Abstract
Background:
The Indonesian government initiated National Health Insurance (NHI) to reduce health service barriers. The study aimed to analyze specific targets for expanding the NHI’s membership in Indonesia.
Methods:
The study population was all populations in Indonesia. Meanwhile, the study involved a 47 644 weighted sample. The analyzed variables included NHI’s membership, residence, age, gender, education, employment, marital status, and wealth. The study employed binary logistic regression in the final step.
Results:
The urban population was 0.608 times less likely than the rural population to become a non-member of NHI. Aging younger was one of the barriers to becoming an NHI member, and the male gender is one of the barriers to becoming an NHI member. Meanwhile, the lower the education level, the greater the obstacles to becoming an NHI member in Indonesia. Besides, the unemployed population was 1.002 more likely than the employed population to become a non-member of NHI. The result shows that never married or married have a higher chance of becoming a non-member of NHI. Finally, all wealth status categories are more likely to become barriers to the most prosperous population becoming an NHI member.
Conclusions:
The study concluded that 7 population characteristics become specific targets for expanding NHI membership in Indonesia. The 7 characteristics are the population who live in rural areas, are young, male, poor education, unemployed, never married or married, and poor.
Keywords: health insurance, National Health Insurance, health policy, big data, population survey, public health
Introduction
In Indonesia, the National Health Insurance (NHI) policy strives to provide the fundamental needs of good public health for everyone who has paid dues or whose contributions are covered by the government. As a result, all Indonesian citizens, including foreigners who have worked in Indonesia for at least 6 months and paid dues, must join the NHI Program, which the Health Social Security Administering Agency (HSSAA) administered.1,2
By 2020, 222.5 million individuals will have signed up for the NHI, equating to 81.3% of Indonesia’s total population. According to the NHI Program’s plan, Indonesia Government has said that Universal Health Coverage (UHC) will be achieved by the end of 2019. Universal participation or all Indonesians have joined the NHI is one indication for UHC. As a result, around 18.7% of the population remains uninsured under NHI. 3 Furthermore, 2019 has passed, and the empirical facts state that UHC has not yet materialized. The government needs even more strenuous efforts to make all people in Indonesia covered by the NHI. The government needs to understand the barriers for people to becoming members of the NHI.
NHI membership consists of CARs (contribution assistance recipients) and non-CARs (non-contribution assistance recipients). As specified by Law No. 40 of 2004 concerning the National Social Security System, people defined as poor and underprivileged whose payments are paid by the government as participants in the NHI program are eligible to participate in the CAR. CAR participants get funding from the State Revenue and Expenditure Budget and the Regional Revenue and Expenditure Budget. 1 The total number of participants in the CAR group was 132.8 million. 3
On the other hand, the regulation classed non-CAR participants as not poor or privileged and made their contributions to HSSAA individually or collectively. These participants can pay through payroll deductions or monthly payments to HSSAA with a premium amount determined by their class participation.1,4 At the end of 2020, the non-CAR category includes 55.1 million people who have premiums taken from their paychecks and 35.3 million self-employed people. 3
The number of participants contributes to the number of HSSAA admissions. In reality, HSSAA often runs a budget deficit, and the expenditure is not proportional to revenue. Furthermore, one of the continuous efforts is to increase the number of participants and participation in premium payments. The situation is inseparable from the attitude of public acceptance to be willing to become an NHI member and comply with premium payments following provisions.4 -6
Previous studies have confirmed several variables that contribute to premium compliance, that is, family members, financial difficulties, participation in other insurance, knowledge of health insurance schemes, and availability of health workers.4,7 -9 The study also finds different drivers in each region. It suggests that policy designs must consider these differences, as effective in one area may not be effective in another location. 10 Moreover, previous studies also indicate that ownership of health insurance can increase public access to health services.11 -13
The government does not just create and implement NHI policy. Both approaches include community engagement. In a democratic democracy, the community’s role is more than just that of a target and policy advocate; it is, nonetheless, a determinant of the policy’s success. As a result, a membership study focusing on the elements contributing to NHI membership is required to ensure the program’s long-term viability. The study analyzed specific targets for expanding the NHI’s membership in Indonesia based on the background.
Materials and Methods
Data Source
The survey was a national-scale survey conducted by the Ministry of Health of the Republic of Indonesia. The research employed secondary data from a previous study (“Abilities and Willingness to Pay, Fee, and Participant Satisfaction in implementing National Health Insurance in Indonesia in 2019”). Meanwhile, the study population was all residents of Indonesia. The study described 47 644 weighted sample participants as research respondents through stratification and multistage random sampling. With this sampling method, the study results are a national representation, involving 715 districts, 1430 villages, and 14 300 households in all Indonesian provinces (34 provinces).
The survey conducted data collection from March to December 2019. The study used household and individual instruments to assess participant characteristics, health insurance ownership, and NHI membership.
Variables
The study employed National Health Insurance (NHI) membership as the dependent variable. NHI membership applies to the respondent’s presence in the NHI, whether as an individual member, a required member (civil servant, police, army), borne by the company, or an NHI. There are 2 types of NHI membership: non-member and member. As independent variables, the analysis used 7 variables. The 7 variables were age group, gender, education level, employment status, marital status, and wealth status. There are 2 forms of residence available: urban and rural. The study split the age group into 3 classes in the sample: ≤17, 18 to 64, and ≥65. Meanwhile, the research classified gender into 2 categories: male and female. There were 4 levels of education: no education, primary, secondary, and higher education. Moreover, there are 2 types of job status: unemployed and employed. Furthermore, the study divided marital status into 3 categories: never married, married, and divorced/widowed.
The study used the wealth index formula to assess wealth status. The wealth index was a weighted estimate of a household’s total spending. Meanwhile, the wealth index was determined using primary data on households’ spending, such as health insurance, food, lodging, and other products. Furthermore, the survey divided the income index into 5 categories: the poorest (quintile 1), poorer (quintile 2), middle (quintile 3), richer (quintile 4), and the richest (quintile 5).14,15
Data Analysis
The study used the Chi-Square test in the initial stage of the sample to make a bivariate comparison. Furthermore, the study employed a collinearity test to ensure no intense correlation between independent variables in the resulting regression model. The research used a binary logistic regression in the study’s final point. The survey carried out this test to explore the multivariable relationship between all independent variables and NHI membership as the dependent variable. The study used the IBM SPSS 26 program for the entire statistical analysis process.
On the other hand, the research used ArcGIS 10.3 (ESRI Inc., Redlands, CA, USA) to map NHI membership distribution by the province in Indonesia in 2019. The study issued a shapefile of administrative boundary polygons by the Indonesian Bureau of Statistics for the task.
Results
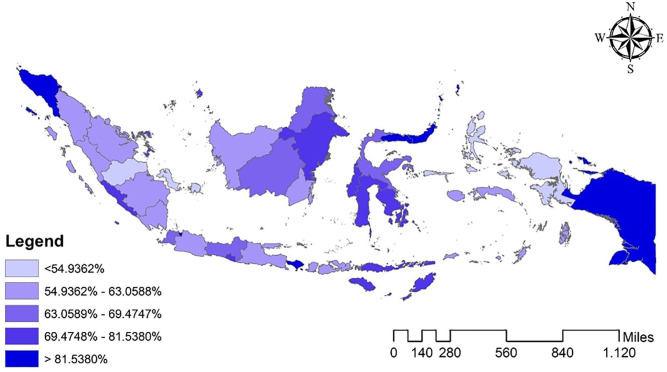
Figure 1 shows the distribution map of NHI membership by the Province in Indonesia. The figure shows the random distribution. Moreover, there is no specific pattern that can indicate a spatial trend.
Figure 1.
Distribution map of NHI membership by the Province in Indonesia in 2019 (n = 47 644).
Table 1 shows the results of descriptive statistics of NHI membership in Indonesia. The work shows the rural area population tends to rule the non-member NHI group based on residence type. The people in the 18 to 64 age group occupied the non-member NHI group regarding age groups. Based on education level, the population in secondary education controls the non-member NHI group.
Table 1.
Descriptive Statistic of NHI Membership in Indonesia (n = 47 644).
| Characteristics | NHI membership | P-value | |
|---|---|---|---|
| Member (n = 32 283) (%) | Non-member (n = 15 361) (%) | ||
| Type of residence | <.001 | ||
| Urban | 31.2 | 20.3 | |
| Rural | 68.8 | 79.7 | |
| Age | <.001 | ||
| ≤17 | 27.0 | 35.2 | |
| 18-64 | 66.5 | 59.6 | |
| ≥65 | 6.5 | 5.1 | |
| Gender | <.001 | ||
| Male | 50.1 | 50.7 | |
| Female | 49.9 | 49.3 | |
| Education level | <.001 | ||
| No education | 13.1 | 21.3 | |
| Primary | 56.6 | 56.8 | |
| Secondary | 24.0 | 18.9 | |
| Higher | 6.3 | 3.0 | |
| Employment status | <.001 | ||
| Unemployed | 51.6 | 56.7 | |
| Formal | 48.4 | 43.3 | |
| Marital status | <.001 | ||
| Never married | 42.0 | 47.5 | |
| Married | 51.7 | 47.1 | |
| Divorced/widowed | 6.3 | 5.4 | |
| Wealth status | <.001 | ||
| Poorest | 19.0 | 22.2 | |
| Poorer | 19.8 | 20.3 | |
| Middle | 19.6 | 20.8 | |
| Richer | 20.4 | 19.1 | |
| Richest | 21.2 | 17.6 | |
According to employment status, the unemployed population overbearing the non-member NHI group. Meanwhile, based on marital status, the people that never married occupied the non-member NHI group. Finally, the most impoverished population rules the non-member NHI group based on wealth status.
The following analysis was the collinearity test of NHI membership in Indonesia. The analysis results indicate that there is not a strong correlation between the independent variables. The tolerance value for all variables is more significant than 0.10, and the variance inflation factor (VIF) value for all factors is less than 10.00 simultaneously. The report then concluded that there were no multicollinearity signs in the regression model, pointing to the test’s decision-making basis.
Table 2 shows the result of binary logistic regression of NHI membership in Indonesia. The urban population is 0.608 times less likely than the rural population to become a non-member of NHI (AOR 0.608; 95% CI 0.607-0.608). The situation informs that living in a rural area was one of the barriers to becoming an NHI member in Indonesia.
Table 2.
The Result of Binary Logistic Regression of NHI Membership in Indonesia (n = 47 644).
| Predictor | Non-member of NHI | |||
|---|---|---|---|---|
| P-value | AOR | 95% CI | ||
| Lower bound | Upper bound | |||
| Residence: Urban | <.001 | 0.608 | 0.607 | 0.608 |
| Residence: Rural | - | - | - | - |
| Age group: ≤17 | <.001 | 1.575 | 1.573 | 1.578 |
| Age group: 18-64 | <.001 | 1.310 | 1.309 | 1.312 |
| Age group: ≥65 | - | - | - | - |
| Gender: Male | <.001 | 1.028 | 1.028 | 1.029 |
| Gender: Female | - | - | - | - |
| Education: No education | <.001 | 2.601 | 2.596 | 2.605 |
| Education: Primary | <.001 | 1.707 | 1.704 | 1.709 |
| Education: Secondary | <.001 | 1.526 | 1.524 | 1.529 |
| Education: Higher | - | - | - | - |
| Employment: Unemployed | <.001 | 1.002 | 1.001 | 1.003 |
| Employment: Employed | - | - | - | - |
| Marital: Never married | <.001 | 1.058 | 1.056 | 1.059 |
| Marital: Married | <.001 | 1.106 | 1.105 | 1.108 |
| Marital: Divorced/widowed | - | - | - | - |
| Wealth: Poorest | <.001 | 1.213 | 1.211 | 1.214 |
| Wealth: Poorer | <.001 | 1.039 | 1.038 | 1.040 |
| Wealth: Middle | <.001 | 1.100 | 1.099 | 1.101 |
| Wealth: Richer | <.001 | 1.022 | 1.021 | 1.023 |
| Wealth: Richest | - | - | - | - |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval.
Regarding age group, Table 2 shows that the population in the ≤17 age group is 1.575 more likely than ≥65 to become a non-member of NHI (AOR 1.575; 95% CI 1.573-1.578). The 18 to 64 age group population is 1.310 more likely than ≥65 to become a non-member of NHI (AOR 1.310; 95% CI 1.309-1.312). This information shows that the younger was one of the barriers to becoming an NHI member in Indonesia.
Table 2 informs that the male population is 1.028 more likely to become a non-member of NHI (AOR 1.028; 95% CI 1.028-1.029). This analysis indicates that the male gender is one of the barriers to becoming an NHI member in Indonesia.
Based on education level, the no education population is 2.601 more likely than the higher education population to become a non-member of NHI (AOR 2.601; 95% CI 2.596-2.605). The primary education population is 1.707, more likely than the higher education population to become a non-member of NHI (AOR 1.707; 95% CI 1.704-1.709). Moreover, the secondary education population is 1.526 more likely than the higher education population to become a non-member of NHI (AOR 1.526; 95% CI 1.524-1.529). This analysis indicates that the lower the level of education, the greater the barriers to becoming an NHI member in Indonesia.
Table 2 shows the unemployed population is 1.002 more likely than the employed population to become a non-member of NHI (AOR 1.002; 95% CI 1.001-1.003). The condition informs that unemployment is one barrier to becoming an NHI member in Indonesia.
The information shows that never married or married is more likely to become a non-member of NHI in Indonesia. According to marital status, the never-married population is 1.058 more likely than the divorced/widowed population to become a non-member of NHI (AOR 1.058; 95% CI 1.056-1.059). The married population is 1.106 more likely than the divorced/widowed population to become a non-member of NHI (AOR 1.106; 95% CI 1.105-1.108).
Regarding wealth status, Table 2 shows the poorest population is 1.213 more likely than the richest population to become a non-member of NHI (AOR 1.213; 95% CI 1.211-1.214). The poorer population is 1.039, more likely than the wealthiest population to become a non-member of NHI (AOR 1.039; 95% CI 1.038-1.040). The middle wealth population is 1.100 more likely than the richest population to become a non-member of NHI (AOR 1.100; 95% CI 1.099-1.101). Moreover, the richer population is 1.022 more likely to become a non-member of NHI (AOR 1.022; 95% CI 1.021-1.023). This analysis indicates that all wealth status categories have a higher probability of becoming a barrier to Indonesia’s most prosperous population becoming an NHI member.
Discussion
The distribution map of NHI membership by Indonesia’s province does not show a particular pattern. Some regions show a higher proportion of the population members of the NHI (indicated by the darker color). Previous studies know this situation as the impact of local policies that expand NHI membership by utilizing local budgets. Provinces of Aceh and Papua recorded local policies with such broad effects. Both have a higher proportion of NHI membership than other provinces.16,17
The analysis found that living in a rural area was one of the barriers to becoming an NHI member in Indonesia. Previous studies have shown that this condition is caused by living in rural areas, having limited access, and expensive transportation costs to reach high-quality health services.18 -21 The results of this study are in line with previous research that living in rural areas makes it possible not to participate in NHI.7,22
The analysis results inform that the younger age was one of the barriers to becoming an NHI member in Indonesia. Increasing age is allegedly causing a decrease in the quality of health, so it tends to increase health investment. This health investment is realized in health insurance. 23 In addition, finances at old age are more stable than at a young age because they already have a relatively more regular. 17 The situation may cause a lack of NHI membership at a young age. Previous studies have also shown that age is associated with NHI membership. 17
The study found that the male gender is one of the barriers to becoming an NHI member in Indonesia. The condition can happen because women get more medical services during childbirth, making it possible to take advantage of health insurance.13,24 In addition, women are more aware of their health status, so they prefer to take advantage of health insurance.25,26 The results of other studies also show similar results that men are significantly associated with lower NHI membership. 24
The analysis results show that the lower the level of education, the greater the barriers to becoming an NHI member in Indonesia. Education has a role in selecting information related to health, one of which is health insurance.27,28 In addition, educated people can better process the information received to make the right decisions.27,29 Highly educated people have opinions regarding the importance of health insurance participation to anticipate unexpected health events in the future. However, people with low education do not have an awareness of this. 25 The study results align with previous research that inadequate education is an obstacle to NHI membership. 7 On the other hand, a person’s level of education has a role in one’s perception of the health insurance benefits.30 -32
The result informs that unemployment is one of the barriers to becoming an NHI member in Indonesia. The situation relates to the income earned. Someone who has worked tends to have health insurance because they already have a fixed income. In addition, the workplace usually facilitates workers with health insurance.4,33 The study results show similarities with previous studies that work influences NHI membership. 24
The multivariate analysis result shows that never married or married are more likely to be a non-member of NHI than the divorced/widowed population in Indonesia. Marital status is often related to household income. 34 Married people have many household needs, so they may choose not to become a member of the NHI. 24 In addition, people who are not married tend not to take advantage of health insurance services because they feel they do not need financial risk protection for their health in the future.17,35 The results of other studies also show that marital status is related to NHI membership. 35
The analysis results show that all wealth status categories are more likely to become a non-member of the NHI than the wealthiest population. This situation is contrary to previous studies, which informed that the better the wealth status, the higher the probability of having health insurance.36 -39 On the other hand, this analysis’s results show that the Indonesian government’s efforts to provide subsidies in the form of NHI contribution assistance to the poor have proven effective. The ownership of health insurance for the poor is no different from the rich, which tends to be higher. This situation is also indicated in people’s access to health services.2,15,40 The study results confirm that wealth status is associated with NHI membership.7,23,35
The Indonesian government needs to develop policies targeting rural area residents to expand NHI membership. On the other hand, young people are potential targets and also those who are socially vulnerable (low education, unemployed, and poor). Moreover, further qualitative studies are needed on these targets to determine their perceptions of NHI and their reasons for becoming or not becoming NHI members.
The study found education level is the most potent factor related to NHI membership in Indonesia. Focusing on targets with poor education can have a more significant effect on increasing NHI membership in Indonesia.
Study Limitation
This study has strengths related to using big data as an analysis material so that the conclusions can get generalized up to the national level. On the other side, the analysis in this study utilizes secondary data from a previous survey (“Abilities and Willingness to Pay, Fee, and Participant Satisfaction in implementing National Health Insurance in Indonesia in 2019”). The accepted variables are limited to those given by the Ministry of Health of the Republic of Indonesia. Several other variables previously known to affect health insurance ownership could not be analyzed. These variables include cognitive capacity, prior commercial insurance ownership, having children, and family size.24,41,42
Conclusions
Based on the results, the study concluded that 7 population characteristics become specific targets for expanding NHI membership in Indonesia. The 7 characteristics are the population who live in rural areas, are young, male, poor education, unemployed, never married or married, and poor.
The government needs to focus its policy on this specific target to accelerate the expansion of NHI membership in Indonesia.
Acknowledgments
The author would like to thank the Ministry of Health of the Republic of Indonesia, who has agreed to allow the author to analyze the “Abilities and Willingness to Pay, Fee, and Participant Satisfaction in the Implementation of NHI in Indonesia 2019” data in this article.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The National Ethics Committee has approved the Ethical clearance of the survey “Abilities and Willingness to Pay, Fee, and Participant Satisfaction in the Implementation of NHI in Indonesia in 2019” (Number: LB.0201/2/KE.340/2019). The study removed from the dataset all the identities of respondents.
ORCID iD: Ratna Dwi Wulandari  https://orcid.org/0000-0003-4365-5747
https://orcid.org/0000-0003-4365-5747
References
- 1. The Republic of Indonesia. Law Number 40 of 2004 Concerning the National Social Security System. 2004. p. 1–28. [Google Scholar]
- 2. Wulandari RD, Laksono AD, Matahari R. The effects of health insurance on maternity care in health services in Indonesia. Int J Innov Creat Chang. 2020;14(2):478-497. [Google Scholar]
- 3. Lidwina A. The Number of HSSAA (BPJS Kesehatan) Participants Reaches 222.5 Million People by 2020 (Jumlah Peserta BPJS Kesehatan Capai 222,5 Juta Orang hingga 2020) [Internet]. 2021. p. 1–2. Accessed June 12, 2021. https://databoks.katadata.co.id/datapublish/2021/01/06/jumlah-peserta-bpjs-kesehatan-capai-2225-juta-orang-hingga-2020?__cf_chl_jschl_tk__=437a2ebbdb136f3d5950b28fac76bc311c62b8ef-1623435823-0-ARTDPon0iYwnRXk3vHr1man3KVnLuPbf9Z10cZrv6r79TzOzduZTL0yKzMFkvg
- 4. Sari B, Idris H. Determinant of independent national health insurance ownership in Indonesia. Malaysian J Public Heal Med. 2019;19(2):109-115. [Google Scholar]
- 5. Indiraswari T, Supriyanto S, Ernawaty E, Putri NK. Health insurance literacy: discussion and reaction of Facebook users’ towards the national health insurance in Indonesia. J Public Health Res. 2020;9(2):1844-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dartanto T, Pramono W, Lumbanraja AU, et al. Enrolment of informal sector workers in the national health insurance system in Indonesia: a qualitative study. Heliyon. 2020;6(11):e05316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Andayani Q, Koesbardiati T, Prahastuti AD, Masruroh M, Laksono AD. The barrier to access health insurance for maternity care: case study of female workers in Indonesia. Med Leg Update. 2021;21(2):926-932. [Google Scholar]
- 8. Rahmadani S, Abadi MY, Marzuki DS, Fajrin MA. Analysis of independent national health insurance ownership of informal workers: Study of market traders in Gowa District, Indonesia. Enferm Clin. 2020;30:295-299. [Google Scholar]
- 9. Kur’aini SN, Razak A, Daud A, Mallngi A. Economic status of community interest in membership of BPJS health in Duampanua district, Pinrang regency. Open Access Maced J Med Sci. 2020;8(T2):36-40. [Google Scholar]
- 10. Dartanto T, Halimatussadiah A, Rezki JF, et al. Why do informal sector workers not pay the premium regularly? Evidence from the national health insurance system in Indonesia. Appl Health Econ Health Policy. 2020;18(1):81-96. [DOI] [PubMed] [Google Scholar]
- 11. Laksono AD, Wulandari RD, Soedirham O. Regional disparities of health center utilization in rural Indonesia. Malaysian J Public Heal Med. 2019;19(1):158-166. [Google Scholar]
- 12. Laksono AD, Wulandari RD, Efendi F. Determinants of hospital utilisation among urban poor societies in Indonesia. Int J Innov Creat Chang. 2020;12(9):375-387. [Google Scholar]
- 13. Laksono AD, Wulandari RD, Rukmini R. The determinant of healthcare childbirth among young people in Indonesia. J Public Health Res. 2021;10(1):1890-1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Laksono AD, Paramita A, Wulandari RD. Socioeconomic disparities of facility-based childbirth in Indonesia. Int Med J. 2020;25(1):291-298. [Google Scholar]
- 15. Wulandari RD, Supriyanto S, Qomaruddin B, Laksono AD. Socioeconomic disparities in hospital utilization among elderly people in Indonesia. Indian J Public Health Res Dev. 2019;10(11):2192-2194. [Google Scholar]
- 16. Khairunnisa K, Abdullah A. Implikasi Jaminan Kesehatan Aceh terhadap Jumlah Persalinan Pada Rumah Sakit/Rumah Bersalin Swasta dan Rumah Sakit Kesdam di Banda Aceh (Aceh Health Insurance Scheme Implications to Total Labor at Private Hospital/Maternity Home and Kesdam Hospital in Ba). J Kesehat Masy Aceh. 2016;2(1):28-37. [Google Scholar]
- 17. Laksono AD, Wulandari RD, Matahari R. The determinant of health insurance ownership among pregnant women in Indonesia. BMC Public Health. 2021;21(1):1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Seran AA, Laksono AD, Sujoso ADP, et al. Does contraception used better in urban areas?: an Analysis of the 2017 IDHS (Indonesia Demographic and health survey). Syst Rev Pharm. 2020;11(11):1892-1897. [Google Scholar]
- 19. Wulandari RD, Laksono AD, Rohmah N. Urban-rural disparities of antenatal care in South East Asia: a case study in the Philippines and Indonesia. BMC Public Health. 2021;21(1):1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Laksono AD, Wulandari RD, Soedirham O. Urban and rural disparities in hospital utilization among Indonesian adults. Iran J Public Health. 2019;48(2):247-255. [PMC free article] [PubMed] [Google Scholar]
- 21. Wulandari RD, Laksono AD, Nantabah ZK, Rohmah N, Zuardin Z. Hospital utilization in Indonesia in 2018: do urban-rural disparities exist? BMC Health Serv Res. 2022;22:491. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mahmudiono T, Laksono AD. Disparity in the hospitals utilization among regions in Indonesia. Open Access Maced J Med Sci. 2021;9:1461-1466. [Google Scholar]
- 23. Mulenga JN, Bwalya BB, Gebremeskel Y. Demographic and socio-economic determinants of women’s health insurance coverage in Zambia. Epidemiol Biostat Public Heal. 2017;14(1):1-9. [Google Scholar]
- 24. Okedo-Alex I, Alo C, Akamike I. Determinants of willingness to participate in health insurance amongst people living with HIV in a tertiary hospital in south-East Nigeria. Niger Postgrad Med J. 2020;27(3):196-201. [DOI] [PubMed] [Google Scholar]
- 25. Laksono AD, Wulandari RD. Predictors of hospital utilization among Papuans in Indonesia. Indian J Forensic Med Toxicol. 2020;14(2):2319-2324. [Google Scholar]
- 26. Sisira Kumara A, Samaratunge R. Health insurance ownership and its impact on healthcare utilization: Evidence from an emerging market economy with a free healthcare policy. Int J Soc Econ. 2020;47(2):244-267. [Google Scholar]
- 27. Wulandari RD, Laksono AD. Education as predictor of the knowledge of pregnancy danger signs in rural Indonesia. Int J Innov Creat Chang. 2020;13(1):1037-1051. [Google Scholar]
- 28. Kusrini I, Fuada N, Supadmi S, Laksono AD. Education as predictor of low birth weight among female worker in Indonesia. Medico-Legal Updat. 2021;21(1):360-365. [Google Scholar]
- 29. Rohmah N, Yusuf AA, Hargono R, et al. Determinants of teenage pregnancy in Indonesia. Indian J Forensic Med Toxicol. 2020;14(3):2080-2085. [Google Scholar]
- 30. Megatsari H, Laksono AD, Ridlo IA, Yoto M, Azizah AN. Community perspective about health services access. Bull Heal Syst Res. 2018;21:247-253. [Google Scholar]
- 31. Maślach D, Karczewska B, Szpak A, Charkiewicz A, Krzyżak M. Does place of residence affect patient satisfaction with hospital health care? Ann Agric Environ Med. 2020;27(1):86-90. [DOI] [PubMed] [Google Scholar]
- 32. Laksono AD, Wulandari RD, Ibad M, Kusrini I. The effects of mother’s education on achieving exclusive breastfeeding in Indonesia. BMC Public Health. 2021;21(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Denny HM, Laksono AD, Matahari R, Kurniawan B. The determinants of four or more antenatal care visits among working women in Indonesia. Asia-Pacific J Public Heal. 2022;34(1):51-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Megatsari H, Laksono AD, Herwanto YT, et al. Does husband/partner matter in reduce women’s risk of worries?: study of psychosocial burden of covid-19 in Indonesia. Indian J Forensic Med Toxicol. 2021;15(1):1101-1106. [Google Scholar]
- 35. Liu M, Luo Z, Zhou D, et al. Determinants of health insurance ownership in Jordan: a cross-sectional study of population and family health survey 2017-2018. BMJ Open. 2021;11(3):e038945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mekonnen T, Dune T, Perz J, Ogbo FA. Trends and determinants of antenatal care service use in Ethiopia between 2000 and 2016. Int J Environ Res Public Health. 2019;16(5):748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wilson M, Patterson K, Nkalubo J, et al. Assessing the determinants of antenatal care adherence for Indigenous and non-Indigenous women in southwestern Uganda. Midwifery. 2019;78:16-24. [DOI] [PubMed] [Google Scholar]
- 38. Nasution SK, Mahendradhata Y, Trisnantoro L. Can a national health insurance policy increase equity in the utilization of skilled birth attendants in Indonesia? A secondary analysis of the 2012 to 2016 National Socio-Economic Survey of Indonesia. Asia-Pacific J Public Heal. 2020;32(1):19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wulandari RD, Laksono AD, Prasetyo YB, Nandini N. Socioeconomic disparities in hospital utilization among female workers in Indonesia: a cross-sectional study. J Prim Care Community Health. 2022;13(2):21501319211072679-21501319211072687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Putri NK, Laksono AD. Predictors of childbirth services in Indonesia. Int J Public Health Sci. 2022;11(2):566-573. [Google Scholar]
- 41. McGarry BE, Tempkin-Greener H, Grabowski DC, Chapman BP, Li Y. Consumer decision-making abilities and long-term care insurance purchase. J Gerontol Ser B Psychol Sci Soc Sci. 2018;73(4):e1-e10. [DOI] [PubMed] [Google Scholar]
- 42. Wang Q, Abiiro GA, Yang J, Li P, De Allegri M. Preferences for long-term care insurance in China: results from a discrete choice experiment. Soc Sci Med. 2021;281:114104. [DOI] [PubMed] [Google Scholar]