Abstract
Particulate matters with a diameter of less than 10 µm (PM10) or less than 2.5 µm (PM2.5) are major air pollutants. Their relationship to psychiatric disorders has not yet been extensively studied. We aimed to explore the relationship between PM10 and PM2.5 air pollution peaks and the daily number of emergency visits for psychotic and mood disorders. Clinical data were collected from the Emergency Department of a Paris suburb (Créteil, France) from 2008 to 2018. Air pollution data were measured by the Paris region air quality network (Airparif) and collected from public databases. Pollution peak periods were defined as days for which the daily mean level of PM was above nationally predefined warning thresholds (20 µg/m3 for PM2.5, and 50 µg/m3 for PM10), and the 6 following days. Multivariable analyses compared the number of daily visits for psychotic and mood (unipolar and bipolar) disorders according to pollution peak, using negative binomial regression. After adjustment on meteorological variables (temperature, humidity, amount of sunshine in minutes), the daily number of emergency visits for psychotic disorders was significantly higher during PM2.5 and PM10 air pollution peak periods; while the number of visits for unipolar depressive disorders was higher only during PM10 peak periods (β = 0.059, p-value = 0.034). There were no significant differences between peak and non-peak periods for bipolar disorders. Differences in the effects of PM air pollution on psychotic and mood disorders should be analyzed in further studies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11356-022-21964-7.
Keywords: Air pollution peak, Emergency department, Mood disorders, Particulate matter, Psychotic disorders
Introduction
Ambient outdoor air pollution is presumed to cause 4.2 million premature deaths worldwide yearly, particularly as it is related to cardiovascular and pulmonary diseases as well as cancer (estimate for 2016) (World Health Organization (WHO), 2018). Exposure to particulate matter with a diameter of less than 2.5 (PM2.5) and 10 µm (PM10) is assumed to be among the main causal factors of this association (Risom et al. 2005; Ling and van Eeden 2009; Cao et al. 2012). Alongside these premature deaths, PM have also been linked to neurological diseases, such as multiple sclerosis and cerebral stroke (Leiva et al. 2013; Palacios et al. 2017; Zhang et al. 2018).
Concurrently, urbanicity has long been (and still is) considered to be a risk factor for several psychiatric disorders, including psychotic disorders as well as autism spectrum disorders (Vassos et al. 2012; Lauritsen et al. 2014). Indeed, the level of urbanicity (both as it concerns birthplace and place of residence during development to adulthood) is associated with the incidence of these psychiatric disorders, in a dose–response relationship. Air pollution has been mentioned as a factor that could (at least partly) explain these associations. Moreover, in vitro animal studies are in favor of a neuroinflammatory effect of exposure to PM (Block and Calderón-Garcidueñas 2009), which could also have implications for psychiatric disorders (Buoli et al. 2018). PM could affect the brain directly by translocating along the olfactory nerve and/or indirectly via systemic inflammation. This translocation could be involved in the neuroinflammation and oxidative stress which have been shown to be involved in the pathophysiology of psychotic and mood disorders (Réus et al. 2015; Howes and McCutcheon 2017).
The potential associations between air pollution and psychiatric conditions have been poorly studied thus far. In 2004, a first study displayed associations between the risk of schizophrenia and exposure to benzene and carbon monoxide (CO) — this study did not analyze the role of PM (Pedersen et al. 2004). In the second study, Khan et al. (2019) analyzed data from the USA and Denmark — PM were included in a global air quality indicator. Their results showed that the risk of several psychiatric disorders, including psychotic and mood (unipolar and bipolar) disorders, was associated with air quality. In addition, the relationships of exposure to PM (PM2.5 and PM10) with the severity of the course of psychiatric disorders have been studied in several studies and have recently been summarized in a systematic review of literature (Bernardini et al. 2020). These studies analyzed the associations between PM concentrations and the daily number of emergency visits for several psychiatric disorders which is believed to reflect the number of subjects with a first episode or relapse of these psychiatric disorders. A putative association between PM pollution peaks and this daily number would suggest an effect of PM on the course of these disorders. With regard specifically to psychotic disorders, different studies have found inconsistent results. For instance, in Israel, among patients suffering from schizophrenia, no association was found between the concentration of PM and the number of psychotic episodes; only a trend toward a positive correlation during periods with dominant eastern winds (which, according to the authors, are associated with significant variations in the level of air pollution) (Yackerson et al. 2014). In Beijing (China), analyzing different lag periods after a 10 μg/m3 increase in concentrations of PM, Gao et al. (2017) found a significant increase in the percentage of daily hospital admissions for psychotic disorders only among women with a lag of 0–6 days (1.74% increase for PM10, 1.38% for PM2.5, 2.20% for PM with diameters between 2.5 and 10 µm). Similarly, in another area of China, Duan et al. (2018) found a significant effect of PM10 concentration (90th and 95th percentiles) at various single- and multi-day periods and hospital admission for schizophrenia (e.g., lag 3 days for the 95th percentile of PM10 concentration: RR = 1.97, 95% CI [1.66–2.36], or lag 4 days: RR = 1.92, 95% CI [1.57–2.36]).
With regard to mood disorders, the situation is quite similar: the published studies found conflicting results with non-significant or only slightly significant associations (Braithwaite et al. 2019; Bernardini et al. 2020). For instance, in Edmonton (Canada), Szyszkowicz (2007) found significant associations between PM concentration and emergency visits for depression for women only and only during the cold season (increase in daily visits: 7.2%, 95% CI [2.7–12.0] for PM10 and 7.2%, 95% CI [2.0–12.8] for PM2.5). In 26 Chinese cities, both PM2.5 and PM10 levels were positively associated with the number of hospital admissions for depression (PM2.5: risk of hospitalization peaked 2.9% (95% CI [1.37–4.50]) on the first day of the pollution peak (lag 0 day) and 3.7% (95% CI [2.09–5.24]) for a lag of 5 days)) (Wang et al. 2018). Interestingly, like with subthreshold psychotic symptoms (Newbury et al. 2019), another study found a similar pattern for subthreshold symptoms of depression among older adults (lag 7 days: RR = 1.09 95 CI% [1.01–1.17]) (Pun et al. 2017).
The inconsistent results of the different studies on the influence of PM concentration on the number of emergency visits are probably related to the differing methodological designs of these studies including the following: different methods to estimate the impact of PM concentrations (deciles, increase of 10 μg/m3 in the concentrations), different risk periods (lag 0–6 days, lag 3 days, etc.), separate analyses by gender (Bernardini et al. 2020). Further reliable studies are necessary on this topic. Rather than the variety of methods used to measure the influence of PM concentration (increase, deciles, etc.), predefined PM air pollution peak thresholds could be used; and rather than multiple analyses (which are associated with an increase of the alpha risk), a unique level of lag days should be predefined. In addition, as pollution is closely linked to meteorological variables (temperature, humidity, etc.), they should be considered in the statistical analyses as adjustment factors. Finally, very few of the studies that considered the links between air pollution and psychiatric disorders took place in Europe, and none in France, and to our best knowledge, no studies have specifically examined the relationships between PM concentrations and emergency visits for bipolar disorders or whole mood — unipolar and bipolar — disorders (Buoli et al. 2018; Bernardini et al. 2020; Pignon et al. 2020b). If the association with air pollution is demonstrated and we accept causality, air pollution should be considered a population-level target to improve the course of psychotic and mood disorders.
With these issues in mind, in the present study, we explored the possible links between PM2.5 and PM10 air pollution peaks and the daily number of visits for psychotic and mood (unipolar and bipolar) disorders in one of the largest psychiatric emergency departments of the Paris suburbs. We hypothesized that the 3 considered outcome (the daily number of emergency visits for psychotic and mood (unipolar and bipolar)) disorders are associated with PM air pollution peaks.
Materials and methods
Data collection
Psychiatric emergency department visits outcomes
Clinical data were collected from the Emergency Department of the Centre Hospitalo-Universitaire Henri Mondor, a university-affiliated hospital based in Créteil (a suburb of Paris, France). It is the largest emergency department in the county (Val-de-Marne). The daily number of emergency visits for psychotic and mood disorders was extracted from January 1st, 2008, to December 31st, 2018 (11 years). Information about each case included the following: the date of the visit, the sex and age of the patient, and their diagnosis according to the International Classification of Diseases (10th Revision, ICD-10) (recorded by a psychiatrist). The selected diagnoses for the study were psychotic (F20-F29) and mood — unipolar depressive (F32-F39) and bipolar (F30-F31) — disorders.
Air pollution data
Air pollution data were collected and made available by the Airparif air quality monitoring network (https://www.airparif.asso.fr/). We selected the 5 measurement sites closest to the emergency department in a 20 km radius: Vitry-sur-Seine at 3.7 km, Nogent-sur-Marne at 5.5 km, Bobigny at 12.2 km, Lognes at 14.0 km, and Tremblay-en-France at 19.2 km. All of these sites are classified as urban, with the exception of Tremblay-en-France which is considered suburban. Airborne mass concentrations of PM were provided hourly at 2 sites for PM2.5 (Vitry-sur-Seine, Bobigny), and in all 5 sites for PM10. French guidelines were used to define the thresholds for a pollution peak: daily concentration of 20 µg/m3 for PM2.5, and 50 µg/m3 for PM10 (Haut Conseil de la Santé Publique 2012). A daily mean concentration of PM above the threshold, for any one of the measurement sites, was used as the definition for the presence of a PM peak day.
Meteorological data
As the impact of air pollution on health is dependent on meteorological conditions (Niu et al. 2021), the following variables were used as adjustment variables: temperature (T, °C), relative humidity (%), and daily duration of sunshine (in minutes) for the nearest meteorological station (7.1 km distance from the Henri-Mondor hospital). Meteorological data are freely available from the internet site of Météo France (https://www.meteofrance.com/) which is the official provider for meteorological and climate data in France.
Statistical analyses
Pollution peak day definition
This study compared the daily number of emergency visits between “pollution-peak days” and “non-pollution-peak days.” The “pollution-peak days” were defined as days during which the pollution threshold was exceeded in at least one of the 5 measurement sites and the 6 following days.
Multivariable analyses
Multivariable analyses compared the number of daily visits for psychotic and mood disorders according to the presence of a PM pollution peak on a given day or in the 6 following days. We used Poisson regression or, in the presence of an over-dispersion, negative binomial regression. Adjustment factors were daily temperature, daily relative humidity, and daily duration of sunshine.
Supplementary (correlation) analyses
To study the relationship between PM peaks and emergency visits on an annual basis, correlation analyses (Spearman correlation tests) were also conducted between the annual number of emergency visits and the number of annual PM pollution peaks.
Moreover, air pollution varies according to season, and the association with psychiatric outcomes could be different according to season (Kan et al. 2008). To test the hypothesis of a differential effect of air pollution according to season, the correlation between the number of episodes and the number of PM2.5 peaks was also tested in each quarter of the year (Spearman correlation tests).
All analyses were conducted using R software version 3.6.0.
Results
Descriptive statistics
From January 1st, 2008, to December 31st, 2018, a daily mean of 5.16 emergency visits (psychotic disorders: 2.16, unipolar depressive disorders: 2.54, bipolar disorders: 0.70) for the diagnoses of interest was recorded. The sociodemographic characteristics (age, sex) of the sample are available in Table 1.
Table 1.
Number of emergency room visits for psychotic and mood disorders from 2008 to 2018, and characteristics of patients
| N (%) or mean (standard-deviation) | ||
|---|---|---|
| Daily number of emergency visits for the diagnoses of interest | 5.16 (2.4) | |
| Total number of emergency visits for the diagnoses of interest | 20,727 | |
| Daily number of emergency visits |
Psychotic disorders Unipolar depressive disorders Bipolar disorders |
1.92 (1.4) 2.54 (1.6) 0.70 (0.8) |
| Sex (female) |
Psychotic disorders Unipolar depressive disorders Bipolar disorders |
2,838 (36.9%) 6,572 (64.4%) 1,706 (60.6%) |
| Age (years) |
Psychotic disorders Bipolar disorders Unipolar depressive disorders |
40.11 (11) 44.61 (14.7) 46.11 (12.5) |
During the study, 1040 PM2.5 peaks and 234 PM10 peaks were measured; 2355 (58.6% of the days in a calendar year) days were considered to be PM2.5 peak days, including 1550 without PM10 peaks (38.6% of the total number of days), and 805 (20.0%) as both PM2.5 and PM10 peak days. No PM10 peak was present in the absence of a PM2.5 peak, while 65.8% of the PM2.5 peak days occur in the absence of a PM10 peak (1550/2355, with a significant association between PM10 and PM2.5 peaks, see Supplementary Table 1). Thus, PM2.5 and PM10 peaks were not included together in the multivariable analyses, but we analyzed associations with PM2.5 peaks without a PM10 peak. The number of days with and without PM peaks, and the weather characteristics of the days according to PM peak are available in Table 2.
Table 2.
Weather characteristics (mean) of days with and without PM2.5 and PM10 peak1 pollution between 2008 and 2018
| Daily temperature (°C) | PM2.5 peak days | 9.8 |
| PM10 peak days | 7.4 | |
| Without PM2.5 days | 15.5 | |
| Without PM10 days | 13.3 | |
| Daily relative humidity (%) | PM2.5 peak days | 77.7 |
| PM10 peak days | 77.5 | |
| Without PM2.5 days | 71.9 | |
| Without PM10 days | 74.7 | |
| Daily time of sunshine (min) | PM2.5 peak days | 259.5 |
| PM10 peak days | 256.3 | |
| Without PM2.5 days | 343.7 | |
| Without PM10 days | 305.5 |
Regarding the raw rates, the average daily number of emergency visits for psychotic disorders was higher during PM2.5 and PM10 pollution peak days than in non-peak pollution days (PM2.5: 1.95 visits/day during peak vs. 1.87 visits/day without peak; PM10: 2.00 vs. 1.90), likewise for mood disorders (unipolar: PM2.5: 2.58 vs. 2.48, PM10: 2.68 vs. 2.51; bipolar: PM2.5: 0.71 vs. 0.69, PM10: 0.71 vs. 0.68). Details are available in the Table 3.
Table 3.
Daily number of emergency visits for psychotic disorders according to the presence of PM2.5 or PM10 peak
| Psychotic disorders | Unipolar depressive disorders | Bipolar disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PM2.5 peak days1 | No PM2.5 peak day | PM10 peak days | No PM10 peak day | PM2.5 peak days | No PM2.5 peak day | PM10 peak days | No PM10 peak day | PM2.5 peak days | No PM2.5 peak day | PM10 peak days | No PM10 peak day | |
| Total number of visits | 4,601 | 3113 | 1612 | 6102 | 6082 | 4118 | 2154 | 8046 | 1629 | 1184 | 548 | 2265 |
| Proportion (%) | 59.6 | 40.4 | 20.9 | 79.1 | 59.6 | 40.4 | 21.1 | 78.9 | 57.9 | 42.1 | 19.5 | 80.5 |
| Mean daily number of consultations | 1.95 | 1.87 | 2.00 | 1.90 | 2.58 | 2.48 | 2.68 | 2.51 | 0.71 | 0.69 | 0.71 | 0.68 |
| Standard-deviation | 1.4 | 1.4 | 1.4 | 1.4 | 1.7 | 1.7 | 1.7 | 1.7 | 0.9 | 0.8 | 0.8 | 0.8 |
Association between PM pollution peaks and daily number of emergency visits
For both psychotic and mood disorders, as the data displayed significant overdispersion, multivariable analyses used negative binomial regression. The daily number of emergency visits for psychotic disorders was not associated with the presence of PM2.5 nor PM10 peaks in the univariate analysis, while the multivariable analyses displayed a significant positive association with PM2.5 (β = 0.066, 95% CI [0.013–0.119], p-value = 0.014) and PM10 peaks (β = 0.064, 95% CI [0.000–0.127], p-value = 0.048). Details of these analyses are available in Table 4.
Table 4.
Relationships between the daily number of emergency visits for psychotic disorders and the presence of a PM2.5 and/or PM10 air pollution peak
| Univariate analysis | Multivariable analyses concerning PM10 | Multivariable analyses concerning PM2.5 | Multivariable analyses concerning only PM2.51 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | |
| PM10 | 0.052 | − 0.00283–0.10695 | 0.062 | 0.06433 | 0.00036–0.12773 | 0.048 | - | - | - | - | - | - |
| PM2.5 | 0.0415 | − 0.00385–0.08712 | 0.073 | 0.06592 | 0.01332–0.11858 | 0.014 | 0.02001 | − 0.02941–0.06924 | 0.427 | |||
| Daily temperature | 0.0024 | − 0.00095–0.00577 | 0.160 | 0.00427 | − 0.00021–0.00877 | 0.062 | 0.00473 | 0.00024–0.00923 | 0.039 | 0.00272 | − 0.00144–0.00691 | 0.201 |
| Daily relative humidity | -0.0010 | − 0.00274–0.00084 | 0.299 | − 0.00009 | − 0.00322–0.00306 | 0.956 | − 0.00055 | − 0.00367–0.00259 | 0.731 | -0.00051 | − 0.00366–0.00265 | 0.750 |
| Daily amount of sunshine | 0.0001 | − 0.00004–0.00015 | 0.231 | 0.00001 | − 0.00014–0.00016 | 0.893 | − 0.00000 | − 0.00015–0.00015 | 0.999 | 0.00001 | − 0.00014–0.00016 | 0.913 |
Legend:
Abbreviations: PM2.5 and PM10: particulate matter less than 2.5 and 10 µm
1PM2.5 pollution peak without PM10 pollution peak
Significant associations appear in bold
With regard to unipolar depressive disorders, the daily number of emergency visits was negatively associated with PM2.5 peaks and positively associated with PM10 peaks in univariate analyses, but only with PM10 peaks (β = 0.059, 95% CI [0.004–0.114], p-value = 0.034) in the multivariable analyses. Details of these analyses are available in the Table 5.
Table 5.
Relationships between the daily number of emergency visits for unipolar depressive disorders and the presence of a PM2.5 and/or PM10 air pollution peak
| Univariate analysis | Multivariable analyses concerning PM10 | Multivariable analyses concerning PM2.5 | Multivariable analyses concerning only PM2.51 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | |
| PM10 | 0.0409 | 0.01788–0.11298 | 0.007 | 0.0594 | 0.0042–0.1142 | 0.034 | - | - | - | - | - | - |
| PM2.5 | − 0.0034 | 0.00134–0.08045 | 0.043 | - | - | - | 0.0205 | − 0.0255–0.0665 | 0.382 | -0.0180 | -0.0612–0.0251 | 0.413 |
| Daily temperature | − 0.0011 | − 0.00633– − 0.00049 | 0.022 | − 0.0022 | − 0.0061–0.0017 | 0.269 | − 0.0031 | − 0.0070–0.0008 | 0.120 | -0.0039 | − 0.0075– − 0.0003 | 0.035 |
| Daily relative humidity | 0.0005 | − 0.00104–0.00209 | 0.513 | 0.0007 | − 0.0020–0.0035 | 0.609 | 0.0004 | − 0.0023–0.0031 | 0.776 | 0.0006 | − 0.0022–0.0033 | 0.680 |
| Daily amount of sunshine | 0.0000 | − 0.00007–0.00009 | 0.762 | 0.0001 | − 0.0001–0.0002 | 0.268 | 0.0001 | − 0.0001–0.0002 | 0.284 | 0.0001 | − 0.0001–0.0002 | 0.244 |
Legend:
Abbreviations: PM2.5 and PM10: particulate matter less than 2.5 and 10 µm
1PM2.5 pollution peak without PM10 pollution peak
Significant associations appear in bold
No significant association was found where involving bipolar mood disorders. Details of these analyses are available in the Table 6.
Table 6.
Relationships between the daily number of emergency visits for bipolar disorders and the presence of a PM2.5 and/or PM10 air pollution peak
| Univariate analysis | Multivariable analyses concerning PM10 | Multivariable analyses concerning PM2.5 | Multivariable analyses concerning only PM2.51 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | |
| PM10 | − 0.0356 | − 0.12977–0.05688 | 0.455 | − 0.0081 | − 0.1144–0.0965 | 0.880 | - | - | - | - | - | - |
| PM2.5 | − 0.0301 | − 0.10476–0.04495 | 0.431 | - | - | - | − 0.0192 | − 0.1052–0.0670 | 0.662 | − 0.0122 | − 0.0935–0.0686 | 0.769 |
| Daily temperature | 0.0016 | − 0.00394–0.00719 | 0.568 | − 0.0013 | − 0.0086–0.0060 | 0.724 | − 0.0017 | − 0.0091–0.0056 | 0.643 | − 0.0012 | − 0.0080–0.0056 | 0.732 |
| Daily relative humidity | − 0.0018 | − 0.00475–0.00116 | 0.233 | 0.0001 | − 0.0050–0.0053 | 0.960 | 0.0002 | − 0.0049–0.0054 | 0.934 | 0.0003 | − 0.0049–0.0054 | 0.924 |
| Daily amount of sunshine | 0.0001 | − 0.00005–0.00025 | 0.173 | 0.0001 | − 0.0001–0.0004 | 0.315 | 0.0001 | − 0.0001–0.0004 | 0.304 | 0.0001 | − 0.0001–0.0004 | 0.309 |
Legend:
Abbreviations: PM2.5 and PM10: particulate matter less than 2.5 and 10 µm
1PM2.5 pollution peak without PM10 pollution peak
Supplementary (correlation) analyses
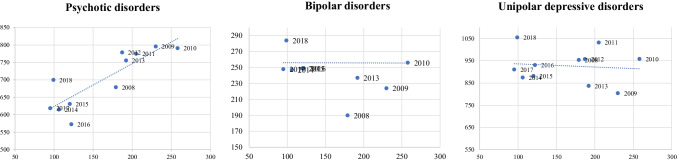
Correlation tests revealed a significant positive correlation between annual PM2.5 pollution peaks and number of emergency visits for psychotic disorders (correlation coefficient = 0.79, p-value = 0.004), and non-significant correlations for unipolar depressive and bipolar disorders (see Supplementary Table 2 for details). The scatter plots of the annual number of emergency visits for psychotic, bipolar, and unipolar depressive disorders according to the annual number of pollution peaks of PM2.5 are available in the Fig. 1.
Fig. 1.
Scatter plots of annual number of emergency visits (y) and number of PM2.5 pollution peak days (x)
Correlation analyses per quarter concerning psychotic disorders revealed that correlations were similar in the first quarter (from January to March), and not significant for the other quarters, while for unipolar depressive disorders, the correlations were significant (and negative) for the third quarter, and not significant in the other quarters. With regard to bipolar disorders, the correlations were not significant for the four quarters (see Supplementary Table 3 for details).
Discussion
This 11-year cohort study analyzes the relationships between PM air pollution and psychiatric outcomes, namely the number of emergency department visits for psychotic and mood (unipolar and bipolar) disorders for the first time in France. The results show a significant association between PM2.5 and PM10 air pollution peaks and the daily number of emergency visits for psychotic disorders. The number of daily emergency visits for unipolar depressive disorders was also higher during PM10 peak. Finally, no associations were found for bipolar disorders.
Comparisons with previous studies
In a systematic review of studies focusing on associations between air pollutants and daily hospital admissions and/or emergency department admissions for psychiatric care, Bernardini et al. (2020) identified 19 studies (including 9 that analyzed psychiatric disorders as a whole, without specifying the diagnoses). Among the different analyzed air pollutants, the strongest and most consistent evidence of an association with psychiatric disorders was found with PM10: regarding all the considered psychiatric disorders, 13 of the 16 studies that analyzed the influence of PM10 and 8 of the 12 studies for PM2.5 found significant associations. Interestingly, these consistent results were found with different methods: (i) analyzing the influence of PM with different lag periods (e.g., lag 0 and lag 0–1 days (Lee et al. 2019), lag 0 to 3 (Kim et al., 2019), etc.) and (ii) most analyzed the influence of a 10 μg/m3 increase of PM, whereas we analyzed the number of visits according to the presence or not of a pollution peak (i.e., above predefined official thresholds defining a risk to humans). Thus, our study using another design (lag 7 days, and a binary PM peak variable according to predefined air pollution thresholds) confirms an exarcerbating effect of air pollution on psychotic and unipolar depressive episodes. A strength of our analyses is the adjustments for daily temperature, daily relative humidity, and daily sunshine (which are associated with the outcomes, cf. for instance a negative association between daily temperature and number of admissions for unipolar depressive disorders, consistent with the literature (Wortzel et al. 2019)). The fact that annual correlations were significant suggests that PM air pollution could also have a cumulative effect. However, multivariable analyses are necessary to clarify this issue (that were not possible in the present study, because of statistical power issues, N = 11 in the present study).
Regarding psychotic disorders specifically, as stated previously, the results of prior studies were inconsistent — with some showing significant results (Duan et al. 2018), and some that did not find any significant associations, or only among subgroups (Yackerson et al. 2014; Gao et al. 2017; Bernardini et al. 2020). Interestingly, only one study analyzed hospital admissions according to similar PM thresholds (25 µg/m3 for PM2.5 vs. 20 in the current study, and 50 µg/m3 for PM10 in both studies) and found consistent results (fraction of hospital admission for schizophrenia attributable to exceeding PM2.5 threshold: 15.13%, 95% CI [1.83–25.50%], PM10: 15.32%, 95% CI [3.49–24.56%]) (Qiu et al. 2019).
Results concerning unipolar depressive disorders were similar to those for psychotic disorders, with a significant positive association between the number of daily emergency visits and PM10 peak. The Qiu et al. (2019) study that analyzed hospital admissions according to PM threshold found consistent results (fraction of hospital admission for depression attributable to exceeding PM2.5 threshold: 12.07%, 95% CI [0.10–21.81%], PM10: 6.10%, 95% CI [1.40–10.32%]). Consistently, in their systematic review focusing on the psychiatric consequences of exposures of PM, Braithwaite et al. (2019) found that short-term increases in PM exposures appeared to be globally positively associated with emergency department visits for depression in seven studies. Of note, the negative association between PM2.5 peak and the number of emergency visits for unipolar depressive disorders in univariate analysis was not confirmed in the multivariable analyses and could be related to confounding factors, for instance weather conditions, which are known to have a significant impact on mood disorders (Geoffroy et al., 2017; Geoffroy et al., 2014).
An association between PM peaks and bipolar disorders had never been studied before and thus our results could not be compared with prior studies, but the absence of any significant variations is still surprising, particularly with regard to the fact that bipolar disorders share some (environmental or genetic) risk factors and pathophysiology with psychotic disorders (Demjaha et al. 2012; Bellivier et al. 2013; Pignon et al. 2019) and unipolar depressive disorders (Arango et al. 2021).
Pathophysiological considerations
Several pathophysiological hypotheses have been formed to explain the role of PM pollution in the etiology and severity of psychiatric disorders. The central nervous system may be affected by inflammatory and oxidative processes — particularly due to increased levels of inflammatory cytokines (Block and Calderón-Garcidueñas 2009; Buoli et al. 2018) that are considered to be causal mechanisms of psychiatric disorders (Leboyer et al. 2012, 2016; Howes and McCutcheon 2017; Müller 2018). Increased stress cortisol production and hypothalamo-pituitary-adrenal axis dysregulation — which are also involved in the etiology of psychiatric disorders (Zorn et al. 2017; Cherian et al. 2019) — may also play a role (Li et al. 2017; Miller et al. 2020). A body of evidence is in favor of global blood vessel pollution-related damage affecting white matter, cortical gray matter, and basal ganglia (de Prado Bert et al. 2018). PM may also affect cognitive development (Zhang et al. 2018), or global psychological well-being (Orru et al. 2016; Nakao et al. 2017). Of note, these alterations may reflect chronic more than acute (e.g., recent PM peak) exposure. Research remains to be done on the specific pathways and neurobiological impact of short and long-term PM exposures, and their relationships with specific psychiatric disorders, such as mood and psychotic disorders, that have specific pathophysiology. This research could address the issue of the observed differences in associations between air pollution and the different psychiatric disorders.
Limitations
Several limitations to our study should be acknowledged. First, individual factors related to mood or psychotic exacerbation, such as stressful-life events, socioeconomic status, cannabis consumption, or inflammatory events and physical comorbidities, could not be analyzed within the scope of our study. Environmental factors such as noise levels, or access to and use of green space, were also not within the scope of our study (Gascon et al. 2018; Engemann et al. 2020). Moreover, indoor pollution, daily exposure to other air pollutants (such as nitrogen dioxide or ozone) automobile traffic, and/or tobacco use, which may have a large impact on the level of PM exposure, could also not be analyzed. Finally, in the analyses, as the data was anonymous, we were unable to remove duplicate subjects.
Unfortunately, the lockdown period linked to the COVID-19 pandemic was not included in our study. This period could be very interesting to study. In a prior study, we showed that the number of emergency visits for psychiatric disorders dramatically decreased during the 4 first weeks of lockdown, in comparison to the corresponding weeks of 2019 (more than 50% decrease) (Pignon et al. 2020a). During the same time, the level of air pollution decreased, potentially explaining (at least in part) the decrease in the number of emergency visits (Hamzaoui et al. 2021). However, several other factors were modified during this period and could also be involved, such as diet and/or sleep habits and the use of alcohol and other substances (Rolland et al. 2020; Bennett et al. 2021; Bertrand et al. 2022).
Conclusions
For the first time in France, we analyzed the relationships between recent exposure to a PM air pollution peak (according to predefined thresholds) and emergency department visits for psychotic, unipolar, and bipolar mood disorders. After adjustment on meteorological data, multivariable analyses show a significant association between PM10 and PM2.5 air pollution peak and the daily number of visits for psychotic disorders, and between PM10 air pollution peak and the daily number of visits for unipolar depressive disorders. These analyses were confirmed by a significant correlation between the annual number of PM2.5 air pollution peaks and the number of visits for psychotic disorders. The major strengths of this study are the long period of data collection, the ecological design, the adjustment on weather variables, and the study of three psychiatric outcomes using the same methodology. Moreover, contrary to similar prior studies (Gao et al. 2017; Duan et al. 2018), we did not use a large number of statistical analyses. These results move us toward a better understanding of the pathophysiology of psychotic disorders and reinforce arguments for reducing PM emissions, especially in densely populated areas. Other studies — particularly prospective studies — are necessary to understand the relationships between air pollution (including PM and their sources or other air pollutants, such as nitrogen dioxide) and the severity and course of psychiatric disorders.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- 95% CI
95% Confidence interval
- OR
Odds-ratio
- PM
Particulate matter
- PM10
Particulate matter with diameter less than 10 µm
- PM2.5
Particulate matter with diameter less than 2.5 µm
- RR
Relative risk
- WHO
World Health Organization
Author contribution
Baptiste Pignon, Cynthia Borel, Jean-Romain Richard, Andrei Szöke, Gilles Foret, and Franck Schürhoff participated in the conception and design of the study; François Hemery and Gilles Foret participated in the acquisition of data; Mohamed Lajnef and Jean-Romain Richard performed the analyses; Baptiste Pignon and Cynthia Borel wrote the first draft of the manuscript. All authors participated in the writing and revision of the successive drafts of the manuscript and approved the final version.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethical approval
The study was performed in accordance with the Declaration of Helsinki. The data were extracted anonymously from registers, in accordance with the ethical standards of the French National Data Protection Authority.
Consent to participate
As the data was extracted anonymously, without possible identifying information, consent for inclusion was not requested.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Arango C, Dragioti E, Solmi M, et al. Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World Psychiatry off J World Psychiatr Assoc WPA. 2021;20:417–436. doi: 10.1002/wps.20894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellivier F, Geoffroy PA, Scott J, et al. Biomarkers of bipolar disorder: specific or shared with schizophrenia? Front Biosci Elite Ed. 2013;5:845–863. doi: 10.2741/e665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett G, Young E, Butler I, Coe S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: a scoping review. Front Nutr. 2021;8:626432. doi: 10.3389/fnut.2021.626432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardini F, Trezzi R, Quartesan R, Attademo L. Air pollutants and daily hospital admissions for psychiatric care: a review. Psychiatr Serv. 2020;71:1270–1276. doi: 10.1176/appi.ps.201800565. [DOI] [PubMed] [Google Scholar]
- Bertrand L, Schröder C, Bourgin P, et al. Sleep and circadian rhythm characteristics in individuals from the general population during the French COVID-19 full lockdown. J Sleep Res. 2022;31:e13480. doi: 10.1111/jsr.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32:506–516. doi: 10.1016/j.tins.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite I, Zhang S, Kirkbride JB, et al. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect. 2019;127:126002. doi: 10.1289/EHP4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buoli M, Grassi S, Caldiroli A, et al. Is there a link between air pollution and mental disorders? Environ Int. 2018;118:154–168. doi: 10.1016/j.envint.2018.05.044. [DOI] [PubMed] [Google Scholar]
- Cao J, Xu H, Xu Q, et al. Fine particulate matter constituents and cardiopulmonary mortality in a heavily polluted Chinese city. Environ Health Perspect. 2012;120:373–378. doi: 10.1289/ehp.1103671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherian K, Schatzberg AF, Keller J. HPA axis in psychotic major depression and schizophrenia spectrum disorders: cortisol, clinical symptomatology, and cognition. Schizophr Res. 2019;213:72–79. doi: 10.1016/j.schres.2019.07.003. [DOI] [PubMed] [Google Scholar]
- de Prado BP, Mercader EMH, Pujol J, et al. The Effects of air pollution on the brain: a review of studies interfacing environmental epidemiology and neuroimaging. Curr Environ Health Rep. 2018;5:351–364. doi: 10.1007/s40572-018-0209-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demjaha A, MacCabe JH, Murray RM. How genes and environmental factors determine the different neurodevelopmental trajectories of schizophrenia and bipolar disorder. Schizophr Bull. 2012;38:209–214. doi: 10.1093/schbul/sbr100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan J, Cheng Q, Luo X, et al. Is the serious ambient air pollution associated with increased admissions for schizophrenia? Sci Total Environ. 2018;644:14–19. doi: 10.1016/j.scitotenv.2018.06.218. [DOI] [PubMed] [Google Scholar]
- Engemann K, Pedersen CB, Agerbo E, et al. Association between childhood green space, genetic liability, and the incidence of schizophrenia. Schizophr Bull. 2020;46:1629–1637. doi: 10.1093/schbul/sbaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Q, Xu Q, Guo X, et al. Particulate matter air pollution associated with hospital admissions for mental disorders: a time-series study in Beijing, China. Eur Psychiatry J Assoc Eur Psychiatr. 2017;44:68–75. doi: 10.1016/j.eurpsy.2017.02.492. [DOI] [PubMed] [Google Scholar]
- Gascon M, Sánchez-Benavides G, Dadvand P, et al. Long-term exposure to residential green and blue spaces and anxiety and depression in adults: a cross-sectional study. Environ Res. 2018;162:231–239. doi: 10.1016/j.envres.2018.01.012. [DOI] [PubMed] [Google Scholar]
- Geoffroy PA, Bellivier F, Scott J, Etain B. Seasonality and bipolar disorder: a systematic review, from admission rates to seasonality of symptoms. J Affect Disord. 2014;168:210–223. doi: 10.1016/j.jad.2014.07.002. [DOI] [PubMed] [Google Scholar]
- Geoffroy PA, Godin O, Mahee D, et al. Seasonal pattern in bipolar disorders and cardio-vascular risk factors: a study from the FACE-BD cohort. Chronobiol Int. 2017;34:845–854. doi: 10.1080/07420528.2017.1324472. [DOI] [PubMed] [Google Scholar]
- Hamzaoui I, Duthil B, Courboulay V, Medromi H. Environmental impacts of pre/during and post-lockdown periods on prominent air pollutants in France. Environ Dev Sustain. 2021;23:14140–14161. doi: 10.1007/s10668-021-01241-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haut Conseil de la Santé Publique (2012) Pollution par les particules dans l’air ambiant. Synthèse et recommandations pour protéger la santé. In: Ministère Solidar. Santé. https://solidarites-sante.gouv.fr/IMG/pdf/av_0412.pdf. Accessed 9 Jun 2022
- Howes OD, McCutcheon R. Inflammation and the neural diathesis-stress hypothesis of schizophrenia: a reconceptualization. Transl Psychiatry. 2017;7:e1024. doi: 10.1038/tp.2016.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan H, London SJ, Chen G, et al. Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: the public health and air pollution in asia (PAPA) Study. Environ Health Perspect. 2008;116:1183–1188. doi: 10.1289/ehp.10851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A, Plana-Ripoll O, Antonsen S, et al. Environmental pollution is associated with increased risk of psychiatric disorders in the US and Denmark. PLOS Biol. 2019;17:e3000353. doi: 10.1371/journal.pbio.3000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Shin SD, Song KJ, et al. Association between ambient PM2.5 and emergency department visits for psychiatric emergency diseases. Am J Emerg Med. 2019;37:1649–1656. doi: 10.1016/j.ajem.2018.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauritsen MB, Astrup A, Pedersen CB, et al. Urbanicity and autism spectrum disorders. J Autism Dev Disord. 2014;44:394–404. doi: 10.1007/s10803-013-1875-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leboyer M, Berk M, Yolken RH, et al. Immuno-psychiatry: an agenda for clinical practice and innovative research. BMC Med. 2016;14:173. doi: 10.1186/s12916-016-0712-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leboyer M, Soreca I, Scott J, et al. Can bipolar disorder be viewed as a multi-system inflammatory disease? J Affect Disord. 2012;141:1–10. doi: 10.1016/j.jad.2011.12.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Lee W, Kim D, et al. Short-term PM2.5 exposure and emergency hospital admissions for mental disease. Environ Res. 2019;171:313–320. doi: 10.1016/j.envres.2019.01.036. [DOI] [PubMed] [Google Scholar]
- Leiva MAG, Santibañez DA, Ibarra SE, et al. A five-year study of particulate matter (PM2.5) and cerebrovascular diseases. Environ Pollut. 2013;181:1–6. doi: 10.1016/j.envpol.2013.05.057. [DOI] [PubMed] [Google Scholar]
- Li H, Cai J, Chen R, et al. Particulate matter exposure and stress hormone levels. Circulation. 2017;136:618–627. doi: 10.1161/CIRCULATIONAHA.116.026796. [DOI] [PubMed] [Google Scholar]
- Ling SH, van Eeden SF. Particulate matter air pollution exposure: role in the development and exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2009;4:233–243. doi: 10.2147/copd.s5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JG, Gillette JS, Kircanski K, et al. Air pollution is associated with elevated HPA-axis response to stress in anxious adolescent girls. Compr Psychoneuroendocrinology. 2020;4:100015. doi: 10.1016/j.cpnec.2020.100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller N. Inflammation in schizophrenia: pathogenetic aspects and therapeutic considerations. Schizophr Bull. 2018;44:973–982. doi: 10.1093/schbul/sby024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakao M, Yamauchi K, Ishihara Y, et al. Effects of air pollution and seasons on health-related quality of life of Mongolian adults living in Ulaanbaatar: cross-sectional studies. BMC Public Health. 2017;17:594. doi: 10.1186/s12889-017-4507-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbury JB, Arseneault L, Beevers S, et al. Association of air pollution exposure with psychotic experiences during adolescence. JAMA Psychiat. 2019;76:614–623. doi: 10.1001/jamapsychiatry.2019.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu Z, Qi Y, Zhao P, et al. Short-term effects of ambient air pollution and meteorological factors on tuberculosis in semi-arid area, northwest China: a case study in Lanzhou. Environ Sci Pollut Res. 2021;28:69190–69199. doi: 10.1007/s11356-021-15445-6. [DOI] [PubMed] [Google Scholar]
- Orru K, Orru H, Maasikmets M, et al. Well-being and environmental quality: Does pollution affect life satisfaction? Qual Life Res. 2016;25:699–705. doi: 10.1007/s11136-015-1104-6. [DOI] [PubMed] [Google Scholar]
- Palacios N, Munger KL, Fitzgerald KC, et al. Exposure to particulate matter air pollution and risk of multiple sclerosis in two large cohorts of US nurses. Environ Int. 2017;109:64–72. doi: 10.1016/j.envint.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen CB, Raaschou-Nielsen O, Hertel O, Mortensen PB. Air pollution from traffic and schizophrenia risk. Schizophr Res. 2004;66:83–85. doi: 10.1016/S0920-9964(03)00062-8. [DOI] [PubMed] [Google Scholar]
- Pignon B, Geoffroy PA, Thomas P, et al. Environment risk factors have different impact on bipolar and psychotic disorders: an analysis of MHGP survey. Psychol Med. 2019;49:1229–1232. doi: 10.1017/S0033291719000229. [DOI] [PubMed] [Google Scholar]
- Pignon B, Gourevitch R, Tebeka S, et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin Neurosci. 2020;74:557–559. doi: 10.1111/pcn.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignon B, Szöke A, Forêt G, et al. Air pollution and psychiatric disorders: current and future challenges. Bipolar Disord. 2020;22:437–439. doi: 10.1111/bdi.1296. [DOI] [PubMed] [Google Scholar]
- Pun VC, Manjourides J, Suh H. Association of Ambient air pollution with depressive and anxiety symptoms in older adults: results from the NSHAP study. Environ Health Perspect. 2017;125:342–348. doi: 10.1289/EHP494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu H, Zhu X, Wang L, et al. Attributable risk of hospital admissions for overall and specific mental disorders due to particulate matter pollution: a time-series study in Chengdu, China. Environ Res. 2019;170:230–237. doi: 10.1016/j.envres.2018.12.01. [DOI] [PubMed] [Google Scholar]
- Réus GZ, Fries GR, Stertz L, et al. The role of inflammation and microglial activation in the pathophysiology of psychiatric disorders. Neuroscience. 2015;300:141–154. doi: 10.1016/j.neuroscience.2015.05.01. [DOI] [PubMed] [Google Scholar]
- Risom L, Møller P, Loft S. Oxidative stress-induced DNA damage by particulate air pollution. Mutat Res. 2005;592:119–137. doi: 10.1016/j.mrfmmm.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N (2020) Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early covid-19 containment phase in the general population in France: Survey Study. JMIR Public Health and Surveillance 6(3):e19630 [DOI] [PMC free article] [PubMed]
- Szyszkowicz M. Air pollution and emergency department visits for depression in Edmonton, Canada. Int J Occup Med Environ Health. 2007;20:241–245. doi: 10.2478/v10001-007-0024-2. [DOI] [PubMed] [Google Scholar]
- Vassos E, Pedersen CB, Murray RM, et al. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38:1118–1123. doi: 10.1093/schbul/sbs096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Liu H, Li H, et al. Ambient concentrations of particulate matter and hospitalization for depression in 26 Chinese cities: a case-crossover study. Environ Int. 2018;114:115–122. doi: 10.1016/j.envint.2018.02.012. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2018) Ambient (outdoor) air pollution. https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. Accessed 16 Oct 2020
- Wortzel JR, Norden JG, Turner BE, et al. Ambient temperature and solar insolation are associated with decreased prevalence of SSRI-treated psychiatric disorders. J Psychiatr Res. 2019;110:57–63. doi: 10.1016/j.jpsychires.2018.12.017. [DOI] [PubMed] [Google Scholar]
- Yackerson NS, Zilberman A, Todder D, Kaplan Z. The influence of air-suspended particulate concentration on the incidence of suicide attempts and exacerbation of schizophrenia. Int J Biometeorol. 2014;58:61–67. doi: 10.1007/s00484-012-0624-9. [DOI] [PubMed] [Google Scholar]
- Zhang X, Chen X, Zhang X. The impact of exposure to air pollution on cognitive performance. Proc Natl Acad Sci. 2018;115:9193–9197. doi: 10.1073/pnas.1809474115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorn JV, Schür RR, Boks MP, et al. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;77:25–36. doi: 10.1016/j.psyneuen.2016.11.036. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.