Abstract
Introduction
Pathogenic Escherichia coli strains cause diarrheal infection in children due to their virulence factors. A nonanalytical observational study followed by a purposive sampling technique was conducted from October 2017 to June 2018, to determine the antimicrobial susceptibility patterns and molecularly detect pathogenic Escherichia coli strains in under-five children at Wolaita Sodo town using molecular and the Kirby-Bauer disc diffusion method.
Result
In the current investigation, out of 110 stool samples, Escherichia coli was isolated in 68 (61.8%) (95% CI: 52.1–70.9%). Out of 68 Escherichia coli isolates, 61.9% of Escherichia coli isolates were resistant, 9.4% were intermediately resistant, and 28.7% were susceptible. Among the antimicrobial agents, 91.2% of Escherichia coli isolates were highly sensitive to ciprofloxacin followed by norfloxacin (86.8%). Virulence genes were detected in 55.9% (38/68) (95% CI 52.1%–70.9%) of isolates. The following genes were detected: stx1 (6 (8.8%)), stx2 (4 (5.9%)), eaeA (5 (7.4%)), eaat (14 (20.5%)), and St (4 (5.9%)). Out of 68 Escherichia coli isolates, 43 (63.2%) isolates had shown multidrug resistance patterns. Furthermore, 11.8% of Escherichia coli isolates had shown resistance to eight different drugs. The multidrug resistance index value of Diarrheagenic Escherichia coli pathotypes was greater than or equal to 0.4, which indicates the high risk of resistance.
Conclusion
This study demonstrated important pathogenic Escherichia coli strains and multidrug resistance in isolates containing virulence genes. Wise use of antimicrobials and improving the hygienic practices amongst parents of children reduce its occurrence. Therefore, appropriate usage of antimicrobial agents should also be highly practiced in hospitals.
1. Introduction
In developing countries, children, particularly those under the age of five years, are vulnerable to diarrhea, which is one of the leading causes of mortality and morbidity [1, 2], resulting in the deaths of nearly 2.6 million people each year, the majority of whom are African children [3]. In 2010, it was anticipated that over 1.7 billion episodes of diarrhea occurred worldwide, with 700,000 of those resulting in death in children under the age of five years [4, 5].
Children's diarrhea is a frequent ailment in most impoverished countries, including Ethiopia. Consumption of contaminated foods, such as undercooked meat and unpasteurized milk, close contact with reservoir animals, caregivers' lack of hand-washing with soap, lack of proper breastfeeding for children until the age of six months, and poor health infrastructure have all been linked to bacterial pathogens that cause diarrhea [6]. According to a global review, infections (sepsis, pneumonia, tetanus, and diarrhea) and preterm delivery resulted in newborn fatalities, which were responsible for 4 million neonatal deaths [7]. However, the early beginning of breastfeeding (or human milk feeding) and exclusive nursing can avoid or decrease the negative consequences of infections and preterm delivery [8].
Diarrhea syndromes can be caused by single or many etiologic agents such as bacterial, viral, or parasite diseases [9]. Enteric bacterial pathogens, and their products, are the major causes of acute diarrhea, including diarrheagenic Escherichia coli (DEC), nontyphoidal Salmonella (NTS), Shigella spp., and Vibrio cholera, among others [10, 11].
Among the causal agents of diarrhea in humans and animals, diarrheagenic Escherichia coli (DEC) is the most frequent of the numerous enteropathogenic organisms, especially in poor countries and in diarrhea-related mortality in children under the age of five [12]. These bacteria are genetically the most versatile and are the source of many plasmid and phage-mediated genes. Even though its members are typically nonpathogens that are a part of the normal microflora of the intestinal tract of humans and animals, certain subsets of this bacterial species have acquired genes that enable them to cause intestinal or extraintestinal disease [13, 14].
Diarrheagenic Escherichia coli are identified and differentiated from Escherichia coli of the intestinal flora by the presence of specific virulence markers [15]. This bacterium, which is classified under the family Enterobacteriaceae, is Gram-negative, rod-shaped, flagellated, motile, oxidase-negative, and facultatively anaerobic. It produces septicemia and diarrhea in a wide range of hosts including humans and animals [16].
Pathogenic Escherichia coli strains are divided into intestinal pathogens causing diarrhea and extraintestinal Escherichia coli (ExPEC) causing a variety of infections in both humans and animals including urinary tract infections, meningitis, and septicemia [17]. Pathogenic Escherichia coli causing diarrhea in children are also further divided into two types: enteropathogenic Escherichia coli and uropathogenic Escherichia coli. Uropathogenic Escherichia coli causes 90% of the urinary tract infection. Based on their specific virulence factors, phenotypic traits, and mechanisms by which they cause disease, DEC strains are divided into six pathotypes: enteropathogenic Escherichia coli (EPEC), enterotoxigenic Escherichia coli (ETEC), Vero toxin-producing/Shiga toxin-producing Escherichia coli (VTEC/STEC), which include its well-known subgroup enterohemorrhagic Escherichia coli (EHEC), enteroinvasive Escherichia coli (EIEC), enteroaggregative Escherichia coli (EAEC), and diffusely adherent Escherichia coli (DAEC) [18].
Improper usage of antimicrobial agents is one of the main reasons for the pathogenic bacteria to develop antibiotic resistance to the commonly used antimicrobial agents [19]. According to [20], the prevalence of antibiotic resistance among Escherichia coli isolates from patients with acute diarrhea in Egypt was 68.2%, 57.2%, and 24.2% for ampicillin, trimethoprim-sulfamethoxazole, and ampicillin-sulbactam, respectively. In contrast, studies in Vietnam found that 86.4%, 77.2%, and 19.1% of Escherichia coli isolates were resistant to resistant to ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole, respectively [21]. The widespread use of these antibiotics has resulted in an increased prevalence of resistance to these antibiotics by diarrheagenic bacteria, thereby raising concern in children, especially in developing countries [22].
Escherichia coli also represents a major reservoir of resistance genes that may be responsible for treatment failures in both human and veterinary medicine. An increasing number of resistance genes have been identified in Escherichia coli isolates during the last decades, and many of these resistance genes were acquired by horizontal gene transfer [23] or clonal transfer of resistant strains via direct contact, indirect contact, and consumption of fecally contaminated food [24].
The identification of DEC is done based on the presence of different chromosomal and/or plasmid-encoded virulence genes that are absent in commensal Escherichia coli via molecular methods [25]. Although different virulence groups of DEC can also be detected by culture, biochemical reactions, serotyping, and other phenotypic assays [26], polymerase chain reaction (PCR) has proved to be more sensitive and specific than most conventional techniques and has been used to identify DEC in several studies [27]. Antimicrobial resistance and virulence types in Escherichia coli have been studied in a variety of countries [28–34]. Limited studies on antimicrobial susceptibility patterns and molecular detection of pathogenic Escherichia coli strains in diarrheic children at Wolaita Sodo town initiated this research work [21]. Therefore, the objective of the current study was to determine antimicrobial susceptibility patterns and molecularly detect pathogenic Escherichia coli strains in diarrheic children at Wolaita Sodo town.
2. Materials and Methods
2.1. Study Area
The current research work was carried out in the Sodo Christian Hospital from October 2017 to June 2018. Wolaita Sodo is a town in the Southern nation nationalities and people of the republic (SNNPR) situated 383 kilometers from Addis Ababa. The region is bordered on the north by Damot gale woreda, on the south by Humbo woreda, on the east by Damot Wilde woreda, and on the west by Damot Sore woreda (Figure 1). It has an annual rainfall of 100–1200 mm and a temperature of 25–35°C. Its height ranges from 1650 to 2980 meters above sea level. The area is Woina-Dega (mid-altitude) at an elevation below 1600 feet, and the livestock population in the Wolaita Sodo zone includes 128,919 cattle, 29191 sheep, and 4606 equines, and 55278 poultry [35]. According to the results of the May 2007 housing and population census, Wolaita Sodo town has a population of 102,922, with 54,315 men and 48,617 females, and a 5.3% annual population growth rate. This makes Wolaita Sodo the second most populous city in South Region after Hawassa. Mixed farming, which includes the development of grain crops, cash crops, especially coffee, and animal production, is the most important economic activity [36].
Figure 1.
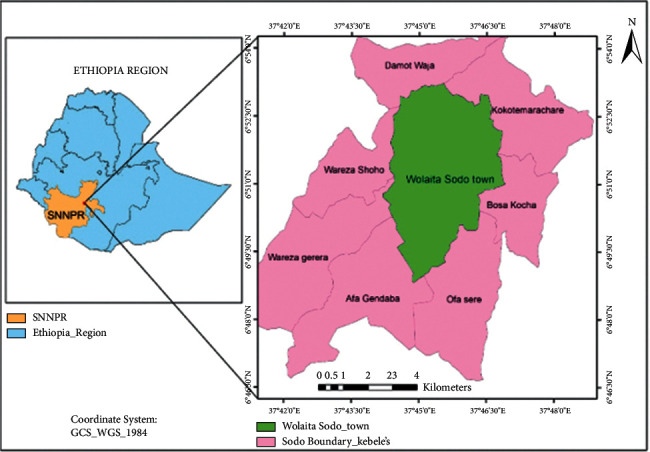
Map of the study area.
2.2. Study Population
All under-five children with diarrhea who visited Sodo Christian hospital in Wolaita Sodo town were included in the study as described by Black et al. [35]. Diarrheic children under the age of five who attended Sodo Christian Hospital with diarrhea and whose caregivers were willing to participate in the study were included in the study's sample population.
2.3. Study Design
A nonanalytical observational study starting from October 2017 to June 2018 was conducted in the Sodo Christian Hospital found in Wolaita Sodo town. The Sodo Christian hospital was chosen purposefully, based on the availability of clinical cases (diarrheic youngsters) and the willingness of the children's parents. The pediatrician provided information about the children's health. Children with normal stool consistency and/or indications of dehydration, sunken eye, diarrhea, and weakness were categorized as healthy, whereas ill children with abnormal stool consistency and/or signs of dehydration, sunken eye, diarrhea, and weakness were classified as diarrhea. The kind, features, and color of diarrhea were also documented.
2.3.1. Sample Size Determination
The selection of participants from Sodo Christian hospital and stool samples from children was based on a nonprobability purposive sampling technique. During sampling, the availability of clinical cases (diarrheic children) and the willingness of the parents of the children were the main factors considered to determine the total number of stool samples. Accordingly, 110 stool samples were collected from children that have diarrhea.
2.3.2. Sample Collection
The sample collection procedure was applied by medical laboratory technicians having the stool laboratory request of the pediatricians for diarrheic children under-five years of age who visit Sodo Christian hospital. The stool samples were collected by researchers, and it was collected from the diaper of the children. The collected stool samples were labeled properly and aseptically transported to the Wolaita Sodo regional veterinary laboratory in an icebox containing ice packs and then immediately processed for bacterial isolation.
2.3.3. Isolation and Identification of Escherichia coli
Escherichia coli was isolated and identified based on the standard procedures described by Quinn et al. [37] and the techniques recommended by the ISO [38]. After immediately arriving at the laboratory and/or overnight storage in the refrigerator at 4°C and thawing at room temperature, the samples were manually homogenized by using a vortex mixer for about 40 seconds. When there is a small number of samples in a sterile flask, 25 g of fecal samples were mixed into 225 mL of sterile buffered peptone water (Himedia, India) in a 1 : 9 ratio. The preenriched samples were homogenized in the flask for two minutes before being incubated aerobically for 24 hours at 37°C. All the study's media were prepared according to the manufacturer's instructions. The sample dilution of preenriched broth was inoculated aseptically onto sterile MacConkey agar (Himedia, India) and incubated at 37°C for 24 hours. The presence of growth on MacConkey agar was employed as the major criterion for moving on with Escherichia coli isolation and identification. A few representative Escherichia coli colonies were subcultured on Eosin methylene blue (EMB) agar medium (Himedia, India) to confirm their identity as Escherichia coli. The green metallic sheen appearance of Escherichia coli colonies on EMB was used to identify their features. For biochemical testing, all isolated colonies were maintained on a nutrient agar slant (Oxoid, England). Gram staining was used to evaluate the morphology and purity of all isolates [39], and they were subjected to the standard biochemical tests: Indole test, Methyl red (MR), Voges Proskauer (VP) test, Citrate test, and triple sugar iron. The isolates that exhibited an IMViC pattern (++−−) were presumed to be Escherichia coli isolates. All the presumed Escherichia coli isolates were subcultured on a nutrient agar slant (Oxoid, England) for antimicrobial testing.
2.3.4. Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was performed according to the “Kirby and Bauer” method on Mueller-Hinton agar medium [40], following the standard agar disk diffusion method [41] using antimicrobial disks of commonly used drugs such as Ampicillin, Chloramphenicol, Ciprofloxacin, Clindamycin, Neomycin, Norfloxacillin, Oxytetracycline Streptomycin, Sulphonamides, Tetracycline, and Trimethoprim. Following this, the diameter of the inhibition zone formed around each disc was measured using a calibrated ruler. The results were classified as sensitive, intermediate, and resistant according to the standardized table supplied by the manufacturer of the discs [41]. Also, the multidrug resistance index (MDRI) of individual isolates was calculated by dividing the number of antimicrobial agents to which the isolate was resistant by the total number of drugs to which the isolate was exposed. Values lower than 0.2 are considered low risk, while a value higher than 0.2 is considered high risk [42].
2.3.5. Molecular Characterization of Escherichia coli Isolates
(1) DNA Extraction. Bacterial DNA extraction was performed using the boiling method. A Loopful colony was taken from each medium for inoculation of Escherichia coli isolates in nutrient broth at 37°C overnight. Exactly 1.5 ml of the young nutrient broth culture was harvested and spanned by centrifugation at 13,000 rpm for 10 minutes in a sterilized Eppendorf tube. The supernatant was discarded; then, 50 µl of nuclease-free water was added to the pellet and boiled to lyse in a water bath at 95°C for 10 minutes. It was then centrifuged again as before, and an aliquot of the supernatant was transferred to another autoclaved Eppendorf tube as the test DNA template and stored at −20°c for later use in PCR experiments. Three µl of the extracted DNA was used directly as a template for PCR amplification [43].
(2) Polymerase Chain Reaction. After extraction of the target DNA, all Escherichia coli isolates were subjected to PCR to detect virulence genes. The optimized PCR protocol was carried out with a PCR mix of a 25 μl mixture containing 16 μl double distilled water, 2.5 μl 10x PCR buffer with MgCl2, 1 μl dNTP, 1 μl forward primer, 1 μl reverse primer, 0.5 μl Taq DNA polymerase (5 U/µl) (Himedia India), and 3 μl of template DNA. Negative control was performed by adding 3 μl of sterile nuclease-free water; a positive control was performed by adding 3 μl of a known DNA sample. For those strains where positive control is not available in the laboratory, pooled target DNA samples were used as a positive control. According to optimized PCR conditions, the amplification of the reaction mixtures was performed in a PCR machine, Eppendorf thermal-cycler, Biometra, Geotting, Germany. The primer sequences and optimized PCR protocol used in this work and their features are indicated in Table 1.
Table 1.
Primer sequences specific for each virulence gene, their amplicon size, and optimized PCR protocol.
| Target gene | Primer name | Sequence 5′ to 3′ | Amplicon size (bp) | PCR amplification | Escherichia coli strain detected | References | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial denaturation C/min | Denaturation °C/sec. | Annealing °C/sec | Extension °C/sec | Final extension °C/min | No. of cycle | ||||||
| eaeA | EAE1 | F: AAACAGGTGAAACTGTTGCC | 490 | 95/3 | 95/40 | 55/60 | 72/60 | 72/10 | 35 | EPEC/EHEC | [44] |
| EAE2 | R: CTCTGCAGATTAACCTCTGC | ||||||||||
| Stx 1 | EVS1 | F: ATCAGTCGTCACTCACTGGT | 110 | 95/3 | 95/40 | 57/40 | 72/30 | 72/8 | 30 | STEC/EHEC | [45] |
| EVC2 | R: CTGCTGTCACAGTGACAAA | ||||||||||
| Stx 2 | EVT1 | F: CAACACTGGATGATCTCAG | 350 | 95/3 | 95/40 | 57/40 | 72/30 | 72/8 | 30 | STEC/EHEC | |
| EVT2 | R: CCCCCTCAACTGCTAATA | ||||||||||
| Bfp | bfpA1 | F: TTCTTGGTGCTTGCGTGTCTTTT | 324 | 95/3 | 95/40 | 57/40 | 72/30 | 72/8 | 30 | Typical EPEC | [44] |
| bfpA2 | R: TTTTGTTTGTTGTATCTTTGTAA | ||||||||||
| HlyA | hlyA-1 | F: GGT GCA GCA GAA AAA GTT GTA G | 190 | 95/3 | 95/40 | 45/60 | 72/60 | 72/10 | 30 | EHEC | [46] |
| hlyA-2 | R: TCT CGC CTG ATA GTG TTT GGT a | ||||||||||
| aatA | aatA1 | F: GGT GCA GAA CAC GAT GCA | 590 | 95/3 | 95/40 | 45/60 | 72/60 | 72/10 | 30 | EAEC | [44] |
| aatA2 | R: CCA CGT CTT GTG CTA CGT | ||||||||||
| Lt | LT-1 | F: TCTCTATGTGCATACGGAGC | 696 | 95/3 | 95/40 | 53/60 | 72/30 | 72/8 | 30 | ETEC | [47] |
| LT-2 | R: CCATACTGATTGCCGCAAT | ||||||||||
| St | ST-1 | F: TGCTAAACCAGTAGAGTCTTCAAAA | 294 | 95/3 | 95/40 | 52/60 | 72/60 | 72/10 | 35 | ETEC | [48] |
| ST-2 | R:GCAGGATTACAACACAATTCACAGCAG | ||||||||||
| Dae | daeE 1 | F: GAA CGT TGG TTA ATG TGG GGT AA | 542 | 95/3 | 95/40 | 45/60 | 72/60 | 72/10 | 37 | DAEC | [49] |
| daeE 2 | R: TAT TCA CCG GTC GGT TAT CAG | ||||||||||
EPEC = enteropathogenic Escherichia coli; ETEC = enterotoxigenic Escherichia coli; STEC = shiga toxin-producing Escherichia coli; EHEC = enterohaemorrhagic Escherichia coli; EAEC = enteroaggregative Escherichia coli; DAEC = diffusely adherent Escherichia coli; EAE = effacing and attaching, Stx = shiga toxin, bp = Base pair.
(3) Agarose Gel Electrophoresis. Amplified PCR products were separated by agarose gel electrophoresis at 120 volts for 30 minutes in 1.5% agarose containing Ethidium Bromide in 1x in TBE buffer using a marker 100 bp DNA ladder (Himedia; India and Promega, Madison, Wisconsin, USA). Loading dye was used to load PCR products in each well in a gel. The products were then visualized by a UV transilluminator [50] and photographed under ultraviolet light using a digital Polaroid camera.
2.4. Data Analysis
All of the data were subject to contingency table analysis, and Pearson's Chi-square test was used to determine the statistical significance of the relationships and or associations between the virulence genes and corresponding pathogenic Escherichia coli strains. Throughout the investigation, a significance level of p < 0.05 at 95% confidence intervals was employed. All data from the laboratory tests were coded, filtered, and recorded in Microsoft Excel spreadsheet 2007 (Microsoft Corporation) before being analyzed with SPSS version 20.0 software (SPSS INC. Chicago, IL).
2.5. Ethical Considerations
This study received ethical approval from the Jimma University of Research Ethics and Review Committee. Before collecting samples, the parents or guardians of the patients were asked for verbal agreement to collect samples from their children while adhering to stringent sanitary guidelines. All of the studies were done following the Helsinki Declaration. The best practices for human care were followed, and the patients' parents or guardians were told of the study's objective and that the Jimma University of Research Ethics and Review Committee authorized the oral informed consent process.
3. Results
3.1. Pathogenic Escherichia coli Strains Identified
In the current investigation, out of 110 stool samples, Escherichia coli was isolated in 68 (61.8%) (95% CI: 52.1–70.9%). Among those Escherichia coli isolates, 38 (55.8%) were detected as harboring one or more virulence genes (Figures 2–5). Out of these, 35 (92.1%) isolates harbored one virulence gene, and the rest 3 (7.9%) isolates harbored more than one virulence gene. According to the occurrence of virulence genes, the 38 Escherichia coli isolates were classified as follows: 14 EAEC (eaat gene), 10 STEC (6 harbored stx1 gene and 4 harbored the stx2 gene), 2 EHEC (1 harbored stx 2+ eaeA genes, 1 harbored as stx 1+ eaeA genes), 5 atypical EPEC (eaeA gene), 4 ETEC (st gene), and 2 DAEC (data gene) (Table 2). All isolates were checked for the presence of the bfp gene, but none of them contained this gene. Also, neither EHEC nor STEC harbored the hlyA gene. All virulence genes detected were significantly associated (p < 0.05) with diarrheal infection due to Escherichia coli in children.
Figure 2.
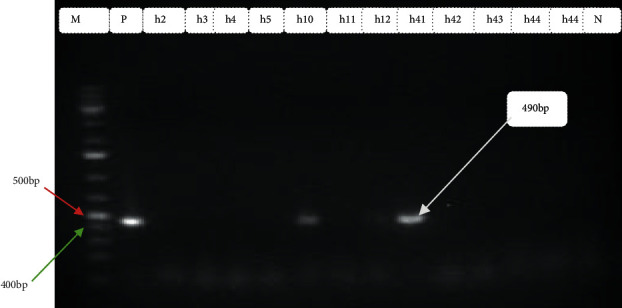
Amplification of eae gene in Escherichia coli isolates from diarrheic children: M Marker (100 bp DNA ladder) P positive control, Lane No. h10 and h41 indicate positive samples, Lane No. h2-h5, and h43-h44 indicates negative samples and N negative control.
Figure 3.
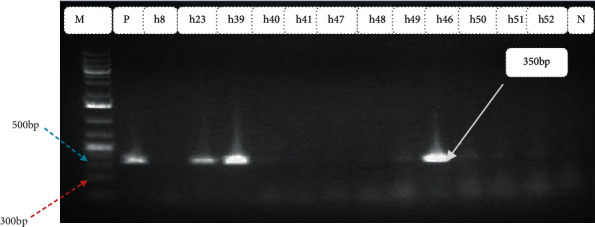
Amplification of stx1 gene in Escherichia coli isolates from diarrheic children: M Marker (100 bp DNA ladder) P positive control, Lane No. h23, h39, and h49 indicate positive samples, Lane No. h8, h40, h41, h47, h48, h49, h51, and h52 indicates negative samples and N negative control.
Figure 4.
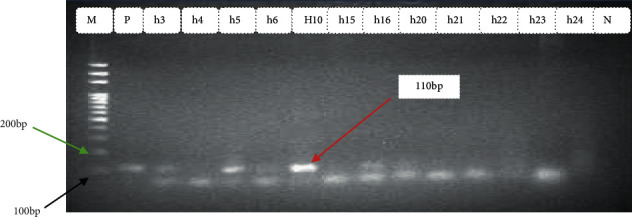
Amplification of stx2 gene in Escherichia coli isolates from diarrheic children: M Marker (100 bp DNA ladder) P positive control, Lane No. h5, and h10 indicates positive samples, Lane No. h3, h4, h6, h15, h16, and h20–h25 indicates negative samples and N negative control.
Figure 5.
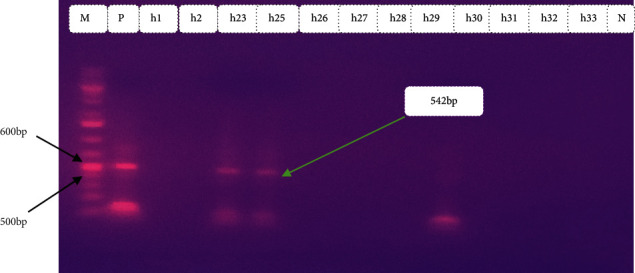
Amplification of dae gene in Escherichia coli isolates from diarrheic children: M marker (100 bp DNA ladder) P positive control, lane no. h23, and h25 indicates positive samples, lane no. h1, h2, and h26–h33 indicates negative samples and N negative control.
Table 2.
Frequency of virulence genes and corresponding pathogenic Escherichia coli strains in diarrheic children.
| Virulence genes detected | Frequency of virulence genes among Escherichia coli isolates (N = 68) | Pathogenic Escherichia coli strains | χ 2 | p-value (95% CI) |
|---|---|---|---|---|
| stx 1 | 6 (8.8%) | STEC | 15.1 | 0.02 (7.3–25.4%) |
| stx 2 | 4 (5.9%) | STEC | ||
| stx 2+ eaeA | 1 (1.5%) | EHEC | 6.8 | 0.041 (0.9–12.4%) |
| stx 1+ eaeA | 2 (2.9%) | EHEC | ||
| eaeA+ only | 5 (7.4%) | Atypical EPEC | 7.4 | 0.003 (2.4–16.3%) |
| St | 4 (5.9%) | ETEC | 10 | 0.002 (1.6–14.4%) |
| Data | 2 (2.9%) | DAEC | 9.4 | 0.01 (0.4–10.2%) |
| Eaat | 14 (20.5%) | EAEC | 13.9 | 0.01 (17.7–32.1%) |
| Total | 38 (55.9%) |
(χ2)-chie square; CI-confidence interval; p-probability.
Typical gel pictures for the specific virulence genes investigated are indicated in Figures 2–5.
3.2. Antimicrobial Susceptibility Patterns of Escherichia coli Isolates
3.2.1. Mono-Drug Resistance
The antimicrobial susceptibility patterns of 68 Escherichia coli isolates were shown in Table 3. Accordingly, the highest sensitivity to ciprofloxacin (91.2%) followed by norfloxacin (86.8%) was observed in Escherichia coli isolates. Chloramphenicol, clindamycin, neomycin, streptomycin, and norfloxacin did not show intermediate resistance, while the other tested drugs showed intermediate resistance in two or more of the tested isolates. The highest resistance was observed to neomycin (97.1%) followed by streptomycin (95.6%).
Table 3.
Antimicrobial susceptibility patterns in Escherichia coli isolates.
| Antimicrobial agents | Susceptible | Intermediate | Resistant |
|---|---|---|---|
| Ampicillin | 8 (11.8) | 12 (17.6) | 48 (70.6) |
| Chloramphenicol | 30 (44.1) | — | 38 (55.9 |
| Ciprofloxacin | 62 (91.2) | 2 (2.9) | 4 (5.9) |
| Clindamycin | 5 (7.4) | — | 63 (92.6) |
| Neomycin | 2 (2.9) | — | 66 (97.1) |
| Norfloxacillin | 59 (86.8) | — | 9 (13.2) |
| Oxytetracycline | 13 (19) | 15 (22) | 40 (58.8) |
| Streptomycin | 3 (4.4) | — | 65 (95.6) |
| Sulphonamides | 7 (10.3) | 21 (30.9) | 40 (58.8) |
| Tetracycline | 10 (14.7) | 14 (20.6) | 44 (64.7) |
| Trimethoprim | 16 (23.5) | 6 (8.8) | 46 (67.6) |
| Total (%) | 215 (28.7) | 70 (9.4) | 463 (61.9) |
3.2.2. Multidrug Resistance
Multidrug resistance patterns of the Escherichia coli isolates are shown in Table 4. Of the 68 Escherichia coli isolates, 43 (63.2%) were resistant to two or more (up to ten) antimicrobials, respectively. Eight (11.8%) of Escherichia coli isolates had shown resistance to seven different drugs, while 7 (10.3%) of Escherichia coli isolates had shown resistance to eight drugs.
Table 4.
Multidrug resistance patterns of Escherichia coli isolates.
| Number of antimicrobial agents | Isolates from children (n = 68) | Number of isolates (%) |
|---|---|---|
| Multidrug resistance patterns/number of isolates | ||
| Two | SNM-OT (1); NOR-CLN (1); STM-NE (1) | 3 (4.4) |
| Three | TE-NE-CHL (1); TRM-CLN-AMP (1); STM, CLN, OT (2) | 4 (5.9) |
| Four | AMP-OT-NE-CLN (1); CHL, CLN, TRM, NE (1); CLN, TRM, TE, AMP (1) | 3 (4.4) |
| Five | NOR-CLN-SNM-CHL-STM (1); OT-NE- -CHL-NE-TRM (1) TRM-NOR-CLN-SNM-TE (1); STM-NOR TE-CIP-CHL (1) | 4 (5.9) |
| Six | NE-TE-CIP-CHL-TRM-NOR (2); NOR-CLN-SNM-OT AMP-STM (1); CHL-TRM-NOR-AMP-STM-TE (3). | 6 (8.8) |
| Seven | TE-STM-CLN-NOR-CHL-NE-TRM (3); SNM-OT-CHL-TRM-NOR-STM-NE-TE (3); CLN-SNM-CHL-STM-NE-TE-AMP (2) | 8 (11.8) |
| Eight | CIP-TRM-NOR-SNM-OT-AMP-STM-NE (2); TE-CIP-CHL-TRM-NOR-CLN-SNM-OT (3); AMP-STM-NE-TE-CIP-CHL-TRM-NOR (2); | 7 (10.3) |
| Nine | OT-TE-AMP-STM-NE-CIP-CHL-TRM-CLN (2); NOR-AMP-CLN-SNM-OT-NE-CHL-TRM-STM (1); CHL-TRM-NOR-CLN-STM-NE-TE-SNM-OT (3) | 6 (8.8) |
| Ten | TRM-AMP-STM-CLN-OT-NOR-CHL-NE-NOR-TE (1); TRM-CLN-SNM-CHL-STM-NE-CIP-TE-OT-NOR (1) | 2 (2.9) |
| Total | 43 (63.2%) |
AMP-ampicillin; CLN-clindamycin; CHL-chloramphenicol; CIP-ciprofloxacillin; STM-Streptomycin; NE-neomycin; NOR-norfloxacillin; OT-oxytetracycline; TE-tetracycline; TRM-trimethoprim; SNM-sulphonamides; n = number.
The STEC, EPEC, EAEC, EHEC, DAEC, and St (ETEC) strains in diarrheic children were highly resistant to neomycin and ampicillin 38 (100%) and clindamycin 36 (94.7%). Moderately high resistance was detected towards norfloxacin 18% (47.4) and chloramphenicol 24 (63.2%). The DEC pathotypes were least resistant to ciprofloxacin, 2 (5.3%) (Table 5).
Table 5.
Antimicrobial resistance percentage of pathogenic Escherichia coli strains/virulence genes.
| Antimicrobial agents | Detected virulence genes/strains in children (N = 38) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resistant pathogenic Escherichia coli strains or genes/(%) | ||||||||||||||
| STEC (n = 10) | Atypical EPEC (only eae+) (n = 5) | EAEC (eat gene) (n = 14) | EHEC (n = 3) | DAEC (dae gene) (n = 2) | St (ETEC) (n = 4) | Total | ||||||||
| R | S | R | S | R | S | R | S | R | S | R | S | R | S | |
| Ampicillin | 10(100) | — | 5(100) | — | 14 (100) | — | 3(100) | — | 2(100) | — | 4(100) | — | 38 (100) | — |
| Streptomycin | 9(90) | 1 (10) | 4(80) | 1 (20) | 14 (100) | — | 3(100) | — | 2(100) | — | 4(100) | — | 36 (94.7) | 2 (5.3) |
| Neomycin | 10(100) | — | 5(100) | — | 14 (100) | — | 3(100) | — | 2(100) | — | 4(100) | — | 38 (100) | — |
| Tetracycline | 8(80) | 2 (20) | 4(80) | 1 (20) | 12 (85.7) | 2 (14.3) | 2(66.7) | 1(33.3) | 2(100) | — | 4(100) | — | 32 (84.2) | 6 (15.8) |
| Ciprofloxacillin | — | 10 (100) | — | 5 (100) | — | 14 (100) | — | 3(100) | — | 2 (100) | 2(50) | 2 (50) | 2 (5.3%) | 36 (94.7) |
| Chloramphenicol | 6(60) | 4 (40) | 3(60) | 2 (40) | 9 (64.3) | 5 (35.7) | 1(33.3) | 2(66.7) | 2(100) | 2 (100) | 3(75) | 1 (25) | 24 (63.2) | 14 (36.8) |
| Trimethoprim | 6(60) | 4 (40) | 4(80) | 1 (20) | 11 (78.6) | 3 (21.4) | 1(33.3) | 2(66.7) | 2(100) | — | 4(100) | — | 28 (73.7) | 10 (26.3) |
| Norfloxacillin | 3(30) | 7 (70) | 3(60) | 2 (40) | 8 (57.1) | 6 (42.9) | — | 3(100) | 1(50) | 1 (50) | 3(75) | 1 (25) | 18 (47.4) | 20 (52.6) |
| Clindamycin | 10(100) | — | 4(80) | 1 (20) | 13 (92.9) | 1 (7.1) | 3(100) | — | 2(100) | — | 4(100) | — | 36 (94.7) | 2 (5.3) |
| Sulphonamides | 5(50) | 5(50) | 4(80) | 12 (85.7) | 2 (14.3) | 2(66.7) | 1(33.3) | 2(100) | — | 4(100) | — | 29 (76.3) | 9 (23.7) | |
N = number of strains; R = resistant; S = susceptible.
Thirty-eight (100%) of the Escherichia coli strains showed multidrug resistance, and 3 (7.9%) strains showed resistance to at least four drugs and at most to ten drugs (Table 6).
Table 6.
Multidrug resistance of pathogenic Escherichia coli strains.
| Number of drugs resisted | Multidrug resistance patterns/number of strains | Number of strains/% |
|---|---|---|
| Four | CLN-SNM-CHL-TRM (1); AMP-CHL-NE-STM (2) | 3 (7.9) |
| Five | AMP-NE-CHL-NOR-SNM-(1); CLN-TRM-OT-STM-AMP (2); STM-NOR-CLN-SNM-TE (3) | 6 (15.9) |
| Six | NE-OT-CHL-TRM-NOR-CLN (1); AMP-STM-NE-OT-CHL-TRM (1); NOR-CHL-NE-SNM-CLN-AMP-(2) | 4 (10.5) |
| Seven | STM-CLN-NE-SNM-CHL-TRM-NOR (2); NE-NOR-CLN-SNM-OT-AMP-STM (1); CHL-TRM-NE-OT-STM-TE-CLN (1) | 4 (10.5) |
| Eight | SNM-TRM-NOR-TE-CIP-OT-AMP-NE (4); STM-AMP-CHL-TRM-CLN-TE-NOR-OT (3); AMP-STM-NE-TE-CIP-CHL-CLN-TRM (3) | 10 (26.4) |
| Nine | CLN-NOR-TRM-STM-NE-CIP-CHL-AMP-TE (2); NOR-AMP-CLN-SNM-OT-NE-CHL-TRM-STM (3); AMP-STM-NE-TE-SNM-OT-TE-CHL-CIP-TRM (3) | 8 (21) |
| Ten | CLN-NE-CHL-AMP-OT-SNM-TRM-STM-NOR-TE (2) AMP-OT-CIP-TRM-TE-CHL-CLN-TRM-NE-SNM (1) | 3 (7.9) |
| Total | 38 (100%) |
AMP-ampicillin; CLN-clindamycin; CHL-chloramphenicol; CIP-ciprofloxacillin; STM-streptomycin; NE-neomycin; NOR-norfloxacillin; OT-oxytetracycline; TE-tetracycline; TRM-trimethoprim; SNM-sulphonamides.
Four (10.5%) and three (7.9%) strains were found to have the highest (0.9) and lowest (0.4) MDR index values, respectively, out of a total of 38 stool samples from diarrheic children (Table 7). In diarrheic children, a calculated MDR index value greater than or equal to 0.3 and 0.4 suggests a high chance of resistance.
Table 7.
Multidrug resistance index of pathogenic Escherichia coli strains.
| (n = 38) | |
|---|---|
| MDR index value | Number of strains/% |
| 0.3 | — |
| 0.4 | 3 (7.9) |
| 0.45 | 6 (15.9) |
| 0.54 | 3 (7.9) |
| 0.6 | 4 (10.5) |
| 0.7 | 10 (26.4) |
| 0.8 | 8 (21) |
| 0.9 | 4 (10.5) |
| Total | 38 (100%) |
(n = number of strains).
4. Discussion
Diarrhea is a multifactorial illness caused by a complex interaction between the body, its environment, diet, and infectious pathogens [51]. In the current study, Escherichia coli isolates were found in 68 (61.8%) of the 110 stool samples, which were higher compared with the findings of [52–54], and [55] who reported an isolation rate of 31% in Austria, 48.3% in Bahir Dar, 22.6% in Mozambique, and 2.3% in Nepal from diarrheic under-five years children. It was, however, lower than the 86.5% reported by [56] in Kenya and the 88% reported by [57] in Nigeria. Different sociodemographic factors, sample size variance, and the season when the research was conducted could all contribute to the difference in isolation rate [58].
Antimicrobial resistance levels of Ampicillin, chloramphenicol, tetracycline, and streptomycin for Escherichia coli isolates were revealed to be 48 (70.6%), 38 (55.9%), 44 (64.7%), and 65 (95.6%), respectively. The resistance levels of Escherichia coli isolates to ampicillin were approximately similar to those [21, 27, 53, 54, 59], and [54] who reported a resistance level of 86% in Vietnam, 73% in Mexico, 72% in Mozambique, and 84% in Kenya, 89% and 93.3% in Iran, but lower resistant levels were previously reported by [60] who revealed that 55.6% of Escherichia coli isolates were resistant to ampicillin. The extensive and indiscriminate use of antibiotics, as well as the creation of beta-lactamase enzymes, may be contributing to Escherichia coli resistance to ampicillin as already described by [61]. Contrary to this finding, the moderate resistance levels of Escherichia coli isolates for chloramphenicol by 27%, tetracycline by 16%, and streptomycin by 9% were previously reported by [27, 62].
The resistance of Escherichia coli isolates to tetracycline in our study was consistent with reports from Mexico [27] and Iran [63], which found 85% and 83% resistance, respectively. This could be due to indiscriminate antibiotic use, which was supported by [64]. The current study's high susceptibility of Escherichia coli isolates to ciprofloxacin (91.2%) contradicted previous findings by [27, 65], which found 97.2% and 100% susceptibility of Escherichia coli isolates to ciprofloxacin, respectively.
In this study, 63.2% of Escherichia coli isolates were found to be multidrug resistant. Multidrug resistance in Escherichia coli isolates was highest at seven drugs, followed by eight drugs, which was similar to the findings of [53, 56], who found multidrug resistance in Escherichia coli isolates.
In the current study, from 68 Escherichia coli isolates, 55.9% of DEC with five distinct pathotypes was detected, which was responsible for 30–40% of acute diarrhea episodes in children as indicated by [66]. All virulence genes detected in each pathogenic Escherichia coli strain were significantly associated with diarrheal infection. This study revealed a higher frequency of DEC as compared to [15, 67, 68], and [69] who reported 23% and 18.4% by [70] in Nigeria. However, it was slightly agreed with [66] in Iran, [71] in India, and [72] in Sweden, who reported 30.4%, 52%, and 48% DEC pathotypes, respectively.
In the present study, EAEC was the most isolated Escherichia coli pathotype with a prevalence of 14 20.5% followed by EHEC (14.7%), EPEC (11.8%), ST (5.9%), and DAEC (2.9%). Similarly, in the report [69], EAEC was the most commonly isolated category, followed by EPEC and ETEC. These three pathotypes of diarrheagenic Escherichia coli were also detected most frequently in children with acute diarrhea in Brazil by [67], in Tanzania by [15], and in Lybia by [73]. Moreover, [66, 67, 74, 75], and [69] also reported 10.7%, 14%, 3.86%, 8%, and 12.2% of EAEC pathotype, respectively. The high frequency of EAEC described in our study, along with the high resistance to antibiotics, supports the need for follow-up epidemiological studies, pathogenesis, and its role in the different forms of diarrhea [76]. An increasing number of studies support the association of EAEC with diarrhea in populations in developing countries [77]. It has also been shown that EAEC is a heterogeneous group of Escherichia coli and that not all strains are capable of causing diarrhea [3].
STEC (14.7%) was the second most prevalent strain, which was higher than the previous report [74] in Peru recorded a prevalence of 1%. Also, in another study conducted by [66], 7(1.6%) were positive for stx1 only, and 6 (1.3%) were positive for stx2 only.
Atypical EPEC (eaeA+ and bfp) (11.76%) was the third most prevalent strain. In this study, all isolates were identified as atypical EPEC. However, typical EPEC were more prevalent than atypical EPEC in children less than 2 years old in the study conducted in Mexico by [27], and epidemiological studies in several countries showed that atypical EPEC strains have become a more frequent cause of diarrhea than typical EPEC [78]. These observations have been linked to the duration of the diarrheal disease [21, 79].
However, 39 (17.7%) and 45 (40.5%) Escherichia coli isolates in Thailand by [80] and in Iran by [81] were reported, respectively, are possessing the eaeA gene. Also, [82] found that all EPEC isolates harbored the eaeA gene. Ochoa et al. [74] reported a 7% prevalence of EPEC in stool samples and such pathotype was also isolated with a prevalence of 19.3% in Kenya by [75] and 5.1% in Mexico by [69]. Atypical and typical EPEC were detected in 9.4% and only in one sample, respectively, in Brazil, which was reported by [67].
On the other hand, a lower percentage of eaeA gene distribution among EPEC was reported in Japan by [83] who showed that all EPEC strains isolated from children with diarrhea did not react with eaeA-specific primer. Also, in a report of [22], from 21 EPEC strains, 13 had only the eaeA gene, only one strain harbored the bfp gene, and 5 strains were positive for eae and bfp. None of the 77 serological identified EPEC strains contained the eaeA gene in a study conducted by [84]. Atypical EPEC is an emergent enteric pathogen that has only recently begun to attract the attention of investigators [85].
A prior study in Brazil and other countries found that enterotoxigenic Escherichia coli (ETEC) was the most usually isolated pathotype in children under the age of five who had diarrhea [3, 86]. All Escherichia coli isolates were tested for the presence of heat-labile and heat-stable toxins in this study, but none of the isolates tested positive for heat-labile toxin (Lt), and only 4 (5.8%) tested positive for heat-stable toxin (St). This result was lower than the previous reports of [3, 87], and [66] who recorded 21.6%, 20.5%, and 14.4% of ETEC, respectively. Furthermore, Vila [22] isolated 12.7% of ETEC strains with 33 strains (75%) that produced the heat-stable toxin (St), 6 strains (14%) synthesized the heat-labile toxin (Lt), and 5 strains (11%) produced both toxins. On the other hand, a low isolation rate of Enterotoxigenic Escherichia coli was reported in Peru by [74], in South India by [71], Kenya by [75], Mexico by [69], and Brazil by [67] who reported an isolation rate of 4%, 4.1%, 7.25%, 4.3%, and 3.7%, respectively.
EHEC was another Escherichia coli strain that was found in 3 (4.4%) of the 68 isolates and which was found in higher [3, 67, 71, 87, 88], and [66] who identified a frequency of 1.6%, 0.6%, 2.1%, 1.3%, 2.0%, and 3.8% from various regions of the world. In contrast, [69] in Mexico and [75] in Kenya found EHEC with isolation rates of 0.3% and 0.97%, respectively. In another study [66], 1 (0.2%) out of 17 EHEC strains was tested positive for stx1/eaeA, whereas 3 (0.7%) were tested positive for stx2/eaeA. On the contrary, Canizalez-ROman [69] were not found EHEC strains on his study.
The current study's high frequency of DAEC strains 2 (2.9%) differed from the work of [69] in Mexico and [71] in South India, which reported 1.4% and 0.5% of DAEC strains, respectively, but was lower than the report described by [74] in Peru, which indicated an isolation rate of 4%. Furthermore, DAEC strains were the second most often isolated pathotype linked with diarrhea in Brazilian children aged 2 to 5 years who lived in low socioeconomic areas [89]. DAEC strains have been recovered often from adults with diarrhea in Brazil, according to Mansan-Almeida [90].
EPEC strains were tested for the presence of the virulence EPEC gene in Escherichia coli isolates, but none of them carried the gene, which contradicted the findings of [22] in Tanzania, who showed that 1 EPEC strain had just the bfp gene, and 5 strains were eae and bfp positive. The hlyA gene was also not found in EHEC or STEC.
In this study, MDR was found in all pathogenic Escherichia coli strains (38 (100%)). Other authors [69] in Northwestern Mexico, [27, 68] in Iran, and [60] in Nigeria, on the other hand, found MDR of diarrheagenic Escherichia coli of over 80%, 62%, 67%, and 25.9%, respectively. However, in their studies, [91] in India and [74] in Peruvian reported that only 75% and 63% of pathogenic Escherichia coli strains were found to be MDR, respectively. Multidrug resistance in pathogenic Escherichia coli strains could be mostly owing to acquired antimicrobial resistance phenotypes, which are most commonly acquired through conjugative transfer of plasmid genes [92].
Plasmid genes may contain class I integrons, which are mobile DNA elements that have a role in the spread of bacterial MDR, particularly among Gram-negative enteric bacteria. Five (100%) atypical EPEC, four (100%) St (ETEC), and fourteen (100%) EAEC resisted ampicillin in diarrheic youngsters in this investigation. Similarly, Roy [93] found that ampicillin was resistant to EPEC in 96% of cases, ETEC in 73% of cases, and EAEC in 100% of cases. Isolated pathogenic Escherichia coli strains in Thailand also exhibited strong resistance to ampicillin [94]. According to [69], EPEC and DAEC strains had the highest rates of resistance to ampicillin and chloramphenicol. STEC, EPEC, EAEC, and EHEC are all extremely sensitive to ciprofloxacin in this investigation. In contrast to these findings, in a study conducted by [93], ciprofloxacin resistance was shown to be 39% in EPEC, 36% in ETEC, and 38% in EAEC. Despite the findings of this investigation, EPEC and DAEC strains showed the highest rates of ciprofloxacin resistance, as previously reported by [69]. 70% of DEC strains were reported to be resistant to ampicillin in research conducted on diarrheic children in Mexico [27], but most strains were found to be sensitive to ciprofloxacin. According to [95], the high prescription rate of ciprofloxacin in the study area as a treatment for enteric infections caused by Gram-negative bacteria is the source of varied rates of resistance to this antibiotic.
The resistance patterns among the DEC groups in our investigation were significantly varied. DAEC and EAEC were likely to have higher resistance levels than STEC, which was consistent with the findings of [69], who found the EPEC and DAEC categories to be the most resistant. This is due to their frequent exposure to antimicrobials, as well as the fact that they produce chronic diarrhea and/or are frequently carried asymptomatically. As a result, long-term use of human hosts raises the risk of antimicrobial exposure and/or the acquisition of resistant genes from the resident flora. As previously noted by [96], this study could represent an association of resistance genes with plasmid-associated virulence genes, such as adherence factors present in DAEC (i.e., Dr. Adhesins) and EAEC (i.e., AAF or aggregative adherence fimbria). Multiple antibiotic resistance has been linked to a range of mobile genetic elements, including plasmids, transposons, and gene cassettes in integrins [97] as well as changes in the Escherichia coli multiple antibiotic resistance operon (mar) [98].
The high degree of resistance is most likely the outcome of selection pressure caused by the uncontrolled and inappropriate use of these Antimicrobials in hospitals and across the country. Antimicrobial resistance in pathogenic bacteria, as well as the formation of resistant strains in flora bacteria, could result from improper usage of antimicrobial drugs. Historically, much of the focus has been on pathogenic bacteria; however, according to [99], the significance of commensal organisms as a reservoir or vehicle for transferring resistance genes to more dangerous, pathogenic bacteria has lately been proposed.
5. Conclusion
The overall high proportion of Escherichia coli isolates and their significant pathogenic strains indicates the wide distribution of the infection in children in the study area. Escherichia coli isolate showed susceptibility mostly to ciprofloxacin and norfloxacin; therefore, they are considered the best choice of treatment. A higher proportion of eaat gene-positive Escherichia coli strains was detected in children. Multiple drug resistance was mostly observed in pathogenic Escherichia coli strains harboring one or more virulence genes. The calculated MDR index value for all Escherichia coli pathotypes indicates the high risk of resistance. Antibiotics dosage and frequency should be used inappropriate methods to minimize drug resistance. Further research using whole-genome DNA sequencing and Phylogenetic tree analysis in diarrheic children should be done for the detection of variant genes, and emerging multidrug resistance encoding genes for all molecularly detected Escherichia coli strains in this study.
Acknowledgments
The authors would like to acknowledge the staff of Christian hospital, the institute of biotechnology, and Wolaita Sodo veterinary regional laboratory for their kind support during the research work.
Abbreviations
- A/E:
Attaching and effacing
- CFU:
Colony forming unit
- cGMP:
Cyclic guanine monophosphate
- CI:
Confidence interval
- COR:
Crude odd ratio
- DAEC:
Diffusely adherent Escherichia coli
- DDW:
Double distilled water
- DEC:
Diarrheagenic Escherichia coli
- DNA:
Deoxyribonucleic acid
- eae:
Escherichia coli attaching and effacing gene
- EDTA:
Ethylene diamine tetra-acetic acid
- EIEC:
Enteroinvasive Escherichia coli
- EPEC:
Enteropathogenic Escherichia coli
- EtBr:
Ethidium bromide
- ETEC:
Enterotoxigenic Escherichia coli
- EVC:
Escherichia coli verocytotoxin
- GTPase:
Guanine triphosphatase
- H:
Flagellar antigen
- IMViC:
Indole methyl red voges proskauer citrate
- LEE:
Locus of enterocyte effacement
- LT1:
Heat labile toxin type one
- M.a.s.l:
Meter above sea level
- MDR:
Multidrug resistance
- MDRI:
Multidrug resistance index
- MDa:
Megadalton
- MF:
Method of feeding
- NT:
Navel treatment
- O:
Somatic antigen
- p:
Probability
- PCR:
Polymerase chain reaction
- Rpm:
Revolution per minute
- SFT:
Supplementary feed type
- STEC:
Shiga toxin-producing Escherichia coli
- SIM:
Sulfide indole motility
- SPSS:
Statistical procedure for social science
- St:
Heat stable toxin
- Stx:
Shiga toxin
- Stx1 and Stx2:
Shiga toxin gene-one and two
- TBE:
Tris base boric acid
- TD:
Types of diarrhea
- TFCF:
Time of first colostrum feeding
- Tir:
Translocated intimin receptor
- TSI:
Triple sugar iron
- χ 2:
Chi-square.
Data Availability
The datasets used and analyzed throughout the study can be obtained from the corresponding author upon reasonable request.
Ethical Approval
This study received ethical approval from the Jimma University of Research Ethics and Review Committee. Before collecting the samples, the parents or guardians of the patients were asked for verbal agreement to collect samples from their children while adhering to stringent sanitary guidelines.
Consent
The best practices for human care were followed, and the patients' parents or guardians were told of the study's objective and that the Jimma University of Research Ethics and Review Committee authorized the oral informed consent process.
Disclosure
All the studies were done following the Helsinki Declaration.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, or study design.
References
- 1.Boschi-Pinto C., Velebit L., Shibuya K. Estimating child mortality due to diarrhoea in developing countries. Bulletin of the World Health Organization . 2008;86:710–717. doi: 10.2471/BLT.07.050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kosek M., Bern C., Guerrant R. L. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bulletin of the World Health Organization . 2003;81:197–204. [PMC free article] [PubMed] [Google Scholar]
- 3.Vilchez S., Reyes D., Paniagua M., Bucardo F., Möllby R., Weintraub A. Prevalence of diarrhoeagenic Escherichia coli in children from Leon, Nicaragua. Journal of Medical Microbiology . 2009;58(5):630–637. doi: 10.1099/jmm.0.007369-0. [DOI] [PubMed] [Google Scholar]
- 4.Liu L., Johnson H. L., Cousens S., et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. The lancet . 2012;379(9832):2151–2161. doi: 10.1016/s0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 5.Walker C. L. F., Rudan I., Liu L., et al. Global burden of childhood pneumonia and diarrhoea. The Lancet . 2013;381(9875):1405–1416. doi: 10.1016/s0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. !!! Invalid citation !!! [4, 6, 7]
- 7.Lawn J. E., Wilczynska-Ketende K., Cousens S. N. Estimating the causes of 4 million neonatal deaths in the year 2000. International Journal of Epidemiology . 2006;35(3):706–718. doi: 10.1093/ije/dyl043. [DOI] [PubMed] [Google Scholar]
- 8. !!! Invalid citation !!! [4, 5, 9]
- 9.O’Ryan M., Prado V., Pickering L. K. Seminars in Pediatric Infectious Diseases . 2. Vol. 16. Elsevier; 2005. A millennium update on pediatric diarrheal illness in the developing world; pp. 125–136. [DOI] [PubMed] [Google Scholar]
- 10.Zhang S.-X., Zhou Y. M., Tian L. G., et al. Antibiotic resistance and molecular characterization of diarrheagenic Escherichia coli and non-typhoidal salmonella strains isolated from infections in southwest China. Infectious diseases of poverty . 2018;7(1):p. 53. doi: 10.1186/s40249-018-0427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang S.-X., Zhou Y. M., Xu W., et al. Impact of co-infections with enteric pathogens on children suffering from acute diarrhea in southwest China. Infectious Diseases of Poverty . 2016;5(1):p. 64. doi: 10.1186/s40249-016-0157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viswanathan V. K., Hodges K., Hecht G. Enteric infection meets intestinal function: how bacterial pathogens cause diarrhoea. Nature Reviews Microbiology . 2009;7(2):110–119. doi: 10.1038/nrmicro2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdalla M., Siham E., Suliman Y., Alian A. Microbial contamination of sheep carcasses at el kadero slaughterhouse–khartoum state. Sudan Journal of Veterinary Science and Animal Husbandry . 2009;48:1–2. [Google Scholar]
- 14.Bélanger L., Garenaux A., Harel J., Boulianne M., Nadeau E., Dozois C. M. Escherichia coli from animal reservoirs as a potential source of human extraintestinal pathogenic E. coli. FEMS Immunology and Medical Microbiology . 2011;62(1):1–10. doi: 10.1111/j.1574-695x.2011.00797.x. [DOI] [PubMed] [Google Scholar]
- 15.Moyo S. J., Maselle S. Y., Matee M. I., Langeland N., Mylvaganam H. Identification of diarrheagenic Escherichia coli isolated from infants and children in dar es Salaam, Tanzania. BMC Infectious Diseases . 2007;7(1):p. 92. doi: 10.1186/1471-2334-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Darsema G. Major causes of calf mortality in dairy farms and two cattle ranches in western Amhara region, north western Ethiopia. Ethiopian veterinary journal . 2008;12:59–68. [Google Scholar]
- 17.Kaper J. B., Nataro J. P., Mobley H. L. T. Pathogenic Escherichia coli. Nature Reviews Microbiology . 2004;2(2):123–140. doi: 10.1038/nrmicro818. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt M. A. LEEways: tales of EPEC, ATEC and EHEC. Cellular Microbiology . 2010;12(11):1544–1552. doi: 10.1111/j.1462-5822.2010.01518.x. [DOI] [PubMed] [Google Scholar]
- 19.Prestinaci F., Pezzotti P., Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathogens and Global Health . 2015;109(7):309–318. doi: 10.1179/2047773215y.0000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Putnam S., Riddle M., Wierzba T., et al. Antimicrobial susceptibility trends among Escherichia coli and shigella spp. isolated from rural Egyptian paediatric populations with diarrhoea between 1995 and 2000. Clinical Microbiology and Infections . 2004;10(9):804–810. doi: 10.1111/j.1469-0691.2004.00927.x. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen T. V., Le P. V., Le C. H., Weintraub A. Antibiotic resistance in diarrheagenic Escherichia coli and shigella strains isolated from children in Hanoi, Vietnam. Antimicrobial Agents and Chemotherapy . 2005;49(2):816–819. doi: 10.1128/aac.49.2.816-819.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vila J., Vargas M., Casals C., et al. Antimicrobial resistance of diarrheagenic Escherichia coli isolated from children under the age of 5 years from Ifakara, Tanzania. Antimicrobial Agents and Chemotherapy . 1999;43(12):3022–3024. doi: 10.1128/aac.43.12.3022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poirel L., Madec J. Y., Lupo A., et al. Antimicrobial resistance in Escherichia coli. Microbiology Spectrum . 2018;6(4):6–4. doi: 10.1128/microbiolspec.arba-0026-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reshadi P., Heydari F., Ghanbarpour R., et al. Molecular characterization and antimicrobial resistance of potentially human‐pathogenic Escherichia coli strains isolated from riding horses. BMC Veterinary Research . 2021;17(1):p. 131. doi: 10.1186/s12917-021-02832-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. !!! Invalid citation !!! [16, 18, 19]
- 26.Nataro J. P., Kaper J. B. Diarrheagenic Escherichia coli. Clinical Microbiology Reviews . 1998;11(1):142–201. doi: 10.1128/cmr.11.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Estrada-Garcia T., Lopez-Saucedo C., Thompson-Bonilla R., et al. Association of diarrheagenic Escherichia coli pathotypes with infection and diarrhea among Mexican children and association of atypical enteropathogenic E. coli with acute diarrhea. Journal of Clinical Microbiology . 2009;47(1):93–98. doi: 10.1128/jcm.01166-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trevisani M., Mancusi R., Delle Donne G., Bacci C., Bassi L., Bonardi S. Detection of shiga toxin (Stx)-producing Escherichia coli (STEC) in bovine dairy herds in northern Italy. International Journal of Food Microbiology . 2014;184:45–49. doi: 10.1016/j.ijfoodmicro.2013.12.033. [DOI] [PubMed] [Google Scholar]
- 29.Ombarak R. A., Hinenoya A., Awasthi S. P., et al. Prevalence and pathogenic potential of Escherichia coli isolates from raw milk and raw milk cheese in Egypt. International Journal of Food Microbiology . 2016;221:69–76. doi: 10.1016/j.ijfoodmicro.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Ribeiro L. F., Barbosa M. M. C., Pinto FdR., et al. Antimicrobial resistance and virulence factors of Escherichia coli in cheese made from unpasteurized milk in three cities in Brazil. Foodborne Pathogens and Disease . 2016;13(9):469–476. doi: 10.1089/fpd.2015.2106. [DOI] [PubMed] [Google Scholar]
- 31.Tark D.-S., Moon D. C., Kang H. Y., et al. Antimicrobial susceptibility and characterization of extended-spectrum β-lactamases in Escherichia coli isolated from bovine mastitic milk in south Korea from 2012 to 2015. Journal of Dairy Science . 2017;100(5):3463–3469. doi: 10.3168/jds.2016-12276. [DOI] [PubMed] [Google Scholar]
- 32.Hinthong W., Pumipuntu N., Santajit S., et al. Detection and drug resistance profile of Escherichia coli from subclinical mastitis cows and water supply in dairy farms in Saraburi province, Thailand. PeerJ . 2017;5:p. e3431. doi: 10.7717/peerj.3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tabaran A., Mihaiu M., Tabaran F., et al. First study on characterization of virulence and antibiotic resistance genes in verotoxigenic and enterotoxigenic E. coli isolated from raw milk and unpasteurized traditional cheeses in Romania. Folia Microbiologica . 2017;62(2):145–150. doi: 10.1007/s12223-016-0481-8. [DOI] [PubMed] [Google Scholar]
- 34.Liu H., Li S., Meng L., et al. Prevalence, antimicrobial susceptibility, and molecular characterization of Staphylococcus aureus isolated from dairy herds in northern China. Journal of Dairy Science . 2017;100(11):8796–8803. doi: 10.3168/jds.2017-13370. [DOI] [PubMed] [Google Scholar]
- 35.Black R. E., Cousens S., Johnson H. L., et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. The lancet . 2010;375(9730):1969–1987. doi: 10.1016/s0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 36.Wolde A., Deneke Y., Sisay T., Mathewos M., Fesseha H. Isolation of Escherichia coli and its associated risk factor from diarrheic children in Wolaita Sodo town, southern Ethiopia. Research and Reports in Tropical Medicine . 2021;12:227–234. doi: 10.2147/rrtm.s327129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quinn P., Markey B., Carter M., Donnelly W., Leonard F. Veterinary Microbiology and Bacterial Disease . London, UK: Black Well Science; 2002. pp. 1–648. [Google Scholar]
- 38.Tozzoli R., Maugliani A., Michelacci V., Minelli F., Caprioli A., Morabito S. Validation on milk and sprouts of EN ISO 16654: 2001-microbiology of food and animal feeding stuffs-horizontal method for the detection of Escherichia coli O157. International Journal of Food Microbiology . 2019;288:53–57. doi: 10.1016/j.ijfoodmicro.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 39.Sagar V. A., Davies E. J., Briscoe S., et al. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. Open heart . 2015;2(1) doi: 10.1136/openhrt-2014-000163.e000163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farshad S., Ranjbar R., Anvarinejad M., Shahidi M. A., Hosseini M. Emergence of multi drug resistant strains of Eschetichia coli isolated from urinary tract infection. The Open Conference Proceedings Journal . 2010;1(1):196. doi: 10.2174/22102892010010100192. [DOI] [Google Scholar]
- 41.Patel J. B., Cockerill F., Bradford P. A. Performance Standards for Antimicrobial Susceptibility Testing: 25th Informational Supplement . Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2015. [Google Scholar]
- 42.Oladoja M., Onifade A. Dissemination of multi-drug resistance in Escherichia coli isolated from apparently healthy school children in ondo state, Nigeria. Clinical Microbiology: Open Access . 2015;4(5) [Google Scholar]
- 43.He F. E. coli genomic DNA extraction. Bio-Protocol Bio101 . 2011;1 [Google Scholar]
- 44.Khan A., Das S. C., Ramamurthy T., et al. Antibiotic resistance, virulence gene, and molecular profiles of shiga toxin-producing Escherichia coli isolates from diverse sources in Calcutta, India. Journal of Clinical Microbiology . 2002;40(6):2009–2015. doi: 10.1128/jcm.40.6.2009-2015.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pal A., Ghosh S., Ramamurthy T., et al. Shiga-toxin producing Escherichia coli from healthy cattle in a semi-urban community in Calcutta, India. Indian Journal of Medical Research . 1999;110:83–85. [PubMed] [Google Scholar]
- 46.Gallien P. PCR Detection of Microbial Pathogens . Berlin, Germany: Springer; 2003. Detection and subtyping of shiga toxin-producing Escherichia coli (STEC) pp. 163–184. [DOI] [PubMed] [Google Scholar]
- 47.Vidal M., Kruger E., Durán C., et al. Single multiplex PCR assay to identify simultaneously the six categories of diarrheagenic Escherichia coli associated with enteric infections. Journal of Clinical Microbiology . 2005;43(10):5362–5365. doi: 10.1128/jcm.43.10.5362-5365.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arif S. K., Salih L. I. Identification of different categories of diarrheagenic “Escherichia coli” in stool samples by using multiplex PCR technique. Asian Journal of Medical Sciences . 2010;2(5):237–243. [Google Scholar]
- 49.Nishikawa Y., Zhou Z., Hase A., et al. Diarrheagenic Escherichia coli isolated from stools of sporadic cases of diarrheal illness in Osaka city, Japan between 1997 and 2000: prevalence of enteroaggregative E. coli heat-stable enterotoxin 1 gene-possessing E. coli. Japanese Journal of Infectious Diseases . 2002;55(6):183–190. [PubMed] [Google Scholar]
- 50.Hegde A., Ballal M., Shenoy S. Detection of diarrheagenic Escherichia coli by multiplex PCR. Indian Journal of Medical Microbiology . 2012;30(3):279–284. doi: 10.4103/0255-0857.99485. [DOI] [PubMed] [Google Scholar]
- 51.Stipp D. T., Barry A. F., Alfieri A. F., Takiuchi E., Amude A. M., Alfieri A. A. Frequency of BCoV detection by a semi-nested PCR assay in faeces of calves from Brazilian cattle herds. Tropical Animal Health and Production . 2009;41(7):1563–1567. doi: 10.1007/s11250-009-9347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nguyen R. N., Taylor L. S., Tauschek M., Robins-Browne R. M. Atypical enteropathogenic Escherichia coli infection and prolonged diarrhea in children. Emerging Infectious Diseases . 2006;12(4):597–603. doi: 10.3201/eid1204.051112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adugna A., Kibret M., Abera B., Nibret E., Adal M. Antibiogram of E. coli serotypes isolated from children aged under five with acute diarrhea in Bahir Dar town. African Health Sciences . 2015;15(2):p. 656. doi: 10.4314/ahs.v15i2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mandomando I. M., Alonso P. L., Macete E. V., et al. Etiology of diarrhea in children younger than 5 years of age admitted in a rural hospital of southern Mozambique. The American Journal of Tropical Medicine and Hygiene . 2007;76(3):522–527. doi: 10.4269/ajtmh.2007.76.522. [DOI] [PubMed] [Google Scholar]
- 55.Ansari S., Sherchand J. B., Parajuli K., et al. Bacterial etiology of acute diarrhea in children under five years of age. Journal of Nepal Health Research Council . 2012;10(22):218–223. [PubMed] [Google Scholar]
- 56.Shah M., Kathiiko C., Wada A., et al. Prevalence, seasonal variation, and antibiotic resistance pattern of enteric bacterial pathogens among hospitalized diarrheic children in suburban regions of central Kenya. Tropical Medicine and Health . 2016;44(1):p. 39. doi: 10.1186/s41182-016-0038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mc U., Gi E., Cp E., Okezie U., So E. Antibiotic susceptibility profile of Escherichia coli and salmonella causing childhood diarrhoea in awka municipality, south-eastern Nigeria. Clinical Microbiology . 2017;6(2):p. 2. doi: 10.4172/2327-5073.1000277. [DOI] [Google Scholar]
- 58.Shetty V. A., Kumar S. H., Shetty A. K., Karunasagar I., Karunasagar I. Prevalence and characterization of diarrheagenic Escherichia coli isolated from adults and children in Mangalore, India. Journal of Laboratory Physicians . 2012;4(1):24–29. doi: 10.4103/0974-2727.98666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kipkorir C. K., Bett P., Onyango P. O., Onyango D. M., Ayieko C., Ang’İenda P. O. Epidemiology of antimicrobial resistance among Escherichia coli strains in Trans-Nzoia county, Kenya. Journal of microbiology and infectious diseases . 2016;6(3):107–112. [Google Scholar]
- 60.Akingbade O. A., Damola A. B., Shobayo B. I., Nwanze J. C., Okonko I. O. Multi-drug resistant (MDR) Escherichia coli among children suffering from diarrhea infections in abeokuta, Nigeria. School of Medical Laboratory Science . 2014;6:42–47. [Google Scholar]
- 61.Sack D. A., Lyke C., McLaughlin C., Suwanvanichkij V., Organization W. H. Antimicrobial Resistance in Shigellosis, Cholera and Campylobacteriosis . Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 62.Amaya E., Reyes D., Vilchez S., et al. Antibiotic resistance patterns of intestinal Escherichia coli isolates from Nicaraguan children. Journal of Medical Microbiology . 2011;60(2):216–222. doi: 10.1099/jmm.0.020842-0. [DOI] [PubMed] [Google Scholar]
- 63.Heidary M., Momtaz H., Madani M. Characterization of diarrheagenic antimicrobial resistant Escherichia coli isolated from pediatric patients in Tehran, Iran. Iranian Red Crescent Medical Journal . 2014;16(4) doi: 10.5812/ircmj.12329.e12329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Usein C.-R., Tatu-Chitoiu D., Ciontea S., Condei M., Damian M. Escherichia coli pathotypes associated with diarrhea in Romanian children younger than 5 years of age. Japanese Journal of Infectious Diseases . 2009;62(4):289–293. [PubMed] [Google Scholar]
- 65.Manikandan C., Amsath A. Antimicrobial resistance of enteric pathogens isolated from children with acute diarrhoea in Pattukkottai, Tamil Nadu, India. International Journal of Pure and Applied Zoology . 2013;1(2):139–145. [Google Scholar]
- 66.Haghi F., Zeighami H., Hajiahmadi F., Khoshvaght H., Bayat M. Frequency and antimicrobial resistance of diarrhoeagenic Escherichia coli from young children in Iran. Journal of Medical Microbiology . 2014;63(3):427–432. doi: 10.1099/jmm.0.064600-0. [DOI] [PubMed] [Google Scholar]
- 67.Bueris V., Sircili M. P., Taddei C. R., et al. Detection of diarrheagenic Escherichia coli from children with and without diarrhea in Salvador, Bahia, Brazil. Memórias do Instituto Oswaldo Cruz . 2007;102:839–844. doi: 10.1590/s0074-02762007005000116. [DOI] [PubMed] [Google Scholar]
- 68.Alikhani M. Y., Hashemi S. H., Aslani M. M., Farajnia S. Prevalence and antibiotic resistance patterns of diarrheagenic Escherichia coli isolated from adolescents and adults in Hamedan, western Iran. Iranian Journal of Microbiology . 2013;5(1):42–47. [PMC free article] [PubMed] [Google Scholar]
- 69.Canizalez-Roman A., Flores-Villasenor H. M., Gonzalez-Nunez E., et al. Surveillance of diarrheagenic Escherichia coli strains isolated from diarrhea cases from children, adults and elderly at northwest of Mexico. Frontiers in Microbiology . 2016;7:p. 1924. doi: 10.3389/fmicb.2016.01924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Onanuga A., Igbeneghu O., Lamikanra A. A study of the prevalence of diarrhoeagenic Escherichia coli in children from Gwagwalada, Federal capital territory, Nigeria. The Pan African medical journal . 2014;17:p. 146. doi: 10.11604/pamj.2014.17.146.3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rajendran P., Ajjampur S. S. R., Chidambaram D., et al. Pathotypes of diarrheagenic Escherichia coli in children attending a tertiary care hospital in south India. Diagnostic Microbiology and Infectious Disease . 2010;68(2):117–122. doi: 10.1016/j.diagmicrobio.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Saeed A., Abd H., Sandstrom G. Microbial aetiology of acute diarrhoea in children under five years of age in Khartoum, Sudan. Journal of Medical Microbiology . 2015;64(4):432–437. doi: 10.1099/jmm.0.000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ali D. A., Tesema T. S., Belachew Y. D. Retracted article: molecular detection of pathogenic Escherichia coli strains and their antibiogram associated with risk factors from diarrheic calves in Jimma Ethiopia. Scientific Reports . 2021;11(1) doi: 10.1038/s41598-021-93688-6.14356 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 74.Ochoa T. J., Molina M., Lanata C. F., et al. High frequency of antimicrobial drug resistance of diarrheagenic Escherichia coli in infants in Peru. The American Journal of Tropical Medicine and Hygiene . 2009;81(2):296–301. doi: 10.4269/ajtmh.2009.81.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Makobe C. K., Sang W. K., Kikuvi G., Kariuki S. Molecular characterization of virulence factors in diarrhoeagenic Escherichia coli isolates from children in Nairobi, Kenya. The Journal of Infection in Developing Countries . 2012;6(08):598–604. doi: 10.3855/jidc.2082. [DOI] [PubMed] [Google Scholar]
- 76.Nakhjavani F. A., Emaneini M., Hosseini H., et al. Molecular analysis of typical and atypical enteropathogenic Escherichia coli (EPEC) isolated from children with diarrhoea. Journal of Medical Microbiology . 2013;62(2):191–195. doi: 10.1099/jmm.0.046516-0. [DOI] [PubMed] [Google Scholar]
- 77.Nataro J. P., Mai V., Johnson J., et al. Diarrheagenic escherichia coli infection in Baltimore, Maryland, and New haven, Connecticut. Clinical Infectious Diseases . 2006;43(4):402–407. doi: 10.1086/505867. [DOI] [PubMed] [Google Scholar]
- 78. !!! INVALID CITATION !!! [38, 60, 74, 76, 77]
- 79.Afset J. E., Bevanger L., Romundstad P., Bergh K. Association of atypical enteropathogenic Escherichia coli (EPEC) with prolonged diarrhoea. Journal of Medical Microbiology . 2004;53(11):1137–1144. doi: 10.1099/jmm.0.45719-0. [DOI] [PubMed] [Google Scholar]
- 80.Ratchtrachenchai O.-A., Subpasu S., Hayashi H., Ba-Thein W. Prevalence of childhood diarrhoea-associated Escherichia coli in Thailand. Journal of Medical Microbiology . 2004;53(3):237–243. doi: 10.1099/jmm.0.05413-0. [DOI] [PubMed] [Google Scholar]
- 81.Graves D., Liu R., Alikhani M., Al-Mashat H., Trackman P. Diabetes-enhanced inflammation and apoptosis—impact on periodontal pathology. Journal of Dental Research . 2006;85(1):15–21. doi: 10.1177/154405910608500103. [DOI] [PubMed] [Google Scholar]
- 82.Chen C., Ridzon D. A., Broomer A. J., et al. Real-time quantification of microRNAs by stem-loop RT-PCR. Nucleic Acids Research . 2005;33(20):p. e179. doi: 10.1093/nar/gni178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fukuda M., Ohkubo T., Katsuya T., et al. Association of a mast cell chymase gene variant with HDL cholesterol, but not with blood pressure in the ohasama study. Hypertension Research: Official Journal of the Japanese Society of Hypertension . 2002;25(2):179–184. doi: 10.1291/hypres.25.179. [DOI] [PubMed] [Google Scholar]
- 84.Phantouamath B., Sithivong N., Insisiengmay S., et al. The incidence of Escherichia coli having pathogenic genes for diarrhea: a study in the People’s Democratic Republic of Lao. Japanese Journal of Infectious Diseases . 2003;56(3):103–106. [PubMed] [Google Scholar]
- 85. !!! Invalid citation !!! [67, 74, 75]
- 86.Regua-Mangia A., Gomes T., Vieira M., Andrade J., Irino K., Teixeira L. Frequency and characteristics of diarrhoeagenic Escherichia coli strains isolated from children with and without diarrhoea in Rio de Janeiro, Brazil. Journal of Infection . 2004;48(2):161–167. doi: 10.1016/s0163-4453(03)00138-5. [DOI] [PubMed] [Google Scholar]
- 87.Nweze E. Virulence properties of diarrheagenic E. coli and etiology of diarrhea in infants, young children and other age groups in southeast, Nigeria. American-Eurasian Journal of Scientific Research . 2009;4(3):173–179. [Google Scholar]
- 88.Pabst W. L., Altwegg M., Kind C., Mirjanic S., Hardegger D., Nadal D. Prevalence of enteroaggregative Escherichia coli among children with and without diarrhea in Switzerland. Journal of Clinical Microbiology . 2003;41(6):2289–2293. doi: 10.1128/jcm.41.6.2289-2293.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lozer D. M., Souza T. B., Monfardini M. V., et al. Genotypic and phenotypic analysis of diarrheagenic Escherichia coli strains isolated from Brazilian children living in low socioeconomic level communities. BMC Infectious Diseases . 2013;13(1):p. 418. doi: 10.1186/1471-2334-13-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mansan-Almeida R., Pereira A. L., Giugliano L. G. Diffusely adherent Escherichia coli strains isolated from children and adults constitute two different populations. BMC Microbiology . 2013;13(1):p. 22. doi: 10.1186/1471-2180-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vaishnavi C., Kaur S. The epidemiological and resistogram patterns of enteropathogenic and enterotoxigenic Escherichia coli isolated from diarrhoeal stools in a north Indian hospital. Tropical Gastroenterology: Official Journal of the Digestive Diseases Foundation . 2003;24(2):70–72. [PubMed] [Google Scholar]
- 92.Di Conza J., Ayala J. A., Power P., Mollerach M., Gutkind G. Novel class 1 integron (InS21) carrying bla CTX-M-2 in Salmonella enterica serovar infantis. Antimicrobial Agents and Chemotherapy . 2002;46(7):2257–2261. doi: 10.1128/aac.46.7.2257-2261.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roy S., Shamsuzzaman S., Mamun K. Antimicrobial resistance pattern of diarrheagenic Escherichia coli isolated from acute diarrhea patients. International Journal of Pharmaceutical Science Invention . 2013;2(6):43–46. [Google Scholar]
- 94.Kalnauwakul S., Phengmak M., Kongmuang U., Nakaguchi Y., Nishibuchi M. Examination of diarrheal stools in Hat Yai city, south Thailand, for Escherichia coli O157 and other diarrheagenic Escherichia coli using immunomagnetic separation and PCR method. Southeast Asian Journal of Tropical Medicine and Public Health . 2007;38(5):871–880. [PubMed] [Google Scholar]
- 95.Yang C.-M., Lin M.-F., Lin C.-H., Huang Y.-T., Hsu C.-T., Liou M.-L. Characterization of antimicrobial resistance patterns and integrons in human fecal Escherichia coli in Taiwan. Japanese Journal of Infectious Diseases . 2009;62(3):177–181. [PubMed] [Google Scholar]
- 96.Harrington S. M., Dudley E. G., Nataro J. P. Pathogenesis of enteroaggregative Escherichia coli infection. FEMS Microbiology Letters . 2006;254(1):12–18. doi: 10.1111/j.1574-6968.2005.00005.x. [DOI] [PubMed] [Google Scholar]
- 97.Brueggemann A. B. Antibiotic resistance mechanisms among pediatric respiratory and enteric pathogens: a current update. The Pediatric Infectious Disease Journal . 2006;25(10):969–973. doi: 10.1097/01.inf.0000239365.60595.d5. [DOI] [PubMed] [Google Scholar]
- 98.Barbosa T. M., Levy S. B. Differential expression of over 60 chromosomal genes in Escherichia coli by constitutive expression of MarA. Journal of Bacteriology . 2000;182(12):3467–3474. doi: 10.1128/jb.182.12.3467-3474.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sharada R., Ruban S. W. Isolation, characterization and antibiotic resistance pattern of Escherichia coli isolated from poultry. American-eurasian Journal of Scientific Research . 2010;5(1):18–22. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed throughout the study can be obtained from the corresponding author upon reasonable request.


