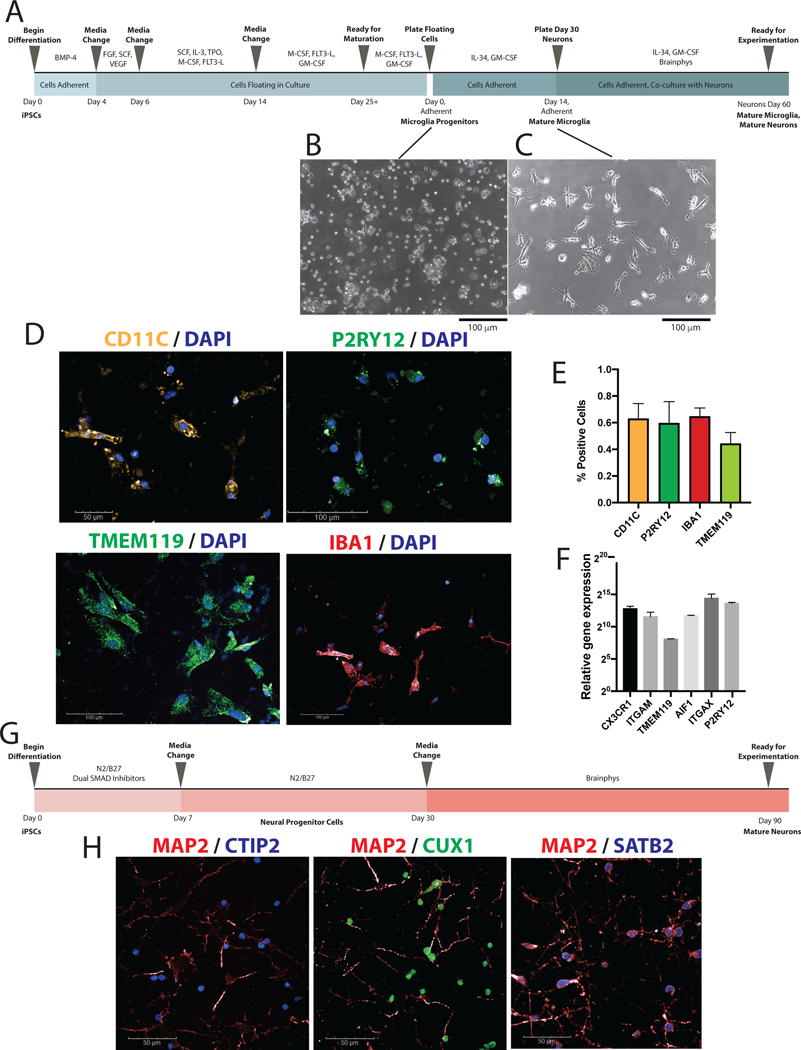
2.1
A schematic outlining the microglia differentiation protocol is depicted in Figure 1A. All media should be warmed to room temperature prior to use. Day 0: Perform a complete medium change with SCM medium supplemented with 80ng/mL BMP-4. Perform daily medium changes for Days 1–3.
-
2.2
Day 4: Prepare Day 4–5 medium: hematopoietic medium (HM), supplemented with 25ng/mL FGF, 100ng/mL SCF, and 80ng/mL VEGF. Remove medium and replace with Day 4–5 medium containing 5μM Y-27632.
-
2.2.1
NOTE: Cells begin to float at this point
-
2.2.1
-
2.3
Day 6: Prepare Day 6–13 medium: HM supplemented with 50ng/mL SCF, 50ng/mL IL-3, 5ng/mL TPO, 50ng/mL m-CSF, and 50ng/mL Flt3-L. Collect supernatant and add to a 15-mL conical tube and spin down for 8 min at 300 x g. Resuspend pellet in Day 6–13 medium with 5μM Y-27632.
-
2.4
Day 10: Add 8mL Day 6–13 medium on top of existing medium.
-
2.5
Day 14: Prepare Day 14+ medium: HM supplemented with 50ng/mL m-CSF, 50ng/mL Flt3-L, 50ng/mL GM-CSF. Collect supernatant and add to a 50-mL conical tube and spin down for 8 min at 300 x g. Resuspend pellet in day 14+ medium containing 5μM Y-27632.
-
2.6
Day 18: Add 8mL Day14+ medium.
-
2.7
Day 22: Add 8mL Day14+ medium.
-
2.8
Day 25: Cells may be moved to next differentiation step or may continue to be maintained in Day14+ medium until day 50 of differentiation.
-
2.9
After Day 25, collect supernatant in a 50-mL conical tube and spin down for 8 min at 300 x g. Prepare adherent medium: RPMI supplemented with 1% 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution, 25ng/mL GM-SCF and 100ng/mL IL-34. Resuspend pellet in adherent medium containing 5μM Y-27632. Plate cells on specific plating for different experiments: LDEV-free reduced growth factor basement membrane matrix-coated plates for microglial monoculture, 10ug/mL poly-L-ornithine and 10μg/mL laminin coated glass imaging plates for imaging experiments. Dilute poly-L-ornithine and laminin in DPBS and add 250uL / well for a 24 well imaging plate.
-
2.9.1
Note: Cells are now adherent in culture (Figure 1C).
-
2.9.1
-
2.10
Maintain cells in culture for at least 14 days, with bi-weekly medium changes. After day 14 post-adherence, cells have reached maturation and may be used for experiments.
Figure 1.
Differentiation and validation of iPSC-derived microglia. A. Schematic depiction of microglial differentiation from iPSCs through microglial maturity and co-culture with cortical neurons. B. Representative image of microglial progenitor cells after re-plating following day 25 of differentiation at 10x magnification. C. Representative image of mature microglia at day 14 at 10x magnification. D. Immunocytochemistry staining of CD11c, P2RY12, IBA1, and TMEM119 to confirm expression of microglial markers, shown at 20x magnification. E. Percentage of cells positively stained for microglial markers CD11c, P2RY12, IBA1, and TMEM119. F. qPCR validation showing microglia exhibiting microglial-signature genes including AIF1, CX3CR1, ITGAM, ITGAX, P2RY12, and TMEM119. G. Schematic depicting cortical neuron differentiation from iPSCs. H. Immunocytochemistry staining of CTIP2, CUX1, SATB2, and MAP2 to confirm generation of cortical neurons, shown at 63X magnification.
3. Cortical Neuron Differentiation
-
3.1
A schematic outlining the cortical neuron differentiation protocol is depicted in Figure 1G. Day 0: Once iPSCs are confluent on LDEV-free reduced growth factor basement membrane matrix-coated plates, switch from SCM to a 50/50 mix of N2/B27 medium supplemented with 10μM SB431542, 1μM dorsomorphin, 100nM LDN193189. N2 medium consists of basal medium supplemented with 1% N-2 supplement, 1% 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution, 1% pen/strep. B27 medium consists of DMEM/F12 supplemented with 2% B-27 supplement, 1% 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution, 1% pen/strep. Change medium with the above supplements added daily for 7 days.
-
3.2
Day 7: Pre-coat plates in LDEV-free reduced growth factor basement membrane matrix for at least 2 h. Passage cells 1:1 onto pre-coated plates. Rinse cells with 1mL/well HBSS and remove after letting sit for 30 s. Add 1mL/well enzymatic dissociation agent and incubate for 4–5 min at 37°C. While incubating, prepare 15mL conical tubes with 5mL DMEM. Gently pipette enzymatic dissociation agent to remove cells from the plate with a P1000 pipettor. Collect enzymatic dissociation agent and cell mixture in a 15mL centrifuge tube. Centrifuge the tubes for 5 min at 300 x g. Resuspend pellet in N2/B27 medium containing 10μM Y-27632. Continue daily feedings with N2/B27 medium with no supplements.
-
3.3
Day 12: Passage cells 1:1 using methods described in 3.2. Continue daily feedings with N2/B27 medium.
-
3.4
Day 15/16: Passage cells 1:2 using methods described in 3.2. Continue daily feedings with N2/B27 medium.
-
3.5
Day 18/19: Passage cells 1:3 using methods described in 3.2. Continue daily feedings with N2/B27 medium until day 30.
-
3.6
Day 30: Passage cells using methods described in 3.2 onto the microglia culture plates, where they will now be maintained in neuronal medium (NM) supplemented with 1% B-27 supplement.
4. Microglia/Neuron Co-cultures
-
4.1
Pre-coat 24-well glass imaging plates in 10ug/mL poly-L-ornithine and 10μg/mL laminin diluted in DPBS.
-
4.2
Plate Day 30 cortical neurons on top of microglial cultures. Supplement medium with laminin 1μg/mL to improve cell adherence.
-
4.3
Maintain cultures in a mix of 50% adherent medium and 50% NM. Perform half-medium change bi-weekly until experimentation.
-
4.4
Perform experiments after neurons reach day 60.
5. Interferon-γ Treatment
-
5.1
Prepare fresh medium supplemented with 100ng/mL IFN-γ. Add medium and let incubate for 24 h. Replace with fresh medium without IFN-γ immediately prior to experimentation.
6. Immunocytochemistry
-
6.1
Fix cells with 4% paraformaldehyde at room temperature for 20 min.
-
6.2
Rinse cells in PBS thrice for 5 min each.
-
6.3
Add PBST (PBS + 0.1% Triton X) for 10 min.
-
6.4
Add blocking buffer: PBS plus 5% goat serum for 1 h.
-
6.5
Add primary antibody diluted in PBS + 1% goat serum - overnight at 4°C. Optimize all primary antibodies accordingly.
-
6.6
Rinse cells in PBS thrice for 5 min each.
-
6.7
Add secondary antibody, diluted in PBS plus 1% goat serum - for 1 h at room temperature.
7. Spine Analysis
-
7.1
Obtain images on a confocal microscope at 60x magnification.
-
7.2
Use ImageJ function NeuronJ52 to analyze images.
-
7.3
Obtain measurements for neurite length, spine length, and spine count through Neuron J.
8. Calcium Imaging
-
8.1
Prepare fresh medium with 3μM Fluo-4AM dye. Incubate co-cultures in this medium for 30 min at 37°C. Then rinse the cells with PBS and add live-cell imaging solution to the cells and proceed to imaging.
-
8.2
Using a confocal microscope equipped for live-cell imaging, obtain time-lapse images at 40x for 2 min. Activity can recorded at baseline, with exposure to 15mM glutamate or in the setting of depolarization with 5mM potassium chloride.
-
8.3
Using ImageJ, measure fluorescence intensity over time for individual cell bodies. Using the selection tool, select individual region of interest (ROI) surrounding each cell body. Open the “ROI manager” and press “add” to select. Continue to add new selections to the ROI manager. Use the “set measurements” tool to measure “mean gray area”. When the number of desired cell bodies has been added to the ROI manager, select them all and then use the “multi-measure” tool. This will provide a readout of the mean gray area for each over the time course of the video file. The exported data will give mean fluorescence intensity for the region of interest for each frame.
-
8.4
Determine fluorescence intensity ratio, F/F0, where F is the fluorescence intensity at a given time and F0 is the initial fluorescence intensity. F/F0 can be graphed over time to examine spontaneous activity in neurons, or examined at the maximum fluorescent intensity in the setting of stimulation.
REPRESENTATIVE RESULTS:
Protocol Validation
The iPSC-derived microglia were generated from seven iPSC lines and validated using ICC and qPCR. Microglia generated from the adapted protocol exhibited typical ramified microglial morphology (Figure 1C), and expressed microglial markers CD11c, TMEM119, and IBA1, as examined by immunocytochemistry (Figure 1D,E). Cells with nuclei expressing microglial markers CD11c, P2RY12, and IBA1 were quantified. CD11c, P2RY12, IBA1 and TMEM119 were present in 63%, 60%, 65%, and 44% of the cells respectively. These experiments were performed with 3 iPSC lines. Expression of specific genes was examined using qPCR to confirm the expression of microglial genes AIF1, CX3CR1, ITGAM, ITGAX, P2RY12, and TMEM119 (Figure 1F). This data was obtained from iPSC-derived microglia from two lines and normalized to an iPSC line. The SYBR Green real-time PCR protocol was used.
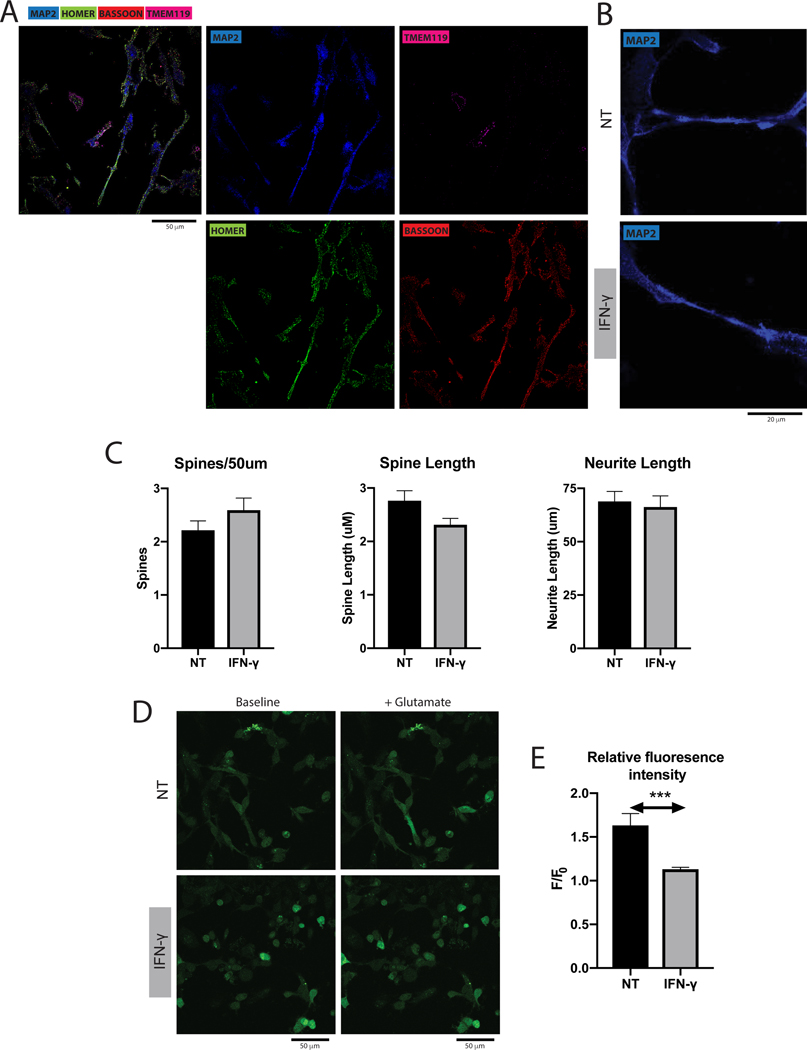
Dendritic Spines
Cortical neurons and microglia in co-culture were visualized using confocal microscopy (Figure 2A). Dendritic spines were quantified in the co-cultured cortical neurons (Figure 2B). Cortical neurons co-cultured with microglia treated with IFN-γ exhibited no significant differences in spine count, spine length, and neurite length when compared to cortical neurons co-cultured with untreated microglia (Figure 2C). This data was collected for four iPSC lines, with two separate wells per experimental condition and ten images obtained from each well.
Figure 2.
A. Representative image of microglia and cortical neuron co-culture, with neurons stained for MAP2, pre-synaptic marker bassoon and post-synaptic marker homer, and microglia stained for TMEM119. B. Representative image of dendritic spines in microglia/neuron co-cultures, with and without IFN-γ treatment. Scale bar = 50 μm. C. Cortical neurons co-cultured with microglia treated with IFN-γ showed no significant differences when compared to untreated microglia in terms of spine count (Mann-Whitney test, P > 0.05, mean + SEM), spine length (Mann-Whitney test, P > 0.05, mean + SEM), or neurite length (unpaired t test, P > 0.05, mean + SEM). D. Representative images of cortical neurons in the presence of the calcium indicator Fluo-4AM, before and after glutamate stimulation and with and without IFN-γ treatment. E. Cortical neurons co-cultured in the presence of microglia treated with IFN-γ had significantly lower fluorescence intensity with glutamate stimulation when compared to neurons co-cultured with untreated microglia (Mann-Whitney test, P = 0.0003, mean + SEM).
Calcium Imaging
Neurons co-cultured with microglia were stained with calcium fluorescence indicator in order to examine differences in neuronal firing with stimulation from glutamate with and without IFN-γ induced microglial activation (Figure 2D). Cortical neurons co-cultured with microglia treated with IFN-γ showed significant reduction in fluorescence intensity after stimulation with glutamate compared to cortical neurons co-cultured with untreated microglia (Figure 2E). This data was collected for three lines with two wells per experimental condition and five images obtained from each well.
DISCUSSION
The development of differentiation methods along different trajectories for pluripotent stem cells have opened many avenues for the investigation of brain function and disease processes53–55. Initial studies had focused on the development of specific neuronal cell types hypothesized to be important in specific brain disorders56,57. Recently, brain organoids have also provided new ways to study disease biology using patient-specific three-dimensional models51,58. The two-dimensional and three-dimensional cellular models provide specific advantages when trying to tackle different scientific questions59. While the early studies focused on cells along the neuronal lineage, recent developments now enable generation of other cell types in the brain, i.e. microglial cells and brain microvascular endothelial cells60,61. While studying the development of these cell types have provided valuable information and knowledge, it is important understand the interplay between these cell types to fully understand the role of neuroimmune and neurovascular interactions on brain function and development. This paper provides a detailed protocol on generating and co-culturing cortical neurons and microglia derived from the same iPSC line in order to develop personalized ex vivo co-culture models to study the effects of different cell types on neuronal biology. By optimizing a method to efficiently differentiate microglia from iPSCs, we are now poised to examine disease-specific phenotypes using microglia and cortical neurons differentiated from iPSCs from disease subjects. Furthermore, this experimental approach allows for cross-culturing of microglia and neurons from control and disease subjects that can be leveraged to delineate specific contributions of microglia and neurons in disease-related phenotypes.
A number of rodent studies have examined co-cultures of microglia and neurons. A tri-culture with astrocytes, microglia and primary neurons reported significant improvement in neuronal health and reduced caspase 3/7 activity in the co-cultures62. An additional co-culture protocol for primary cerebellar granule neurons and primary cortical microglia from mice revealed that the use of co-culture methodology helps prevent the negative effect of toxicants on neuronal function and survival by mediating the release of cytokines.63 These findings suggest that it is important to study co-cultures of different cell types to accurately depict relevant neurobiology, and highlight the need for these experiments to be undertaken using human cells to understand the role neuro-immune interactions in psychiatric disease biology.
Only one previous study has investigated co-cultures of human iPSC-derived microglia or precursor macrophages with cortical neurons48. Co-cultures of embryonic MYB-independent iPSC-derived macrophages with iPSC-derived cortical neurons found that co-culture with microglia led to downregulation in pathogen-response pathways, upregulation in homeostatic function pathways, and promoted an anti-inflammatory and pro-remodeling cytokine response than corresponding monocultures, further suggesting the important crosstalk between microglia with neurons that can be recapitulated in ex vivo co-culture models48. This study used iPSC-derived neurons to help mature MYB-independent iPSC-derived macrophages into microglial cells whereas the current protocol utilizes iPSC-derived microglia that had been differentiated to maturity separately. Given the significant interplay between these cell types, using a methodology where the maturation of microglia is dependent on the health of the neurons may present challenges and confounding factors when studying disease-related phenotypes.
Critical Steps
There are three critical steps in this protocol that should be followed to ensure success. First, spinning cells for medium change for the floating microglial cultures should be kept to a minimum, which is why it is outlined that media should be added on top of the existing media during this stage instead of exchanging media. This step helps prevent loss and death of differentiating microglial cells. Second, when plating cortical neurons onto microglial cultures, it is crucial to add laminin to the medium in order to ensure that neurons will adhere to the plate. Neurons have a tendency to lift off of the plate and adding laminin helps prevent this. Third, for calcium imaging experiments, ensure that the confocal microscope used is equipped with an incubation chamber for live-cell imaging. This allows the cells to remain healthy throughout the experimentat and prevents variability in data due to the timing of when the imaging data was collected.
Modifications and Troubleshooting
This protocol adapted an aspect of the Fossati group protocol that had led to significant loss and death of differentiating microglial cells. Rather than collecting the supernatant and floating cell mixture and pelleting the cells every four days as originally described, fresh media was added on top to prevent cell loss and death in the centrifugation process. Cells were grown in 75mm flasks rather than in 6-well plates in order to maximize volume of media that could be added during this stage.
This protocol also removed a sorting step described in the Fossatti group protocol. The sorting step resulted in a much lower cellular yield and high cell death in our hands. Hence, floating cells at day 25+ were plated without using this sorting step. Cells differentiated using this modified approach had ramified morphology characteristic of microglial cells, expressed microglial genes and showed robust staining of microglial markers.
Limitations
Though the specific protocols for generating co-culturing iPSC-derived microglia and cortical neurons involved adapting from two well-established protocols, the microglia generated with this adapted approach have not been as extensively characterized as the original protocol. The downsides of this protocol relates to length and cost of differentiation. The differentiation process takes at least 40 days and requires the use of a number of expensive reagents, especially the cytokines. Also, in this report, IFN-γ was used as an activator of microglia, but it should also be noted that this pro-inflammatory cytokine can elicit direct changes in cortical neurons as well64 and there is a need to undertake further studies to delineate the effect of cytokines on microglia and neurons.
Future Applications
These experiments provide proof-of-concept approaches to examine the effect of microglia on neuronal biology, which sets the stage for interesting explorations of various facets of neuro-immune interactions in the context of disease biology using microglia and neurons generated from patients with specific neurodevelopmental and neuropsychiatric disorders. The ability to cross-culture microglia and neurons from healthy subjects and disease subjects provide interesting avenues to dissect the specific roles of these cell types in the manifestation of disease-related phenotypes. Furthermore, co-culture models can be expanded to include astrocytes, oligodendrocytes and endothelial cells in order to develop novel ex vivo models that reflect the different niches found in the brain.
Supplementary Material
Table 1.
Overview of current protocols for differentiation of iPSCs to microglial cells.
| Protocol | Supplements used | Sorting stage | Length of Differentiation | Protein markers |
|---|---|---|---|---|
|
| ||||
| Abud et al. 45 | FGF, BMP4, Activin A, LiCl, FGF, VEGF, TPO, SCF, IL-3, IL-6, M-CSF, IL-34, TGFβ1, insulin, CD200, CX3CL1 | At day 10, isolate CD34+ cells | 38 days | CD45 CX3CR1 ITGB5 MERTK PROS1 TGFβR1 P2RY12 TREM2 |
| Douvaras et al. 49 | BMP4, FGF, SCF, VEGF, IL-3, TPO, M-CSF, Flt-3L, GM-CSF, IL-34 | At day 25, for CD14+/ CX3CR1+ cells |
40 days | CD11b CD11c CX3CR1 IBA1 P2RY12 TMEM119 |
| Haensler et al. 48 | BMP4, SCF, VEGF, M-CSF, IL-3, GM-CSF | At day 21, for CD11b+ / CD45+ cells | 42 days | CD11b CD14 CD45 IBA1 MERTK |
Table 2.
Overview of media used for microglial differentiation, listed with the concentration of cytokines used.
| Day | Medium | Cytokines | Concentration |
|---|---|---|---|
|
| |||
| 0–3 | Stem Cell Medium | BMP-4 | 80ng/mL |
| 4–5 | Hematopoietic Medium | FGF SCF VEGF |
25ng/mL 100ng/mL 80ng/mL |
| 6–13 | Hematopoietic Medium | SCF IL-3 TPO M-SCF Flt3-Ligand |
50ng/mL 50ng/mL 5ng/mL 50ng/mL 50ng/mL |
| 14–25+ | Hematopoietic Medium | M-SCF Flt3-Ligand GM-SCF |
50ng/mL 50ng/mL 50ng/mL |
| Adherent | RPMI 1640 | GM-SCF IL-34 |
25ng/mL 100ng/mL |
Table 3.
Brief overview of neuronal differentiation protocol from Shi et al. and adaptations made in this study.
| Protocol | Neural Maintenance Medium | Neural Induction Medium | Supplements | Notable Differences |
|---|---|---|---|---|
|
| ||||
| Shi et al. 2012 | N2/B27 medium. N2 medium: Basal medium with 1% N-2 supplement, 1% 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution, 1% pen/strep, 5ug/mL insulin, 1mM ;-glutamine, 100μM non-essential amino acids, 100μM 2-mercaptoethanol. B27 medium: DMEM/F12 supplemented with 2% B-27 supplement, 200mM L-glutamine, 1% pen/strep. |
N2/B27 medium supplemented with 10μM SB431542 and 100ng/mL noggin OR 10μM SB431542 and 1μM dorsomorphin. | 20ng/mL FGF2 upon appearance of rosettes | Use of Insulin, NEAA, 2-mercaptoethanol |
| This protocol | N2/B27 medium. N2 medium: Basal medium with 1% N-2 supplement, 1% 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution, 1% pen/strep. B27 medium: DMEM/F12 supplemented with 2% B-27 supplement, 1% 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution, 1% pen/strep. |
N2/B27 medium supplemented with 10μM SB431542, 1μM dorsomorphin, 100nM LDN193189. | Use of 200mM L-alanyl-L-glutamine dipeptide in 0.85% NaCl solution in B27 medium, use of 100nM LDN193189 in Neural Induction Medium | |
ACKNOWLEDGMENTS:
This work was supported by a National Institute of Mental Health Biobehavioral Research Awards for Innovative New Scientists (BRAINS) Award R01MH113858 (to R.K.), National Institute of Mental Health Clinical Scientist Development Award K08MH086846 (to R.K.), the Doris Duke Charitable Foundation Clinical Scientist Development Award (to R.K.), the Ryan Licht Sang Bipolar Foundation (to R.K.), the Jeanne Marie Lee-Osterhaus Family Foundation and the NARSAD Young Investigator Award from the Brain & Behavior Research Foundation (to A.K.), the Phyllis & Jerome Lyle Rappaport Foundation (to R.K.), the Harvard Stem Cell Institute (to R.K.) and by Steve Willis and Elissa Freud (to R.K.). We would like to thank Dr. Bruce M. Cohen and Dr. Donna McPhie from Harvard Medical School and McLean Hospital for providing us with the fibroblasts used in the study.
Footnotes
A complete version of this article that includes the video component is available at http://dx.doi.org/10.3791/62480.
DISCLOSURES:
The authors have nothing to disclose.
REFERENCES:
- 1.Lenz KM, Nelson LH Microglia and beyond: innate immune cells as regulators of brain development and behavioral function. Frontiers in immunology. 9 698, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoshiko M, Arnoux I, Avignone E, Yamamoto N, Audinat E.Deficiency of the microglial receptor CX3CR1 impairs postnatal functional development of thalamocortical synapses in the barrel cortex. Journal of Neuroscience. 32 (43), 15106–15111, (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunningham CL, Martínez-Cerdeño V, Noctor SC Microglia regulate the number of neural precursor cells in the developing cerebral cortex. Journal of Neuroscience. 33 (10), 4216–4233, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hagemeyer N.et al. Microglia contribute to normal myelinogenesis and to oligodendrocyte progenitor maintenance during adulthood. Acta neuropathologica. 134 (3), 441–458, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lenz KM, Nugent BM, Haliyur R, McCarthy MM Microglia are essential to masculinization of brain and behavior. Journal of Neuroscience. 33 (7), 2761–2772, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyamoto A.et al. Microglia contact induces synapse formation in developing somatosensory cortex. Nature communications. 7 (1), 1–12, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pont‐Lezica L.et al. Microglia shape corpus callosum axon tract fasciculation: functional impact of prenatal inflammation. European Journal of Neuroscience. 39 (10), 1551–1557, (2014). [DOI] [PubMed] [Google Scholar]
- 8.Schafer DP et al. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron. 74 (4), 691–705, (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hornik TC, Vilalta A, Brown GC Activated microglia cause reversible apoptosis of pheochromocytoma cells, inducing their cell death by phagocytosis. Journal of cell science. 129 (1), 65–79, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown GC, Neher JJ Microglial phagocytosis of live neurons. Nature Reviews Neuroscience. 15 (4), 209–216, (2014). [DOI] [PubMed] [Google Scholar]
- 11.Sierra A.et al. Microglia shape adult hippocampal neurogenesis through apoptosis-coupled phagocytosis. Cell stem cell. 7 (4), 483–495, (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schafer DP et al. Microglia contribute to circuit defects in Mecp2 null mice independent of microglia-specific loss of Mecp2 expression. Elife. 5 e15224, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vainchtein ID et al. Astrocyte-derived interleukin-33 promotes microglial synapse engulfment and neural circuit development. Science. 359 (6381), 1269–1273, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Datwani A.et al. Classical MHCI molecules regulate retinogeniculate refinement and limit ocular dominance plasticity. Neuron. 64 (4), 463–470, (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Färber K.et al. C1q, the recognition subcomponent of the classical pathway of complement, drives microglial activation. Journal of neuroscience research. 87 (3), 644–652, (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wlodarczyk A.et al. A novel microglial subset plays a key role in myelinogenesis in developing brain. The EMBO Journal. 36 (22), 3292–3308, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim S-H et al. Neuronal synapse formation induced by microglia and interleukin 10. PloS one. 8 (11), e81218, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Squarzoni P.et al. Microglia modulate wiring of the embryonic forebrain. Cell reports. 8 (5), 1271–1279, (2014). [DOI] [PubMed] [Google Scholar]
- 19.Shin WH et al. Microglia expressing interleukin‐13 undergo cell death and contribute to neuronal survival in vivo. Glia. 46 (2), 142–152, (2004). [DOI] [PubMed] [Google Scholar]
- 20.Giulian D, Li J, Leara B, Keenen C.Phagocytic microglia release cytokines and cytotoxins that regulate the survival of astrocytes and neurons in culture. Neurochemistry international. 25 (3), 227–233, (1994). [DOI] [PubMed] [Google Scholar]
- 21.Petanjek Z.et al. Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proceedings of the National Academy of Sciences. 108 (32), 13281–13286, (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giedd JN et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nature neuroscience. 2 (10), 861–863, (1999). [DOI] [PubMed] [Google Scholar]
- 23.Lewis DA, Lieberman JA Catching up on schizophrenia: natural history and neurobiology. Neuron. 28 (2), 325–334, (2000). [DOI] [PubMed] [Google Scholar]
- 24.Jablensky A.Epidemiology of schizophrenia: the global burden of disease and disability. European archives of psychiatry and clinical neuroscience. 250 (6), 274–285, (2000). [DOI] [PubMed] [Google Scholar]
- 25.Van Berckel BN et al. Microglia activation in recent-onset schizophrenia: a quantitative (R)-[11C] PK11195 positron emission tomography study. Biological psychiatry. 64 (9), 820–822, (2008). [DOI] [PubMed] [Google Scholar]
- 26.Doorduin J.et al. Neuroinflammation in schizophrenia-related psychosis: a PET study. Journal of Nuclear Medicine. 50 (11), 1801–1807, (2009). [DOI] [PubMed] [Google Scholar]
- 27.Van Kesteren C.et al. Immune involvement in the pathogenesis of schizophrenia: a meta-analysis on postmortem brain studies. Translational psychiatry. 7 (3), e1075-e1075, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bloomfield PS et al. Microglial activity in people at ultra high risk of psychosis and in schizophrenia: an [11C] PBR28 PET brain imaging study. American Journal of Psychiatry. 173 (1), 44–52, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fillman S.et al. Increased inflammatory markers identified in the dorsolateral prefrontal cortex of individuals with schizophrenia. Molecular psychiatry. 18 (2), 206–214, (2013). [DOI] [PubMed] [Google Scholar]
- 30.Radewicz K, Garey LJ, Gentleman SM, Reynolds R.Increase in HLA-DR immunoreactive microglia in frontal and temporal cortex of chronic schizophrenics. Journal of Neuropathology & Experimental Neurology. 59 (2), 137–150, (2000). [DOI] [PubMed] [Google Scholar]
- 31.Steiner J.et al. Distribution of HLA-DR-positive microglia in schizophrenia reflects impaired cerebral lateralization. Acta neuropathologica. 112 (3), 305–316, (2006). [DOI] [PubMed] [Google Scholar]
- 32.De Picker LJ, Morrens M, Chance SA, Boche D.Microglia and brain plasticity in acute psychosis and schizophrenia illness course: a meta-review. Frontiers in psychiatry. 8 238, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garey L.et al. Reduced dendritic spine density on cerebral cortical pyramidal neurons in schizophrenia. Journal of Neurology, Neurosurgery & Psychiatry. 65 (4), 446–453, (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glantz LA, Lewis DA Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Archives of general psychiatry. 57 (1), 65–73, (2000). [DOI] [PubMed] [Google Scholar]
- 35.Konopaske GT, Lange N, Coyle JT, Benes FM Prefrontal cortical dendritic spine pathology in schizophrenia and bipolar disorder. JAMA psychiatry. 71 (12), 1323–1331, (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petanjek Z.et al. Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proc Natl Acad Sci U S A. 108 (32), 13281–13286, (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sekar A.et al. Schizophrenia risk from complex variation of complement component 4. Nature. 530 (7589), 177–183, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Landry RP, Jacobs VL, Romero-Sandoval EA, DeLeo JA Propentofylline, a CNS glial modulator does not decrease pain in post-herpetic neuralgia patients: In vitro evidence for differential responses in human and rodent microglia and macrophages. Experimental Neurology. 234 (2), 340–350, (2012). [DOI] [PubMed] [Google Scholar]
- 39.Sievers J, Parwaresch R, Wottge HU Blood monocytes and spleen macrophages differentiate into microglia‐like cells on monolayers of astrocytes: morphology. Glia. 12 (4), 245–258, (1994). [DOI] [PubMed] [Google Scholar]
- 40.Simard AR, Rivest S.Bone marrow stem cells have the ability to populate the entire central nervous system into fully differentiated parenchymal microglia. The FASEB Journal. 18 (9), 998–1000, (2004). [DOI] [PubMed] [Google Scholar]
- 41.Asheuer M.et al. Human CD34+ cells differentiate into microglia and express recombinant therapeutic protein. Proceedings of the National Academy of Sciences. 101 (10), 3557–3562, (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ohgidani M.et al. Direct induction of ramified microglia-like cells from human monocytes: dynamic microglial dysfunction in Nasu-Hakola disease. Scientific reports. 4 (1), 1–7, (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Melief J.et al. Characterizing primary human microglia: A comparative study with myeloid subsets and culture models: Characterizing Primary Human Microglia. Glia. 64 (11), 1857–1868, (2016). [DOI] [PubMed] [Google Scholar]
- 44.Muffat J.et al. Efficient derivation of microglia-like cells from human pluripotent stem cells. Nature medicine. 22 (11), 1358–1367, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abud EM et al. iPSC-derived human microglia-like cells to study neurological diseases. Neuron. 94 (2), 278–293. e279, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pandya H.et al. Differentiation of human and murine induced pluripotent stem cells to microglia-like cells. Nature neuroscience. 20 (5), 753–759, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pocock JM, Piers TM Modelling microglial function with induced pluripotent stem cells: an update. Nature Reviews Neuroscience. 19 (8), 445–452, (2018). [DOI] [PubMed] [Google Scholar]
- 48.Haenseler W.et al. A Highly Efficient Human Pluripotent Stem Cell Microglia Model Displays a Neuronal-Co-culture-Specific Expression Profile and Inflammatory Response. Stem Cell Reports. 8 (6), 1727–1742, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Douvaras P.et al. Directed differentiation of human pluripotent stem cells to microglia. Stem Cell Reports. 8 (6), 1516–1524, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shi Y, Kirwan P, Livesey FJ Directed differentiation of human pluripotent stem cells to cerebral cortex neurons and neural networks. Nature protocols. 7 (10), 1836–1846, (2012). [DOI] [PubMed] [Google Scholar]
- 51.Kathuria A.et al. Transcriptomic Landscape and Functional Characterization of Induced Pluripotent Stem Cell–Derived Cerebral Organoids in Schizophrenia. JAMA psychiatry. (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meijering E.et al. Design and validation of a tool for neurite tracing and analysis in fluorescence microscopy images. Cytometry Part A: the journal of the International Society for Analytical Cytology. 58 (2), 167–176, (2004). [DOI] [PubMed] [Google Scholar]
- 53.Watmuff B.et al. Disease signatures for schizophrenia and bipolar disorder using patient-derived induced pluripotent stem cells. Molecular and Cellular Neuroscience. 73 96–103, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karmacharya R, Haggarty SJ Stem cell models of neuropsychiatric disorders. Molecular and cellular neurosciences. 73 1, (2016). [DOI] [PubMed] [Google Scholar]
- 55.Karmacharya R, Kieling C, Mondelli V.Integrating stem cell-based experiments in clinical research. European Psychiatry. 63 (1), (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kathuria A.et al. Synaptic deficits in iPSC-derived cortical interneurons in schizophrenia are mediated by NLGN2 and rescued by N-acetylcysteine. Translational psychiatry. 9 (1), 1–13, (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Watmuff B, Liu B, Karmacharya R.Stem cell-derived neurons in the development of targeted treatment for schizophrenia and bipolar disorder. Pharmacogenomics. 18 (5), 471–479, (2017). [DOI] [PubMed] [Google Scholar]
- 58.Kathuria A.et al. Transcriptome analysis and functional characterization of cerebral organoids in bipolar disorder. Genome medicine. 12 1–16, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kathuria A, Lopez-Lengowski K, Watmuff B, Karmacharya R.Comparative transcriptomic analysis of cerebral organoids and cortical neuron cultures derived from human induced pluripotent stem cells. Stem Cells and Development. 29 (21), 1370–1381, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pong S, Lizano P, Karmacharya R.Derivation, Expansion, Cryopreservation and Characterization of Brain Microvascular Endothelial Cells from Human Induced Pluripotent Stem Cells. Journal of Visualized Experiments: Jove. (165), (2020). [DOI] [PubMed] [Google Scholar]
- 61.Pong S, Karmacharya R, Sofman M, Bishop JR, Lizano P.The Role of Brain Microvascular Endothelial Cell and Blood-Brain Barrier Dysfunction in Schizophrenia. Complex Psychiatry. 6 (1–2), 30–46, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goshi N, Morgan RK, Lein PJ, Seker E.A primary neural cell culture model to study neuron, astrocyte, and microglia interactions in neuroinflammation. Journal of neuroinflammation. 17 (1), 155–155, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roqué PJ, Costa LG Co‐Culture of Neurons and Microglia. Current Protocols in Toxicology. 74 (1), 11.24.11–11.24.17, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Warre-Cornish K.et al. Interferon-γ signaling in human iPSC–derived neurons recapitulates neurodevelopmental disorder phenotypes. Science advances. 6 (34), eaay9506-eaay9506, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.