Abstract
Background and Objectives
The objective of this work was to examine the association between deployment-related traumatic brain injury (TBI) severity, frequency, and other injury characteristics with headache outcomes in veterans evaluated at a Veterans Administration (VA) polytrauma support clinic.
Methods
We conducted a retrospective chart review of 594 comprehensive TBI evaluations between 2011 and 2021. Diagnostic criteria were based on the Department of Defense/VA Consensus-Based Classification of Closed TBI. Adjusted odds ratios (AORs) and 95% CIs were estimated for headache prevalence (logistic), headache severity (ordinal), and prevalence of migraine-like features (logistic) with multiple regression analysis. Regression models were adjusted for age, sex, race/ethnicity, time since injury, and mental health diagnoses.
Results
TBI severity groups were classified as sub concussive exposure (n = 189) and mild (n = 377), moderate (n = 28), and severe TBI (n = 0). Increased headache severity was reported in veterans with mild TBI (AOR 1.72 [95% CI 1.15, 2.57]) and moderate TBI (AOR 3.89 [1.64, 9.15]) compared to those with subconcussive exposure. A history of multiple mild TBIs was associated with more severe headache (AOR 2.47 [1.34, 4.59]) and migraine-like features (AOR 5.95 [2.55, 13.77]). No differences were observed between blast and nonblast injuries; however, greater headache severity was reported in veterans with both primary and tertiary blast effects (AOR 2.56 [1.47, 4.49]). Alteration of consciousness (AOC) and posttraumatic amnesia (PTA) >30 minutes were associated with more severe headache (AOR 3.37 [1.26, 9.17] and 5.40 [2.21, 13.42], respectively). The length of time between the onset of last TBI and the TBI evaluation was associated with headache severity (AOR 1.09 [1.02, 1.17]) and prevalence of migraine-like features (AOR 1.27 [1.15, 1.40]). Last, helmet use was associated with less severe headache (AOR 0.42 [0.23, 0.75]) and lower odds of migraine-like features (AOR 0.45 [0.21, 0.98]).
Discussion
Our data support the notion of a dose-response relationship between TBI severity and headache outcomes. A history of multiple mild TBIs and longer duration of AOC and PTA are unique risk factors for poor headache outcomes in veterans. Furthermore, this study sheds light on the poor headache outcomes associated with subconcussive exposure. Past TBI characteristics should be considered when developing headache management plans for veterans.
Traumatic brain injury (TBI) is the signature injury among combat veterans returning from recent US military operations. Indeed, the Defense and Veterans Brain Injury Center reports that 434,618 service members have sustained TBI since 2000.1 Co-occurring TBI sequalae, posttraumatic stress disorder (PTSD), and chronic pain constitute a complex and prevalent clinical profile in veterans called the polytrauma triad, which can perpetuate long-term functional disability after injury.2,3 Posttraumatic headache (PTH) is the most frequent manifestation of comorbid chronic pain within this population.4,5 The International Classification of Headache Disorders, 3rd edition, defines PTH as (1) a secondary headache disorder that develops or (2) a primary headache disorder that becomes chronic or made significantly worse in close temporal relation to a TBI.6 The most common clinical presentation of PTH is comparable to migraine (i.e., headache, nausea, photophobia, phonophobia); however, PTH is often refractory to conventional migraine therapies.7-9 An estimated 27% to 62% of veterans with sustained TBI experience persistent PTH (lasting >3 months).4,5,10 The problem is that persistent PTH is associated with higher rates of disability, higher health care and societal costs, and poorer health outcomes in veterans.11,12
While comorbid psychiatric conditions strongly influence chronic TBI symptomology,13,14 the extent to which TBI characteristics affect PTH is largely unknown. Studies have come to varied conclusions regarding the role that TBI severity (i.e., mild, moderate, or severe) plays in headache occurrence and severity. Some analyses demonstrate null findings,10,15 whereas others suggest a direct16-18 or possible inverse relationship between TBI severity and headache outcomes.4,19,20 Further investigation into discrete measures correlated with TBI severity such as loss/alteration of consciousness (LOC/AOC) and posttraumatic amnesia (PTA) duration, is warranted. Nonetheless, heterogeneous symptomatology within comparable TBI severities emphasizes the multidimensional etiology of PTH.12,21 Emerging evidence suggests that there may be a cumulative effect of TBI on long-term sequelae such as postural control deficits, psychiatric distress, and neurocognitive dysfunction; however, it is unknown whether this relationship extends to postinjury headache.22,23 Blast exposure is the most common mechanism of injury during deployment.16,24 There are no published data on headache outcomes related to different types of injury mechanism in veterans. Blast-induced neurotrauma is complex in that individuals are exposed not only to the primary blast wave but also to possible secondary and tertiary effects (e.g., acoustic damage, penetrating debris, coup-countercoup injury).25 Moreover, blast proximity and personal protective equipment (PPE) also contribute to the variability in trauma received by an individual. Preclinical studies suggest that blast TBI may alter the integrity of cerebral vasculature and blood-brain barrier.26 Therefore, we hypothesize that blast-related TBI could be associated with poorer headache outcomes compared to blunt-trauma injury.
The aims of the present cross-sectional, retrospective chart review were (1) to compare headache characteristics across TBI severity groups, (2) to examine the cumulative effect of TBI on headache outcomes, and (3) to evaluate injury characteristics (i.e., mechanism of injury, LOC/AOC, PTA, PPE) that may be associated with headache outcomes in veterans. Identifying unique TBI characteristics associated with postinjury headache severity and migraine-like features can help facilitate earlier and more individualized intervention for veterans at risk for persistent PTH.
Methods
Data Source
This study is a retrospective chart review of 594 Operation Iraqi Freedom/Operation Enduring Freedom/Operation New Dawn (OIF/OEF/OND) veterans who were administered a comprehensive TBI evaluation (CTBIE) at a local Southeastern Department of Veterans Affairs (VA) polytrauma support clinic. Data were extracted from electronic medical records of OEF/OIF/OND veterans evaluated between January 2011 and January 2021.
Procedure
All OIF/OEF/OND veterans are administered the VA Traumatic Brain Injury Screening Tool (VATBIST) by the veteran's case manager or primary care provider or a registered nurse at the time of the initial VA visit.27 A positive VATBIST requires the endorsement of at least 1 item for each of the 4 questions regarding the following: (1) an event that may have exposed the veteran to brain injury during OEF/OIF/OND deployment (i.e., blast or explosion, vehicular accident/crash, fragment or bullet wound above the shoulders, and/or fall); (2) an AOC or head injury immediately after that event (i.e., losing consciousness/being knocked out, being dazed, feeling confused or “seeing stars,” not remembering the event, experiencing concussion and/or head injury); (3) the presence of new or worsened symptoms after the event (i.e., memory problems or lapses, balance problems or dizziness, sensitivity to bright light, irritability, headaches, and/or sleep problems); and (4) the continued presence of any of those symptoms in the week before the VATBIST.
Veterans with a positive VATBIST are referred to a trained physiatrist or specialty clinic for a CTBIE if the veteran agrees to further assessment and care of a potentially previously undiagnosed TBI. In regard to the present study, CTBIEs were administered by a trained physiatrist within the local polytrauma support clinic. The CTBIE confirms deployment-related TBI diagnoses and is the starting point to develop an interdisciplinary follow-up treatment plan. The physiatrist first collects relevant sociodemographic information and self-reported injury characteristics: mechanism(s) of injury (e.g., motor vehicle accident, blast, fall, blunt trauma), approximate blast effects and proximity (if applicable), years since the most recent TBI, PPE use at the time of injury, and LOC, AOC, and PTA duration. The Neurobehavioral Symptom Inventory (NSI) was administered to each veteran to rate their symptoms in regard to the past 30 days.28 The NSI is a 22-item subjective assessment of postconcussive symptomatology rated on a 5-point Likert scale ranging from 0 (none; symptom is rarely ever present/not a problem at all) to 4 (very severe; symptom is almost always present/impairs performance at work, school, or home/individual probably cannot function without help). Last, the physiatrist and multidisciplinary TBI team come to a conclusion regarding the TBI diagnoses, present/suspected/probable comorbid diagnoses determined by trained clinicians (PTSD, depression, anxiety, etc), and the degree to which these diagnoses are consistent with the veteran's current clinical symptom presentation. A more detailed review of the VA TBI screening process has been described in previous literature.27,29
TBI Diagnosis Ascertainment
A diagnosis of TBI was made only if the physiatrist believed that the reported deployment-related events fit criteria for TBI beyond reasonable doubt. TBI severity was ascertained with the Department of Defense/VA Consensus-Based Classification of Closed TBI Severity.30 Mild TBI is defined by a duration of LOC <30 minutes, AOC <24 hours, and/or PTA <24 hours. Moderate TBI is defined by a duration of LOC >30 minutes and <24 hours, AOC >24 hours, and/or PTA >1 day but <7 days. Severe TBI is defined by a duration of LOC >24 hours and/or PTA >7 days. Those who did not meet the minimum criteria for mild TBI but had a positive VATBIST were categorized as the subconcussive exposure group due to insufficient information to make a severity rating. For the purposes of the present study, veterans were grouped into 3 groups—subconcussive exposure (n = 189), mild TBI (n = 377), and moderate TBI (n = 28)—based on their TBI severity using the aforementioned criteria. No veterans were identified as having a history of severe TBI.
Outcome Measures
Outcome variables focused on in the present study were measures of headache characteristics, including headache prevalence, headache severity, and the prevalence of migraine-like features. Veterans who endorsed headaches in the 30 days before evaluation were classified as having headache. The prevalence of headache was coded as a binary variable (present/absent). Headache severity and prevalence of migraine-like symptoms were measured among those who endorsed headache. Headache severity was measured with the headache item from the NSI and was thus coded as an ordinal variable from 0 (none) to 4 (very severe). Veterans who reported headache and endorsed nausea, sensitivity to light (photophobia), or sensitivity to noise (phonophobia) from respective items on the NSI were classified as having migraine-like features. The prevalence of migraine-like features was coded as a binary variable (present/absent).
Statistical Analysis
All data analyses were performed in R version 4.0 (R Core Team, Vienna, Austria, 2019) with the Rmimic (version 1.0.3) R package.31 We used χ2 tests for categorical and ordinal variables and linear regression for continuous variables to compare key sociodemographic factors and postconcussive symptomatology across TBI severity groups. Logistic regression analyses were conducted to compare the prevalence of headache and headache with migraine-like features across TBI severity groups. Ordinal logistic regression analyses were conducted to compare headache severity across TBI severity groups. Only 28 veterans had a confirmed history of moderate TBI; thus, this sample size was inadequate to achieve appropriate statistical power for analyzing headache differences in moderate TBI. Separate regression analyses for veterans with a history of mild TBI were conducted to examine the association between TBI frequency and headache characteristics: prevalence (logistic), severity (ordinal), and prevalence of migraine-like features (logistic). These models also included mechanism(s) of injury, blast effects (primary, secondary, or tertiary), approximate blast distance (feet), years since the most recent TBI, helmet use at the time of injury (yes/no), LOC duration, AOC duration, and PTA duration to identify any injury characteristics that may be associated with postinjury headache characteristics. All regression analyses were adjusted for potential confounders according to conceptual importance and prior literature (i.e., biological sex [0 = male, 1 = female], age, race/ethnicity [0 = White, 1 = Black, 2 = other, 3 = unknown], PTSD diagnosis [0 = no, 1 = yes], depression diagnosis [0 = no, 1 = yes], and anxiety diagnosis [0 = no, 1 = yes]). Effect sizes were calculated for regression models as odds ratio (OR)/adjusted OR (AOR) with 95% CI. An a priori family-wise α level was set to p = 0.05. Bonferroni correction was applied to adjust for multiple comparisons when applicable.
Standard Protocol Approvals, Registrations, and Patient Consents
This study was approved by the Columbia VA Healthcare System Human Subjects Institutional Review Board. Participant consent was waived for this chart review study. All data were deidentified before data cleaning.
Data Availability
Due to VA regulations and Veterans Health Administration ethics agreements, the analytical datasets used for this study are not permitted to leave the VA firewall without a data-use agreement. This limitation is consistent with other studies based on VA data. However, VA data are made freely available to researchers with an approved VA study protocol. More information can be obtained online32 or by contacting the VA Information Resource Center at VIReC@va.gov.
Results
Participants
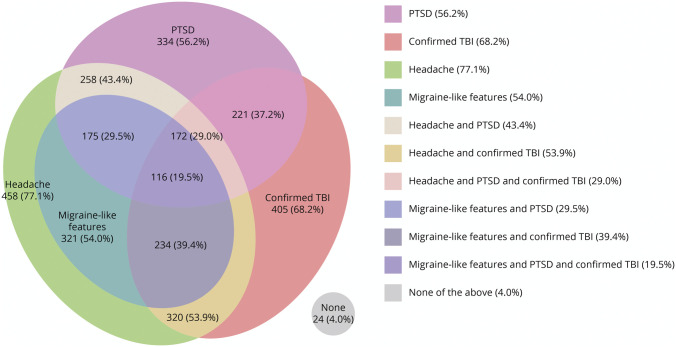
The current sample was predominantly male (92.8%) with a mean age of 34.41 ± 8.69 years. Overall, 405 veterans had a confirmed history of TBI and were screened at an average of 6.29 ± 4.12 years since their most recent TBI. Demographic characteristics grouped by TBI severity can be found in Table 1. TBI severity groups were comparable with respect to sex, age, educational attainment, marital status, and PTSD and anxiety prevalence but differed significantly with respect to race/ethnicity and employment status. PTSD was diagnosed in 344 (56.2%) veterans. The prevalence of mental health diagnoses grouped by TBI severity can be found in Table 2. Veterans with subconcussive exposure had a greater prevalence of depression than veterans with mild TBI (36.5% vs 25.7%; p = 0.008). The distribution of veterans in this cohort with PTSD, confirmed mild/moderate TBI, and headache is shown in the Figure.
Table 1.
Demographic Characteristics Grouped by TBI Severity Among Veterans Who Were Administered a CTBIE, 2011 to 2021
Table 2.
Headache Characteristics and Mental Health Diagnoses Grouped by TBI Severity Among Veterans Who Were Administered a CTBIE, 2011 to 2021
Figure. Distribution of Veterans With PTSD, Confirmed TBI, and Headache/Migraine-Like Features Who Presented for Comprehensive TBI Evaluation, 2011 to 202131.
PTSD = posttraumatic stress disorder; TBI = traumatic brain injury.
Association Between Headache Characteristics and TBI Severity
The prevalence of headache, mean headache severity, and prevalence of migraine-like features for the subconcussive exposure, mild TBI, and moderate TBI groups can be found in Table 2. Unadjusted and adjusted (covariates including sex, age, race/ethnicity, PTSD, depression, and anxiety diagnoses) associations between headache characteristics and TBI severity can be found in Table 3. Veterans with a history of mild TBI were at higher odds of reporting more severe headache compared to veterans with subconcussive exposure (AOR 1.72; 95% CI 1.15, 2.57; p = 0.008); however, these groups did not differ in prevalence of headache or migraine-like symptoms (p > 0.080). While veterans with a history of moderate TBI did not differ in headache prevalence compared to veterans with less severe injuries after adjustment for covariates and Bonferroni correction (p > 0.027), those with a history of moderate TBI had higher odds of reporting severe headache (AOR 3.89; 95% CI 1.64, 9.15; p = 0.002) and migraine-like features (AOR 15.34; 95% CI 1.99, 177.7; p = 0.009) than those with subconcussive exposure. Furthermore, veterans with a history of moderate TBI had higher odds of endorsing migraine-like symptoms (AOR 12.25; 95% CI 1.63, 92.65; p = 0.015) compared to those with a history of mild TBI.
Table 3.
Association Between Headache Characteristics and TBI Severity Among Veterans Who Were Administered a CTBIE, 2011 to 2021
Association Between Headache Characteristics and Mild TBI Frequency
Of the 377 veterans with a history of mild TBI, 71.6% had sustained a single mild TBI, 14.6% had sustained 2 mild TBIs, and 13.8% had sustained ≥3 TBIs. Descriptive statistics for headache prevalence, headache severity, and prevalence of migraine-like features with respect to mild TBI frequency can be found in Table 4. Associations between headache characteristics and TBI frequency with Bonferroni correction can be found in Table 5. No association was found between mild TBI frequency and headache prevalence. Veterans with a history of multiple mild TBIs (≥2) had higher odds of reporting severe headache (AOR 2.47; 95% CI 1.34, 4.59; p = 0.004) and migraine-like features (AOR 5.95; 95% CI 2.55, 13.77; p < 0.001) compared to those with a single mild TBI. Veterans with a history of 2 mild TBIs did not differ statistically in headache severity from veterans with a history of ≥3 mild TBIs (AOR 0.93; 95% CI 0.37, 0.82; p = 0.883). Similarly, the prevalence of migraine-like features did not significantly differ between veterans with a history of 2 mild TBIs and those with ≥3 mild TBIs (84.9% vs 81.8%; p = 0.390).
Table 4.
Headache and Injury Characteristics Among Veterans With a Confirmed History of Deployment-Related Mild TBI, 2011 to 2021
Table 5.
Association Between Headache and Injury Characteristics in Veterans With a Confirmed History of Deployment-Related Mild TBI, 2011 to 2021
Association Between Headache Characteristics and Injury Characteristics
Blast exposure was the most common type of mechanism of injury among veterans with mild TBI (57.2%), followed by falls (16.8%), blunt trauma (16.5%), and motor vehicle accidents (9.5%). Improvised explosive device blast exposure accounted for more TBIs than any other type of blast exposure (67.7%). Primary blast effects were experienced by 188 veterans with mild TBI; 66 veterans experienced secondary blast effects; and 113 veterans experienced tertiary blast effects. A combination of primary and tertiary blast effects was experienced by 95 veterans with mild TBI. Blast distances ranged from 0 to >50 ft away, and the mode estimated blast distance was <10 ft away. Although the majority of veterans with a history of mild TBI did not experience LOC (63.4%) or PTA (74.8%) related to their injury or injuries, most experienced an AOC lasting <30 minutes (70.3%) and wore a helmet during the time of injury (69.2%). Descriptive statistics for headache prevalence, headache severity, and prevalence of migraine-like features among injury characteristics can be found in Table 4. Associations between headache and injury characteristics can be found in Table 5. Higher number of years since the veteran's most recent TBI was significantly associated with higher odds of more severe headache (AOR 1.09; 95% CI 1.02, 1.17; p = 0.009) and migraine-like features (AOR 1.27; 95% CI 1.15, 1.40; p = 0.001). Fall-related mild TBI was associated with lower odds of severe headache (AOR 0.42; 95% CI 0.19, 0.92; p = 0.031); however, associations were no longer significant after Bonferroni correction. No other mechanisms of injury were associated with headache characteristics. Veterans who reported incurring both primary and tertiary blast effects had higher odds of reporting severe headache (AOR 2.56; 95% CI 1.47, 4.49; p < 0.001) compared to those who endorsed only a single type of blast effect or no blast injury.
No associations between LOC duration and headache characteristics were observed. Compared to no AOC, AOC duration between 30 minutes and 24 hours after TBI was associated with higher odds of headache (AOR 6.75; 95% CI 2.08, 21.89; p = 0.001). Furthermore, AOC duration between 30 minutes and 24 hours was associated greater headache severity (AOR 3.37; 95% CI 1.26, 9.17; p = 0.016) compared to no AOC. No differences were observed between AOC duration <30 minutes and duration between 30 minutes and 24 hours. Similarly, PTA duration between 30 minutes and 24 hours after TBI was associated with greater headache severity compared to no PTA (AOR 5.40; 95% CI 2.21, 13.42; p < 0.001) and PTA duration <30 minutes (AOR 5.04; 95% CI 1.92, 13.50; p = 0.001). Helmet use at the time of injury was associated with lesser headache severity (AOR 0.42; 95% CI 0.23, 0.75; p = 0.003) and decreased odds of migraine-like features (AOR 0.45; 95% CI 0.21, 0.98; p = 0.043).
Discussion
We conducted a retrospective, cross-sectional, multivariate analysis of OIF/OEF/OND veterans who were administered a CTBIE to investigate the association between headache characteristics and remote deployment-related TBI characteristics while concurrently adjusting for age, sex, race/ethnicity, and comorbid mental health diagnoses. Our study found that veterans with a history of mild or moderate TBI who endorsed headache reported greater headache severity compared to veterans with subconcussive exposure. In addition, veterans with a history of moderate TBI had a greater prevalence of migraine-like features compared to veterans with a history of mild TBI or subconcussive exposure. Veterans with a history of multiple mild TBIs had greater headache severity and odds of reporting migraine-like features than those with a single mild TBI. No differences were observed between mechanisms of injury; however, veterans who sustained both primary and tertiary blast effects did report greater headache severity. Furthermore, longer AOC and PTA duration after mild TBI was associated with poorer headache outcomes. In this cohort, earlier CTBIE in relation to the onset of TBI and helmet use at the time of injury were protective against migraine-like features and more severe headache. Last, we observed that almost one-third of veterans had overlapping symptoms of headache, PTSD, and TBI (mild and moderate) and that 1 in 5 veterans had overlapping symptoms of migraine-like headache, PTSD, and TBI. Overall, these findings suggest that several injury characteristics related to deployment-related TBI are independently associated with headache outcomes years after injury.
Consistent with existing literature,16,17 we found that veterans with a history of mild or moderate TBI had 1.72 and 3.89 times greater odds of more severe headache, respectively, compared to veterans with subconcussive exposure. While the prevalence of headache and migraine-like symptoms was similar between the mild TBI and subconcussive exposure groups, we identified moderate TBI as an independent risk factor for reporting headache with migraine-like features. The present findings provide contrary evidence to studies that suggest that individuals who sustain mild TBI are more likely to endorse headache than those with moderate TBI.4,19,20 Our findings further reflect a linear relationship between TBI severity and headache characteristics when more discrete methodology is used to classify TBI severity with LOC, AOC, and PTA duration. Veterans who reported an AOC or PTA duration lasting 30 minutes to 24 hours were more likely to endorse headache and greater headache severity than veterans with no or shorter duration of AOC/PTA. To the best of our knowledge, no prior studies have examined the relationship between AOC duration and headache. Bomyea et al.33 found that veterans with mild/moderate TBI and PTH were more likely to experience PTA than those without PTH; however, a number of prior studies showed no such association.10,15 The wide variety of TBI severity measures used in the existing literature (i.e., diagnostic TBI severity, presence/absence or duration of LOC, AOC, or PTA) may account for the incongruency in their findings. It has been suggested that categorizing LOC, AOC, or PTA to ascertain remote TBI severity may contribute to the misclassification of TBI injury severity.34
Our findings demonstrate a cumulative effect of mild TBI on headache severity and prevalence of migraine-like features in veterans. Veterans with a history of ≥2 mild TBIs are more than twice as likely to report severe headache and almost 6 times more likely to report migraine-like symptoms compared to those with a single mild TBI. Additional injury did not correspond to poorer headache outcomes in those with a history of ≥2 mild TBIs. Wilk et al.35 observed that veterans with a history of multiple mild TBIs were more likely to report headache (OR 4.0); however, only mild TBI with LOC was examined in that study. Nonetheless, the current literature suggests that an increasing frequency of mild TBI is neurologically detrimental. A cumulative effect of mild TBI has been observed for neurocognitive impairments, PTSD, depression, general pain, and suicidal behavior.36-39 It is hypothesized that multiple TBIs may incrementally compromise cerebral white matter integrity, which can produce potential long-term neurologic dysfunction.40,41 Additional longitudinal research is needed to elucidate the pathophysiologic mechanism(s) by which cumulative mild TBI increases the risk of PTH.
In this cohort, blast-related TBI was the most common mechanism of injury, which is consistent with prior findings.16,24 Prior evidence suggests that a difference between blast-related and nonblast TBI is indeterminant; however, most studies that report significant findings are in reference to posttraumatic symptoms.42,43 Similar to Wilk et al.,44 we found no differences between blast and nonblast mild TBI in terms of headache outcomes when including veterans with/without LOC. We observed that veterans who reported incurring sequential primary (i.e., direct effect of the blast) and tertiary (i.e., hitting one's head on the ground or other object) blast effects at the time of a mild TBI endorsed greater headache severity, possibly resulting from compounded neurotrauma. Inconsistencies in PPE may also partially account for the current findings. We observed that veterans who wore helmets during injury had a 58% decrease in odds of reporting severe headache and a 55% decrease in odds of migraine-like symptoms compared to those who did not wear a helmet. While helmet use did not differ between injury mechanisms, other forms of body armor were not accounted for. Advances in military PPE have certainly increased survival rates in the combat theater; however, increased surface area of body armor may intensify blast wave effects.25,45 Future studies should continue to investigate the potential biomechanical differences between distinct mechanisms of injury to gain a better understanding of how to effectively protect against and manage the long-term sequalae of TBI.
The present study has several strengths. First, we used a relatively large cohort that was representative of veterans with suspected TBI. Second, the VATBIST and CTBIE are both standardized methods used by the VA, which provided reliable demographic and health information from patient records to be controlled for in analyses. Several limitations should be considered in the interpretation of the present findings. First, the true number of veterans with TBI may not be fully represented by our sample. For example, veterans who sustained TBI but whose symptoms resolved or those failed to recall important TBI information would not have been identified by the VATBIST. In addition, the CTBIE is a tool intended to capture previously undiagnosed traumatic brain injuries and is not completed for veterans with known preexisting diagnosis of TBI. That is, a service member identified with a mild, moderate, or severe TBI by the Department of Defense immediately after deployment would not be referred to have a CTBIE. It is likely that the majority of these patients are veterans with moderate/severe TBI injuries that required immediate medical intervention at that time. Given that the focus of this work is on mild TBI, we do not anticipate that this affected the findings significantly. In addition, the high percentage of veterans (31.8%) with subconcussive exposure within our cohort may reflect the poor specificity of the VATBIST, a patient's misattributing symptoms to an origin event, or difficulty in distinguishing AOC from combat-induced emotional trauma. Second, the items included on the NSI are self-reported, are nonspecific to TBI and headache, and could be particularly influenced by psychiatric symptoms.13,14 Thus, the NSI is susceptible to bias, and caution is warranted when this measure is given to patients with comorbid mental health disorders. We attempted to compensate for potential bias by adjusting for common comorbid mental health disorders. While the presence of migraine-like symptoms may be indicative of migraine-type headache, the NSI does not provide sufficient information to classify specific headache type. We suspect that many veterans in this cohort are likely experiencing chronic PTH; however, without establishing temporal relationship between headache and TBI onset, it is difficult to differentiate headache types. Last, due to insufficient data, we failed to control for potential confounders, including military branch/rank, number of deployments, use of prophylactic or rescue headache mediation, and other posttraumatic symptoms. Replication analyses are needed to verify the current findings while accounting for these variables.
Our results suggest that clinicians may achieve greater precision for the prognosis of headache related to TBI by examining the duration of LOC, AOC, and PTA as semicontinuous variables rather than categorical criteria. Regardless of TBI diagnosis or severity, both headache with migraine-like features and psychiatric conditions were prevalent in the current cohort. These concurrent conditions pose a significant health burden for veterans and clinical challenges for health care providers.46 The overlapping nature of these conditions emphasizes a need for multidisciplinary care in veterans with a confirmed history of TBI and those with subconcussive exposure within the VA polytrauma system of care. Diagnosis-based treatments may exclude veterans with subconcussive exposure from more beneficial treatment options, despite sharing similar physiologic pathways with chronic TBI symptoms. Focusing on a symptom-based approach to treatment may be more appropriate for veterans with multiple co-occurring postconcussive symptoms. For example, targeted treatments for autonomic dysfunction may help ameliorate shared symptom burden among several psychiatric conditions, migraine, and persistent TBI symptomology.47-50 Furthermore, we found that later administration of CTBIE was associated with greater headache severity and prevalence of migraine-like features. This is consistent with prior research suggesting that early diagnosis and intervention may be protective against poorer headache outcomes.51 Taking our findings together with extant literature, we advocate for earlier TBI/headache intervention and similar integrative multidisciplinary headache care for veterans with and without a confirmed history of TBI.
Acknowledgment
The authors thank Alexandra Ross for her assistance with data collection for this manuscript.
Glossary
- AOC
alteration of consciousness
- AOR
adjusted OR
- CTBIE
comprehensive TBI evaluation
- LOC
loss of consciousness
- NSI
Neurobehavioral Symptom Inventory
- OIF/OEF/OND
Operation Iraqi Freedom/Operation Enduring Freedom/Operation New Dawn
- OR
odds ratio
- PPE
personal protective equipment
- PTA
posttraumatic amnesia
- PTH
posttraumatic headache
- PTSD
posttraumatic stress disorder
- TBI
traumatic brain injury
- VA
Department of Veterans Affairs
- VATBIST
VA Traumatic Brain Injury Screening Tool
Appendix. Authors
Footnotes
CME Course: NPub.org/cmelist
Study Funding
Funding provided by the VA Headache Center of Excellence Program. The contents of this article do not represent the views of the VA or the US government.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Defense and Veterans Brain Injury Center. DoD TBI worldwide numbers: military health system. Accessed May 30, 2021. health.mil/About-MHS/OASDHA/Defense-Health-Agency/Research-and-Development/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBI-Worldwide-Numbers
- 2.Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev. 2009;46(6):697. [DOI] [PubMed] [Google Scholar]
- 3.Pugh MJV, Finley EP, Copeland LA, et al. Complex comorbidity clusters in OEF/OIF veterans: the polytrauma clinical triad and beyond. Med Care. 2014;52(2):172-181. [DOI] [PubMed] [Google Scholar]
- 4.Lucas S, Hoffman JM, Bell KR, Dikmen S. A prospective study of prevalence and characterization of headache following mild traumatic brain injury. Cephalalgia. 2014;34(2):93-102. [DOI] [PubMed] [Google Scholar]
- 5.Nampiaparampil DE. Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA. 2008;300(6):711-719. [DOI] [PubMed] [Google Scholar]
- 6.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211. [DOI] [PubMed] [Google Scholar]
- 7.Metti A, Schwab K, Finkel A, et al. Posttraumatic vs nontraumatic headaches: a phenotypic analysis in a military population. Neurology. 2020;94(11):e1137–e1146. [DOI] [PubMed] [Google Scholar]
- 8.Labastida-Ramírez A, Benemei S, Albanese M, et al. Persistent post-traumatic headache: a migrainous loop or not? The clinical evidence. J Headache Pain. 2020;21(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashina H, Iljazi A, Al-Khazali HM, et al. Persistent post-traumatic headache attributed to mild traumatic brain injury: deep phenotyping and treatment patterns. Cephalalgia. 2020;40(6):554-564. [DOI] [PubMed] [Google Scholar]
- 10.Theeler BJ, Flynn FG, Erickson JC. Headaches after concussion in US soldiers returning from Iraq or Afghanistan. Headache J Head Face Pain. 2010;50(8):1262-1272. [DOI] [PubMed] [Google Scholar]
- 11.Vanderploeg RD, Curtiss G, Luis CA, Salazar AM. Long-term morbidities following self-reported mild traumatic brain injury. J Clin Exp Neuropsychol. 2007;29(6):585-598. [DOI] [PubMed] [Google Scholar]
- 12.Ashina H, Porreca F, Anderson T, et al. Post-traumatic headache: epidemiology and pathophysiological insights. Nat Rev Neurol. 2019;15(10):607-617. [DOI] [PubMed] [Google Scholar]
- 13.Porter KE, Stein MB, Martis B, et al. Postconcussive symptoms (PCS) following combat-related traumatic brain injury (TBI) in veterans with posttraumatic stress disorder (PTSD): influence of TBI, PTSD, and depression on symptoms measured by the Neurobehavioral Symptom Inventory (NSI). J Psychiatr Res. 2018;102:8-13. [DOI] [PubMed] [Google Scholar]
- 14.Verfaellie M, Lafleche G, Spiro A III, Bousquet K. Neuropsychological outcomes in OEF/OIF veterans with self-report of blast exposure: associations with mental health, but not MTBI. Neuropsychology. 2014;28(3):337-346. [DOI] [PubMed] [Google Scholar]
- 15.Walker WC, Seel RT, Curtiss G, Warden DL. Headache after moderate and severe traumatic brain injury: a longitudinal analysis. Arch Phys Med Rehabil. 2005;86(9):1793-1800. [DOI] [PubMed] [Google Scholar]
- 16.Suri P, Stolzmann K, Iverson KM, et al. Associations between traumatic brain injury history and future headache severity in veterans: a longitudinal study. Arch Phys Med Rehabil. 2017;98(11):2118-2125.e1. [DOI] [PubMed] [Google Scholar]
- 17.Couch JR, Stewart KE. Headache prevalence at 4-11 years after deployment-related traumatic brain injury in veterans of Iraq and Afghanistan wars and comparison to controls: a matched case-controlled study. Headache J Head Face Pain. 2016;56(6):1004-1021. [DOI] [PubMed] [Google Scholar]
- 18.Bryan CJ, Hernandez AM. Predictors of post-traumatic headache severity among deployed military personnel. Headache J Head Face Pain. 2011;51(6):945-953. [DOI] [PubMed] [Google Scholar]
- 19.Lucas S, Hoffman JM, Bell KR, Walker W, Dikmen S. Characterization of headache after traumatic brain injury. Cephalalgia. 2012;32(8):600-606. [DOI] [PubMed] [Google Scholar]
- 20.Couch JR, Bearss C. Chronic daily headache in the posttrauma syndrome: relation to extent of head injury. Headache J Head Face Pain. 2001;41(6):559-564. [DOI] [PubMed] [Google Scholar]
- 21.Maleki N, Finkel A, Cai G, et al. Post-traumatic headache and mild traumatic brain injury: brain networks and connectivity. Curr Pain Headache Rep. 2021;25(3):20. [DOI] [PubMed] [Google Scholar]
- 22.Yumul JN, McKinlay A. Do multiple concussions lead to cumulative cognitive deficits? A literature review. PM R. 2016;8(11):1097-1103. [DOI] [PubMed] [Google Scholar]
- 23.Ruff RL, Riechers RG, Wang X-F, Piero T, Ruff SS. A case–control study examining whether neurological deficits and PTSD in combat veterans are related to episodes of mild TBI. BMJ Open. 2012;2(2):e000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.1Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358(5):453-463. [DOI] [PubMed] [Google Scholar]
- 25.Cernak I, Noble-Haeusslein LJ. Traumatic brain injury: an overview of pathobiology with emphasis on military populations. J Cereb Blood Flow Metab. 2010;30(2):255-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bryden DW, Tilghman JI, Hinds SR. Blast-related traumatic brain injury: current concepts and research considerations. J Exp Neurosci. 2019;13:1179069519872213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Donnelly K, Donnelly J, Dunnam M, et al. Reliability, sensitivity, and specificity of the VA traumatic brain injury screening tool. J Head Trauma Rehabil. 2011;26:439-453. [DOI] [PubMed] [Google Scholar]
- 28.Levin HS, Mattis S, Ruff RM, et al. Neurobehavioral outcome following minor head injury: a three-center study. J Neurosurg. 1987;66(2):234-243. [DOI] [PubMed] [Google Scholar]
- 29.Ruff R, Ruff S, Wang X-F. Headaches among Operation Iraqi Freedom/Operation Enduring Freedom veterans with mild traumatic brain injury associated with exposures to explosions. J Rehabil Res Dev. 2008;45:941-952. [DOI] [PubMed] [Google Scholar]
- 30.The Management of Concussion/mTBI Working Group. Management of concussion/mild traumatic brain injury. US Department of Veterans Affairs and US Department of Defense. Washington, DC: 2009. [Google Scholar]
- 31.Pontifex MB. Rmimic: an R package that mimic outputs of popular commercial statistics software packages with effect sizes and confidence intervals. 2020. github.com/mattpontifex/Rmimic. [Google Scholar]
- 32.US Department of Veterans Affairs. VA Information Resource Center. Accessed May 30, 2021. virec.research.va.gov.
- 33.Bomyea J, Lang AJ, Delano‐Wood L, et al. Neuropsychiatric predictors of post-injury headache after mild-moderate traumatic brain injury in veterans. Headache J Head Face Pain. 2016;56(4):699-710. [DOI] [PubMed] [Google Scholar]
- 34.Ponsford JL, Spitz G, McKenzie D. Using post-traumatic amnesia to predict outcome after traumatic brain injury. J Neurotrauma. 2016;33(11):997-1004. [DOI] [PubMed] [Google Scholar]
- 35.Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257. [DOI] [PubMed] [Google Scholar]
- 36.Lieb DA, Raiciulescu S, DeGraba T, Sours Rhodes C. Investigation of the relationship between frequency of blast exposure, mTBI history, and post-traumatic stress symptoms. Mil Med. Epub 2021 June 11. [DOI] [PubMed]
- 37.Seal KH, Bertenthal D, Samuelson K, Maguen S, Kumar S, Vasterling JJ. Association between mild traumatic brain injury and mental health problems and self-reported cognitive dysfunction in Iraq and Afghanistan veterans. J Rehabil Res Dev. 2016;53(2):185-198. [DOI] [PubMed] [Google Scholar]
- 38.Lindquist LK, Love HC, Elbogen EB. Traumatic brain injury in Iraq and Afghanistan veterans: new results from a national random sample study. J Neuropsychiatry Clin Neurosci. 2017;29(3):254-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bryan CJ, Clemans TA. Repetitive traumatic brain injury, psychological symptoms, and suicide risk in a clinical sample of deployed military personnel. JAMA Psychiatry. 2013;70(7):686. [DOI] [PubMed] [Google Scholar]
- 40.Goswami R, Dufort P, Tartaglia MC, et al. Frontotemporal correlates of impulsivity and machine learning in retired professional athletes with a history of multiple concussions. Brain Struct Funct. 2016;221(4):1911-1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ivanov I, Fernandez C, Mitsis EM, et al. Blast exposure, white matter integrity, and cognitive function in Iraq and Afghanistan combat veterans. Front Neurol. 2017;8:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manners JL, Forsten RD, Kotwal RS, Elbin RJ, Collins MW, Kontos AP. Role of pre-morbid factors and exposure to blast mild traumatic brain injury on post-traumatic stress in United States military personnel. J Neurotrauma. 2016;33(19):1796-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ryan-Gonzalez C, Kimbrel NA, Meyer EC, et al. Differences in post-traumatic stress disorder symptoms among post-9/11 veterans with blast- and non-blast mild traumatic brain injury. J Neurotrauma. 2019;36(10):1584-1590. [DOI] [PubMed] [Google Scholar]
- 44.Wilk JE, Thomas JL, McGurk DM, Riviere LA, Castro CA, Hoge CW. Mild traumatic brain injury (concussion) during combat: lack of association of blast mechanism with persistent postconcussive symptoms. J Head Trauma Rehabil. 2010;25(1):9-14. [DOI] [PubMed] [Google Scholar]
- 45.Phillips YY, Mundie TG, Yelverton JT, Richmond DR. Cloth ballistic vest alters response to blast. J Trauma Inj Infect Crit Care. 1988;28(suppl):S149-S152. [DOI] [PubMed] [Google Scholar]
- 46.Arcaya MC, Lowe SR, Asad AL, Subramanian SV, Waters MC, Rhodes J. Association of posttraumatic stress disorder symptoms with migraine and headache after a natural disaster. Health Psychol. 2017;36(5):411-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Howard L, Dumkrieger G, Chong CD, Ross K, Berisha V, Schwedt TJ. Symptoms of autonomic dysfunction among those with persistent posttraumatic headache attributed to mild traumatic brain injury: a comparison to migraine and healthy controls. Headache J Head Face Pain. 2018;58(9):1397-1407. [DOI] [PubMed] [Google Scholar]
- 48.Lagos L, Thompson J, Vaschillo E. A preliminary study: heart rate variability biofeedback for treatment of postconcussion syndrome. Biofeedback. 2013;41(3):136-143. [Google Scholar]
- 49.Tan G, Dao TK, Farmer L, Sutherland RJ, Gevirtz R. Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): a pilot study. Appl Psychophysiol Biofeedback. 2011;36(1):27-35. [DOI] [PubMed] [Google Scholar]
- 50.Minen MT, Corner S, Berk T, et al. Heartrate variability biofeedback for migraine using a smartphone application and sensor: a randomized controlled trial. Gen Hosp Psychiatry. 2021;69:41-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scher AI, Midgette LA, Lipton RB. Risk factors for headache chronification. Headache J Head Face Pain. 2008;48(1):16-25. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to VA regulations and Veterans Health Administration ethics agreements, the analytical datasets used for this study are not permitted to leave the VA firewall without a data-use agreement. This limitation is consistent with other studies based on VA data. However, VA data are made freely available to researchers with an approved VA study protocol. More information can be obtained online32 or by contacting the VA Information Resource Center at VIReC@va.gov.