Abstract
The COVID-19 pandemic has massively changed people’s working lives all over the world. While various studies investigated the effects from pandemic-induced unemployment and telecommuting, there is a lack of research regarding the impact of workplace COVID-19 countermeasures on well-being and mental health for employees who are still working on site. Thus, the aim of the present study was to investigate the prevalence of workplace COVID-19 countermeasures in organizations in Luxembourg. A person-centered approach was applied in order to explore how employees’ psychological well-being and health (i.e., general psychological well-being, vigor, work satisfaction, work-related burnout, somatic complaints, fear of COVID-19 infection) are impacted by organizational countermeasures and whether there are certain employee groups that are less protected by these. Results of a latent class analysis revealed four different classes (Low level of countermeasures, Medium level of countermeasures, High level of countermeasures, High level of countermeasures low distance). Employees working in a healthcare setting were more likely than employees working in a non-healthcare setting to be members of the High level of countermeasures low distance class. Class membership was meaningfully associated with all well-being outcomes. Members of the High level of countermeasures class showed the highest level of well-being, whereas Members of the Low level of countermeasures class and the High level of countermeasures low distance class showed the lowest level of well-being. Policy makers and organizations are recommended to increase the level of COVID-19 countermeasures as an adjunctive strategy to prevent and mitigate adverse mental health and well-being outcomes during the COVID-19 pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12144-022-03377-4.
Keywords: Occupational health, Well-being, SARS-CoV-2, Organizational COVID-19 countermeasures, Infection control
Introduction
The COVID-19 pandemic has massively changed people’s working lives all over the world. While some employees have lost their jobs due to the triggered economic crisis, others have started to telecommute in order to apply social distancing, and others still have to work on site for various reasons. Each of these groups may face different challenges and effects on personal health and well-being (e.g., Görlich & Stadelmann, 2020; Rudolph et al., 2021; Sinclair et al., 2020). So far, some studies have investigated the effects of the pandemic induced unemployment on health and well-being (e.g., Berkowitz & Basu, 2021). Furthermore, research has examined the effects of telecommuting due to the pandemic on work characteristics and subsequent well-being and perceived productivity (e.g., Carillo et al., 2020; Chang et al., 2021; Sischka & Steffgen, 2021a; Wang et al., 2021). Moreover, the psychological effects of the COVID-19 pandemic on employees’ mental health and well-being in general have been studied (e.g., Lovreglio et al., 2021; Meyer et al., 2021; Rathod et al., 2020). However, one might hypothesize that particularly the psychological health and well-being of employees who still have to work on site might be affected more intensively by the pandemic situation compared to employees who are able to telecommute as on site workers are more at risk of getting infected.
The COVID-19 pandemic and psychological well-being/mental health in employees
The COVID-19 pandemic represents an extraorganizational stressor (Biggs et al., 2014) that differs from typical workplace stressors in terms of its scope, magnitude, and impact on employees (Lovreglio et al., 2021). Especially during the onset of the pandemic, because of the growing number of COVID-19 (death) cases, lack of knowledge of how to protect oneself, lack of specific medications, and extensive media coverage, individuals began worrying about COVID-19 (Ahorsu et al., 2020; Arnetz et al., 2020). This fear can be manifold and includes the fear of infection for oneself and one’s loved ones as well as the fear of transmitting the disease to others (including one’s co-workers). Fear can be viewed as an adaptive reaction to a perceived threat that promotes survival (Gullone, 2000). Indeed, fear of COVID-19 has been linked with increased safety behavior (e.g., social distancing) during the pandemic (Harper et al., 2021). However, fear can become dysfunctional and detrimental to well-being and mental health when it becomes excessive (Taylor, 2019). Indeed, fear of COVID-19 had been meta-analytically linked with ill-health, such as anxiety, stress, depression, and insomnia (Şimşir et al., 2022) that can translate into somatic complaints (Lundberg et al., 1999). With regard to workplace, especially healthcare workers and other frontline workers (i.e., workers with jobs that are seen as essential to maintain critical infrastructure which cannot feasibly be realized via telecommuting) have been discussed as occupation groups that are at risk of an infection with COVID-19 (Baker et al., 2020; Debus et al., 2021; Giorgi et al., 2020; Laufs & Waseem, 2020; Nabe-Nielsen et al., 2021; Nguyen et al., 2020; Ravikumar, 2022; Rudolph et al., 2021; Sasaki et al., 2020a; Sinclair et al., 2020) and, thus, are especially prone to fear of COVID-19 and impaired psychological health (e.g., Görlich & Stadelmann, 2020; Labrague & de Los Santos, 2021; Rathod et al., 2020; Rossi et al., 2020).
The role of COVID-19 countermeasures in organizations
Individuals can engage in safety behavior to reduce the risk of getting infected (Harper et al., 2021). However, within an organization, not only the individual safety behavior but also the organizational countermeasures matter (e.g., Arnetz et al., 2020; Nabe-Nielsen et al., 2021). For instance, organizations can ensure that employees get all relevant information about COVID-19 and protective measures, that everyone at work wears a face mask, or that employees always have a minimum distance from other people (e.g., by providing enough workspace). These countermeasures, taken together, might form the employee’s perceived COVID-19-specific safety climate. Perceived safety climate is defined as “individual perceptions of policies, procedures, and practices relating to safety in the workplace” (Neal & Griffin, 2006, p. 946-947). A low perceived safety climate can lead to occupational stress with the effect of reduced physical and psychological well-being (Clarke, 2010). Thus, enhancing the COVID-19-specific safety climate might be a successful means to reduce the fear of COVID-19 and to maintain employees’ mental health and well-being. Although implemented COVID-19 countermeasures might reduce the negative effect of working on site on employee’s mental health and well-being as they might be perceived as reducing the risk of an infection, employers and occupational groups certainly differ in terms of protection through these countermeasures (e.g., Sinclair et al., 2021).
Studies that investigated COVID-19 countermeasures (and its impact on psychological well-being) so far mainly focused on specific working groups, in particular healthcare workers (e.g., Arnetz et al., 2020; Firew et al., 2020; Havaei et al., 2021; Kim et al., 2021; Nabe-Nielsen et al., 2021). Only a few studies in the Asian region have investigated the prevalence of workplace COVID-19 countermeasures in the general working population (Ishimaru et al., 2021; Nomura et al., 2020; Sasaki et al., 2021; Sasaki et al., 2020a, b, c; Wong et al., 2020; Hu et al., 2021). Smaller organizations seem to have implemented less countermeasures (Ishimaru et al., 2021; Sasaki et al., 2020b). Moreover, the number of countermeasures increased slightly over time (between March and May; Sasaki et al., 2021). Some studies investigated the prevalence of individual as well as social and political countermeasures over time and found some age-effects (Nomura et al., 2020). Moreover, as one would expect, workplace countermeasures differ across occupation groups (Wong et al., 2020). For instance, ‘blue-collar’ employees and employees working in the industrial sector reported more often that no COVID-19 countermeasure was implemented in their organization. These groups showed also higher perceptions of being at risk of an infection (Wong et al., 2020). Moreover, a study showed that deep compliance with COVID-19 countermeasures includes a four-stage psychological process that is underpinned by management safety practices and organizational crisis strategies (Hu et al., 2021).
With regard to mental health and well-being, Sasaki et al. (2020c) found that the number of implemented COVID-19 countermeasures was negatively associated with psychological distress and self-reported work performance. Surprisingly, the number of countermeasures was positively associated with fear and worries about COVID-19. Sasaki et al (2020c) explained this finding with an increased awareness about COVID-19 that comes with the implementation of these measures. Furthermore, Uehara et al. (2021) showed that perceived workplace infection control efforts were negatively related with psychological distress.
Aim of the present study
This short literature overview points to important knowledge gaps: All studies investigating the prevalence of countermeasures and their effects on mental health and well-being in a general working population were conducted in the Asian region. Thus, we know little about implemented countermeasures and their effects on mental health and well-being in other regions. Moreover, most of the studies either investigated specific occupational groups or made use of convenience sampling and, thus, lack generalizability. Finally, the studies used a variable-centered approach (e.g., number of COVID-19 countermeasures) to investigate the association between countermeasures and mental health and well-being. However, one might argue that the different countermeasures are not equivalent or interchangeable. Moreover, depending on the occupational context, different countermeasures might have been implemented. For instance, protective clothing might be especially relevant for healthcare workers but less so for service and sales workers. Thus, a person-centered approach (i.e., latent class analysis) might be more suitable to unravel a more fine-grained perspective on the topic. A person-centered approach investigates how variables combine within individuals, whereas a variable-centered approach investigates how variables operate separately between individuals (Wang & Hanges, 2011). Person-centered approaches consider the possibility that the sample might include multiple subpopulations that are characterized by different sets of parameters (Morin et al., 2018). Thus, these approaches capture sample heterogeneity that might stay undetected in variable-centered approaches (Wang & Hanges, 2011). Specifically, latent class analysis is able to identify distinct classes that vary in the absolute level of the indicators (quantitative differences) and in their shape (qualitative differences).
Failure to comply with COVID-19 countermeasures might endanger the health and well-being of employees, the viability of the business of the organization, and the general public health. Thus, utilizing a nationally representative sample, the aim of the present study was to investigate a) the prevalence of workplace COVID-19 countermeasures in organizations in Luxembourg, b) whether there are certain employee groups that are less protected through organizational countermeasures and c) the impact of these countermeasures on psychological well-being and health. To this end, eight different organizational COVID-19 countermeasures were assessed that were recommended by the World Health Organization at the onset of the pandemic (World Health Organization, 2020). We used a person-centered approach (i.e., latent class analysis) to identify groups that differ regarding COVID-19 countermeasures implemented by their organizations and groups that are less protected through these countermeasures. We investigated the following research questions.
Research question 1: Do distinct classes of COVID-19 countermeasures exist that vary quantitatively (in level) and qualitatively (in shape)?
Research question 2: Do sociodemographic (i.e., gender, age, education) and professional characteristics (i.e., occupation, organization size, working in the healthcare sector) differentiate COVID-19 countermeasure classes?
Research question 3: Do COVID-19 countermeasure classes relate differently to employee well-being (i.e., general psychological well-being, work-related burnout, vigor, work satisfaction, somatic complaints, fear of COVID-19 infection)?
Method
Data collection and survey design
The present study was conducted as part of a research project on the quality of work and its effects on health and well-being in Luxembourg (Steffgen et al., 2020). This project was implemented by the University of Luxembourg in collaboration with the Luxembourg Chamber of Labor as an assessment over yearly waves since 2014. We used data from the survey 2020 (for details regarding the study see Sischka & Steffgen, 2021b). The Luxembourgish social security register was used to draw a stratified random sample of address data from Luxembourg’s working population (i.e., Luxembourgish residents and commuters from France, Belgium, and Germany).1 After data collection, a weighting variable was calculated that calibrated the sample distribution of the combined characteristics of age, gender, and place of residence to known distributions in the population. The sample of address data included addresses from Luxembourg residents and commuters from Belgium, France, and Germany who received wages for working at least 10 hrs/week. The contacted employees then had the opportunity to participate in the survey via Computer-Assisted Telephone Interviews (CATI) or Computer-Assisted Web Interviews (CAWI). The survey was conducted according to the Declaration of Helsinki (i.e., voluntary participation, participants were free to withdraw their consent at any time throughout the interviews without negative consequences for them). Informed consent was obtained from all respondents prior to the start of the survey, either by clicking a box (CAWI) or verbally on the phone (CATI). Data were collected between 09.06.2020 and 05.10.2020. The survey questionnaire exists in five language versions: Luxembourgish, French, German, English, and Portuguese. For the translation of the questionnaire two translators had been used. After the initial translation the questionnaire was tested for comprehensibility and semantic meaning by five native speakers (on for each language version). They discussed and refined the translation and generated the final version of the questionnaire. All data reported in the present study are cross-sectional.
Participants
The initial sample consisted of 2,364 employees working in Luxembourg. Due to incomplete data (i.e., missing values on all COVID-19 protective measures or on permanent telecommuting status; n = 12), and because one respondent was underage (i.e., 17 years old), 0.5% of respondents had to be excluded from the analyses. Therefore, the effective sample consisted of 2,351 employees (41.4% females; n = 973). The majority of employees resided in Luxembourg (54.9%, n = 1289), followed by France (23.2%, n = 545), Germany (11.1%, n = 260), and Belgium (10.9%, n = 256). The respondents’ ages ranged from 18 to 67 years (M = 40.3, SD = 10.6). Almost half of the respondents had an academic degree. (49.0%, n = 1153). About 9.5% (n = 223) of the respondents worked in the healthcare sector. According to the International Standard Classification of Occupations (ISCO-08; International Labour Organization, 2012), most respondents worked in a profession (38.6%, n = 902) followed by technicians and associate professionals (22.1%, n = 517), craft and related trades workers (8.3%, n = 193), clerical support workers (8.1%, n = 190), service and sales workers (8.1%, n = 189), managers (6.9%, n = 161), plant and machine operators, and assemblers (3.7%, n = 85), elementary occupations (3.5%, n = 81), skilled agricultural, forestry and fishery workers (0.7%, n = 16), and armed forces (0.2%, n = 5). About 19.6% (n = 458) of the respondents worked in organizations with 1-14 employees, 17.7% (n = 415) in organizations with 15-49 employees, 28.7% (n = 672) in organizations with 50-249 employees, and 34.0% (n = 796) in organizations with 250 and more employees. About 46.9% (n = 946) of the respondents reported that they began to telecommute at least partially because of the COVID-19 pandemic. However, the percentage of permanent telecommuters (see definition below) was much lower (4.2%, n = 99).2
Measures
Latent class indicators
COVID-19 countermeasures
We asked for potential organizational COVID-19 countermeasures that were recommend by the World Health Organization (2020) at the beginning of the spreading in Europe. Respondents got the following instruction: “There are various measures available to employers in order to protect their employees from the coronavirus. To what extent do the following statements about COVID-19 protective measures apply to your organisation?” This instruction was followed by the following items: (1) “My employer provides sufficient information about COVID-19 and protective measures.”, (2) “The necessary minimum 2-metre distance from other people can always be guaranteed at work.”, (3) “The workspace is regularly disinfected (e.g., desk, telephone, keyboard).”, (4) “It is always possible to disinfect your hands.”, (5) “Areas where several people work together are well ventilated.”, (6) “Everyone wears a face mask at work.”, (7) “My employer provides protective clothing.”, (8) “My employer makes sure that employees are signed off sick even if they present only mild cold-like symptoms (e.g., light coughing, slight fever).” Responses were made on a 5-point scale (1 = to a very low extent; 5 = to a very large extent).
Permanent telecommuting
Respondents were also asked how often they are working from home and how often they are working at their employer’s premises (e.g., office, factory, shop, school etc.) with five response categories (1 = every day; 2 = several times a week; 3 = several times a month; 4 = less often; 5 = never). Employees indicating that they worked from home every day or several times a week while at the same time indicating that they worked several times a month, less often or never at their employer’s location were coded as permanent telecommuters (4.2%; n = 99).
The organizational COVID-19 countermeasures were used as indicators for the latent class analysis and only non-permanent telecommuters were included. However, permanent telecommuting was added as an additional (manifest) class in subsequent analyses concerning antecedents and outcomes of class membership.
Predictors of latent class membership
We wanted to know whether there are gender, age, education, and occupation differences regarding class membership. Moreover, based on previous research (Ishimaru et al., 2021; Sasaki et al., 2020a, b), we also considered organization size and working in the healthcare sector as potential predictors of class membership. Thus, we included gender (0 = male, 1 = female), age (as continuous variable), organization size (1 = 1-14 employees, 2 = 15-49 employees, 3 = 50-249 employees, 4 = 250 and more employees), education (1 = ISCED 1-3 (primary education, lower and upper secondary education), 2 = ISCDED 4-5 (post-secondary non-tertiary education, short-cycle tertiary education), 3 = ISCED 6-8 (bachelor, master, doctoral or equivalent)), working in the healthcare sector (0 = no, 1 = yes), and occupation (1 = Managers, 2 = Professionals, 3 = Technicians, 4 = Clerical support workers, 5 = Service and sales workers, 6 = Craft workers, 7 = Others)3 as predictors of latent class membership.
Outcomes of latent class membership
General psychological well-being
The five-item WHO-5 Well-Being Index is a well-validated and psychometrically sound brief general index of subjective psychological well-being (Topp et al., 2015; Sischka et al., 2020) with a response format ranging from 1 (= at no time) to 6 (= all of the time). A sample item is “Over the past two weeks I have felt cheerful and in good spirits.”
Work-related burnout
We used a six-item measure of work-related burnout (Sischka & Steffgen, 2021b). A sample item is “How often is your work emotionally exhausting?”. The response scale is a 5-point Likert scale ranging from 1 (= never) to 5 (= almost always).
Vigor
The three-item subscale of the Utrecht Work Engagement Scale (Schaufeli et al., 2006) is characterized by high levels of energy and the willingness to invest effort in one’s work, even when it comes to difficulties and problems. A sample item is “At my work, I feel bursting with energy.” The response format ranges from 1 (= never) to 5 (= almost always).
Work satisfaction
Work satisfaction was assessed with a three-item measure that assesses global judgment of work satisfaction (Sischka & Steffgen, 2021b). It evaluates an employee’s satisfaction with important work characteristics, such as work climate and work conditions. Higher scores imply that the employee is satisfied with her/his work. A sample item is “How satisfied are you at present with your work?”. Responses were made on a 5-point scale (1 = to a very low extent; 5 = to a very large extent).
Somatic complaints
This seven-item index is concerned with physiological health problems (i.e., general health problems, headaches, heart problems, back problems, joint problems, stomach pain, sleeping problems). Higher scores signify that an employee faces somatic complaints. A sample item is “How often do you suffer from headaches?”. The response scale is a 5-point Likert scale ranging from 1 (= never) to 5 (= almost always).
Fear of COVID-19 infection
The fear of an infection was assessed with a single item: “How worried are you that you might catch COVID-19 in your current working situation?” Responses were made on a 5-point scale (1 = to a very low extent; 5 = to a very large extent).4
Statistical analysis
We started the latent class analysis (LCA) with a one-class model that estimates the observed indicator endorsement probability for the items and serves as a comparative baseline model for models with more classes (Nylund-Gibson & Choi, 2018; Nylund et al., 2007). In a next step, the number of classes was increased, and it was evaluated whether these more complex models resulted in conceptually and statistically superior solutions (Nylund-Gibson & Choi, 2018). To determine the number of classes we used the following statistical criteria: Akaike’s information criterion (AIC; Akaike, 1987), consistent AIC (CAIC; Bozdogan, 1987), Bayesian information criterion (BIC; Schwarz, 1978), sample-size adjusted BIC (SABIC; Sclove, 1987), approximate weight of evidence (AWE; Banfield & Raftery, 1993), and the Lo-Mendell-Rubin likelihood ratio test (LMR-LRT; Lo et al., 2001). The ideal class solution should contain the smallest AIC, CAIC, BIC, SABIC, AWE, and a significant LMR-LRT statistic.5 However, it is not uncommon that the information criteria continue to decrease for each additional class added until no further class can be added due to identification issues (Masyn, 2013; Nylund-Gibson & Choi, 2018), thus, there exists no global minimum. In such cases, one can explore the diminishing gains in model fit with an “elbow plot” (Masyn, 2013; Nylund-Gibson & Choi, 2018). Moreover, we used Bayes factors (BF) as a pairwise comparison of fit between two neighboring class models, where 1 < BF < 3 indicates weak evidence for the model with less classes, 3 < BF < 20 positive evidence, 20 < BF < 150 strong evidence, and BF > 150 very strong support (Raftery, 1995). Finally, we calculated the approximate correct model probability (cmP) that allows relative comparison of all models considered, while assuming that the true model is among them (Masyn, 2013; Nylund-Gibson & Choi, 2018).
Because fit indices often point to different solutions, it is recommended to jointly consider statistical fit indices, substantive interpretability and utility, as well as classification diagnostics to determine the number of classes (Masyn, 2013; Nylund-Gibson & Choi, 2018). Moreover, classes should not be redundant and relative class size should not be too small (e.g., less than 5% of the sample; Nylund-Gibson & Choi, 2018) as this indicates class overextraction (Masyn, 2013). After the selection of a final model, we created a conditional distribution and profile plot6. We also calculated entropy (Celeux & Soromenho, 1996) as an index of the overall precision of classification, where values above .80 indicate good classification (Clark & Muthén, 2009). Moreover, average posterior probabilities (AvePP) were calculated that enable evaluation of the specific classification uncertainty for each latent class (Masyn, 2013). As a rule of thumb, all AvePP values should be at least .70 (Nagin, 2005). The COVID-19 countermeasure items were treated as ordinal indicators. The robust maximum likelihood estimator (MLR) in conjunction with Full Information Maximum Likelihood (FIML; Enders, 2010) to handle missing data was used. Moreover, LCAs were estimated with 5,000 random start values, allowed 1,000 iterations each, and retaining the 200 best solutions for final optimization to avoid converging on a local maximum (Hipp & Bauer, 2006).
To explore the relationships between the latent categorical variable and the other variables (i.e., demographic variables as predictors, well-being variables as outcomes), we followed the recommended three-step procedure (Asparouhov & Muthén, 2014; Nylund-Gibson et al., 2014; Vermunt, 2010). First, the best-fitting latent class model is identified, using only the latent class indicators. Second, the most likely class membership is obtained based upon the posterior distribution from the latent class model identified in the first step. Third, auxiliary variables (i.e., predictors, outcomes) are linked to the classes from the best-fitting latent class model, taking the potential misclassification in the second step into account. We conducted separate analyses to test class antecedents and outcomes (Lanza et al., 2013). A multinomial logistic regression was applied to test whether predictor variables change the probability that a person belongs to one class or another. For ease of interpretation, we also calculated odds ratios (OR) that reflect the change in likelihood of being a member of a target class versus a comparison class when the predictor variable increases by one unit. Furthermore, we examined latent class effects by estimating the class-specific mean and variance for each outcome and then conducting pairwise class comparisons. For the outcomes, we applied confirmatory factor analysis (CFA) with robust weight least square estimator (WLSMV) to account for the ordered-categorical nature of the indicators (Finney & DiStefano, 2013). The calculated factor scores (with M = 0 and SD = 1) from these CFAs were used as outcome variables for the structural LCA model (fit indices are reported in the online supplement, Table A1). Then it was determined whether latent classes display statistically significant mean-level differences in the outcome variables. The Benjamini-Hochberg (1995) adjustment was employed to control for multiple testing. We calculated categorical omega (ωC) with 95% confidence intervals obtained via the bias-corrected and accelerated bootstrapping approach (10,000 bootstrap samples) to get an estimate (along with its precision) of the internal consistency of our implemented scales (Kelley & Pornprasertmanit, 2016). Mplus Version 8.8 (Muthén & Muthén, 1998-2017) and R version 4.1.3 (R Core Team, 2022) were used for the data analyses.
Results
Latent class solutions
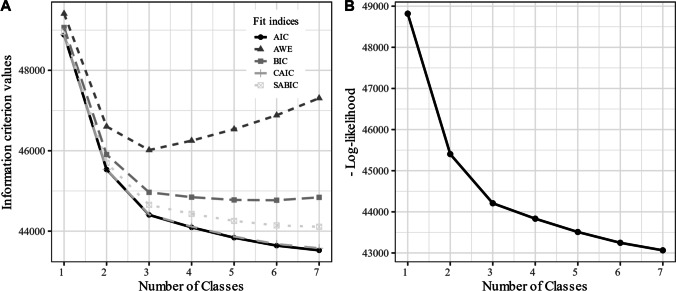
Table 1 shows the fit indices associated with the different LCA solutions including 1 to 7 classes whereas Figure 1 displays the elbow plots of these indices. The indices did not converge on a single solution. The AWS and the LMR-LRT indicated a 3-class solution. On the other hand, the BIC as well as the BF and cmP clearly favored a 6-class solution. The AIC, CAIC and SABIC failed to converge on any specific solution. However, examination of Figure 1 suggests diminishing gains in model fit and a flattening out in the decrease of information criteria values and the log-likelihood located around the 3-class solution. Thus, we examined the 3- to 7-class solutions more comprehensively. Comparing the 3-class with the 4-class solution, the 4-class solution was an expanded version of the 3-class model, as the previous three classes appeared almost unchanged in the 4-class solution and the added class was substantially different compared to the other classes. Comparing the 4-class solution with the 5- to 7-class solution, the added classes were not substantially different and showed mainly differences in the absolute level of the indicators (quantitative differences) but not in their shape (qualitative differences). Thus, we decided to retain the 4-class solution with an entropy of .809. Table 2 shows that the 4-class solutions had a high level of classification accuracy (AvePP) of participants into their most likely class, ranging from .850 to .918.
Table 1.
Latent class analysis models fit statistics
| k | LL | #FP | Scaling | AIC | CAIC | BIC | SABIC | AWE | LMR-LRT (p) | BF | cmP | Entropy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | -24409.318 | 32 | 2.000 | 48882.635 | 48883.580 | 49065.888 | 48964.218 | 49409.142 | NA | 0.000 | 0.000 | NA |
| 2 | -22701.662 | 65 | 1.962 | 45533.324 | 45537.220 | 45905.557 | 45699.041 | 46602.789 | 0.000 | 0.000 | 0.000 | 0.810 |
| 3 | -22104.333 | 98 | 1.967 | 44404.667 | 44413.613 | 44965.879 | 44654.516 | 46017.090 | 0.000 | 0.000 | 0.000 | 0.795 |
| 4 | -21916.712 | 131 | 1.949 | 44095.424 | 44111.615 | 44845.615 | 44429.406 | 46250.807 | 0.695 | 0.000 | 0.000 | 0.809 |
| 5 | -21754.983 | 164 | 1.960 | 43837.965 | 43863.700 | 44777.137 | 44256.080 | 46536.308 | 0.766 | 0.019 | 0.019 | 0.758 |
| 6 | -21623.551 | 197 | 2.005 | 43641.103 | 43678.790 | 44769.254 | 44143.351 | 46882.404 | 0.760 | >150.000 | 0.981 | 0.758 |
| 7 | -21531.882 | 230 | 1.959 | 43523.763 | 43575.928 | 44840.894 | 44110.144 | 47308.025 | 0.809 | NA | 0.000 | 0.765 |
k: number of classes, LL log-likelihood, #FP Number of free parameters, Scaling Scaling factor associated with MLR loglikelihood estimates, AIC Akaike information criterion, CAIC Consistent AIC, BIC Bayesian information criterion, SABIC Sample-size adjusted BIC, AWE Approximate weight of evidence, BF Bayes factor, cmP Approximate correct model probability, LMR-LRT Adjusted Lo-Mendel-Rubin likelihood ratio test. Bolded values indicate best fit for each respective statistic
Fig. 1.
Plot of information criterion and Log-likelihood values. Note. The AIC and CAIC lines in plot A are overlapping
Table 2.
Posterior classification probabilities for most likely latent class membership (Row) by latent class (Column)
| Class | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| (1) Low level of countermeasures | .896 | .084 | .006 | .014 |
| (2) Medium level of countermeasures | .038 | .886 | .054 | .022 |
| (3) High level of countermeasures | .002 | .054 | .918 | .026 |
| (4) High level of countermeasures low distance | .022 | .057 | .072 | .850 |
Values indicate probabilities of most likely class membership (column) by latent class modal assignment (row). Bolded values indicate average posterior probabilities (AvePP)
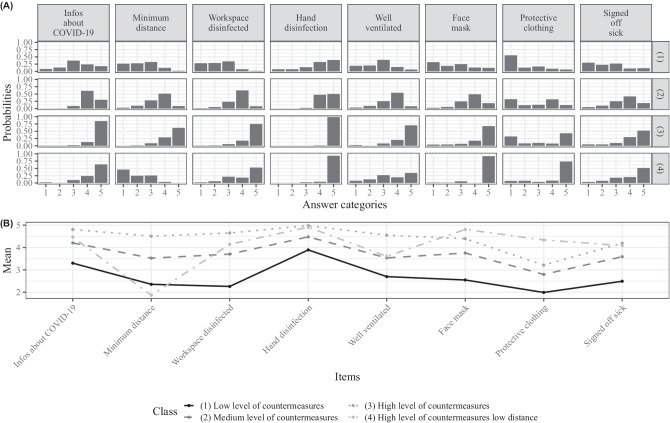
Figure 2 displays the conditional distributions of the items and the profile plot of each class. Members of the first class experienced the lowest levels of countermeasures (M ranged between 1.99 and 3.89), and thus, were labeled as Low level of countermeasures class. The second class describes employees who showed medium levels of countermeasures compared to class 2 and 3 (M ranged between 2.80 and 4.48), and thus were labeled Medium level of countermeasures class, accordingly. The third class describes employees who showed high levels on all COVID-19 countermeasures (M ranged between 3.21 and 4.98) labeled as High level of countermeasures class. Finally, the fourth class encompassed employees who experienced a high level of COVID-19 countermeasures except for minimum distance (M ranged between 1.87 and 4.91) labeled as High level of countermeasures low distance class.7
Fig. 2.
Conditional item distribution (A) and profile plot (B)
Based on most likely latent class membership, 20.1% (n = 472) of the employees were members of the Low level of countermeasures (1) class, 32.7% (n = 769) members of the Medium level of countermeasures (2) class, 30.4% (n = 716) members of the High level of countermeasures (3) class, 12.6% (n = 296) members of the High level of countermeasures low distance (4) class, and 4.2% (n = 99) members of the (manifest) permanent telecommuting (5) class.
Predictors of class membership
In addition to the four identified latent classes, the group of permanent telecommuters was included in the analysis as manifest class. Table 3 shows the distribution of gender, age, organization size, education, working in the healthcare setting and occupation across classes. Table 4 shows the associations between the various classes and the predictors considered in the present study. Gender was unrelated to the likelihood of membership in any of the classes. Age was associated with a decreased likelihood of membership in the High level of countermeasures low distance (4) and Low level of countermeasures (1) classes relative to the Medium level of countermeasures (2) class. Furthermore, age was associated with an increased likelihood of membership in the High level of countermeasures (3) class relative to the High level of countermeasures low distance (4) class. Moreover, age was associated with a decreased likelihood of membership in the Low level of countermeasures (1) class relative to the High level of countermeasures (3) class. Employees working in organization with 15-49 employees were less likely than employees working in organization with 1-14 employees to be members of the High level of countermeasures (3) class relative to the Medium level of countermeasures (2) class. Employees working in organization with 15-49 employees were more likely than employees working in organization with 1-14 employees to be members of the Low level of countermeasures (1) class relative to the High level of countermeasures (3) class. Employees in the highest educational group were less likely than employees in the lowest educational group to be members of High level of countermeasures low distance (4) class relative to the Medium level of countermeasures (2) class. Furthermore, they were more likely to be members of High level of countermeasures (3) and Low level of countermeasure (1) classes, relative to the High level of countermeasures low distance (4) class. Moreover, employees in the highest educational group were more likely than employees in the lowest educational group to be members of the permanent telecommuting (5) class, class relative to the Low level of countermeasures (1), High level of countermeasures (3), and High level of countermeasures low distance (4) classes. In contrast, employees working in a healthcare setting were less likely than employees working in a non-healthcare setting to be members of the Low level of countermeasures (1), Medium level of countermeasures (2), High level of countermeasures (3), or permanent telecommuting (5) classes, relative to the High level of countermeasures low distance (4) class. Furthermore, employees working in a healthcare setting were less likely than employees working in a non-healthcare setting to be members of the permanent telecommuting (5) class, relative to all other classes. Service and sales workers were more likely than employees working as professionals to be members of the High level of countermeasures low distance (4) and less likely to be members of the permanent telecommuting (5) class relative to all other classes. Clerical support workers were less likely than employees working as professionals to be members of the High level of countermeasures (3) and permanent telecommuting (5) classes relative to the Medium level of countermeasures (2) class. Managers were less likely than employees working as professionals to be members of the Low level of countermeasures (1) class relative to the Medium level of countermeasures (2) class. Especially service and sales workers, craft workers and employees in other occupations were less likely to be members of the permanent telecommuting (5) class, relative to all other classes.
Table 3.
Class descriptives
| Class | n | Gender (% female) | Age M (SD) |
Orga. Size (%) 1-14 employees/ 15-49 employees/ 50-249 employees/ 250+ employees |
Education (%) ISCED 1/ ISCED 2/ ISCED 3 |
Healthcare setting (%) | Occupation (%) Manager/ Technicians/ Clerical support workers/ Service and sales / workers Craft workers / Others |
|---|---|---|---|---|---|---|---|
| Low level (Class 1) | 472 | 41.7 | 38.1 (10.6) | 20.6/24.1/28.1/27.3 | 40.9/14.8/44.3 | 3.7 | 3.1/39.4/18.5/ 8.6/ 7.1/14.7/ 8.6 |
| Medium level (Class 2) | 769 | 40.1 | 41.2 (10.3) | 15.9/18.3/30.2/35.7 | 31.3/14.4/54.2 | 6.8 | 8.9/39.4/21.9/11.8/ 5.3/ 6.0/ 6.6 |
| High level (Class 3) | 716 | 39.8 | 41.5 (10.5) | 21.8/13.2/27.5/37.4 | 36.5/10.6/53.0 | 8.4 | 8.1/42.2/23.0/ 6.6/ 6.3/ 6.3/ 7.5 |
| High level low distance (Class 4) | 296 | 52.1 | 38.2 (11.2) | 23.6/18.6/30.7/27.1 | 61.8/17.4/20.8 | 31.6 | 3.0/16.7/28.1/ 2.7/23.7/11.2/14.6 |
| Permanent telecommuting (Class 5) | 99 | 28.4 | 40.4 (9.8) | 15.1/12.9/23.7/48.3 | 8.3/ 4.1/87.5 | 0.4 | 12.0/67.9/15.9/ 4.2/0/0/0 |
These class descriptives are based on the most likely latent class membership
Table 4.
Results from the R3STEP procedure for the effects of the predictors on latent class membership
| Class 1 vs. 2 | Class 1 vs. 3 | Class 1 vs. 4 | Class 1 vs. 5 | Class 2 vs. 3 | ||||||
| Coef. (SE) | OR | Coef. (SE) | OR | Coef. (SE) | OR | Coef. (SE) | OR | Coef. (SE) | OR | |
| Intercept | -1.304 (0.575)* | -0.492 (0.506) | -1.526 (0.995) | -2.724 (0.898)** | 0.812 (0.482) | |||||
| Gender | -0.289 (0.228) | 0.749 | -0.305 (0.217) | 0.737 | 0.173 (0.357) | 1.188 | -0.724 (0.382) | 0.485 | -0.016 (0.196) | 0.984 |
| Age | 0.027 (0.009)** | 1.028 | 0.029 (0.009)*** | 1.03 | -0.002 (0.013) | 0.998 | 0.019 (0.017) | 1.02 | 0.002 (0.008) | 1.002 |
| Orga. size (ref: 1-14 e.) | ||||||||||
| 15-49 | 0.143 (0.337) | 1.154 | -0.686 (0.308)* | 0.503 | -0.243 (0.481) | 0.784 | -0.477 (0.566) | 0.621 | -0.829 (0.308)** | 0.436 |
| 50-249 | 0.377 (0.315) | 1.458 | -0.145 (0.281) | 0.865 | 0.262 (0.447) | 1.299 | -0.211 (0.506) | 0.81 | -0.522 (0.274) | 0.593 |
| 250+ | 0.515 (0.319) | 1.673 | 0.180 (0.284) | 1.197 | 0.397 (0.469) | 1.487 | 0.399 (0.482) | 1.49 | -0.335 (0.262) | 0.715 |
| Education (ref: ISCED 1-3) | ||||||||||
| ISCED 4-5 | 0.259 (0.318) | 1.296 | -0.410 (0.310) | 0.664 | -0.214 (0.406) | 0.807 | -0.196 (0.731) | 0.822 | -0.670 (0.296)* | 0.512 |
| ISCED 6-8 | 0.512 (0.312) | 1.669 | 0.058 (0.289) | 1.06 | -1.235 (0.460)** | 0.291 | 1.328 (0.460)** | 3.775 | -0.454 (0.247) | 0.635 |
| Healthcare setting | 0.591 (0.553) | 1.805 | 0.761 (0.522) | 2.141 | 3.222 (0.518)*** | 25.074 | -2.314 (1.126)* | 0.099 | 0.171 (0.419) | 1.186 |
| Occupation (ref: Professional) | ||||||||||
| Manager | 1.299 (0.517)* | 3.667 | 0.891 (0.490) | 2.438 | 1.140 (1.039) | 3.127 | 1.116 (0.667) | 3.053 | -0.408 (0.366) | 0.665 |
| Technicians | 0.342 (0.306) | 1.407 | 0.065 (0.284) | 1.068 | 0.632 (0.560) | 1.881 | -0.052 (0.508) | 0.949 | -0.276 (0.262) | 0.759 |
| Clerical support workers | 0.660 (0.385) | 1.935 | -0.374 (0.379) | 0.688 | -1.379 (1.771) | 0.252 | -0.460 (0.603) | 0.631 | -1.034 (0.318)*** | 0.356 |
| Service and sales workers | 0.104 (0.546) | 1.11 | -0.133 (0.464) | 0.875 | 2.154 (0.730)** | 8.621 | -24.906 (0.730)*** | 0.000 | -0.237 (0.465) | 0.789 |
| Craft workers | -0.681 (0.450) | 0.506 | -0.945 (0.408)* | 0.389 | 0.750 (0.793) | 2.117 | -25.761 (0.793)*** | 0.000 | -0.264 (0.427) | 0.768 |
| Others | 0.021 (0.502) | 1.021 | -0.224 (0.459) | 0.799 | 1.565 (0.763)* | 4.781 | -25.111 (0.763)*** | 0.000 | -0.245 (0.420) | 0.783 |
| Class 2 vs. 4 | Class 2 vs. 5 | Class 3 vs. 4 | Class 3 vs. 5 | Class 4 vs. 5 | ||||||
| Coef. (SE) | OR | Coef. (SE) | OR | Coef. (SE) | OR | Coef. (SE) | OR | Coef. (SE) | OR | |
| Intercept | -0.222 (1.011) | -1.420 (0.868) | -1.034 (0.981) | -2.232 (0.859)** | -1.198 (1.234) | |||||
| Gender | 0.461 (0.358) | 1.586 | -0.435 (0.367) | 0.647 | 0.478 (0.357) | 1.612 | -0.419 (0.367) | 0.658 | -0.897 (0.479) | 0.408 |
| Age | -0.030 (0.012)* | 0.971 | -0.008 (0.016) | 0.992 | -0.032 (0.012)* | 0.969 | -0.010 (0.016) | 0.99 | 0.022 (0.019) | 1.022 |
| Orga. size (ref: 1-14 e.) | ||||||||||
| 15-49 | -0.387 (0.490) | 0.679 | -0.620 (0.555) | 0.538 | 0.443 (0.493) | 1.557 | 0.210 (0.557) | 1.233 | -0.233 (0.687) | 0.792 |
| 50-249 | -0.116 (0.453) | 0.891 | -0.588 (0.493) | 0.555 | 0.407 (0.444) | 1.502 | -0.066 (0.490) | 0.936 | -0.472 (0.619) | 0.624 |
| 250+ | -0.118 (0.466) | 0.889 | -0.116 (0.468) | 0.89 | 0.217 (0.446) | 1.242 | 0.219 (0.461) | 1.245 | 0.002 (0.607) | 1.002 |
| Education (ref: ISCED 1-3) | ||||||||||
| ISCED 4-5 | -0.474 (0.393) | 0.623 | -0.455 (0.716) | 0.634 | 0.196 (0.421) | 1.216 | 0.214 (0.721) | 1.239 | 0.019 (0.781) | 1.019 |
| ISCED 6-8 | -1.748 (0.428)*** | 0.174 | 0.816 (0.428) | 2.262 | -1.293 (0.438)** | 0.274 | 1.271 (0.423)** | 3.563 | 2.564 (0.562)*** | 12.986 |
| Healthcare setting | 2.631 (0.454)*** | 13.888 | -2.905 (1.067)** | 0.055 | 2.460 (0.478)*** | 11.71 | -3.075 (1.050)** | 0.046 | -5.536 (1.085)*** | 0.004 |
| Occupation (ref: Professional) | ||||||||||
| Manager | -0.159 (0.958) | 0.853 | -0.183 (0.570) | 0.832 | 0.249 (1.003) | 1.282 | 0.225 (0.574) | 1.252 | -0.024 (1.077) | 0.976 |
| Technicians | 0.290 (0.551) | 1.337 | -0.394 (0.492) | 0.674 | 0.567 (0.545) | 1.762 | -0.118 (0.491) | 0.889 | -0.684 (0.692) | 0.504 |
| Clerical support workers | -2.039 (1.784) | 0.13 | -1.120 (0.556)* | 0.326 | -1.005 (1.772) | 0.366 | -0.086 (0.562) | 0.918 | 0.919 (1.837) | 2.507 |
| Service and sales workers | 2.050 (0.741)** | 7.769 | -25.010 (0.741)*** | 0.000 | 2.287 (0.724)** | 9.847 | -24.773 (0.724)*** | 0.000 | -27.060 (0.000)a | 0.000 |
| Craft workers | 1.431 (0.813) | 4.183 | -25.080 (0.813)*** | 0.000 | 1.695 (0.804)* | 5.449 | -24.816 (0.804)*** | 0.000 | -26.511 (0.000)a | 0.000 |
| Others | 1.544 (0.750)* | 4.684 | -25.132 (0.750)*** | 0.000 | 1.789 (0.751)* | 5.984 | -24.887 (0.751)*** | 0.000 | -26.676 (0.000)a | 0.000 |
* p < .05; ** p < .01; *** p < .001; a these parameters were fixed to avoid singularity of the information matrix that were caused by empty cells in the joint distribution of the (latent) class variable and the predictor variables. SE Standard error of the coefficient; OR Odds ratio; Gender: 0 = male, 1 = female; Healthcare setting: 0 = no, 1 = yes; Class 1: Low level of countermeasures; Class 2: Medium level of countermeasures; Class 3: High level of countermeasures; Class 4: High level of countermeasures low distance; Class 5: Permanent telecommuting
Outcomes of class membership
The associations between the different classes and the outcome variables are displayed in Table 5 (for a quick graphical overview see Figure A1 and A2 in the online supplement). The reliabilities of the outcome measures ranged between .74 and .91 (see Table 5 first column). On average, members of the High level of countermeasures (3) class showed the highest level of well-being (i.e., highest mean on general psychological well-being, vigor, and work satisfaction and lowest mean on work-related burnout, somatic complaints, and second lowest mean on fear of COVID-19 infection), followed by the members of the permanent telecommuting (5) and Medium level of countermeasures (2) classes. Members of the permanent telecommuting (5) class could not be differentiated from members of the Medium level of countermeasures (2) class with regard to general psychological well-being, work-related burnout, vigor, and work satisfaction. However, members of the permanent telecommuting (5) class showed lower levels of somatic complaints and lower fear of COVID-19 infection compared to members of the Medium level of countermeasures (2) class. Members of the Low level of countermeasures (1) and High level of countermeasures low distance (4) classes showed the lowest levels of well-being (i.e., lowest means on general psychological well-being, vigor, and work satisfaction and highest means on work-related burnout, somatic complaints, and fear of COVID-19 infection). Members of the Low level of countermeasures (1) class showed a higher level of work-related burnout and lower work satisfaction than members of the High level of countermeasures low distance (4) class.
Table 5.
Associations between latent class membership and the outcomes
| Outcome variable | Class 1 M [CI95] | Class 2 M [CI95] | Class 3 M [CI95] | Class 4 M [CI95] | Class 5 M [CI95] | Summary of statistically significant differences (p < .05) after Benjamini-Hochberg adjustment |
|---|---|---|---|---|---|---|
| General psychological well-being (ωC [CI95] = .91 [.90, .92]) | -0.817 [-1.066; -0.568] | -0.044 [-0.207; 0.119] | 0.888 [0.792; 0.984] | -0.423 [-0.960; 0.114] | 0.150 [-0.121; 0.421] | 1 < 2 < 3; 1 = 4; 1 < 5; 2 = 4 = 5; 4 < 3; 5 < 3 |
| Work-related burnout (ωC [CI95] = .85 [.84, .87]) | 1.086 [0.898; 1.274] | -0.027 [-0.178; 0.124] | -0.934 [-1.032; -0.836] | 0.393 [-0.033; 0.819] | -0.092 [-0.355; 0.171] | 3 < 2 < 1; 4 < 1; 5 < 1; 2 = 4 = 5; 3 < 4; 3 < 5 |
| Vigor (ωC [CI95] = .74 [.71, .76]) | -0.828 [-1.046; -0.610] | 0.009 [-0.132; 0.150] | 0.730 [0.646; 0.814] | -0.239 [-0.672; 0.194] | -0.061 [-0.308; 0.186] | 1 < 2 < 3; 1 = 4; 1 < 5; 2 = 4 = 5; 4 < 3; 5 < 3; 4 = 5 |
| Work satisfaction (ωC [CI95] = .83 [.80, .85]) | -0.985 [-1.169; -0.801] | 0.027 [-0.059; 0.113] | 0.779 [0.673; 0.885] | -0.303 [-0.554; -0.052] | 0.308 [0.010; 0.606] | 1 < 2 < 3; 4 < 2; 2 = 5; 4 < 3; 4 < 5 |
| Somatic complaints (ωC [CI95] = .78 [.76, .80]) | 0.698 [0.545; 0.851] | -0.043 [-0.153; 0.067] | -0.626 [-0.740; -0.512] | 0.481 [0.269; 0.693] | -0.411 [-0.709; -0.113] | 3 < 2 < 1; 1 = 4; 5 < 1; 2 < 4; 5 < 2; 3 < 4; 3 = 5; 5 < 4; |
| Fear of COVID-19 infection | 3.260 [3.048; 3.472] | 2.580 [2.437; 2.723] | 2.148 [2.003; 2.293] | 3.235 [2.915; 3.555] | 2.036 [1.677; 2.395] | 3 < 2 < 1; 1 = 4; 5 < 1; 2 < 4; 5 < 2; 3 < 4; 3 = 5; 5 < 4 |
M [CI95] = Class-specific mean with 95% confidence interval; Values of general psychological well-being, work-related burnout, vigor, work satisfaction, and somatic complaints represent factor scores (M = 0; SD = 1) estimated from CFA’s with WLSMV estimator; ωC [CI95] = Categorical Omega with 95% confidence interval; Class 1: Low level of countermeasures; Class 2: Medium level of countermeasures; Class 3: High level of countermeasures; Class 4: High level of countermeasures low distance; Class 5: Permanent telecommuting. Last column represents the statistically significant differences (p < .05) after Benjamini-Hochberg adjustment
Discussion
Our results revealed four latent classes with regard to organizational COVID-19 countermeasures. Whereas the classes 1, 2, and 3 (Low level of countermeasures, Medium level of countermeasures, High level of countermeasures, respectively) particularly present differences in the absolute level of the indicators (quantitative differences), class 4 (High level of countermeasures low distance) is qualitatively different from the other classes. On one hand, as one would expect, the classes 1, 2, and 3 showed a clear ranking regarding the different well-being outcomes, with members of class 3 (High level of countermeasures) showing the highest level of well-being and members of class 1 (Low level of countermeasures) yielding the lowest level of well-being in terms of general psychological well-being, vigor, work satisfaction, work-related burnout, somatic complaints, and fear of COVID-19 infection. On the other hand, despite the high level on most countermeasures (except minimum distance), members of class 4 (High level of countermeasures low distance) showed similarly low levels of well-being as members of class 1 (Low level of countermeasures). This might be explained by the fact that this class showed a profile of countermeasures that is typically faced by employees working in the healthcare setting where wearing face masks and protective clothing is obligatory. Indeed, employees working in the healthcare setting were far more likely to be members of class 4 (High level of countermeasures low distance) relative to all other classes (odds ratios between 11.765 and 250)8. These employees are generally more at risk of getting an infection as they face higher levels of exposure to infected individuals due to work demands (Nguyen et al., 2020). Moreover, it has been shown that the current COVID-19 pandemic has a pervasive and profound impact on the mental health and well-being of healthcare workers (e.g., Busch et al., 2021).
The present study showed that the working situation and workplace safety in terms of COVID-19 countermeasures is related to mental health and well-being outcomes. Low levels of countermeasures are related to low levels of mental health and well-being. This finding is in line with previous studies showing that the COVID-19 countermeasures are associated with reduced psychological distress (Sasaki et al., 2020c). Somewhat contrary to Sasaki et al. (2020c) we found that classes with higher levels of COVID-19 countermeasures yielded lower fear of COVID-19 infection (with the exception of the High level of countermeasures low distance class). This might be explained by the fact that Sasaki et al. (2020c) implemented a variable-centered approach (i.e., number of COVID-19 countermeasures). As our results revealed, this approach might be less suitable as the different countermeasures are not equivalent or interchangeable.9 Additionally, this result might be influenced by the time of data collection (that was between March 19-22, 2020), where the pandemic was in an early stage and implementing theses countermeasures raised awareness, and, thus, fear in the employees. Moreover, our results are also in line with results from studies that investigated the effect of COVID-19 countermeasures on well-being and mental health within specific occupation groups (Arnetz et al., 2020; Havaei et al., 2021). However, the person-centered approach in the current study revealed that employees do not only differ regarding the absolute level of the countermeasures but also regarding qualitative differences, thus, making the number of countermeasures a limited approach to investigate the relationship between countermeasures and well-being and mental health.
Implications
The COVID-19 pandemic and the global reaction to it has reinforced past inequalities while at the same time also creating new ones. Inequalities emerge in terms of health (Abedi et al., 2020; Gibson et al., 2021), job satisfaction, and productivity (Feng & Savani, 2020), as well as job and income loss (Witteveen & Velthorst, 2020). The present study showed that inequalities also emerge in terms of access to organizational COVID-19 countermeasures and related mental health and well-being. Policy makers and organizations should implement COVID-19 countermeasures more comprehensively as a strategy to prevent and mitigate adverse mental health and well-being outcomes during the COVID-19 pandemic. One fifth (20.1%) of the employees were members of the Low level of countermeasures class that had means on many countermeasures below 3 (which equals the response category to a medium extent). These employees suffered the most in terms of psychological health and well-being. Thus, organizations should either try to facilitate permanent telecommuting or, if not possible, increase safety measures at work, particularly, social distancing. More globally, organizations might consider implementing safety climate interventions to increase the overall safety level (Lee et al., 2019). Either way, organizations play a crucial role during the COVID-19-related changes in workplace practices to maintain psychological safety (Lee, 2021).
Study strengths and limitations
The strength of the study is the large sample that is nationally representative in terms of the Luxembourgish workforce. However, some limitations of the current study warrant consideration. First, a cross-sectional design was implemented, precluding a causal interpretation between the COVID-19 countermeasure classes and well-being. Although reversed causation seems unlikely, it has to be noted that important covariates of well-being, i.e., work related stressors such as mental strain (Steffgen et al., 2015), emotional demands (Hülsheger & Schewe, 2011), or workplace mobbing (Sischka et al., 2021) that also might have increased with the pandemic, were not adjusted and, thus, might have confounded the results (MacKinnon et al., 2000). Second, only self-reported measures were employed, possibly contaminating associations with common method variance (Podsakoff et al., 2012). Third, self-reports on countermeasures might only be regarded as rough indicators of the actual workplace safety situation. Finally, data collection was conducted during a time interval where the number of active infections was relatively low. It is conceivable that the COVID-19 prevalence at different stages of the pandemic might moderate the reported associations. Following this notion, one might argue that the association between COVID-19 countermeasures and well-being as well as mental health would be more pronounced at stages with higher numbers of active infections.
Conclusion
The working situation and workplace safety in terms of COVID-19 countermeasures is directly related to mental health and well-being outcomes. Employees who have to work under a low level of countermeasures are especially at risk of reduced mental health and well-being. On the other hand, employees who work in organizations with a high level of countermeasures or are able to permanently telecommute show higher level of mental health and well-being.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank Sylvain Hoffmann and David Büchel.
Author contributions
Conceptualization: Philipp E. Sischka, Alexander F. Schmidt, Georges Steffgen.
Data curation: Philipp E. Sischka.
Formal analysis: Philipp E. Sischka.
Funding acquisition: Georges Steffgen, Philipp E. Sischka.
Methodology: Philipp E. Sischka.
Writing – original draft: Philipp E. Sischka.
Writing – review & editing: Philipp E. Sischka, Alexander F. Schmidt, Georges Steffgen.
Funding
This research was supported by a grant from the Luxembourg Chamber of Labor (no grant number available). The study design and data collection were discussed and decided together with the Chamber of Labor. The Chamber of Labor was not involved in the interpretation of data, in the writing of the report, nor in the decision to submit the article for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position of the Chamber of Labor.
Data and software code availability
Part of the data, i.e., the organizational COVID-19 countermeasures and the well-being indicators, as well as the R and Mplus scripts are stored on OSF (https://osf.io/eqf4n/). The other part of the data, e.g., gender, age, etc. are available from the corresponding author on reasonable request.
Declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki and APA ethics policy regarding the treatment of participants.
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Software information
Data analysis was done in R (Version 4.1.3, R Core Team, 2022) and Mplus (v8.8; Muthén & Muthén, 2017). Data transformations were done with the tidyverse (Wickham et al., 2019), car (Fox & Weisberg, 2018), labelled (Larmarange et al., 2021), and sjlabelled (Lüdecke & Ranzolin, 2021) packages. Descriptive statistics were calculated with the weights (Pasek et al., 2021) package. Reliabilities were calculated with the MBESS (Kelley, 2021) package. The latent class analyses were done in Mplus (v8.8; Muthén & Muthén, 2017) and read in R with the package MplusAutomation (Hallquist & Wiley, 2018 ). The graphs were created with the ggplot2 (Wickham et al., 2016) and ggpubr (Kassambara, 2020 ) packages. The data codebook was created with the codebook (Arslan, 2019) package.
Footnotes
Due to the experience from previous data collection waves that younger employees take part in the survey less often, these were disproportionally oversampled (see Schütz & Thiele, 2020).
The low percentage of permanent telecommuters might be due to the data collection time interval between 09.06.2020 and 05.10.2020. During that time interval – between the first and second wave of infections – the number of active infections was relatively low (see https://covid19.public.lu/fr/graph.html).
Occupations with less than 100 respondents were summarized in Others.
Unfortunately, due to a programming error this item was only shown if respondents answered the previous question “How much has the crisis impacted on your professional situation?” with 1 = a great deal, 2 = quite a lot, and 3 = not a lot (85.8%, n = 2017), while respondents that chose the answer category 4 = not at all have not seen this item (14.2%, n = 333).
The calculation of the Bootstrap likelihood ratio test (BLRT; McLachlan & Peel, 2000) that is also recommended to determine the number of classes (Nylund et al., 2007) is currently not supported in combination with survey weights within Mplus.
Profile plots are usually used for continuous class indicators but are also useful for ordinal class indicators (Oberski, 2016).
Class 4 (High level of countermeasures low distance) was the added class between the 3-class and the 4-class solution.
In Table 4 the odds ratios are displayed with High level of countermeasures low distance as reference class. Thus, we reported here the inverse values (i.e., 1/0.085 and 1/0.004) for ease of interpretation.
As a control analysis, we calculated the mean for the different COVID-19 countermeasures. Members of the High level of countermeasures (3) class had the highest values (M = 3.41; 95% CI [3.38; 3.44], SD = 0.40), followed by members of High level of countermeasures low distance (4) (M = 3.03; 95% CI [2.98; 3.07], SD = 0.36), members of Medium level of countermeasures (2) (M = 2.70; 95% CI [2.67; 2.73], SD = 0.37), and members of Low level of countermeasures (4) (M = 1.66; 95% CI [1.61; 1.70], SD = 0.45) classes. Thus, despite the second highest value on the mean of the different COVID-19 countermeasures, members of the High level of countermeasures low distance (4) class showed the second highest fear of infection. Nevertheless, the correlation between the mean of the different COVID-19 countermeasures and fear of infection was negative (r = -.22; 95% CI [-.27; -.18]; t = -9.637; p < .001).
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abedi, V., Olulana, O., Avula, V., Chaudhary, D., Khan, A., Shahjouei, S., Li, J., & Zand, R. (2020). Racial, economic, and health inequality and COVID-19 infection in the United States. Journal of Racial and Ethnic Health Disparities,8(3), 732–742. 10.1007/s40615-020-00833-4 [DOI] [PMC free article] [PubMed]
- Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed]
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. doi: 10.1007/bf02294359. [DOI] [Google Scholar]
- Arnetz JE, Goetz CM, Sudan S, Arble E, Janisse J, Arnetz BB. Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. Journal of Occupational and Environmental Medicine. 2020;62(11):892–897. doi: 10.1097/jom.0000000000001999. [DOI] [PubMed] [Google Scholar]
- Arslan RC. How to automatically document data with the codebook package to facilitate data reuse. Advances in Methods and Practices in Psychological Science. 2019;2(2):169–187. doi: 10.1177/2515245919838783. [DOI] [Google Scholar]
- Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling. 2014;21(3):329–341. doi: 10.1080/10705511.2014.915181. [DOI] [Google Scholar]
- Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PloS one. 2020;15(4):e0232452. doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banfield JD, Raftery AE. Model-based Gaussian and non-Gaussian clustering. Biometrics. 1993;49(3):803–821. doi: 10.2307/253220. [DOI] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological) 1995;57(1):289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- Berkowitz SA, Basu S. Unemployment insurance, health-related social needs, health care access, and mental health during the COVID-19 Pandemic. JAMA Internal Medicine. 2021;181(5):699–702. doi: 10.1001/jamainternmed.2020.7048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs A, Brough P, Barbour JP. Exposure to extraorganizational stressors: Impact on mental health and organizational perceptions for police officers. International Journal of Stress Management. 2014;21(3):255–282. doi: 10.1037/a0037297. [DOI] [Google Scholar]
- Bozdogan H. Model selection and Akaike’s information criterion (AIC): The general theory and its analytical extensions. Psychometrika. 1987;52(3):345–370. doi: 10.1007/bf02294361. [DOI] [Google Scholar]
- Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychotherapy and Psychosomatics. 2021;90(3):178–190. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carillo K, Cachat-Rosset G, Marsan J, Saba T, Klarsfeld A. Adjusting to epidemic-induced telework: Empirical insights from teleworkers in France. European Journal of Information Systems. 2020;30(1):69–88. doi: 10.1080/0960085X.2020.1829512. [DOI] [Google Scholar]
- Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13(2):195–212. doi: 10.1007/bf01246098. [DOI] [Google Scholar]
- Chang Y, Chien C, Shen LF. Telecommuting during the coronavirus pandemic: Future time orientation as a mediator between proactive coping and perceived work productivity in two cultural samples. Personality and Individual Differences. 2021;171:110508. doi: 10.1016/j.paid.2020.110508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, S. L., & Muthén, B. O. (2009). Relating latent class analysis results to variables not included in the analysis. https://www.statmodel.com/download/relatinglca.pdf
- Clarke S. An integrative model of safety climate: Linking psychological climate and work attitudes to individual safety outcomes using meta-analysis. Journal of Occupational and Organizational psychology. 2010;83(3):553–578. doi: 10.1348/096317909X452122. [DOI] [Google Scholar]
- Debus, M. E., Unger, D., & Probst, T. M. (2021). Dirty work on the COVID-19 frontlines: Exacerbating the situation of marginalized groups in marginalized professions. Industrial and Organizational Psychology, 14(1-2). 10.1017/iop.2021.33
- Enders, C. K. (2010). Applied missing data analysis. Guilford.
- Feng Z, Savani K. Covid-19 created a gender gap in perceived work productivity and job satisfaction: implications for dual-career parents working from home. Gender in Management. 2020;35(7/8):719–736. doi: 10.1108/GM-07-2020-0202. [DOI] [Google Scholar]
- Finney, S. J., & DiStefano, C. (2013). Nonnormal and categorical data in structural equation modeling. In G. R. Hancock & R. O. Mueller (Eds.), Structural equation modeling – a second course (2nd ed., pp. 439–492). Information Age Publishing.
- Firew, T., Sano, E. D., Lee, J. W., Flores, S., Lang, K., Salman, K., Greene, M. C., & Chang, B. P. (2020). Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open,10, e042752. 10.1136/bmjopen-2020-042752 [DOI] [PMC free article] [PubMed]
- Fox, J., & Weisberg, S. (2018). An R companion to applied regression. Sage publications.
- Gibson B, Schneider J, Talamonti D, Forshaw M. The impact of inequality on mental health outcomes during the COVID-19 pandemic: A systematic review. Canadian Psychology. 2021;62(1):101–126. doi: 10.1037/cap0000272. [DOI] [Google Scholar]
- Giorgi, G., Lecca, L. I., Alessio, F., Finstad, G. L., Bondanini, G., Lulli, L. G., Arcangeli, G., & Mucci, N. (2020). COVID-19-related mental health effects in the workplace: a narrative review. International Journal of Environmental Research and Public Health,17, 7857. 10.3390/ijerph17217857 [DOI] [PMC free article] [PubMed]
- Görlich Y, Stadelmann D. Mental health of flying cabin crews: depression, anxiety, and stress before and during the CoViD-19 pandemic. Frontiers in Psychology. 2020;11:581496. doi: 10.3389/fpsyg.2020.581496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gullone E. The development of normal fear: A century of research. Clinical Psychology Review. 2000;20(4):429–451. doi: 10.1016/S0272-7358(99)00034-3. [DOI] [PubMed] [Google Scholar]
- Hallquist MN, Wiley JF. MplusAutomation: An R package for facilitating large-scale latent variable analyses in Mplus. Structural Equation Modeling. 2018;25(4):621–638. doi: 10.1080/10705511.2017.1402334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction. 2021;19(5):1875–1888. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havaei, F., Ma, A., Staempfli, S., & MacPhee, M. (2021, January). Nurses’ workplace conditions impacting their mental health during COVID-19: A cross-sectional survey study. Healthcare, 9(1), 84. 10.3390/healthcare9010084 [DOI] [PMC free article] [PubMed]
- Hipp JR, Bauer DJ. Local solutions in the estimation of growth mixture models. Psychological Methods. 2006;11(1):36–53. doi: 10.1037/1082-989X.11.1.36. [DOI] [PubMed] [Google Scholar]
- Hu X, Yan H, Casey T, Wu CH. Creating a safe haven during the crisis: How organizations can achieve deep compliance with COVID-19 safety measures in the hospitality industry. International Journal of Hospitality Management. 2021;92:102662. doi: 10.1016/j.ijhm.2020.102662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hülsheger UR, Schewe AF. On the costs and benefits of emotional labor: a meta-analysis of three decades of research. Journal of Occupational Health Psychology. 2011;16:361–389. doi: 10.1037/a0022876. [DOI] [PubMed] [Google Scholar]
- International Labour Organization. (Eds.). (2012). International standard classification of occupations: ISCO-08. Vol. 1. Structure, group definitions and correspondence tables. Geneva, Switzerland: International Labour Office. https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms_172572.pdf. Accessed 06.07.2022.
- Ishimaru, T., Nagata, M., Hino, A., Yamashita, S., Tateishi, S., Tsuji, M., Ogami, A., Matsuda, S., Fujino, Y., & Fujino, Y. (2021). Workplace measures against COVID-19 during the winter third wave in Japan: company size-based differences. Journal of Occupational Health,63(1), e12224. 10.1101/2021.02.14.21251716 [DOI] [PMC free article] [PubMed]
- Kassambara, A. (2020). ggpubr: ’ggplot2′ based publication ready plots (Version 0.4.0) [R package]. https://cran.r-project.org/web/packages/ggpubr/index.html . Accessed 06.07.2022.
- Kelley K, Pornprasertmanit S. Confidence intervals for population reliability coefficients: Evaluation of methods, recommendations, and software for composite measures. Psychological Methods. 2016;21(1):69–92. doi: 10.1037/a0040086. [DOI] [PubMed] [Google Scholar]
- Kelley, K. (2021). MBESS: The MBESS R Package (Version 4.8.1) [R package]. https://cran.r-project.org/web/packages/MBESS/index.html. Accessed 06.07.2022.
- Kim, H., Hegde, S., LaFiura, C., Raghavan, M., Sun, N., Cheng, S., Rebholz, C. M., & Seidelmann, S. B. (2021). Access to personal protective equipment in exposed healthcare workers and COVID-19 illness, severity, symptoms and duration: A population-based case-control study in six countries. BMJ Global Health,6(1), e004611. 10.1136/bmjgh-2020-004611 [DOI] [PMC free article] [PubMed]
- Labrague LJ, de Los Santos JAA. Fear of Covid-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management. 2021;29(3):395–403. doi: 10.1111/jonm.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Tan X, Bray BC. Latent class analysis with distal outcomes: A flexible model-based approach. Structural Equation Modeling. 2013;20(1):1–26. doi: 10.1080/10705511.2013.742377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larmarange, J., Ludecke, D., Wickham, H., Bojanowski, M., Briatte, F. (2021). labelled: Manipulating labelled data. R package Version 2.8.0. https://cran.r-project.org/web/packages/labelled/index.html. Accessed 06.07.2022.
- Laufs, J., & Waseem, Z. (2020). Policing in pandemics: A systematic review and best practices for police response to COVID-19. International Journal of Disaster Risk Reduction,101812,. 10.1016/j.ijdrr.2020.101812 [DOI] [PMC free article] [PubMed]
- Lee H. Changes in workplace practices during the COVID-19 pandemic: the roles of emotion, psychological safety and organisation support. Journal of Organizational Effectiveness: People and Performance. 2021;8(1):97–128. doi: 10.1108/JOEPP-06-2020-0104. [DOI] [Google Scholar]
- Lee J, Huang YH, Cheung JH, Chen Z, Shaw WS. A systematic review of the safety climate intervention literature: Past trends and future directions. Journal of Occupational Health Psychology. 2019;24(1):66–91. doi: 10.1037/ocp0000113. [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. doi: 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- Lovreglio, P., Leso, V., Riccardi, E., Stufano, A., Pacella, D., Cagnazzo, F., Luigia Ercolano, M., & Iavicoli, I. (2021). Coronavirus disease (COVID-19) pandemic: the psychological well-being in a cohort of workers of a multinational company. Advance online publication. 10.1016/j.shaw.2021.10.006 [DOI] [PMC free article] [PubMed]
- Lüdecke, D., Ranzolin, D. (2021). sjlabelled: Labelled data utility functions. R package Version 1.1.8. https://cran.r-project.org/web/packages/sjlabelled/index.html. Accessed 06.07.2022.
- Lundberg, U., Dohns, I. E., Melin, B., Sandsjö, L., Palmerud, G., Kadefors, R., Ekström, M., & Parr, D. (1999). Psychophysiological stress responses, muscle tension, and neck and shoulder pain among supermarket cashiers. Journal of Occupational Health Psychology,4(3), 245–255. 10.1037/1076-8998.4.3.245 [DOI] [PubMed]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prevention Science. 2000;1(4):173–181. doi: 10.1023/A:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masyn, K. E. (2013). Latent class analysis and finite mixture modeling. In T. D. Little (Ed.), The Oxford handbook of quantitative methods: Vol. 2. Statistical analysis (pp. 551–611). Oxford University Press. 10.1093/oxfordhb/9780199934898.013.0025
- McLachlan G, Peel D. Finite mixture modeling. Wiley. 2000 doi: 10.1002/0471721182. [DOI] [Google Scholar]
- Meyer B, Zill A, Dilba D, Gerlach R, Schumann S. Employee psychological well-being during the COVID-19 pandemic in Germany: A longitudinal study of demands, resources, and exhaustion. International Journal of Psychology. 2021;56(4):532–550. doi: 10.1002/ijop.12743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin AJS, Bujacz A, Gagné M. Person-centered methodologies in the organizational sciences. Organizational Research Methods. 2018;21(4):803–813. doi: 10.1177/1094428118773856. [DOI] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2017). Mplus user’s guide (version 8). Muthén & Muthén.
- Nabe-Nielsen K, Nilsson CJ, Juul-Madsen M, Bredal C, Hansen LOP, Hansen ÅM. COVID-19 risk management at the workplace, fear of infection and fear of transmission of infection among frontline employees. Occupational and Environmental Medicine. 2021;78(4):248–254. doi: 10.1136/oemed-2020-106831. [DOI] [PubMed] [Google Scholar]
- Nagin D. Group-based modeling of development. Harvard University Press; 2005. [Google Scholar]
- Neal A, Griffin MA. A study of the lagged relationships among safety climate, safety motivation, safety behavior, and accidents at the individual and group levels. Journal of Applied Psychology. 2006;91(4):946–953. doi: 10.1037/0021-9010.91.4.946. [DOI] [PubMed] [Google Scholar]
- Nguyen, L. H., Drew, D. A., Graham, M. S., Joshi, A. D., Guo, C. G., Ma, W., Mehta, R. S., Warner, E. T., Sikavi, D. R., Lo, C. H., Kwon, S., Song, M., Mucci, L. A., Stampfer, M. J., Willett, W. C., Eliassen, A. H., Hart, J. E., Chavarro, J. E., Rich-Edwards, J. W., Davies, R., … Coronavirus Pandemic Epidemiology Consortium (2020). Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health,5(9), e475–e483. 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed]
- Nomura S, Yoneoka D, Tanoue Y, Kawashima T, Shi S, Eguchi A, Miyata H. Time to reconsider diverse ways of working in Japan to promote social distancing measures against the COVID-19. Journal of Urban Health. 2020;97(4):457–460. doi: 10.1007/s11524-020-00464-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Nylund-Gibson K, Choi AY. Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science. 2018;4(4):440–461. doi: 10.1037/tps0000176. [DOI] [Google Scholar]
- Nylund-Gibson K, Grimm R, Quirk M, Furlong M. A latent transition mixture model using the three-step specification. Structural Equation Modeling. 2014;21(3):439–454. doi: 10.1080/10705511.2014.915375. [DOI] [Google Scholar]
- Oberski, D. (2016). Mixture models: Latent profile and latent class analysis. In J. Robertosn & M. Kaptein (Eds.), Modern statistical methods for HCI (pp. 275-287). Springer, Cham. 10.1007/978-3-319-26633-6_12
- Pasek, J., Tahk, A., Culter, G., Schwemmle, M. (2021). weights: Weighting and weighted statistics. R package Version 1.0.2. https://cran.r-project.org/web/packages/weights/index.html. Accessed 06.07.2022.
- Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology. 2012;63:539–569. doi: 10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing.
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. doi: 10.2307/271063. [DOI] [Google Scholar]
- Rathod, S., Pallikadavath, S., Young, A. H., Graves, L., Rahman, M. M., Brooks, A., Soomro, M., Rathod, P., & Phiri, P. (2020). Psychological impact of COVID-19 pandemic: Protocol and results of first three weeks from an international cross-section survey-focus on health professionals. Journal of Affective Disorders Reports,1, 100005. 10.1016/j.jadr.2020.100005 [DOI] [PMC free article] [PubMed]
- Ravikumar, T (2022). Occupational stress and psychological wellbeing during COVID 19: Mediating role of positive psychological capital. Current Psychology. Advance online publication. 10.1007/s12144-022-02861-1 [DOI] [PMC free article] [PubMed]
- Rossi R, Socci V, Pacitti F, Mensi S, Di Marco A, Siracusano A, Di Lorenzo G. Mental Health Outcomes Among Healthcare Workers and the General Population During the COVID-19 in Italy. Frontiers in Psychology. 2020;11:608986. doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph CW, Allan B, Clark M, Hertel G, Hirschi A, Kunze F, Shockley K, Shoss M, Sonnentag S, Zacher H. Pandemics: Implications for Research and Practice in Industrial and Organizational Psychology. Industrial and Organizational Psychology. 2021;14(1–2):1–35. doi: 10.1017/iop.2020.48. [DOI] [Google Scholar]
- Sasaki N, Kuroda R, Tsuno K, Kawakami N. The deterioration of mental health among healthcare workers during the COVID-19 outbreak: A population-based cohort study of workers in Japan. Scandinavian Journal of Work, Environment & Health. 2020;46(6):639–644. doi: 10.5271/sjweh.3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki, N., Kuroda, R., Tsuno, K., & Kawakami, N. (2020). Workplace responses to COVID-19 and their association with company size and industry in an early stage of the epidemic in Japan. Environmental and Occupational Health Practice,2020–0007,. 10.1539/eohp.2020-0007-oa
- Sasaki N, Kuroda R, Tsuno K, Kawakami N. Workplace responses to COVID-19 associated with mental health and work performance of employees in Japan. Journal of Occupational Health. 2020;62(1):e12134. doi: 10.1002/1348-9585.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki, N., Imamura, K., Kataoka, M., Kuroda, R., Tsuno, K., Sawada, U., Asaoka, H., Iida, M., & Kawakami, N. (2021). COVID-19 measurements at the workplace in various industries and company sizes: a 2-month follow-up cohort study of full-time employees in Japan. Environmental and Occupational Health Practice,2020–0017,. 10.1539/eohp.2020-0017-oa
- Schaufeli WB, Bakker AB, Salanova M. The measurement of work engagement with a short questionnaire a cross-national study. Educational and Psychological Measurement. 2006;66(4):701–716. doi: 10.1177/0013164405282471. [DOI] [Google Scholar]
- Schütz, H., & Thiele, N. (2020). Quality of Work Luxembourg 2020. infas Institut für angewandte Sozialwissenschaft GmbH. https://www.csl.lu/wp-content/uploads/2021/01/infas-rapport-quality-of-work-index-luxembourg-2020-allemand.pdf. Accessed 06.07.2022.
- Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6(2):461–464. doi: 10.1214/aos/1176344136. [DOI] [Google Scholar]
- Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52(3):333–343. doi: 10.1007/bf02294360. [DOI] [Google Scholar]
- Şimşir Z, Koç H, Seki T, Griffiths MD. The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death studies. 2022;46(3):515–523. doi: 10.1080/07481187.2021.1889097. [DOI] [PubMed] [Google Scholar]
- Sinclair, R. R., Allen, T., Barber, L., Bergman, M., Britt, T., Butler, A., Ford, M., Hammer, L., Kath, L., Probst, T., & Yuan, Z. (2020). Occupational health science in the time of COVID-19: Now more than ever. Occupational Health Science,4(1–2), 1–22. 10.1007/s41542-020-00064-3 [DOI] [PMC free article] [PubMed]
- Sinclair RR, Probst TM, Watson GP, Bazzoli A. Caught between Scylla and Charybdis: How economic stressors and occupational risk factors influence workers’ occupational health reactions to COVID-19. Applied Psychology. 2021;70(1):85–119. doi: 10.1111/apps.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sischka PE, Costa AP, Steffgen G, Schmidt AF. The WHO-5 Well-Being Index – Validation based on item response theory and the analysis of measurement invariance across 35 countries. Journal of Affective Disorders Reports. 2020;1:100020. doi: 10.1016/j.jadr.2020.100020. [DOI] [Google Scholar]
- Sischka PE, Melzer A, Schmidt AF, Steffgen G. Psychological contract violation or basic need frustration? Psychological mechanisms behind the effects of workplace bullying. Frontiers in Psychology. 2021;12:627968. doi: 10.3389/fpsyg.2021.627968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sischka, P. E., & Steffgen, G. (2021a). Extended telecommuting due to COVID-19 and the impact on working life. In G. Mein, & J. Pause (eds.), Self and Society in the Corona Crisis. Perspectives from the Humanities and Social Sciences. Melusina Press.
- Sischka, P., & Steffgen, G. (2021b). Quality of Work. Forschungsbericht zur Erhebungswelle 2020. Working Paper. Luxembourg: Universität Luxemburg. https://www.csl.lu/wp-content/uploads/2021/01/sischka-p.-steffgen-g.-2021-quality-of-work.-forschungsbericht-zur-erhebungswelle-2020.-working-paper.-university-of-luxembourg-luxembourg-allemand.pdf. Accessed 06.07.2022.
- Steffgen G, Kohl D, Reese G, Happ C, Sischka P. Quality of work: Validation of a new instrument in three languages. International Journal of Environmental Research and Public Health. 2015;12(12):14988–15006. doi: 10.3390/ijerph121214958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffgen G, Sischka PE, Fernandez de Henestrosa M. The Quality of Work Index and the Quality of Employment Index: A Multidimensional Approach of Job Quality and Its Links to Well-Being at Work. International Journal of Environmental Research and Public Health. 2020;17(21):7771. doi: 10.3390/ijerph17217771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. (2019). The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing.
- Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychotherapy and Psychosomatics. 2015;84(3):167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- Uehara, M., Ishimaru, T., Ando, H., Tateishi, S., Eguchi, H., Tsuji, M., Mori, K., Matsuda, S., Fujino, Y., & CORoNaWork Project. (2021). Worries about COVID-19 infection and psychological distress at work and while commuting. Journal of Occupational and Environmental Medicine,63(9), e631–e635. 10.1097/JOM.0000000000002309 [DOI] [PubMed]
- Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Political Analysis. 2010;18(4):450–469. doi: 10.1093/pan/mpq025. [DOI] [Google Scholar]
- Wang M, Hanges PJ. Latent class procedures: Applications to organizational research. Organizational Research Methods. 2011;14(1):24–31. doi: 10.1177/1094428110383988. [DOI] [Google Scholar]
- Wang B, Liu Y, Qian J, Parker SK. Achieving effective remote working during the COVID-19 pandemic: A work design perspective. Applied Psychology. 2021;70(1):16–59. doi: 10.1111/apps.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H. Ggplot2: elegant graphics for data analysis. Springer; 2016. [Google Scholar]
- Wickham, H., Averick, M., Bryan, J., Chang, W., McGowan, L., François, R., Grolemund, G., Hayes, A., Henry, L., Hester, J., Kuhn, M., Pedersen, T. L., Miller, E., Bache, S. M., Müller, K., Ooms, J., Robinson, D., Seide, D. P., Spinu, V., Yutani, H. (2019). Welcome to the Tidyverse. Journal of Open Source Software, 4(43), 1686. 10.21105/joss.01686
- Witteveen, D., & Velthorst, E. (2020). Economic hardship and mental health complaints during COVID-19. Proceedings of the National Academy of Sciences, 117(44), 27277–27284. www.pnas.org/cgi/doi/10.1073/pnas.2009609117 [DOI] [PMC free article] [PubMed]
- Wong, E. L. Y., Ho, K. F., Wong, S. Y. S., Cheung, A. W. L., Yau, P. S. Y., Dong, D., & Yeoh, E. K. (2020). Views on workplace policies and its impact on health-related quality of life during coronavirus disease (COVID-19) pandemic: Cross-sectional survey of employees. International Journal of Health Policy and Management, 11(3), 344–353. 10.34172/ijhpm.2020.127 [DOI] [PMC free article] [PubMed]
- World Health Organization (2020). Getting your workplace ready for COVID-19. https://www.who.int/docs/default-source/coronaviruse/getting-workplace-ready-for-covid-19.pdf. Accessed 06.07.2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Part of the data, i.e., the organizational COVID-19 countermeasures and the well-being indicators, as well as the R and Mplus scripts are stored on OSF (https://osf.io/eqf4n/). The other part of the data, e.g., gender, age, etc. are available from the corresponding author on reasonable request.