Abstract
Electrocardiographic findings including irregularity of the rhythm, a very rapid ventricular response, and the presence of a delta wave should raise the suspicion of pre‐excited atrial fibrillation with a rapid ventricular response. Urgent cardioversion is needed due to the risk of sudden cardiac death.
Keywords: accessory pathway, atrial fibrillation, sudden cardiac death, Wolff–Parkinson–White syndrome
Electrocardiographic findings including irregularity of the rhythm, a very rapid ventricular response, and the presence of a delta wave should raise the suspicion of pre‐excited atrial fibrillation with a rapid ventricular response. Urgent cardioversion is needed due to the risk of sudden cardiac death.

1. CLINICAL IMAGE
A 37‐year‐old man was admitted to the emergency department of our hospital complaining of palpitations and dizziness that started an hour ago. His past medical history was unremarkable. His blood pressure was 95/45 mmHg in the supine position, while the oxygen saturation was 97%. In the physical examination, the patient had a Glasgow Coma Scale of 15/15, while the inspection revealed cold, pale, and clammy skin. The cardiac auscultation revealed an abnormally fast and irregular heart rate, and an electrocardiogram (ECG) was immediately obtained (Figure 1A).
FIGURE 1.
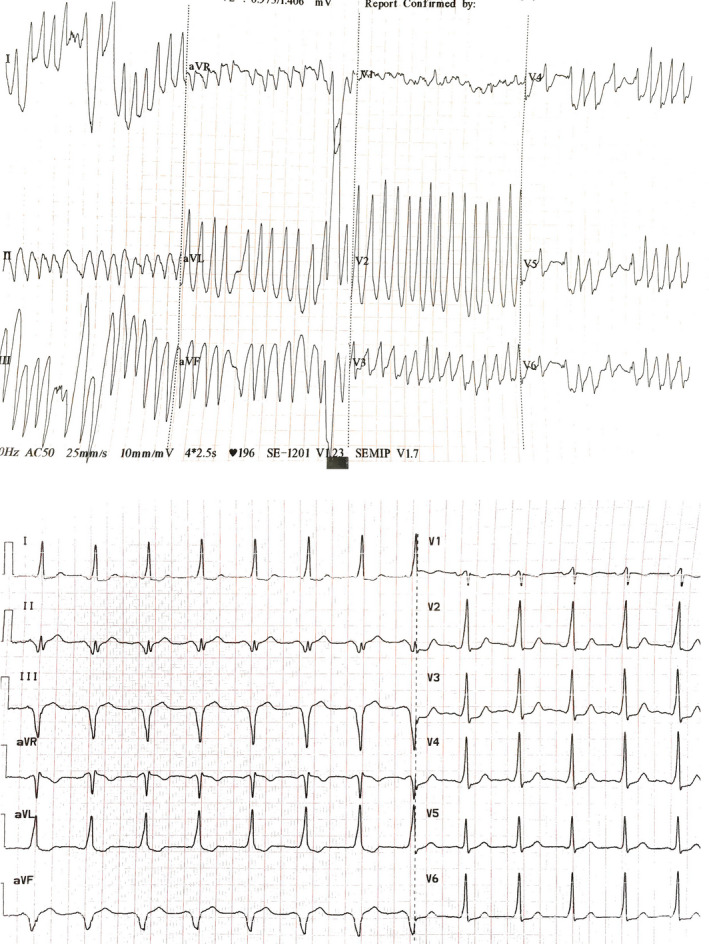
(A) (top) The initial electrocardiogram of the patient at the emergency department. (B) (bottom) Normal sinus rhythm with pre‐excitation was revealed in the electrocardiogram following the cardioversion
2. WHAT IS YOUR DIAGNOSIS?
Atrial fibrillation with anterograde conduction over an accessory pathway with a rate exceeding 200 pulses per minute was diagnosed, and urgent synchronized cardioversion at 150 J was performed under midazolam‐induced sedation. Normal sinus rhythm with pre‐excitation was revealed in the ECG following the cardioversion (Figure 1B). A posteroseptal localization of the accessory pathway was predicted using the R/S ratio in leads V1 and V2. 1 The patient was admitted to the intensive care unit, and an electrophysiological study was performed. An early signal with a clear accessory pathway potential was mapped within the coronary sinus at the ostium of the middle cardiac vein. Radiofrequency ablation was applied with power limited to 25 W and resulted in right posteroseptal accessory pathway elimination within 2.3 s. No evidence of pathway reconnection following 40 min waiting period was observed.
In conclusion, on an emergency basis, urgent cardioversion is the cornerstone for achieving a better outcome due to the risk of ventricular fibrillation and sudden cardiac death.
AUTHOR CONTRIBUTIONS
George Bazoukis involved in management of the patient, writing the first draft, major revisions, and approval of the final manuscript. Elias Papasavvas, Michalis Tsielepis, Lorentzos Kapetis, Panagiota Georgiou, Dimitrios Patestos, and Marios Pavlou involved in management of the patient, major revisions, and approval of the final manuscript. Konstantinos Vlachos, Konstantinos P. Letsas, Michael Efremidis, and Athanasios Saplaouras involved in major revisions and approval of the final manuscript.
CONFLICT OF INTEREST
The authors declare no conflicts of interest related to the manuscript.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENT
None.
Bazoukis G, Papasavvas E, Pavlou M, et al. Atrial fibrillation and Wolff–Parkinson–White syndrome: A double blow for the cardiologist. Clin Case Rep. 2022;10:e06035. doi: 10.1002/ccr3.6035
DATA AVAILABILITY STATEMENT
All data are available upon request.
REFERENCES
- 1. Taguchi N, Yoshida N, Yamamoto T, et al. Abstract 9410: a simple and accurate algorithm for localizing accessory pathways in patients with Wolff‐Parkinson‐white syndrome. Circulation. 2011;124:A9410. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available upon request.


