Abstract
Objectives
Resident physicians are particularly prone to sleep disturbance due to long shift hours and excessive workload. Despite the numerous measures undertaken to improve their wellbeing, it is still unknown if limiting the work shift duration would improve sleep quality. We sought to compare sleep quality, anxiety, and depression before and after implementing duty hour limits. We also aim to evaluate how satisfaction with life is related to sleep quality, anxiety, and depression.
Methods
We used a self-reported questionnaire to obtain data about sleep quality, anxiety, and depression using the Pittsburgh Sleep Quality Index and Patient Health Questionnaire-4 (PHQ-4) scales, respectively. Using data from a previous study, we compared those parameters before and after implementing duty hour reduction across several specialties at King Abdullah University Hospital, Jordan. Furthermore, we investigated residents’ life satisfaction using the Satisfaction with Life Scale.
Results
One hundred and eighty residents filled the questionnaire (median age = 26.5 years). Males reported higher rates of poor sleep quality while females had higher rates of anxiety and depression. Decreasing the duration of on-call shifts from 32 to 24 hours decreased the prevalence of poor sleep quality from 91.5% to 83.2% (p = 0.038), and smoking rates decreased from 30.4% to 12.5% (p < 0.001). More than six on-calls per month were associated with poorer quality of sleep. Night float shifts significantly decreased rates of moderate and severe PHQ-4 scores (p < 0.001). In addition, 63.3% of residents were satisfied with life. Life satisfaction was associated with enhanced sleep quality and lower PHQ-4 scores (p = 0.007 and p < 0.001, respectively).
Conclusions
Optimizing shift scheduling and duration can positively influence rates of sleep quality, anxiety, depression, and smoking. More interventions should be tackled along with duty hour limits to optimize residents’ life satisfaction.
Keywords: Sleep Quality, Internship and Residency, Workload, Physicians, Work Schedule Tolerance
Introduction
Maintaining optimal sleep quality, duration, timing, and regularity is a biological imperative.1 The American Academy of Sleep Medicine and Sleep Research Society recommends that adults sleep seven hours or more per night to avoid adverse health outcomes such as depression, increased risk of death, impaired performance, and increased errors and accidents.2-4 Resident physicians are particularly vulnerable to sleep deprivation owing to long working hours, frequent on-call shifts, and the demanding nature of their education. Sleep deprivation negatively affects learning, memory consolidation, cognitive performance, physical and psychological wellbeing, and personal life, and residents are no exception to this.5-7 One in three residents has reported poor sleep quality in previous studies.8,9 One study reported a 28.8% prevalence of depression among resident physicians.10 Depressed residents tend to make more medical errors than their non-depressed peers.11 In Jordan, we previously found that around 90% of residents had poor sleep quality, which marked the highest reported prevalence of poor sleep quality among residents.12 We also found that 21.4% and 18.9% had moderate or severe anxiety and depression, respectively.12
Extended work shift (≥ 24 hours) is a common practice in many regions, although it was demonstrated to threaten the safety of both residents and patients.13-15 A study conducted in intensive care settings showed that the traditional work schedule was associated with a 36% increase in serious medical errors and a 5.6-times increase in serious diagnostic errors compared with a modified schedule with limited working hours.16 Therefore, restricting work hours has been advocated since 2003 to decrease the adverse effects of traditional schedules.17,18 Working for > 80 hours and 100 hours per week has been associated with a three-fold and seven-fold higher risk of depression, respectively, compared to < 60 working hours per week.19 Currently, the Accreditation Council for Graduate Medical Education (ACGME) limits clinical and educational work hours to no > 80 hours per week and 24 hours of continuous work.20 The Faculty of Medicine at Jordan University of Science and Technology (JUST) has, since October 2019, limited resident working hours following the requirements of ACGME accreditation. Evidence of the impact of work hour limitations on resident and patient outcomes is still limited.17
To the best of our knowledge, the impact of reducing work hours on sleep quality and the prevalence of anxiety and depression among residents has not yet been investigated. Therefore, we compared sleep quality, anxiety, and depression before and after implementing duty hour limits in the same center. We also sought to evaluate how satisfaction with life is related to sleep quality, anxiety, and depression.
Methods
A questionnaire-based cross-sectional study was conducted among resident physicians from different specialties at King Abdullah University Hospital (KAUH), Jordan between September and November 2020. The institutional review board committee at JUST and KAUH approved the study (digital proposal number 212/132/2020). Confidential data and informed consent were secured in locked cabinets and handled with research members only. Participants were given serial numbers before data entry and analysis.
This study targeted resident physicians in the residency program at KAUH who had spent at least six months in residency and signed the informed consent for participation in the study. Residents with diagnosed sleep disorders were excluded. The estimated number of post-graduate physicians enrolled in the residency program at the study time was around 460. We previously evaluated sleep quality among residents in KAUH, which was about 90%. Accordingly, we calculated the minimum required sample size using version 3 of the OpenEpi online calculator, assuming the following parameters: hypothesized prevalence of 90%, margin of error of 0.05, 95% CI, and design effect of 1 for random sampling, and power set for 80%. The calculated sample size was 107 physicians. Our final sample size was 180. The study participants were randomly selected using the hospital’s resident record. Residents were then contacted to check for their eligibility and signed the informed consent. The response rate was 98.9%.
Residency programs in KAUH consist of four to six training years, while the number of on-calls depends on specialty and the residency level. Until October 2020, an on-call shift lasted a continuous 32 hours. Then, 24-hour shift limits were applied across all departments, except neurosurgery which opted not to implement any changes, and internal medicine, which applied night float shifts from 10 pm to 8 am (including some day shifts from 4 pm to 10 pm). Pathology and dermatology have no on-call shifts except for postgraduate year (PGY) 1 dermatology residents. Nonetheless, they were involved in this study as a reference to test associations. Residents with no on-calls were excluded from analysis when studying the effects of duty hour limits.
We used a self-reported English questionnaire to collect data on demographics (age, gender), specialty, PGY level (i.e., year of residency), number of on-call shifts per month, smoking status (smoker, never smoked, ex-smoker), sleep quality, anxiety and depression, and satisfaction with life.
We compared our previous data on sleep quality and anxiety and depression, which was collected in early 2019 before the implementation of duty hour limits, with this study’s new data. Two new work schedules have been implemented at KAUH since October 2019. The first includes a 24-hour limit on the on-call shift, while the other involves rotating night floating shifts (working 12 hours daily for one week every two months, with otherwise normal eight-hour work schedules and intermittent six-hour on-calls from the end of a normal workday until 10 pm).
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI), which measures seven domains: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping pills, and daytime dysfunction over the past month. Poor sleep quality was determined by a cutoff PSQI score of at least 5. Higher scores implied worse sleep quality.21
We utilized the four-item Patient Health Questionnaire for anxiety and depression (PHQ-4), a brief, valid tool to assess the prevalence of anxiety and depression among residents. The scale comprises four questions, each with four possible answers corresponding to specific points. The total score is calculated by adding the scores of individual items. Subsequently, scores are rated as normal (0–2), mild (3–5), moderate (6–8), and severe (9–12). A total score ≥ 3 for the first two items suggests anxiety, whereas the same score for the last two implies depression.22
The Satisfaction with Life Scale (SWLS) was implemented to measure life satisfaction among resident physicians. It incorporates five items, each with a possible seven-point Likert style response scale. The range of scores is between 5–35 (20 is the neutral point). Scores between 5–9 indicate extreme dissatisfaction with life, whereas scores between 31–35 indicate extreme satisfaction.23
Data were presented as frequencies and proportions (%) for categorical variables and as median (interquartile range (IQR)) for continuous data (age and SWLS). Univariate and multivariate analyses of the associations between sleep quality (poor, adequate) or PHQ-4 stages (normal, mild, moderate, severe) with several factors were implemented using binary logistic regression and ordinal logistic regression, respectively.
A Kruskal-Wallis test was done, followed by Dunn’s pairwise tests for multiple comparisons to analyze predictors of SWLS. Two proportions Z-test and chi-square test were used to compare sleep quality and PHQ-4 scores before and after working hours limitations, respectively. Statistical significance was established at p < 0.05. Statistical analysis was performed using SPSS (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.).
Results
A total of 180 resident physicians from different specialties completed the survey. The median age (IQR) was 26.5 (25–28) years, and females constituted 52.2% of the sample. Table 1 lists the personal characteristics of the study sample.
Table 1. Characteristics of study subjects (N = 180).
| Characteristics | n (%) |
|---|---|
| Age, median (IQR) | 26.5 (25–28) |
| Gender | |
| Male | 86 (47.8) |
| Female | 94 (52.2) |
| Number of on-calls/month | |
| 0 | 21 (11.7) |
| 1–2 | 4 (2.2) |
| 3–4 | 19 (10.6) |
| 5–6 | 48 (26.7) |
| > 6 | 88 (48.9) |
| Residency level | |
| R1 | 53 (29.4) |
| R2 | 47 (26.1) |
| R3 | 33 (18.3) |
| R4 | 33 (18.3) |
| R5 | 14 (7.8) |
| Smoking status | |
| Never smoked | 138 (76.7) |
| Smoker | 29 (16.1) |
| Ex-smoker | 13 (7.2) |
| Sleep quality (PSQI) | |
| Adequate | 31 (17.2) |
| Poor | 149 (82.8) |
| PHQ-4 | |
| Normal | 49 (27.2) |
| Mild | 54 (30.0) |
| Moderate | 46 (25.6) |
| Severe | 31 (17.2) |
| SWLS | |
| Extremely satisfied | 48 (26.7) |
| Satisfied | 35 (19.4) |
| Slightly satisfied | 31 (17.2) |
| Neutral | 6 (3.3) |
| Slightly dissatisfied | 28 (15.6) |
| Dissatisfied | 22 (12.2) |
| Extremely dissatisfied | 10 (5.6) |
IQR: interquartile range; R: residency year; PSQI: Pittsburgh Sleep Quality Index; PHQ-4: four-item Patient Health Questionnaire for anxiety and depression; SWLS: Satisfaction with Life Scale.
Poor sleep quality was prevalent in 82.8% of resident physicians. After multivariable regression, male gender and having more than six monthly on-call shifts were significantly associated with poor sleep quality (p = 0.001, OR = 9.4, 95% CI: 2.5–35.4 and p = 0.003, OR = 10.4, 95% CI: 2.2–48.7, respectively). On the other hand, the SWLS score was negatively associated with poor sleep quality (p = 0.007, OR = 0.9, 95% CI: 0.8–0.9) [Table 2]. Fifth-year residents showed lesser odds for poor sleep quality, although this finding did not reach statistical significance (p = 0.07, OR = 0.2, 95% CI: 0.02–1.2).
Table 2. Univariate and multivariate binary logistic regression analyses of predictors for sleep quality, N = 180.
| Factors | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| p-value | OR | 95% CI | p-value | OR | 95% CI | |
| Gender | ||||||
| Female | ref | ref | ref | ref | ref | ref |
| Male | 0.001* | 4.8 | 1.9–12.5 | 0.001* | 9.4 | 2.5–35.4 |
| PHQ-4 | ||||||
| Normal | ref | ref | ref | ref | ref | ref |
| Mild | 0.8 | 1.1 | 0.5-2.8 | 0.85 | 1.1 | 0.3–4.3 |
| Moderate | 0.03* | 3.8 | 1.1–12.7 | 0.82 | 1.3 | 0.1–18.2 |
| Severe | 0.026* | 10.8 | 1.3–87.7 | 0.44 | 4.9 | 0.1–278.6 |
| PHQ-4 | ||||||
| Anxiety | 0.001* | 5.7 | 2–15.7 | 0.18 | 3.5 | 0.6–22.8 |
| Depression | 0.003* | 4.6 | 1.7–12.6 | 0.98 | 0.98 | 0.1–6.9 |
| SWLS | < 0.001* | 0.8 | 0.8–0.9 | 0.007* | 0.9 | 0.8–0.9 |
| Number of on-calls/month | ||||||
| 0 | ref | ref | ref | ref | ref | ref |
| 1–2 | 0.6 | 1.8 | 0.16–20.9 | 0.16 | 8.4 | 0.4–156.8 |
| 3–4 | 0.2 | 2.3 | 0.6–9.4 | 0.051 | 12.1 | 0.9–148.2 |
| 5–6 | 0.02* | 4.3 | 1.3–14.7 | 0.199 | 3.1 | 0.6–17.2 |
| > 6 | 0.013* | 3.9 | 1.3–11.4 | 0.003* | 10.4 | 2.2–48.7 |
| Residency level | ||||||
| R1 | ref | ref | ref | ref | ref | ref |
| R2 | 0.14 | 2.2 | 0.8–6.4 | 0.49 | 1.7 | 0.4–7.7 |
| R3 | 0.085* | 3.3 | 0.9–12.4 | 0.1 | 4.4 | 0.7–25.6 |
| R4 | 0.042* | 5.0 | 1.0–24.0 | 0.2 | 3.7 | 0.5–28.2 |
| R5 | 0.07 | 0.3 | 0.1–1.1 | 0.07 | 0.2 | 0.02–1.2 |
OR: odds ratio; ref: reference group; PHQ-4: four-item Patient Health Questionnaire for anxiety and depression; SWLS: Satisfaction with Life Scale; R: year of residency. * p < 0.05.
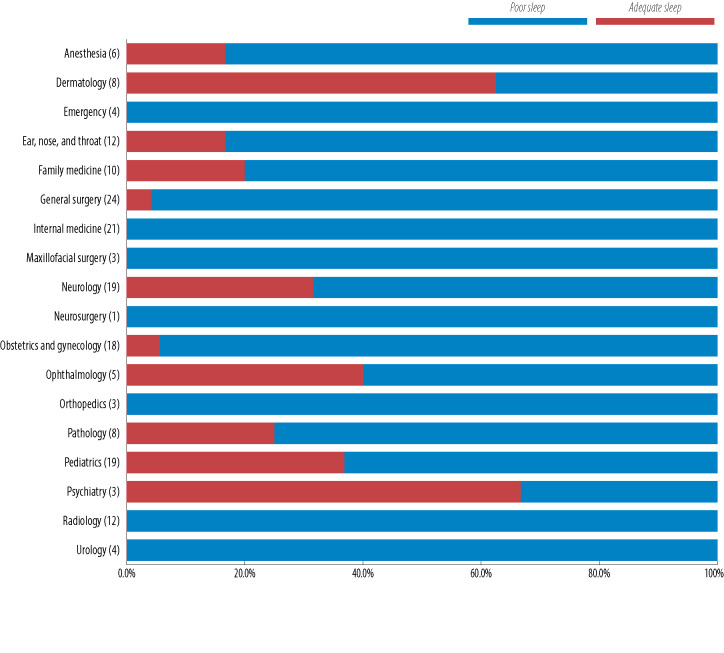
Among the different specialties, dermatology and psychiatry showed the highest adequate sleep rates (62.5% and 66.7%, respectively). However, all residents (100%) in urology, radiology, orthopedics, neurology, maxillofacial surgery, internal medicine, and emergency reported poor sleep quality [Figure 1].
Figure 1.
Sleep quality among physician residents across different specialties (frequency) presented as percentage per specialty.
Mild, moderate, and severe anxiety and depression (as measured by PHQ-4 score) were reported as 30.0%, 25.6%, and 17.2% of resident physicians, respectively. Females recorded significantly higher PHQ-4 scores than males (p = 0.002), as shown in Table 3. Higher SWLS scores were associated with lower PHQ-4 scores (p < 0.001). Post-graduate residency level and the number of monthly on-calls were not significantly associated with PHQ-4 scores [Table 3].
Table 3. Univariate and multivariate ordinal logistic regression of predictors for PHQ-4, N = 180.
| Factor | Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|---|
| p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | |||
| Lower bound | Upper bound | Lower bound | Upper bound | |||||
| Gender | ||||||||
| Female | ref | ref | ref | ref | ref | ref | ||
| Male | 0.038* | -0.560 | -1.095 | -0.032 | 0.002* | -0.889 | -1.461 | -0.317 |
| SWLS | < 0.001* | -0.158 | -0.198 | -0.118 | < 0.001* | -0.161 | -0.204 | -0.119 |
| Number of on-calls/month | ||||||||
| 0 | ref | |||||||
| 1–2 | 0.086 | -1.816 | -3.889 | 0.256 | ||||
| 3–4 | 0.075 | -1.025 | -2.155 | 0.105 | ||||
| 5–6 | 0.6 | -0.246 | -1.167 | 0.674 | ||||
| > 6 | 0.21 | -0.550 | -1.407 | 0.307 | ||||
| Residency level | ||||||||
| R1 | ref | |||||||
| R2 | 0.008* | 0.968 | 0.25 | 1.687 | 0.385 | 0.340 | -0.427 | 1.106 |
| R3 | 0.33 | 0.391 | -0.395 | 1.176 | 0.984 | 0.009 | -0.816 | 0.833 |
| R4 | 0.1 | 0.657 | -0.13 | 1.444 | 0.479 | 0.308 | -0.545 | 1.160 |
| R5 | 0.62 | -0.270 | -1.349 | 0.810 | 0.185 | 0.185 | -0.918 | 1.288 |
PHQ-4: four-item Patient Health Questionnaire for anxiety and depression; ref: reference group; SWLS: Satisfaction with Life Scale; R: year of residency. *p < 0.05
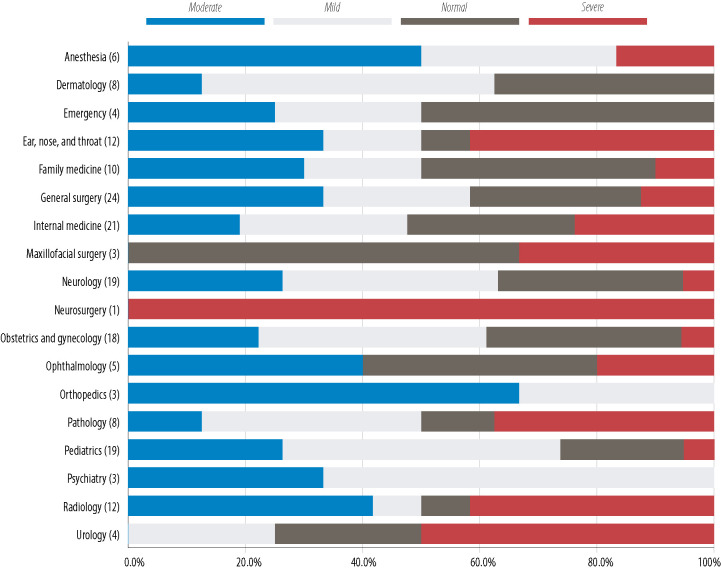
The specialties in which > 50.0% of residents reported moderate or severe PHQ-4 scores were internal medicine, maxillofacial surgery, ophthalmology, and urology [Figure 2]. Neither orthopedics nor psychiatry residents had moderate or severe PHQ-4 scores.
Figure 2.
four-item Patient Health Questionnaire for anxiety and depression stages for physician residents across different specialties (frequency) presented as percentage per specialty.
Only 13 (7.2%) residents reported that they used sleep aid medication during the past month. Medications used were alprazolam (n = 5), diphenhydramine (n = 4), melatonin (n = 3), chlorpheniramine (n = 2), and amitriptyline (n = 1).
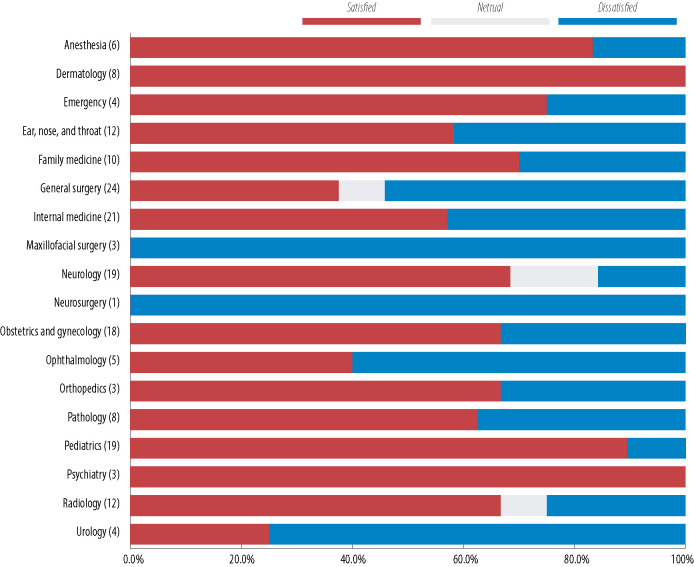
The median (IQR) SWLS score for all 180 physicians was 25.14 Satisfaction with life (sum of ‘extremely satisfied’, ‘satisfied’, and ‘slightly satisfied’) was reported by 63.3% of residents in the sample. SWLS score was significantly lower for residents in their R2, R3, and R4 years compared to their first year (p = 0.001, < 0.001, and 0.049, respectively, Dunn’s test) [Figure 3]. Gender and number of on-calls per month were not significant predictors of SWLS score (p = 0.53 and 0.66, Mann-Whitney U and Kruskal-Wallis tests, respectively).
Figure 3.
Satisfaction with Life Scale score (SWLS) as a function of residency level. Error bars represent interquartile range.
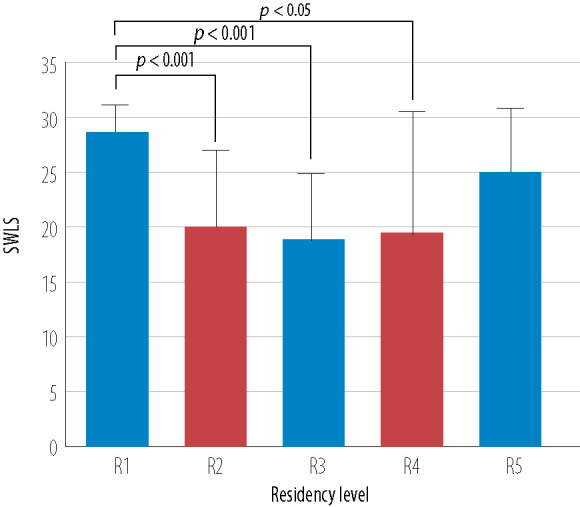
All psychiatry and dermatology residents were satisfied with their lives, and all maxillofacial surgery residents were dissatisfied. Urology and ophthalmology residents also reported high dissatisfaction rates (75.0% and 60.0%, respectively) [Figure 4].
Figure 4.
Satisfaction with life among residents across different specialties (frequency) presented as percentage per specialty.
A new sample was created after excluding residents from departments that either did not implement the new limitations or did not operate on-calls. Figure 5 compares sleep quality scores between this new sample and the older sample surveyed before work hour limitations were introduced. The bar charts compare scores between night floaters, residents working 24-hour shifts, and both groups summed together. Sample sizes are listed on the bars. Briefly, the implementation of 24-hour shifts (as opposed to the previous 32-hour long shifts) significantly decreased the percentage of residents who reported poor sleep quality (p = 0.038, Z = 2.08), while night float shifts did not change the poor PSQI percentage significantly (p = 0.2, Z = 1.29). Overall, the limitation of work hours, either by night float or 24-hour shifts decreased poor sleep quality among residents from 91.7% to 85.4%, but this change did not reach the significance threshold (p = 0.067, Z = 1.83).
Figure 5.
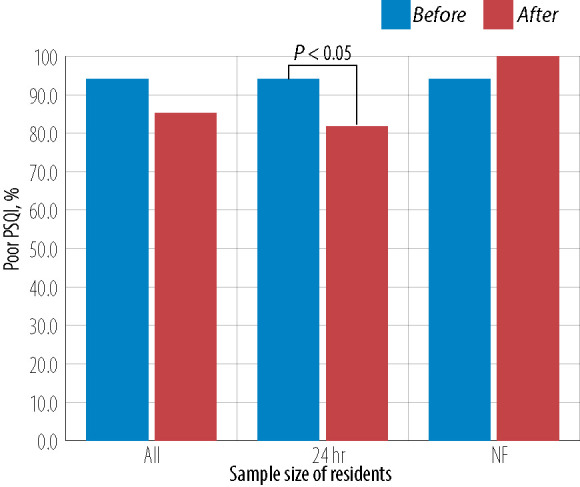
Percentage of poor sleep quality as measured by Pittsburgh Sleep Quality Index (PSQI) among residents with regular on-call shifts. The number on each bar represents sample size of residents before and after the implementation of 24-hour shift limit, night float (NF), or both added together (all). Two proportions Z-test was used for 24-hour shift.
As explained above, only residents with an effective reduction of working hours were included in this analysis. Limiting work shifts to a maximum of 24 hours decreased the prevalence of mild and severe PHQ-4 scores while increasing normal and moderate percentages [Table 4]. However, these changes were not significant (χ2 = 7.72, degree of freedom (df) = 3, p = 0.052). For night float shifts, the prevalence of moderate and severe PHQ-4 scores was lower than the older 32-hour shifts, while normal and mild PHQ-4 scores were higher (χ2 = 18.89, df = 3, p < 0.001).
Table 4. Comparison of prevalence of four-item Patient Health Questionnaire (PHQ-4) stages in residents before and after implementing duty hour limits.
| Work schedule/ PHQ-4 Stage |
All, % | 24-hour, % | Night float, % | |||
|---|---|---|---|---|---|---|
| After, n = 158 |
Before, n = 181 |
After, n = 137 |
Before, n = 141 |
After, n = 21 |
Before, n = 40 |
|
| Normal | 29.7 | 18.8 | 32.8 | 22.0 | 38.1 | 7.5 |
| Mild | 29.1 | 39.2 | 33.6 | 40.4 | 57.1 | 35.0 |
| Moderate | 24.7 | 22.1 | 23.4 | 19.1 | 4.8 | 32.5 |
| Severe | 16.5 | 19.9 | 10.2 | 18.4 | 0.0 | 25.0 |
| χ2 | 7.53 | 7.72 | 18.89, Fisher’s exact test | |||
| p-value | 0.057 | 0.052 | < 0.001 | |||
In our sample, 32.6% of males and 1.1% of females were current smokers. Among residents with regular on-call shifts, the proportion of smokers dropped significantly from 37.0% to 14.9% upon the implementation of work-hour limitations (p < 0.001, Z = 4.1). The same results were obtained for the 24-hour shift limit (p < 0.001, Z = 4.2). There was a decrease in smoking prevalence from 6.0% to 2.2% for night float shifts, but this difference was not significant (p = 0.47, Z = 0.7). Among males, smoking rates had dropped from 56.4% to 31.4% after implementing 24-hour shift limits (p = 0.002, Z = 3.17) [Figure 6].
Figure 6.
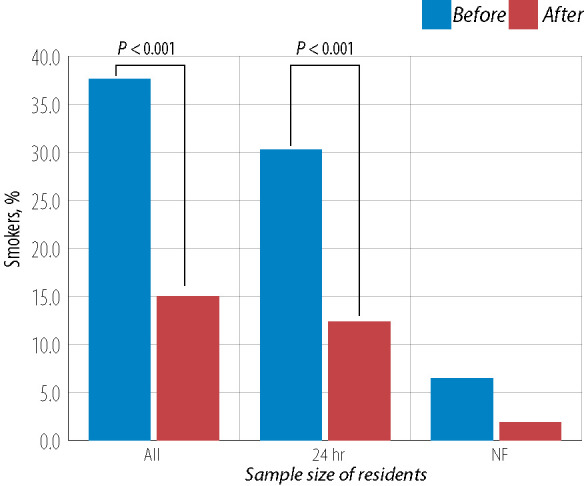
Prevalence of smoking among residents with regular on-call shifts. The number on each bar represents the sample size of residents before and after the implementation of the 24-hour shift limit, night float (NF), or both (All). Two proportions Z-test were use for both (all) and 24-hour.
Discussion
Resident physicians are exposed to excessive workloads leading to sleep deprivation, which in turn poses threats to both physician and patient health and safety.24 Many efforts are undertaken worldwide to optimize residents’ work schedules to enhance their wellbeing to the level that does not compromise their training efficiency and continuity of patient care. While many studies debate the effect of work hours’ limitation on financial implications, patient care, and physician education, its effect on residents’ wellbeing is undervalued.25 Burnout, which is a state of mental and physical exhaustion, has been gaining more attention among resident physicians recently, particularly during the first two years, with a prevalence of up to 74% of residents.26,27 Insufficient sleep is a risk factor for burnout among residents that is under-studied.28 In this study, we evaluated how reducing the working hours of medical residents influenced the quality of their sleep and their levels of anxiety and depression by evaluating those parameters before and after the duty hour limits.
Overall, the prevalence of poor sleep quality among the study sample remained high (82.8%). However, it represented a decline from the prevalence recorded in our earlier survey (90%), which was conducted in the same institution before the new work shift limitations.12 Such a high prevalence of poor sleep is not unusual among resident physicians.29,30 For instance, the prevalence of poor sleep quality was 86.3% and 85.7% among residents from Saudi Arabia and India, respectively.30,31 This study found a significant association between the male gender and poor PSQI scores, which has been demonstrated in another cohort of residents.32 In addition, a high frequency of on-call shifts per month (more than six) was significantly associated with a 10-times greater risk of poor sleep quality.Similarly, several previous studies have shown an inverse relationship between sleep quality and the number of monthly on-calls, illustrating the impact of night shifts on residents’ sleep.30,33 Residents in dermatology and psychiatry departments reported the highest prevalence of adequate sleep quality compared with other, mostly surgical specialties, consistent with previous findings.12 This could be related to the stressful lifestyle inherent to surgical training, where emergencies are abundant, work hours are longer, and caffeine intake is higher.33 In our institution, dermatology residents have no on-calls except in the first year, and psychiatry residents tend to have more quiet and less busy on-calls than other departments.
Residents with on-call shifts limited to 24 hours had significantly lower poor sleep quality than residents with 32-hour on-call shifts (p = 0.038). However, night floating residents did not demonstrate a similar trend, although the new arrangement meant that they worked shorter hours overall, possibly due to the small size of both before and after samples (40 and 21 residents, respectively). It is also likely that the benefits of these shorter hours were offset by the disruption of endogenous circadian rhythms and the atypical sleep-wake schedules precipitated by this work system.34 Previous studies have illustrated that night floating residents suffered from significant impairments in sleep duration, sleep latency, and an increased frequency of sleep interruptions, in addition to a higher prevalence of cognitive slowing in comparison with residents in normal daytime rotations.35,36
Thirteen (7.2%) residents used sleep aid medications during the past month such as first-generation antihistamines (chlorpheniramine and diphenhydramine), benzodiazepines (alprazolam), melatonin, and tricyclic antidepressants (amitriptyline). Previous studies found that 46% of 602 emergency medicine residents and 54.2% of 59 psychiatry residents regularly used medications or alcohol to induce or maintain sleep.37,38 Poor sleep quality was significantly associated with lower life satisfaction, suggesting that the relationship between human wellbeing and sleep goes beyond sleep quantity and includes the different measures of sleep quality and sleep variability.39 Moreover, satisfaction with life was significantly higher among junior residents compared to second-year residents in our survey, which could be a reflection of the cumulative impacts of residency-related lifestyle changes over time.
Our survey found an overall prevalence of 72.8% for mild, moderate, and severe anxiety and depression among residents as measured by the PHQ-4 scale. This percentage marked a marginal decrease compared to the earlier survey that reported an overall prevalence of 78.6% among residents in the same institution.12 Other studies have also reported a high prevalence of depression and anxiety (41.85% to 83.9%).8,40,41 The fact that these figures are much higher than the prevalence of both disorders in the general population underscores the significant psychological impact of the residency lifestyle and highlights the need for appropriate interventions to prevent lasting effects later in life.41,42 Although night floater shifts did not reduce rates of poor sleep quality, they were associated with a significant reduction in the prevalence of moderate and severe PHQ-4 scores in our sample compared with scores obtained during the older, traditional 32-hour shifts, which could indicate a possible positive effect of the night float system on residents.43 Setting aside its impacts on residents’ wellbeing, it is noteworthy that the effects of the night float system on clinical performance are still debated nearly 30 years after its introduction.44
Smoking rates are alarmingly high in Jordan, especially among men.45 In our previous sample, 37% of resident physicians who perform regular on-call duties were smokers.12 This study shows that smokers’ proportion significantly decreased to 14.9% after duty hour limits. However, the proportion of males was higher in the previous study (60.7% compared to 47.8% in this sample). To ensure that this association is not influenced by gender, we analyzed men before and after work hour limits to 24 hours, and the association remained significant. Increased levels of stress resulting from increased shift hours and workload can increase smoking prevalence.46,47
This study offered a rare insight into the impact of work hour limitations on resident sleep quality and levels of anxiety and depression. However, to better understand the effect of night float shift on sleep quality, we might need a larger sample size for this category of residents, especially since they showed insignificant trends for increasing rates of poor sleep quality.
Additionally, the study was deferred until three months after the country’s lockdown was over to minimize the effects the COVID-19 pandemic dictated on the changes in the workday schedule. We also cut subjects’ recruitment immediately when the second wave of COVID-19 approached the country. Nonetheless, the effects might not be fully minimized.
Conclusion
Poor sleep quality, depression, and anxiety remain highly prevalent among resident physicians. This study shows that these rates can be reduced by optimizing shift scheduling and duration, which may positively affect the efficiency of their training and continuity of patient care. We also recommend that public health authorities specifically tailor sleep hygiene practices to address residents’ needs and increase the medical workforce to better enhance sleep quality and the psychological and physical well-being of resident doctors.
Disclosure
The authors declared no conflicts of interest. The project was supported by the Jordan University of Science and Technology (grant number 20200452).
Acknowledgments
The authors would like to thank all resident physicians who participated in this study and shared their information and experiences.
References
- 1.Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015. Jun;38(6):843-844. 10.5665/sleep.4716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009. Jun;18(2):148-158. 10.1111/j.1365-2869.2008.00732.x [DOI] [PubMed] [Google Scholar]
- 3.Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety 2015. Sep;32(9):664-670. 10.1002/da.22386 [DOI] [PubMed] [Google Scholar]
- 4.Papp KK, Stoller EP, Sage P, Aikens JE, Owens J, Avidan A, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med 2004. May;79(5):394-406. 10.1097/00001888-200405000-00007 [DOI] [PubMed] [Google Scholar]
- 5.Worley SL. The Extraordinary Importance of Sleep: The detrimental effects of inadequate sleep on health and public safety drive an explosion of sleep research. P T 2018. Dec;43(12):758-763. [PMC free article] [PubMed] [Google Scholar]
- 6.Surani AA, Surani A, Zahid S, Ali S, Farhan R, Surani S. To Assess Sleep Quality among Pakistani Junior Physicians (House Officers): A Cross-sectional Study. Ann Med Health Sci Res 2015. Sep-Oct;5(5):329-333. 10.4103/2141-9248.165246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Abri MA, Jaju D, Al-Sinani S, Al-Mamari A, Albarwani S, Al-Resadi K, et al. Habitual sleep deprivation is associated with type 2 diabetes: a case-control study. Oman Med J 2016. Nov;31(6):399-403. 10.5001/omj.2016.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loria J, Rocha-Luna JM, Márquez-Ávila G. Sleep pattern and perception of sleep quality among medical residents and the relation to anxiety and depression. Emergencias 2010;22(1):33-39. [Google Scholar]
- 9.Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015. Dec;314(22):2373-2383. 10.1001/jama.2015.15845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Houqani F, Al-Mukhaini A, Al-Kindi R. Prevalence of depression among oman medical specialty board (OMSB) residents. Oman Med J 2020. Apr;35(2):e116. 10.5001/omj.2020.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ 2008. Mar;336(7642):488-491. 10.1136/bmj.39469.763218.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaradat R, Lahlouh A, Mustafa M. Sleep quality and health related problems of shift work among resident physicians: a cross-sectional study. Sleep Med 2020. Feb;66:201-206. 10.1016/j.sleep.2019.11.1258 [DOI] [PubMed] [Google Scholar]
- 13.Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J. Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ 2001. Nov;323(7323):1222-1223. 10.1136/bmj.323.7323.1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med 2006. Dec;3(12):e487. 10.1371/journal.pmed.0030487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Harvard Work Hours, Health, and Safety Group . Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med 2005. Jan;352(2):125-134. 10.1056/NEJMoa041401 [DOI] [PubMed] [Google Scholar]
- 16.Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med 2004. Oct;351(18):1838-1848. 10.1056/NEJMoa041406 [DOI] [PubMed] [Google Scholar]
- 17.Mansukhani MP, Kolla BP, Surani S, Varon J, Ramar K. Sleep deprivation in resident physicians, work hour limitations, and related outcomes: a systematic review of the literature. Postgrad Med 2012. Jul;124(4):241-249. 10.3810/pgm.2012.07.2583 [DOI] [PubMed] [Google Scholar]
- 18.Weiss P, Kryger M, Knauert M. Impact of extended duty hours on medical trainees. Sleep Health 2016. Dec;2(4):309-315. 10.1016/j.sleh.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogawa R, Seo E, Maeno T, Ito M, Sanuki M, Maeno T. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ 2018. Mar;18(1):50. 10.1186/s12909-018-1171-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.(ACGME), A.C.f.G.M.E. Common Program Requirements (Residency). effective July 1, 2020 [cited 2021 January 13]. Available from: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2020.pdf.
- 21.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989. May;28(2):193-213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009. Nov-Dec;50(6):613-621. [DOI] [PubMed] [Google Scholar]
- 23.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess 1985. Feb;49(1):71-75. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- 24.Lockley SW, Barger LK, Ayas NT, Rothschild JM, Czeisler CA, Landrigan CP, Harvard Work Hours, Health and Safety Group . Effects of health care provider work hours and sleep deprivation on safety and performance. Jt Comm J Qual Patient Saf 2007. Nov;33(11)(Suppl):7-18. 10.1016/S1553-7250(07)33109-7 [DOI] [PubMed] [Google Scholar]
- 25.McHill AW, Czeisler CA, Shea SA. Resident physician extended work hours and burnout. Sleep 2018. Aug;41(8):zsy112. 10.1093/sleep/zsy112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 2014. Mar;89(3):443-451. 10.1097/ACM.0000000000000134 [DOI] [PubMed] [Google Scholar]
- 27.Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry 2004;28(3):240-242. 10.1176/appi.ap.28.3.240 [DOI] [PubMed] [Google Scholar]
- 28.Kancherla BS, Upender R, Collen JF, Rishi MA, Sullivan SS, Ahmed O, et al. What is the role of sleep in physician burnout? J Clin Sleep Med 2020. May;16(5):807-810. 10.5664/jcsm.8412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murthy VS, Nayak AS. Assessment of sleep quality in post-graduate residents in a tertiary hospital and teaching institute. Ind Psychiatry J 2014. Jan;23(1):23-26. 10.4103/0972-6748.144952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.AlSaif HI. Prevalence of and risk factors for poor sleep quality among residents in training in KSA. J Taibah Univ Med Sci 2018. Dec;14(1):52-59. 10.1016/j.jtumed.2018.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mastin D, Siddalingaiah HS, Singh A, Lal V. Excessive daytime sleepiness, sleep hygiene, and work hours among Medical residents in India. J Trop Psychol. [cited 2012 July 12]. Available from: https://www.cambridge.org/core/journals/journal-of-tropical-psychology/article/excessive-daytime-sleepiness-sleep-hygiene-and-work-hours-among-medical-residents-in-india/F39919E9E675939CA5741648F37223C0.
- 32.Mota MC, De-Souza DA, Rossato LT, Silva CM, Araújo MB, Tufik S, et al. Dietary patterns, metabolic markers and subjective sleep measures in resident physicians. Chronobiol Int 2013. Oct;30(8):1032-1041. 10.3109/07420528.2013.796966 [DOI] [PubMed] [Google Scholar]
- 33.Esen A, Mercan GN, Kacar E, Toprak D. Sleep quality and related factors in medical residents. Turkish J Family Med Prim Care 2017;11(4):271-277 . 10.21763/tjfmpc.359842 [DOI] [Google Scholar]
- 34.Boudreau P, Dumont GA, Boivin DB. Circadian adaptation to night shift work influences sleep, performance, mood and the autonomic modulation of the heart. PLoS One 2013. Jul;8(7):e70813. 10.1371/journal.pone.0070813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cavallo A, Jaskiewicz J, Ris MD. Impact of night-float rotation on sleep, mood, and alertness: the resident’s perception. Chronobiol Int 2002. Sep;19(5):893-902. 10.1081/CBI-120014106 [DOI] [PubMed] [Google Scholar]
- 36.Dunn LK, Kleiman AM, Forkin KT, Bechtel AJ, Collins SR, Potter JF, et al. Anesthesiology resident night float duty alters sleep patterns: an observational study. Anesthesiology 2019. Aug;131(2):401-409. 10.1097/ALN.0000000000002806 [DOI] [PubMed] [Google Scholar]
- 37.Handel DA, Raja A, Lindsell CJ. The use of sleep aids among Emergency Medicine residents: a web based survey. BMC Health Serv Res 2006. Oct;6(1):136. 10.1186/1472-6963-6-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carvalho Aguiar Melo M, das Chagas Medeiros F, Meireles Sales de Bruin V, Pinheiro Santana JA, Bastos Lima A, De Francesco Daher E. Sleep Quality Among Psychiatry Residents. Can J Psychiatry 2016. Jan;61(1):44-49. 10.1177/0706743715620410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ness TE, Saksvik-Lehouillier I. The Relationships between life satisfaction and sleep quality, sleep duration and variability of sleep in university students. Journal of European Psychology Students 2018;9:28-39 . 10.5334/jeps.434 [DOI] [Google Scholar]
- 40.Pereira-Lima K, Loureiro SR. Burnout, anxiety, depression, and social skills in medical residents. Psychol Health Med 2015;20(3):353-362. 10.1080/13548506.2014.936889 [DOI] [PubMed] [Google Scholar]
- 41.Pereira-Lima K, Loureiro SR, Crippa JA. Mental health in medical residents: relationship with personal, work-related, and sociodemographic variables. Braz J Psychiatry 2016. Oct-Dec;38(4):318-324. 10.1590/1516-4446-2015-1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bellini LM, Baime M, Shea JA. Variation of mood and empathy during internship. JAMA 2002. Jun;287(23):3143-3146. 10.1001/jama.287.23.3143 [DOI] [PubMed] [Google Scholar]
- 43.Gottlieb DJ, Peterson CA, Parenti CM, Lofgren RP. Effects of a night float system on housestaff neuropsychologic function. J Gen Intern Med 1993. Mar;8(3):146-148. 10.1007/BF02599762 [DOI] [PubMed] [Google Scholar]
- 44.Saddawi-Konefka D, Baker KH. If you thought that night float solved everything, keep dreaming. Anesthesiology 2019. Aug;131(2):236-237. 10.1097/ALN.0000000000002790 [DOI] [PubMed] [Google Scholar]
- 45.Jaghbir M, Shreif S, Ahram M. Pattern of cigarette and waterpipe smoking in the adult population of Jordan. East Mediterr Health J 2014. Oct;20(9):529-537. 10.26719/2014.20.9.529 [DOI] [PubMed] [Google Scholar]
- 46.Finkelstein DM, Kubzansky LD, Goodman E. Social status, stress, and adolescent smoking. J Adolesc Health 2006. Nov;39(5):678-685. 10.1016/j.jadohealth.2006.04.011 [DOI] [PubMed] [Google Scholar]
- 47.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg 2009. Apr;144(4):371-376. 10.1001/archsurg.2008.575 [DOI] [PubMed] [Google Scholar]