Abstract
Objectives:
This study sought to (1) determine the number of persons evicted from the Durham Housing Authority (DHA) over a 5-year period, (2) explore changes in the number of persons with various medical diagnoses and health care utilization patterns before and after eviction, and (3) examine how many persons evicted from DHA became literally homeless.
Design:
This was a pre/post cross-sectional quantitative study.
Sample:
Heads of households evicted from DHA properties from January 1, 2013 through December 31, 2017 were included in the study.
Measurements:
We matched people evicted by the DHA in a university health system electronic health record system to determine changes in diagnoses and health care utilization before and after eviction. We also matched the cohort in the homeless management information system to determine how many persons evicted became literally homeless.
Results:
Findings indicate statistically significant increases in persons with medical diagnoses in five of ten categories, total hospital admissions, and emergency department visits after eviction. Of the 152 people included in the study, 34 (22%) became literally homeless.
Conclusions:
Health and health care utilization patterns were different before and after eviction. Implications for clinicians are explored.
Eviction is a national crisis. From 2000 to 2016, there was an eviction filing for approximately 1 in every 17 renter households, and 1 in every 40 renter households were evicted (Eviction Lab, 2018). Studies on the health issues of persons experiencing homelessness are increasing; however, there is a dearth of literature on the health and health care utilization patterns of individuals evicted from their housing. Little is known about the health of individuals evicted from public housing and whether eviction from public housing leads to literal homelessness. This study reports (a) the characteristics of heads of households evicted from Durham Housing Authority (DHA) public housing over a 5-year period, (b) their health diagnoses, (c) their health care utilization patterns before and after eviction, and (d) their use of homeless services that would indicate literal homelessness after eviction. For the purpose of this study, we used the U.S. Department of Housing and Urban Development (HUD) Category 1 Literally Homeless definition, which includes having nighttime residence in places not intended for human habitation (e.g., emergency shelters, vehicles, unsheltered) but excludes residing temporarily with friends or family (HUD, n.d.).
Despite economic growth, income stagnation for most low- and middle-class Americans has negatively affected their ability to obtain affordable housing over the past three decades; in 2018, 50% of renters in America spent more than 30% of their income on housing (National Low Income Housing Coalition, 2019). This economic barrier to access continues to fuel a rising rate of eviction. Most evictions affect low-income Black households and may lead to homelessness (Desmond & Kimbro, 2015). A systematic review of papers published from 1900 to 2017 identified four factors associated with eviction: financial hardship, sociodemographic characteristics, substance use, and other health problems (Tsai & Huang, 2019). Eviction and the threat of eviction are linked to irreparable harm affecting physical and mental health outcomes in both children and adults (Desmond & Kimbro, 2015; Vasquez-Vera et al., 2017).
Stable housing is associated with improved health and reduced health care costs (Levy, 2018; Sandel & Desmond, 2017). Housing instability can be detrimental to health and has been associated with increased alcohol use as well as substance use disorder and exposure to violence (Tsai & Huang, 2019), an increase in sexually transmitted infections (Niccolai et al., 2019), and adverse birth outcomes (Khadka et al., 2020). Chronic illness frequently precedes eviction, but eviction can exacerbate preexisting health conditions in healthy individuals and may result in poor health outcomes (Tsai & Huang, 2019; Vasquez-Vera, et al., 2017). Eviction is also associated with suicide (Fowler et al., 2015) as well as increased utilization of services for mental health and substance use disorders (Cusack & Montgomery, 2017).
Public Housing
In 1937, the U.S. Housing Act established permanent public housing funded by the federal government under the jurisdiction of the U.S. Department of Housing and Urban Development (U.S. Department of Housing and Urban Development [HUD], 2020). The aim was to provide decent and safe rental housing for eligible low-income families, elderly persons, and persons with disabilities. Public housing is available in all 50 states. Rent for public housing is based on household income. HUD administers federal aid to local agencies (i.e., housing authorities) that manage public housing, oversee housing programs, and furnish technical and professional assistance in planning, developing, and managing these housing units. In 2017, there were approximately 2.1 million low-income Americans residing in public housing (Center on Budget and Policy Priorities, 2017).
Durham Housing Authority (DHA)
Durham Housing Authority, established in 1949, is a public housing authority funded by HUD. In order to qualify for DHA’s Public Housing program, an individual must
have an annual income at or below 80% of the median income for the area, adjusted for family size,
have at least one family member who is either a U.S. citizen or an eligible immigrant, and
provide proof of Social Security numbers for every family member.
Families are also subject to DHA’s suitability screening criteria, which include, but are not limited to, previous rental and tenancy history and past criminal activity. At the time of this study, DHA owned and managed 12 public housing communities that offered a total of 1,409 units, 50% of which were occupied by female heads of household with children.
Public housing is the housing safety net for many low-income families, elderly persons, and individuals with disabilities (Galvez et al., 2017). Evidence suggests that public housing residents have a higher prevalence of diabetes, asthma, and hypertension than persons living in other housing situations (Ruel et al., 2010) and higher rates of smoking and less fruit and vegetable consumption than general population samples (Noonan et al., 2017). Loss of housing assistance may result in homelessness or living in overcrowded housing (Smith et al., 2014), which can exacerbate health conditions or contribute to early mortality. These factors make public-housing residents particularly vulnerable to the poor health outcomes associated with eviction.
In 2017, Durham residents identified affordable housing as the top community health priority and expressed concern that eviction had reached crisis levels (Durham County, NC Department of Public Health, 2017). Between 2013 and 2016, more than 50% of Durham rental households were rent-burdened, with residents paying more than 30% of their household income towards rent (DataWorks NC, n.d.) During this period, Durham’s eviction rate decreased from 6.75% to 5.07% but remained higher than the national rate, which was under 3% (Eviction Lab, 2018). Amid this housing crisis, we could find little current data on how eviction affects the health of individuals living in public housing. Through this research project, we sought to answer the following questions:
In the 5-year period from January 1, 2013 to December 31, 2017, how many individuals were evicted from DHA public housing communities?
What were the mental and physical health conditions of the cohort before and after eviction?
What were the health service utilization patterns (i.e., ED, inpatient, and outpatient visits) before and after eviction?
How many evictions resulted in literal homelessness?
Methods
Design
This was a pre/post cross-sectional quantitative study utilizing data from three sources: financial records from DHA to identify residents who had received a writ of possession, electronic health record (EHR) data from Duke University Health System (DUHS), and homeless management information system (HMIS) data managed by the North Carolina Coalition to End Homelessness (NCCEH). Prior to data collection, data-sharing agreements were established between DHA and DUHS and between NCCEH and DUHS. The agreements are formal contracts included in the institutional review board (IRB) process that details data security measures. The Duke Health IRB approved all study activities.
Sample
The sample included heads of households who were evicted from DHA properties during the 5-year period from January 1, 2013 to December 31, 2017. Identifying the sample from DHA and then matching electronic health record data with entry into the homeless system were separate processes as described below.
Identifying the Sample within DHA
To identify individuals who had been evicted from DHA properties during the study period, financial records of court costs associated with 12 properties were searched for transaction amounts indicating a filing for eviction between January 1, 2013 and December 31, 2017. These data were exported into a Microsoft Excel spreadsheet and cross-checked across properties to capture individuals who may have moved between properties during the study period. Financial transactions were then organized chronologically. Individuals were identified when the most recent transactions on their accounts showed a charge of $126 for filing an eviction, followed by a charge of $55 for a writ of possession. Move-out dates served as confirmation; however, individuals were excluded if (a) the anticipated move-out dates were outside of the study dates, (b) clear documentation of accounting errors was found, or (c) later transactions indicated that a resolution was reached prior to the court date. An additional subset of individuals were excluded because they had transactions indicating a filing for eviction and a move-out date but no charge for the writ of possession. These individuals were assumed to have moved of their own volition before the eviction process was finalized (See Figure 1). The names, dates of birth, addresses, and phone numbers of persons considered evicted from DHA within the study period (n = 258) were shared with DUHS and NCCEH via a secure electronic platform for matching within their respective systems. Additional data obtained included address and household size and composition (i.e., number of adults and number of children).
Figure 1.
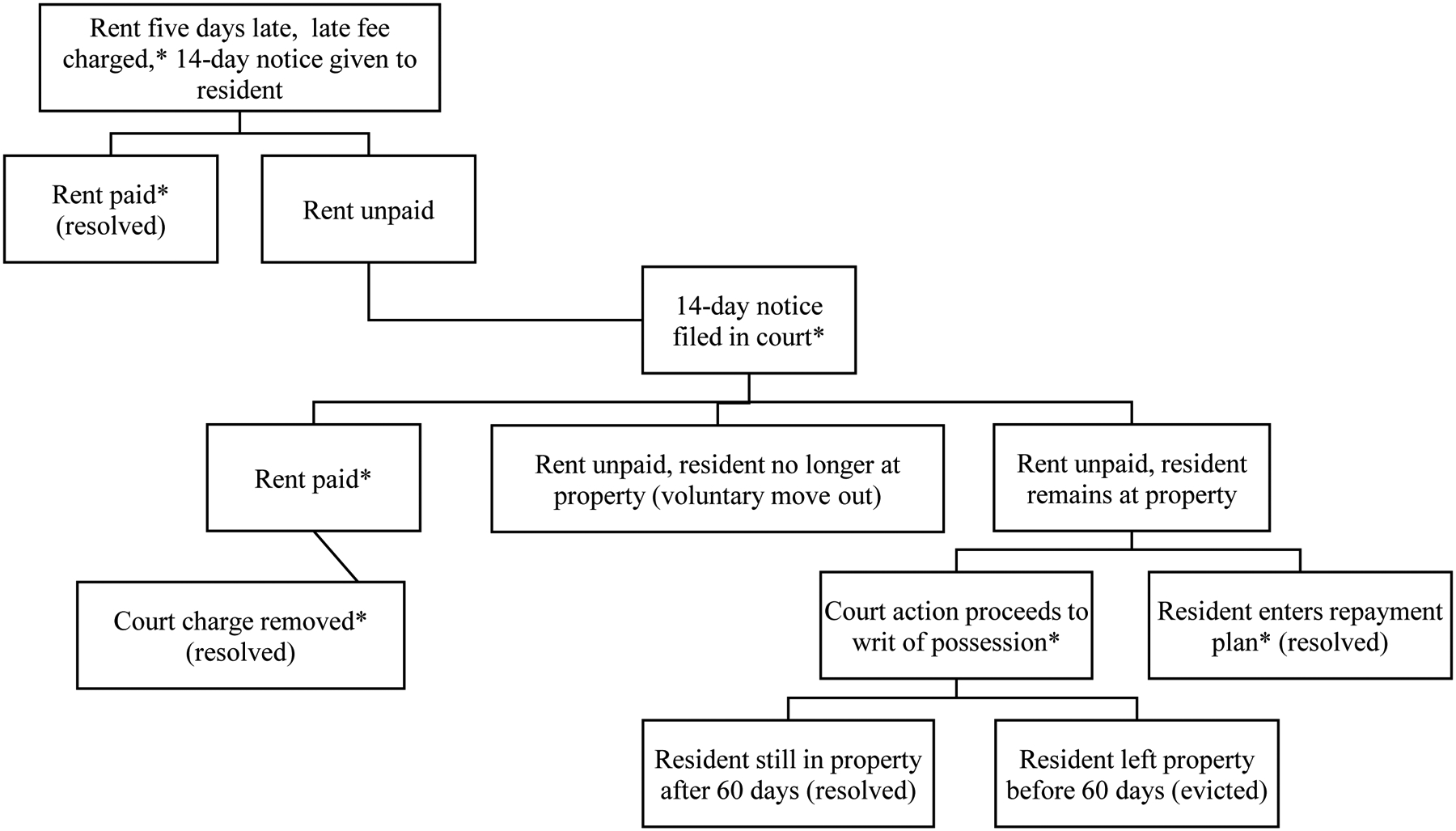
Finding persons evicted using DHA financial records
*Financial transaction associated with this event
Matching the Sample within DUHS and Abstracting Data from the EHR
DUHS is the largest medical provider in Durham, NC and operates two medical centers and numerous outpatient facilities in the region. DUHS has a relationship with the Lincoln Community Health Center, a federally qualified health center (FQHC), and they share an EHR. Persons evicted from DHA were matched within the DUHS Epic EHR with the minimum threshold identifiers of an exact match on first name, last name, and date of birth. A total of 231 evicted persons (90%) were identified and matched using this procedure. We later learned that the wrong date of birth had been given for 11 of the initial 258 evictees, which resulted in their exclusion from the study.
All available data between January 1, 2013 and December 31, 2017 were abstracted for each participant. Variables included participant characteristics (e.g., gender, race, age at encounter, insurance status), utilization data (all DUHS and FQHC encounters including date, type, and location), and diagnoses information (source, diagnosis name, ICD-9 and ICD-10 codes). Data accuracy was ensured by verifying that encounter types were restricted to valid encounters; encounters such as “Deleted Record-Please Ignore” and “Committee Review” were excluded as these reflect nonclinical entries.
Verifying Entries into Homelessness after Eviction
The names, dates of birth, and addresses of persons evicted from DHA within the study period were shared with the NCCEH for matching within the HMIS. HMIS is a technology platform for entering, storing, and transferring client data from homeless service providers to HUD. HUD-funded service providers are mandated to use the HMIS system. The NCCEH maintains the HMIS system for 3 of the 12 continuums of care (CoCs) covering 81 of the 100 North Carolina counties. A CoC is a local or regional group that plans and coordinates housing and homeless services. DHA and the primary DUHS hospitals and clinics associated with this study are located within the CoCs maintained by NCCEH. Prior to data transfer, NCCEH and the study PI received permission from the three CoC leads for HMIS data to be used in the study. All data were de-identified at the CoC and agency levels prior to transfer via a secure electronic platform. Persons evicted who had a post-eviction entry in the HMIS system were considered to have become literally homeless per the HUD definition.
Measures
Categorization of Diagnoses
International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM; hereafter referred to as ICD-10) codes are used for medical documentation and billing. It is common for patients to have multiple ICD-10 codes for each encounter. ICD-10 codes were abstracted from all encounters with corresponding diagnoses groups (e.g., blood and blood forming organs, circulatory system, compromised) and diagnosis (e.g., sickle cell trait, accelerated essential hypertension, financial difficulties). Two independent coders (DB and PC-B) used the diagnosis (n = 3272 unique names) to sort the 1CD-10 codes into 10 distinct categories: Chronic Top 7 (i.e., heart disease, cancer, chronic lung disease, stroke, Alzheimer’s disease, diabetes, chronic kidney disease), which, per the Centers for Disease Control and Prevention, are the leading causes of death and disability in the U.S.; Chronic Other (e.g., chronic pain, skin conditions, and other disorders); Acute (e.g., injuries, acute infections, other acute disorders); Mental Health (e.g., depression, stress, all serious mental illnesses); Substance Use (e.g., alcohol, tobacco, illicit substance use); Infectious Diseases (e.g., sexually transmitted illnesses, Hepatitis C, infectious diarrhea); Disabling Conditions (e.g., extremity amputation, wheelchair dependent, vision impairment); Social Diagnoses (e.g., domestic violence, financial difficulties, homeless); Pregnancy Related (e.g., gestational diabetes, gestational hypertension, pre-term labor); and Preventive (e.g., screening, contraception, vaccination). A total of 3,232 diagnoses were categorized. The remainder were not considered substantial or reflective of a medical diagnosis requiring one-time or ongoing care (e.g., “administrative encounter,” “tattoo of skin”).
Analytic Strategy
The data set was first refined to include only persons who had at least one health care encounter during the study period (n = 224), then to patients who had at least one health care encounter both before and after eviction (n = 152). We computed descriptive statistics, means, and standard deviations for interval variables as well as frequencies and percentages for categorical variables. Inpatient and ambulatory health care utilization were summarized by frequencies, means, and standard deviations.
Summaries of utilization before and after eviction date are presented (Table 3). Because a full year of data before and after eviction was not available for every participant, each model comparing the utilization and diagnosis categories was adjusted by the observed utilization time (difference in days of the date of last encounter after eviction - date of first encounter before eviction divided by 365.25). Adjusted paired t-tests were performed to measure the difference in health care utilization before and after eviction, and conditional logistic regression adjusting for observed utilization time was used to compare the presence of diagnosis categories before and after eviction. All analysis was conducted using SAS 9.4 (Cary, NC), and significance level was 0.05 for all inferential tests.
Table 3.
Comparison of participant health care utilization before and after eviction
| Variable | Before Eviction Events | After Eviction Events |
Mean Difference (After-Before)a | Std Erra | t-statistica | p a |
|---|---|---|---|---|---|---|
| Total number of hospital admissions | 115 | 271 | 0.92 | 0.35 | 2.64 | 0.009 |
| Total bed days (LOS) | 557.8 | 516.3 | −0.76 | 1.49 | −0.51 | 0.608 |
| Total Outpatient Visits | 3324 | 4205 | 2.13 | 3.36 | 0.63 | 0.528 |
| Total number of ED visits | 517 | 930 | 1.99 | 0.80 | 2.50 | 0.013 |
| 30-Day ED Revisit | 182 | 363 | 0.90 | 0.59 | 1.52 | 0.130 |
| 60-Day ED Revisit | 238 | 491 | 1.26 | 0.71 | 1.78 | 0.078 |
| 90-Day ED Revisit | 280 | 561 | 1.38 | 0.75 | 1.84 | 0.068 |
Results from a linear regression model adjusting for the observed utilization time before and after eviction.
Results
Sample characteristics are presented for heads of households (a) evicted from DHA during the study time period (n = 258), (b) identified in DUHS EHR (n = 224), (c) having at least one encounter pre- and post-eviction within the study timeframe (n = 152), and (d) identified as having experienced homelessness as noted in the HMIS system (n = 34). Across all three subgroups, participants were primarily non-Hispanic Black (> 96%) and female (>73%), which is similar to the demographics of persons living in the corresponding public housing properties sampled. The mean age for all persons evicted was 39.82 (±14.03), and about half of the participants were between the ages 25 – 40 years old. Most represented single adult households (>88%), and most households (>69.5%) had at least one child. Most participants (>83%) across all three subgroups were uninsured.
Table 2 presents the number of study participants by diagnostic category pre- and post-eviction. All diagnostic categories demonstrated an increase, with five of the ten showing a statistically significant increase following eviction: Chronic Top 7 (p = .020), Chronic Other (p = .048), Acute (p = .015), Mental Health (p = .020), and Preventive (p < .001).
Table 2.
Change in number of patients with various diagnoses before and after eviction (n=152)
| ICD-10 Category | Before eviction (n=152) | After eviction (n=152) | % change | Difference between Proportions | P-valuea |
|---|---|---|---|---|---|
| Chronic - Top 7b | 45 | 64 | 42.22 | 0.13 | 0.020 |
| Chronic – Other | 62 | 83 | 33.87 | 0.14 | 0.048 |
| Acute | 80 | 104 | 30.00 | 0.16 | 0.015 |
| Mental Health | 30 | 50 | 66.67 | 0.13 | 0.020 |
| Substance Usec | 36 | 47 | 30.56 | 0.07 | 0.373 |
| Infectious Diseases | 29 | 33 | 13.79 | 0.03 | 0.840 |
| Disabling Conditions | 8 | 11 | 37.50 | 0.02 | 0.427 |
| Social Diagnosesd | 5 | 12 | 140.00 | 0.05 | 0.137 |
| Pregnancy Related | 21 | 30 | 42.86 | 0.06 | 0.264 |
| Preventivee | 61 | 98 | 60.66 | 0.24 | <0.001 |
Results from conditional logistic regression adjusting for observed utilization time before and after eviction
Per the Center for Disease Control and Prevention, the leading causes of death and disability in the U.S (Heart disease, cancer, chronic lung disease, stroke, Alzheimer’s disease, diabetes, chronic kidney disease)
Includes tobacco
ICD-10 Z-55 through Z-65 Persons with potential health hazards related to socioeconomic and psychosocial circumstances
Physical exams, screening, contraception, vaccinations
Health care utilization pre- and post-eviction is summarized in Table 3. The total number of hospital admissions and total number of ED visits had statistically significant increases post-eviction (p = .009 and p = .013 respectively). ED revisits (i.e., a subsequent visit within the defined time frames) increased at 30, 60, and 90 days after eviction with mean differences of 1.99, 1.26, and 0.75 respectively; however, none of these changes were statistically significant (p > .05). Total bed days was the only category with a decrease; however, this change was not statistically significant (p = .608).
Of the 34 study participants who entered the homeless service system after eviction, 12 (35%) used single services while the remainder used family services. Of the service types, 10 single persons (83.3%) and 18 families (81.1%) utilized an emergency shelter. Rapid rehousing was utilized by 16 (72.7%) of families but only by one single person. The remaining housing and supportive services were not utilized as readily.
Discussion
This study characterizes residents who were evicted from public housing in Durham, North Carolina; their most common health conditions grouped by ICD-10 codes; and changes in the number of persons experiencing those health conditions before and after eviction. All diagnoses categories demonstrated increases in the number of people with those health conditions post eviction, and these increases were statistically significant in five of the ten categories. Previous studies have documented high levels of mental health disorders, substance use disorders, chronic illness, obesity, and disability in public housing residents (Digenis-Bury et al., 2008; Simning et al., 2011); however, to our knowledge, this is the first study to document increases in these types of diagnoses after eviction from public housing. The increase in preventative services was unexpected and was not reflected elsewhere in the literature, perhaps because housing instability often leads to postponing needed care, as previous studies have shown (Jaworsky et al., 2016; Reid et al., 2008). This increase may represent individuals accessing care post-eviction to connect with social workers or other clinic resources. Further study is warranted.
Overall, our sample demonstrated an increase in inpatient admissions and outpatient and ED visits post-eviction. The increased number of hospital admissions could suggest that individuals who were evicted experienced more medical issues needing hospitalization. This finding is supported in other studies that examine the effect of housing instability on acute care utilization, especially those that research whether individuals experiencing housing insecurity delay needed care (Buck et al., 2012; Harris et al., 2019; Jaworsky et al., 2016; Reid et al., 2008). The increased total number of ED visits after eviction could suggest that heads of household are experiencing acutely worse health or worse health care access after eviction. Other studies that have explored the relationship between ED utilization and housing instability have found similar results (Buck et al., 2012; Jaworsky et al., 2016; Marfil-Garza et al., 2018; Nosyk et al., 2007; Zhang et al., 2011). While the increase in 30-, 60-, and 90-day ED repeat visits was not statistically significant, there were substantial increases that may demonstrate that our cohort was cycling in and out of the health care system more regularly, using lower threshold but higher cost care in the ED.
Interestingly, although the number of hospital admissions increased, the length of stay (indicated by overall number of bed days) decreased after eviction. The change in length of stay was not significant, but the decrease represents an interesting finding as previous studies have demonstrated that hospital stays are lengthened by factors such as low socioeconomic status and lack of social support (Lam et al., 2016; Lin et al., 2015; Rollins et al., 2012). In fact, homelessness is associated with increased length of inpatient stay (Hwang et al., 2011). Lack of a stable residence to which a person can be discharged, along with the worsening material hardship associated with eviction, likely provide impediments to earlier discharge after a hospital admission. There are a variety of interventions such as medical respite programs for homeless patients that have been tested to improve care transitions for housing unstable patients, and there is evidence that such programs can decrease the number of inpatient days (Biederman et al., 2019). It is possible that after eviction, programs such as these were utilized to help coordinate care. The decrease we found may not be fully explained by this possibility and deserves further investigation.
In our study, 34 (13%) heads of households who were evicted used homeless services, indicating literal homelessness status. While it is often assumed that eviction leads to homelessness, there are few empirical U.S. studies to substantiate this claim. A Minnesota study demonstrated that about 17% of Hennepin County residents who were evicted entered the shelter system within the following 3-year period, with the majority entering the system during the year after eviction (Holdener et al., 2018). In that study, “Black families” and “increased household size” were identified as higher risk factors for shelter entry. While our sample size did not allow for risk assessment or modeling, we noted that families had greater entry into homeless services than single individuals, and that all persons with HMIS entry in our study were Black. Nonetheless, both studies demonstrate that eviction may lead to homelessness, and suggests this may be particularly true for Black families. Because homeless persons tend to have worse health and increased mortality compared to their housed peers (Fazel et al., 2014), eviction may increase health disparities. Further research to explore housing and health trajectories of persons who lose their housing through eviction is warranted.
Implications for Public Health Nurses
Social context influences health. It is imperative that clinicians explore and document social context with their patients, particularly in cases of worsening health. Addressing social determinants of health is increasingly prioritized by clinicians and health care practices across the country. However, as demonstrated in this study, documentation remains a challenge. Although the number of social diagnoses increased after eviction, less than 8% of our study participants had a documented social diagnosis reflecting housing instability. Previous studies have demonstrated low utilization of social diagnoses ICD-9 and ICD-10 codes (Biederman et al., 2019; Torres et al., 2017). Numerous groups and agencies, including the American Hospital Association and American Medical Association, advocate the use of social diagnoses ICD-10 codes and acknowledge their underuse. Challenges in documentation of social factors is common; one study of over 100 community health centers found significant variation in how practices screened for and documented social determinants of health as well as in the number of patients screened (Cottrell et al., 2019). Clinics and hospital systems should develop standardized protocols to allow clinicians (e.g., registered nurses, social workers) to document social diagnoses with ICD-10 codes in order to reduce provider (i.e., physician, nurse practitioner, physician assistant) burden. Such protocols exist in the University of Wisconsin Health System (G. Klinkner, personal communication, March 21, 2017) and the Duke Outpatient Clinic (J. Gamble, personal communication, September 17, 2020).
Limitations
This study adds to the literature on health and health care utilization of persons evicted from public housing, but it is not without limitations. The method used to determine resident eviction status from financial records may have resulted in missing individuals. Persons evicted may have used health care organizations other than those included in this study or left the area immediately after eviction, resulting in their not having both before and after eviction health data and not being included in the final analyses. Persons evicted may have moved to other locations, entered other housing arrangements that are tenuous but not considered indicative of homelessness, or not presented to homeless service agencies within the local and surrounding HMIS system catchment area, thus preventing them from being recognized as literally homeless. As the sample was from one city and state, results may not be generalizable to other locations. These limitations notwithstanding, our study results indicate that public housing residents, in general, have a substantial health burden that worsened after eviction, further strengthening the need for eviction prevention efforts. Advanced practice nurses and other health care providers need further education and support in documenting social determinants ICD-10 codes. Extending this documentation into the clinician (e.g. nursing, social work) realm can increase use of these codes and help to identify housing-insecure, homeless, or other socially disadvantaged populations.
Table 1.
Participant characteristics
| Characteristic | All persons evicted (N=258) |
In BUHS her (N=224) |
In BUHS EHR before and after evictiona (N=152) |
In HMIS after eviction (N=34) |
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Sex | ||||||||
| Female | 205 | 79.5 | 176 | 78.6 | 125 | 82.2 | 25 | 73.5 |
| Male | 53 | 20.5 | 48 | 21.4 | 27 | 17.8 | 9 | 26.5 |
| Age in years | ||||||||
| ≤ 24 | 17 | 6.6 | 17 | 7.6 | 12 | 7.9 | 4 | 11.8 |
| 25 – 40 | 133 | 51.5 | 115 | 51.3 | 73 | 48.0 | 16 | 47.1 |
| 41 – 60 | 92 | 35.7 | 79 | 35.3 | 55 | 36.2 | 12 | 35.3 |
| 60+ | 16 | 6.2 | 13 | 5.8 | 12 | 7.9 | 2 | 5.9 |
| Race/Ethnicity | ||||||||
| Non-Hispanic Black | 250 | 96.9 | 218 | 97.3 | 147 | 96.7 | 34 | 100 |
| Non-Hispanic White | 5 | 1.9 | 3 | 1.3 | 3 | 2.0 | 0 | 0 |
| Otherb | 3 | 1.2 | 3 | 1.3 | 0 | 0 | 0 | 0 |
| Adults in householdc | ||||||||
| 1 | 228 | 88.4 | 198 | 88.4 | 137 | 90.1 | 32 | 94.1 |
| 2 | 23 | 8.9 | 20 | 8.9 | 11 | 7.2 | 2 | 5.9 |
| 3+ | 7 | 2.7 | 6 | 2.7 | 4 | 2.6 | 0 | 0 |
| Children in household | ||||||||
| 0 | 78 | 30.2 | 71 | 31.7 | 47 | 30.9 | 10 | 29.4 |
| 1–2 | 124 | 48 | 108 | 48.2 | 77 | 50.7 | 15 | 44.1 |
| 3–5 | 56 | 21.7 | 45 | 20.1 | 28 | 18.4 | 9 | 26.5 |
| Insurance Status | ||||||||
| Public | 20 | 8.5 | 18 | 8.0 | 10 | 6.6 | - | - |
| Private | 8 | 3.4 | 8 | 3.6 | 2 | 1.3 | - | - |
| Uninsured | 196 | 83.4 | 198 | 88.4 | 140 | 92.1 | - | - |
Individuals with at least one pre and post encounter in the BUHS EHR. Note: these individuals may have varying pre and post number of surveillance years.
Non-Hispanic two or more races and Hispanic Black/African American
Includes head of household
Table 4.
Participants using homeless services use after eviction (n=34)
| Service type1 | Singles (n=12) | Families (n=22) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Emergency shelter | 10 | 83.3 | 18 | 81.1 |
| Rapid re-housing | 1 | 8.3 | 16 | 72.7 |
| Transitional housing | 1 | 8.3 | 3 | 13.6 |
| Permanent supportive housing | 2 | 16.7 | 1 | 4.5 |
| Services only | 0 | 0 | 1 | 4.5 |
Services are not mutually exclusive; column totals may be greater than 100%.
Contributor Information
Donna J. Biederman, Duke University School of Nursing, DUMC 3322, Durham, NC 27710.
Peter Callejo-Black, University of California San Francisco, San Francisco, CA.
Christian Douglas, Duke University School of Nursing, Durham, NC.
Heather A. O’Donohue, Alumna of Duke University School of Nursing, Durham, NC.
Monica Daeges, Alumna of Duke University School of Nursing, Durham, NC.
Olamiji Sofela, Children’s Hospital Colorado, Aurora, CO
Ashanti Brown, Durham Housing Authority, Durham, NC.
Data Availability Statement:
Research data are not shared.
References
- Biederman DJ, Gamble J, Wilson S, Douglas C, & Feigal J (2019). Health care utilization following a homeless medical respite pilot program. Public Health Nursing, 36(3), 296–302. 10.1111/phn.12589 [DOI] [PubMed] [Google Scholar]
- Biederman DJ, Modarai F, Gamble J, Sloane R, Brown A, Wilson S, & Douglas C (2019). Identifying patients experiencing homelessness in an electronic health record and assessing qualification for medical respite: A five-year retrospective review. Journal of Health Care for the Poor and Underserved, 30(1), 297–309. 10.1353/hpu.2019.0022 [DOI] [PubMed] [Google Scholar]
- Buck DS, Brown CA, Mortensen K, Riggs JW, & Franzini L (2012). Comparing homeless and domiciled patients’ utilization of the Harris County, Texas public hospital system. Journal of Health Care for the Poor and Underserved, 23(4), 1660–1670. 10.1353/hpu.2012.0171 [DOI] [PubMed] [Google Scholar]
- Center on Budget and Policy Priorities. (2017, November 15). Policy basics: Public housing. https://www.cbpp.org/research/policy-basics-public-housing
- City of Durham. (2018). The Durham Human Relations Commission 2018 report on evictions crisis in Durham County. https://durhamnc.gov/DocumentCenter/View/20496/Durham-Eviction-Report-and-Recommendations---March-6-2018-?bidId=
- Cottrell EK, Dambrun K, Cowburn S, Mossman N, Bunce AE, Marino M, … Gold R (2019). Variation in electronic health record documentation of social determinants of health across a national network of community health centers. American Journal of Preventive Medicine, 57(6). 10.1016/j.amepre.2019.07.014 [DOI] [PubMed] [Google Scholar]
- Cusack M, & Montgomery AE (2017). Examining the bidirectional association between veteran homelessness and incarceration within the context of permanent supportive housing. Psychological Services, 14(2), 250–256. 10.1037/ser0000110 [DOI] [PubMed] [Google Scholar]
- DataWorks NC. (n.d.) Cost burdened renters. Durham Neighborhood Compass, https://compass.durhamnc.gov/en/compass/UNFRENT/blockgroup. Accessed 13 Feb. 2021.
- Desmond M, & Kimbro RT (2015). Eviction’s fallout: Housing, hardship, and health. Social Forces, 94(1), 295–324. 10.1093/sf/sov044 [DOI] [Google Scholar]
- Digenis-Bury EC, Brooks DR, Chen L, Ostrem M, & Horsburgh CR (2008). Use of a population-based survey to describe the health of Boston public housing residents. American Journal of Public Health, 98(1), 85–91. 10.2105/ajph.2006.094912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durham County, NC Department of Public Health. (2017). Community health assessment. https://www.dcopublichealth.org/resources/health-resources-data/community-health-assessment.
- Eviction Lab. (2018, May 11). National estimates: Eviction in America. https://evictionlab.org/national-estimates/
- Eviction Lab. (2020). COVID-19 Housing policy scorecard. https://evictionlab.org/covid-policy-scorecard/
- Fazel S, Geddes JR, & Kushel M (2014). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. The Lancet, 384(9953), 1529–1540. 10.1016/s0140-6736(14)61132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler KA, Gladden RM, Vagi KJ, Barnes J, & Frazier L (2015). Increase in suicides associated with home eviction and foreclosure during the US housing crisis: Findings from 16 national violent death reporting system states, 2005–2010. American Journal of Public Health, 105(2), 311–316. 10.2105/ajph.2014.301945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvez M, Brennan M, Meixell B, & Pendall R (2017). Housing as a safety net. Urban Institute. https://www.urban.org/sites/default/files/publication/93611/housing-as-a-safety-net_1.pdf [Google Scholar]
- Harris M, Gadermann A, Norena M, To M, Hubley AM, Aubry T, … Palepu A (2018). Residential moves and its association with substance use, healthcare needs, and acute care use among homeless and vulnerably housed persons in Canada. International Journal of Public Health, 64(3), 399–409. 10.1007/s00038-018-1167-6 [DOI] [PubMed] [Google Scholar]
- Holdener A, Nelson J, Quint L, Rea N, Svitavsky K, Uhrich M, … Zanoni C (2018). Eviction and homelessness in Hennepin County [Master’s thesis, University of Minnesota]. UMN Digital Conservancy. http://hdl.handle.net/11299/206597 [Google Scholar]
- Hwang SW, Weaver J, Aubry T, & Hoch JS (2011). Hospital costs and length of stay among homeless patients admitted to medical, surgical, and psychiatric services. Medical Care, 49(4), 350–354. 10.1097/mlr.0b013e318206c50d [DOI] [PubMed] [Google Scholar]
- Jaworsky D, Gadermann A, Duhoux A, Naismith TE, Norena M, To MJ, … Palepu A (2016). Residential stability reduces unmet health care needs and emergency department utilization among a cohort of homeless and vulnerably housed persons in Canada. Journal of Urban Health, 93(4), 666–681. 10.1007/s11524-016-0065-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadka A, Fink G, Gromis A, & McConnell M (2020). In utero exposure to threat of evictions and preterm birth: Evidence from the United States. Health Services Research, 55, 823–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam C, Arora S, & Menchine M (2016). Increased 30-day emergency department revisits among homeless patients with mental health conditions. Western Journal of Emergency Medicine, 17(5), 607–612. 10.5811/westjem.2016.6.30690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy S, Tice M, Sperduto M, Yucha R, Perler R, Huang B, … Tsai J (2018). Public health implications of evictions: Modeling the costs for landlords, tenants, and society. (Practice Based Community Health Research Reports. 16.). Yale School of Public Health. https://elischolar.library.yale.edu/ysph_pbchrr/16 [Google Scholar]
- Lin W-C, Bharel M, Zhang J, O’Connell E, & Clark RE (2015). Frequent emergency department visits and hospitalizations among homeless people with Medicaid: implications for Medicaid expansion. American Journal of Public Health, 105(S5). 10.2105/ajph.2015.302693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marfil-Garza BA, Belaunzarán-Zamudio PF, Gulias-Herrero A, Zuñiga AC, Caro-Vega Y, Kershenobich-Stalnikowitz D, & Sifuentes-Osornio J (2018). Risk factors associated with prolonged hospital length-of-stay: 18-year retrospective study of hospitalizations in a tertiary healthcare center in Mexico. Plos One, 13(11). 10.1371/journal.pone.0207203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure L, & Killeen J (2020, April 28). COVID-19 and evictions in Durham. https://dataworks-nc.org/2020/covid-19-and-evictions-in-durham/
- National Low Income Housing Coalition (2019, September 30). Census bureau releases data from 2018 ACS on cost-burdened households. https://nlihc.org/resource/census-bureau-releases-data-2018-acs-cost-burdened-households
- Niccolai LM, Blankenship KM, & Keene DE (2019). Eviction from renter-occupied households and rates of sexually transmitted infections: A county-level ecological analysis. Sexually Transmitted Diseases, 46(1), 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan D, Hartman AM, Briggs J, & Biederman DJ (2017). Collaborating with public housing residents and staff to improve health: A mixed-methods analysis. Journal of Community Health Nursing, 34(4), 203–213. 10.1080/07370016.2017.1369810 [DOI] [PubMed] [Google Scholar]
- Nosyk B, Li X, Sun H, & Anis AH (2007). The effect of homelessness on hospitalisation among patients with HIV/AIDS. AIDS Care, 19(4), 546–553. 10.1080/09540120701235669 [DOI] [PubMed] [Google Scholar]
- Reid KW, Vittinghoff E, & Kushel MB (2008). Association between the level of housing instability, economic standing and health care access: A meta-regression. Journal of Health Care for the Poor and Underserved, 19(4), 1212–1228. 10.1353/hpu.0.0068 [DOI] [PubMed] [Google Scholar]
- Rollins C, Glass NE, Perrin NA, Billhardt KA, Clough A, Barnes J, … Bloom TL (2011). Housing instability is as strong a predictor of poor health outcomes as level of danger in an abusive relationship. Journal of Interpersonal Violence, 27(4), 623–643. 10.1177/0886260511423241 [DOI] [PubMed] [Google Scholar]
- Ruel E, Oakley D, Wilson GE, & Maddox R (2010). Is public housing the cause of poor health or a safety net for the unhealthy poor? Journal of Urban Health, 87(5), 827–838. 10.1007/s11524-010-9484-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandel M, & Desmond M (2017). Investing in housing for health improves both mission and margin. JAMA, 318(23), 2291. 10.1001/jama.2017.15771 [DOI] [PubMed] [Google Scholar]
- Simning A, Wijngaarden EV, & Conwell Y (2010). Anxiety, mood, and substance use disorders in United States African-American public housing residents. Social Psychiatry and Psychiatric Epidemiology, 46(10), 983–992. 10.1007/s00127-010-0267-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RE, Popkin S, George T, & Comey J (2014). What happens to housing assistance leavers? (Low Income Working Families Paper 27). Urban Institute. https://www.huduser.gov/portal/oup/pdf/hsg_asst_leavers_rpt.pdf [Google Scholar]
- Tai DBG, Shah A, Doubeni CA, Sia IG, & Wieland ML (2020, June 20). Disproportionate impact of covid-19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases, ciaa815, 10.1093/cid/ciaa815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temporary Halt in Residential Evictions to Prevent the Further Spread of COVID-19 2020, 85. Fed. Reg 55292 (September 4, 2020). [Google Scholar]
- Torres JM, Lawlor J, Colvin JD, Sills MR, Bettenhausen JL, Davidson A, … Gottlieb LM (2017). ICD social codes. Medical Care, 55(9), 810–816. 10.1097/mlr.0000000000000764 [DOI] [PubMed] [Google Scholar]
- Tsai J, & Huang M (2019). Systematic review of psychosocial factors associated with evictions. Social Forces, 27(3), e1–e9. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Housing and Urban Development (HUD; n.d.). Definition of homeless. https://files.hudexchange.info/resources/documents/HomelessDefinition_RecordkeepingRequirementsandCriteria.pdf
- U.S. Department of Housing and Urban Development (HUD; n.d.). Key HUD statutes. https://www.hud.gov/hudprograms/keystatutes
- Vásquez-Vera H, Palència L, Magna I, Mena C, Neira J, & Borrell C (2017). The threat of home eviction and its effects on health through the equity lens: A systematic review. Social Science & Medicine, 175, 199–208. 10.1016/j.socscimed.2017.01.010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


