Abstract
Few studies have examined the psychological impact on adolescents of family confinement and infection exposure during the COVID-19 pandemic. However, these surveys lacked follow-up data to determine how the family confinement affects participants’ depression and anxiety. The purpose of this study was to evaluate the psychological status and related risk and protective factors of adolescents after two months of family confinement for preventing COVID-19 in China, and compare them with baseline data. We surveyed teenagers in January 2020 before the COVID-19 outbreak (T1) and after home confinement (T2). We used the Patient Health Questionnaire (PHQ), the Generalized Anxiety Disorder (GAD) Scale and the Childhood Trauma Questionnaire (CTQ). 13,637 valid questionnaires were collected at T1, of which 22.34% reported depressive symptoms (PHQ-9 ≥ 10) and 14.42% reported anxiety symptoms (GAD-7 ≥ 10). At T2, the rates decreased to 14.86 and 7.44%, respectively (all P < 0.0001). Of the adolescents, 223 reported potential risk of exposure to COVID-19. We then compared them to the 9639 non-risk adolescents using a propensity score matching analysis. The adolescents with potential exposure risk had higher rates of depression (26.91 vs 15.32%, P = 0.0035) and anxiety (14.80 vs 7.21%, P = 0.01) than risk-free adolescents. Among adolescents with an exposure risk, psychological resilience was protective in preventing depression and anxiety symptoms, while emotional abuse, a poor parent–child relationship were risk factors. Long-term home confinement had minimal psychological impact on adolescents, but COVID-19 infection rates accounted for 50% of the variance in depression and anxiety among adolescents even with low community rates.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00406-022-01459-9.
Keywords: Adolescents, COVID-19, Mental health, Family confinement, Depression, Anxiety
Introduction
With the spread of COVID-19 across the world, closing schools and keeping social-distance have been regarded as the only effective strategy to stop the spread of the pandemic[1, 2], especially covert infections[3]. The World Health Organization (WHO) reports that since governments closed schools and substituted teaching at home online, more than 1.5 billion children and 90% of global students have remained at home and been relatively isolated from peers, raising concerns about home confinement[4, 5]. In China, there are few online surveys showing that COVID-19 may affect the adolescents’ psychological status [5–9]. Moreover, these surveys lack baseline data to determine whether the pandemic has exacerbated the participants’ depression and anxiety. Therefore, a longitudinal study on the psychological profile of adolescents before and after the COVID-19 outbreak is warranted.
On the other hand, poor parent–child relationships and abuse have been shown to directly increase the occurrence of depression and anxiety among adolescents [10, 11]. Meanwhile, psychological resilience to cope with difficulties can moderate depression and anxiety caused by an adverse environment [12]. However, these important factors were not taken into account in previous studies on the mental status of adolescents in home confinement. Therefore, our study of adolescents in confinement at home was designed to assess the parent–child relationships, adverse experiences, and resilience for coping with depression or anxiety.
In this longitudinal study, we have baseline information because just before the outbreak of COVID-19 we conducted a Nationwide Investigation on Psychological Health in Early Adolescents of China (NIPHEAC) and completed the first round (T1) in January 2020 in five cities’ middle schools. After two months of the home confinement, in March 2020, we conducted the second-round survey (T2) on the participants from the T1 survey. T2 survey was done after COVID-19 infections had spread minimally in these five cities. Our purpose for this paper was to assess the impact of both home confinement and its interaction with early stage COVID-19 infection on these adolescents’ psychological status and compare it to their pre-pandemic status. We expected to better understand changes in these adolescents’ anxiety and depression during long-term home confinement, and to formulate better quarantine policies for the future.
Methods
Longitudinal study setting and participants
NIPHEAC is a school-based, two-round survey on anxiety, depression, childhood abuse and correlative factors among students of middle school [grade 7 (age 13), 8 (age 14) and 9 (age 15)]. This study began in November 2019 and was designed for two rounds of surveys, with 3 months between each survey. The first round was a pen-paper survey, while the second rounds were online surveys. All the procedures of survey were shown in Flowchart (Supplementary file).
At the baseline, the middle school samples were selected through a two-stage cluster sampling method. In the first stage, 5 cities or counties were randomly selected from the stratified regional framework of China. In the second stage, a whole middle school was randomly selected from the list of middle schools provided by the local education bureau of the selected city or county. We adopted the whole sampling method, and conducted a survey of all students in the school according to our protocol. We selected five representative middle schools in the general population across China. These five representative middle schools were located in the cities of QingDao, ZaoZhuang, GongYi, Yulin and DongGang across the provinces of Shandong, Henan, Shanxi and Liaoning, respectively. We surveyed all the students in these schools at the round one.
Our data collection protocol followed the American Association for Public Opinion Research (AAPOR) reporting guidelines, and was approved by the Ethics in Human Research Committee of the Third Affiliated Hospital of Beijing University of Chinese Medicine (No. BZYSY-2019KYKTPJ-21). On the day before the investigation, the head teacher informed each student in the class of the details of the survey and asked the students to tell their parents or guardians. The head teachers collected signed forms from the adolescents and their parents or guardians before handing out the questionnaire. All students participated in this study voluntarily and students had a choice to decline participation. In addition, all adolescents were anonymous because no privacy-related information, such as name, ID, cell phone, and home phone number, was recorded in the questionnaire.
Patient and Public Involvement statement: patients and the public were not or will not be involved in the design, or conduct, or reporting, or dissemination plans of the research.
Longitudinal survey administration practices
First round of survey
We conducted the first survey (T1) from November 22, 2019 to January 4, 2020. Eight experienced staff administered this survey to all students in 5 middle schools. The staff distributed uniform-printed questionnaires to each classroom, read the instructions aloud in Mandarin, answered the students’ questions, observed the students during the survey and collected the completed surveys.
The criteria of invalid questionnaires are pre-defined as follows: (1) Less than 90% of the paper questionnaire was completed. (2) Unreasonable or illogical data was found in the questionnaire. (3) Important data such as gender or age were not completed. (4) Staff confirmed that the student hadn’t filled in the questionnaire seriously.
Second round of survey
We conducted the second survey round from March 21 to March 31, 2020, using exactly the same questions from the first round questionnaire and converting them into online digital questionnaires by the professional version of Wenjuanxing. Wenjuanxing (www.wjx.cn) is an online crowd source platform in mainland China, which is equivalent to Amazon Machinery Turkey [13].
In order to ensure the effectiveness of the online survey, we conducted online training for the head teachers in advance. After online class, all teachers released the link of questionnaire to students according to the protocol, and supervised the students to fill out and submit the questionnaire. During the online survey, the head teacher obtained a list of students who had not participated in the online survey. If the response rate of a grade was less than 80%, then 5% of no-responders were randomly selected and contacted by the head teacher by phone to make sure that they completed the online survey. The data of 5% of non-respondents were used to investigate the bias of non-respondents and adjust the effect of non-response.
The criteria of invalid questionnaires are pre-defined as follows: (1) We added two questions to test the validity of the answers, namely, “I answered all questions honestly.” “All of my answers were based on my real experiences and thoughts.” We provided a “yes” and “no” option and arranged them in a different order in the two questions. If either of these two questions was answered as “no”, then the questionnaire was considered invalid. (2) Participants spent less than 3 min (result from internal test) to complete the survey. (3) Different data was repeatedly submitted from the same IP address. (4) Unreasonable and illogical data were found.
We retrieved 14,241 questionnaires in the first survey round (T1) and 10,768 in the second round (T2). Excluding invalid questionnaires left 96% (13,637) from T1 and 95% (10,216) from T2 as valid questionnaires. The valid follow-up rate was 75% (10,216/13,637) and varied by region (P < 0.001). To examine whether the 25% T2 non-responders differed from the T2 responders, we randomly selected and had 202 T2 non-respondents complete the questionnaire. We found no substantial differences between these two groups (Supplemental Table 1).
Main outcome measures
We used Chinese versions of validated measurement tools, and all interpretations of the scores and cutoff values were based on previous studies [14–21]. We measured depression symptoms using the 9-item Patient Health Questionnaire (PHQ-9; range 0–27), and anxiety symptoms using the 7-item Generalized Anxiety Disorder (GAD-7) Scale (range, 0–21). The total scores were interpreted as: PHQ-9, normal (0–4), mild (5–9), moderate (10–14), and severe (15–27) depression [22, 23]; GAD-7, normal (0–4), mild (5–9), moderate (10–14), and severe (15–21) anxiety [24]. The cut-off value for clinically relevant depression and anxiety symptoms was all set as 10 [14, 22, 25]. We considered students who scored over the cut-off point as having symptoms.
We assessed childhood abuse using the short form of the Childhood Trauma Questionnaire (CTQ-SF; range 25–125) [12, 18], which is a retrospective self-reporting quantitative measurement tool consisting of 28 items and five subscales. The names and cutoff values of each subscale are as follows: emotional abuse (> = 13), physical abuse (> = 10), sex abuse (> = 8), emotional neglect (> = 15) and physical neglect (> = 10) [26, 27]. The Cronbach alpha for total questionnaire composed of these scales was 0.851 in the first round survey and 0.773 in the second round.
We measured psychological resilience using the Connor-Davidson Resilience Scale (CD-RISC; range 0–100) [12, 20, 21]. The CD-RISC consists of 25 items to assess stress and coping ability. Higher scores indicate stronger resilience. These scales showed high internal consistency (Cronbach alpha = 0.927in first round, 0.918 in second round) in these study samples.
The background factors and demographic data were gender, age, siblings, parent marital status, baseline diseases, and parent–child relationship. Parent–child relationship were collected by asking whether he/she got along well with his/her parents. In T2 survey, we designed the question to survey exposure risk to COVID-19: “Is there anyone in your living environment who is infected with COVID-19?”. We provided four available options, namely “Yes, it’s my relatives/friends”, “Yes, it’s someone in my community”, “Definitely not”, and “I don’t know”. If a participant chose the first or second option, or both, the participant was considered to have a potential risk of exposure to COVID-19. All the data were self-reported by the participants through these questionnaires.
Statistical analysis
We used a Shapiro–Wilk test, Q–Q plot and p–p plot to confirm normality for continuous variables. Age and psychological resilience score were reported as the mean ± standard deviation (SD), and non-normally distributed continuous variables, such as depression, anxiety and childhood abuse scores, were described using the median and interquartile ranges (IQRs). We used Student’s t or the nonparametric Wilcoxon test to assess any statistically significant differences.
We presented gender, status of siblings, marital status of parents, parent–child relationship, depression, anxiety and childhood abuse as numbers and percentages, and used χ2 tests. The Pearson analysis was performed to assess the correlation coefficient between the incidence of COVID-19 in enrolled cities and the scores of depression and anxiety. We adjusted the effect of non-response using the Ratio and Regression Estimation [28].
To compare the scores and severity of depressive and anxiety symptoms in adolescents with and without potential risk of exposure to COVID-19 and to account for selection bias caused by non-random assignment of participants with different demographic and abuse factors, we performed propensity score matching (PSM). A propensity score (probability of exposure to risk) was estimated using multivariate logistic regression, using a caliper from 0.0001 to 0.1 of the SD, with adolescents with or without risk as the dependent variable.
We performed all statistical analyses using SAS (Version 9.2; SAS Institute Inc., Cary, North Carolina, USA) software with statistical significance set at P = 0.05 (2-sided).
Results
The rate of valid questionnaires and follow-up
We retrieved 14,241 questionnaires in the first survey round (T1) and 10,768 in the second round (T2). Excluding invalid questionnaires left 96% (13,637) from T1 and 95% (10,216) from T2 as valid questionnaires. The valid follow-up rate was 75% (10,216/13,637) and varied by region (P < 0.001). To examine whether the 25% T2 non-responders differed from the T2 responders, we randomly selected and had 202 T2 non-respondents complete the questionnaire (Supplementary Table 1). The data were applied to adjust the effect of non-response using the Ratio and Regression Estimation.
Psychological outcomes of adolescents in two rounds of survey
As shown in Table 1, the adolescents had lower depression and anxiety and higher psychological resilience scores at T2 than at T1 (Table 1). For depressive symptoms, the rate was 22.34%(3046/13637) in T1 decreased to 14.86%(1518/10216) in T2, and the adjusted rate was 14.81% in the T2. For anxiety symptom, the rate was 14.42%(1961/13637) in T1 decreased to 7.44%(760/10216) in T2, and the adjusted rate was 8.05% in the T2.
Table 1.
Demographic and psychological characteristics of first and second round responders
| First round(N = 13,637) | Second round(N = 10,216) | P value | Effect size dCohen (95%CI) | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, mean ± SD | 13.77 ± 1.02 | 14.33 ± 1.12 | < .0001 | 0.53 (0.50, 0.55) |
| Gender, categories no. (%) | 0.7908 | |||
| Boys | 6993(51.28) | 5221(51.11) | ||
| Girls | 5221(48.72) | 4995(48.89) | ||
| Regions, categories no. (%) | < .0001 | |||
| YuLin city | 1924(14.11) | 1892(18.52) | ||
| ZaoZhuang city | 3380(24.79) | 2363(23.13) | ||
| DanDong city | 1001(7.34) | 580(5.68) | ||
| QingDao city | 3524(25.84) | 2694(26.37) | ||
| GongYi city | 3808(27.92) | 2687(26.3) | ||
| Only child, categories no. (Yes/No) | 3291/10294 | 2532/7684 | 0.3205 | |
| Marital status of parents, categories no. (%) | 0.1945 | |||
| Married | 12,323(90.73) | 9291(90.95) | ||
| Divorced | 631(4.65) | 461(4.51) | ||
| Remarried | 394(2.9) | 262(2.56) | ||
| Single | 234(1.72) | 202(1.98) | ||
| Parent–child relationship, categories no. (%) | 0.1105 | |||
| Poor | 345(2.54) | 266(2.6) | ||
| Moderate | 3145(23.19) | 2485(24.32) | ||
| Good | 10,074(74.27) | 7465(73.07) | ||
| Live with parents, categories no. (%) | 0.0006 | |||
| No | 675(7.96) | 411(4.02) | ||
| Yes | 12,932(92.04) | 9805(95.98) | ||
| Psychological characteristics | ||||
| PHQ-9, depression symptoms score, median (IQR) | 5(2,9) | 3(0,7) | < .0001 | 0.30 (0.27,0.33) |
| Categories no. (%) | < .0001 | |||
| No symptom (0–9) | 10,591(77.66) | 8698 (85.14) | ||
| With symptoms (10–27) | 3046 (22.34) | 1518 (14.86) | ||
| Categories no. (%) | < .0001 | |||
| Normal (0–4) | 6612(48.49) | 6304(61.71) | ||
| Mild (5–9) | 3979(29.18) | 2394(23.43) | ||
| Moderate (10–14) | 1685(12.36) | 878(8.59) | ||
| Severe (15–27) | 1361(9.98) | 640(6.26) | ||
| GAD-7, anxiety symptoms score, median (IQR) | 3(1,7) | 1(0,4) | < .0001 | 0.39 (0.36, 0.42) |
| Categories no. (%) | < .0001 | |||
| No symptom (0–9) | 11,670 (85.58) | 9456 (92.56) | ||
| With symptoms (10–21) | 1967 (14.42) | 760 (7.44) | ||
| Categories no. (%) | < .0001 | |||
| Normal (0–4) | 8382(61.47) | 7792(76.27) | ||
| Mild (5–9) | 3288(24.11) | 1664(16.29) | ||
| Moderate (10–14) | 1217(8.92) | 438(4.29) | ||
| Severe (15–21) | 750(5.5) | 322(3.15) | ||
| Resilience score, mean ± SD | 2.27 ± 0.73 | 3.43 ± 0.74 | < .0001 | 1.58 (1.55, 1.61) |
| Emotional abuse score, median (IQR) | 6(5,9) | 7(5,9) | < .0001 | 0.12 (0.09, 0.14) |
| Categories no. (%) | 0.5548 | |||
| No experience (< 13) | 12,526(91.85) | 9362(91.64) | ||
| With experience (> = 13) | 1111(8.15) | 854(8.36) | ||
| Physical abuse score, median (IQR) | 5(5,6) | 5(5,5) | < .0001 | 0.15 (0.12, 0.18) |
| Categories no. (%) | < .0001 | |||
| No experience (< 10) | 12,852(94.24) | 9803(95.96) | ||
| With experience (> = 10) | 785(5.76) | 413(4.04) | ||
| Sex abuse score, median (IQR) | 5(5,5) | 5(5,5) | < .0001 | 0.11 (0.08, 0.13) |
| Categories no. (%) | < .0001 | |||
| No experience (< 8) | 13,209(96.86) | 10,008(97.96) | ||
| With experience (> = 8) | 428(3.14) | 208(2.04) | ||
| Emotional neglect score, median (IQR) | 10(7,14) | 9(6,13) | < .0001 | 0.12 (0.09, 0.14) |
| Categories no. (%) | < .0001 | |||
| No experience (< 15) | 10,613(77.83) | 8356(81.79) | ||
| With experience (> = 15) | 3024(22.17) | 1860(18.21) | ||
| Physical neglect score, median (IQR) | 8(6,10) | 6(5,9) | < .0001 | 0.29 (0.27, 0.32) |
| Categories no. (%) | < .0001 | |||
| No experience (< 10) | 9899(72.59) | 8236(80.62) | ||
| With experience (> = 10) | 3738(27.41) | 1980(19.38) | ||
PHQ-9 9-item patient health questionnaire, GAD-7 7-item generalized anxiety disorder
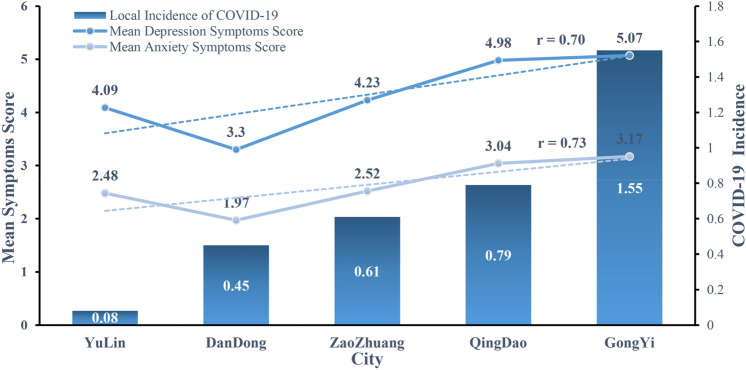
In the second round (T2), the incidence of COVID-19 in each city was associated with depressive symptoms in the cities (Fig. 1). The T2 survey was done after COVID-19 infections had spread minimally in these five cities, but COVID-19 infection rates accounted for half of the variance (r2 = 0.53) in depression and anxiety among adolescents.
Fig. 1.
Correlation Between the Mean Depression or Anxiety Symptoms Scores and the COVID-19 Incidence in Enrolled Cities. Shown are the mean scores of depression and anxiety symptoms, the local incidence of COVID-19 (per 100,000 population) and their correlation in five cities
Outcomes in adolescents with and without risk of exposure to COVID-19
Among 10,216 adolescents surveyed in T2, 223 adolescents reported that their relatives/friends, or someone in community were infected, 354 adolescents reported that they didn’t know whether there was infected case in living environment. 10,216-223-354 = 9639. A total of 9639 adolescents reported that there was definitely no infected case in their living environment. Because the mean symptom scores and infection rates were low, we focused on the 223 adolescents who reported a risk of COVID-19 exposure. Among them, 195 reported that someone in their community was infected with COVID-19, 21 reported that their close relatives or friends were infected, and 7 adolescents reported both. These three groups did not differ (all P > 0.05) in their depression and anxiety symptoms (Supplementary Table 2).
However, these 223 reported significantly higher rates of depression and anxiety than adolescents without such risk (N = 9639), as shown in (Table 2). Because the two groups differed on demographic and abuse factors, we used PSM analysis to match and statistically adjust for regions, age, sex, siblings, parental marital status, parent–child relationship, child abuse and psychological resilience score. After applying the matching algorithm, 222 respondents were retained, and adolescents at risk for exposure still had more depression (median [IQR] PHQ-9 scores: 6 [2, 10] vs 3 [1, 8]; P < 0.0001, rate: 60 [26.91%] vs 34 [15.32%]; P = 0.0035) and anxiety symptoms (median [IQR] GAD-7 scores: 3 [0,7] vs 1 [0,5]; P = 0.0002, rate: 33 [14.80%] vs 16 [7.21%]; P = 0.01) than those without risk (Table 2).
Table 2.
Comparison between adolescents with and without potential risk of exposure to COVID-19
| Adolescents with potential risk N = 223 |
Adolescents without risk N = 9639 |
P value | Matched adolescents without risk N = 222 |
P value | |
|---|---|---|---|---|---|
| Psychological characteristics | |||||
| PHQ-9, depression symptoms score, median (IQR) | 6 (2,10) | 3 (0, 7) | < .0001 | 3 (1,8) | < .0001 |
| Categories no. (%) | 0.0035 | ||||
| No symptom (0–9) | 163 (73.09) | 8305 (86.16) | < .0001 | 188 (84.68) | |
| With symptoms (10–27) | 60 (26.91) | 1334 (13.84) | 34 (15.32) | ||
| Categories no. (%) | < .0001 | < .0001 | |||
| Normal (0–4) | 88 (39.46) | 6103 (63.32) | 137 (61.71) | ||
| Mild (5–9) | 75 (33.63) | 2202 (22.84) | 51 (22.97) | ||
| Moderate (10–14) | 30 (13.45) | 781 (8.1) | 19 (8.56) | ||
| Severe (15–27) | 30 (13.45) | 553 (5.74) | 15 (6.76) | ||
| GAD-7, anxiety symptoms score, median (IQR) | 3 (0,7) | 1 (0, 4) | < .0001 | 1 (0,5) | 0.0002 |
| Categories no. (%) | |||||
| No symptom (0–9) | 190 (85.20) | 8982 (93.18) | < .0001 | 206 (92.79) | 0.0100 |
| With symptoms (10–21) | 33 (14.80) | 657 (6.82) | 16 (7.21) | ||
| Categories no. (%) | < .0001 | 0.0339 | |||
| Normal (0–4) | 131 (58.74) | 7480 (77.6) | 156 (70.27) | ||
| Mild (5–9) | 59 (26.46) | 1502 (15.58) | 50 (22.52) | ||
| Moderate (10–14) | 18 (8.07) | 383 (3.97) | 9 (4.05) | ||
| Severe (15–21) | 15 (6.73) | 274 (2.84) | 7 (3.15) | ||
Association between COVID-19 exposure risk and psychological outcomes
Univariate logistic regression analysis showed that depression (OR, 2.3; 95%CI, 1.7–3.1; P < 0.0001) and anxiety symptoms (OR, 2.4; 95%CI, 1.6–3.5; P < 0.0001) were more common in adolescents with than without exposure risk to COVID-19. In the meantime, being girls (OR, 1.7; 95%CI, 1.4–1.8; P < 0.0001; OR, 1.6; 95%CI, 1.4–2.0; P < 0.0001) and having experience of emotional abuse (OR, 5.6; 95%CI, 4.7–6.8; P < 0.0001; OR, 5.0; 95%CI, 4.1–6.2; P < 0.0001) were also risk factors, while psychological resilience (OR, 0.45; 95%CI, 0.41–0.50; P < 0.0001; OR, 0.46; 95%CI, 0.41–0.53; P < 0.0001) and good parent–child relationship (OR, 0.18; 95%CI, 0.13–0.25; P < 0.0001; OR, 0.26; 95%CI, 0.18–0.37; P < 0.0001) were protective factors of depression and anxiety respectively. After controlling for age, gender, resilience score, childhood abuse scores, marital status of parents and parent–child relationship, we continued to show that the adolescents with high exposure risk had greater depression (OR, 1.8; 95%CI, 1.2–2.5; P = 0.0018) and anxiety symptoms (OR, 1.7; 95%CI, 1.1–2.7; P = 0.0126) (Table 3).
Table 3.
Impacts of potential risk of exposure to COVID-19 on depression and anxiety symptoms identified by multivariable logistic regression analysis
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | |
| Depression symptoms | ||||||||
| Adolescents without potential risk | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Adolescents with potential risk | 2.292 (1.695,3.098) | < .0001 | 1.916 (1.390,2.641) | < .0001 | 1.874 (1.323,2.656) | 0.0004 | 1.766 (1.235,2.526) | 0.0018 |
| Anxiety symptoms | ||||||||
| Adolescents without potential risk | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Adolescents with potential risk | 2.376 (1.628,3.467) | < .0001 | 1.966 (1.325,2.916) | 0.0008 | 1.832 (1.194,2.809) | 0.0055 | 1.737 (1.126,2.681) | 0.0126 |
NA not applicable
Model 1: Univariate logistic regression;
Model 2: Model 1 and further adjusted for Resilience Score;
Model 3: Model 2 and further adjusted for Childhood abuse;
Model 4: Model 3 and further adjusted for Marital Status of Parents, Parent–child relationship, Age and Gender
Behavioral protective and risk factors in adolescents with COVID-19 exposure risk
Multivariable stepwise forward logistic regression analysis showed that in the 223 adolescents with exposure risk, greater psychological resilience was protective in preventing depression (OR, 0.35; 95% CI, 0.21–0.61; P = 0.0002) and anxiety symptoms (OR, 0.32; 95% CI, 0.16–0.65; P = 0.0013). Adolescents reporting emotional abuse were more likely to develop depression (OR, 1.3; 95%CI, 1.2–1.4; P < 0.0001) and anxiety symptoms (OR, 1.2; 95% CI, 1.1–1.4; P = 0.0001). Other risk and protective factor relevant to anxiety alone was a good parent–child relationship (OR, 0.12; 95% CI, 0.02–0.68; P = 0.0168) (Table 4).
Table 4.
Associated factors of depression and anxiety symptoms in 223 adolescents with potential risk of exposure to COVID-19
| Depression symptoms | Anxiety symptoms | |||
|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Resilience score | 0.354 (0.206,0.608) | 0.0002 | 0.324 (0.162,0.644) | 0.0013 |
| Emotional abuse score | 1.287 (1.166,1.420) | < .0001 | 1.224 (1.104,1.357) | 0.0001 |
| Parent–child relationship | ||||
| Poor | NA | NA | 1 [Reference] | NA |
| Moderate | NA | NA | 0.121 (0.021,0.684) | 0.0168 |
| Good | NA | NA | 0.133 (0.025,0.724) | 0.0796 |
NA not applicable
Discussion
Our study had four major findings. (1) The incidence and severity of anxiety and depression in 10,216 adolescents were lower after the outbreak of the pandemic than that before confinement. (2) The potential risk of exposure to COVID-19 even with low community rates of infection was a strong independent risk factor for anxiety and depression during confinement. (3) The adolescents with risk of exposure to COVID-19 not only had significantly higher rates and severity of anxiety and depression based on infection risk, but had additive risks from emotional abuse. (4) Psychological resilience or coping strategies and a good parent–child relationship were protective in preventing depression and anxiety, when faced with COVID-19 infection risk.
The mental status impact of confinement on adolescents
Overall, the study found no increase in anxiety and depressive symptoms after two months of home confinement, the rates were considerably higher at T1 than at T2. Although several other studies have reported relatively high rates of anxiety and depressive symptoms among adolescents during the COVID-19 outbreak [6–9], however, according to the review of Racine et al. these surveys lack baseline data [29] to determine whether participants’ depression and anxiety are a pre-pandemic continuation of the or are caused only by the pandemic. In addition, the results of these studies are similar to our results at T2. For example, Chen et al. reported that 13.35% of adolescents had depressive symptoms during the outbreak [6], while in our study, the rate was 14.86% at T2. Only one survey of American adolescents had baseline data and found that the scores of depression and anxiety scale increased slightly after the outbreak of COVID-19, compared with those before the outbreak. However, in this study, the depression and anxiety scores of adolescents before and after the pandemic were low, which had no clinical significance. For example, the average values of GAD-7 before and after the outbreak were 1.64 and 1.85, respectively [30].
Our study suggests that many Chinese children are better off in quarantine than at school. Although this finding is counterintuitive and at odds with most other studies, it generally seems premature to recommend school closures as soon as possible. We think that this may be due to the objective school or education environment in China. As we all know, the main purposes of education in Chinese schools are to obtain higher scores in the National College Entrance Examination through repeated exercises and examinations [31]. The examination-centered pedagogy has been proved to be the main stressor and cause of anxiety and inadequate psychological development of Chinese students [32]. In schools, there are many tests and examinations, as well as strict rules and regulations, while during home confinement, children simply stay at home without extracurricular activities, school tests and examination, and without a strict school environment, which may help reduce anxiety and depression[31].
According to Brooks et al. [33], the main stressors during quarantine were long duration of quarantine, fear of infection[34], withdraw from one’s social network (no phone or internet), insufficient supplies of food or other necessities, reduced income[35], and stigma[36]. Brooks suggested that increased communication with family and friends could reduce the negative impact of quarantine. Therefore, there are several other reasons that may explain why we found no negative psychological impact in our adolescents after home confinement during this early phase of COVID-19 infection.
First, among the 10,216 adolescents, only 223 had COVID-19 cases in their living circumstance, therefore, most adolescents had no fear of infection. Second, in our study, 95.98% of the adolescents were at home confinement with their parents, and communicated with them or other family members daily, to mitigate any stress caused by confinement. Third, when adolescents attended class online, they could interact with teachers and friends, without feeling isolated from their social networks. Fourth, adolescents have no financial or daily responsibilities for essential supplies, unlike their parents or other adults. Fifth, since all the schools were shut down and all the student were at home, no stigma would be acquired. Sixth, the relatively low incidence of COVID-19 in our surveyed regions, ranging from 0.8 to 1.3 per 100,000 populations [37], might have produced low levels of anxiety and depression. However, the simple five-point correlation between the mean symptom levels with the five local rates of COVID-19 infection showed a significant positive association of more symptoms with higher incidence of infection, which accounted for half of the variance in these measures (Fig. 1). This association was more pronounced when adolescents with a high risk of infection were compared to those with a low risk of infection.
The psychological impact of exposure risk of COVID-19
Consistent with the quarantine literature[7, 34, 36, 38], we found that the 223 adolescents with a high risk of COVID-19 exposure had a significantly higher rate of depression (26.91%) and anxiety (14.8%) symptoms than those without this risk (15.32 and 7.21% respectively). Furthermore, the exposure risk outweighed other risk factors such as few abuse experiences, meanwhile the exposure risk also outweighed the protective factors of the family structure, a good parent–child relationship and high psychological resilience, in reducing these adolescents’ anxiety and depression symptoms. Previous studies identified the fear of infection as a primary stressor during quarantine [39, 40], and another study also showed that acquaintance with or exposure to a confirmed case of SARS was correlated with depressive symptoms [38]. A third study from the USA reported that 30% of children, who were quarantined after contacting confirmed cases of SARS or H1N1, met criteria for Posttraumatic Stress Disorder (PTSD) [41]. Therefore, previous studies have shown that adolescents who are at high risk of exposure to severe infections have a higher rate of depression and anxiety symptoms. Although in this study, during the COVID-19 epidemic, depression and anxiety scores were not substantially higher than the T1 scores, the incidence of depression and anxiety was significantly higher among the 223 high-risk adolescents exposed to COVID-19 than that of the control group.
The risk factors of depression and anxiety in adolescents with exposure risk
Previous emotional abuse is also a risk factor of anxiety and depression in the 223 adolescents with exposure risk for COVID-19. These associations are consistent with a broader literature of Chinese adolescents, which shows that for every 1 point increase of emotional abuse scores, the risk of multiple suicidal attempts increased by 12 and 23%, respectively [26]. Furthermore, strong associations are observed between childhood emotional abuse and the diagnoses of major depression and anxiety disorders [42–44], and having poor family relationships leads to anxiety and depression in adolescents [45].
In contrast, psychological resilience or an ability to show positive defenses [46] and effective adaptations [47] to adversity, moderates the effects of adverse circumstances [48] and childhood abuse among Chinese [12] and Turkish [49] adolescents. Psychological resilience is dynamic and can increase after natural disasters, often called post-traumatic growth (PTG) [50]. With PTG, adolescents take more responsibility and develop prosocial behaviors after adverse experiences. Overall, consistent with the PTG literature, most of our adolescent’s resilience scores significantly increased after two months of home confinement, in spite of no significant changes in emotional or physical abuse during these two months. Family support and family structure also play important roles during PTG. The good parent–child relationship is regarded as primary preventive measure of children’s psychological disorders, Numerous studies show that learning effective parenting skills and improving family relationships can promote adolescent mental health.
In summary, our results suggest that adolescents at risk of exposure to COVID-19 should be regularly monitored by parents and education workers, especially those adolescents with poor parent–child relationships, and emotional abuse. Moreover, parents need to communicate with adolescents and seek professional mental health intervention when faced with a high risk of COVID-19 infection [5]. Some factors would be interesting to assess in future studies (extended home confinement, brutal grief, intrafamilial violence, overuse of the Internet and social media) [51]. The assessment of addictive behaviors may also be pertinent in future studies [52].
Our study had both limitations and strengths. We had three main limitations. First, paper and pencil questionnaires were used to collect baseline data at the T1 survey, while we conducted the T2 survey online, which may cause instrumental bias. Second, a quarter of the participants from the T1 survey did not respond to the T2 survey, although no obvious non-respondent bias were found based on the analysis in 202 no-respondents at T2, we have used Ratio and Regression Estimation [28] to adjust the non-responder effect. Third, all our data were adolescents’ self-reports. These self-reports from the adolescents might have limited the accuracy of their own parent–child relationship assessments and of their risk for exposure to COVID-19. In addition, the parent–child relationship was only collected by verbally asking him/her if he/she got along well with his/her parents, and we did not use psychological tools to collect this information. However, we also had several strengths. First, we obtained pre-pandemic baseline psychological data on a relatively large sample of adolescents for investigating the changes in them after confinement. Second, we collected factors related to depression and anxiety, such as abuse, psychological resilience, and parent–child relationships. Third, we found 223 cases of adolescents with potential exposure to COVID-19, and performed PSM analyses to confirm the adverse psychological effects of potential COVID-19 exposure on these adolescents.
In these five cities with a low incidence of COVID-19, we found no adverse psychological impact on adolescents after home confinement for 2 months unless the adolescent had a perceived direct risk of COVID-19 exposure. Thus, it is suggested that school closure should be implemented as soon as possible before an epidemic with a high contagion risk spread. This action will also minimize the psychological impact of adolescents becoming exposed to the trauma of a risk for infection, which appears to induce both depression and anxiety symptoms. Moreover, adolescents at potential risk of exposure to COVID-19, or living in an area with high rates of infection might be at serious risk of psychological harm, and interventions should be considered quickly, especially for adolescents with a poor parent–child relationship, and emotional abuse. However, our finding should be interpreted with caution, as adolescents may report fewer symptoms of psychological distress during the initial few months into the pandemic. The current data suggest that prolonged home confinement is associated with academic struggles and significantly increased depressive and anxiety symptoms reporting by adolescents.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
MQ and KY: participated in the design of the study, conducted the analyses, and wrote the manuscript. YJC: conducted the survey and collected data. XW: contributed to interpretation of the data. XYZ and MHX: conceived and coordinated the design of the study, and wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Key R&D Program of China (2020YFC2003100, 2020YFC2003103) and the National Natural Science Foundation of China (Grant No.81973759).
Declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Miao Qu and Kun Yang contributed equally to this work.
Contributor Information
Mei Hong Xiu, Email: xiumeihong97@163.com.
Xiang Yang Zhang, Email: zhangxy@psych.ac.cn.
References
- 1.Pan A, Liu L, Wang C, Guo H, et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. Jama. 2020;323:1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prem K, Liu Y, Russell TW, Kucharski AJ, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qiu J (2020) Covert coronavirus infections could be seeding new outbreaks. Nature News [DOI] [PubMed]
- 4.Organization WH (2020) Coronavirus disease 2019 (COVID-19) Situation Report–77. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200406-sitrep-77-covid-19.pdf?sfvrsn=21d1e632_2. Accessed 06 Apr 2020
- 5.Wang G, Zhang Y, Zhao J, Zhang J, et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen F, Zheng D, Liu J, Gong Y, et al. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav Immun. 2020;88:36–38. doi: 10.1016/j.bbi.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duan L, Shao X, Wang Y, Huang Y, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qi M, Zhou SJ, Guo ZC, Zhang LG, et al. The effect of social support on mental health in chinese adolescents during the outbreak of COVID-19. J Adolesc Health. 2020;67:514–518. doi: 10.1016/j.jadohealth.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harkness KL, Monroe SM. Childhood adversity and the endogenous versus nonendogenous distinction in women with major depression. Am J Psychiatry. 2002;159:387–393. doi: 10.1176/appi.ajp.159.3.387. [DOI] [PubMed] [Google Scholar]
- 11.Stein MB, Walker JR, Anderson G, Hazen AL, et al. Childhood physical and sexual abuse in patients with anxiety disorders and in a community sample. Am J Psychiatry. 1996;153:275–277. doi: 10.1176/ajp.153.2.275. [DOI] [PubMed] [Google Scholar]
- 12.Ding H, Han J, Zhang M, Wang K, et al. Moderating and mediating effects of resilience between childhood trauma and depressive symptoms in Chinese children. J Affect Disord. 2017;211:130–135. doi: 10.1016/j.jad.2016.12.056. [DOI] [PubMed] [Google Scholar]
- 13.Wu SJ, Bai X, Fiske ST. Admired rich or resented rich? How two cultures vary in envy. J Cross Cult Psychol. 2018;49:1114–1143. doi: 10.1177/0022022118774943. [DOI] [Google Scholar]
- 14.Leung DYP, Mak YW, Leung SF, Chiang VCL, et al. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry n/a. 2020;12:e12381. doi: 10.1111/appy.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang W, Bian Q, Zhao Y, Li X, et al. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36:539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 16.Qing Z. Reliability and validity of Chinese version of the generalized anxiety disorder 7-item(GAD-7) scale in screening anxiety disorders in outpatients from traditional Chinese internal department. Chin Mental Health J. 2013;53:29–137. [Google Scholar]
- 17.Tiirikainen K, Haravuori H, Ranta K, Kaltiala-Heino R, et al. Psychometric properties of the 7-item generalized anxiety disorder scale (GAD-7) in a large representative sample of finnish adolescents. Psychiatry Res. 2019;272:30–35. doi: 10.1016/j.psychres.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Bernstein DP, Stein JA, Newcomb MD, Walker E, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 19.Xingfu Z, Yalin Z, Longfei L, Yunfei Z. Evaluation on reliability and validity of Chinese version of childhood trauma questionnaire. Chin J Clin Rehab. 2005;9:209–211. [Google Scholar]
- 20.KM, C. and D. JR, Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 21.Yu X-N, Lau JTF, Mak WWS, Zhang J, et al. Factor structure and psychometric properties of the connor-davidson resilience scale among Chinese adolescents. Compr Psychiatry. 2011;52:218–224. doi: 10.1016/j.comppsych.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Lai J, Ma S, Wang Y, Cai Z, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xing-chen H, Ying-li Z, Wei L, Hong-mei Z, et al. Reliability and validity of the patient health questionnaire-9 in Chinese adolescents. Sichuan Mental Health. 2014;27:357–360. [Google Scholar]
- 24.Yu W, Singh SS, Calhoun S, Zhang H, et al. Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden. J Affect Disord. 2018;234:89–96. doi: 10.1016/j.jad.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 25.Zhang YL, Liang W, Chen ZM, Zhang HM, et al. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 26.Guo L, Wang W, Gao X, Huang G, et al. Associations of childhood maltreatment with single and multiple suicide attempts among older Chinese adolescents. J Pediatr. 2018;196:244–250.e1. doi: 10.1016/j.jpeds.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 27.Tietjen GE, Brandes JL, Peterlin BL, Eloff A, et al. Childhood maltreatment and migraine (part I). Prevalence and adult revictimization: a multicenter headache clinic survey. Headache. 2010;50:20–31. doi: 10.1111/j.1526-4610.2009.01556.x. [DOI] [PubMed] [Google Scholar]
- 28.Okafor FC, Lee H. Double sampling for ratio and regression estimation with sub sampling the non-respondent. Surv Methodol. 2000;26:183–188. [Google Scholar]
- 29.Racine N, Cooke J, Eirich R, Korczak D, et al. Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Res. 2020;292:113307. doi: 10.1016/j.psychres.2020.113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rogers AA, Ha T, Ockey S. Adolescents' perceived socio-emotional impact of COVID-19 and implications for mental health: results from a US-based mixed-methods study. J Adolesc heaLth: Off Publ Soc Adolesc Med. 2020;S1054–139X(20):30592–9. doi: 10.1016/j.jadohealth.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmitz R (2011) The downside of exam-based education in China. Available from: www.marketplace.org/2011/06/07/downside-exam-based-education-china/amp. Accessed 17 Apr 2020
- 32.Kirkpatrick RM, Zang Y. The negative influences of exam-oriented education on chinese high school students: backwash from classroom to child. Language Testing in Asia. 2011;1:2. doi: 10.1186/2229-0443-1-3-36. [DOI] [Google Scholar]
- 33.Brooks SK, Webster RK, Smith LE, Woodland L, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jeong H, Yim H, Song Y, Ki M, et al. Mental health status of people isolated due to middle east respiratory syndrome. Epidemiol Health. 2016;38:e2016048. doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mihashi M, Otsubo Y, Yinjuan X, Nagatomi K, et al. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol. 2009;28:91–100. doi: 10.1037/a0013674. [DOI] [PubMed] [Google Scholar]
- 36.Lee S, Chan LY, Chau AM, Kwok KP, et al. The experience of SARS-related stigma at amoy gardens. Soc Sci Med. 2005;61:2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.China, N.H.C.o.t.P.s.R.o (2020) Update on COVID-19 outbreak in China. Available from: http://www.nhc.gov.cn/yjb/s7860/202004/35d096269e2848cdb4d3cb38e4c6bd1b.shtml. Accessed 15 Apr 2020
- 38.Hawryluck L, Gold W, Robinson S, Pogorski S, et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caleo G, Duncombe J, Jephcott F, Lokuge K, et al. The factors affecting household transmission dynamics and community compliance with Ebola control measures: a mixed-methods study in a rural village in Sierra Leone. BMC Public Health. 2018;18:248. doi: 10.1186/s12889-018-5158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.DiGiovanni C, Conley J, Chiu D, Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror. 2004;2:265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- 41.Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- 42.McCabe R, Antony M, Summerfeldt L, Liss A, et al. Preliminary examination of the relationship between anxiety disorders in adults and self-reported history of teasing or bullying experiences. Cogn Behav Ther. 2003;32:187–193. doi: 10.1080/16506070310005051. [DOI] [PubMed] [Google Scholar]
- 43.Gibb BE, Chelminski I, Zimmerman M. Childhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatients. Depress Anxiety. 2007;24:256–263. doi: 10.1002/da.20238. [DOI] [PubMed] [Google Scholar]
- 44.Infurna M, Reichl C, Parzer P, Schimmenti A, et al. Associations between depression and specific childhood experiences of abuse and neglect: a meta-analysis. J Affect Disord. 2016;190:47–55. doi: 10.1016/j.jad.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Nuttman-Shwartz O. Behavioral responses in youth exposed to natural disasters and political conflict. Curr Psychiatry Rep. 2019;21:42. doi: 10.1007/s11920-019-1030-3. [DOI] [PubMed] [Google Scholar]
- 46.Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. 2010;30:479–495. doi: 10.1016/j.cpr.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 47.Luthar SS, Cicchetti D. The construct of resilience: implications for interventions and social policies. Dev Psychopathol. 2000;12:857–885. doi: 10.1017/S0954579400004156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schulz A, Becker M, Van der Auwera S, Barnow S, et al. The impact of childhood trauma on depression: does resilience matter? Population-based results from the study of health in pomerania. J Psychosom Res. 2014;77:97–103. doi: 10.1016/j.jpsychores.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 49.Arslan G. Psychological maltreatment, emotional and behavioral problems in adolescents: the mediating role of resilience and self-esteem. Child Abuse Negl. 2016;52:200–209. doi: 10.1016/j.chiabu.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 50.Bernstein M, Pfefferbaum B. Posttraumatic growth as a response to natural disasters in children and adolescents. Curr Psychiatry Rep. 2018;20:37. doi: 10.1007/s11920-018-0900-4. [DOI] [PubMed] [Google Scholar]
- 51.Guessoum SB, Lachal J, Radjack R, Carretier E, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mallet J, Dubertret C, Le Strat Y. Addictions in the COVID-19 era: current evidence, future perspectives a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2020;106:110070. doi: 10.1016/j.pnpbp.2020.110070. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.