Abstract
Aims
Our study explored the perceived feasibility of using a home-based telerehabilitation service for older adults with chronic health conditions in Israel.
Method
This mixed-methods study included two focus groups of registered occupational therapists (n = 10) working in rehabilitation wards in Israel. Participants completed an open-ended questionnaire and Likert scale items so that data could be gathered on their perspectives regarding using an in-home telerehabilitation service for older adults after discharge from rehabilitation units. Thematic analysis with an a priori coding approach was applied to the data.
Results
Perceived advantages included transfer to the natural environment and the overcoming of geographical distance. Caregiver support and patient motivation were recognized as enabling factors. Perceived barriers included lack of hands-on contact and the concern that safety could be impeded by technological challenges and the patients’ cognitive status.
Conclusions
Findings from this study can potentially contribute to facilitating the implementation of a home-based telerehabilitation service as a practical alternative for elderly patients after discharge from rehabilitation units in Israel.
Keywords: Telemedicine, older adults, rehabilitation, occupational therapy, technologies, intervention
Introduction
The rapid increase in accessible and affordable technology offers the potential to deliver some healthcare services remotely via telerehabilitation (Saywell & Taylor, 2015). Telerehabilitation is the use of technologies to provide distant support, rehabilitation services, and information exchange between people with various health conditions and their health care providers (Chumbler et al., 2010; Fong & Kwan, 2020). In the last decade, before the COVID-19 pandemic, telerehabilitation had already become an important avenue in occupational therapy (OT) services, enabling independence at home by providing person-centered intervention (AOTA Position Paper, 2018).
Given the rapid growth of the aging population, the global burden of chronic illnesses, disabilities, and loss of functional independence of elders is increasing. It is predicted that this strain will continue to expand exponentially worldwide in the decades to come (Bleibler et al., 2013). Therefore, novel rehabilitation strategies and care management to optimize function and reduce disability for elders coping with chronic health conditions are urgently needed (O’Mara et al., 2017). A major advantage of telerehabilitation is service accessibility, allowing elders to be treated in their homes instead of requiring them to travel to a clinic (Cottrell et al., 2019; Shaw et al., 2019). Studies have demonstrated the potential of home-based telerehabilitation to successfully deliver OT services for older adults with a variety of health conditions (Bedra & Finkelstein, 2015; Hung & Fong, 2019; Llorens et al., 2015).
Currently, the vast majority of telerehabilitation services use impairment level (bottom-up) approaches which aim to improve body functions such as balance and hand function (Benvenuti et al., 2014; Kizony et al., 2014). Nevertheless, models of rehabilitation service delivery need to expand to a chronic disease management model that incorporates outcomes that are meaningful to clients using occupation-based (top-down) approaches (Beit-Yosef et al., 2019; Woolf et al., 2015). In the occupation-based approach, occupational therapists help clients identify their meaningful occupations based on their occupational needs. Performance analysis is conducted by observing the identified occupations, followed by setting realistic and occupation-focused goals (Ishikawa et al., 2021). In particular, healthcare providers should be aware of the necessity for individualized, holistic, long-term, and cost-effective post-hospitalization intervention programs to prevent functional decline and encourage community reintegration (Gilboa et al., 2019; Saywell & Taylor, 2015).
In Israel, some initiatives have begun to establish feasibility and effectiveness as a basis of clinical use of technologies for delivering telerehabilitation services for the geriatric population (Beit-Yosef et al., 2019; Gilboa et al., 2019). Moreover, the Israeli Ministry of Health has recently published (May 2019) service standards for remote delivery of medical services (MOH, 2019). However, successful clinical implementation and adoption of telehealth before the COVID-19 pandemic had been slow with many challenges noted in its delivery (Nibbelink, 2019; Shulver et al., 2017). Currently, telemedicine is not pervasive in the continuum of rehabilitation care (Langan et al., 2017).
The success of organizational innovations becoming part of existing and new clinical routines relies on clinician acceptability, adoption, and sustained compliance (Kairy et al., 2014; Serwe, 2018). Even though there is increased use of information and communication technology in society at large and within health care and rehabilitation, knowledge of the perceived barriers and provider’s concerns in implementing person-centered telerehabilitation is sparse and needs further exploration. Moreover, health professionals in general tend to view telehealth less positively and have more concerns than the clients. (Barber et al., 2019; Damhus et al., 2018; Serwe, 2018).
The present study was performed as part of a larger project aimed to develop an occupation-based telerehabilitation program focusing on the continuity of rehabilitative care post-hospitalization. This current study is a step toward elucidating the factors that will enable successful implementation of the intervention as an effective and secure method within the entire rehabilitation process for the geriatric population. The aim of this study was to explore Israeli occupational therapists’ attitudes regarding the feasibility of an occupation-based telerehabilitation service in geriatric rehabilitation. Specifically, we aimed to identify and conceptualize the perceived factors that could potentially help or hinder the implementation of such a service to older adults with chronic health conditions.
Materials and methods
Study design
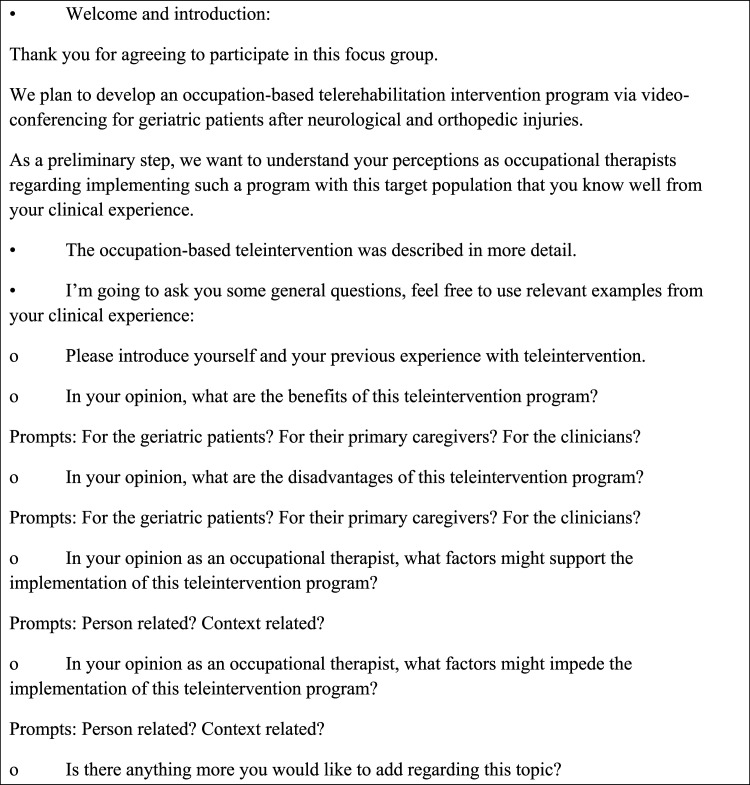
Given the explorative nature of the research aim, we considered a mixed-methods approach to be the most appropriate. Triangulation was incorporated by using more than one source of data—an experiential focus group, an open-ended questionnaire, and Likert scale items to ensure validity and credibility of the data (Portney & Watkins, 2009). Data collection was conducted through directed theory-based content analysis (Hsieh & Shannon, 2005). We selected an experiential focus group design because of its focus on a very homogenous population with shared experiences, and because perspectives are more likely to be revealed by interaction and discussion with peers (Fern, 2001). A semi-structured interview guide (see Figure 1) and a questionnaire were developed for this study on the basis of an extensive literature review, the clinical and educational experiences with telerehabilitation of all the investigators, and feedback from local university faculty. We have detailed the methods used in this study by applying the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist (Tong et al., 2007).
Figure 1.
Topic guide for occupational therapist focus groups.
Recruitment and inclusion
The study was performed at a central hospital in Jerusalem, Israel. The rehabilitation department at the hospital provides inpatient and outpatient multidisciplinary neurological and orthopedic care. A convenience sampling method was used for recruitment. Participants were recruited based on the following criteria: 1. certified occupational therapist and 2. at least 1 year of working experience in rehabilitation wards (inpatient or outpatient) with geriatric patients after neurological or orthopedic injuries. All occupational therapists who worked at the rehabilitation department and met the inclusion criteria were invited in person by the third author (FK) to participate. Potential participants were aware that the study was part of the thesis research project of the third author, who is also an employee at the hospital.
Data collection
Data was collected in two steps. We organized two focus groups with five participants in each group, to ensure that all participants would have time to adequately express their opinions. The focus group meetings took place in a private room at the rehabilitation center lasting between 55 and 64 minutes and were audio-recorded. The five participants and the moderator, who was well-acquainted with the participants, were present in the room. The moderator was a female occupational therapist (third author) who worked at the rehabilitation department in the Hadassah Medical Center and is also a trained qualitative interviewer. The moderator contributed with questions, made sure all participants were involved in the discussion, and managed the tape-recorder and time.
First, each group was presented with a brief background about telerehabilitation and the occupation-based intervention protocol. The protocol includes 10 synchronized videoconferencing sessions led by an occupational therapist aimed at promoting daily function among older adults post inpatient rehabilitation. During the remote intervention, the occupational therapist guides the patient to achieve their self-identified functional goals using a problem-solving strategy (see full description of the protocol at Gilboa et al., 2019). After the protocol was presented, participants were asked to give their professional opinion on the feasibility of conducting the protocol through telerehabilitation for the target population. Specifically, they were asked to address issues including the hypothesized acceptability of telerehabilitation among occupational therapists, patients, and caregivers and the therapeutic approach in the context of long-term geriatric rehabilitation.
At the end of the focus group meetings, each participant was invited to complete a questionnaire. The questionnaire included demographic data and the same five open-ended questions used during the focus group meetings regarding advantages and disadvantages of the teleintervention program and factors that can enable or impede successful implementation of the protocol. In addition, the occupational therapists were asked to state their level of agreement on a 5-point Likert scale (from 1-totally disagree to 5-totally agree) regarding seven statements about the acceptability and feasibility of the suggested teleintervention. The questionnaires allowed us to confirm how much certain topics that were discussed in the group setting were of actual concern to all participants and enabled participants who were not highly orally communicative to share their views. Moreover, the open-ended questions allowed the participants to communicate additional concerns, suggestions, and comments confidentially. (Carter et al., 2014).
Data analysis
Data analysis consisted of mixed methods analysis to integrate qualitative and quantitative data at two stages. Descriptive statistics were used to describe the participants’ characteristics and the questionnaire results. In addition, a qualitative method was used to analyze the data from the focus groups and open-ended questionnaires. The focus group discussions were audio-recorded and transcribed. Analysis was performed first individually by two researchers (third and last authors) and then together through a series of meetings. Authors kept an audit trail to track the data analysis process. The individual analysis process occurred through reading and rereading transcripts and then making notes of conceptual, descriptive, and linguistic comments in relation to parts of the data. During coding of the meeting transcripts and the written questionnaire answers, several codes were assigned to the a priori (Hsieh & Shannon, 2005) defined four thematic categories: advantages, disadvantages, enabling factors, and inhibitory factors. Subsequently, codes were grouped into subthemes. In addition, representative quotes were extracted. In the joint meetings, investigators reread the data multiple times and discussed discrepancies until consensus was achieved, to strengthen the trustworthiness of the data. This was an iterative process that incorporated both inductive and deductive approaches, (Creswell et al., 2011) until it was finalized. Finally, we reported the qualitative themes and quotes followed by the quantitative results, highlighting ways in which they confirm the qualitative findings.
Results
Out of the 30 occupational therapists who worked at the hospital, twelve worked at the rehabilitation department and met the inclusion criteria and ten of them were recruited for this study. One occupational therapist declined to participate due to personal circumstances and one agreed to participate but could not attend the focus group meeting. All participants were licensed female occupational therapists (mean age: 29.6 ± 3.78; years of seniority: 4.6 ± 4.14) working in the inpatient (n = 5) and outpatient (n = 5) rehabilitation departments and were inexperienced with telerehabilitation.
A qualitative analysis of the main themes was conducted based on the written transcriptions of the focus groups’ discussions and the written answers from the open-ended questionnaire questions that dealt with the feasibility of the occupation-based telerehabilitation program. The data was organized according to the four major themes focusing on the advantages and disadvantages of the occupation-based telerehabilitation program as well as factors that can support or impede the implementation of the telerehabilitation protocol. The themes sometimes overlapped, but by articulating them specifically they constituted distinct ways of relating to the occupation-based telerehabilitation program for the geriatric population.
Advantages of occupation-based telerehabilitation
Subtheme A1. Application and transfer of rehabilitation achievements to the natural environment (home): The most consistent finding, which was agreed upon by all occupational therapists, is that conducting therapy in the client’s natural environment is a great advantage. It allows for the setting of more accurate goals and more precise treatment plans for achieving those goals. A participant stated: “The main advantage as I see it, is the ability to apply (rehabilitation) in the natural environment, that is dynamic and constantly changing, as opposed to practicing in a protected and modified environment of the rehabilitation department.”
Other occupational therapists who work at the inpatient ward claimed that the treatment continuation using telerehabilitation can support the patient’s discharge from the hospital and ease the adjustment back home: “I think there’s something about it that can make the return home more gradual, it will probably reduce anxiety and make the patients feel they are not alone.”
Occupational therapists suggested that the service can also be used for counseling and giving guidance to the patient and/or the caregiver regarding adaptation and organization of the home environment, using assistive devices if needed and practicing functional tasks. One occupational therapist stated, for example: “Another advantage is that we can see them doing (the tasks) in their very own kitchen and we can provide on-line synchronic guidance”. Another occupational therapist added: “Giving guidance is very important and effective; We can teach patients about energy conservation techniques and safety rules by watching on-line presentations together or sending them pictures of different assistive devices.” In addition, other occupational therapists noted that telerehabilitation allows the therapist to see the actual home environment. That way the therapist can recommend more adequate home modifications and make sure they are implemented, allowing the patient maximum independence: “The possibility of seeing the patient’s natural environment is an advantage. When they are here (hospitalized) we can’t see their homes… using telerehabilitation can allow us to see the patient’s bathroom, the size and angles there, instead of standing here struggling to explain to us how the toilet in their house is set up.”
Subtheme A2. Saving time and overcoming geographical distance: The participants agreed that telerehabilitation makes rehabilitation treatment more accessible to anyone who can’t come continuously to rehabilitation facilities for a variety of reasons, including lack of rehabilitation services in their residential area, mobility difficulties and more. An occupational therapist who works at the outpatient ward said: “(Telerehabilitation is) suitable for patients who live in areas that do not have occupational therapy services or patients who cannot leave the house... for my patient who lives in the Jordan Valley (a rural area in Israel), this would be a great option.”
Factors that can enable occupation-based telerehabilitation
Subtheme B1. Patients’ motivation: Some of the occupational therapists claimed that telerehabilitation is suitable for highly motivated patients who are actively involved in the intervention process. One of the occupational therapists described which patients can most likely benefit from occupation-based telerehabilitation: “…clients with will power and inner drive... who can understand the goals of the intervention and have personal goals they are interested in achieving.”
Subtheme B2. Collaboration with the patient’s caregiver: Approximately half of the occupational therapists thought cooperation with the main caregiver is crucial for successful occupation-based telerehabilitation treatment. This is due to the nature of the proposed intervention which may be demanding for the caregiver who is sometimes asked to be present during sessions to oversee continued implementation of the guidelines between sessions. One of the occupational therapists described: “(the caregivers) need to offer the optimal amount of help…. but also, not doing things instead of them (the patients). This is not an easy job….” The occupational therapists emphasized that the telerehabilitation protocol might add to the caregiver burden during the period of intervention. However, if therapeutic goals are achieved in the long run, this might help to reduce it, resulting in physical relief and greater quality of life: “I’m assuming that if the main caregivers know that thanks to their current effort, things will get easier over time, they will be more motivated.”
Subtheme B3. Creating initial therapeutic relationships: Some occupational therapists felt it would be important to first meet the client face to face and establish a relationship and create a sense of commitment. “I think there should be a face to face meeting which would encourage a trustful relationship. And only then begin telerehabilitation.”
Disadvantages of occupation-based telerehabilitation
Subtheme C1. No hands-on contact: The main disadvantage that was mentioned in both focus groups was the inability to use physical mediation and manual therapy if needed: “I think a clear disadvantage is the inability to do hands-on therapy and touch the patient.” Another disadvantage an occupational therapist mentioned was that it wouldn’t be appropriate to assign any kind of exercise through telerehabilitation: “Some exercises require more knowledge of anatomy, I might tell a caregiver not to lift the patient’s arm above 90 degrees, but I might do it myself, because I know how to do it right.”
Subtheme C2. Safety: Occupational therapists expressed concerns regarding safety issues due to the physical and cognitive status of the patient as well as the caregiver’s ability to keep the client safe. They claimed it would be unsafe for clients to perform some of the functional activities in their homes without the presence of a certified therapist. They felt that even when a main caregiver is present, the client’s safety could be at risk. One occupational therapist describes it: “You’re not really there to keep him safe. If the patient does a wrong movement it might not be enough to shout ‘be careful’ through the video.” Another occupational therapist added: “This might limit the ability to practice functional activities, I might prefer to keep my patient sitting to ensure her safety.” Another occupational therapist mentioned that sometimes we have to rely on the caregivers to ensure the patients safety: “A (remote) rehabilitation process can demand a lot from the main caregiver…. We need to trust the caregiver that is next to them, but we don’t know how professional the caregiver is.”
Factors that can inhibit occupation-based telerehabilitation
Subtheme D1. Technological challenges: Many occupational therapists claimed that the lack of knowledge about technology often observed in seniors might impede the implementation of the telerehabilitation protocol. Problems such as operating the computer, positioning the camera, and lack of infrastructure for the technology were brought up. An occupational therapist described: “Some clients never used a computer, even though (I think) the iPad is very easy to use, it might not be for everyone.” It was also mentioned that using a camera limits observing the client fully: “It is limiting that I can only see the client straight ahead of me. Sometimes clients compensate in a certain movement by using a different body part which I won’t see.”
Subtheme D2. Patients’ cognitive status: Impaired cognitive status was mentioned multiple times as a perceived inhibiting factor. All occupational therapists agreed that a broad cognitive screening would help identify patients that may benefit from this telerehabilitation protocol. One occupational therapist said: “Using only a screening cognitive assessment is not enough; we need to know more about the clients’ awareness, judgment and impulsivity before carrying out telerehabilitation.” Another therapist spoke about dangers that might occur due to cognitive decline: “I would be nervous working with a patient who is highly impulsive or has cognitive decline using telerehabilitation. He might succeed in doing a task, like making an omelet, during a session with me and his caregiver, but not realize the danger (of fire).”
Quantitative findings of the occupational therapists’ attitude questionnaire are presented in Table 1. Results of the questionnaire have been contracted from a 5-point Likert scale to three basic categories of “disagree,” “unsure,” and “agree” regarding the use of the telerehabilitation program for patients after a neurological or an orthopedic injury. The findings showed that 70% of the occupational therapists agreed that the occupation-based telerehabilitation protocol is suitable for promoting functional goals. Half of them thought that this protocol can promote participation in meaningful activities in the community and quality of life (QoL). There were different opinions as to whether the use of this telerehabilitation protocol has the potential to reduce caregiver burden and is suitable for implementation in Israel. Most occupational therapists were unsure if patients would be interested in participating and willing to comply with this occupation-based telerehabilitation program.
Table 1.
Distribution of the results on the occupational therapists’ attitude questionnaire regarding occupation-based telerehabilitation (n = 10).
| Disagree (%) | Unsure (%) | Agree (%) | |
|---|---|---|---|
| Telerehabilitation is suitable for promoting functional goals of older adult patients | 20 | 10 | 70 |
| Telerehabilitation is suitable for promoting participation in meaningful activities in the community | 20 | 30 | 50 |
| Telerehabilitation is suitable for promoting quality of life of older adult patients | 20 | 30 | 50 |
| Telerehabilitation may reduce caregiver burden | 30 | 40 | 30 |
| Telerehabilitation is a suitable mean for receiving therapy for patients in Israel | 20 | 40 | 40 |
| Patients will be interested in receiving telerehabilitation | 0 | 70 | 30 |
| Patients will comply with the telerehabilitation program | 20 | 70 | 10 |
Discussion
This study explored the perspectives of occupational therapists in Israel on benefits and barriers of providing a remote occupation-based rehabilitation service for older adults with chronic health conditions. This study was performed before the COVID-19 pandemic; nevertheless, its results might be useful for the current rapidly reshaping of the entire organization of rehabilitation services to support successful implementation of occupation-based teleinterventions for older adults in Israel. At the same time, it highlights the need to incorporate clinicians’ perspectives into the design and delivery of such programs, so as to overcome barriers to implementation in real world settings.
In the current study, the occupational therapists described the potential of occupation-based telerehabilitation to deliver inexpensive home-based intervention, encouraging the transfer and maintenance of the rehabilitation achievements to the home context. This two-way visual interaction would allow therapists to see their patients in their natural environment and thus enable more precise and personal care in addition to reducing costs and travelling time. Previous researchers (Dew et al., 2013; Gardner et al., 2016) also have identified the benefit of telerehabilitation in allowing therapists to see where clients carry out their occupations and of eliminating the need to travel.
Occupation-based telerehabilitation intervention, which utilizes patient and caregiver coaching, requires the therapist to feel comfortable using different therapeutic modes, such as demonstrating and instructing. (Gardner et al., 2016) In order to deliver successful telerehabilitation, the therapist must feel competent using mainly verbal communication and some physical gestures that can be seen through the camera. This is quite different from using the traditional therapeutic model of hands-on manual therapy. Therefore, the occupational therapists were convinced that not all interventions could be carried out remotely, not all therapists could conduct a successful session, and not all patients would comply with treatment. As expected, (Ashburner et al., 2016; Gardner et al., 2016) all agreed that remote technology should augment rather than replace face-to-face contact.
Our findings reinforce the current literature as we identified perceived barriers and enablers that previously have been reported in the context of telecare. Based on the current results, a remotely delivered occupation-based rehabilitation intervention for a geriatric population in the chronic phase of neurological and orthopedic injuries must take several unique factors into account when being implemented into the integrated care networks. They must be exceedingly safe, be based on the patients’ and caregivers’ motivation and collaboration, include at least initial personal contact, be as free as possible from any technological challenges, and consider the patients’ prior technological experience. Our findings are consistent with a recent study that reported that some clinicians perceived the lack of patient experience or confidence with technology or older age as a potential barrier to use (Morse et al., 2020) and therefore might be hesitant to introduce telerehabilitation into their practice with older patients. However, previous research demonstrated that older people with limited experience of technology can be taught to successfully use telehealth equipment (Nancarrow et al., 2016).
The findings from the current study can be used as initial guidelines (Jacobs et al., 2015) for clinical reasoning to allow appropriate selection of clients and goals for occupation-based telerehabilitation. In addition, this study presents factors that need to be considered in the development of an occupation-based telerehabilitation program. An important conclusion derived from the results of the attitude questionnaires was that the occupational therapists did not have fully formed views about how a large telehealth service would be successfully operated. This suggests that the construction of large-scale telehealth services remains in its very early stages, and its use with this population is not yet part of the general consensus among clinicians (Wade et al., 2016) in Israel. In line with previous literature (Kairy et al., 2014), findings from this study suggest that routine use of telerehabilitation is more likely to be successfully integrated in services that were already part of rehabilitation routine practice (in this case, occupational therapy guidance for patients and caregivers).
A main avenue of promoting the use of occupation-based telerehabilitation should be working to change therapists’ views by more directly addressing their concerns. One way to do that would be to construct the guidelines with clear references to issues clinicians have with the use of occupation-based telerehabilitation. For example, they need to be made aware of how their perceptions might be limiting their willingness to try tools that could be quite successful. The guidelines should also clarify ways to enhance successful implementation, such as how to encourage collaboration with the patient’s caregiver. Highlighting these points in the guidelines could help overcome the hesitations of clinicians inexperienced in telerehabilitation.
This study has several limitations. One limitation of this study is that all ten occupational therapists were working together in a rehabilitation ward in Hadassah Medical center. Although having a homogeneous group of participants in an experiential focus group is recommended by qualitative researchers (Curtis & Redmond, 2007), this implies that the generalizability of the study results is limited. Hadassah medical center is located in Jerusalem and is one of the largest hospitals in Israel; however, it might be that occupational therapists working in more rural areas in Israel would have different perspectives regarding telerehabilitation. At the same time, understanding these specific views is important in order to recognize barriers that need to be addressed in the planning of these services. In addition, focus group discussions as a method, could be biased if all participants could not actively take part in discussions due to intimidation or influence by dominant or aggressive participants. It should be noted that member checking was not performed after data analysis which reduces the reliability of the themes generated in the study. Lastly, the participants in the focus groups only heard a description of the teleintervention, but due to ethical considerations they could not observe a real therapy session. Future studies should include a larger and more heterogeneous OT sample in addition to patients and caregivers, which might shed more light on the facilitating and inhibiting factors. Additionally, it would be highly interesting to assess the changes in occupational therapists’ perspectives about occupational-based telerehabilitation following their COVID-19 period experiences.
Conclusions
During the COVID-19 pandemic, telerehabilitation unveiled itself as a promising method of care to be adopted alternatively, or in combination with face-to-face usual care for older adults. Occupational therapists, researchers, and health stakeholders are called to action to discover when and how telerehabilitation can be a useful tool for the geriatric population beyond the COVID-19 pandemic period. Future efforts must focus on achieving clinicians’ acceptance (Wade et al., 2016) of occupation-based telerehabilitation through providing appropriate evidence-based therapeutic protocols. Findings from this study can potentially contribute to facilitating a home-based telerehabilitation service as a practical alternative for older adult patients with chronic health conditions after discharge from rehabilitation units in Israel.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author’s Note: The data that support the findings of this study are available on request from the corresponding author.
ORCID iD: Yafit Gilboa https://orcid.org/0000-0002-0734-3626
References
- AOTA Position Paper . (2018). Telehealth in Occupational Therapy. The American Journal of Occupational Therapy,, 72(Suppl 2), 1–18. 10.5014/ajot.2018.72S219 [DOI] [Google Scholar]
- Ashburner J., Vickerstaff S., Beetge J., Copley J. (2016). Remote versus face-to-face delivery of early intervention programs for children with autism spectrum disorders: Perceptions of rural families and service providers. Research in Autism Spectrum Disorders, 23, 1–14. 10.1016/j.rasd.2015.11.011 [DOI] [Google Scholar]
- Barber T., Sharif B., Teare S., Miller J., Shewchuk B., Green L. A., Marlett N., Cibere J., Mrklas K., Wasylak T. (2019). Qualitative study to elicit patients’ and primary care physicians’ perspectives on the use of a self-management mobile health application for knee osteoarthritis. BMJ Open, 9(1), e024016. 10.1136/bmjopen-2018-024016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedra M., Finkelstein J. (2015). Feasibility of post-acute hip fracture telerehabilitation in older adults. European Federation for Medical Informatics (EFMI). [PubMed] [Google Scholar]
- Beit-Yosef A., Jacobs J. M., Shenkar S., Shames J., Schwartz I., Doryon Y., Naveh Y., Khalailh F., Berrous S., Gilboa Y. (2019). Activity performance, participation, and quality of life among adults in the chronic stage after acquired brain injury—the feasibility of an occupation-based telerehabilitation intervention. Frontiers in Neurology, 10, 1247. 10.3389/fneur.2019.01247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benvenuti F., Stuart M., Cappena V., Gabella S., Corsi S., Taviani A., Albino A., Scattareggia Marchese S., Weinrich M. (2014, Sep). Community-based exercise for upper limb paresis: a controlled trial with telerehabilitation. Neurorehabilitation & Neural Repair 28(7), 611–620. 10.1177/1545968314521003 [DOI] [PubMed] [Google Scholar]
- Bleibler F., Konnopka A., Benzinger P., Rapp K., König H.-H. (2013). The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany—a demographic simulation model. Osteoporosis International, 24(3), 835–847. 10.1007/s00198-012-2020-z [DOI] [PubMed] [Google Scholar]
- Carter N., Bryant-Lukosius D., DiCenso A., Blythe J., Neville A. J. (2014, Sep). The use of triangulation in qualitative research. Oncology Nursing Forum, 41(5), 545–547. 10.1188/14.onf.545-547 [DOI] [PubMed] [Google Scholar]
- Chumbler N. R., Rose D. K., Griffiths P., Quigley P., McGee-Hernandez N., Carlson K. A., Vandenberg P., Morey M. C., Sanford J., Hoenig H. (2010). Study protocol: home-based telehealth stroke care: A randomized trial for veterans. Trials, 11, 74. 10.1186/1745-6215-11-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottrell M. A., O’Leary S. P., Raymer M., Hill A. J., Comans T., Russell T. G. (2019). Does telerehabilitation result in inferior clinical outcomes compared with in-person care for the management of chronic musculoskeletal spinal conditions in the tertiary hospital setting? A non-randomised pilot clinical trial. Journal of Telemedicine and Telecare. 10.1177/1357633X19887265. [DOI] [PubMed] [Google Scholar]
- Creswell J. W., Klassen A. C., Plano Clark V. L., Smith K. C. (2011). Best practices for mixed methods research in the health sciences (pp. 541–545). National Institutes of Health, 2013. [Google Scholar]
- Curtis E., Redmond R. (2007). Focus groups in nursing research. Nurse Researcher, 14(2), 25–37. 10.7748/nr2007.01.14.2.25.c6019 [DOI] [PubMed] [Google Scholar]
- Damhus C. S., Emme C., Hansen H. (2018). Barriers and enablers of COPD telerehabilitation–a frontline staff perspective. International Journal of Chronic Obstructive Pulmonary Disease, 13, 2473–2482. 10.2147/COPD.S167501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dew A., Bulkeley K., Veitch C., Bundy A., Gallego G., Lincoln M., Brentnall J., Griffiths S. (2013, Aug). Addressing the barriers to accessing therapy services in rural and remote areas. Disability and Rehabilitation, 35(18), 1564–1570. 10.3109/09638288.2012.720346 [DOI] [PubMed] [Google Scholar]
- Fern E. F. (2001). Advanced focus group research. Sage Publishing. [Google Scholar]
- Fong K. N. K., Kwan R. (2020). Telerehabilitation (remote therapy). In Gu D., Dupre M. E. (Eds.), Encyclopedia of gerontology and population aging (pp. 1–7). Springer International Publishing. 10.1007/978-3-319-69892-2_1088-1 [DOI] [Google Scholar]
- Gardner K., Bundy A., Dew A. (2016). Perspectives of rural carers on benefits and barriers of receiving occupational therapy via information and communication technologies. Australian Occupational Therapy Journal, 63(2), 117–122. 10.1111/1440-1630.12256 [DOI] [PubMed] [Google Scholar]
- Gilboa Y., Maeir T., Karni S., Eisenberg M. E., Liebergall M., Schwartz I., Kaufman Y. (2019, May 20). Effectiveness of a tele-rehabilitation intervention to improve performance and reduce morbidity for people post hip fracture - study protocol for a randomized controlled trial. BMC Geriatrics, 19(1), 135. 10.1186/s12877-019-1141-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- G. K. N., & Fong, K. N. K (2019, June). Effects of telerehabilitation in occupational therapy practice: A systematic review. Hong Kong Journal of Occupational Therapy, 32(1), 3–21. 10.1177/1569186119849119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H.-F., Shannon S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Ishikawa T., Tomori K., Nagayama H., Okita Y. (2021). The occupational experience helps to express the clients’ occupational needs in goal setting: A retrospective study in subacute care setting. Occupational Therapy in Health Care. 10.1080/07380577.2021.2003498 [DOI] [PubMed] [Google Scholar]
- Jacobs K., Cason J., McCullough A. (2015). The process for the formulation of the international telehealth position statement for occupational therapy. International Journal of Telerehabilitation, 7(1), 21–32. 10.5195/ijt.2015.6163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kairy D., Lehoux P., Vincent C. (2014, May-Jun). Exploring routine use of telemedicine through a case study in rehabilitation. La Revista Panamericana de Salud Pública, 35(5–6), 337–344. [PubMed] [Google Scholar]
- Kizony R., Weiss P. L., Elion O., Harel S., Baum-Cohen I., Krasovsky T., Feldman Y., Shani M. (2014). Development and validation of tele-health system for stroke rehabilitation. International Journal on Disability and Human Development, 13(3), 361–368. 10.1515/ijdhd-2014-0329 [DOI] [Google Scholar]
- Langan J., Subryan H., Nwogu I., Cavuoto L. (2017). Reported use of technology in stroke rehabilitation by physical and occupational therapists. Disability and Rehabilitation: Assistive Technology, 10.1080/17483107.2017.1362043 [DOI] [PubMed] [Google Scholar]
- Llorens R., Noe E., Colomer C., Alcaniz M. (2015, Mar). Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 96(3), 418–425.e412. 10.1016/j.apmr.2014.10.019 [DOI] [PubMed] [Google Scholar]
- MOH (2019). Standards for Operating Telemedicine Services (In Hebrew). Jerusalem. The Israeli Ministry of Health. 06/2019. https://www.gov.il/he/Departments/policies/mk06-2019
- Morse H., Biggart L., Pomeroy V., Rossit S. (2020). Virtual reality telerehabilitation for spatial neglect post-stroke: Perspectives from stroke survivors, carers and clinicians. medRxiv. 10.1101/2020.01.07.20016782 [DOI] [PubMed]
- Nancarrow S., Banbury A., Buckley J. (2016). Evaluation of a National Broadband Network-enabled Telehealth trial for older people with chronic disease. Australian Health Review, 40(6), 641–648. 10.1071/AH15201 [DOI] [PubMed] [Google Scholar]
- Nibbelink G. (2019). Improving the implementation of telerehabilitation in rehabilitation centres, University of Twente. [Google Scholar]
- O’Mara A., Rowland J. H., Greenwell T. N., Wiggs C. L., Fleg J., Joseph L., McGowan J., Panagis J. S., Washabaugh C., Peng G. C. Y., Bray R., Cernich A. N., Cruz T. H., Marden S., Michel M. E., Nitkin R., Quatrano L., Spong C. Y., Shekim L., Begg L. (2017, Apr 1). National institutes of health research plan on rehabilitation: NIH medical rehabilitation coordinating committee. Physical Therapy, 97(4), 104–407. 10.1093/ptj/pzx026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portney L. G., Watkins M. P. (2009). Foundations of clinical research: Applications to practice (Vol. 892). Pearson/Prentice Hall Upper. [Google Scholar]
- Saywell N., Taylor D. (2015, Mar). Focus group insights assist trial design for stroke telerehabilitation: a qualitative study. Physiotherapy Theory and Practice, 31(3), 160–165. 10.3109/09593985.2014.982234 [DOI] [PubMed] [Google Scholar]
- Serwe K. M. (2018). The provider’s experience of delivering an education-based wellness program via telehealth. International Journal of Telerehabilitation, 10(2), 73–80. 10.5195/IJT.2018.6268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw M. T., Best P., Frontario A., Charvet L. E. (2019). Telerehabilitation benefits patients with multiple sclerosis in an urban setting. Journal of Telemedicine and Telecare. 10.1177/1357633X19861830 [DOI] [PubMed] [Google Scholar]
- Shulver W., Killington M., Morris C., Crotty M. (2017). ‘Well, if the kids can do it, I can do it’: Older rehabilitation patients' experiences of telerehabilitation. Health Expectations, 20(1), 120–129. 10.1111/hex.12443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A., Sainsbury P., Craig J. (2007, Dec).Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Wade V. A., Taylor A. D., Kidd M. R., Carati C. (2016, May 16).Transitioning a home telehealth project into a sustainable, large-scale service: A qualitative study. BMC Health Services Research, 16, 183. 10.1186/s12913-016-1436-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf C., Caute A., Haigh Z., Galliers J., Wilson S., Kessie A., Hirani S., Hegarty B., Marshall J. (2015, Apr 24). A comparison of remote therapy, face to face therapy and an attention control intervention for people with aphasia: A quasi-randomised controlled feasibility study. Clinical Rehabilitation. 10.1177/0269215515582074 [DOI] [PubMed] [Google Scholar]