Abstract
The stress and violence to fire-based emergency medical service responders (SAVER) Systems-Level Checklist is an organizational-level intervention to address stress and violence in emergency medical service (EMS), focused on the development of policy and training. Fire and EMS leadership, first responders, dispatchers, and labor union representatives participated in the SAVER Model Policy Collaborative to develop model policies that resulted from the most feasible checklist items. ThinkLets technology was employed to achieve consensus on the model policies, and an Action SWOT analysis was then conducted to assess facilitators and barriers to policy implementation. The resultant model policies are a systems-level workplace violence intervention for the U.S. fire and rescue service that is ready for implementation. Expected improvements to organizational outcomes such as burnout, job engagement, and job satisfaction are anticipated, as are decreasing assaults and injuries. The SAVER Model Policies have the potential to inform national standards and regulations on workplace violence in EMS.
Keywords: firefighters, EMS, policy, workplace violence, burnout, stress
Introduction
This paper presents the development of model policies to address stress and violence in emergency medical service (EMS) at the organizational level. The stress and violence to fire-based EMS responders (SAVER) systems-level checklist was first created as an organizational-level intervention to address stress and violence in EMS, focused on the development of policy and training. Fire and EMS leadership, first responders, dispatchers, and labor union representatives then participated in the SAVER Model Policy Collaborative to develop model policies that resulted from the most feasible checklist items. ThinkLets technology was employed to achieve consensus on the model policies, and an Action SWOT (strengths, weaknesses, opportunities, and threats) analysis was then conducted to assess facilitators and barriers to policy implementation. The resultant model policies are a systems-level workplace violence intervention for the U.S. fire and rescue service that is ready for implementation. Expected improvements to organizational outcomes such as burnout, job engagement, and job satisfaction are anticipated, as are decreasing assaults and injuries. The SAVER Model Policies have the potential to inform national standards and regulations on workplace violence in EMS. In the section that follows, we present the need for and utility of the SAVER Model Policies.
Background
There are 1.1 million U.S. firefighters, 67 percent of whom are volunteers. 1 The term firefighter includes single role firefighters, cross-trained firefighters (e.g., firefighter-emergency medical technician (EMT), firefighter-paramedic), single role EMTs, and single role paramedics. Even single role firefighters perform first response on EMS calls; therefore, in this manuscript, we use the terms firefighter and EMS responder interchangeably to be inclusive of all of these roles and the fact that every fire department operates differently. Fire departments provide 40 percent of the nation's EMS. 2 On average, 64 percent of fire department 911 calls are for EMS. 3 Between 1980 and 2018, the number of calls for EMS increased 367 percent. 3 Fire-based EMS responders believe they are under severe stress and are concerned about impacts on their physical and mental health. 4 The annual rate of non-fatal injuries among U.S. paramedics is five times higher than the national average for all workers. 5 The annual rate of occupational fatalities among paramedics is two times higher than the national average for all workers. 6
Workplace Stress. EMS has a number of features that make it a stressful occupation: inadequate sleep, 7 insufficient recovery time after each shift, 8 shiftwork, 9 low job satisfaction, 10 and trauma response leading to burnout and post-traumatic stress disorders (PTSD). 10 Stress is also the most frequently reported injury among EMS providers. 11 A number of studies indicate that the prevalence of PTSD in EMS workers is higher than 20 percent.12–18 EMS responders have high rates of suicidal ideation and attempts. 19 These outcomes are very costly to employers and threaten the stability of the healthcare safety net EMS provides.20–23 The Firefighter Behavioral Health Alliance tracks and validates all firefighter, EMS, and dispatcher suicides. Since 2000, it recorded 1586 firefighter and EMS suicides. 24
In a national survey of 4000 EMS responders, 25 86 percent reported experiencing critical stress, 37 percent reported suicidal ideation, and 7 percent attempted suicide. An EMS World survey of 903 paramedics and EMTs in Missouri, Illinois, Kentucky, and Iowa found almost a third of respondents (31 percent) indicated heightened future risk of suicidal behavior and nearly as many (27 percent) indicated suicidal ideation in the past twelve months. 26 Respondents discussed contributing factors to poor mental health on the job: inadequate organizational support, lack of recovery time after traumatic calls, and Employee Assistance Programs unfamiliar with EMS work. 26
Fire-based EMS responders describe the 911 system as strained by the high volume of low acuity calls that occupy much of their workload, divert resources from true emergencies, and lead to unwarranted occupational hazards like speeding to respond to non-serious calls. 27 As a result, firefighters reported high occupational stress, low morale, and desensitization to community needs. 27 According to Cannuscio et al., firefighters are calling for improvements to the 911 system: better triage, more targeted use of EMS resources, continuing education to align with expanding job demands, and a strengthened social safety net to address the persistent needs of poor and elderly populations. 27
Workplace Violence. Violence exposure is associated with increased anxiety, stress, and fear among EMS workers.28,29 In a retrospective cohort study of nationally registered EMTs, 8 percent of fatalities were due to assaults. 30 A study of firefighter injury found paramedics had a 14-fold higher odds of violent injuries than firefighters. 4 In a systematic literature review of violence against fire-based EMS responders, between 57 and 93 percent of EMS responders experienced an act of verbal and/or physical violence at least once. 31 Verbal violence was the most prevalent form. The range of physical violence ever experienced by EMS responders is estimated between 23 and 90 percent with patients being the most common perpetrator. 31 Combined with the increasing demand for services, the threat of violence adds another significant source of workplace stress. Fire-based EMS responders frequently describe their work as “doing more with less” because their city and municipal budgets do not provide enough staffing, apparatus, training, or rest to accommodate the emotional demands of the job. 27
Interventions to Reduce Workplace Stress and Violence. Previous research developed the SAVER Sytems-level Checklist, a policy and training checklist intervention ready for fire departments to implement to reduce violence-related injury, reduce work stress, and improve organizational outcomes (e.g., burnout, job satisfaction, engagement) for EMS responders. 32 The checklist was comprehensive, including 174 policy and training items across the phases of EMS response, including pre-event, traveling to the scene, scene arrival, patient care, assessing readiness to return to service, and post-event. While the fire department holds responsibility for these 174 items, the fire-based EMS responder has a separate six-item checklist, called the SAVER Pause Points. Pause points empower the individual responder to speak up to the organization sharing their experiences in the field as a way to give feedback on how the checklist intervention is working.33,34 Pause points flatten the organizational hierarchy by giving autonomy and decision-making to those who previously had little. As the demand for 911 services is continually growing, job demand and control theory 35 provides evidence that the best relief is to enhance organizational resources that increase worker control by involving them in the design of the system in which they work and looking to them for feedback when the system fails.
When the checklist was initially developed, it was designed to be all-inclusive, fully encompassing all possible policy, training, technological or engineering modifications, and individual-level actions desired by fire departments and subject matter experts. Through a multi-step, rigorous process, the checklist was refined to arrive at the 174-item list and subsequently each item was rated on feasibility of implementation. 34 We subsequently re-evaluated the checklist items with twenty representatives from the three fire departments who would be testing the implementation. Those processes indicated that 45.5 percent of votes across all phases rated items as most feasible, 34.9 percent as less feasible, and 19.6 percent as extremely difficult. 36 Thus, we recognized that the checklist as designed was not immediately feasible for implementation, with length and feasibility presenting a realistic impediment. To prepare for implementation and evaluation of the checklist among our study sites, we narrowed our focus to the most feasible checklist items, with the intent to address less feasible items over time. We also preemptively identified the need to implement the checklist items that best support operationalization of the pause points, as those items are important feedback mechanisms for organizational change. Eight categories emerged that became the draft SAVER Model Policies, which then underwent a multi-step, rigorous process of streamlining, consensus, and pre-meditation of implementation efficacy.
Conceptual Framework
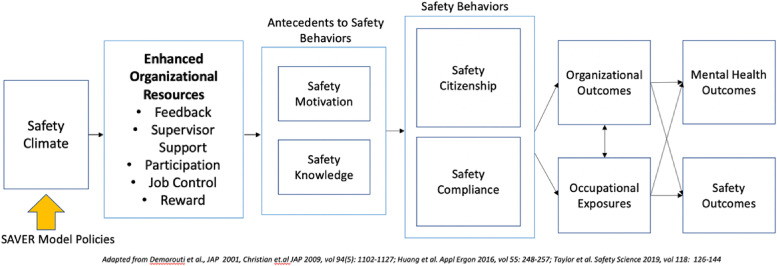
The conceptual model that guided this research and the development of the SAVER Model Policies (Figure 1) is based on organizational safety climate as a predictor of organizational and safety outcomes.32,37,38 Safety climate, if positive, can create improvements to organizational outcomes such as turnover, job satisfaction, and employee engagement.38,39 These organizational outcomes predict each other and then predict physical and mental injuries. We also incorporated Demerouti's job demand-resource (JDR) framework into the safety climate framework. 35 According to JDR, occupational contexts of high demands yet low resources are likely to be perceived as stressful, negatively influencing workers’ job satisfaction. 35 Prolonged exposure to the non-satisfactory, stressful work environment and one's continuing efforts to cope with it can deplete the person's psychophysical resources, leading to burnout as suggested by Selye. 40 Meanwhile, workers may want to avoid the stressful work environment by leaving the job (“flight”) if their efforts to improve the work environment (“fight”) are not successful. 41
Figure 1.
Conceptual framework.
The relationship between job satisfaction and turnover/intention to leave has been consistently and widely noted. 42
Lack of engagement can be associated with stressful experiences such as work disruption and reduced motivation, increasing the chance of burnout.43,44 Workers who are less engaged are likely to have greater intention to leave due to these negative psychological and behavioral outcomes.45,46 Organizational factors are directly and indirectly related to occupational safety.47,48 Occupational injuries are closely associated with workers’ safety behaviors41,42 and workers’ behaviors are influenced largely by the organization.
Lack of engagement can also lead to failure to comply with safety rules and policies. 48 If workers are dissatisfied with work, stressed, and burnt-out, the chance of making errors while performing tasks escalates resulting in higher frequency and greater severity of occupational injuries. 49 The negative impact of firefighter and EMS worker burnout on various psychological well-being variables such as PTSD50,51 and psychological symptoms such as depression and anxiety52,53 has been well documented. If burnout and psychological health are not properly addressed, severe mental health outcomes such as suicidal ideation or suicide are more likely.54,55 The SAVER Model Policy intervention is a set of enhanced organizational resources that address the negative effects of job demand.
Methods
The SAVER Model Policies were developed in three stages: (1) the development of the draft model policies by experts, (2) a policy collaborative including subject matter experts from the fire and rescue service, and (3) a SWOT analysis of the policies by the participants at the policy collaborative in preparation for implementation.
Stage 1 consisted of the research team carefully reviewing the SAVER Checklist, with a specific focus on the approximately eighty checklist items that were rated as “most feasible” during the SAVER Checklist Consensus Conference and a subsequent feasibility assessment conducted with the study sites.34,36 Though preference was given to the most feasible items, some less feasible items were chosen for inclusion, based on their importance and relevance to EMS responder safety and well-being, and best supported the operationalization of the pause points. These checklist items were then organized thematically along the continuum of EMS response. Checklist items were refined, deduplicated, and in some minor circumstances, combined with similar checklist items to arrive at the draft SAVER Model Policies. The draft policies were placed into one of eight policy categories. Then we reviewed all checklist items to see if any of the lesser feasibility items mapped onto these categories. From this review, eighty-nine checklist items were included. The policy statements were drafted and a goal statement was developed for each policy.
Stage 2 consisted of the SAVER Model Policy Collaborative, an innovative science-based and practical review of the model policies by subject matter experts from the fire and rescue service. In February 2020, twenty representatives from three large municipal fire departments, already planning for immediate implementation of the policies, convened for a two-day policy collaborative allowing for revision, consensus-building, and evaluation of the SAVER Model Policies.
The stakeholders represented the three SAVER study sites and had a wide range of service levels, with a particular emphasis on emergency medical responder expertise and leadership. Multiple members from each study site were invited to ensure organizational and occupational representation at the following fire department levels: leadership, labor union, EMS field supervisor, paramedic with ten to fifteen years of experience, and dispatch. It was encouraged that the leadership representative be very familiar with the policy process within their department. Due to the diverse nature of some departments, additional representation was also invited to participate in the collaborative (e.g., lifeguards, third-party ambulance providers).
To facilitate the model policy review process, we utilized a series of structured focus groups constructed using ThinkLet systems, a facilitated consensus-building facilitation technique and collaboration method. 56 The facilitated collaboration ThinkLet system developed for the review was based on previous research 57 and referred to as ThinkLets 1-8: Policy Review. Prior to the sessions, the facilitation team received training to ensure consistency across the ThinkLet sessions. Each ThinkLet session was facilitated by a lead facilitator with an assistant to take notes and manage logistics. Initial event planning anticipated a total of twenty Policy Review sessions (ThinkLets 1-8), comprised of two policy review sessions as a large-group, and six policy review sessions among three separate groups.58,59 Adjustments were made on the day of the event due to the unanticipated nature of fire and rescue work and the lack of anticipated representation from one of the study sites. The schedule shifted to hosting fourteen policy review sessions, comprised of two policy review sessions as a large-group, and six policy review sessions among two separate groups. Extensive event planning and staff training allowed for smooth and swift transition to accommodate the new processes.
The ThinkLet sessions ranged from thirty to fifty minutes long, followed by a fifteen-to-thirty-minute break. The variation in timing coincided with the variation in length of each policy being reviewed. The longer the policy, the longer the session and break. The breaks allowed the facilitators essential time to check in with one another on each session's progress, make process adjustments, and affirm goals. The breaks also afforded participants with cognitive rest and networking opportunities. This iterative process allowed for constant refinement of the policies throughout the sessions, inclusive of feedback on policy formatting, language, and definitions. At the end of Day One, the facilitators then compiled all the changes in preparation for Day Two, which included a final review as a large group and Stage 3, consisting of the Action SWOT analysis.
Stage 3 occurred on Day Two of the SAVER Model Policy Collaborative when an action SWOT analysis was conducted 60 (Figure 2). This process identified specific actions departments and leadership teams could take to ensure the success of the policy intervention, including identifying the internal strengths of the policies as currently constituted, the internal weaknesses, the external opportunities they present for the fire and rescue service and communities they serve, and the external threats to their implementation and success. Participants were divided into four groups of four to five individuals, with at least one representative from each participating department. Each group rotated clockwise among each of the four SWOT domains. Therefore, if they began in the strengths group, they subsequently rotated among weaknesses, opportunities, then threats. If they began in threats, they rotated to strengths, weaknesses, and opportunities. Each SWOT domain was led by a facilitator who clarified and synthesized contributions and directed the scribe who wrote responses on large poster paper to summarize and thematically group responses. The facilitators asked the following questions:
(Internal) Strengths: What actions will we need to take to preserve and protect the current strengths? How can we prevent slippage of existing strengths?
(Internal) Weaknesses: What can mitigate these weaknesses, to reduce their power or influence? What would it take to overcome the weaknesses?
(External) Opportunities: How can we capitalize on the opportunities? What strategies can we design that will enhance those opportunities?
(External) Threats: What can prevent these threats in the future? How can threats be isolated ?
Figure 2.
SWOT participants.
The process was iterative and each group rotation built upon the previous groups’ responses. As the process progressed, each rotation decreased in time and ranged from thirty minutes to fifteen minutes. This allowed for a longer break and cognitive rest before engaging the group for the last component of the SWOT analysis. During the break, the research team compiled and organized the responses for each SWOT domain and then reconvened the entire participant group for a discussion of the results lasting approximately two hours (Figure 3).
Figure 3.
SWOT results discussion.
As an ensemble, we gained clarification from the participants and eliminated any redundancies in each SWOT domain. These decisions were all live-scribed manually and electronically in order to send participants home with the raw results.
Our last activity was to review the Model Policies that had been developed in the collaborative to-date and review the SWOT analysis to pre-meditate implementation efficacy. These reviews were led by fire and rescue service participants with facilitation by the research team, with opportunities for discussion and clarification by all participants. We then shared the raw results of the SWOT analysis. Participants were sent home with the refined Model Policies and raw results of the SWOT analysis. The intent was for participants to have everything they needed to begin policy implementation. Participants also received instruction to convene a policy workgroup and identify a point-person to oversee the department-level policy process.
Participants completed an evaluation of the SAVER Model Policy Collaborative assessing their level of satisfaction, degree of collaboration, and their competencies communicating the SAVER Model Policies and implementation issues raised during the SWOT analysis (Supplemental material).
After the policy collaborative, the research team conducted a qualitative analysis of the raw SWOT results. Participant elicitations were grouped into themes for each SWOT dimension. Action items were summarized based on participant ideas to ensure successful policy implementation. These results were then shared with the study sites in preparation for implementation.
Results
Thematic Arrangement of Policies
From the approximately eighty checklist items rated as “most feasible” by the study sites,34–36 the following policies were developed: (1) Mission Statement; (2) Defining Violence; (3) Dispatch: Communication & Coordination; (4) Assessment and Communication of Scene Conditions; (5) Standard Operating Procedures During Patient Care; (6) Readiness to Return to Service; (7) Reporting of Violence; and (8) Mental and Physical Health Support (Table 1).
Table 1.
The SAVER Model Policies.
| Preamble/Purpose: |
| This department does not tolerate violence of any kind against members. Therefore, the following eight (8) policies have been enacted and training goals identified: |
| 1. Mission statement |
|
Goal: To promote the health and safety of members by focusing on organizational structure. This Policy/ Standard Operating Procedure (SOP)/Standard Operating Guideline (SOG) will establish a strong organizational commitment to Emergency Medical Services which will elevate and prioritize EMS work to the level fire suppression receives. This will support two goals: safe EMS workers and quality patient care to the communities served.
Goal: There is a strong potential for violence to occur on every call, therefore we have established policies, procedures, and practices for managing this reality. |
| 1.1 The safety, health, well-being, and after-care of our members is paramount in order to provide quality community service. |
| 1.2 We value equally all duties, roles, and responsibilities in our department [department should include all roles]. |
| 1.3 EMS responders, firefighters, dispatchers, and leadership will use a team-centric approach in the patient care process. |
| 1.4 We recognize that violence is an omnipresent hazard in our work and will implement policies, procedures, and practices to prevent and respond to harm to our members. |
| 1.5 Regardless of rank or experience members [will/are encouraged to/have the power and right to] express any and all violence concerns to each other, to their company officers, to administration, and to the union. |
| Especially with regard to verbal and physical violence, no member shall fear harassment, embarrassment, or punishment. |
| 1.6 There will be a standing joint labor management and EMS committee that meets regularly to discuss responder safety issues. |
| 1.7 The department provides ride-alongs and fire/EMS 101 for local politicians, media, researchers, clinicians, etc. |
| 2. Defining violence |
| Goal: To use common language in the definition of violence. |
| 2.1 This is how our department defines violence against members: |
| Perpetrator is defined as: patient/client/bystander/civilian, the patients’ friend(s), family member(s), other professional(s). |
| Verbal abuse: any use of offensive language or yelling by a perpetrator, regardless of intent. To include, but not limited to, threats of abuse over the phone, social media, email, texts, and other forms of written communication. |
| Property damage or theft: any action that results in damage or theft of property belonging to the EMS provider, their family or workplace by a perpetrator. To include, but not limited to, damage to or theft of a vehicle, personal effects, home contents, office equipment and supplies, or office furnishings. Attempted theft or attempted damage of the above items is also included. |
| Intimidation: any threat, following/stalking, loitering, or use of gestures that provoke offense or fear by a perpetrator. |
| Physical abuse: any physical attack or attempted physical attack by a perpetrator. To include, but not limited to, behaviors such as punching, slapping, spitting, biting, kicking, or using a weapon or other object with the intent of causing bodily harm. |
|
Sexual harassment: any form of sexual propositioning or unwelcome sexual attention from a perpetrator. To include, but not limited to, behaviors such as humiliating or offensive jokes and remarks with sexual overtones; suggestive looks or physical gestures; inappropriate gifts or requests for inappropriate physical examinations; pressure for dates; and brushing, touching, or grabbing excluding sexual touching (e.g., the genital, buttocks, or breast area). Training: The department will hold an annual training/bulletin/IST/to train members on these definitions. |
| 3. Dispatch: Communication & coordination |
| Goal: To establish a collaborative and communicative relationship with, EMS responders, dispatch, and law enforcement designed to provide EMS responders with ample notice, knowledge, and preparation for responding to all calls, especially with regard to any previously known violent location, patient, or circumstances. |
| Pause point: If you have knowledge that this is a previously known violent location, request and wait for law enforcement back-up. |
| 3.1 The department will operationalize a “flag/premise history/caution note” in the dispatch system to alert EMS responders to previously known violent locations and individuals. |
| 3.2 The department has developed the following Policy/SOP/SOGs for law enforcement notification of emergency response calls that require or request law enforcement backup: [Insert Policy/SOP/SOG here] |
| 3.3 The department is equipped with the necessary resources to share radio frequency between police and fire dispatch to allow for transparent sharing of information during EMS calls that request or require police assistance. |
| 3.4 The department has developed the following dispatch Policy/SOP/SOGs for launching additional resources to support scene safety: [Insert Policy/SOP/SOG here] |
| 3.5 If feasible, dispatchers are required to keep the caller on the line until EMS arrives to ensure information is shared correctly and effectively. Training: Fire and Police Dispatchers, EMS responders, and law enforcement officers will receive annual training on the above policies. |
| 4. Assessment and communication of scene conditions |
|
Goal: To establish procedures for assessing scene safety and communication of needs during unsafe conditions. Goal: To establish standardized language understood by everyone who communicates that a member is in trouble and immediately initiates actions to rescue the member(s) without further need for input or clarifications. |
| Pause point: Before exiting the emergency vehicle, are all of the resources you need in place to safely begin patient care? |
| 4.1 The department has invoked Policy/SOP/SOGs and tools for scene assessment: [Insert Policy/SOP/SOG here] |
| 4.2 The department has comprehensive policies for unit staging during events with a potential for violence: [e.g., mental health, suicide, domestic violence, etc.] [Insert link to your policy here] |
| 4.3 The department has initiated the following Policy/SOP/SOGs for EMS responders which requires communicating scene conditions and assessing any risks to personal safety upon scene arrival: [Insert link to your policy here] |
| 4.4 The department has developed the following Policy/SOP/SOGs which outline contextually specific scenarios that may require communicating field updates to dispatch and vice versa: [Insert link to your policy here] |
| 4.5 The department has enacted Policy/SOP/SOGs that safeguard members by calling for back-up at the earliest recognition of a threat: [Insert link to your policy here] |
| 4.6 To enhance multi-departmental collaboration, universal codes for distress or emergency are shared between police and EMS responders. [insert department defined codes here] |
| 4.7 Personnel will use a department-specific term [i.e., “mayday/assist/cover now”] when they feel threatened and need immediate assistance. |
| 4.8 If EMS responders require additional assistance, dispatch will initiate the response of the requested agencies (EMS responders, fire engines, or police). |
| 4.9 In the event that verbal communication is not a safe option, there are ‘panic button’ mechanisms that will signal the need for assistance. Training: Fire and police dispatchers, EMS responders, and law enforcement officers will receive annual training on the above policies. |
| 5. Standard operating procedures during patient care |
| Goal: To establish policies, procedures, and practices to protect EMS responders during patient care activities. |
| Pause point: During patient care and before transport, does your patient require physical or chemical (i.e., sedation) restraint and have they been checked for weapons? |
| 5.1 The following standard operating procedures (SOPs) have been integrated with departmental policies to support EMS responders in potentially threatening calls (e.g., drug or alcohol, underlying health condition, altered mental status): [Insert Policy/SOP/SOG here] |
| 5.2 If the EMS responders’ safety on scene is at risk, the department has initiated a Policy/SOP/SOG detailing how and when to leave the scene—with or without the patient: [Insert link to your policy here] |
| 5.3 The following safe practice Policy/SOP/SOGs (e.g., if weapons are found on patient or bystander, etc.) have been enacted: [Insert link to your policy here] |
| 5.4 For patient and provider safety and security, the following Policy/SOP/SOGs must be followed if weapons are discovered when in transit: [Insert link to your policy here] |
| 5.5 EMS responders will request police escort and/or accompaniment for violent or arrested patients. |
| 5.6 Patients will be properly secured and/or physically or chemically (sedated) restrained in the emergency vehicle using department approved methods consistent with upholding patient and provider safety. |
| 5.7 The following Policy/SOP/SOGs outline when to use restraints (chemical/sedation or physical) on patients: [Insert link to your policy here]. In some circumstances, physical or chemical (sedation) restraints may require interagency involvement (Police, Medical Control, etc.) as described in the Policy/SOP/SOGs. |
| 5.8 If body armor is used, the department has the following Policy/SOP/SOGs that supports and encourages the EMS responders in their decision to don body armor: [Insert link to your policy here] |
| 5.9 Individuals may ride in the cab or patient care compartment of the emergency vehicle at the EMS responder's discretion. Violent patients must be indicated to receiving staff at the Emergency Department or healthcare facility prior to arrival. During patient handoff, verbal and/or written communication will alert pertinent staff of patient or bystander violence. |
| There is a reporting Policy/SOP/SOG in place to notify hospitals that an EMS responder has been injured by a patient/bystander: [insert Policy/SOP/SOG here] Training: EMS responders will receive annual training on the above policies. |
Consensus on the Model Policies
During the SAVER Model Policy Collaborative, our subject matter experts refined the goal statements, objectives, pause points, and language within each policy. Policy language was frequently refined (from the original checklist item and draft policy language) in order to meet the allowable policy vernacular deemed necessary by the departments to avoid any anticipated legal/risk management/Human Resource review or pushback. Participants also came to consensus that each policy should contain only one training item. This reduced the total number of training items to eight and focused training on the policy as a whole rather than the individual components comprised within the policy. During the ThinkLets, facilitators prompted participants to identify if their department had a policy or element of a policy already existing, and that information was documented by recording the policy number and requesting the participant to email the policy language to the research team during the meeting or afterward. Since multiple department members from the same organization were in each policy review group, these colleagues were able to converse and quickly identify the correct departmental policy to share with the research team. This allowed us to modify the draft language and share existing policies with other participants as their departments initiated local modifications.
The largest discussion of any policy item during the collaborative related to Policy 6.2: “All department members are entitled to breaks for food, rest room use, and rest during their shift.” In prior feasibility assessments, the original checklist item that this policy item derived from received the most “most feasible” votes at the SAVER Systems-level Checklist Conference, yet the most “extremely difficult” votes in the study site reassessment.34,36 The research team chose to include this item in the model policies due to its immense power in granting workers autonomy, and also time to tend to basic personal needs. Ultimately, participants deemed this item necessary to include. Though each department recognized that this particular item would be challenging to implement, they also recognized that by advocating for its inclusion they had the opportunity to lead the nation and change the culture surrounding worker health, safety, and well-being.
The resultant SAVER model policies comprised fifty-seven of the original checklist items (a reduction of thirty-two items from the start of the policy collaborative). The refined policies are generally arranged by the Pre-Event through Post-Event phases of an EMS call from the original checklist. 34
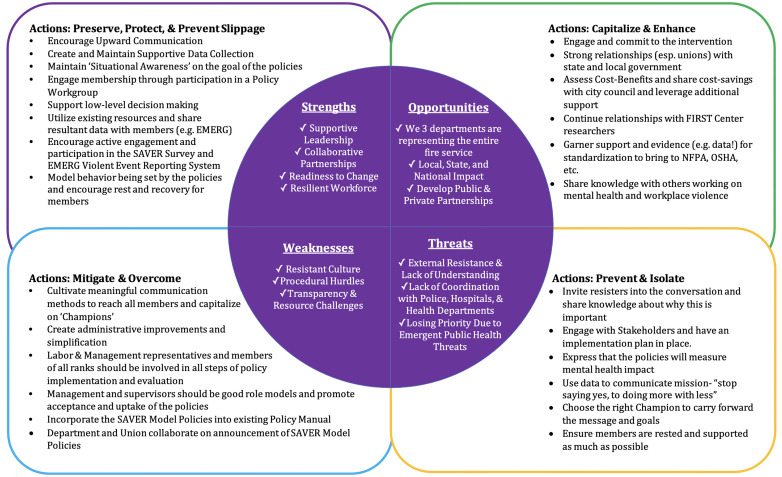
Action SWOT Analysis of Model Policy Implementation
The SWOT analysis took four hours, included seventeen participants, four facilitators, four logistical assistants, and ten research team observers. The raw SWOT results elicited thirty-five internal strengths and seventy actions to preserve and protect them; twenty-two internal weaknesses and twenty actions to mitigate and overcome them; nineteen external opportunities and fifteen actions to capitalize and enhance them; and, twenty-four external threats and twenty-seven actions to prevent and isolate them. Participant elicitations were deduplicated, prioritized, and grouped into themes for each dimension. The results are summarized in Figure 4. Ideas to ensure successful policy implementation were summarized as action items.
Figure 4.
SWOT analysis results.
Strengths. Four themes emerged during the discussion of the internal strengths associated with adopting the SAVER Model Policies.
Supportive Leadership
Collaborative Partnerships
Readiness to Change
Resilient Work force
These themes speak to the existing organizational capacity to implement the model policies and desire to create a positive culture of safety by both leadership and the membership. These themes further capture the progressive, innovative, and forward-thinking perspectives of the study site representatives. Collectively, there was an overwhelming response that the SAVER Model Policies send a message to members of all levels that health and safety is prioritized.
Action Items. Four action items were identified to preserve and protect the strengths:
Encourage upward communication
Create and maintain supportive data collection
Maintain ‘situational awareness’ on the goal of the policies
Engage membership through participation in a Policy Work group
These action items capitalize on the positive culture and buy-in that is already present in departments. It is through supportive leadership and collaborative partnerships that departments can express to their members the importance of these policies to their health, safety, and well-being. Departments can keep all entities focused on the goal by sharing project updates and data back with members. This “give-back” helps members to feel heard and that their participation in initiatives is meaningful and worthy of their time and commitment.
Weaknesses. Three themes emerged during the discussion of the internal weaknesses associated with policy adoption.
Resistant Culture
Procedural Hurdles
Transparency & Resource Challenges
While all three departments referenced strong, supportive leadership during the strengths, they also mentioned that there is some resistance to changing the overall culture of the department. Resistance was often discussed using terms such as “pride” and “tradition” and “that's the way it's always been.” Concerns were also raised that there is a lack of knowledge about what the policies are meant to accomplish, and therefore members attempting to enact the policies will run into a lot of procedural “red tape.” Furthermore, the success of the policies are dependent on many factors and some members expressed that lack of transparency, lack of resources, and lack of accountability could impact implementation.
Action Items
Cultivate meaningful communication
Create administrative improvements and simplification
Inclusion of labor, management, and all ranks in process
The creation of a professional, safe, and respectful work environment should prioritize communication, administrative simplification, and inclusion of all members regardless of rank. Through these continuous methods of engagement and modeling desired behaviors, leadership can create a culture of acceptance. The SAVER Model Policies should be seen as supportive—not just another protocol they must follow. The policies are being implemented by leadership and management. The six SAVER Pause Points are the only responsibility that members have.
Opportunities. Three themes emerged during the discussion of the external opportunities associated with policy adoption.
Earlier adopter departments are representing the fire and rescue service
The policies will have Local, State, and National Impact
Develop Public & Private Partnerships
These themes highlight the potential for department benefits, community health advancements, and a multi-level societal impact. The SAVER Model Policies will be evaluated to assess their impact on EMS responder safety and health. This will create an opportunity to develop and strengthen relationships with professions and groups working in mental health, local and state governments, and community partners. Implementation will create a best practice for other departments to use and will inform national standards to address workplace violence.
Action Items
Engage and commit to the intervention
Garner evidence to support standardization
Share cost-savings to encourage wider adoption
These action items are critical to capitalize on the implementation of the SAVER Model Policies. Collaboration across sectors and fields will help promote the impact of the policies. By sharing this knowledge with people in the broader community, a foundation for wide-scale implementation of these practices will be established.
Threats. Three themes emerged during the discussion of the external threats associated with policy adoption.
External Resistance & Lack of Understanding
Lack of Coordination with Police, Hospitals, & Health Departments
Losing priority due to emergent public health threats
Threats to implementation speak to the challenges faced external to the department. There exists a concerning level of resistance and lack of understanding from external entities (e.g., Legal, Risk Management, and politicians) that have the potential to delay or derail implementation of the SAVER Model Policies. There is also a lack of coordination between organizations that EMS is reliant on—police and hospitals. Another challenge to effective implementation are the ever-evolving public health threats and public emergencies (e.g., Coronavirus).
Action Items
Invite conversations with resisters
Stakeholder engagement
Express that the policies will impact mental health
To address threats to the implementation of these eight model policies, a proactive plan must be initiated and shared with partners. By inviting resisters into the conversation, their concerns can be heard and addressed. Prioritization can become an issue during emerging public health concerns (e.g., Coronavirus), which amplifies the need for consistent messaging and training, as well as public health education on the issues facing the emergency response system.
Evaluation Results
Participants positively regarded the process, with all evaluation questions receiving 100 percent scores for “Agree/Strongly agree” (data not shown). The combination of ThinkLets and the Action SWOT analysis elicited feedback citing efficiency and open conversation as hallmarks of the SAVER Model Policy Collaborative. Participants felt united by the process, developing a solidarity in their approach to the core problem.
When asked What part of this collaborative did you enjoy the most? Why?
“The SWOT Analysis, going over it together, I find it interesting and educating to listen to other departments and hear they also have the same issues, but sometimes a better way to solve.”
“I enjoyed the SWOT the most It helped with this project and gave me new job skills.”
“I always love hearing that my department is not the “only one”. Collaborative efforts are effective, and I have a renewed sense of belonging within my department.”
“Watching everything come together. It was outstanding seeing different views and learning from them.”
“The efficiency of the meeting process and amount of information provided and shared by other members of the departments. The information provided in this project will be useful for myself and my own well-being as I strive to be an advocate to my department and peers to implement the policy for the overall health of EMS providers.”
Discussion
Currently only a handful of the existing 30,000 fire and rescue departments have any kind of organizational procedure or policy related to violence. In response, we developed the SAVER Model Policies and critically pre-meditated implementation efficacy using ThinkLets, which yielded a two-day process that otherwise would have taken fifty-two meetings to complete. While the bulk of policy adoption falls to fire department and union leadership, the six pause points challenge and reimagine the traditional para-military culture that exists in the fire and rescue service by allowing the people doing the day-to-day work to speak up and give feedback on system defects. In essence, this gives fire departments extra sets of eyes on hazard remediation that will in turn make the job safer for everyone.
The intention of the SAVER Model Policies is that fire departments will adopt the policies as a compendium, meaning that all eight policies will be integrated into their existing Standard Operating Procedures (SOPs). The Model Policies build upon one another, and taken as a whole, express to membership that leadership in an organization cares about their safety during EMS response and values their contribution to the organization. There are multiple prompts throughout the Model Policies where fire departments are encouraged to tailor an item to their local work environment, hence the “model” descriptor. For example, in Model Policy #6: Readiness to Return to Service, the following prompt is given to reflect certain hazards that are experienced in a department's local environment (e.g., specific drug hazards (“wet,” fentanyl), specific call types (e.g., domestic violence), specific populations (e.g., homeless youth):
6.4 Supervisors will offer wellness check-ins following certain calls or circumstances that may impact EMS responders. [insert department-specific Policy/SOP/SOG for ‘certain calls’]
Each fire department in the United States will have a different definition of what calls warrant a “wellness check-in” of their members. Rather than providing detailed instructions in the Model Policy, departments are encouraged to link to other pre-existing SOPs that will provide further clarification to this item. There are also fire departments that will have no pre-existing SOP to address wellness check-ins following certain call types. In this way the SAVER Model Policies act as a prompt for leadership to recognize gaps in their policies which could help to support their membership during EMS response. Fire department leadership can also consider including non-officer firefighters, paramedics, EMTs, and dispatchers on a policy adoption committee at the adaptation phase so that local modifications include guidance and input from the frontline.
As with any new policy adoption in an organization, there are potential challenges that should be premeditated prior to implementation. The SAVER study sites illuminated potential “weaknesses” and “threats” to implementation when they conducted the SWOT analysis (Figure 4). Of paramount importance is consistent communication and training on the policies in order for them to be effective. Simply putting the SAVER Model Policies in a binder will not create change.
The SAVER Model Policies were constructed to be used by the U.S. fire and rescue service, but since they are grounded in a large body of evidence on the utility of checklists,33,34 we believe the SAVER Model Policies and their parent Systems-Level Checklist 34 could be easily modified for use in other industries—nationally and internationally. The next steps are to evaluate the impact of these policies on violence and mental health outcomes of those they were designed to protect. Fire departments interested in implementing the policies can contact the authors for assistance.
Research Materials Statement
The authors are happy to share materials and data with interested parties provided that they meet IRB conditions.
Supplemental Material
Supplemental material, sj-docx-1-new-10.1177_10482911221085728 for Model Policies to Protect U.S. Fire-Based EMS Responders From Workplace Stress and Violence by Jennifer A. Taylor, Regan M. Murray, Andrea L. Davis, Sherry Brandt-Rauf, Joseph A. Allen, Robert Borse, Diane Pellechia and David Picone in NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy
Supplemental material, sj-docx-2-new-10.1177_10482911221085728 for Model Policies to Protect U.S. Fire-Based EMS Responders From Workplace Stress and Violence by Jennifer A. Taylor, Regan M. Murray, Andrea L. Davis, Sherry Brandt-Rauf, Joseph A. Allen, Robert Borse, Diane Pellechia and David Picone in NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy
Acknowledgments
For assistance organizing and facilitating the SAVER Model Policy Collaborative, we extend our gratitude to: Drexel FIRST Center Research Assistants: Alexandra Eastus, Kelly McLaughlin, Katherine Castro, Alexandra Trautman Fisher, and Victoria Gallogly, as well as FIRST Center Affiliate Faculty Dr. Jin Lee (Kansas State University) and Dr. Christian Resick (Drexel University). The authors extend their appreciation to the following participants of the SAVER Model Policy Collaborative: Dallas Fire-Rescue Department (Robert Borse, Justin Lovvorn, Clinton Demond Page, Charlie Salazar, George Gamez); Philadelphia Fire Department (Diane Pellechia, Jacqulyn Murphy, Nashia Roper, Tommy McKiernan, Theodore Heintzelman, and Kevin Carey); San Diego Fire-Rescue Department and American Medical Response (Cory Beckwith, Dan Froelich, Ted Chialtas, Jeri Mucio, Tracy Lynn, Kirsten Rich, Richard Goulet).
Author Biographies
Jennifer A. Taylor, PhD, MPH, CPPS, is an injury epidemiologist and the Arthur L. and Joanne B. Frank Professor of Environmental and Occupational Health at the Drexel University Dornsife School of Public Health in Philadelphia, PA. Dr. Taylor is the founding director of the FIRST Center at Drexel University. She received her doctorate from Johns Hopkins Bloomberg School of Public Health, specializing in Injury Prevention and Control, where she received the Haddon Fellowship and the ERC-NIOSH Training Fellowship in Occupational Injury. Dr. Taylor's research investigates the impact of safety climate on occupational injury and related psychosocial outcomes among first responders.
Regan M. Murray is a certified emergency medical technician and served as the FIRST Center project manager of the “Stress and Violence in fire-based EMS Responders (SAVER)” grant from 2017 to 2020. Ms. Murray received her Bachelor of Arts degree from St. Lawrence University and her Master of Public Health degree, concentrating in Community Health and Prevention, from Drexel University. She is currently the assistant director of the Center for Media, Technology, and Health in the Department of Health, Human Performance and Recreation at the College of Education and Health Professions at the University of Arkansas.
Andrea L. Davis, MPH, CPH is the senior project manager at the FIRST Center. She earned her Master of Public Health degree from Drexel University in 2012 and holds the designation of Certified in Public Health from the National Board of Public Health Examiners. Ms. Davis holds a Master of Liberal Arts degree from the Harvard University Extension School and Bachelor of Art from the University of Delaware. Ms. Davis's research focuses on safety climate and its impact on firefighter mental health and injury.
Sherry Brandt-Rauf, MPhil, JD, is an associate teaching professor of Environmental and Occupational Health and Affiliate Faculty of the FIRST Center at Drexel University. She completed her master and juris doctorate degrees at Columbia University. Her research focuses on the policy interface between law and occupational safety and health and currently focuses on the ways in which the law shapes the health and safety of first responders.
Joseph A. Allen, PhD, is a professor in Industrial and Organizational Psychology and the director for the Center for Meeting Effectiveness at the University of Utah. He completed his doctorate in Organizational Science at the University of North Carolina at Charlotte in 2010 and received his Master of Arts degree in Industrial and Organizational Psychology at the UNCC in 2008. Dr. Allen's research focuses on three major areas of inquiry including the study of work-place meetings, non-profit organizational effectiveness, and emotional labor in various service-related contexts.
Administrative Lieutenant Robert Borse, Dallas Fire-Rescue Department, served the study site champion for the SAVER grant in Dallas, TX. He is the chairperson of Dallas Fire-Rescue EMS Council and an Adjunct Instructor at Dallas Fire-Rescue. He received his BA from the University of Dallas.
Lieutenant Diane Pellecchia is a paramedic with the City of Philadelphia Fire Department and served the study site champion for the SAVER grant in Philadelphia, PA.
Battalion Chief David Picone is the health and safety officer for the City of San Diego Fire-Rescue Department, served the study site champion for the SAVER grant in San Diego, CA. He received his BA in Vocation Education, Fire Management and Science from California State Long Beach. He was named “Safety Officer of the Year” in 2020 by the Fire Department Safety Officers Association.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Federal Emergency Management Agency (FEMA) FY 2016 Assistance to Firefighters Grant Program, Fire Prevention and Safety Grants (Research & Development); Grant number: EMW-2016-FP-00277.
ORCID iDs: Jennifer A. Taylor https://orcid.org/0000-0002-1929-4454
Regan M. Murray https://orcid.org/0000-0001-7396-6517
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Evarts B, Stein GP. US Fire Department Profile 2018 . National Fire Protection Association 2020, February. https://www.nfpa.org/-/media/Files/News-and-Research/Fire-statistics-and-reports/Emergency-responders/osfdprofile.pdf (accessed 1 September 2021).
- 2.The National Association of State EMS Officials. National EMS Assessment, 2011.
- 3.National Fire Protection Association. Fire Department Calls. https://www.nfpa.org/News-and-Research/Data-research-and-tools/Emergency-Responders/Fire-department-calls, 2018.
- 4.Taylor JA, et al. Expecting the unexpected: a mixed methods study of violence to EMS responders in an urban fire department. AJIM 2016; 59: 150–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maguire BJ, et al. Occupational injuries among emergency medical services personnel. Prehosp Emerg Care 2005; 9: 405–411. [DOI] [PubMed] [Google Scholar]
- 6.Maguire BJ, et al. Occupational fatalities in emergency medical services: a hidden crisis. Ann Emerg Med 2002; 40: 625–632. [DOI] [PubMed] [Google Scholar]
- 7.Patterson PD, et al. Association between poor sleep, fatigue, and safety outcomes in emergency medical services providers. Prehosp Emerg Care 2012; 16: 86–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patterson PD, et al. Recovery between work shifts among emergency medical services clinicians. Prehosp Emerg Care 2015; 19: 365–375. [DOI] [PubMed] [Google Scholar]
- 9.Weaver MD, et al. An observational study of shift length. Crew familiarity, and occupational injury and illness in emergency medical service workers. Occ Env Med 2015; 72: 798–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexander DA, Klein S. Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. Br J Psychiatry 2001; 178: 76–82. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz RJ, Benson L, Jacobs LM. The prevalence of occupational injuries in EMTs in New England. Prehosp Disaster Med 1993; 8: 45–50. [DOI] [PubMed] [Google Scholar]
- 12.Donnelly E, Siebert D. Occupational risk factors in the emergency medical services. Prehosp Disaster Med 2009; 24: 422–429. [DOI] [PubMed] [Google Scholar]
- 13.Grevin F. Posttraumatic stress disorder, ego defense mechanisms, and empathy among urban paramedics. Psychol Rep 1996; 79: 483–495. [DOI] [PubMed] [Google Scholar]
- 14.Marmar C, et al. Stress responses of emergency services personnel to the Loma Prieta earthquake interstate 880 collapse and control traumatic incidents. J Traum Stress 1996; 9: 63–85. [DOI] [PubMed] [Google Scholar]
- 15.Jonsson A, Segesten K, Mattsson B. Post-traumatic stress among Swedish ambulance personnel. Emerg Med J 2003; 20: 79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clohessy S, Ehlers A. PTSD Symptoms, response to intrusive memories and coping in ambulance service workers. Br J Clin Psychol 1999; 38: 251–265. [DOI] [PubMed] [Google Scholar]
- 17.Newland C, Barber E, Rose M, et al. What’s killing our medics?. http://www.revivingresponders.com/s/Whats-Killing-Our-Medics-Final-ub4v.pdf, 2015 [PubMed]
- 18.Sterud T, Ekeberg O, Hem E. Health status in the ambulance services: a systematic review. BMC Health Serv Res 2006; 6: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stanley IH, et al. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev 2016; 44: 25–44. doi: 10.1016/j.cpr.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Bigham BL, et al. Paramedic self-reported exposure to violence in the emergency medical services (EMS) workplace: a mixed- methods cross-sectional survey. Prehosp Emerg Care 2014; 18: 489–494. [DOI] [PubMed] [Google Scholar]
- 21.Nordberg M. In harm’s way. Emerg Med Serv 1992; 21, 23–29, 32, 38-9. [PubMed] [Google Scholar]
- 22.Federiuk CS, et al. Job satisfaction of paramedics the effects of gender and type of agency of employment. Ann Emerg Med 1992; 22: 657–662. [DOI] [PubMed] [Google Scholar]
- 23.Patterson PD, et al. Variation in emergency medical services workplace safety culture. Prehosp Emerg Care 2010; 14: 448–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fahy RF, Molis JL. Firefighter fatalities in the United States. (updated June 2020). National Fire Protection Association. https://www.nfpa.org/News-and-Research/Data-research-and-tools/Emergency-Responders/Firefighter-fatalities-in-the-United-States/Firefighter-deaths, 2019
- 25.Barber E, Newland C, Young A, et al. Survey reveals alarming rates of EMS provider stress and thoughts of suicide. JEMS 2015; 40: 30–34. [PubMed] [Google Scholar]
- 26.Lulla A, Tian L, Moy HP, et al. The EMS suicide threat: new research finds alarmingly high rates of ideation and risk. EMS World 2020; 49: 46–48. [Google Scholar]
- 27.Cannuscio CC, et al. A strained 9-1-1 system and threats to public health. J Community Health 2016; 41: 658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pozzi C. Exposure of prehospital providers to violence and abuse. J Emerg Nurs 1998; 24: 320–323. [DOI] [PubMed] [Google Scholar]
- 29.Gomez-Gutierrez MM, et al. Posttraumatic stress symptomatology in prehospital emergency care professionals assaulted by patients and/or relatives: importance of severity and experience of the aggression. J Interpers Violence 2016; 31: 339–354. [DOI] [PubMed] [Google Scholar]
- 30.Maguire BJ, Smith S. Injuries and fatalities among emergency medical technicians and paramedics in the United States. Prehosp Disaster Med 2013; 28: 376–382. [DOI] [PubMed] [Google Scholar]
- 31.Murray RM, Davis AL, et al. Systematic review of workplace violence against emergency medical services (EMS) responders in the pre-hospital setting. New Solut: J Environ Occup Health Policy 2020; 29: 487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taylor JA, Davis AL, et al. Development and validation of the fire service safety climate scale. Saf Sci 2019; 118: 126–144. [Google Scholar]
- 33.Gawande A. The checklist manifesto: how to Get things right. New York: Picador, 2010. [Google Scholar]
- 34.Taylor JA, et al. Creation of a systems-level checklist to address stress and violence in fire-based EMS responders. Occup Health Sci 2019; 3: 265–295. [PMC free article] [PubMed] [Google Scholar]
- 35.Demerouti E, Bakker AB, Nachreiner F, et al. The job demands-resources model of burnout. J App Psy 2001; 86: 499–512. [PubMed] [Google Scholar]
- 36.Murray RM, Allen JA, et al. “Meeting science meets public health: results from the ‘‘stress and violence in fire-based EMS responders (SAVER) systems checklist consensus conference (SC3)”. J Saf Res 2020;74: 249–261. doi: 10.1016/j.jsr.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Christian MS, et al. Workplace safety: a meta-analysis of the roles of person and situation factors. J App Psy 2009; 94: 1103–1127. [DOI] [PubMed] [Google Scholar]
- 38.Huang Y, et al. Beyond safety outcomes: an investigation of the impact of safety climate on job satisfaction, employee engagement and turnover using social exchange theory as the theoretical framework. Appl Ergon 2016; 55: 248–257. [DOI] [PubMed] [Google Scholar]
- 39.Taylor JA, et al. Triangulating case-finding tools for patient safety surveillance: a cross- sectional case study of puncture/laceration. Injury Prevent 2011; 17: 388–393. [DOI] [PubMed] [Google Scholar]
- 40.Selye H. 1. History and Present Status of the Stress Concept. In Stress and coping: An anthology. New York: Columbia University Press, 1991, pp.21–35. [Google Scholar]
- 41.Cannon WB. The wisdom of the body. New York: Norton & Co, 1932, 312. [Google Scholar]
- 42.Mobley WH. Intermediate linkages in the relationship between job satisfaction and employee turnover. J App Psy 1997; 62: 237–240. [Google Scholar]
- 43.Cresswell SL, Eklund RC. Motivation and burnout among top amateur rugby players. Med Sci Sports Exerc 2005; 3: 469–477. [DOI] [PubMed] [Google Scholar]
- 44.Halbesleben JR. A meta-analysis of work engagement: relationships with burnout, demands, resources, and consequences. In Bakker AB and Leiter MP (eds) Work engagement: a handbook of essential theory and research, Vol. 8. New York: Psychology Press, 2010, 102−117. [Google Scholar]
- 45.Bal PM, et al. Dynamics of psychological contracts with work engagement and turnover intention: the influence of organizational tenure. Eur J Work Org Psy 2013; 22: 107–122. [Google Scholar]
- 46.Schaufeli W, Bakker A. Job demands, job resources, and their relationship with burnout and engagement: a multi-sample study. J Organ Behav 2004; 25: 293–315. [Google Scholar]
- 47.Swaen G, et al. Psychosocial work characteristics as risk factors for being injured in an occupational accident. J Occup Environ Med 2004; 46: 521–527. [DOI] [PubMed] [Google Scholar]
- 48.Nahrgang JD, et al. Safety at work: a meta-analytic investigation of the link between job demands, job resources, burnout, engagement, and safety outcomes. J App Psy 2011; 96: 71–94. [DOI] [PubMed] [Google Scholar]
- 49.Gok A. Decision-making under stress and its implications for managerial decision-making: a review of literature. Int J Bus 2016; 6: 38–47. [Google Scholar]
- 50.Collopy KT, Kivlehan SM, Snyder SR. Are you under stress in EMS. Understanding the slippery slope of burnout and PTSD. EMS World 2012; 41: 47–50. [PubMed] [Google Scholar]
- 51.Katsavouni F, Bebetsos E, Malliou P, et al. The relationship between burnout, PTSD symptoms and injuries in firefighters. Occup Med 2016; 66: 32–37. [DOI] [PubMed] [Google Scholar]
- 52.Lee JY, et al. The association of gratitude with perceived stress and burnout among male firefighters in Korea. Pers Individ Dif 2018; 123: 205–208. [Google Scholar]
- 53.Murphy S, et al. Firefighters and paramedics: years of service, job aspirations, and burnout. AAOHN J 1994; 42: 534–540. [PubMed] [Google Scholar]
- 54.Vigil NH, et al. Death by suicide—The EMS profession compared to the general public. Prehosp Emerg Care 2019; 23: 340–345. [DOI] [PubMed] [Google Scholar]
- 55.Edwards DL, Wilkerson ND. Emotional exhaustion and its relationship with suicide risk in emergency responders. Psychiatry Res 2020; 293: 113379. [DOI] [PubMed] [Google Scholar]
- 56.De Vreede GJ, Kolfschoten GL, Briggs O. Thinklets: a collaboration engineering pattern language. Int J Comput Appl Technol 2006; 125: 140–154. [Google Scholar]
- 57.Kolfschoten GL, et al. A conceptual foundation of the ThinkLet concept for Collaboration Engineering. Int J Hum Comput Stud 2006; 64: 611–621. [Google Scholar]
- 58.Steinhauser L, Read A, de Vreede GJ. Studying the adoption of collaborative work practices using the value frequency model. MWAIS 2008 Proceedings, 3, 2008. [Google Scholar]
- 59.Tracy JS. Qualitative research methods: collecting evidence, crafting analysis, communicating impact. Hoboken. NJ: Wiley-Blackwell, 2013. [Google Scholar]
- 60.Foundation PH. “Stop analysis paralysis! Use an “Action SWOT” as part of your problem solving approach.” Originally published in the Process Excellence Network Newsletter. December 2013; 2. https://www.processexcellencenetwork.com. (April 27, 2019). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-new-10.1177_10482911221085728 for Model Policies to Protect U.S. Fire-Based EMS Responders From Workplace Stress and Violence by Jennifer A. Taylor, Regan M. Murray, Andrea L. Davis, Sherry Brandt-Rauf, Joseph A. Allen, Robert Borse, Diane Pellechia and David Picone in NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy
Supplemental material, sj-docx-2-new-10.1177_10482911221085728 for Model Policies to Protect U.S. Fire-Based EMS Responders From Workplace Stress and Violence by Jennifer A. Taylor, Regan M. Murray, Andrea L. Davis, Sherry Brandt-Rauf, Joseph A. Allen, Robert Borse, Diane Pellechia and David Picone in NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy