Abstract
Background
Compared with the seropositive rheumatic arthritis (sp-RA), seronegative rheumatic arthritis (sn-RA) lacks ultrasound (US) research. It is unknown whether sn-RA patients had more severe synovitis than sp-RA ones at the same level of swollen joint counts (SJCs). We designed the US study to find out the answers.
Methods
All cases satisfied the 2010 classification criteria, first diagnosed and disease-modifying anti-rheumatic drugs (DMARDs) naïve with the characteristics of abnormal swelling or pain in the wrist, proximal interphalangeal (PIPs), and metacarpophalangeal (MCPs) joints. Demographic data was collected. US examinations, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), visual analogue scale scores (VASs), patient global assessment (PGA), physician’s global assessment (PhGA), disease activity score of 28 joints (DAS28), and van der Heijde-modified Sharp score (vdHSS) were used to evaluate the disease activity among these groups. Anticitrullinated peptide antibody (ACPA), rheumatoid factor (RF) and SJCs were used to divide the patients into 3 groups, which were defined as follows: Group A, sp-RA (positive RF and/or ACPA) with SJC >10; Group B, sp-RA with SJC ≤10; and Group C, sn-RA (all negative RF and ACPA with SJC >10 due to the criteria).
Results
A total of 139 cases were recruited. Fifty-six were Group A, 54 were Group B, and 29 were Group C. All indexes above and the total US scores were significantly lower in Group C than Group A (both groups with SJC >10) (ESR, CRP, VASs, PGA, PhGA, DAS28, vdHSS, US total score respectively: 58.8 vs. 37.5, P=0.009; 37.5 vs. 17.8, P=0.008; 61.7 vs. 52.8, P=0.032; 62.2 vs. 53.9, P=0.031; 59.8 vs. 48.3, P=0.029; 6.92 vs. 5.56, P=0.000; 61.7 vs. 44.5, P=0.023; 31.4 vs. 20.9, P=0.000). The difference of the total US scores above was mostly contributed by the symptoms of synovitis. The total US scores were prominently lower in Group C with the duration over 2 years (2–5 years, >5 years, respectively compared to <2 years: 16.3 vs. 27.4, P=0.044; 16.5 vs. 27.4, P=0.048), and vdHSS were remarkably higher in almost all groups with a duration of over 5 years. For the patients with a duration over 2 years, bone erosions occurred earlier in sp-RA than in sn-RA patients.
Conclusions
Sn-RA patients had milder synovitis than sp-RA ones at the same extent of disease activity. In addition, sn-RA had delayed progress of bone erosion than the sp-RA group.
Keywords: Rheumatoid arthritis (RA), ultrasound (US), X-ray
Introduction
Rheumatoid factor (RF) has long been one of the critical pieces of evidence for the diagnosis of rheumatoid arthritis (RA). Both the 1987 American College of Rheumatology (ACR) classification criteria and 2010 ACR/European League Against Rheumatism (EULAR) classification criteria have underlined its role (1,2). Anticitrullinated protein antibodies [ACPA; also called anti-cyclic citrullinated peptide (CCP)] was believed to be a better innovative predictor than RF for RA (3), and the 2010 ACR/EULAR criteria stated its important role. These two serological indexes (ACPA and RF) were used to classify RA patients into two subgroups, namely seropositive RA (sp-RA; RF+ and/or ACPA+) and seronegative RA (sn-RA; RF− and ACPA−). Patients with sp-RA were found to share certain genetic and environmental risk factors, and anti-RA drugs were shown to exert therapeutic effects on this subgroup (4). In contrast to sp-RA, sn-RA has been less studied. Unlike the group of sp-RA, the distinct genetic background and pathogenesis of sn-RA was reported to lead to different prognosis and therapeutic response. From the clinical aspect, it seemed that in comparison to sn-RA, sp-RA progressed more aggressively, had a more severe disease course, and worse prognosis (5-7).
Ultrasound (US) is a useful and convenient tool for detecting synovitis in RA (8,9). Two reports by Nordberg et al. were the first and the only to mainly focus on ultrasonic presentations of sn-RA (10,11). They declared that early RA patients (with a disease duration of <2 years) who were not receiving treatment of disease-modifying anti-rheumatic drugs (DMARDs) had more severe synovitis than those with sp-RA. However, their grouping method of the study might have a problem. US total score is a cumulative score of involved swollen joints, hence more swollen joints result in higher US score. Since 2010 rheumatoid arthritis classification criteria (2) required ≥6 points to diagnose RA, sp-RA patients might have 3 points from positive RF + ACPA, 1 point from increasing ESR or CRP, 1 point from ≥6 weeks disease course, so only 1 swollen joint (1 score) is needed to make the diagnosis of RA. On contrast, sn-RA patients have 0 points from negative RF + ACPA, 1 point from increasing ESR or CRP, 1 point possibly from disease course ≥6 weeks, therefore >10 swollen joint (4 scores) must be needed to make the diagnosis. It is known that SJC is positive correlation to disease activity and US total scores (12), certainly the sn-RA (all cases >10 SJC) would have more severe disease activity, higher US total score than sp-RA (partly cases ≤10). However, would sn-RA patients have more severe synovitis or higher US total score than sp-RA ones while both have SJC >10? It is still unknown. Another problem is about the disease duration. Nordberg et al. research enrolled cases with disease course <2 years (10). The short duration might cause less bone erosion. Whether sn-RA has more severe bone erosion than sp-RA with longer disease duration is also unknown.
To answer the questions above, we designed the study. The grouping method is as follows: (A) sp-RA with SJC >10; (B) sp-RA with SJC ≤10; and (C) sn-RA. The participants in all groups were DMARDs-naïve, and no limitation was placed on disease duration. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2171/rc).
Methods
Sample size estimation
It is a cross-sectional US study. We used the authoritative website “http://powerandsamplesize.com/” to calculate the sample size. Referring to the US total scores of sp-RA and sn-RA in the article by Nordberg et al. (10), two-sample, two-sided comparing 2 means sample size calculation (power =0.9, a=0.05, Na/Nb =5) was carried out. The results showed that 30 cases of sn-RA and 82 cases of sp-RA are needed to be enrolled. Considering better results and the loss visits, we asked for 200 people and 139 cases were finally enrolled.
Patients
Patients with RA who met the requirement of the 2010 classification criteria were recruited in the Rheumatology Inpatient Department of the Third Affiliated Hospital of Sun Yat-sen University between 2013 and 2017. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Ethics Board of Third Affiliated Hospital of Sun Yat-sen University (No. [2013]2-99) and informed consent was provided by all patients. The inclusion and exclusion criteria were as follow: (I) abnormal swelling or pain in one of the wrists, the 2nd and 3rd metacarpophalangeal joints (MCP2/3), or the 2nd and 3rd proximal interphalangeal joints (PIP2/3); (II) first diagnosis in our hospital; (III) DMARDs had not been used before; and (IV) agreement to the clinical trial and informed consents was provided. The exclusion criteria were as follows: (I) comorbidity of other rheumatic diseases; (II) chronic active infections such as tuberculosis, hepatitis B; and (III) any history of malignancy or highly suspicious malignancy present at the time of recruitment.
After admission to our study, patients were classified as: (I) Group A, sp-RA (positive RF and/or ACPA) combined with SJC >10; (II) Group B, sp-RA combined with SJC ≤10; and (III) Group C, sn-RA (negative RF and negative ACPA).
Data collection
The collected data upon recruitment included demographic data (sex, age, history, disease duration), ACPA, RF, and disease activity related indicators: erythrocyte sedimentation rate (ESR) (mm/h), C-reactive protein (CRP) (mg/L), pain on 0–100 mm visual analogue scales (VASs), SJC, patient global assessment (PGA) of disease activity on VASs, the physician’s assessment of disease activity on VASs (PhGA), and the disease activity score of 28 joints (DAS28).
Enzyme-linked immunosorbent assay (ELISA) was used to analyze RF and ACPA. A positive result means any value >10 IU/mL for ACPA and 20 IU/mL for RF.
Radiograms of hands and wrists were acquired and scored according to van der Heijde-modified Sharp score (vdHSS) (13,14) by two experienced readers blinded to one another. An expert (with more than 5 years of experience in the field of musculoskeletal X-ray in the Rheumatology Department) was consulted to make a final decision if the 2 readers obtained different scores.
Ultrasound
US examinations were performed simultaneously with the data collection. Grey-scale images were obtained from an Mylab30 Ultrasound System (Esaote, Genoa, Italy). Each patient was scanned in the position according to EULAR guidelines (14). Each region was studied by at least 2 high-quality pictures in both axial and coronal planes. The two observers who performed the US examinations remained blinded to all other study data. The 5 joints included the MCP2/3, (PIP2/3, and the wrist of the clinically dominant side. An US scoring system (0–122 scores) was derived from Backhaus’ US7 scoring system (12) (Table 1). The final scores were calculated independently by the two observers, with a 3rd person (the US expert with over 5-year experience in the Ultrasound Department) invited to arbitrate if the two observers obtained different scores.
Table 1. Ultrasound scoring system (0–122) for evaluation wrists and hands in RA.
| Scores for US features | Wrist | MCP2/3 | PIP2/3 | Partial scores |
|---|---|---|---|---|
| Synovitis grey-scale scores (0–3) | Dorsal median/ulnar/palmar median | Dorsal/palmar | Dorsal/palmar | 0–33 |
| Synovitis power Doppler scores (0–3) | Dorsal median/ulnar/palmar median | Dorsal/palmar | Dorsal/palmar | 0–33 |
| Tenosynovitis grey-scale scores (no =0, yes =1) | Dorsal median/ulnar/palmar median | Dorsal/palmar | Dorsal/palmar | 0–11 |
| Synovitis power Doppler scores (0–3) | Dorsal median/ulnar/palmar median | Dorsal/palmar | Dorsal/palmar | 0–33 |
| Bone erosion grey-scale scores (no =0, yes =1) | Dorsal median/ulnar/palmar median | Dorsal/palmar + MCP2 radial | Dorsal/palmar | 0–12 |
RA, rheumatoid arthritis; MCP2/3, 2nd and 3rd metacarpophalangeal joints; PIP2/3, the 2nd and 3rd proximal interphalangeal joints.
The inter-observer validity for the evaluation of the US features, including synovitis grey-scale scores, synovitis power Doppler scores, tenosynovitis grey-scale scores, tenosynovitis power Doppler scores, bone erosion scores, were determined between the observers and the US expert by comparing the pictures of 10 patients in random sequence. Intra-observer validity was assessed by the way of rescoring the same pictures after 2 months.
Statistical analysis
Statistical analyses were performed using the software SPSS 23.0 (IBM Corp., Armonk, NY, USA). Continuous variables were presented as means [standard deviation (SD)] or medians (25th, 75th centiles) according to distribution, and dichotomous variables were presented as frequencies and percentages. Disease characteristics were compared between each two subgroups by independent samples t-test, Mann-Whitney U test, or χ2 test as appropriate. Two-sided and P values less than 0.05 were considered statistically significant in all statistical tests.
Results
A total of 139 patients with mean age (SD) 52.0 (14.0) years and median disease duration 60 [24, 120] months were included in our study. Overall, 38 of 139 patients (27.3%) were men, the rest (72.7%) were women. No one had RA family history, though 1 sn-RA case with a systemic lupus erythematous (SLE) mother, 1 sp-RA case with a primary Sjogren’s syndrome sister. In all, 56 (40.3%) participants were sp-RA with SJC >10 (Group A), 54 (38.8%) were sp-RA with ≤10 (Group B), and 29 (20.9%) were sn-RA (Group C). Age and gender distribution were similar but the disease duration of sn-RA patients was much shorter than that of sp-RA (Table 2).
Table 2. Clinical characteristics compared across serology status.
| Variables | Sp-RA + SJC >10 (Group A, n=56) |
Sp-RA + SJC ≤10 (Group B, n=54) | Sn-RA (Group C, n=29) | Sp-RA (Group A + B, n=110) |
|---|---|---|---|---|
| Age, years | 52.0 (13.6) | 52.5 (14.6) | 50.9 (14.1) | 52.2 (14.1) |
| Female, n (%) | 40 (71.4) | 40 (74.1) | 21 (72.4) | 80 (72.7) |
| Disease duration, months | 97.5 (24.0–122.3)1,2 | 113.9 (36.0–147.0)1,3 | 46.3 (47.3)2,3 | 78.0 (27.0–126.8)4 |
| Positive for ACPA (%) | 54 (96.4) | 52 (96.3) | NA | 106 (96.4) |
| Positive for RF IgM (%) | 41 (73.2) | 40 (74.1) | NA | 81 (73.6) |
| Positive for RF IgA (%) | 31 (55.3) | 30 (55.5) | NA | 62 (55.5) |
| DAS28 | 6.92 (1.02)1,2 | 4.73 (0.91)1,3 | 5.56 (0.89)2,3 | 5.84 (1.46) |
| CRP, mg/L | 37.5 (10.5–59.7)1,2 | 29.2 (1.5–41.2)1 | 17.8 (1.65–22.13)2 | 15.5 (4.5–55.8) |
| ESR, mm/h | 58.8 (29.0–95.0)2 | 31.9 (25.0–85.8) | 37.5 (16.5–54.5)2 | 44.5 (29.0–88.5) |
| PhGA, 0–100 mm | 59.8 (17.1)1,2 | 39.7 (14.6)1,3 | 48.3 (17.4)2,3 | 49.9 (16.2) |
| PGA, 0–100 mm | 62.2 (18.0)1,2 | 45.6 (18.8)1,3 | 53.9 (20.6)2,3 | 54.1 (18.5) |
| Pain VAS, 0–100 mm | 61.7 (15.9)1,2 | 44.7 (16.2)1,3 | 52.8 (18.5)2,3 | 53.4 (18.1) |
| Total vdHSS | 61.7 (23.5–108.5)1,2 | 45.0 (3.0–66.8)1 | 44.5 (8.0–64.0)2 | 47.5 (9.5–92.0) |
| Total US score | 31.4 (9.3)1,2 | 19.3 (8.5)1 | 20.9 (10.1)2 | 25.5 (10.8)4 |
Values are median (25th–75th centiles) or mean (SD), unless otherwise indicated. 1, P<0.05 while the parameters of Group A compared to Group B; 2, P<0.05 while the parameters of Group A compared to Group C; 3, P<0.05 while the parameters of Group B compared to Group C; 4, P<0.05 while the parameters of Group A+B compared to Group C. All the above comparisons of indexes between two groups are non-parametric statistics except ages (t-test, B compared to C: t=0.48, sig. =0.79; A compared to C: t=0.32, sig. =0.62; A compared to B: t=0.22, sig. =0.82). ACPA, anticitrullinated peptide antibody; CRP, C-reactive protein; DAS28, disease activity score of 28 joints; ESR, erythrocyte sedimentation rate; PGA, patient global assessment; PhGA, physician’s global assessment; RF, rheumatoid factor; SD, standard deviation; sig., significance; SJC, swollen joint counts; sn-RA, seronegative rheumatoid arthritis; sp-RA, seropositive rheumatoid arthritis; US, ultrasound; VAS, visual analogue scale; vdHSS, van der Heijde-modified Sharp score.
Inter- and intra-observer agreements by US
The inter-observer reliability showed an overall agreement of 96.1%, 91.2%, 93.0%, 87.8%, and 96.4% for the same score of synovitis grey-scale scores, synovitis power Doppler scores, tenosynovitis grey-scale scores, tenosynovitis power Doppler scores, and bone erosion scores, with k-values of 0.942, 0.897, 0.901, 0.869, and 0.955, respectively. The inter-observer and the intra-observer agreements were excellent with k-values of 0.965, 0.957, 0.940, 0.931, and 0.988, respectively. The total US scores were shown to be significantly positively correlated with DAS28 (P<0.05).
Comparisons of clinical characteristics
All disease activity indexes including DAS28, ESR, CRP, PhGA, PGA, and pain VAS, together with vdHSS scores and total US scores were significantly lower in the group with sn-RA (Group C) than in the group with sp-RA + SJC >10 (Group A), but all above indexes in Group C were higher than those of the group with sp-RA + SJC ≤10 (Group B), though without significance of CRP, ESR, vdHSS scores, and the total US scores (Table 2). As shown in Table 2, it was suggested that sn-RA (Group C) had higher disease activity than sp-RA + SJC ≤10 (Group B), but lower disease activity than sp-RA + SJC >10 (Group A). In addition, all above indexes, except ESR, were significantly higher in Group A than in Group B.
Comparisons of US indexes by different disease activity
To study the significant effect of diseases activity on total US scores, sp-RA + SJC ≤10 (Group B) was then divided into two subgroups according to high and moderate disease activity level (DAS28 >5.1 and 3.2≤ DAS28 ≤5.1). As all patients in sp-RA + SJC >10 (Group A) had DAS28 >5.1, it was not divided into a moderate activity subgroup. Meanwhile, no patients in our study had a DAS28 of <3.2, so mild activity and remission subgroups were not established. The comparison of each of the 5 parameters in US scores and total US scores with the reference of the same level of disease activity showed that total US scores were contributed mostly by synovitis grey-scale scores (Table 3). The total US scores and synovitis grey-scale scores were remarkably higher in Group A than the other two groups at the level of DAS >5.1.
Table 3. Ultrasonic and X-ray features compared across serology status with different swollen joint counts in the same DAS28 level.
| Scores for US features | DAS28 >5.1 | DAS28 ≤5.1 | ||||
|---|---|---|---|---|---|---|
| Sp-RA + SJC >10 (Group A, n=56) | Sp-RA + SJC ≤10 (Group B, n=18) | Sn-RA (Group C, n=19) | Sp-RA + SJC ≤10 (Group B, n=36) | Sn-RA (Group C, n=10) | ||
| US total scores | 31.4 (9.3)1,2 | 26.7 (8.9)1 | 24.7 (9.2)2 | 15.6 (5.3) | 12.3 (6.5) | |
| Synovitis grey-scale scores | 20.2 (5.1)1,2 | 16.8 (5.0)1 | 17.2 (12.0–22.0)2 | 13.2 (3.8) | 12 (7.5–16.5) | |
| Synovitis power Doppler scores | 4.6 (2.0–6.0) | 4.2 (2.0–6.0) | 3.4 (1.3–5.0) | 0.9 (0.0–1.8) | NA | |
| Tenosynovitis grey-scale scores | 1.1 (0.0–2.0) | 0.4 (0.0–0.3) | 0.5 (0.0–0.0) | 0.2 (0.0–0.0) | 0.3 (0.0–0.0) | |
| Tenosynovitis power Doppler scores | 0.6 (0.0–0.0)1,2 | 0.1 (0.0–0.0)1 | 0.1 (0.0–0.0)2 | 0.1 (0.0–0.0) | NA | |
| Bone erosion grey-scale scores | 3.9 (1.0–6.0) | 4.1 (4.0) | 2.9 (0.0–5.5) | 1.1 (0–2.0) | NA | |
| Total vdHSS | 70.4 (23.5–108.5) | 72. 2 (32.3–101.0) | 59.2 (28.8–86.0) | 31.4 (1.3–26.8) | 11.7 (0–20.0) | |
Values are median (25th–75th centiles) or mean (SD), unless otherwise indicated. 1, P<0.05 while the parameters of Group A compared to Group B with the same level of DAS28; 2, P<0.05 while the parameters of Group A group compared to Group C with the same level of DAS28. All the above comparisons of indexes between two group are non-parametric statistics. DAS28, disease activity score of 28 joints; SD, standard deviation; SJC, swollen joint counts; sn-RA, seronegative rheumatoid arthritis; sp-RA, seropositive rheumatoid arthritis; vdHSS, van der Heijde-modified Sharp score.
Comparisons of imaging by different disease durations
Disease duration is another factor which should be considered. The average disease duration of sn-RA (Group C) was observed to be shorter than that of sp-RA (Groups A and B). A transverse comparison was also made between subgroups at the same range of disease duration. In the situation of disease duration ≥2 years, the total US scores were significantly higher in Group A than in the other 2 groups; meanwhile, in the case of disease duration <2 years, the total US scores of Group B were significantly lower than those of Group C. In contrast to total US scores, no significant difference was observed in total vdHSS among 3 groups at the same range of disease duration (Table 4). In addition, the sn-RA (Group C) patients seemed to experience more severe synovitis for the first 2 years, which then decreased afterwards. On the contrary, sp-RA patients had almost the same level of synovitis throughout the years (Figure 1). Though all 3 groups had increasing bone erosion accompanied with disease duration, the sn-RA (Group C) patients might have had later progress of bone erosion than the sp-RA patients (Figure 2).
Table 4. Total ultrasound scores and total vdHSS compared across serology status with different SJC in the same disease duration.
| Disease durations | Number/ parameters |
Total US scores | Total vdHSS | |||||
|---|---|---|---|---|---|---|---|---|
| Sp-RA + SJC >10 (Group A) | Sp-RA + SJC ≤10 (Group B) | Sn-RA (Group C) | Sp-RA + SJC >10 (Group A) | Sp-RA + SJC ≤10 (Group B) | Sn-RA (Group C) | |||
| <2 years | N | 23 | 22 | 9 | 23 | 22 | 9 | |
| Parameters | 31.5 (10.2)1 | 22.5 (13.3)1 | 27.4 (7.0) | 43 (15.5) | 32.8 (16.7) | 40.4 (13.1) | ||
| 2–5 years | N | 33 | 31 | 12 | 33 | 31 | 12 | |
| Parameters | 33.0 (7.3)1,2 | 18.3 (6.2)1 | 16.3 (9.7)2 | 58.8 (39.7) | 51 (10.5) | 42.9 (45.1) | ||
| >5 years | N | 56 | 55 | 8 | 56 | 55 | 8 | |
| Parameters | 34.5 (10.0)1,2 | 22.7 (10.0)1 | 16.5 (0.8)2 | 105.7 (78.2) | 92.6 (57.1) | 92 (64.1) | ||
Values are mean (SD), unless otherwise indicated. 1, P<0.05 while the parameters of Group A compared to Group B with the same level of duration; 2, P<0.05 while the parameters of Group A group compared to Group C with the same level of duration. All the above comparisons of indexes between two group are non-parametric statistic. SJC, swollen joint counts; sp-RA, seropositive rheumatoid arthritis; sn-RA, seronegative rheumatoid arthritis; SD, standard deviation; US, ultrasound; vdHSS, van der Heijde-modified Sharp score.
Figure 1.
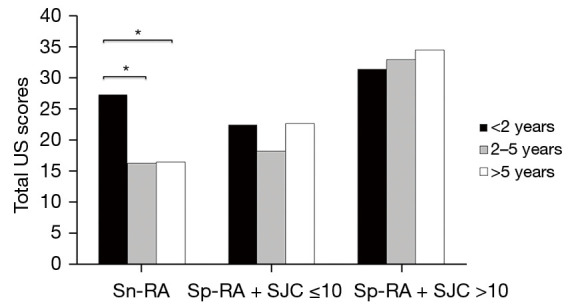
Bar chart of total US scores of different groups with different disease durations. Groups are divided according to sn-RA (Group C), sp-RA + SJC ≤10 (Group B), and sp-RA + SJC >10 (Group A). *, significant difference with P<0.05. SJC, swollen joint counts; sn-RA, seronegative rheumatoid arthritis; sp-RA, seropositive rheumatoid arthritis; US, ultrasound.
Figure 2.
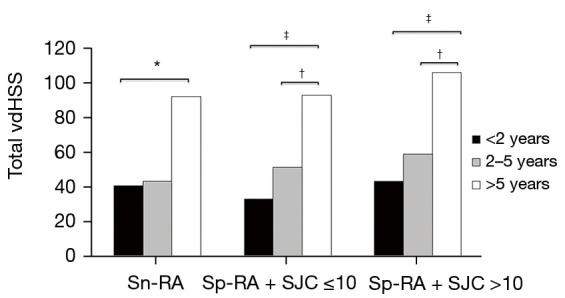
Bar chart of total vdHSS of different groups with different disease durations. Groups are divided according to sn-RA (Group C), sp-RA + SJC ≤10 (Group B), and sp-RA + SJC >10 (Group A). *, significant difference with P<0.05; †, significant difference with P<0.01; ‡, significant difference with P<0.001. sn-RA, seronegative rheumatoid arthritis; sp-RA, seropositive rheumatoid arthritis; SJC, swollen joint counts; vdHSS, van der Heijde-modified Sharp score.
Discussion
This research is the second US-based study on seronegative RA, but the first involving an Asian population. Notably, our conclusion is different to that of the first US study on sn-RA.
The US scoring system of wrists and hands in our study was designed on the basis of Backhaus’ US7 scoring system. Backhaus’ US7 scoring system has been used widely for its great intra- and inter-agreement, and also for its good positive correlation with DAS28 and 14-, 48-, and 72-joint scoring systems in previous studies. The wrist, PIP2/3, MCP2/3, and the 2nd and 3rd metatarsophalangeal joint (MTP2/3) in US7 were found to be most commonly involved in RA patients (10-12,15-17). Our study calculated only 5 joints due to the inclusion criteria including hands involvement, which was better equipped to compare the indicators of vdHSS and disease activity. The method was verified and shown to have good intra- and inter-agreement, and good positive correlation with DAS28. The inclusion criteria of patients to meet the requirement that local inflammation occurs in at least one joint of wrist, PIP2/3, or MCP2/3 which would reflect the disease activity of each patient.
Although Nordberg’s article discovered that disease activity was higher in sn-RA than sp-RA in early RA (<2 years), we detected lower inflammation and disease activity in the wrists and hands of sn-RA patients compared to those of sp-RA patients when both had the same range of SJC (SJC >10). We believe that the above conclusion is not paradoxical. In fact, both studies showed that SJC influenced the disease activity, and US scores had a positive correlation with DAS or DAS28 (10-11,18). In Nordberg’s study, sn-RA patients had a median of 17 swollen joints compared with 8 in sp-RA patients (P=0.001), which led to the higher disease activity and higher total sum US scores (10,11). In our study, the influence of SJC, disease activity, and disease duration were all considered by grouping methods. Thus, the total US scores reflect the extent of local inflammation with no influence by the above factors. As a result, we found that sn-RA patients had milder inflammation than sp-RA patients. Two recent studies in northern Africa also yielded similar results, suggesting that seropositive RA has more severe disease activity and joint damage. In a cohort study from Morocco, by comparing the number of swollen joints and X-ray changes, it was considered that patients with seropositive RA had more synovitis, deformities, and bone destructions on X-rays (19). A cohort study from Sudan also supported the above conclusion (20). Recently, Ramírez et al. collected the US images of both hands of 255 RA patients. They claimed that 55.5% of serum positive patients and 16.1% of serum negative patients had an extreme proliferative US pattern (US PS) (P=0.0001), which was defined as the obvious thickening of the synovium with high PD signal in the medial marginal zone of joint. Through reviewing our images, we confirmed the presence of the features described by Ramírez et al. US PS, but its proportion in sn-RA was slightly higher (17.2%) (20).
Barra et al. reported that among 841 cases of early RA (<2 years) in a Caucasian population, sn-RA patients were older, more males proportionately, and had shorter length of symptoms, higher scores of mean DAS28, and erosive disease (21). Regarding the early Asian RA patients (disease duration <2 years) in our study, we included the factors of age, DAS28, synovitis, and bone erosions on wrists and hands, and there was no difference of those factors between Chinese sn-RA and sp-RA, while shorter length of symptoms (4.2±4.7 vs. 8.2±5.0, P=0.03) and proportionately more males (40.0% vs. 28.6%) were noticed in sn-RA patients compared with sn-RA patients in our study. Large data evidence is required to validate the differences above.
The reason accounting for the different severity level of RA between different populations is perhaps related to the level of national health control. Due to lagging medical diagnosis level, lack of essential drugs such as methotrexate, abuse of irregular glucocorticoids, non-steroidal anti-inflammatory drugs (NSAIDs), and Chinese herbal medicine in China, the symptoms were more severe in RA patients with delayed treatment, as our study revealed. Therefore, it is not surprising that the vdHSS for the group with disease duration <2 years were much higher than Nordberg’s study reported. There were some limitations to our study such as inpatient enrollment bias and limited number of early RA (<2 years) patients, which may have contributed to the fact that the patients from the inpatient department were usually worse-off than the outpatients. However, although confronted by the poor control of RA in China, the US and X-ray features were shown to reflect the pathological progress of RA patients according to disease duration in the Asian population.
Conclusions
Through studying DMARDs-naïve RA patients in a Chinese cohort, it was found that the seronegative RA group had milder inflammation than the seropositive RA group at the same range of SJC (both >10). Seronegative RA had remarkably milder inflammation at over 2 years of disease duration and its progress of bone erosion was slower than that of seropositive RA.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Ethics Board of the Third Affiliated Hospital of Sun Yat-sen University (No. [2013]2-99) and informed consent was provided by all participants.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2171/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2171/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2171/coif). The authors have no conflicts of interest to declare.
(English Language Editor: J. Jones)
References
- 1.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315-24. 10.1002/art.1780310302 [DOI] [PubMed] [Google Scholar]
- 2.Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 2010;69:1580-8. 10.1136/ard.2010.138461 [DOI] [PubMed] [Google Scholar]
- 3.Alemao E, Guo Z, Frits ML, et al. Association of anti-cyclic citrullinated protein antibodies, erosions, and rheumatoid factor with disease activity and work productivity: A patient registry study. Semin Arthritis Rheum 2018;47:630-8. 10.1016/j.semarthrit.2017.10.009 [DOI] [PubMed] [Google Scholar]
- 4.Han B, Diogo D, Eyre S, et al. Fine mapping seronegative and seropositive rheumatoid arthritis to shared and distinct HLA alleles by adjusting for the effects of heterogeneity. Am J Hum Genet 2014;94:522-32. 10.1016/j.ajhg.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ajeganova S, Huizinga TW. Rheumatoid arthritis: Seronegative and seropositive RA: alike but different? Nat Rev Rheumatol 2015;11:8-9. 10.1038/nrrheum.2014.194 [DOI] [PubMed] [Google Scholar]
- 6.Pratt AG, Isaacs JD. Seronegative rheumatoid arthritis: pathogenetic and therapeutic aspects. Best Pract Res Clin Rheumatol 2014;28:651-9. 10.1016/j.berh.2014.10.016 [DOI] [PubMed] [Google Scholar]
- 7.Miner JJ, Aw-Yeang HX, Fox JM, et al. Chikungunya viral arthritis in the United States: a mimic of seronegative rheumatoid arthritis. Arthritis Rheumatol 2015;67:1214-20. 10.1002/art.39027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogura T, Hirata A, Hayashi N, et al. Comparison of ultrasonographic joint and tendon findings in hands between early, treatment-naïve patients with systemic lupus erythematosus and rheumatoid arthritis. Lupus 2017;26:707-14. 10.1177/0961203316676375 [DOI] [PubMed] [Google Scholar]
- 9.Takase-Minegishi K, Horita N, Kobayashi K, et al. Diagnostic test accuracy of ultrasound for synovitis in rheumatoid arthritis: systematic review and meta-analysis. Rheumatology (Oxford) 2018;57:49-58. 10.1093/rheumatology/kex036 [DOI] [PubMed] [Google Scholar]
- 10.Nordberg LB, Lillegraven S, Lie E, et al. Patients with seronegative RA have more inflammatory activity compared with patients with seropositive RA in an inception cohort of DMARD-naïve patients classified according to the 2010 ACR/EULAR criteria. Ann Rheum Dis 2017;76:341-5. 10.1136/annrheumdis-2015-208873 [DOI] [PubMed] [Google Scholar]
- 11.Nordberg LB, Lillegraven S, Aga AB, et al. Comparing the disease course of patients with seronegative and seropositive rheumatoid arthritis fulfilling the 2010 ACR/EULAR classification criteria in a treat-to-target setting: 2-year data from the ARCTIC trial. RMD Open 2018;4:e000752. 10.1136/rmdopen-2018-000752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Backhaus M, Ohrndorf S, Kellner H, et al. Evaluation of a novel 7-joint ultrasound score in daily rheumatologic practice: a pilot project. Arthritis Rheum 2009;61:1194-201. 10.1002/art.24646 [DOI] [PubMed] [Google Scholar]
- 13.van der Heijde DM, van 't Hof M, van Riel PL, et al. Development of a disease activity score based on judgment in clinical practice by rheumatologists. J Rheumatol 1993;20:579-81. [PubMed] [Google Scholar]
- 14.van der Heijde D. How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol 2000;27:261-3. [PubMed] [Google Scholar]
- 15.Hammer HB, Kvien TK. Comparisons of 7- to 78-joint ultrasonography scores: all different joint combinations show equal response to adalimumab treatment in patients with rheumatoid arthritis. Arthritis Res Ther 2011;13:R78. 10.1186/ar3341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Backhaus TM, Ohrndorf S, Kellner H, et al. The US7 score is sensitive to change in a large cohort of patients with rheumatoid arthritis over 12 months of therapy. Ann Rheum Dis 2013;72:1163-9. 10.1136/annrheumdis-2012-201397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skacelova M, Pavel H, Zuzana H, et al. Relationship Between Rheumatoid Arthritis Disease Activity Assessed with the US7 Score and Quality of Life Measured with Questionnaires (HAQ, EQ-5D, WPAI). Curr Rheumatol Rev 2017;13:224-30. 10.2174/1573397113666170517160726 [DOI] [PubMed] [Google Scholar]
- 18.Salma K, Nessrine A, Krystel E, et al. Rheumatoid Arthritis: Seropositivity versus Seronegativity; A Comparative Cross-sectional Study Arising from Moroccan Context. Curr Rheumatol Rev 2020;16:143-8. 10.2174/1573397115666191018115337 [DOI] [PubMed] [Google Scholar]
- 19.Seri A, Kamal Ali Mohamed H, Adam Essa ME, et al. Analysis of Serum Immune Markers in Seropositive and Seronegative Rheumatoid Arthritis Among Sudanese Patients and the Relation Between the Serotype and Joint Involvement: A Cohort Study. Open Access Rheumatol 2021;13:325-32. 10.2147/OARRR.S339134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramírez J, Azuaga-Piñango AB, Frade-Sosa B, et al. Proliferative synovitis, an ultrasound pattern associated with ACPA-positive patients and erosive disease in rheumatoid arthritis. Clin Exp Rheumatol 2022;40:960-6. [DOI] [PubMed] [Google Scholar]
- 21.Barra L, Pope JE, Orav JE, et al. Prognosis of seronegative patients in a large prospective cohort of patients with early inflammatory arthritis. J Rheumatol 2014;41:2361-9. 10.3899/jrheum.140082 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


