Abstract
As a result of the Coronavirus Disease 2019 (Covid-19) pandemic the use of telemedicine and remote assessments for patients has increased exponentially, enabling healthcare professionals to reduce the need for in-person clinical visits and, consequently, reduce the exposure to the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). This development has been aided by increased guidance on digital health technologies and cybersecurity measures, as well as reimbursement options within healthcare systems. Having been able to continue to connect with people with Parkinson's Disease (PwP, PD) has been crucial, since many saw their symptoms worsen over the pandemic. Inspite of the success of telemedicine, sometimes even enabling delivery of treatment and research, further validation and a unified framework are necessary to measure the true benefit to both clinical outcomes and health economics. Moreover, the use of telemedicine seems to have been biased towards people from a white background, those with higher education, and reliable internet connections. As such, efforts should be pursued by being inclusive of all PwP, regardless of geographical area and ethnic background. In this chapter, we describe the effect he Covid-19 pandemic has had on the use of telemedicine for care and research in people with PD, the limiting factors for further rollout, and how telemedicine might develop further.
Keywords: Parkinson's disease, Covid-19, SARS-CoV-2, Telemedicine, Wearables
1. Introduction
As a result of the Coronavirus Disease 2019 (Covid-19) pandemic the use of telemedicine and remote assessments for patients has increased exponentially, including the introduction and use of interdisciplinary telehealth services (Ben-Pazi et al., 2018; Cubo, Hassan, Bloem, & Mari, 2020). Telemedicine has enabled the reduction in the need for in-person clinical visits and has, consequently, reduced exposure to the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). This development was further aided by the increased guidance on digital health technologies (AAN, 2020; Society, 2020) and cybersecurity measures, as well as expanded reimbursement options within healthcare systems (Hassan et al., 2020; Rockwell & Gilroy, 2020). In addition, over the course of the pandemic the advice related to data security management and data protection for video conferencing has become more clear (John & Wellmann, 2020). Moving to remote assessments, care delivery, and clinical appointments was crucial, since lockdowns, as imposed in many countries during the pandemic, had severely detrimental effects on people with Parkinson's Disease (PwP, PD). In a large study with over 2500 PwP, over 40% reported a worsening of symptoms during lockdown, with especially tremor, pain, and rigidity, but also psychic state worsening (Fabbri et al., 2021).
Telemedicine may continue to be necessary, possibly also in relation to future pandemics or other global public health problems, given the option of rapid mobilization of telemedicine (Hassan et al., 2020). Different definitions exist of telemedicine, often also referred to as telehealth or digital health (eHealth). In this respect, the Royal College of Nursing in the United Kingdom provides a useful definition and defines eHealth as technology-based means to empower, promote and facilitate health and wellbeing of individuals, their families and communities (Royal College of Nursing, 2022), offering an alternative to classical face-to-face consultations. Nonetheless, not all patients seem keen on continuing with remote assessments beyond the Covid-19 pandemic, with numbers ranging between 26% and 48% (de Rus Jacquet et al., 2021), necessitating further improvements to the delivery of remote care. In this respect also the delivery of remote care needs to be taken into account, as, e.g., during telephone consultation medication changes are less likely to take place than compared to in-person settings (Ahmad & Postuma, 2021). However, with pressure on hospitals and staff and the eventual almost complete suspension of all outpatient face-to-face appointments due to Covid-19, implementation of telemedicine as the primary care management method has seen a rapid up-scale (Kichloo et al., 2020; Peine et al., 2020).
In this book chapter, we review the evidence for telemedicine and remote assessments for PD and how the Covid-19 pandemic has highlighted the need and underlined the feasibility of such assessments. The use of technology in healthcare can be broadly categorized into two entities: patient-facing and professional services. The former concerns the means to deliver safe, secure, effective and high-quality care to the patients, while the latter focuses on the use of technology to educate staff and streamline or improve the care delivered to the patients.
2. Patient-facing services
With some literature suggesting a wide array of benefits to home-based patient consultations, the proposal for the use of technology to deliver patient care in PD has been made in the years preceding the outbreak of the pandemic (Dorsey et al., 2016; Espay et al., 2016). The call for home-based care has identified six essential features for consideration to deliver a truly patient-centered care: location, driving, mobility, cognition, disease course, and caregivers (Dorsey et al., 2016). It has been highlighted that access to specialist services is limited to those with the ability to physically attend appointments, which further deepens the disparity in the quality of care provided to the patients. However, with most non-urgent outpatient services being moved to telemedicine, patients in remote locations were able to access the multidisciplinary services at their doorstep, which they would not have otherwise had a chance to utilize. For example, specialist referrals and attending multiple appointments far away from home had no longer been considered an issue, as the appointments were now conducted remotely. In addition, the availability of virtual appointments, irrespective of lockdowns and recommendations regarding shielding, ensured regular follow-ups and, therefore, accurate and adequate management. Currently, models of care for remote assessments are being proposed to ensure a uniform basic structure of the consultations, and that both the motor and non-motor concerns are addressed in PwP (Larson, Schneider, & Simuni, 2021; van Munster et al., 2021).
The increased implementation and availability of telehealth allowed healthcare professionals to provide their services to patients who otherwise would not be able to receive the care, worsened by lockdowns limitations or even eliminating in person contact. Especially care and nursing homes have been reported to have been particularly affected given the vulnerability of their populations (Solis, Franco-Paredes, Henao-Martínez, Krsak, & Zimmer, 2020), with some forced to go into full lockdowns with staff having to stay on-site, as the risk of viral transmission remained high. Here, remote services, conducted via means of telehealth, played a vital role in ensuring that these patients were not without review and treatment advice with some preliminary findings showing that in particular, psychiatric, geriatric and palliative care can be provided effectively through telemedicine (Groom, McCarthy, Stimpfel, & Brody, 2021). As such, we have moved away from the rapid and improvised transition from in-person visits to telemedicine at the start of the pandemic to a global increase in the use of telemedicine in movement disorders and PD (Hassan et al., 2020), with some consensus for the delivery format. Currently, policies are varied and flexible, and e.g., in the United States of America (USA) flexibility in platform selection exists (Larson, Schneider, & Simuni, 2021). As a consequence, telemedicine use among PwP increased from 9.7% prior to the pandemic to 63.5% during the pandemic (Feeney et al., 2021). Even management and evaluation of eligibility criteria for device-aided therapies has shifted to telemedicine (Fasano et al., 2020; York et al., 2021).
Other outcomes of the transition to telehealth have been observed in participation of “hard-to-reach” populations. Substantial differences in healthcare access and utilization existed in the USA prior to the Covid-19 pandemic. Here, one study found that Hispanic patients were 40% less likely and Black patients 30% less likely than white patients to see an outpatient neurologist (Saadi, Himmelstein, Woolhandler, & Mejia, 2017), along with a lower referral rate to PD specialists compared to white men (Willis, Schootman, Evanoff, Perlmutter, & Racette, 2011). Moreover, pre-pandemic newly diagnosed Black PwP were up to four times less likely than white patients to be initiated on treatment (12% and 38%, respectively) (Dahodwala, Xie, Noll, Siderowf, & Mandell, 2009). The pandemic seems to have exacerbated disparities in care access, as telemedicine use was highest among those with higher incomes, higher levels of education, and white PwP (Feeney et al., 2021). Similarly, another study has found that the percentage of telemedicine visits compared to face-to-face visits increased for white PwP and decreased for Black PwP (Esper et al., 2021).
3. Videoconferencing and assessments via video systems
The evidence and options behind videoconferencing software for assessment of movement disorder patients have been recently reviewed by Cubo et al. (2021). The authors were able to identify 26 videoconferencing software programs that were available for remote assessment. Of these, half were specifically designed for general healthcare, of which 23.0% were compliant with European and US regulations (including General Data Protection Regulation, GDPR), and 19.2% provided information regarding security (Table 1 ). Limiting factors to videoconferencing and video assessments include slow internet speed, and in some parts of the world, the limited availability of smart phones, but also reduced dexterity impacting on device control (Garg et al., 2021).
Table 1.
Applications for videoconferencing.
| Application | Features |
Security |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chat | Call type | File share | Screen share | Healthcare based | Pricing | Supported OS and platforms | Communications protection | Extra security | Security in group meetings | Security standards compliance | |
| Facebook messenger | √ | Video | √ | X | X | Free | Windows, MacOs, iOS, Android | E2EE | 2FA | Invitation, Admin control | SOC2, GDPR |
| FaceTime | √ | Video | X | X | X | Free | MacOs. iOs | E2EE | 2FA, Face ID and iPhone security | X | ? |
| Google Duo | X | Video | X | X | X | Free | Movil based: Android, iOs, Web browser-based | E2EE | 2FA, Google Account security | Invitation and user block option | HIPAA - BAA, GDPR |
| Google Hangouts | √ | Video | √ | √ | √ | Contact sales | Android, iOs, Web browser-based | IETF, SRTP and DTLS client-Server | 2FA, APP, SSO and Google's MFA | Invitation, admin control PIN | HIPAA, HITRUST, SOC2, GDPR |
| Jitsi Meet | √ | Video | √ | √ | X | Free and License | Windows, Linux, MacOs, iOS, Android | E2EE DTLS-SRTP | X | Password Admin control | ? |
| Line | √ | Video | √ | √ | X | Free | Windows, MacOs, iOS, Android | E2EE | X | Invitation | ? |
| Signal | √ | Video | √ | X | X | Free | Windows, Linux, MacOs, iOS, Android | E2EE | Screen lock | X | X |
| Skype Business | √ | Video | √ | √ | X | License | Windows, Linux, MacOs, iOS, Android | E2EE | 2FA | Invitation, Admin control | GDPR, HIPAA, HITRUST, HITECH, CCPA. |
| Telegram | √ | Video | X | X | X | Free | Windows, Linux, MacOs, iOS, Android | E2EE | 2FA, block code, secret chats, and active sessions | X | GDPR |
| √ | Video | √ | X | X | Free and License | Windows, Web browser-based, MacOs, iOS, Android | TLS client-Server | X | X | EEA | |
| √ | Video | √ | X | X | Free | Windows, Web browser-based, MacOs, iOS, Android | E2EE | 2FA | Invitation | GDPR, EEA | |
| Zoom | √ | Video | √ | √ | √ | License | Windows, Linux, MacOs, iOS, Android | E2EE, DTLS | 2FA, SSO | Invitation, Password, Admin control | HIPAA - BAA, PHIPA/PIPEDA, SOC2 |
| Teams | √ | Video | √ | √ | √ | License | Windows, Linux, MacOs, iOS, Android, Web browser-based | E2EE | 2FA | Invitation, Password, Admin control | HIPAA, HITECH, SOC2, HITRUST, GDPR |
Abbreviations: √, available; X, not available; ?, unknown; 2FA, two factor authentication; APP, advanced protection program; BAA, business associate agreement; CCPA, California Consumer Privacy Act; DTLS, datagram transport layer security; E2EE, end-to-end encryption; EEA, European Economic Area; GDPR, general data protection regulation; HIPAA, hardware as a service program; HITECH, Health Information Technology for Economic and Clinical Health Act; HITRUST, prescriptive set of controls that meet the requirements of multiple regulations and standards; IETF, internet engineering task force; MFA, multi-factor authentication; PHIPA, Personal Health Information Protection Act; PIPEDA, Personal Information Protection and Electronic Documents Act; SRTP, secure real-time transport protocol; SOC, system and organization control; SSO, single sign-on; TLS, transport layer security.
Adapted from Cubo, E., Arnaiz-Rodriguez, A., Arnaiz-González, Á., Díez-Pastor, J. F., Spindler, M., Cardozo, A., … Bloem, B. R. (2021). Videoconferencing software options for telemedicine: A review for movement disorder neurologists. Frontiers in Neurology, 12, 745917. doi:10.3389/fneur.2021.745917.
A field related to telemedicine is that of home videos. Although such home videos appear common place in the field of epilepsy, for movement disorders and PD this appears to be less pronounced. In one small study looking at the value of home videos for movement disorders, it was shown that out of 20 home videos, 50% were determined to be of additional clinical value and in 62.4% of evaluations it was possible to identify the phenomenology from the home videos and were found to be consistent with the final diagnosis. In this respect, it is also important to note that video quality was a key determinant for identifying the correct phenomenology; videos rated as ‘poor quality’ had significantly lower odds of leading to a correct phenomenology (Billnitzer & Jankovic, 2021).
4. Additional telemedicine assessments
In a cohort study of 116 PD outpatients using the telemedicine tool “myParkinsoncoach,” involving periodic monitoring, feedback, knowledge modules, and text message functionality. By using this tool, a 29% reduction in need for outpatient visits was observed in the year after introducing the tool compared to the year before introduction, coinciding with a 39% reduction in overall PD-related healthcare costs. The time needed to be dedicated to the tool monitoring and follow-up activities was on average of 15.5 min per patient per month (Wijers, Hochstenbach, & Tissingh, 2021). Similarly, in another video-based study in 22 PwP who underwent three non-motor assessments and a modified version of the Movement Disorder Society Unified Parkinson's Disease Rating Scale part III (MDS-UPDRS III), showed high satisfaction (100%) among patients, even though the duration to complete the visits was longer (41.3 min for video assessment and 17.5 min for non-motor assessment via telephone). Moreover, in some studies there was an increase in recruitment numbers following the switch to a virtual environment (Quinn, Macpherson, Long, & Shah, 2020).
Interestingly, the estimated costs for the remote assessments were 20-fold lower than for in-person visits (Xu et al., 2021). The latter seems to be backed by other studies (Delgoshaei et al., 2017), although this is not consistent with some studies only reporting increased patient satisfaction without a significant cost reduction (Snoswell et al., 2020). Assessments which are not possible to perform over video, such as rigidity and postural stability, can be complemented with the use of wearable sensors. For example, Safarpour and colleagues showed that, using three inertial sensors measuring over the period of a week, number of walking bouts and turns were significantly associated with the rigidity subscore of the MDS-UPDRS and that the number of turns, foot pitch angle, and sway area while standing were associated with the postural stability and gait subscore (Safarpour et al., 2021).
Questions might arise in relation to the reliability and reproducibility of assessments over video, although the same could also be said for in-person visits. Nevertheless, motor examination, including finger tapping and pronation/supination, showed a high rate of rater agreement and correlations between findings made by experienced examiners were high with low variability (Luiz, Marques, Folador, & Andrade, 2021).
5. Remote delivery of treatment
In relation to delivery of treatment, and more generally to research delivery, Myers and colleagues have recently shown that recruitment of large, geographically dispersed remote cohorts from a single location was feasible, with an average study recruitment of 4.9 participants per week over 1 year across three large PD studies (Myers et al., 2021). An example of remote delivery is the “ParkinDANCE” program, where researchers adapted the in-person visits to online delivery during the Covid-19 pandemic and participants completed eight 1 h sessions of online therapeutic dancing. During the sessions, each participant was assigned their own dance teacher and selected music for the classes, resulting in high attendance (100%) with participants able to quickly adapt to online delivery with support and resources (Morris et al., 2021). The feasibility of this study was echoed in a recent systematic review of 15 studies looking at the effect of telerehabilitation on gait and balance, dexterity of the upper limbs, and speech disorders, but also quality of life and patient satisfaction, where these symptoms could be improved through the use of telemedicine (Vellata et al., 2021). Importantly, patients seem to be satisfied with remote delivery of care and research, as exemplified by the results of the Fox Insight study. It demonstrated that 97.9% of participants were satisfied with the study taking place virtually, 98.5% were willing to participate in a future observational study with virtual visits, and 76.1% were willing to participate in an interventional trial with virtual visits (Myers et al., 2021).
6. Wearable technologies
As also mentioned above, one of the drawbacks of remote outpatient visits compared to classical face-to-face appointments is the limited opportunity to assess motor and non-motor symptoms, although even in a face-to-face setting the risk of reporting bias and symptom recall may not be representative of the patient's real functioning at home (Bot et al., 2016; Ossig et al., 2016). A call for the use of wearable technology to further inform clinical assessments has therefore been made pre-pandemic, though large-scale implementation of such devices had proven difficult operationally. Fueled by the Covid-19 pandemic, and inspite of barriers to engagement, some countries have started adopting objective remote measures as tools to inform clinical assessments. Wearable sensors, such as the Parkinson's KinetiGraph™, which have been validated for use to measure some motor symptoms of PD, such as bradykinesia and dyskinesia (Chen et al., 2020; Pahwa, Bergquist, Horne, & Minshall, 2020), could play an important role in extending the clinical impression based on a telephone or a video consultation.
While wearable sensor systems may be considered costly, also taking into account that such technology might not be available in every country, they could nonetheless play an important role in clinical decisions making. Healthcare systems in countries such as Germany and Sweden now provide full funding of the remote wearable readings, and some other countries such as the UK are currently reviewing evidence to adapt the tool for use in general practice for PD. Moreover, some UK-based centers have demonstrated a good feasibility of such equipment in virtual settings during the Covid-19 pandemic (Evans, Mohamed, & Thomas, 2020). Further evidence is, however, necessary to establish cost-effectiveness, although the preliminary reports suggest that, overall, remote care utilizing wearable technology can lead to a more personalized and effective healthcare delivery (James et al., 2021).
7. Patient education
Education is an important aspect of empowering patients in their care. With shielding having been advised for PwP during the pandemic, most educational seminars and meetings had been moved online to avoid a gap in knowledge delivery, especially for individuals newly diagnosed with PD. This had a significant positive impact on the patients, given that the resources which once were only available locally, could be accessed from anywhere. For example, the King's Parkinson's Educational Evening Clinics, organized by Prof K. Ray Chaudhuri at the Parkinson's Foundation Centre of Excellence at King's College Hospital in London have seen an increase in attendance, from a smaller number of patients who could make their way to the hospital site physically, to a larger number, as more people were able to join the online meeting. In a similar manner, educational meetings for specific aspects of living with PD, such as consideration of advanced therapies, like the levodopa-carbidopa intestinal gel (LCIG) infusion therapy, had been organized and widely publicized, and given its accessibility online, well attended by both patients and clinicians who wished to learn more about the therapies. Associations of PwP, such as the American Parkinson Disease Association (APDA) or the European Parkinson Disease Association (EPDA), have not only created event calendars outlining all the educational online events, but have also started blog and vlog entries and have organized structured meetings based on the needs expressed by patients online. The UK-based Parkinson's Disease Nurse Specialist Association has contributed to a multitude of free accessible online meetings organized for PwP, sharing their knowledge and expertise on the topics relevant to PD during the pandemic.
In addition, in a recent qualitative study, Zipprich and colleagues demonstrated that 30% of the participants had insufficient knowledge and understanding of Covid-19 regulations and preventative measures (Zipprich, Teschner, Witte, Schönenberg, & Prell, 2020), highlighting the need for robust education about the current issues outside of the direct management of PD as a condition. To that end, a recent systematic review recommended a proactive approach to education of PwP regarding Covid-19, including infection prevention (Kubota & Kuroda, 2021). It is therefore clear that technology plays a vital role in the patient education, which is an integral part of effective care management.
Lastly, celebratory events such as the World Parkinson's day, which always provide an opportunity for education, have also moved to online platforms, therefore, becoming more available globally, rather than just locally. Anecdotal feedback demonstrates that PwP, as well as their carers and families, have found the accessibility of online educational events helpful in times of uncertainty and have reported that the role of PD specialists, including the PD Nurse Specialists (PNS), has been instrumental in providing the freely available resources and ensuring that these are accessible.
8. Communication between professionals
Electronic patient records and referrals have been a part of standard practice in many countries, though data sharing and privacy concerns have impacted the extent of implementation of services nationally in many countries. With Microsoft Teams deemed a secure platform for sharing of confidential data, multidisciplinary meetings could continue in the era of social distancing, therefore enabling PNS to effectively engage all the specialists required to provide personalized care, essential to an effective management of PwP (Titova & Chaudhuri, 2017).
9. Limitations and future of telehealth in Parkinson's disease
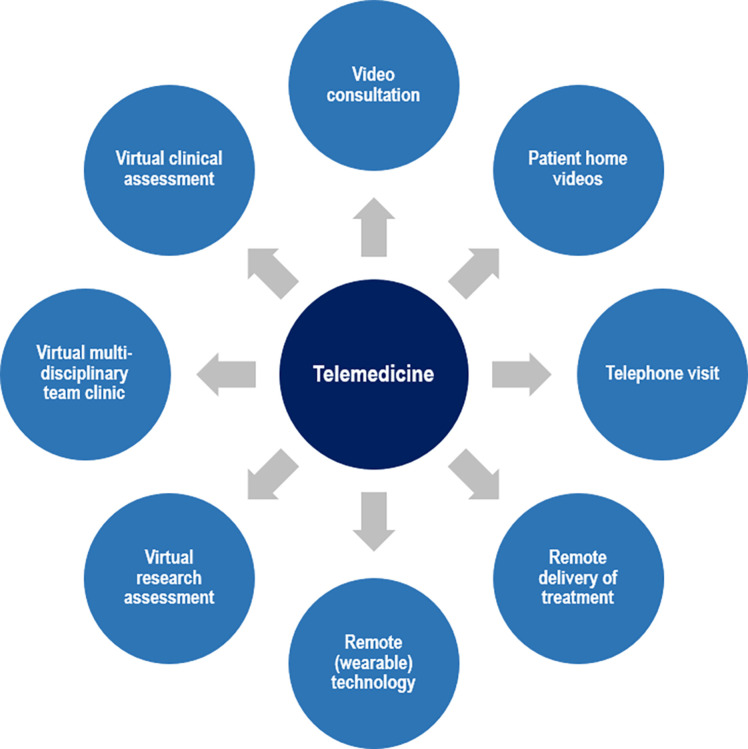
Despite clear progress that has been made with the different aspects of telehealth in PwP (Fig. 1 ) over the course of the Covid-19 pandemic, it is not without its drawbacks. One of the major limitations is the access to the appropriate technology. For example, in many suburban and remote locations, access to internet remains limited and patients may not always own mobile devices with adequate system requirements and features, such as camera, to fully engage in a video consultation with a clinician. Other factors include slow internet speed, and in certain areas, the limited availability of smart phones, but also patient-related factors, such as reduced dexterity and age, impacting on device control (Garg et al., 2021; Scott Kruse et al., 2018). Moreover, cognitive decline, a prominent non-motor symptom present in the majority of PwP across the disease pan (Aarsland et al., 2017, Aarsland et al., 2021), may be a major barrier to implementation of remote care in PD. Finally, the disparities related to healthcare access by PwP from ethnic minority backgrounds need to be taken into account (Mantri & Mitchell, 2021). These factors (Table 2 ) together can, therefore, further drive the disparity between patients and ultimately lead to a difference in the care provided to individuals in different economic situations, thus, creating a digital divide, which could leave the most vulnerable patients at risk (Eyrich, Andino, & Fessell, 2021).
Fig. 1.
Aspects of telemedicine in the care for people with Parkinson's disease.
Table 2.
Benefits and barriers of telehealth in Parkinson's disease.
| Benefits of telehealth | Barriers | |
|---|---|---|
| Integration of telehealth into healthcare systems |
|
|
| Support for PwP |
|
|
| Support for carers |
|
|
Abbreviations: PwP, people with Parkinson's disease.
Modified from Valdovinos, B. Y., Modica, J. S., & Schneider, R. B. (2022). Moving forward from the COVID-19 pandemic: Needed changes in movement disorders care and research. Current Neurology and Neuroscience Reports, 1–10. doi:10.1007/s11910-022-01178-7.
Further areas of improvement include social connection and physical activity in overall well-being, helping PwP to stay connected (Macchi et al., 2021). One strategy to achieve this might be social prescribing, involving the connection of PwP with non-medical services (Alderwick, Gottlieb, Fichtenberg, & Adler, 2018), exemplified by the Togetherness Program at CareMore and the Veteran's Administration Compassionate Contact Corps Program in the USA, which include proactive phone calls and visits to isolated patients (Subramanian, Farahnik, & Mischley, 2020). Also virtual support groups may help to improve social connection of PwP and carers, including programs to help strengthen coping strategies and manage anticipatory grief (Chaudhuri et al., 2021), lifestyle changes, and enhancement of medication adherence (Yogev-Seligmann & Kafri, 2021). Finally, targeted education for caregivers may improve self-management and self-efficacy (Duits, Boots, Mulders, Moonen, & Vugt, 2021).
10. Conclusions
Telemedicine has demonstrated its success in providing access for patients with movement disorders to clinic services and even treatment during the time of the Covid-19 pandemic (Ben-Pazi et al., 2018). Nonetheless, further validation and a unified framework are necessary to measure the true benefit to both clinical outcomes and health economics. The focus should be on creating more robust healthcare systems by optimizing interdisciplinary care models incorporating telehealth, developing novel ways to remotely manage and initiate device-aided therapies, and developing clinical programs to encourage self-management skills and provide access to social support, including that of carers of PwP. These efforts should be pursued by being inclusive of all PwP, regardless of geographical area and ethnic and financial background.
References
- AAN 2020. https://www.aan.com/practice/telemedicine
- Aarsland D., Batzu L., Halliday G.M., Geurtsen G.J., Ballard C., Ray Chaudhuri K., et al. Parkinson disease-associated cognitive impairment. Nature Reviews. Disease Primers. 2021;7(1):47. doi: 10.1038/s41572-021-00280-3. [DOI] [PubMed] [Google Scholar]
- Aarsland D., Creese B., Politis M., Chaudhuri K.R., Ffytche D.H., Weintraub D., et al. Cognitive decline in Parkinson disease. Nature Reviews. Neurology. 2017;13(4):217–231. doi: 10.1038/nrneurol.2017.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad F.A., Postuma R.B. Telephone visit efficacy for Parkinson's disease during the COVID-19 pandemic. Clinical Parkinsonism & Related Disorders. 2021;5 doi: 10.1016/j.prdoa.2021.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderwick H.A.J., Gottlieb L.M., Fichtenberg C.M., Adler N.E. Social prescribing in the U.S. and England: Emerging interventions to address patients' social needs. American Journal of Preventive Medicine. 2018;54(5):715–718. doi: 10.1016/j.amepre.2018.01.039. [DOI] [PubMed] [Google Scholar]
- Ben-Pazi H., Browne P., Chan P., Cubo E., Guttman M., Hassan A., et al. The promise of telemedicine for movement disorders: An interdisciplinary approach. Current Neurology and Neuroscience Reports. 2018;18(5):26. doi: 10.1007/s11910-018-0834-6. [DOI] [PubMed] [Google Scholar]
- Billnitzer A., Jankovic J. The clinical value of patient home videos in movement disorders. Tremor and Other Hyperkinetic Movement (New York, N.Y.) 2021;11:37. doi: 10.5334/tohm.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bot B.M., Suver C., Neto E.C., Kellen M., Klein A., Bare C., et al. The mPower study, Parkinson disease mobile data collected using ResearchKit. Scientific Data. 2016;3 doi: 10.1038/sdata.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri K.R., Rukavina K., McConvey V., Antonini A., Lorenzl S., Bhidayasiri R., et al. The impact of COVID-19 on palliative care for people with Parkinson's and response to future pandemics. Expert Review of Neurotherapeutics. 2021;21(6):615–623. doi: 10.1080/14737175.2021.1923480. [DOI] [PubMed] [Google Scholar]
- Chen L., Cai G., Weng H., Yu J., Yang Y., Huang X., et al. More sensitive identification for bradykinesia compared to tremors in Parkinson's disease based on Parkinson's KinetiGraph (PKG) Frontiers in Aging Neuroscience. 2020;12 doi: 10.3389/fnagi.2020.594701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cubo E., Arnaiz-Rodriguez A., Arnaiz-González Á., Díez-Pastor J.F., Spindler M., Cardozo A., et al. Videoconferencing software options for telemedicine: A review for movement disorder neurologists. Frontiers in Neurology. 2021;12 doi: 10.3389/fneur.2021.745917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cubo E., Hassan A., Bloem B.R., Mari Z. Implementation of telemedicine for urgent and ongoing healthcare for patients with Parkinson's disease during the COVID-19 pandemic: New expectations for the future. Journal of Parkinson's Disease. 2020;10(3):911–913. doi: 10.3233/jpd-202108. [DOI] [PubMed] [Google Scholar]
- Dahodwala N., Xie M., Noll E., Siderowf A., Mandell D.S. Treatment disparities in Parkinson's disease. Annals of Neurology. 2009;66(2):142–145. doi: 10.1002/ana.21774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Rus Jacquet A., Bogard S., Normandeau C.P., Degroot C., Postuma R.B., Dupré N., et al. Clinical perception and management of Parkinson's disease during the COVID-19 pandemic: A Canadian experience. Parkinsonism & Related Disorders. 2021;91:66–76. doi: 10.1016/j.parkreldis.2021.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgoshaei B., Mobinizadeh M., Mojdekar R., Afzal E., Arabloo J., Mohamadi E. Telemedicine: A systematic review of economic evaluations. Medical Journal of the Islamic Republic of Iran. 2017;31:113. doi: 10.14196/mjiri.31.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey E.R., Vlaanderen F.P., Engelen L.J., Kieburtz K., Zhu W., Biglan K.M., et al. Moving Parkinson care to the home. Movement Disorders. 2016;31(9):1258–1262. doi: 10.1002/mds.26744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duits A.A., Boots L.M.M., Mulders A.E.P., Moonen A.J.H., Vugt M.E. Covid proof self-management training for caregivers of patients with Parkinson's disease. Movement Disorders. 2021;36(3):529–530. doi: 10.1002/mds.28457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espay A.J., Bonato P., Nahab F.B., Maetzler W., Dean J.M., Klucken J., et al. Technology in Parkinson's disease: Challenges and opportunities. Movement Disorders. 2016;31(9):1272–1282. doi: 10.1002/mds.26642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esper C.D., Scorr L., Papazian S., Bartholomew D., Esper G.J., Factor S.A. Telemedicine in an academic movement disorders center during COVID-19. Journal of Movement Disorders. 2021;14(2):119–125. doi: 10.14802/jmd.20099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans L., Mohamed B., Thomas E.C. Using telemedicine and wearable technology to establish a virtual clinic for people with Parkinson's disease. BMJ Open Quality. 2020;9(3) doi: 10.1136/bmjoq-2020-001000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyrich N.W., Andino J.J., Fessell D.P. Bridging the digital divide to avoid leaving the most vulnerable behind. JAMA Surgery. 2021;156(8):703–704. doi: 10.1001/jamasurg.2021.1143. [DOI] [PubMed] [Google Scholar]
- Fabbri M., Leung C., Baille G., Béreau M., Brefel Courbon C., Castelnovo G., et al. A French survey on the lockdown consequences of COVID-19 pandemic in Parkinson's disease. The ERCOPARK study. Parkinsonism & Related Disorders. 2021;89:128–133. doi: 10.1016/j.parkreldis.2021.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasano A., Antonini A., Katzenschlager R., Krack P., Odin P., Evans A.H., et al. Management of advanced therapies in Parkinson's disease patients in times of humanitarian crisis: The COVID-19 experience. Movement Disorders Clinical Practice. 2020;7(4):361–372. doi: 10.1002/mdc3.12965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeney M.P., Xu Y., Surface M., Shah H., Vanegas-Arroyave N., Chan A.K., et al. The impact of COVID-19 and social distancing on people with Parkinson's disease: A survey study. NPJ Parkinson's Disease. 2021;7(1):10. doi: 10.1038/s41531-020-00153-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg D., Majumdar R., Chauhan S., Preenja R., Parihar J., Saluja A., et al. Teleneurorehabilitation among person with Parkinson's disease in India: The initial experience and barriers to implementation. Annals of Indian Academy of Neurology. 2021;24(4):536–541. doi: 10.4103/aian.AIAN_127_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groom L.L., McCarthy M.M., Stimpfel A.W., Brody A.A. Telemedicine and telehealth in nursing homes: An integrative review. Journal of the American Medical Directors Association. 2021;22(9):1784–1801.e1787. doi: 10.1016/j.jamda.2021.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan A., Mari Z., Gatto E.M., Cardozo A., Youn J., Okubadejo N., et al. Global survey on telemedicine utilization for movement disorders during the COVID-19 pandemic. Movement Disorders. 2020;35(10):1701–1711. doi: 10.1002/mds.28284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S., Ashley C., Williams A., Desborough J., McInnes S., Calma K., et al. Experiences of Australian primary healthcare nurses in using telehealth during COVID-19: A qualitative study. BMJ Open. 2021;11(8) doi: 10.1136/bmjopen-2021-049095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John N., Wellmann M. Data security management and data protection for video conferencing software. International Cybersecurity Law Review. 2020;1(1):39–50. [Google Scholar]
- Kichloo A., Albosta M., Dettloff K., Wani F., El-Amir Z., Singh J., et al. Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Family Medicine and Community Health. 2020;8(3) doi: 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubota T., Kuroda N. Exacerbation of neurological symptoms and COVID-19 severity in patients with preexisting neurological disorders and COVID-19: A systematic review. Clinical Neurology and Neurosurgery. 2021;200:106349. doi: 10.1016/j.clineuro.2020.106349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson D.N., Schneider R.B., Simuni T. A new era: The growth of video-based visits for remote management of persons with Parkinson's disease. Journal of Parkinson's Disease. 2021;11(s1):S27–s34. doi: 10.3233/jpd-202381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luiz L.M.D., Marques I.A., Folador J.P., Andrade A.O. Intra and inter-rater remote assessment of bradykinesia in Parkinson's disease. Neurologia (Engl Ed) 2021 doi: 10.1016/j.nrl.2021.08.005. [DOI] [PubMed] [Google Scholar]
- Macchi Z.A., Ayele R., Dini M., Lamira J., Katz M., Pantilat S.Z., et al. Lessons from the COVID-19 pandemic for improving outpatient neuropalliative care: A qualitative study of patient and caregiver perspectives. Palliative Medicine. 2021;35(7):1258–1266. doi: 10.1177/02692163211017383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantri S., Mitchell K.T. Falling down the digital divide: A cautionary tale. Parkinsonism & Related Disorders. 2021;93:33–34. doi: 10.1016/j.parkreldis.2021.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris M.E., Slade S.C., Wittwer J.E., Blackberry I., Haines S., Hackney M.E., et al. Online dance therapy for people with Parkinson's disease: Feasibility and impact on consumer engagement. Neurorehabilitation and Neural Repair. 2021 doi: 10.1177/15459683211046254. [DOI] [PubMed] [Google Scholar]
- Movement Disorder Society 2020. https://www.movementdisorders.org/MDS/About/Committees--Other-Groups/Telemedicine-in-Your-Movement-Disorders-Practice-A-Step-by-Step-Guide.htm
- Myers T.L., Augustine E.F., Baloga E., Daeschler M., Cannon P., Rowbotham H., et al. Recruitment for remote decentralized studies in Parkinson's disease. Journal of Parkinson's Disease. 2021 doi: 10.3233/jpd-212935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers T.L., Tarolli C.G., Adams J.L., Barbano R., Cristina Gil-Díaz M., Spear K.L., et al. Video-based Parkinson's disease assessments in a nationwide cohort of Fox Insight participants. Clinical Parkinsonism & Related Disorders. 2021;4 doi: 10.1016/j.prdoa.2021.100094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ossig C., Antonini A., Buhmann C., Classen J., Csoti I., Falkenburger B., et al. Wearable sensor-based objective assessment of motor symptoms in Parkinson's disease. Journal of Neural Transmission (Vienna) 2016;123(1):57–64. doi: 10.1007/s00702-015-1439-8. [DOI] [PubMed] [Google Scholar]
- Pahwa R., Bergquist F., Horne M., Minshall M.E. Objective measurement in Parkinson's disease: A descriptive analysis of Parkinson's symptom scores from a large population of patients across the world using the personal KinetiGraph®. Journal of Clinical Movement Disorders. 2020;7(1):5. doi: 10.1186/s40734-020-00087-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peine A., Paffenholz P., Martin L., Dohmen S., Marx G., Loosen S.H. Telemedicine in Germany during the COVID-19 pandemic: Multi-professional national survey. Journal of Medical Internet Research. 2020;22(8) doi: 10.2196/19745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn L., Macpherson C., Long K., Shah H. Promoting physical activity via telehealth in people with Parkinson disease: The path forward after the COVID-19 pandemic? Physical Therapy. 2020;100(10):1730–1736. doi: 10.1093/ptj/pzaa128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwell K.L., Gilroy A.S. Incorporating telemedicine as part of COVID-19 outbreak response systems. The American Journal of Managed Care. 2020;26(4):147–148. doi: 10.37765/ajmc.2020.42784. [DOI] [PubMed] [Google Scholar]
- Royal College of Nursing What is e-health? 2022. https://www.rcn.org.uk/clinical-topics/ehealth Retrieved from.
- Saadi A., Himmelstein D.U., Woolhandler S., Mejia N.I. Racial disparities in neurologic health care access and utilization in the United States. Neurology. 2017;88(24):2268–2275. doi: 10.1212/wnl.0000000000004025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safarpour D., Dale M.L., Shah V.V., Talman L., Carlson-Kuhta P., Horak F.B., et al. Surrogates for rigidity and PIGD MDS-UPDRS subscores using wearable sensors. Gait & Posture. 2021;91:186–191. doi: 10.1016/j.gaitpost.2021.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. Journal of Telemedicine and Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snoswell C.L., Taylor M.L., Comans T.A., Smith A.C., Gray L.C., Caffery L.J. Determining if telehealth can reduce health system costs: Scoping review. Journal of Medical Internet Research. 2020;22(10):e17298. doi: 10.2196/17298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solis J., Franco-Paredes C., Henao-Martínez A.F., Krsak M., Zimmer S.M. Structural vulnerability in the U.S. revealed in three waves of COVID-19. The American Journal of Tropical Medicine and Hygiene. 2020;103(1):25–27. doi: 10.4269/ajtmh.20-0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian I., Farahnik J., Mischley L.K. Synergy of pandemics-social isolation is associated with worsened Parkinson severity and quality of life. NPJ Parkinson's Disease. 2020;6(1):28. doi: 10.1038/s41531-020-00128-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titova N., Chaudhuri K.R. Personalized medicine in Parkinson's disease: Time to be precise. Movement Disorders. 2017;32(8):1147–1154. doi: 10.1002/mds.27027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Munster M., Stümpel J., Thieken F., Pedrosa D.J., Antonini A., Côté D., et al. Moving towards integrated and personalized care in Parkinson's disease: A framework proposal for training Parkinson nurses. Journal of Personalized Medicine. 2021;11(7):623. doi: 10.3390/jpm11070623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellata C., Belli S., Balsamo F., Giordano A., Colombo R., Maggioni G. Effectiveness of telerehabilitation on motor impairments, non-motor symptoms and compliance in patients with Parkinson's disease: A systematic review. Frontiers in Neurology. 2021;12 doi: 10.3389/fneur.2021.627999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijers A., Hochstenbach L., Tissingh G. Telemonitoring via questionnaires reduces outpatient healthcare consumption in Parkinson's disease. Movement Disorders Clinical Practice. 2021;8(7):1075–1082. doi: 10.1002/mdc3.13280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis A.W., Schootman M., Evanoff B.A., Perlmutter J.S., Racette B.A. Neurologist care in Parkinson disease: A utilization, outcomes, and survival study. Neurology. 2011;77(9):851–857. doi: 10.1212/WNL.0b013e31822c9123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Zeng Z., Qi Y., Ren K., Zhang C., Sun B., et al. Remote video-based outcome measures of patients with Parkinson's disease after deep brain stimulation using smartphones: A pilot study. Neurosurgical Focus. 2021;51(5):E2. doi: 10.3171/2021.8.Focus21383. [DOI] [PubMed] [Google Scholar]
- Yogev-Seligmann G., Kafri M. COVID-19 social distancing: Negative effects on people with Parkinson disease and their associations with confidence for self-management. BMC Neurology. 2021;21(1):284. doi: 10.1186/s12883-021-02313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- York M.K., Farace E., Pollak L., Floden D., Lin G., Wyman-Chick K., et al. The global pandemic has permanently changed the state of practice for pre-DBS neuropsychological evaluations. Parkinsonism & Related Disorders. 2021;86:135–138. doi: 10.1016/j.parkreldis.2021.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zipprich H.M., Teschner U., Witte O.W., Schönenberg A., Prell T. Knowledge, attitudes, practices, and burden during the COVID-19 pandemic in people with Parkinson's disease in Germany. Journal of Clinical Medicine. 2020;9(6):1643. doi: 10.3390/jcm9061643. [DOI] [PMC free article] [PubMed] [Google Scholar]