Abstract
Housing may be at once the most powerful and underused tool at our disposal to improve population health. Using examples from the USA, we argue that current levels of housing insecurity are the result of clear and inequitable policy choices, leading to the entrenchment of health inequities—particularly, across race and class. Solutions to housing insecurity must, therefore, be structural. The COVID-19 pandemic has opened a window of opportunity for these structural housing policy reforms. Through justice- and action-oriented research, health researchers can inform the development and implementation of housing policies that advance health equity. We offer a series of recommendations to better position our field to achieve this goal.
Keywords: EPIDEMIOLOGY, Health inequalities, HOMELESS PERSONS, POLICY, RESEARCH DESIGN
Housing is fundamental to health
In primary school we learn that food, water and shelter are necessary to sustain life. Indeed, this last condition—shelter—has long been a cornerstone of public health. Public health as a discipline emerged from inquiries into the housing conditions of the working poor, when overcrowding in tenement housing at the dawn of the industrial era accelerated the spread of infectious diseases.1 Engels, Chadwick, Du Bois and others documented failing housing and sanitation infrastructure as root causes of health disparities, leading to the founding of the sanitation movement and modern public health.1 2 Since then, thousands of articles have been published linking housing conditions to well-being.3–6 Even among the core determinants of health, housing is often awarded special status as the most fundamental. The ‘Housing First’ model—which prioritises housing for people experiencing homelessness—exemplifies how providing individuals with secure housing lessens other barriers to health, including access to food, employment and healthcare.7
And yet, housing insecurity is exceedingly common in the USA
Among high-income countries of Europe and North America, housing markets in the U.S. stand out as uniquely inhospitable.8 Over one in three US households lives in rental housing, and the vast majority paying market-rate rents.8 Markets have driven rents upward while wages have stagnated, forcing nearly half of renter households to spend over 30% of their incomes on rent.9 For many, this spending is unsustainable: approximately 1 in 40 renter households is formally evicted annually in the USA10 and for every formal eviction, there are approximately 5.5 informal evictions.11 Among homeowners, unregulated financial speculation in housing markets led to a foreclosure crisis that many are still feeling the effects of. Perhaps the most visible and extreme consequence of unaffordable housing in the USA is homelessness, with an estimated 1 in 600 Americans living unhoused during the 2020 point-in-time count.12 These population averages obscure strong social gradients in housing insecurity, whereby marginalised communities (eg, by race, class, gender, sexual orientation or immigration status) are disproportionately affected.
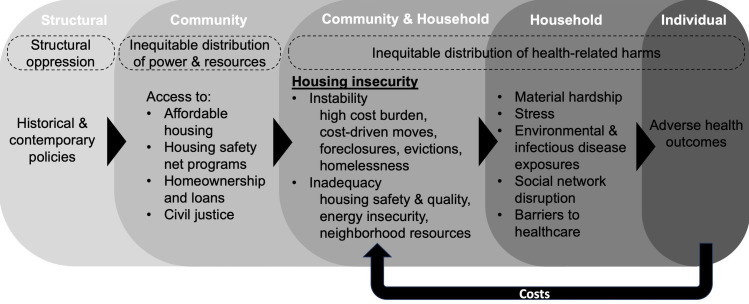
The ubiquity of these various forms of housing insecurity—a term used analogously to food insecurity to describe limited or uncertain access to adequate housing—can be thought of as part of an ongoing structural-environmental-biological process affecting entire populations (figure 1, drawing on a framework by Swope and Hernandez).13 The process occurs in the context of structural oppression, which housing policies either reinforce or dismantle by distributing access to resources and power between communities. One key resource allocated directly and indirectly by housing policies is affordable housing, that is, available housing priced at or below 30% of renters’ incomes within a community. Alone or combined with constrained access to housing safety net programmes, homeownership and loans, and civil justice in housing courts, insufficient affordable housing leads to housing insecurity. Housing insecurity is composed of two major domains: (1) instability, including precariously high cost burden (ie, housing costs so high relative to income that families are uncertain of their ability to pay on a month-to-month basis), cost-driven moves, foreclosures, evictions and homelessness and (2) inadequacy (ie, poor housing and neighbourhood conditions, including energy insecurity).14 From there, housing insecurity operates through multiple mechanisms—including material hardship, stress, environmental and infectious disease exposures, social network disruption and barriers to healthcare—to produce adverse health outcomes over the life course. As a final insult to population well-being, emerging evidence points to a feedback loop through which adverse health conditions and associated costs (eg, healthcare bills, lost income due to missed work) influence future housing insecurity.15 16
Figure 1.
Conceptual framework showing the structural-environmental-biological process through which housing policies, in the context of structural oppression, affect inequities in population well-being.
Housing insecurity is not inevitable, but results from policy choices
In contrast to other essential needs, US policymakers have chosen not to invest in housing, with alarming consequences. In the 20th century, the federal government undertook massive infrastructure programmes to ensure that families had clean water and made food an entitlement through the Supplemental Nutrition Assistance Program and Special Supplemental Nutrition Program for Women, Infants, and Children. Today, 97% of households have access to clean drinking water17 and 90% are food secure.18 Though more work is required to ensure that all households have access to these basic needs, increased access to clean water and sufficient food are among the great success stories in US public health, contributing to dramatic gains in life expectancy.19 20 In contrast, housing infrastructure has deteriorated and been demolished in the face of growing demand and housing is not considered an entitlement in the USA. Consequently, housing assistance only reaches a quarter of eligible families.21
When the USA has intervened in the housing sector, it has often been inequitable. Although these injustices have affected people at the intersections of multiple disadvantaged identities and classes, it is particularly instructive to view US housing policies through the lens of anti-Black racism. Until the late 1960s, explicitly racist Jim Crow laws, zoning regulations and deed restrictions segregated neighbourhoods and restricted the ‘American Dream’ of homeownership to white families.22 When the Fair Housing Act of 1968 banned race-based discrimination in housing sales and rentals, a system of de facto segregation maintained racial inequities in housing.22 Over the same period, the USA effectively defunded and dismantled public housing infrastructure as the percentage of Black residents increased.23 This legacy of public housing disinvestment continues today and is exacerbated by gentrification and racist characterisations of predominantly Black public housing communities as socially disorganised and crime-ridden.23
And so, structurally racist housing policies paved the way for white homeowners to build equity (in the economic sense of the word), all the while cementing racial health inequity.24 Living in a historically redlined neighbourhood (ie, majority-Black neighbourhoods denied mortgages under mid-20th century discriminatory lending policies), for example, predicts poorer health outcomes to this day, including preterm births,25 asthma-related complications,26 tobacco retailer density27 and exposure to violence.28 Ongoing residential segregation appears as a ‘fundamental determinant’ of racial health inequities, stratifying access to housing resources to produce an inequitable distribution of housing insecurity and disparate exposure to health-related harms in the present day.29 In systematically lowering barriers to housing for white families, while building barriers for Black families, policymakers provided a cruel case study in the potential for housing policies to shape health.
What role can health researchers play in changing the status quo?
Now is a critical window for housing policy reform. In recent years, WHO as well as the US Departments of Housing and Urban Development and Health and Human Services have each articulated goals to promote health through housing policies.30–32 The COVID-19 pandemic and economic downturn exacerbated housing insecurity but also ushered in unprecedented innovation in housing policy. Federal, state and local governments in the USA instituted eviction moratoriums, made historic investments in rental assistance and guaranteed right to legal counsel to tenants facing eviction. These policies often had explicit public health objectives.
Health researchers can help sustain momentum in housing policy reform by conducting justice-oriented and action-oriented research. By being more intentional in the way we approach research—the teams we build, the questions we ask, our study designs and our dissemination strategies—we can better position ourselves to inform the development and implementation of housing policies that advance health equity. In the following section, we provide methodological and practice recommendations to researchers, summarised in box 1. While the illustrative examples that we use to support our recommendations are grounded in the US context, our recommendations are relevant to the global research community.
Box 1. Research recommendations to better inform housing policies that advance health equit.
An advocacy orientation and interdisciplinary, community-partnered coalitions
Strive to promote ‘Health in All Policies’.
Embrace advocacy.
Monitor shifting policy landscapes and housing justice movements and respond in real time.
Collaborate in interdisciplinary teams with quantitative and qualitative expertise.
Centre people with lived experience in research teams.
Consequentialist questions and expanded frameworks
Ask questions with the potential to meaningfully alter social, economic and policy landscapes.
Frame housing insecurity as a dynamic outcome of policy regimes.
Study residential instability across a range of severity (ie, housing cost burden to unsheltered homelessness).
Designing studies to strengthen causal interpretations
Leverage longitudinal datasets featuring within-person and between-person variation in exposure to housing insecurity.
Take care to accurately reflect movement of people across geographies and jurisdictional boundaries.
Include appropriate time lags for disease aetiology and policy implementation factors.
Improve capacity for housing policy surveillance.
Ascertain detailed residential histories to facilitate linkages to policy databases.
Use conceptual frameworks to incorporate housing insecurity modules into questionnaires.
Testing for policy impacts on health inequity
Measure effects across structurally vulnerable subgroups (via stratification or interaction models, disparities as primary outcomes).
Oversample populations who stand to reap the most benefits or harms from a particular housing policy.
Communication for change
Partner with community organisers to promote evidence-based policymaking.
Align research agendas with community priorities and advocacy needs.
Make research transparent and freely accessible.
Co-create dissemination plans with community partners and disseminate research via a variety of channels.
Produce absolute estimates (eg, lives saved, cases prevented).
Make results accessible through data visualisation and qualitative narratives.
Highlight clear calls to action for policymakers.
An advocacy orientation and interdisciplinary, community-partnered coalitions
Evidence from health research can be used to inform a ‘Health in All Policies’ approach to housing policy, through which leaders in the housing sector factor health and health equity considerations into their decision-making processes.33 However, to achieve this goal, we cannot shy away from politics and advocacy. We must be attuned to shifts in policy landscapes and housing justice movements, responding to pressing needs for evidence on health, housing and social policy in real time. While this new mindset might seem revolutionary, it merely represents a return to the origins of public health in social reform movements.34
Doing so will require more interdisciplinary research teams, leveraging expertise from such fields as law, political science, urban planning and economics. A Health in All Policies approach also requires an understanding of governance to encourage intersectoral partnerships and address issues of siloed funding.35 By integrating these complementary perspectives and leveraging the combined power of quantitative and qualitative research methods, we can bring a more comprehensive understanding of how housing policies affect health and health equity to policy debates.
Most importantly, we must centre people who have lived experience with housing insecurity in our research teams. This change is essential to conducting better science, ensuring that research and policy recommendations are grounded in reality and results are relevant to affected peoples. Community partners and other stakeholders should be involved in all steps of research, beginning with the crafting of research questions and ending with dissemination. Successful partnerships must go beyond extractive paradigms by building power together and sharing the social and economic benefits of the research enterprise. Working in coalitions, we can produce research that informs movements, pushes policy levers and empowers people with tools to be their own agents of change.36
One such coalition is the Healthy Neighborhoods Study (HNS), an ongoing academic-community partnership investigating the impact of urban development on community health in the Boston metropolitan area.37 38 Academic researchers partnered with community organisations to recruit paid resident researchers, who then took the lead by visioning HNS’ research projects, designing research questions, conducting data collection and disseminating findings to inform community advocacy and drive policy action. Academic HNS epidemiologists provided technical support and coordinated research workshops throughout. Resident researchers have already begun using their results to inform community organising efforts,39 40 and local agencies have used findings from HNS to determine how to allocate funding to benefit community health.
Consequentialist questions and expanded frameworks
Health researchers should pursue research questions with the potential to meaningfully alter social, economic and policy landscapes, an orientation known as ‘consequentialist epidemiology.’41 Through this lens, we can study the health impacts of specific programmes, policies and policy-sensitive processes. As an example, whereas an aetiological study might measure the degree to which housing insecurity is associated with mental distress, a more consequentialist study might ask, ‘How does living in housing subsidized by the Low-Income Housing Tax Credit affect mental distress among US adult renters?’ That being said, studies need not strictly comply with the Potential Outcomes Framework’s ‘well-defined interventions’ prerequisite, often expressed as requiring a currently imaginable randomised controlled trial (RCT).42 By their very nature, grassroots, community-driven housing solutions are difficult to conceive of as an RCT: there is rarely an obvious control group, there are multiple versions of interventions and interventions spill over to benefit neighbours. Nonetheless, these are some of the most vital movements to learn from. Mixed-methods approaches are well-suited to these applications, leveraging quantitative and qualitative data to track implementation and impact. Researchers can also look beyond existing interventions, simulating impacts of future policies through Health Impact Assessments.43
Relatedly, research on housing and health could also be improved by framing housing insecurity as a dynamic outcome of policy regimes with a collective, structural origin.44 By treating housing insecurity as a static state, we limit our analytic scope and obscure the role of power, politics and systems of oppression. For instance, focusing on the ‘neighbourhood resources’ dimension of housing insecurity, a large research base links neighbourhood deprivation to poor health outcomes with little recognition of the policies that deprive communities of wealth or the affluent communities that profit from this deprivation. Operating within this limited scope, the neighbourhood itself is blamed for ill health, rather than the policies and power dynamics that moulded it.
We further advocate for an expanded examination of residential instability, ranging from the everyday strain of living with cost burden all the way to unsheltered homelessness. This more encompassing view allows for a comprehensive understanding of the ways that housing policy failures have harmed health.
Designing studies to strengthen causal interpretations
To measure causal relationships between housing insecurity and health, study samples must include both within-person and between-person variation in exposure to housing insecurity. Absent this variation, studies can suffer from temporal ambiguity, which limits their ability to provide accountability and drive systems change. A common and politically expedient conclusion drawn from cross-sectional studies is that individual behaviours and health (specifically, substance use or mental illness) lead to homelessness—even though the causal arrow often goes the other way. This conveniently absolves those in power of their roles in creating policies and practices that drive housing insecurity. To avoid reifying stigmatising narratives and build evidence for change, researchers must leverage longitudinal datasets to strengthen causal interpretations of their findings. By comparing health trajectories between individuals exposed versus unexposed to housing insecurity, studies can invoke a powerful, prevention-oriented counterfactual: ‘what would happen to health if families were stably housed?’
Studies of housing policies and health must also consider place, taking care to accurately reflect movement of people across geographies. Housing policies are often implemented at the state-level or county-level in the USA, presenting opportunities for quasiexperimental study designs. However, low-income renters in the USA move frequently,45 often crossing jurisdictional boundaries, hindering participant retention and potentially causing misclassification. To complicate matters further, research on housing policies often studies exposures that directly impact a household’s mobility and may therefore cause selection bias.
Additionally, it is important to consider the time horizon over which housing policies might affect various health outcomes by incorporating appropriate time lags that reflect disease aetiology and policy implementation (eg, timing of public notifications, roll-out and enforcement). For instance, whereas an eviction moratorium puts an immediate halt to eviction proceedings, a single-family zoning ban may take decades to transform density and expand access to affordable housing. Flexible designs such as event studies that do not require an a priori specification of effect lags might be well-suited to these questions.46
For researchers to rigorously account for the movement of people across space and time in their study designs, funders must prioritise the development of better data infrastructure. Part of this endeavour will involve improving our capacity for longitudinal housing policy surveillance. Studies should gather high-quality data on residential histories, facilitating linkages to data on place-based policies and neighbourhood characteristics. Researchers can use conceptual frameworks to incorporate housing modules into questionnaires, collecting detailed information on physical aspects of housing and neighbourhoods and differentiating between types of residential instability (eg, formal vs informal evictions).
Testing for policy impacts on health inequity
Studies must be designed to measure disparate policy impacts. Seemingly race-neutral or class-neutral housing interventions can further entrench disparities if not implemented equitably. As an example, lead paint was banned in 1978. However, because lead exposure prevention requires that tenants have either the power to advocate for remediation or the money and housing options to move out if necessary, low-income children—particularly children of colour—continue to be poisoned by lead over four decades later.47 Thus, it is important to evaluate policies not only based on population-wide effect estimates but also by measuring effects across structurally vulnerable subgroups (eg, groups marginalised along lines of race, class, gender, sexual orientation). Analytically, such evaluations may involve stratification, interaction models or modelling of disparities themselves as primary outcomes. Approaches often require researchers to oversample populations who stand to reap the most benefits or harms from a particular housing policy to ensure statistical power.
Communication for change
Teaching researchers how to communicate with policymakers with the hope that policies will simply follow the evidence is short-sighted and ahistorical. Policymaking is an exercise in power as much as it is an exercise in governance; community organising remains critical to policy change. Research will have a limited impact if it does not align with community members’ concerns or if it is not useful for advocacy. Communication must also be bidirectional, such that communities’ knowledge about their own lives informs our future research agendas and how we interpret our findings.
On a basic level, research is only useful to stakeholders when it is freely accessible. Thus, researchers should adhere to the principles of open science and share results with stakeholders via a variety of channels, including both social and traditional media and in-person communication. Dissemination plans should be cocreated in partnership with community stakeholders as well as housing providers and policymakers.
The way we present our results also matters. Advocacy groups and policymakers rarely think in odds ratios. Where possible, we recommend using producing absolute estimates (lives saved, cases prevented) to illustrate the human toll of policy (in)action. Such estimands magnify the humanity of affected communities and inform the public narrative around policy choices. Data visualisation can also make results more accessible, as can qualitative narratives that allow affected populations to speak for themselves. Finally, dissemination efforts should highlight clear calls to action for policymakers.
Conclusion
Housing may be at once the most powerful and underused tool at our disposal to improve population health. The COVID-19 pandemic and related economic downtown has heightened awareness of the long-standing housing crisis in the USA, leading to a groundswell of support for policies to promote housing security and health. Health researchers can join housing justice movements to convert this momentum into lasting change. Meeting the moment means rethinking who we centre in research, the questions we ask and how we answer them and the ways we define and share knowledge. Going against the grain in these ways may be difficult, but keeping families housed and healthy will be worth the effort.
Acknowledgments
The authors thank Dr Katherine L Chen for critical review of the manuscript and conceptual framework as well as Dr Frederick J Zimmerman for conversations that informed some of the thinking reflected in this piece.
Footnotes
Twitter: @LeifScience
Contributors: Conceptualisation: KML, GLS, CEP and SLL. Writing (original draft): KML. Writing (review and editing): KML, GLS, CEP and SLL. Important intellectual content: KML, GLS, CEP and SLL. Revisions and approval of the final version: KML, GLS, CEP and SLL. Guarantor: KML.
Funding: This study was funded by Agency for Healthcare Research and Quality (2T32HS000046).
Competing interests: KML was supported by the Agency for Healthcare Research and Quality (AHRQ; grant no T32HS000046). The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ. CEP works part time on a temporary assignment with the Department of Housing and Urban Development (HUD), assisting the department on housing and health issues. The findings and conclusions in this article are those of the authors and do not necessarily represent those of HUD or other government agencies.
Provenance and peer review: Commissioned; externally peer reviewed.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1. Shaw M. Housing and public health. Annu Rev Public Health 2004;25:397–418. 10.1146/annurev.publhealth.25.101802.123036 [DOI] [PubMed] [Google Scholar]
- 2. Jones-Eversley SD, Dean LT. After 121 Years, It’s Time to Recognize W.E.B. Du Bois as a Founding Father of Social Epidemiology. J Negro Educ 2018. [Google Scholar]
- 3. Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health 2002;92:-:758–68. 10.2105/AJPH.92.5.758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Howden-Chapman P. Housing standards: a glossary of housing and health. J Epidemiol Community Health 2004;58:162–8. 10.1136/jech.2003.011569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dunn JR. Housing and health inequalities: review and prospects for research. Hous Stud 2000;15:341–66. 10.1080/02673030050009221 [DOI] [Google Scholar]
- 6. Jacobs DE, Brown MJ, Baeder A. A systematic review of housing interventions and health: introduction, methods, and summary findings. J Public Health Manag Pract 2010;16:5–10. [DOI] [PubMed] [Google Scholar]
- 7. Padgett D, Henwood BF, Tsemberis SJ. Housing First: Ending Homelessness, Transforming Systems, and Changing Lives. USA: Oxford University Press, 2016. [DOI] [PubMed] [Google Scholar]
- 8. Carliner M, Marya E. Rental Housing : An International Comparison, 2016. [Google Scholar]
- 9. Joint Center for Housing Studies of Harvard University . America’s Rental Housing 2020, 2020. Available: https://www.jchs.harvard.edu/americas-rental-housing-2020
- 10. The Eviction Lab . National estimates, 2018. Available: https://evictionlab.org/national-estimates/
- 11. Gromis A, Desmond M. Estimating the prevalence of eviction in the United States. Cityscape 2021;23:279–90. [Google Scholar]
- 12. National alliance to end homelessness. state of homelessness: 2021 edition, 2021. Available: https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness-2021/
- 13. Swope CB, Hernández D. Housing as a determinant of health equity: a conceptual model. Soc Sci Med 2019;243:112571. 10.1016/j.socscimed.2019.112571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hernández D. Understanding 'energy insecurity' and why it matters to health. Soc Sci Med 2016;167:1–10. 10.1016/j.socscimed.2016.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schwartz GL, Leifheit KM, Berkman LF, et al. Health selection into eviction: adverse birth outcomes and children's risk of eviction through age 5 years. Am J Epidemiol 2021;190:1260–9. 10.1093/aje/kwab007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gold S, Wagner B. Acute care utilization and housing hardships in American children. Child Youth Serv Rev 2022;136. 10.1016/j.childyouth.2022.106447. [Epub ahead of print: 01 Mar 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Our World in Data . Sustainable development goal 6: ensure access to water and sanitation for all. sustainable development goal Tracker, 2020. Available: https://sdg-tracker.org/water-and-sanitation#targets
- 18. USDA Economic Research Service . Food security and nutrition assistance, 2021. Available: https://www.ers.usda.gov/data-products/ag-and-food-statistics-charting-the-essentials/food-security-and-nutrition-assistance/
- 19. Cutler D, Miller G. The role of public health improvements in health advances: the twentieth-century United States. Demography 2005;42:1–22. 10.1353/dem.2005.0002 [DOI] [PubMed] [Google Scholar]
- 20. Heflin CM, Ingram SJ, Ziliak JP. The effect of the supplemental nutrition assistance program on mortality. Health Aff 2019;38:1807–15. 10.1377/hlthaff.2019.00405 [DOI] [PubMed] [Google Scholar]
- 21. Center on Budget and Policy Priorities . 3 in 4 low-income Renters needing Rental assistance do not receive it., 2021. Available: https://www.cbpp.org/research/housing/three-out-of-four-low-income-at-risk-renters-do-not-receive-federal-rental-assistance
- 22. Rothstein R. The color of law: a forgotten history of how our government segregated America. Liveright Publishing, 2017. [Google Scholar]
- 23. Goetz EG. New deal ruins. Cornell University Press, 2013. [Google Scholar]
- 24. Bailey ZD, Krieger N, Agénor M, et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–63. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 25. Krieger N, Van Wye G, Huynh M, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013-2017. Am J Public Health 2020;110:1046–53. 10.2105/AJPH.2020.305656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nardone A, Casey JA, Morello-Frosch R, et al. Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study. Lancet Planet Health 2020;4:e24–31. 10.1016/S2542-5196(19)30241-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schwartz E, Onnen N, Craigmile PF, et al. The legacy of redlining: associations between historical neighborhood mapping and contemporary tobacco retailer density in Ohio. Health Place 2021;68:102529. 10.1016/j.healthplace.2021.102529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jacoby SF, Dong B, Beard JH, et al. The enduring impact of historical and structural racism on urban violence in Philadelphia. Soc Sci Med 2018;199:87–95. 10.1016/j.socscimed.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001;116:404–16. 10.1016/S0033-3549(04)50068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. World Health Organization . WHO housing and health guidelines, 2018. Available: http://www.who.int/phe%0Ahttp://apps.who.int/bookorders
- 31. The U.S. Department of Housing and Urban Development . Fiscal year 2022-2026 strategic plan, 2022. [Google Scholar]
- 32. U.S. Department of Health and Human Services 2030 . Housing and homes. Healthy people, 2020. Available: https://health.gov/healthypeople/objectives-and-data/browse-objectives/housing-and-homes [Accessed 05 Aug 2022].
- 33. Rudolph L, Caplan J, Ben-Moshe K. Health in all policies: a guide for state and local governments. 169, 2013. [Google Scholar]
- 34. Yong E. How public health took part in its own Downfall. The Atlantic, 2021. [Google Scholar]
- 35. de Leeuw E. Engagement of sectors other than health in integrated health governance, policy, and action. Annu Rev Public Health 2017;38:329–49. 10.1146/annurev-publhealth-031816-044309 [DOI] [PubMed] [Google Scholar]
- 36. Harris P, Baum F, Friel S, et al. A glossary of theories for understanding power and policy for health equity. J Epidemiol Community Health 2020;74:548–52. 10.1136/jech-2019-213692 [DOI] [PubMed] [Google Scholar]
- 37. Binet A, Gavin V, Carroll L, et al. Designing and facilitating Collaborative research design and data analysis workshops: lessons learned in the healthy neighborhoods study. Int J Environ Res Public Health 2019;16. 10.3390/ijerph16030324. [Epub ahead of print: 24 Jan 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Arcaya MC, Schnake-Mahl A, Binet A, et al. Community change and resident needs: designing a participatory action research study in metropolitan Boston. Health Place 2018;52:221–30. 10.1016/j.healthplace.2018.05.014 [DOI] [PubMed] [Google Scholar]
- 39. Seeder A. Organizing for healthy housing. conservation law fund, 2020. Available: https://www.clf.org/blog/organizing-for-healthy-housing/ [Accessed 05 Jul 2022].
- 40. Sengupta S. Researchers bring the power of data home. conservation law fund, 2019. Available: https://www.clf.org/blog/researchers-bring-the-power-of-data-home/ [Accessed 05 Jul 2022].
- 41. Galea S. An argument for a consequentialist epidemiology. Am J Epidemiol 2013;178:1185–91. 10.1093/aje/kwt172 [DOI] [PubMed] [Google Scholar]
- 42. Hernán MA, Van Der Laan MJ, Haight TJ. Invited commentary: hypothetical interventions to define causal effects--afterthought or prerequisite? Am J Epidemiol 2005;162:618–20. 10.1093/aje/kwi255 [DOI] [PubMed] [Google Scholar]
- 43. Bever E, Arnold KT, Lindberg R, et al. Use of health impact assessments in the housing sector to promote health in the United States, 2002-2016. J Hous Built Environ 2021;36:1277–97. 10.1007/s10901-020-09795-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kramer MR. Why history? explanation and accountability. Am J Public Health 2020;110:933–4. 10.2105/AJPH.2020.305726 [DOI] [Google Scholar]
- 45. Kang S. Why low-income households become unstably housed: evidence from the panel study of income dynamics. Hous Policy Debate 2019;29:559–87. 10.1080/10511482.2018.1544161 [DOI] [Google Scholar]
- 46. Goodman-Bacon A. Difference-in-differences with variation in treatment timing. J Econom 2021;225:254–77. 10.1016/j.jeconom.2021.03.014 [DOI] [Google Scholar]
- 47. Benfer E. Contaminated childhood: the chronic lead poisoning of low-income children and communities of color in the United States. Heal Aff Blog 2017;10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available.