Abstract
Background
Cerebral small vessel disease is a progressive disease of the brain's deep perforating blood vessels. It is usually diagnosed based on lesions seen on brain imaging. Cerebral small vessel disease is a common cause of stroke but can also cause a progressive cognitive decline. As antithrombotic therapy is an established treatment for stroke prevention, we sought to determine whether antithrombotic therapy might also be effective in preventing cognitive decline in people with small vessel disease.
Objectives
To assess the effects of antithrombotic therapy for prevention of cognitive decline in people with small vessel disease on neuroimaging but without dementia.
Search methods
We searched ALOIS, the Cochrane Dementia and Cognitive Improvement Review Group's Specialised Register, and the Cochrane Stroke Group's Specialised Register; the most recent search was on 21 July 2021. We also searched MEDLINE, Embase, four other databases and two trials registries. We searched the reference lists of the articles retrieved from these searches. As trials with a stroke focus may include relevant subgroup data, we complemented these searches with a focussed search of all antithrombotic titles in the Cochrane Stroke Group database.
Selection criteria
We included randomised controlled trials (RCT) of people with neuroimaging evidence of at least mild cerebral small vessel disease (defined here as white matter hyperintensities, lacunes of presumed vascular origin and subcortical infarcts) but with no evidence of dementia. The trials had to compare antithrombotic therapy of minimum 24 weeks' duration to no antithrombotic therapy (either placebo or treatment as usual), or compare different antithrombotic treatment regimens. Antithrombotic therapy could include antiplatelet agents (as monotherapy or combination therapy), anticoagulants or a combination.
Data collection and analysis
Two review authors independently screened all the titles identified by the searches. We assessed full texts for eligibility for inclusion according to our prespecified selection criteria, extracted data to a proforma and assessed risk of bias using the Cochrane tool for RCTs. We evaluated the certainty of evidence using GRADE. Due to heterogeneity across included participants, interventions and outcomes of eligible trials, it was not possible to perform meta‐analyses.
Main results
We included three RCTs (3384 participants). One study investigated the effect of antithrombotic therapy in participants not yet on antithrombotic therapy; two studies investigated the effect of additional antithrombotic therapy, one in a population already taking a single antithrombotic agent and one in a mixed population (participants on an antithrombotic drug and antithrombotic‐naive participants). Intervention and follow‐up durations varied from 24 weeks to four years.
Jia 2016 was a placebo‐controlled trial assessing 24 weeks of treatment with DL‐3‐n‐butylphthalide (a compound with multimodal actions, including a putative antiplatelet effect) in 280 Chinese participants with vascular cognitive impairment caused by subcortical ischaemic small vessel disease, but without dementia. There was very low‐certainty evidence for a small difference in cognitive test scores favouring treatment with DL‐3‐n‐butylphthalide, as measured by the 12‐item Alzheimer’s Disease Assessment Scale‐Cognitive subscale (adjusted mean difference −1.07, 95% confidence interval (CI) −2.02 to −0.12), but this difference may not be clinically relevant. There was also very low‐certainty evidence for greater proportional improvement measured with the Clinician Interview‐Based Impression of Change‐Plus Caregiver Input (57% with DL‐3‐n‐butylphthalide versus 42% with placebo; P = 0.01), but there was no difference in other measures of cognition (Mini‐Mental State Examination and Clinical Dementia Rating) or function. There was no evidence of a difference in adverse events between treatment groups.
The SILENCE RCT compared antithrombotic therapy (aspirin) and placebo during four years of treatment in 83 participants with 'silent brain infarcts' who were on no prior antithrombotic therapy. There was very low‐certainty evidence for no difference between groups across various measures of cognition and function, rates of stroke or adverse events.
The Secondary Prevention of Subcortical Stroke Study (SPS3) compared dual antiplatelet therapy (clopidogrel plus aspirin) to aspirin alone in 3020 participants with recent lacunar stroke. There was low‐certainty evidence of no effect on cognitive outcomes as measured by the Cognitive Abilities Screening Instruments (CASI) assessed annually over five years. There was also low‐certainty evidence of no difference in the annual incidence of mild cognitive decline between the two treatment groups (9.7% with dual antiplatelet therapy versus 9.9% with aspirin), or the annual stroke recurrence rate (2.5% with dual antiplatelet therapy versus 2.7% with aspirin). Bleeding risk may be higher with dual antiplatelet therapy (hazard ratio (HR) 2.15, 95% CI 1.49 to 3.11; low certainty evidence), but there may be no significant increase in intracerebral bleeding risk (HR 1.52, 95% CI 0.79 to 2.93; low‐certainty evidence).
None of the included trials assessed the incidence of new dementia.
Authors' conclusions
We found no convincing evidence to suggest any clinically relevant cognitive benefit of using antithrombotic therapy in addition to standard treatment in people with cerebral small vessel disease but without dementia, but there may be an increased bleeding risk with this approach. There was marked heterogeneity across the trials and the certainty of the evidence was generally poor.
Keywords: Humans, Aspirin, Aspirin/therapeutic use, Cerebral Small Vessel Diseases, Cerebral Small Vessel Diseases/complications, Cerebral Small Vessel Diseases/diagnostic imaging, Cerebral Small Vessel Diseases/drug therapy, Cognitive Dysfunction, Cognitive Dysfunction/drug therapy, Cognitive Dysfunction/prevention & control, Dementia, Dementia/prevention & control, Neuroimaging, Platelet Aggregation Inhibitors, Platelet Aggregation Inhibitors/therapeutic use, Stroke, Stroke/diagnostic imaging, Stroke/drug therapy, Stroke/prevention & control
Plain language summary
Antithrombotic therapy to prevent cognitive decline in people with small vessel disease on neuroimaging but without dementia
Background
Disruption of blood flow to the brain can cause problems with memory and thinking. In the condition called 'cerebral small vessel disease', there is damage to the smallest blood vessels that run deep in the brain. This damage can cause stroke but can also be seen on brain scans in people with no obvious stroke symptoms. Cerebral small vessel disease usually gets worse over time, and in some people can cause a decline in memory and thinking. If this decline gets severe enough to affect a person's ability to manage their daily activities independently, then it is described as a type of vascular dementia. We know that blood‐thinning medications such as aspirin can prevent stroke. We wanted to know whether blood‐thinning medications might also prevent the decline in memory and thinking that is seen in cerebral small vessel disease.
Review question
Are blood‐thinning medications effective and safe in preventing the decline in memory and thinking in people with cerebral small vessel disease?
What we did
We searched the medical literature up to 21 July 2021 looking for studies that compared blood‐thinning medications given over at least 24 weeks to a comparator, which could have been either usual care or a placebo (dummy) tablet. To make the comparison fair, the studies had to assign people randomly to blood‐thinning medications or the comparator treatment. We were interested in the effects on participants' performance in memory and thinking tests, their ability to look after themselves, their risk of developing dementia and stroke, and side effects (especially from bleeding). Because the studies were so different from each other in terms of the type of participants, medications and assessments, we were unable to combine the results in analyses. Rather, we described the results of individual studies and assessed how confident we were in their findings.
What we found
We included three studies with 3384 participants. These studies were very different in terms of the participants (some with and some without stroke), the medications studied (single and combinations of different blood‐thinners), and how the effects on memory and thinking were measured (different tests used for assessment). No trial consistently demonstrated an improvement in performance in memory and thinking tests or in daily activities. No trial assessed for a new diagnosis of dementia. There was suggestion of blood‐thinning medications possibly causing an increased risk of bleeding, including gastrointestinal bleeding, but the numbers were too small to be certain that this was not just a chance difference. Overall, we considered that the quality of the evidence was poor for answering our review question regarding memory and thinking. Much of the information we needed was not reported. Two of the three studies were small, meaning that there was uncertainty around their results. In the only study that reported any benefit from blood‐thinning medication, different measures of memory and thinking did not all agree with each other. Lastly, where there was an improvement in memory and thinking, the size of this improvement may have been too small to make a noticeable difference to the individual in reality.
Conclusions
We found no convincing evidence that taking blood‐thinning medications is beneficial for memory and thinking in people with cerebral small vessel disease. However, the studies were very different from each other, and each one had limitations with regard to our review question.
Summary of findings
Summary of findings 1. Antiplatelet drug compared to placebo in mixed populations (with or without pre‐existing antiplatelet therapy) for the prevention of cognitive decline and dementia in people with cerebral small vessel disease and no dementia.
| Antiplatelet drug compared to placebo, in populations with mixed prevalence of antiplatelet drug use at baseline, for the prevention of cognitive decline and dementia in people with cerebral small vessel disease and no dementia | |||
| Patient or population: people with cerebral small vessel disease and no dementia either already on antiplatelet therapy or not Setting: outpatient services Intervention: adding antiplatelet therapy in populations where some participants may have been taking antiplatelet Comparison: placebo | |||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) |
| Change in cognitive function from baseline assessed with ADAS‐Cog, CIBIC‐plus, MMSE, CDR, CDR‐SB, | 1 trial reported a beneficial effect across 2 of 5 cognitive outcomes (ADAS‐Cog and CIBIC‐plus), but the size of benefit may be less than the minimal important clinical difference. | 280 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Incident dementia | No studies reported this outcome | — | — |
| Major bleeding (intracranial and extracranial) | 1 trial reported no difference between treatment groups for this outcome. | 280 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Functional ability | 1 trial reported no difference in functional anility between treatment groups | 280 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Stroke or transient ischaemic attack | 1 trial reported no difference in stroke or transient ischaemic attacks between treatment groups | 280 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Any adverse events (excluding major bleeding) | 1 study reported no difference in adverse events between treatment groups | 280 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Withdrawal from study medication | 1 trial reported an increase in medication withdrawal in those taking additional antiplatelets in comparison to those taking a placebo (OR for withdrawal from treatment 1.88, 95% CI 0.90 to 3.42) | 280 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ADAS‐Cog: Alzheimer's Disease Assessment Scale – Cognitive Subscale; ADL: activities of daily living; CDR‐SB: Clinical Dementia Rating scale Sum of Boxes; CI: confidence interval; MMSE: Mini‐Mental State Examination; OR: odds ratio; RCT: randomised controlled trial. | |||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||
aDowngraded one level because all participants had cognitive impairment at baseline, making it difficult to translate these findings to the general small‐vessel disease population. bDowngraded one level as it is arguable whether DL‐3‐n‐butylphthalide should technically be classified as an antithrombotic therapy. cDowngraded one level for imprecision as only one study contributed to this finding.
Summary of findings 2. Antiplatelet therapy compared to placebo for prevention of cognitive decline and dementia in people with cerebral small vessel disease and no dementia.
| Antiplatelet therapy compared to placebo in antiplatelet naive populations for prevention of cognitive decline and dementia in people with cerebral small vessel disease and no dementia | |||
| Patient or population: people with cerebral small vessel disease and no dementia not on antiplatelet therapy Setting: outpatient services Intervention: antiplatelet therapy Comparison: placebo | |||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) |
| Change in cognitive function from baseline assessed with: NPB, MMSE | 1 trial reported no difference between treatment groups. | 50 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Incident dementia | No studies reported this outcome | — | — |
| Major bleeding (intracranial and extracranial) | No studies reported this outcome | — | — |
| Functional ability | 1 trial reported no difference in activities of daily living between treatment groups. | 50 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Stroke or transient ischaemic attack | 1 trial reported no difference between treatment groups. | 50 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Any adverse events (excluding major bleeding) | 1 trial reported no difference between treatment groups. | 50 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Withdrawal from study medication | 1 trial reported slightly more dropout in the intervention group (33.3%) than in the placebo group (19.2%) | 50 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). MMSE: Mini‐Mental State Examination; NPB: Neuropsychological test Battery; RCT: randomised controlled trial. | |||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||
aDowngraded one level as there was no (clear) statement whether participants with dementia were actively excluded. bDowngraded one level due to serious risk of bias in included studies. cDowngraded one level due to imprecision.
Summary of findings 3. Dual antiplatelet therapy compared to single antiplatelet therapy for prevention of cognitive decline and dementia in people with cerebral small vessel disease and no dementia.
| Dual antiplatelet therapy compared to single antiplatelet therapy for prevention of cognitive decline and dementia in people with cerebral small vessel disease and no dementia | |||
| Patient or population: people with cerebral small vessel disease and no dementia Setting: outpatient services Intervention: dual antiplatelet therapy Comparison: single antiplatelet therapy | |||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) |
| Change in cognitive function from baseline assessed with CASI score | 1 trial reported no beneficial effect of additional antiplatelet treatment over placebo on cognitive functioning assessed with the CASI score. | 3020 (1 RCT) | ⊕⊕⊝⊝ Lowa,b |
| Incident dementia | No trials reported this outcome | — | — |
| Major bleeding (intracranial and extracranial) | 1 trial reported a difference in major haemorrhagic events (105/1517 participants with intervention vs 56/1503 participants with control; HR 1.97, 95% CI 1.41 to 2.71) | 3020 (1 RCT) | ⊕⊕⊝⊝ Lowa,b |
| Functional ability | No trials reported this outcome. | — | — |
| Stroke or transient ischaemic attack | 1 trial reported there was probably no effect of additional antiplatelet treatment on stroke or TIA | 3020 (1 RCT) | ⊕⊕⊝⊝ Lowa,b |
| Any adverse events (excluding major bleeding) | No trials reported this outcome. | — | — |
| Withdrawal from study medication | 1 trial reported an increase in medication withdrawal in those taking additional antiplatelets in comparison to those taking a placebo (30% with intervention vs 27% with control; P = 0.02). | 3020 (1 RCT) | ⊕⊕⊝⊝ Lowa,b |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CASI: Cognitive Abilities Screening Instrument; CI: confidence interval; HR: hazard ratio; RCT: randomised controlled trial. | |||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||
aDowngraded one level for imprecision as only one study contributed to this finding. bDowngraded one level for indirectness because most participants had mild cognitive impairment at baseline, making it difficult to translate these findings to the general small‐vessel disease population.
Background
Description of the condition
Dementia is a progressive condition in which acquired cognitive impairment is severe enough to affect a person's ability to manage everyday activities. Usually it occurs in later life and is caused by neurodegenerative conditions, of which the most common are Alzheimer's disease and cerebrovascular disease. Dementia is an international public health concern, affecting 35 million people worldwide (Prince 2013), with a global annual cost of over USD 600 billion (Wimo 2013). By 2050, it is estimated that the impact of dementia will exceed that of heart disease, cancer and stroke combined (World Alzheimer Report 2015). Currently, approved pharmacological treatments for dementia offer symptomatic benefit (Battle 2021; McShane 2019), but there is no proven drug intervention to prevent or reduce cognitive decline.
Cerebral small vessel disease (cSVD) is a dynamic, whole brain syndrome thought to result from pathology in the arterioles, capillaries and venules of the brain. cSVD may be an asymptomatic finding on neuroimaging or may present with a range of clinical manifestations, including clinical stroke, gait impairments, neuropsychiatric problems and frank dementia. The overall prevalence of asymptomatic small vessel ischaemia seen on brain imaging is high, up to 67% of older adults in one community‐based study (Del Brutto 2015). As cSVD is associated with hypertension, diabetes and other vascular risk factors, treatment of cSVD has tended to focus on modifying vascular risk (Wardlaw 2019). Following a lacunar stroke (a form of cSVD), antithrombotic therapy is used to prevent further stroke. Whether this antithrombotic therapy has any effect on the progression or manifestation of the underlying cSVD is unclear.
The pathological changes of cSVD can be visualised using magnetic resonance imaging (MRI) or computed tomography (CT) brain scanning. MRI is the preferred tool for assessing cSVD owing to its greater sensitivity to the essential neuroimaging features of cSVD (Norrving 2015). Classical features of cSVD include subcortical infarcts, lacunes, white matter hyperintensities, prominent perivascular spaces, cerebral microbleeds and atrophy (Arba 2018; Boutet 2016; Mok 2015).
cSVD lesions may be associated with all‐cause dementia, although the supporting evidence is not consistent (Mortamais 2013). The estimated proportion of dementia with contribution from cSVD ranges from 36% to 67% (Grau‐Olivares 2009). Imaging evidence of cSVD is often seen in vascular dementia but the process may also be important in the pathogenesis of other types of dementia. Although the pathogenesis of Alzheimer's disease remains incompletely understood (Jack 2010), there is increasing support for a potential vascular basis (Grammas 2011). Autopsy studies have demonstrated important interactions between cSVD and Alzheimer's pathology (Iadecola 2010), and cSVD risk factors such as diabetes and hypertension appear to be independent predictors of Alzheimer's disease (Akinyemi 2013). Among people with stroke of mild‐to‐moderate severity, MRI evidence of cSVD and medial temporal lobe atrophy (one of the imaging indicators of Alzheimer's pathology) are highly prevalent and can predict post‐stroke dementia at two years (Kwan 2016).
Many experts are already calling for improved vascular risk management for the primary prevention of dementia including Alzheimer's disease (Safouris 2015), yet the effectiveness of these strategies in altering the trajectory of dementia‐related pathologies and cognitive decline remains unclear. The following clinical scenario is a common one: an older adult has no evidence of cognitive impairment or only a minor cognitive complaint but is keen to reduce their risk of developing dementia in the future. They have cSVD on an MRI scan performed for another reason, for example headache. For this patient: should antithrombotic therapy be started to prevent future cognitive decline? In this review, we looked into the effectiveness of antithrombotic therapy for both symptomatic and asymptomatic cSVD for the prevention of (further) cognitive decline and dementia.
Description of the intervention
Antithrombotic therapy reduces the formation of thrombus through acting on one or more aspect of the thrombotic cascade. Based on their mode of action, antithrombotic agents are categorised as antiplatelets, anticoagulants and fibrinolytic agents. In this review, we do not consider fibrinolytics as they tend to be used in the acute setting only and would not be used as a longer‐term primary or secondary preventive intervention.
Antiplatelet agents include: cyclo‐oxygenase inhibitors (e.g. aspirin); inhibitors of phosphodiesterases III and V and inhibitors of adenosine uptake by red cells (e.g. cilostazol, dipyridamole); blockade of the platelet ADP P2Y12 receptor (e.g. clopidogrel, prasugrel, ticagrelor); blockade of glycoprotein IIb/IIIa receptors (e.g. abciximab); and increasing nitric oxide levels (e.g. triflusal) (Geeganage 2010). Oral anticoagulants include traditional vitamin K antagonists (e.g. warfarin) and direct oral anticoagulants (DOACs). DOACs include agents that inhibit activated factor Xa (e.g. apixaban, rivaroxaban and edoxaban) or thrombin (e.g. dabigatran) (Lip 2015).
How the intervention might work
Antiplatelet agents are the usual treatment for secondary stroke prevention after an ischaemic stroke (ATC 2002), including for lacunar (subcortical) stroke. Different regimens have been evaluated in this context, including both single agents and combinations of agents (Ishida 2014). Increasing potency of antiplatelet can often be accompanied by increasing risk of bleeding. Thus the use of antiplatelet agents in people with cSVD needs to balance the potential benefit against risks (Mok 2015).
Oral anticoagulants are the standard treatment for the primary and secondary prevention of stroke in high‐risk patients with atrial fibrillation or certain other cardioembolic stroke aetiologies (Cameron 2014). In this review, we also included participants with cardioembolic stroke so long as they had concomitant cSVD, as we hypothesised that the pathophysiological mechanism for cognitive decline is comparable for this group.
Since antithrombotic agents have demonstrated efficacy in the prevention of symptomatic ischaemic stroke, it seems plausible that they might also prevent the asymptomatic (silent) infarcts that are thought to be part of cSVD. We hypothesised that this could in turn prevent the clinical manifestations of cSVD including cognitive decline.
Why it is important to do this review
There is currently no evidence‐based or licensed drug treatment for the prevention of cognitive decline and dementia. If antithrombotic agents could prevent or delay cognitive impairment associated with cSVD, this could be an inexpensive intervention for the many people living with this condition.
Objectives
To assess the effects of antithrombotic therapy for prevention of cognitive decline in people with small vessel disease on neuroimaging but without dementia.
Methods
Criteria for considering studies for this review
Types of studies
For this review, we considered only randomised controlled trials (RCTs).
Types of participants
To be eligible for inclusion, participants had to have evidence of cSVD on neuroimaging but no dementia, using the following definitions.
Presence of cSVD on neuroimaging (CT or MRI). Where possible, we used the definitions of the STandards for ReportIng Vascular changes on nEuroimaging (STRIVE) guidance as a reference (Wardlaw 2013), but a degree of flexibility of interpretation was employed and noted. Features of cSVD are often measured on ordinal scales; we included those studies where the degree of cSVD change was at least 'mild' (e.g. greater than 1 on the Fazekas scale in assessing white matter hyperintensity). In studies of mixed populations, at least 75% of the participants had to have imaging evidence of cSVD.
Absence of dementia of any cause. Where possible, we aimed to include studies using internationally accepted diagnostic criteria for dementia, however a degree of flexibility was needed because of heterogeneity of the operationalisation of this exclusion criterion in the included studies. Therefore, we also accepted cognitive testing that was plausible to detect incipient or existing dementia.
Participants with or without a history of symptomatic stroke were eligible for inclusion, as long as they met the above criteria for cSVD on neuroimaging and no dementia.
Types of interventions
Antithrombotic therapy included the following three treatment regimens.
Antiplatelet agents (as monotherapy or combination therapy).
Oral anticoagulants (vitamin K antagonists or DOACs).
Antiplatelet agent(s) combined with oral anticoagulant(s).
We considered all studies that compared antithrombotic therapy (administered for at least six months) to no antithrombotic therapy (either placebo or treatment as usual), or that compared different antithrombotic therapy regimens. We did not specify any restrictions based on dose, frequency or method of administration. We opted for a minimal intervention duration of 24 weeks as cognitive decline due to cSVD is a slow process and little effect can be expected on cognitive decline for shorter intervention durations.
Types of outcome measures
We included the following primary and secondary outcomes.
Primary outcomes
Change in cognitive function between baseline and final follow‐up using validated cognitive assessment measures.
Incident dementia of any cause as defined by internationally accepted diagnostic criteria.
Bleeding, including new intracranial haemorrhagic events (intracerebral, subdural, subarachnoid and extradural) or major extracranial haemorrhagic events.
Secondary outcomes
Functional outcome using validated functional assessment measures.
Incident ischaemic stroke or transient ischaemic attack.
Death.
Adverse events (excluding bleeding, as this is already reported as primary outcome).
Withdrawal from the allocated treatment within the scheduled follow‐up period.
New cerebral microbleeds on repeat neuroimaging.
Incident mild cognitive impairment (MCI).
Search methods for identification of studies
We used the following search method to identify studies.
Electronic searches
We searched ALOIS (alois.medsci.ox.ac.uk) – the Cochrane Dementia and Cognitive Improvement Review Group's Specialised Register, and the Cochrane Stroke Group's Specialised Register.
ALOIS is maintained by the Review Group's Information Specialist and contains dementia and cognitive improvement studies identified from:
monthly searches of several major healthcare databases: MEDLINE, Embase, CINAHL, PsycINFO and Lilacs;
monthly searches of the trial registers: the World Health Organization (WHO) International Clinical Trials Registry Platform (which covers ClinicalTrials.gov, ISRCTN, the Chinese Clinical Trials Register, the German Clinical Trials Register, the Iranian Registry of Clinical Trials, and the Netherlands National Trials Register, plus others) and ClinicalTrials.gov;
quarterly search of the Cochrane Library's Central Register of Controlled Trials (CENTRAL);
six‐monthly searches of several grey literature sources from ISI Web of Science Core Collection.
Details of the search strategies used for the retrieval of reports of trials from the healthcare databases, CENTRAL and conference proceedings can be viewed in the 'Methods used in reviews' section within the editorial information about the Dementia and Cognitive Improvement Group (dementia.cochrane.org/resources-review-authors). We performed additional searches in many of the sources listed above to ensure that the search for the review was as up‐to‐date and comprehensive as possible.
We recognised that potentially relevant data may be available through subgroup analysis of stroke trials, for example a study of antiplatelet in stroke that had cognitive outcome data and where a subgroup of participant with lacunar stroke (a form of cSVD) could be derived. We worked with the Cochrane Stroke Group and handsearched all antithrombotic trials in their Centralised Register. Our search strategies used are described in Appendix 1. The most recent search was carried out on 21 July 2021.
Searching other resources
We checked the reference lists of articles retrieved from the above searches. For included studies, we retrieved additionally published subpapers where appropriate, to ensure a comprehensive data extraction. Where clarification of information was needed, we attempted to contact the investigators of the relevant studies.
Data collection and analysis
We used the following method for data collection and data analysis.
Selection of studies
A minimum of two review authors independently screened all titles and abstracts of publications identified by the searches to assess their eligibility. Publications that clearly did not meet the inclusion criteria were excluded at this stage. We retrieved the full‐text versions of potentially relevant studies. A minimum of two review authors independently assessed each full‐text study according to the prespecified selection criteria. Disagreements were resolved by discussion.
Data extraction and management
A minimum of two authors independently extracted data from the published reports. Disagreements were resolved by discussion.
Assessment of risk of bias in included studies
A minimum of two review authors independently assessed risk of bias for each included study. We used the RoB 1 tool as described in the original Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This RoB assessment considered five domains: selection bias, performance bias, attrition bias, detection bias and reporting bias. Domains were assessed for eligible papers and we classified them as low or high risk of bias. Where there was insufficient detail in a study to assess the risk, we reported it as unclear.
Measures of treatment effect
For dichotomous data, we expressed relative treatment effects as odds ratio (OR) or risk ratios (RR) with 95% confidence intervals (CI). For continuous data, we used mean differences (MD) with 95% CIs.
Unit of analysis issues
The participant was the unit of analysis. Where studies reported outcomes at more than one time point, we used the outcome data from the end of the intervention period where possible.
Dealing with missing data
We reported the amount of missing outcome data in each trial. When reporting trialists' own analyses, we favoured intention‐to‐treat analyses and reported any imputation methods.
Assessment of heterogeneity
Assessment of heterogeneity was performed in accordance with the guidance in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We assessed clinical heterogeneity and considered the characteristics of the participants, how cSVD was diagnosed, the type of antithrombotic agents tested, and how the outcomes were assessed and reported.
Assessment of reporting biases
If the trial data had allowed, we would have used visual inspection of funnel plot analyses to assess for potential reporting biases. However, for this review, there were insufficient studies to allow for this analysis.
Data synthesis
Due to the small number of eligible studies and the significant heterogeneity between them, we were unable to conduct any meta‐analyses to derive summary treatment effects. We instead described the individual studies using a narrative approach and created a summary table detailing the potential class effects of antithrombotic therapy.
Subgroup analysis and investigation of heterogeneity
We did not conduct any subgroup analyses.
Sensitivity analysis
We did not conduct any sensitivity analyses.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of the supporting evidence behind each estimate of treatment effect (Schünemann 2008). We presented key findings of the review including a summary of the amount of data, the magnitude of the effect size and the overall certainty of the evidence, in summary of findings tables, created using GRADEpro software (GRADEpro GDT). We had preselected the following outcomes for inclusion in the summary of findings tables.
Change in cognitive function from baseline.
Incident dementia.
Major bleeding events.
Functional outcome.
Ischaemic stroke or transient ischaemic attack.
Adverse events (excluding bleeding).
Withdrawal from the allocated treatment.
Results
Description of studies
See Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, and Characteristics of ongoing studies tables for details of the studies considered for this review.
Results of the search
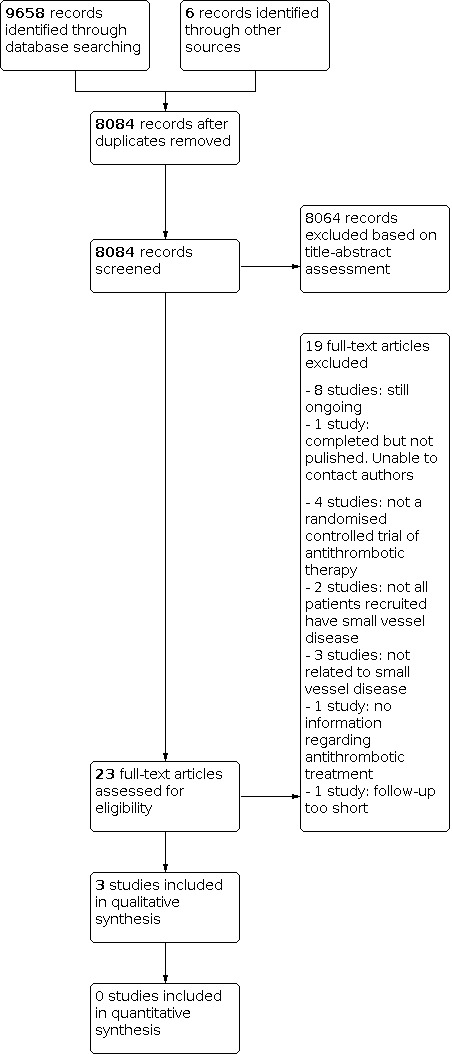
The Information Specialists of the Cochrane Dementia and Cognitive Improvement Group performed electronic searches on 7 July 2016, 4 May 2017, 22 June 2018, 6 June 2019, 16 September 2020 and 21 July 2021. In total, we retrieved 9658 results through database searching and six results through other sources. After deduplication, there remained 8084 records, 8064 of which we excluded at the title and abstract stage. We downloaded the full‐texts or sought further information for 23 articles to assess their eligibility. See Figure 1 and Appendix 1 for more details.
1.
The review includes three studies (Jia 2016; Maestrini SILENCE 2018; Pearce SPS3 2014). We excluded 11 studies because they did not meet our inclusion criteria (AVERROES‐MRI assessment study; COMPASS MRI; Douiri 2013; Han 2013; Jacobs 2015; Kwok 2015; Kwon 2016; LACI‐1; Shinod‐Tagawa 2002; Xu 2020; Zhang 2014). There are eight ongoing studies (ASPREE‐NEURO; CAF; CHALLENGE; ChiCTR‐TCS‐14005054; LACI‐2; NCT01932203; PICASSO‐Cog; Reid ENVIS‐ion 2012) and one study is awaiting classification as we were unable to contact the author for the necessary details (CAVAD). Details on these ongoing studies is reported in Ongoing studies. No studies that looked at white matter hyperintensity or lacunar infarctions only were identified.
See Figure 1 PRISMA Study flow diagram for the summary of our selection process.
Included studies
We included three RCTs (3384 participants) (Jia 2016; Maestrini SILENCE 2018; Pearce SPS3 2014).
Study design
Jia 2016 was a randomised, double‐blind, placebo‐controlled trial that assessed the effects of DL‐3‐n‐butylphthalide in participants with vascular cognitive impairment without dementia, caused by subcortical ischaemic cSVD. DL‐3‐n‐butylphthalide has multimodal effects and while not classically considered an antithrombotic agent, one of its actions is inhibition of platelet aggregation.The intervention period was 24 weeks and the follow‐up duration six months.
The SILENCE trial was a randomised, placebo‐controlled trial that assessed aspirin in a population with silent brain infarcts (Maestrini SILENCE 2018). A large proportion of 33 participants (40%) refused randomisation and were followed up as an observational cohort. The intervention and follow‐up duration was four years.
The Secondary Prevention of Small Subcortical Strokes (SPS3) trial was a randomised, placebo‐controlled, multicentre clinical trial that studied the effects of dual (aspirin plus clopidogrel) versus single (aspirin alone) antiplatelet therapy (Pearce SPS3 2014). The intervention duration was three years and the median follow‐up for cognitive outcomes was 3.4 years.
Participants
Jia 2016 assessed 563 people at 15 Chinese academic medical centres and recruited 280 participants aged 50 to 70 years who had a diagnosis of subcortical vascular cognitive impairment with cSVD but without dementia. Of these participants, 76% had a history of stroke at baseline. Participants had subjective cognitive complaints or evidence of cognitive decline from an informant, but not sufficient to warrant a diagnosis of dementia. Dementia at baseline was ruled out according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM‐IV), with Clinical Dementia Rating (CDR) 0.5 or greater on at least one domain and global score of 0.5 or less; a Mini‐Mental State Examination (MMSE) score of 20 or greater (with primary school education) or 24 or greater (with junior school education or above); and normal or slightly impaired activities of daily living (ADL) as defined by a total score of 1.5 or less on the three functional CDR domains (home and hobbies, community affairs and personal care). MRI inclusion criteria were evidence of cSVD, no cortical stroke and no medial temporal lobe atrophy. All participants were Han Chinese.
The SILENCE RCT recruited people from Italian neurology clinics on the basis of MRI evidence of silent brain infarcts, with most included participants having infarcts in keeping with our cSVD definition (Maestrini SILENCE 2018). The study assessed 350 participants of whom 50 were enrolled in the RCT (aspirin group 24; placebo group 26) and 33 in a non‐randomised follow‐up. In this review, we include only data from the 50 randomised participants.
The SPS3 study recruited 3020 participants aged 30 years or above from 81 clinical centres across seven different countries in the North and South Americas (Pearce SPS3 2014). People who had recent symptomatic small subcortical stroke (within six months) with MRI confirmation were eligible for this trial. This study differed from Jia 2016 and Maestrini SILENCE 2018 because it included participants with acute SVD. Of the 3020 recruited participants, 2916 had baseline assessment using the Cognitive Abilities Screening Instrument (CASI) and were included in the cognitive substudy. The study reported 26% of participants with incomplete testing (either left the study early or did not complete cognitive testing at their last follow‐up). Compared to those with complete data, they were more educated and more likely to have MCI at study entry. Participants were excluded if they had an MMSE score less than 24 points at baseline.
Intervention
Participants in Jia 2016 were randomly assigned to receive either DL‐3‐n‐butylphthalide capsule or placebo, taken orally three times daily for six months. The number of unused capsules were counted in the medicine bottles to assess drug compliance. Concomitant aspirin was used in 61.4% of the DL‐3‐n‐butylphthalide group and 65.7% of the placebo group.
Participants in Maestrini SILENCE 2018 were randomly assigned to receive either enteric‐coated aspirin 100 mg daily or placebo with identical appearance.
Participants in Pearce SPS3 2014 were randomly assigned to receive either enteric‐coated aspirin 325 mg daily plus clopidogrel 75 mg daily or enteric‐coated aspirin 325 mg daily plus matching placebo. Compliance was measured by tablet counts, and follow‐up was five years.
Outcome measures
The primary outcomes in Jia 2016 included Alzheimer's Disease Assessment Scale – Cognitive subscale (ADAS‐Cog; a 12‐item global cognitive score ranging from 0 (best) to 70 (worst)); and Clinician Interview‐Based Impression of Change‐Plus Caregiver Input (CIBIC‐plus; a global assessment of change based on a semi‐structured, patient/caregiver interview, with scores ranging from 1 to 7, where 1 is "very much improved", 4 is "no change", and 7 is "very much worse"). Secondary outcomes were MMSE (range 30 with higher scores indicates better performance), Clinical Dementia Rating (CDR) global score (range 0 = no impairment to 3 = severe impairment), CDR‐sum of boxes (CDR‐SB, range 0 to 18, with higher scores representing greater severity of cognitive and functional impairment), Neuropsychiatric Inventory (NPI, a composite symptom domain score ranging from 0 = absence of behavioural symptoms to 144 = maximum severity of behavioural symptoms), Chinese Activities of Daily Living (ADL; range 20–80, with higher scores indicating worse functioning) and adverse events. Assessments were at baseline, week 12 and week 24.
The primary outcome in Maestrini SILENCE 2018 was a composite of clinical and radiological stroke events. Secondary outcomes included change in cognition using a multidomain neuropsychological test battery and the MMSE, an unspecified ADL measure and adverse events. Assessments were performed annually over four years of follow‐up.
The primary outcomes in Pearce SPS3 2014 were recurrent stroke and bleeding. Cognitive function was a secondary outcome as measured by CASI; a global measure of cognition assessing attention, concentration, orientation, short‐term memory, long‐term memory, language abilities, visual construction, list‐generating fluency, abstraction and judgement, with scores of 0 to 100, with higher scores indicating better performance. The CASI assessment was performed annually during five years of follow‐up, and participants were only included in the cognitive substudy if they had at least one year of follow‐up. Incident MCI was recorded. MCI (definition derived in posthoc analysis) was defined psychometrically at entry and annually on the basis of test scores as no cognitive impairment, MCI (single amnestic), MCI (multidomain) and MCI (non‐amnestic). For a full description of MCI assessment see Characteristics of included studies table.
Excluded studies
We excluded 12 studies as they did not meet our predefined inclusion criteria. For the full details of the reasons for exclusion, see Characteristics of excluded studies table. The most common reasons for exclusion were using a non‐randomised controlled trial design (Douiri 2013; Jacobs 2015; Kwok 2015; Zhang 2014), having a mixed population with no or too few participants with cSVD (ASPREE‐NEURO; AVERROES‐MRI assessment study; COMPASS MRI), or having no outcomes that were relevant to this review (Han 2013; Shinod‐Tagawa 2002; Xu 2020).
Risk of bias in included studies
The quality of included studies was variable. See the risk of bias in the Characteristics of included studies table, Figure 2, and Figure 3 for full details.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Allocation
Both Pearce SPS3 2014 and Jia 2016 were at low risk of selection bias. We judged Maestrini SILENCE 2018 at unclear risk of bias, as we could not be sure how the possibility to combined randomised and non‐randomised trial design had influenced the allocation of participants.
Blinding
We considered Jia 2016, Maestrini SILENCE 2018, and Pearce SPS3 2014 at low risk of performance and detection bias. Studies were described as double‐blind with matching placebo. Participants, investigators and outcome assessors were masked to the treatment allocation and were unable to preview the randomised assignments.
Incomplete outcome data
There was substantial attrition in both Maestrini SILENCE 2018 and Pearce SPS3 2014. It is possible that missing follow‐up data could have influenced the outcomes of interest, that is, those with cognitive or functional decline might be more likely to drop out of the full follow‐up period. Jia 2016 was at low risk of attrition bias.
Selective reporting
We judged Jia 2016 at possible risk of reporting bias, as the protocol was retrospectively registered, the projected sample size did not match the recruitment as proposed by the authors, and several differing outcomes were labelled as "primary outcomes" in their protocol. We also judged Maestrini SILENCE 2018 at possible risk of reporting bias, as the trial was prematurely terminated and the protocol was no longer available on the protocol repository.
Other potential sources of bias
The study medication used in Jia 2016 was donated by Shijiazhuang Pharmaceutical Group Company, but the company was reported as having no other role in the study. The discussion section of Jia 2016 stated that they had underestimated their sample size due to an overestimation of the drug effect at the clinical trial planning stage. We considered that these two issues posed an unclear risk of other biases. Maestrini SILENCE 2018 and Pearce SPS3 2014 were at low risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3
As the studies differed in their included participants, interventions and outcomes, we decided that a quantitative meta‐analysis was inappropriate. Therefore, we described the three included studies in turn, assessing the strength of evidence at study level, and describing the relevant quantitative data in Table 4, Table 5, and Table 6, and present a narrative summary of the evidence in Summary of main results.
1. Results of Jia 2016 (efficacy outcomes in intention‐to‐treat population at week 24).
| Psychometric scores | Adjusted mean change from baseline | Difference in adjusted mean (95% CI) | |
|
DL‐3‐n‐butylphthalide (n = 140) |
Placebo (n = 140) |
||
| ADAS‐Cog | −2.46 (SE 0.35) | −1.39 (SE 0.35) | −1.07 (−2.02 to −0.12) |
| CIBIC‐plus | 3.24 (SE 0.07) | 3.53 (SE 0.07) | −0.29 (−0.48 to −0.10) |
| MMSE | 1.51 (SE 0.19) | 1.26 (SE 0.18) | 0.26 (−0.25 to 0.76) |
| CDR | −0.05 (SE 0.01) | −0.02 (SE 0.01) | −0.02 (−0.06 to 0.02) |
| CDR‐SB | −0.03 (SE 0.08) | −0.07 (SE 0.07) | 0.04 (−0.16 to 0.24) |
| ADL | −0.62 (SE 0.33) | −0.80 (SE 0.33) | 0.18 (−0.70 to 1.07) |
| NPI | −0.13 (SE 0.17) | −0.43 (SE 0.17) | 0.29 (−0.15 to 0.74) |
Results table extracted from Table 2, Jia 2016. The adjustments made to the mean were not clearly stated in the publication. ADAS‐Cog: 12‐item Alzheimer's Disease Assessment Scale‐Cognitive subscale; ADL: activities of daily living; CDR: Clinical Dementia Rating; CDR‐SB: Clinical Dementia Rating scale Sum of Boxes; CI: confidence interval; CIBIC‐plus: Clinician's Interview‐Based Impression of Change‐Plus Caregiver Input; MMSE: Mini‐Mental State Examination; n: number of participants; NPI: Neuropsychiatric Inventory; SE: standard error.
2. Results of SPS3 2014 (mean Cognitive Abilities Screening Instrument (CASI) z‐score over time by assigned antiplatelet treatment).
| Time since baseline assessment (years) | Aspirin + clopidogrel | Aspirin + placebo | ||||
| n | Mean | SD | n | Mean | SD | |
| 0 | 1468 | −0.58 | 1.38 | 1448 | −0.61 | 1.48 |
| 1 | 1242 | −0.38 | 1.28 | 1230 | −0.42 | 1.43 |
| 2 | 974 | −0.31 | 1.28 | 994 | −0.39 | 1.37 |
| 3 | 752 | −0.28 | 1.32 | 769 | −0.39 | 1.42 |
| 4 | 559 | −0.27 | 1.35 | 576 | −0.33 | 1.45 |
| 5 | 392 | −0.29 | 1.37 | 411 | −0.43 | 1.60 |
Results table extracted from Pearce SPS3 2014. Higher score indicates better performance. n: number of participants; SD: standard deviation.
3. Results of SILENCE 2018 (efficacy outcomes of the randomised participants).
| Outcome |
Aspirin (n = 24) |
Placebo (n = 26) |
| MMSE (median) | 29 (IQR 27–30) | 29 (IQR 27–30) |
| IADL (median) | 8 (IQR 8–8) | 8 (IQR 8–8) |
| ADL (median) | 6 (IQR 6–6) | 6 (IQR 6–6) |
| Loss to follow‐up (n) | 8 (33.3%) | 5 (19.2%) |
| Adverse events (n) | 2 (8.3%) | 1 (3.8%) |
| Change in global cognitive score (mean) | −0.10 (SD 0.40) | −0.06 (SD 0.55) |
Unpublished data provided by the authors of Maestrini SILENCE 2018. ADL: activities of daily living; IADL: Instrumental Activities of Daily Living; IQR: interquartile range; MMSE: Mini‐Mental State Examination; n: number of participants; SD: standard deviation.
1. Change in cognitive function from baseline
Jia 2016: intention‐to‐treat (ITT) analysis involving 280 participants showed a difference in favour of DL‐3‐n‐butylphthalide using the ADAS‐Cog (adjusted MD −1.07, 95% CI −2.02 to −0.12), which equated to an effect size of 0.26 standard deviation. In the per‐protocol analysis, the observed MD was slightly larger at 1.21 points in the same direction. The mean CIBIC‐plus global score also showed a difference in favour of DL‐3‐n‐butylphthalide (drug‐placebo difference −0.29, 95% CI −0.48 to −0.10, P = 0.003), which equated to an effect size of 0.35 standard deviation. In the per‐protocol analysis, the observed MD was larger at −0.33 points (P < 0.001) in the same direction. There is no consensus on what is a clinically important difference in ADAS‐Cog or CIBIC‐plus for a trial examining cognitive decline, but differences of these magnitudes is unlikely to be of clinical relevance. There were no significant differences for MMSE, CDR global score or CDR‐SB between groups (Table 4). We considered this low‐certainty evidence, downgrading twice for indirectness as it is arguable whether DL‐3‐n‐butylphthalide should technically be classified as an antithrombotic therapy and because all participants had cognitive impairment at baseline, and for imprecision.
Maestrini SILENCE 2018 described various cognitive tests. There was no evidence of a difference between the aspirin and placebo groups in change in cognition, measured with a neuropsychological test battery, or in MMSE scores at the end of follow‐up (Table 6). We considered this very low‐certainty evidence, downgrading for risk of bias, indirectness and imprecision.
Pearce SPS3 2014: there was improvement in the CASI z‐score from baseline to each of the years one to five in both the aspirin plus clopidogrel and placebo groups, but the study reported that only the improvement from study entry to year one was statistically significant (MD 0.11, SD 0.84, P < 0.0001). The CASI z‐scores were not different between the two treatment groups over time (P = 0.858) (Pearce SPS3 2014). We considered this low‐certainty evidence, downgrading for indirectness as most participants had MCI at baseline, making it difficult to translate these findings to the general small‐vessel disease population, and for imprecision.
2. Incident dementia
No studies reported incident dementia.
3. Major bleeding events (intracranial and extracranial)
Jia 2016 reported two intracranial haemorrhagic events, one in each group (0.7% with DL‐3‐n‐butylphthalide group versus 0.7% with placebo; P = 1.00). We considered this very low‐certainty evidence, downgrading it twice for indirectness as it is arguable whether DL‐3‐n‐butylphthalide should technically be classified as an antithrombotic therapy and because most participants had cognitive impairment at baseline, and once for imprecision because only one study contributed to this finding. The study did not report extracranial haemorrhage.
Maestrini SILENCE 2018 did not report major bleeding events. They reported fatal and non‐fatal stroke rates, but these are not categorised as ischaemic or haemorrhagic. There were gastrointestinal adverse events, but it was unclear whether these related to bleeding.
Pearce SPS3 2014 reported both intracranial and extracranial haemorrhagic events. The overall risk of major haemorrhage was almost doubled with dual antiplatelet therapy (105 haemorrhages, 2.1% per year) compared with aspirin alone (56 haemorrhages, 1.1% per year) (HR 1.97, 95% CI 1.41 to 2.71; P < 0.001). Intracranial haemorrhagic events occurred in 15 participants assigned to aspirin and 22 participants assigned to aspirin plus clopidogrel (HR 1.52, 95% CI 0.79 to 2.93; P = 0.21). Extracranial haemorrhagic events occurred in 42 participants assigned to aspirin and 87 assigned to aspirin plus clopidogrel (HR 2.15, 95% CI 1.49 to 3.11; P < 0.001); 28 of these bleedings were gastrointestinal in the aspirin group and 58 in the aspirin plus clopidogrel group (HR 2.14, 95% CI 1.36 to 3.36; P < 0.001). There were four fatal haemorrhagic events in the aspirin group and nine in the aspirin plus clopidogrel group (HR 2.29, 95% CI 0.7 to 7.42; P = 0.17). All four fatal haemorrhages in the aspirin group were intracranial haemorrhage versus seven fatal intracranial haemorrhages in the aspirin plus clopidogrel group (HR 1.78, 95% CI 0.52 to 6.07; P = 0.36). The remaining two fatal haemorrhagic events in the aspirin plus clopidogrel group were extracranial. We considered this low‐certainty evidence, downgrading once for indirectness because most participants had MCI at baseline and once for imprecision because only one study contributed to this finding.
4. Functional outcome (activities of daily living)
Jia 2016: there was no evidence of a difference in ADL between DL‐3‐n‐butylphthalide and placebo groups (adjusted MD 0.18, 95% CI −0.70 to 1.07). It was unclear what the minimum clinically important difference would be for the ADL scale employed as it is not a commonly used measure. We considered this very low‐certainty evidence, downgrading twice for indirectness and once for imprecision.
Maestrini SILENCE 2018: there was no evidence of a difference in ADL between aspirin and placebo (Table 6). The ADL scale employed was not described. We considered this to be very low certainty evidence, downgrading it for risk of bias, indirectness and imprecision.
Pearce SPS3 2014 did not report functional outcome.
5. Incident ischaemic stroke or transient ischaemic attack
Jia 2016: reported five participants who experienced new ischaemic stroke: two (1.4%) in the DL‐3‐n‐butylphthalide group and three (2.1%) in the placebo group (P = 1.00). There was one TIA (0.7%) in the DL‐3‐n‐butylphthalide group versus none in the placebo group. We considered this very low‐certainty evidence, downgrading twice for indirectness and once for imprecision.
Maestrini SILENCE 2018 reported clinical stroke and TIA with no difference between groups. In the aspirin group, there was one stroke event (3%) and no TIA, while in the placebo group there were two strokes (4%) and two TIAs (2%). We considered this very low‐certainty evidence, downgrading once each for risk of bias, indirectness and imprecision.
Pearce SPS3 2014 reported both ischaemic stroke and TIA. In total, 124 participants in the aspirin group versus 100 participants in the aspirin plus clopidogrel group had ischaemic stroke (HR 0.82, 95% CI 0.63 to 1.09; P = 0.13); while 39 participants in the aspirin group versus 28 in the aspirin plus clopidogrel group had TIA (HR 0.73, 95% CI 0.45 to 1.18; P = 0.19). We considered this low‐certainty evidence, downgrading once for indirectness and once for imprecision.
6. Death
Jia 2016 reported four participants who died during the study: two (1.5%) in the DL‐3‐n‐butylphthalide group and two (1.5%) in the place group (P = 1.00).
Maestrini SILENCE 2018 reported two (6%) cases of fatal myocardial infarction in the aspirin group and one (2%) event of fatal myocardial infarction in the placebo group. There were no other deaths reported.
Pearce SPS3 2014 reported 78 deaths in the aspirin group versus 113 deaths in the aspirin plus clopidogrel group (HR 1.5, 95% CI 1.1 to 2.0; P = 0.004). There were four fatal haemorrhagic events in the aspirin group and nine fatal haemorrhage events in the aspirin plus clopidogrel group (HR 2.29, 95% CI 0.7 to 7.42; P = 0.17).
7. Any adverse events (excluding bleeding)
Jia 2016: adverse events were mostly mild to moderate in severity. The overall adverse event rate was 21% in the DL‐3‐n‐butylphthalide group versus 14% in the placebo group (P = 0.08). Adverse events were deemed possibly or probably related to the study drug in nine participants: five (3.6%) in the DL‐3‐n‐butylphthalide group and four (2.9%) in the placebo group (P = 1.00). We considered this very low‐certainty evidence, downgrading twice for indirectness and once for imprecision.
Maestrini SILENCE 2018 reported any adverse event, including two events (8.3%) in the aspirin group and one event (3.8%) in the placebo group. We considered this very low‐certainty evidence, downgrading once each for risk of bias, indirectness and imprecision.
Pearce SPS3 2014 did not report any adverse event (excluding bleeding).
8. Withdrawal from the allocated treatment (excluding death)
Jia 2016 reported 33/280 participants discontinued the allocated treatment: seven participants withdrew consent (four from the DL‐3‐n‐butylphthalide group versus three from the placebo group); 18 participants were lost to follow‐up (10 from the DL‐3‐n‐butylphthalide group versus eight from the placebo group); three participants withdrew from the treatment due to possibly drug‐related gastrointestinal reactions (all from the DL‐3‐n‐butylphthalide group); and five participants withdrew due to worsened comorbidities (four from the DL‐3‐n‐butylphthalide group versus one from the placebo group). The OR for withdrawal from treatment was 1.88 favouring placebo (95% CI 0.90 to 3.42). We considered this very low‐certainty evidence, downgrading twice for indirectness and once for imprecision.
Maestrini SILENCE 2018 reported numbers completing follow‐up as 16 (66.7%) in the aspirin group and 21 (80.8%) in the control group. We considered this very low‐certainty evidence, downgrading once each for risk of bias, indirectness and imprecision.
Pearce SPS3 2014 reported mean rate of adherence to the assigned antiplatelet regimen was 94%. Permanent discontinuation of the assigned antiplatelet therapy occurred in 30% of participants receiving aspirin plus clopidogrel and 27% of those receiving aspirin (P = 0.02). We considered this low‐certainty evidence, downgrading once for indirectness and once for imprecision.
9. New cerebral microbleeds on neuroimaging
No trial reported new cerebral microbleeds on neuroimaging.
10. Incident mild cognitive impairment
Jia 2016: not applicable as all participants had cognitive impairment at baseline.
Maestrini SILENCE 2018 did not report incident MCI.
Pearce SPS3 2014 reported the incidence of MCI. At study entry, 1303 (45%) participants already fulfilled a diagnosis of MCI. Of the remaining 1413 participants without MCI at study entry, 376 (27%) participants developed MCI and there was no difference between groups (annual incidence 9.7% (189 events in 721 participants over a mean of 2.7 years of follow‐up) in the aspirin plus clopidogrel group versus 9.9% (187 events in 692 participants over a mean of 2.7 years of follow‐up) in the aspirin plus placebo group (P = 0.704).
Discussion
The three included trials were too heterogeneous to allow quantitative meta‐analysis. We described each study as a narrative with corresponding tables describing the study results.
Summary of main results
We identified three studies that included 3384 participants in total and assessed the effects of antithrombotic therapy for the prevention of cognitive decline in people with cSVD on neuroimaging but without dementia (Jia 2016; Maestrini SILENCE 2018; Pearce SPS3 2014).
There was considerable heterogeneity across the studies in terms of population assessed, antithrombotic strategy studied and outcomes described. We considered it inappropriate to create quantitative summary estimates using these three very different studies. However, there were consistent findings across many of the outcomes of interest and this allowed us to offer a class effect summary of the evidence for a potent versus less potent antithrombotic approach in people living with cSVD.
Across the various measures of general cognition, incident cognitive syndromes (i.e. dementia and MCI) and ADL, there was no convincing evidence of a beneficial effect of antithrombotic therapy in addition to usual care. The single study that reported some potential improvement in cognitive function found inconsistent results with some cognitive outcomes suggesting benefit and others suggesting no effect. Even if we consider the positive cognitive outcomes from this trial in isolation, the size of effect was probably less than would be considered clinically meaningful. Based on the evidence from all three included studies, there is little support for a strategy of routinely using antithrombotic therapy to prevent cognitive decline associated with cSVD.
A signal of potential harm was suggested in the outcomes of bleeding (both intracranial and extracranial), adverse events and treatment discontinuation. This is a reminder that antithrombotic therapy is not a completely benign intervention and can be associated with risks of harm. However, there was also a signal, albeit not statistically significant, that a more potent antithrombotic strategy may reduce the risk of stroke, which is a common complication of cSVD. Recurrent stroke is a powerful risk factor for cognitive decline, so if antithrombotic therapy can reduce stroke incidence then, in theory at least, they could indirectly reduce the cognitive effects of further cerebrovascular events.
Overall completeness and applicability of evidence
The process of conducting this review highlighted general issues with research in the field of small vessel disease.
The first issue was with the definition of the population. Our interest was people who had neuroimaging markers of cSVD, but no evidence of dementia. We based our definition of neuroimaging cSVD on the STRIVE criteria where possible but majored on white matter disease and covert stroke lesions. Increasingly, other brain imaging lesions associated cSVD are recognised and these may serve as better biomarkers of cerebrovascular cognitive problems, for example enlarged perivascular spaces and certain patterns of atrophy (Arba 2018).
Our operationalisation of the neuroimaging of cSVD included any person with lacunar stroke. Baseline neuroimaging is mandated in stroke trials of antithrombotic therapy to exclude intracerebral haemorrhage. So, potentially any stroke trial of antithrombotic therapy that included cognitive outcomes could be eligible for our review. To ensure we did not miss relevant information, we complemented our primary search of the literature, which used a search strategy designed around cSVD and vascular cognitive impairment, with a second focussed search of all the antithrombotic therapy trials held within the Cochrane Stroke Group database. We found several studies that could have contributed data to our review if the results were presented for a subgroup restricted to lacunar stroke. Such subgroup analyses were not available in the primary studies and results were only presented in an aggregate format for all ischaemic stroke types. Requests to authors to share these data did not return data that we could have used.
Another issue with the population was around defining a minimum degree of cSVD change. Study populations with baseline neuroimaging were often mixed, with some participants showing evidence of a spectrum of cSVD and others showing none of the common features. We had to set a threshold for the proportion of baseline cSVD that we would accept and in doing so we had to exclude certain studies that could have been relevant to the broader question around antithrombotic therapy and progression of radiological and clinical features of cSVD. At the individual level, there are many markers of cSVD and these tend to increase with increasing age. There is then the issue of when are small vessel changes 'acceptable for age' and when do they become 'pathological'. There is no consensus on this issue, and many believe that all 'age‐related changes' are pathological, although there have been attempts to offer age‐related normative values (Smith 2017). Again, we had to set a threshold of a minimum of at least 'mild' cSVD, but we recognise that this is an arbitrary threshold with no agreed definition, and through this categorisation we may have excluded certain studies that could have been relevant to the broader issue of antithrombotic therapy and cognitive decline. Furthermore, we included both participants with recent lacunar infarctions (Pearce SPS3 2014) and with more chronic forms of SVD (Jia 2016; Maestrini SILENCE 2018). These populations are probably slightly different in risk profiles and secondary prevention, potentially mitigating the effect of the intervention. For our included studies, there was no effect of the intervention both for populations with acute and more chronic SVD.
As there are several antithrombotic agents used in vascular medicine, we were deliberately inclusive. All the included trials were of antiplatelet agents, with no eligible studies describing the effects of anticoagulants. Within the review remit, we included differing potency of drugs or combinations with one study assessing low‐dose aspirin, one study comparing dual antiplatelet therapy versus single antiplatelet therapy, and one study of a compound (DL‐3‐n‐butylphthalide) that some might argue does not primarily belong within the antithrombotic drug class.
Given the differing contexts of the studies, the comparator also differed between the studies and usual care could have included the routine use of an antithrombotic agent, for example in participants who were included on the basis of lacunar stroke. Thus, while our initial interest was the effect of antithrombotic compared to no antithrombotic, for many of the participants included in eligible studies the data described additional versus single antithrombotic.
The intervention and follow‐up durations were different between included studies (varying from 24 weeks to four years of intervention and six months to four years of follow‐up). Trials investigating preventive strategies for cognitive decline and dementia require long‐term surveillance of participants due to the slow progression and low incidence of the condition under study (Richard 2012). Similarly, trials with a short intervention duration might pick up changes in cognition that are not sustainable over time (Beishuizen 2016). Therefore, some caution is warranted when interpreting findings from studies with a relatively short intervention or follow‐up (or both) duration. Future trials should aim for long‐term follow‐up of cognitive decline or dementia and could potentially consider adding surrogate markers for cognitive decline and dementia (e.g. imaging markers or simple clinical (memory) test) as an interim outcome.
The decision to study a population free of dementia at baseline was taken because we anticipated that progression to frank dementia would be an important clinical outcome of relevant trials. In fact no trials reported useable data on incident dementia, although one study described incident MCI. Moreover, one study did not report how (or if) they formally excluded dementia, though this is highly likely as participants were able to give informed consent. Rather, the included studies reported a heterogeneous mix of cognitive assessment tools. This inconsistency in cognitive assessment methods is common to both dementia and stroke research.
The natural history and management of lacunar stroke, early‐stage vascular cognitive impairment and incidentally detected neuroimaging features of cSVD are very different. In retrospect, and for future studies, it may have been more useful to distinguish 'silent' or 'covert' cSVD (with no clinical stroke and no frank cognitive syndrome) from 'clinically apparent' cSVD presenting with a stroke.
Quality of the evidence
We could not perform meta‐analysis as the included trials were heterogeneous. Many of our prespecified key outcomes were not reported in the included trials, for example, no trial reported incident dementia. Moreover, the observed evidence was of very low to low certainty, meaning our confidence in the reported effect estimates is limited. The certainty of our evidence was compromised by several factors. Risk of bias was a major issue for one trial (Maestrini SILENCE 2018), while applicability to the study question was also an issue. Of the remaining trials, Pearce SPS3 2014 was a stroke secondary prevention trial and cognition was a secondary aim. Arguably Jia 2016 was the study closest to our original aim in terms of population and outcomes assessed, but the medication studied was not primarily tested as an antithrombotic therapy, although it does possess antithrombotic properties. Moreover, this study had relatively restricted age range (50 to 70 years), making it difficult to generalise these findings to the general population. Both Jia 2016 and Maestrini SILENCE 2018 had a small sample size and relatively short follow‐up for a cognitive prevention study, and this is reflected in the uncertainty around their results. Even the largest trial may not have been adequately powered for some of our efficacy and safety outcomes, for example, incident MCI and intracerebral bleeding (Pearce SPS3 2014).
Potential biases in the review process
To keep our review focussed, we operationalised our definitions of cSVD. This may have excluded some studies with potentially relevant data. The data did not allow for an assessment of publication bias. See Figure 2 and Figure 3 for full details.
Agreements and disagreements with other studies or reviews
Agreements with guidelines
The recently published European Stroke Organisation (ESO) guideline on covert cSVD gave a weak recommendation against using antithrombotic therapy such as aspirin for cognitive decline, but recognised that the quality of supporting evidence was weak (Wardlaw 2021). However, the ESO guideline did recommend people with covert cSVD and hypertension to have their blood pressure well controlled, and it emphasised that RCTs with specific clinical endpoints were a priority for covert cSVD. An accompanying expert consensus statement noted that antiplatelets should not be used unless there is another clinical indication as these drugs may be harmful, especially in older adults. While this guideline considered randomised and non‐randomised evidence and had a broader definition of cSVD, the conclusions are aligned with the findings of our review.
The Geriatric Neurology Group of the Chinese Society of Geriatrics published a clinical practice guideline on cognitive impairment in cSVD (Peng 2019). This guideline referred to Pearce SPS3 2014, but did not make any recommendations on antithrombotic therapy; it recognised that the evidence around pharmacological treatment of vascular risk factors for cSVD was weak.
The American Heart Association/American Stroke Association published guidelines on prevention of stroke in people with silent cerebrovascular disease. Their neuroimaging definition of silent cerebrovascular disease is similar to our review definition of cSVD. No formal recommendations were made around antithrombotic therapy due to the lack of suitable trials (Smith 2017).
Agreements with other studies
While we strived to ensure that we included all studies relevant to our review question, there were other studies that offered insights into antithrombotic therapy and vascular cognitive decline. The ASPREE (Aspirin in Reducing Events in the Elderly) study described the use of aspirin to prevent cardiovascular events, and physical and cognitive decline in older adults (McNeil 2018). Although baseline neuroimaging was not mandated in this study, it is possible that a proportion of the participants might have had a degree of cSVD changes. The primary results of ASPREE are aligned with the summary findings in this review, and aspirin did not appear to have any apparent benefit on cognitive or physical function, but was associated with increased harm.
There are studies that describe the effect of antithrombotic therapy on the progression of neuroradiological markers of cSVD. We found two trials of an antiplatelet agent, cilostazol. In one RCT, 89 participants with type II diabetes mellitus and no brain lesions on baseline MRI scans were randomised to cilostazol or placebo, and followed up for three years (Shinoda‐Tagawa 2002). The study found fewer silent infarcts in the cilostazol group. The LACI‐1 (LACunar Intervention‐1) RCT of 57 participants with recent lacunar stroke reported that 11 weeks of cilostazol reduced progression in white matter lesions compared to placebo (Blair 2019). While these data are interesting, the relationship between neuroimaging features of cSVD and clinical manifestations was unclear and so for our review, we did not include studies that only reported surrogate measures such as silent brain infarction.
Although we were unable to obtain individual participant data or subgroup data limited to cSVD, studies of antithrombotic therapy for stroke can still give some relevant information. The Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial showed no significant differences in cognitive outcomes between two antiplatelet regimens (aspirin plus extended‐release dipyridamole versus clopidogrel) (Diener 2008). The agent DL‐3‐n‐butylphthalide has also been studied in acute ischaemic stroke, where there was no difference in cognitive test scores. However, the sample size was small for a cognitive study (104 participants) and follow‐up was only for one month (Yan 2017).
Agreement with other reviews
In a systematic review and meta‐analysis looking at antithrombotic therapy following lacunar stroke (a form of cSVD), the authors described benefit of single antiplatelet versus placebo for prevention of recurrent stroke. However, there was no signal of superiority of one antithrombotic agent over another, and long‐term dual antiplatelet was associated with harm. The review did not examine cognitive outcomes (Kwok 2015).
One Cochrane Review describing aspirin for prevention of cognitive decline found few studies, but noted no clear signal of benefit and the potential for harmful adverse effects (Jordan 2020).
We found no primary studies or reviews examining oral anticoagulants in our population of interest. In one systematic review that examined the relationship between atrial fibrillation thromboprophylaxis and cognitive decline (Moffitt 2016), the authors found no definitive evidence of cognitive benefit or harm from anticoagulation over antiplatelet therapy. Since the publication of this review, one large observational cohort study of 3284 older (over 65 years) Chinese people with AF followed up for 3.6 years found that anticoagulation with warfarin was associated with a significantly lower risk of new‐onset dementia compared those with no therapy or aspirin, with an HR of 0.14 (95% CI 0.05 to 0.36; P < 0.001) (Wong 2020). Interestingly, in this study, people receiving warfarin with time in therapeutic range (TTR) of greater than 65% had a non‐significant trend towards a lower risk of dementia compared with those with TTR less than 65% (Wong 2020).
In one narrative review of cSVD, Mok 2015 noted the substantial risk of bleeding when antithrombotics were used. Given the theoretical reduced bleeding risk with certain antithrombotic classes, a recommendation was made to consider using cilostazol or triflusal (over aspirin) in people living with cSVD.
Authors' conclusions
Implications for practice.
There is insufficient evidence to support the routine use of antithrombotic therapy to prevent cognitive decline in people with small vessel disease on neuroimaging but without dementia. We identified only three studies reporting on our research question and their results were inconclusive. The overall evidence reported in this review was of very low to low certainty, meaning our confidence in the reported effect estimates is limited.
In this review, we considered cerebral small vessel disease (cSVD) as a single condition, but under this rubric is a spectrum of severity of neuroimaging and phenotypic features and people living with cSVD may have other potential indications for antithrombotics. At the individual patient level, a degree of risk stratification is required around antithrombotic prescription. Recommendations on antithrombotic therapy in practice cannot be made based on the findings of this review, as the studies were too heterogeneous in terms of populations (including both acute and chronic small vessel disease in both naïve and therapeutic populations) and interventions (including single and double antithrombotic therapy).
Implications for research.
Our review highlights unanswered questions and aspects of research methods that could be improved for future studies.
The available evidence on adverse effects, particularly bleeding, is a reminder that longer‐term administration of antithrombotics presents risks. Any potential long‐term cognitive or stroke benefit would need to be greater than the bleeding risk. Arguments around using antithrombotic agents that have lesser bleeding risk and may have beneficial effects on other aspects of vascular biology (e.g. cilostazol) are compelling but so far lack convincing clinical trial evidence.
While one could argue that large‐scale, long‐term follow‐up RCTs of antithrombotic therapy in cSVD are needed, given the associated bleeding risk and increasing evidence of no cognitive benefit of aspirin primary prevention, these trials may need more sophisticated risk stratification than presence/absence of cSVD change.
Novel antithrombotic agents with lower bleeding risk could have potential efficacy and we would support the calls for all future (cerebro) vascular trials to include cognitive outcomes.
The focus of our review is on cognition, but the clinical manifestations of cSVD are not restricted to cognitive decline. No cSVD trials assessed other aspects of the cSVD phenotype such as disordered gait, apathy, mood disturbance, continence, etc. It would be useful to find out the clinical features of greatest relevance to people living with cSVD and design trial outcomes around these.
Finally, the review process highlighted the difficulty of searching the published literature for studies of cSVD. Greater standardisation of terminology and indexing (as has been achieved for the neuroimaging aspects of cSVD) would aid future evidence synthesis. In the meantime, the development and validation of search syntax for cSVD would be a useful step.
What's new
| Date | Event | Description |
|---|---|---|
| 14 July 2022 | Amended | Minor typos corrected, author order changed. |
History
Protocol first published: Issue 7, 2016 Review first published: Issue 7, 2022
Acknowledgements
We are grateful to the Editors of the Cochrane Dementia and Cognitive Improvement Group and to peer reviewers Linxin Li and Fergus Doubal and consumer reviewer Cathie Hofstetter for their comments and advice in writing this review.
Appendices
Appendix 1. Sources searched and search strategies
|
Source |
Search strategy | Hits retrieved |
| CENTRAL (the Cochrane Library) crso.cochrane.org/SearchSimple.php [Date of most recent search: 21 July 2021] |
#0 ("micro‐bleed*" or microbleed*):TI,AB,KY #1 ("white matter" adj3 (ischemi* or ischaemi*)):TI,AB,KY #2 (Brain Ischemia):MH #3 Ischemia:MH #4 (White Matter/pathology):MH #5 (White Matter):MH #6 Leukoencephalopathies:MH #7 Leukoaraiosis:MH #8 Microhemorrhage*:TI,AB,KY #9 Microhaemorrhage*:TI,AB,KY #10 #0 OR #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 #11 antithrombo*:TI,AB,KY #12 Aspirin:MH #13 Aspirin:TI,AB,KY #14 dipyridamole*:TI,AB,KY #15 Dipyridamole:MH #16 clopidogrel*:TI,AB,KY #17 triflusal:TI,AB,KY #18 prasugrel:TI,AB,KY #19 ticagrelor:TI,AB,KY #20 ticlopidine:TI,AB,KY #21 cilostazol:TI,AB,KY #22 vorapaxar:TI,AB,KY #23 abciximab:TI,AB,KY #24 eptifibatide:TI,AB,KY #25 tirofiban:TI,AB,KY #26 terutroban:TI,AB,KY #27 disgren:TI,AB,KY #28 plavix:TI,AB,KY #29 effient:TI,AB,KY #30 brilinta:TI,AB,KY #31 ticlid:TI,AB,KY #32 pletal:TI,AB,KY #33 zontivity:TI,AB,KY #34 ReoPro:TI,AB,KY #35 integrilin:TI,AB,KY #36 aggrastat:TI,AB,KY #37 persantine:TI,AB,KY #38 ("acetylsalicylic acid"):TI,AB,KY #39 ("antiplatelet drug*"):TI,AB,KY #40 Thromboxanes:MH #41 Glycoproteins:MH #42 (Adenosine Diphosphate):MH #43 Anticoagulants:MH #44 Antithrombins:MH #45 ("vitamin k"):MH #46 phylloquinone:TI,AB,KY #47 phytomenadione:TI,AB,KY #48 phytonadione:TI,AB,KY #49 ("thrombin* inhibitor*"):TI,AB,KY #50 (Factor Xa):TI,AB,KY #51 (Fibrinolytic Agents):MH #52 dabigatran:MH #53 rivaroxaban:MH #54 apixaban:MH #55 coumarin*:MH #56 dabigatran:TI,AB,KY #57 rivaroxaban:TI,AB,KY #58 apixaban:TI,AB,KY #59 coumarin*:TI,AB,KY #60 warfarin:TI,AB,KY #61 Warfarin:MH #62 Heparin:MH #63 heparin:TI,AB,KY #64 phenprocoumon:TI,AB,KY #65 Acenocoumarol:TI,AB,KY #66 atromentin:TI,AB,KY #67 brodifacoum:TI,AB,KY #68 phenindione:TI,AB,KY #69 ("Xa inhibitor*"):TI,AB,KY #70 #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 #71 #10 AND #70 |
Jul 2016: 722 May 2017: 27 Jun 2018: 335 Jun 2019: 51 Sep 2020: 290 July 2021: 240 |
| MEDLINE In‐process and other non‐indexed citations and MEDLINE 1950‐present (OvidSP) [Date of most recent search: 21 July 2021] |
1 ("white matter" adj3 (ischemi* or ischaemi*)).ti,ab. 2 ("micro‐bleed*" or microbleed*).ti,ab. 3 *Brain Ischemia/ or *Ischemia/ or White Matter/pathology 4 Leukoencephalopathies/ or Leukoaraiosis/ 5 (Microhemorrhage* or Microhaemorrhage*).ti,ab. 6 or/1‐5 7 antithrombo*.ti,ab. 8 Aspirin/ 9 aspirin.ti,ab. 10 dipyridamole*.ti,ab. 11 Dipyridamole/ 12 clopidogrel*.ti,ab. 13 triflusal.ti,ab. 14 prasugrel.ti,ab. 15 ticagrelor.ti,ab. 16 ticlopidine.ti,ab. 17 cilostazol.ti,ab. 18 vorapaxar.ti,ab. 19 abciximab.ti,ab. 20 eptifibatide.ti,ab. 21 tirofiban.ti,ab. 22 terutroban.ti,ab. 23 disgren.ti,ab. 24 plavix.ti,ab. 25 effient.ti,ab. 26 brilinta.ti,ab. 27 ticlid.ti,ab. 28 pletal.ti,ab. 29 zontivity.ti,ab. 30 ReoPro.ti,ab. 31 integrilin.ti,ab. 32 aggrastat.ti,ab. 33 persantine.ti,ab. 34 "acetylsalicylic acid".ti,ab. 35 "antiplatelet drug*".ti,ab. 36 Thromboxanes/ 37 Glycoproteins/ 38 Adenosine Diphosphate/ 39 Anticoagulants/ 40 Antithrombins/ 41 "vitamin k".ti,ab. 42 phylloquinone.ti,ab. 43 phytomenadione.ti,ab. 44 phytonadione.ti,ab. 45 "thrombin* inhibitor*".ti,ab. 46 Factor Xa/ 47 Fibrinolytic Agents/ 48 dabigatran.ti,ab. 49 rivaroxaban.ti,ab. 50 apixaban.ti,ab. 51 coumarin*.ti,ab. 52 warfarin.ti,ab. 53 Warfarin/ 54 Heparin/ 55 heparin.ti,ab. 56 phenprocoumon.ti,ab. 57 Acenocoumarol.ti,ab. 58 atromentin.ti,ab. 59 brodifacoum.ti,ab. 60 phenindione.ti,ab. 61 "Xa inhibitor*".ti,ab. 62 or/7‐61 63 6 and 62 64 (randomized controlled trial or controlled clinical trial).pt. or randomized.tw. or placebo.tw. or clinical trials as topic.sh. or randomly.tw. or trial.ti. 65 animals/ not humans/ 66 64 not 65 67 63 and 66 |
Jul 2016: 794 May 2017: 83 Jun 2018: 121 Jun 2019: 84 Sep 2020: 146 July 2021: 128 |
| Embase (OvidSP) 1974 to 5 June 2019 [Date of most recent search: 21 July 2021] |
1 ("white matter" adj3 (ischemi* or ischaemi*)).ti,ab. 2 ("micro‐bleed*" or microbleed*).ti,ab. 3 *Brain Ischemia/ or *Ischemia/ or *white matter/ 4 Leukoencephalopathies/ or Leukoaraiosis/ 5 (Microhemorrhage* or Microhaemorrhage*).ti,ab. 6 or/1‐5 7 antithrombo*.ti,ab. 8 Aspirin/ 9 aspirin.ti,ab. 10 dipyridamole*.ti,ab. 11 Dipyridamole/ 12 clopidogrel*.ti,ab. 13 triflusal.ti,ab. 14 prasugrel.ti,ab. 15 ticagrelor.ti,ab. 16 ticlopidine.ti,ab. 17 cilostazol.ti,ab. 18 vorapaxar.ti,ab. 19 abciximab.ti,ab. 20 eptifibatide.ti,ab. 21 tirofiban.ti,ab. 22 terutroban.ti,ab. 23 disgren.ti,ab. 24 plavix.ti,ab. 25 effient.ti,ab. 26 brilinta.ti,ab. 27 ticlid.ti,ab. 28 pletal.ti,ab. 29 zontivity.ti,ab. 30 ReoPro.ti,ab. 31 integrilin.ti,ab. 32 aggrastat.ti,ab. 33 persantine.ti,ab. 34 "acetylsalicylic acid".ti,ab. 35 "antiplatelet drug*".ti,ab. 36 Thromboxanes/ 37 Glycoproteins/ 38 Adenosine Diphosphate/ 39 Anticoagulants/ 40 Antithrombins/ 41 "vitamin k".ti,ab. 42 phylloquinone.ti,ab. 43 phytomenadione.ti,ab. 44 phytonadione.ti,ab. 45 "thrombin* inhibitor*".ti,ab. 46 Factor Xa/ 47 Fibrinolytic Agents/ 48 dabigatran.ti,ab. 49 rivaroxaban.ti,ab. 50 apixaban.ti,ab. 51 coumarin*.ti,ab. 52 warfarin.ti,ab. 53 Warfarin/ 54 Heparin/ 55 heparin.ti,ab. 56 phenprocoumon.ti,ab. 57 Acenocoumarol.ti,ab. 58 atromentin.ti,ab. 59 brodifacoum.ti,ab. 60 phenindione.ti,ab. 61 "Xa inhibitor*".ti,ab. 62 or/7‐61 63 6 and 62 64 randomized controlled trial/ 65 controlled clinical trial/ 66 random$.ti,ab. 67 randomization/ 68 intermethod comparison/ 69 placebo.ti,ab. 70 (compare or compared or comparison).ti. 71 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 72 (open adj label).ti,ab. 73 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 74 double blind procedure/ 75 parallel group$1.ti,ab. 76 (crossover or cross over).ti,ab. 77 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 78 (assigned or allocated).ti,ab. 79 (controlled adj7 (study or design or trial)).ti,ab. 80 (volunteer or volunteers).ti,ab. 81 trial.ti. 82 or/64‐81 83 63 and 82 |
Jul 2016: 1286 May 2017: 214 Jun 2018: 570 Jun 2019: 388 Sep 2020: 446 July 2021: 388 |
| PsycINFO (OvidSP) [Date of most recent search: 21 July 2021] |
1 ("white matter" adj3 (ischemi* or ischaemi*)).ti,ab. 2 ("micro‐bleed*" or microbleed*).ti,ab. 3 Cerebral Ischemia/ or White Matter/ 4 Leukoencephalopathies/ or Leukoaraiosis/ 5 (Microhemorrhage* or Microhaemorrhage*).ti,ab. 6 or/1‐5 7 antithrombo*.ti,ab. 8 Aspirin/ 9 aspirin.ti,ab. 10 dipyridamole*.ti,ab. 11 clopidogrel*.ti,ab. 12 triflusal.ti,ab. 13 prasugrel.ti,ab. 14 ticagrelor.ti,ab. 15 ticlopidine.ti,ab. 16 cilostazol.ti,ab. 17 vorapaxar.ti,ab. 18 abciximab.ti,ab. 19 eptifibatide.ti,ab. 20 tirofiban.ti,ab. 21 terutroban.ti,ab. 22 disgren.ti,ab. 23 plavix.ti,ab. 24 effient.ti,ab. 25 brilinta.ti,ab. 26 ticlid.ti,ab. 27 pletal.ti,ab. 28 zontivity.ti,ab. 29 ReoPro.ti,ab. 30 integrilin.ti,ab. 31 aggrastat.ti,ab. 32 persantine.ti,ab. 33 "acetylsalicylic acid".ti,ab. 34 "antiplatelet drug*".ti,ab. 35 Globulins/ 36 Adenosine/ 37 "vitamin k".ti,ab. 38 phylloquinone.ti,ab. 39 phytomenadione.ti,ab. 40 phytonadione.ti,ab. 41 "thrombin* inhibitor*".ti,ab. 42 dabigatran.ti,ab. 43 rivaroxaban.ti,ab. 44 apixaban.ti,ab. 45 coumarin*.ti,ab. 46 warfarin.ti,ab. 47 heparin.ti,ab. 48 phenprocoumon.ti,ab. 49 Acenocoumarol.ti,ab. 50 atromentin.ti,ab. 51 brodifacoum.ti,ab. 52 phenindione.ti,ab. 53 "Xa inhibitor*".ti,ab. 54 or/7‐53 55 exp Clinical Trials/ 56 randomly.ab. 57 randomi?ed.ti,ab. 58 placebo.ti,ab. 59 groups.ab. 60 "double‐blind*".ti,ab. 61 "single‐blind*".ti,ab. 62 RCT.ti,ab. 63 or/55‐62 64 6 and 54 and 63 |
Jul 2016: 38 May 2017: 20 Jun 2018: 3 Jun 2019: 1 Sep 2020: 5 July 2021: 4 |
| CINAHL (EBSCOhost) [Date of most recent search: 21 July 2021] |
S1 TX ("white matter" N3 (ischemi* or ischaemi*)) S2 TX "micro‐bleed*" or microbleed* S3 MH Ischemia S4 TX Microhemorrhage* or Microhaemorrhage* S5 (S1 OR S2 OR S3 OR S4) S6 TX antithrombo* S7 MH Aspirin S8 TX Aspirin S9 MH dipyridamole S10 TX dipyridamole* S11 TX clopidogrel* S12 TX triflusal S13 TX prasugrel S14 TX ticagrelor S15 TX ticlopidine S16 TX cilostazol S17 TX vorapaxar S18 TX abciximab S19 TX tirofiban S20 TX disgren S21 TX plavix S22 TX effient S23 TX brilinta S24 TX ticlid S25 TX pletal S26 TX zontivity S27 TX ReoPro S28 TX integrilin S29 TX aggrastat S30 TX "acetylsalicylic acid" S31 TX "antiplatelet drug*" S32 MH Thromboxanes S33 MH Glycoproteins S34 MH Adenosine Diphosphate S35 MH Anticoagulants S36 TX "vitamin k" S37 TX phylloquinone S38 TX phytomenadione S39 TX phytonadione S40 TX "thrombin* inhibitor*" S41 MH Fibrinolytic Agents S42 TX dabigatran S43 TX rivaroxaban S44 TX apixaban S45 TX coumarin* S46 TX warfarin S47 MH warfarin S48 MH Heparin S49 TX Heparin S50 TX phenprocoumon S51 TX Acenocoumarol S52 TX atromentin S53 TX brodifacoum S54 TX "Xa inhibitor*" S55 (S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54) S56 MH "Clinical Trials" OR TX trial OR TX "single‐blind*" OR TX "double‐blind*" OR TX "treatment as usual" OR TX randomly S57 (S5 AND S55 AND S56) |
Jul 2016: 99 May 2017: 16 Jun 2018: 99 Jun 2019: 24 Sep 2020: 19 July 2021: 20 |
| Web of Science (Clarivate) – all databases [includes: Web of Science (1945‐present); BIOSIS Previews (1926‐present); MEDLINE (1950‐present); Journal Citation Reports] [Date of most recent search: 21 July 2021] |
# 1 TS=("white matter ischemi*" Or "white matter ischaemi*" OR "micro‐bleed*" OR microbleed* OR "Brain Ischemia" OR "White Matter pathology" OR Leukoencephalopathies OR Leukoaraiosis OR Microhemorrhage* OR Microhaemorrhage*) # 2 TS=(antithrombo* OR asprin OR dipyridamole* OR clopidogrel* OR Thromboxanes OR Glycoproteins OR "Adenosine Diphosphate" OR Anticoagulants OR Antithrombins OR "Factor Xa" OR "Fibrinolytic Agents" OR Warfarin OR Heparin) # 3 TS=(randomly OR randomised OR randomized OR "random allocat*" OR RCT OR CCT OR "double blind*" OR "single blind*" OR "double blind*" OR "single blind*") # 4 #3 AND #2 AND #1 Timespan=All years Search language=Auto |
Jul 2016: 941 May 2017: 95 Jun 2018: 167 Jun 2019: 9 Sep 2020: 15 July 2021: 112 |
| LILACS (BIREME) [Date of most recent search: 21 July 2021] |
ischemi$ OR micro‐bleed$ OR microbleed$ OR Brain Ischemia OR Leukoencephalopathies OR Leukoaraiosis OR Microhemorrhage$ OR Microhaemorrhage$ [Words] and antithrombo$ OR dipyridamole OR clopidogrel OR Thromboxanes OR Glycoproteins OR Adenosine Diphosphate OR Anticoagulants OR Antithrombins OR Factor Xa OR Fibrinolytic Agents OR Warfarin OR Heparin [Words] and randomly OR randomised OR randomized OR RCT OR "controlled trial" OR "double blind$" OR placebo [Words] | Jul 2016: 17 May 2017: 3 Jun 2018: 4 Jun 2019: 0 Sep 2020: 0 July 2021: 0 |
| ClinicalTrials.gov (www.clinicaltrials.gov) [Date of most recent search: 21 July 2021] |
ischemiA OR micro‐bleed$ OR microbleed OR Brain Ischemia OR Leukoencephalopathies OR Leukoaraiosis OR Microhemorrhage OR Microhaemorrhage | antithromboTIC OR dipyridamole OR clopidogrel OR Thromboxanes OR Glycoproteins OR Adenosine Diphosphate OR Anticoagulants OR Antithrombins OR Factor Xa OR Fibrinolytic Agents OR Warfarin OR Heparin | Jul 2016: 955 May 2017: 0 Jun 2018: 134 Jun 2019: 125 Sep 2020: 139 July 2021: 108 |
| ALOIS (via CRS web) [Date of most recent search: 21 July 2021] |
(ischemia OR micro‐bleed OR microbleed OR Brain Ischemia OR Leukoencephalopathies OR Leukoaraiosis OR Microhemorrhage OR Microhaemorrhage) AND (antithrombotic OR dipyridamole OR clopidogrel OR Thromboxanes OR Glycoproteins OR Adenosine Diphosphate OR Anticoagulants OR Antithrombins OR Factor Xa OR Fibrinolytic Agents OR Warfarin OR Heparin) |
Jul 2016: 9 May 2017: 4 Jun 2018: 3 Jun 2019: 0 Sep 2020: 18 July 2021: 0 |
| ICTRP [Date of most recent search: 6 June 2019. Database not available 16 September 2020, or July 2021] |
(ischemia OR micro‐bleed OR microbleed OR Brain Ischemia OR Leukoencephalopathies OR Leukoaraiosis OR Microhemorrhage OR Microhaemorrhage) AND (antithrombotic OR dipyridamole OR clopidogrel OR Thromboxanes OR Glycoproteins OR Adenosine Diphosphate OR Anticoagulants OR Antithrombins OR Factor Xa OR Fibrinolytic Agents OR Warfarin OR Heparin) |
Jul 2016: 59 May 2017: 111 Jun 2018: 24 Jun 2019: 22 |
| TOTAL before deduplication | Jul 2016: 4920 May 2017: 573 Jun 2018: 1380 Jun 2019: 706 Sep 2020: 1078 July 2021: 1001 TOTAL: 9658 |
|
| TOTAL after deduplication | Jul 2016: 4015 May 2017: 368 Jun 2018: 1211 Jun 2019: 663 Sep 2020: 934 July 2021: 893 TOTAL: 8084 |
|
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jia 2016.
| Study characteristics | ||
| Methods |
Design: randomised, double‐blind, placebo‐controlled trial Location/setting: 15 academic medical centres in China Date of study: 29 June 2009 to 2 May 2015 (participants screening: September 2008 to December 2009) Sample size: 563 people with a diagnosis of subcortical vascular cognitive impairment without dementia were enrolled and assessed for eligibility. 282 were excluded and 281 entered the study and underwent randomisation. Randomisation: among the 281 people who underwent randomisation, 141 were assigned to DL‐3‐n‐butylphthalide (117/141 completed the 24 weeks' treatment) and 140 were assigned to placebo (126/140 completed the 24 weeks' treatment). Participants were randomly assigned in a 1:1 ratio to receive kits containing DL‐3‐n‐butylphthalide 200 mg or placebo, which were labelled with sequential numbers according to a randomisation list (stratified by investigation site, in blocks of 4) generated by an independent statistician. |
|
| Participants |
Number in study: 281 Participant diagnosis: subcortical vascular cognitive impairment without dementia Inclusion criteria
Exclusion criteria
Mean age: DL‐3‐n‐butylphthalide: 68.0 (SD 8.8) years; placebo: 66.7 (SD 7.7) years Females: DL‐3‐n‐butylphthalide: 48 participants (34.3%); placebo: 48 participants (34.3%) Education: DL‐3‐n‐butylphthalide: < 5 years: 50 participants (35.7%); > 5 years: 90 participants (64.3%); placebo: < 5 years: 52 participants (37.1%); > 5 years: 88 participants (62.9%) Baseline comorbidities
Baseline concomitant aspirin: DL‐3‐n‐butylphthalide: 61.4%; placebo: 65.7% Consent: written informed consent |
|
| Interventions |
Pharmacological intervention: DL‐3‐n‐butylphthalide 200 mg for 24 weeks Control: placebo for 24 weeks |
|
| Outcomes |
Primary outcomes (all measured at baseline and after 6 months of treatment)
Secondary outcomes (all measured at baseline and after 6 months of treatment)
Withdrawal from trial drug Of the 280 participants initially included: DL‐3‐n‐butylphthalide: 3 had drug‐related adverse events, 10 lost to follow‐up, 4 comorbidities worsened, 4 withdrew from treatment in the group; placebo: 8 lost to follow‐up, 1 comorbidity worsened and 3 withdrew from treatment. 37 participants discontinued treatment across both arms, therefore only 243 participants completed the 24 weeks of either DL‐3‐n‐butylphthalide or placebo treatment. |
|
| Notes |
PubMed link: www.ncbi.nlm.nih.gov/pubmed/26086183 Chinese Clinical Trial Registry number: ChiCTR‐TRC‐09000440 Funding source: "Eleven Five‐Year" Scientific Support Plan Project of State Science and Technology Commission: Diagnosis and Intervention of Mild Cognitive Impairment. The State Science and Technology Commission had no other role in the study. Research protocol approval: institutional review board at each participating institution Study medication: donated by Shijiazhuang Pharmaceutical Group Company. It was stated that, "The company had no other role in the study." Conduct, safety and adherence to protocol monitoring: by an independent data and safety monitoring board. Declaration of interest: (quote) "Authors declared that they have no conflicts of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned in a 1:1 ratio to received three times daily oral DL‐3‐n‐butylphthalide 200 mg or placebo of identical appearance for 24 weeks. The randomisation list (stratified by investigation site, in blocks of four) was generated by an independent statistician." |
| Allocation concealment (selection bias) | Low risk | Quote: "Every site was supplied with kits of study drug that were labelled with sequential numbers corresponding to the randomisation list." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Patients, caregivers and site investigators were blinded to the treatment allocation." Comment: the trial drug and placebo were of identical appearance. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The clinician completing the CIBIC‐plus was blind to the other psychometric assessments and adverse events." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: DL‐3‐n‐butylphthalide: 23/140 (16.4%) participants; placebo: 14/140 (10%) participants. |
| Selective reporting (reporting bias) | Unclear risk | Comment: outcome measures were reported as adjusted mean, but the adjustments made were not clearly stated. Multiple outcomes listed as primary on trial register. Sample size in protocol and sample size reported in study did not correspond. |
| Other bias | Unclear risk | Industry support Quote: "The Shijiazhuang Pharmaceutical Group Company donated the study medication but had no other role in the study." Sample size Quote: "Thus, the sample size was under‐estimated, and the desired power was not achieved." Potential "significant‐result bias." |
Maestrini SILENCE 2018.
| Study characteristics | ||
| Methods |
Design: longitudinal, randomised, double‐blind controlled vs placebo study Location/setting: 8 Italian centres Sample size: 350 people underwent baseline screening, 124 people recruited, 41 excluded after neuroradiological diagnosis review, 50 participants enrolled in double‐blind study (aspirin: 24; placebo: 26) |
|
| Participants |
Number in study: 50 Inclusion criteria
Exclusion criteria
Median age: 66 (IQR: 54–72) years; placebo: 68 years (IQR: 60–73) years Education: ≥ 9 years: aspirin: 11 (32.4%); placebo: 18 (42.9%) Baseline comorbidities
|
|
| Interventions |
Active intervention: aspirin 100 mg administered as an enteric‐coated white tablet for 4 years Control intervention: enteric‐coated white tablet with identical appearance for 4 years Management of vascular risk factors was administered to all eligible participants at screening visits and throughout study. |
|
| Outcomes | Follow‐up: 4 years Primary outcome
Secondary outcomes
|
|
| Notes | EudraCT Number: 200‐000996‐16; Sponsor Protocol Number: 694/30.06.04 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A group of patients were not enrolled in the study because they refused to participate in the pharmacological trial. These subjects were studied prospectively and underwent the same baseline screening and flow chart of exams of those who were randomized." For this study, only randomised participants were included. However, we regarded this domain at unclear risk of bias, as we could not be certain how the combined randomised and non‐randomised trial design influenced allocation of participants. |
| Allocation concealment (selection bias) | Unclear risk | No details givens. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Treatment allocation remained blinded to investigators and subjects until the conclusion of the study, except for patients who withdraw for any collateral or adverse effect and/or any new cardiovascular events." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "A neuroradiologist, blinded to the patient's medical history, classified SBIs according to size and location." An experienced neurologist, blinded to MRI results, reviewed the medical history to exclude any previous cerebrovascular overt episode. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Lost to follow‐up: aspirin: 9 (25%); placebo: 9 (19%) Withdraws consent: aspirin: 4 (11%); placebo: 0 Completed follow‐up: aspirin: 15 (42%); placebo: 23 (49%) |
| Selective reporting (reporting bias) | Unclear risk | EudraCT stated, "Trial prematurely ended" (not described in paper). Full protocol no longer available through EudraCT. |
| Other bias | Low risk | No other bias detected. |
Pearce SPS3 2014.
| Study characteristics | ||
| Methods |
Design: randomised, double‐blind, placebo‐controlled trial Location/setting: 81 clinical centres in North America, Latin America and Spain (7 countries) Date of study: March 2003 to May 2012 (enrolment period 2003–2011) Sample size: 3020 people, but only 2916 participants had cognitive assessment (CASI) assessment at study entry. Randomisation: among the 2916 participants with CASI assessment at study entry, 1468 were assigned to aspirin + clopidogrel and 1448 to aspirin + placebo; 74% of the 2916 participants had the CASI assessment completed at their last annual visit. Quote: "Participants were simultaneously randomised in a 2‐by‐2 factorial design to both an antiplatelet intervention (1:1. double‐blind, aspirin + placebo vs. aspirin + clopidogrel). Randomization assignments (permuted block design of variable size, stratified by clinical centre and hypertension status) were unavailable for preview and stored electronically at each clinical centre and at the SPS3 Statistical Centre." |
|
| Participants |
Number in study: 2916 Mean age: aspirin + clopidogrel: 63.5 (SD 10.8) years; aspirin + placebo: 63.1 (SD 10.7) years Female: aspirin + clopidogrel: 557 (38%); aspirin + placebo: 531 (37%) Education: aspirin + clopidogrel: 0–8 years: 391 (27%); 9–12 years: 527 (36%); > 12 years: 550 (37%); aspirin + placebo: 0–8 years: 374 (26%); 9–12 years: 578 (40%); > 12 years: 496 (34%) Ethnicity: aspirin + clopidogrel: White, not Hispanic: 751 (51%); Hispanic: 454 (31%); Black: 237 (16%); other or multiracial: 26 (2%); aspirin + placebo: White, not Hispanic: 745 (51%); Hispanic: 452 (31%); Black: 236 (16%); other or multiracial: 15 (1%) Medical history: aspirin + clopidogrel: diabetes: 524 (36%); hypertension: 1107 (75%); ischaemic heart disease: 157 (11%); lacunar stroke: 154 (11%); subcortical TIA: 80 (5%); aspirin + placebo: diabetes: 546 (38%); hypertension: 1172 (74%); ischaemic heart disease: 150 (10%); lacunar stroke: 146 (10%); subcortical TIA: 78 (5%) Days from index event to neuropsychological testing, mean: aspirin + clopidogrel: 78 (SD 50) days; aspirin + placebo: 74 (SD 51) days Modified Rankin stroke disability score: aspirin + clopidogrel: 0: 230 (16%); 1: 763 (52%); 2: 348 (24%); 3: 127 (9%); aspirin + placebo: 0: 209 (14%); 1: 741 (51%); 2: 368 (25%); 3: 130 (9%) Barthel index score ≥ 95: aspirin + clopidogrel: 1173 (80%); aspirin + placebo: 1148 (79%) Mild cognitive impairment: aspirin + clopidogrel: 649 (45%); aspirin + placebo: 654 (46%) Additional small subcortical infracts on MRI: aspirin + clopidogrel: 573 (40%); aspirin + placebo: 553 (39%) White matter lesion (ARWMC score): aspirin + clopidogrel: none/mild (score 0–4): 709 (49%); moderate (score 5–8): 407 (28%); severe (score ≥ 9): 327 (23%); aspirin + placebo: none/mild (score 0–4): 728 (51%); moderate (score 5–8): 397 (28%); severe (≥ 9): 298 (21%) Inclusion criteria People with symptomatic small subcortical stroke (S3) confirmed by MRI, randomised within 6 months of S3 qualification and satisfying all the following criteria
Exclusion criteria
Consent: (quote): "Participation required written informed consent and study protocol approval by the human research subjects committee at each study centre." Protection of human participants: (quote): "All clinical sites are required to comply with their local Institutional Review Boards and Human Subject Protection policies. All participants provide written informed consent in their preferred language (English, French, or Spanish) before undergoing any study procedures. The safety of all participants is closely monitored." |
|
| Interventions | Both groups received antiplatelet intervention. Pharmacological intervention (dual antiplatelet therapy): aspirin + clopidogrel Control (single antiplatelet therapy): aspirin + placebo Treatment duration: 3 years |
|
| Outcomes | Mean follow‐up: 3.4 years Primary cognitive outcome
SPS3 primary outcome
SPS3 secondary outcomes
|
|
| Notes |
PubMed link: www.ncbi.nlm.nih.gov/pubmed/25453457 ClinicalTrials.gov Registry number: NCT00059306 Funding source: National Institute of Neurological Disorders and Stroke (US) (U01 NS38529‐04A1) Role of funding source: (quote) "The sponsor of the study participated in study design, data collection, data analysis and data interpretation." Declaration of interest: (quote) "The authors declare that they have no conflicts of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were simultaneously randomised in a 2‐by‐2 factorial design to both an antiplatelet intervention (1:1, double‐blind, aspirin + placebo vs. aspirin + clopidogrel)." |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization assignments (permuted block design of variable size, stratified by clinical centre and hypertension status) were unavailable for preview and stored electronically at each clinical centre and at the SPS3 Statistical Centre." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All SPS3 participants take enteric‐coated aspirin 325mg daily and are randomly assigned (double‐blind) to take clopidogrel 75mg daily or the matching placebo. Antiplatelet medications are provided to patients at randomisation and each quarterly follow‐up visit, with adherence measured by pill counts." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All possible outcome and safety events are reviewed by the blinded Events Adjudication Committee made up of neurologists, cardiologists, and internists who are not otherwise involved in SPS3. Event materials, including diagnostic information, blinded to patient identity are submitted by the clinical sites to the Events Coordinator, who blinds them to any information potentially revealing SPS3 treatment assignments and distributes to at least two committee members for review." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 74% of the 2916 participants had the CASI assessment completed at their last annual visit. Missing cognitive assessments likely to be related to cognitive outcome. |
| Selective reporting (reporting bias) | Low risk | Comment: both primary and secondary outcomes were reported as described in the study protocol. |
| Other bias | Low risk | No evidence of other bias noted. |
ADL: activities of daily living; ARWMC: age‐related white matter change; CASI: Cognitive Abilities Screening Instrument; CDR: Clinical Dementia Rating; CDR‐SB: Clinical Dementia Rating scale Sum of Boxes; CIBIC‐plus: Clinician Interview‐Based Impression of Change‐Plus Caregiver Input; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders Fourth Edition; ECG: electrocardiogram; HAMD: Hamilton Depression Scale; INR: international normalised ratio; IQR: interquartile range; MMSE: Mini‐Mental State Examination; MRI: magnetic resonance imaging; NPI: Neuropsychiatric Inventory; NYHA: New York Heart Association; SBI: silent brain infarction; SD: standard deviation; SPS3: Secondary Prevention of Small Subcortical Strokes; TIA: transient ischaemic attack; WML: white matter lesions.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ASPREE‐NEURO | Wrong population. |
| AVERROES‐MRI assessment study | Too few participants with small vessel disease and no subgroup data available. |
| COMPASS MRI | Too few participants with small vessel disease and no subgroup data available. |
| Douiri 2013 | Not an RCT. |
| Han 2013 | Irrelevant outcomes. |
| Jacobs 2015 | Not an RCT. |
| Kwok 2015 | Not an RCT. |
| Kwon 2016 | Not an antithrombotic trial. |
| LACI‐1 | Follow‐up too short. |
| Shinod‐Tagawa 2002 | Irrelevant outcomes#. |
| Xu 2020 | Irrelevant outcomes. |
| Zhang 2014 | Not an RCT. |
RCT: randomised controlled trial.
Characteristics of studies awaiting classification [ordered by study ID]
CAVAD.
| Methods | Randomised, blinded trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Cilostazol 100 mg twice daily for 12 months Aspirin 100 mg once daily for 12 months |
| Outcomes | Primary outcomes: changes in cognitive scores (MMSE, Montreal Cognitive Assessment, Clinical Dementia Rating and Blessed‐Roth (time frame 1 year) |
| Notes | Requested further information but no response from trial team. |
CT: computed tomography; MMSE: Mini‐Mental State Examination; MRI: magnetic resonance imaging; mRS: Modified Rankin Score; NIHSS: National Institutes of Health Stroke Scale.
Characteristics of ongoing studies [ordered by study ID]
CAF.
| Study name | Impact of anticoagulation therapy on the cognitive decline and dementia in patients with nonvalvular –atrial fibrillation (CAF) |
| Methods | Phase 4 randomised parallel assignment open‐label trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: dabigatran etexilate 150 mg twice daily (if CrCl > 30 mL/minute) or 75 mg twice daily (CrCl 15–30 mL/minute) Active comparator: warfarin Dose‐adjusted warfarin (INR 2.0–3.0) |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | 2017 |
| Contact information | Contact: T Jared Bunch, MD; 801‐507‐4701; jared.bunch@imail.org Contact: Patti Spencer; 801‐507‐4778; patti.spencer@imail.org |
| Notes |
CHALLENGE.
| Study name | Efficacy study of cilostazol and aspirin on cerebral small vessel disease (Challenge) |
| Methods | Multicentre, randomised, double‐blind study |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Aspirin 100 mg once daily for 104 weeks Cilostazol 200 mg once daily for 104 weeks |
| Outcomes | Primary outcome
Secondary outcomes
'Other' outcomes
|
| Starting date | 2013 |
| Contact information | Principal Investigator: Seong Hye Choi, Inha University Hospital |
| Notes |
ChiCTR‐TCS‐14005054.
| Study name | Cilostazol in decreasing progression of cerebral white matter hyperintensities (DREAM) |
| Methods | Parallel double‐blind randomised trial |
| Participants | 140 men and women aged 65–85 years |
| Interventions | Cilostazol Placebo |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | 27 October 2014 |
| Contact information | Name: Prof Vincent Chung Tong Mok Address: Rm 124010, 10/F, Clinical Sciences Building, Prince of Wales Hospital, Shatin, N.T. Hong Kong Contact number: +852 2632 2195 Contact email: vctmok@cuhk.edu.hk |
| Notes | CUHK_CCT00430; ChiCTR‐TCS‐14005054 www2.ccrb.cuhk.edu.hk/registry/public/269 |
ECISBI.
| Study name | Efficacy of Clopidogrel on Incidence of Silent Brain Infarction (ECISBI) |
| Methods | Randomised controlled trial |
| Participants | 152 participants admitted for stroke/TIA, with indication for antiplatelet therapy as secondary prevention (decision independent of the study and based on individual clinical decision for each patient by the treating physician) |
| Interventions | Clopidogrel Aspirin |
| Outcomes | Primary outcome
Secondary outcome
|
| Starting date | 30 September 2021 |
| Contact information | Calin I Prodan, MD; 405‐456‐1479; calin.prodan@va.gov |
| Notes |
LACI‐2.
| Study name | LACunar Intervention (LACI‐2) Trial‐2: assessment of safety and efficacy of cilostazol and isosorbide mononitrate to prevent recurrent lacunar stroke and progression of cerebral small vessel disease |
| Methods | Phase 2b preparatory to phase 3 randomised, partial factorial, open‐label, blinded endpoint trial |
| Participants | 400 |
| Interventions | Isosorbide mononitrate oral titrated dosing Cilostazol oral titrated dosing Isosorbide mononitrate + cilostazol |
| Outcomes |
|
| Starting date | 2018 |
| Contact information | Chief Investigator: Joanna M Wardlaw, University of Edinburgh, UK |
| Notes |
NCT01932203.
| Study name | A multicenter, randomized, double blind study to compare the efficacy between cilostazol and aspirin on white matter changes by cerebral small vessel disease |
| Methods | Parallel double‐blind randomised trial |
| Participants | 255 adults aged 50–85 years |
| Interventions | Enteric‐coated aspirin 100 mg Cilostazol 200 mg once a day |
| Outcomes | Primary outcome
Secondary outcomes
Other outcomes
|
| Starting date | July 2013 |
| Contact information | Principal Investigator: Seong Hye Choi, MD, PhD: Inha University Hospital; 82 32 890 3659; seonghye@inha.ac.kr |
| Notes | ClinicalTrial.gov: NCT01932203 |
PICASSO‐Cog.
| Study name | PreventIon of CArdiovascular events in iSchemic Stroke patients with high risk of cerebral hemOrrhage for reducing COGnitive decline |
| Methods | Substudy of the PICASSO trial – an ongoing randomised, double‐blind, placebo‐controlled multinational trial |
| Participants | Key inclusion criteria
|
| Interventions | Cilostazol 100 mg twice daily Aspirin 100 mg once daily Probucol 250 mg twice daily No probucol The trial is a double‐blind and double‐dummy study using matched placebo to compare cilostazol versus aspirin groups, and an open‐labelled, blinded endpoint evaluation to compare probucol versus non‐probucol groups. |
| Outcomes |
|
| Starting date | |
| Contact information | Sun U Kwon, MD, PhD, Stroke Center and Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, 388‐1 Pungnap‐dong, Songpa‐gu, Seoul 138‐736, Republic of Korea. E‐mail: sukwon@amc.seoul.kr |
| Notes |
Reid ENVIS‐ion 2012.
| Study name | Aspirin for the prevention of cognitive decline in the elderly: rationale and design of a neurovascular imaging study (ENVIS‐ion) Substudy of: Aspirin in Reducing Events in the Elderly (ASPREE) |
| Methods | Double‐blind, placebo‐controlled trial of 3 years' duration set in 2 Australian academic medical centre outpatient clinics |
| Participants | 600 adults aged ≥ 70 years with normal cognitive function and without overt cardiovascular disease |
| Interventions | Aspirin 100 mg daily Placebo |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | January 2010 |
| Contact information | Principal Investigators: Richard Grimm, MD, PHD: Berman Center for Outcomes and Clinical Research, Minneapolis, MN, US; John McNeil, MBBS, PHD: Monash University; Berman Center for Outcomes & Clinical Research; ASPREE Project Manager, Brenda Kirpach Contact number: 612‐873‐6905 Contact email: bkirpach@bermancenter.org |
| Notes | Clinicaltrial.gov: NCT01038583 Study protocol: www.ncbi.nlm.nih.gov/pmc/articles/PMC3297524/ |
ADAS‐Cog‐11: 11‐item Alzheimer's Disease Assessment Scale – Cognitive Subscale; ALT: alanine aminotransferase; AST: aspartate transaminase; CHADS: Congestive heart failure, Hypertension, Age ≥ 75 years, Diabetes mellitus, previous Stroke/transient ischaemic attack; CrCl: creatinine clearance; CSF: cerebrospinal fluid; DAD: Disability Assessment for Dementia; INR: international normalised ratio; MMSE: Mini‐Mental State Examination; MRI: magnetic resonance imaging; NINDS‐CSN: National Institute of Neurological Disorders and Stroke – Canadian Stroke Network; TIA: transient ischaemic attack; VCI: vascular cognitive impairment; WMC: white matter change; WMH: white matter hyperintensity.
Differences between protocol and review
We made the following changes from the published protocol (Kwan 2016b).
"Absence of dementia of any cause as defined by internationally‐accepted diagnostic criteria" was one of the inclusion criteria for participants. However, all three included studies reported differing inclusion/exclusion criteria at baseline. We updated the wording to "Absence of dementia of any cause as defined by internationally accepted diagnostic criteria, however a degree of flexibility was needed because of heterogeneity of the operationalisation of this exclusion criterion in the included studies. Therefore, we also accepted cognitive testing that was plausible to detect incipient or existing dementia."
We added the secondary outcome mild cognitive impairment, as there was important evidence on this outcome, but we wanted to keep a distinction with incident dementia.
We further operationalised our definition of cSVD, by setting criteria around a minimum proportion of people with cSVD in studies of mixed populations and a minimum degree of cSVD features for individual participants.
We had a minimum intervention duration of six months; however, we also accepted studies with an intervention duration of minimum 24 weeks (5.5 months).
Contributions of authors
Lead review author (designed, conducted and led the writing of the review): JK.
Main co‐review authors (conducted and co‐wrote the review): LLWC, MH, LSW, TQ.
Specialist advisory co‐reviewer (consulted, advised, and edited the review): PM.
Sources of support
Internal sources
Department of Medicine, the University of Hong Kong, Hong Kong
School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, UK
External sources
-
National Institute for Health Research (NIHR), UK
This review was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Dementia and Cognitive Improvement Group. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS) or the Department of Health.
Declarations of interest
JK: none.
MH: none.
LC: none.
PM: none.
TQ: none.
LW: none.
Edited (no change to conclusions)
References
References to studies included in this review
Jia 2016 {published data only}
- Jia J, Wei C, Liang J, Zhou A, Zuo X, Song H, et al. The effects of DL-3-n-butylphthalide in patients with vascular cognitive impairment without dementia caused by subcortical ischaemic small vessel disease: a multicentre, randomised, double-blind, placebo-controlled trial. Alzheimer's & Dementia: the Journal of the Alzheimer's Association 2016;12(2):89-99. [DOI: 10.1016/j.jalz.2015.04.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Maestrini SILENCE 2018 {published data only}
- Maestrini I, Altieri M, Clemente LD, Vicenzini E, Pantano P, Raz E, et al. Longitudinal study on low-dose aspirin versus placebo administration in silent brain infarcts: the SILENCE study. Stroke Research and Treatment 2018;2018(7532403):1-9. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pearce SPS3 2014 {published data only}
- Pearce LA, McClure LA, Anderson DC, Jacova C, Sharma M, Hart RG, et al. Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke: a secondary analysis from the SPS3 randomised trial. Lancet Neurology 2014;13:1177-85. [CENTRAL: PMC4284947] [DOI: 10.1016/S1474-4422(14)70224-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M, Pearce LA, Benavente OR, Anderson DC, Connolly SJ, Palacio S, et al. Predictors of mortality in patients with lacunar stroke in the Secondary Prevention of Small Subcortical Strokes trial. Stroke; a Journal of Cerebral Circulation 2014;45(10):2989–94. [CENTRAL: PMC4175186] [DOI: ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- The SPS3 Investigators, Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, et al. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. New England Journal of Medicine 2012;367(9):817-25. [DOI: 10.1056/NEJMoa1204133] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
ASPREE‐NEURO {published data only}ACTRN12613001313729
- Ward SA, Raniga P, Ferris NJ, Woods RL, Storey E, Bailey MJ, et al. ASPREE-NEURO study protocol: a randomized controlled trial to determine the effect of low-dose aspirin on cerebral microbleeds, white matter hyperintensities, cognition, and stroke in the healthy elderly. International Journal of Stroke 2017;12(1):108-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
AVERROES‐MRI assessment study {published data only}
- O'Donnell MJ, Eikelboom JW, Yusuf S, Diener HC, Hart RG, Smith EE, et al. Effect of apixaban on brain infarction and microbleeds: AVERROES – MRI assessment study. American Heart Journal 2016;178:145-50. [DOI: 10.1016/j.ahj.2016.03.019] [DOI] [PubMed] [Google Scholar]
COMPASS MRI {published data only}
- Sharma M, Hart RG, Smith EE, Bosch J, Eikelboom JW, Connolly SJ, et al. Rivaroxaban for prevention of covert brain infarcts and cognitive decline: the COMPASS MRI substudy. Stroke 2020;51:2901-9. [DOI] [PubMed] [Google Scholar]
Douiri 2013 {published data only}
- Douiri A, McKevitt C, Emmett ES, Rudd AG, Wolfe CD. Long-term effects of secondary prevention on cognitive function in stroke patients. Circulation 2013;128(12):1341-8. [DOI: 10.1161/CIRCULATIONAHA.113.002236] [PMID: ] [DOI] [PubMed] [Google Scholar]
Han 2013 {published data only}
- Han SW, Lee S, Kim SH, Lee JH, Kim GS, Kim O, et al. Effect of cilostazol in acute lacunar infarction based on pulsatility index of transcranial Doppler (ECLIPse): a multicenter, randomized, double-blind, placebo-controlled trial. European Neurology 2013;69:33-40. [DOI: DOI: 10.1159/000338247] [DOI] [PubMed] [Google Scholar]
Jacobs 2015 {published data only}
- Jacobs V, May HT, Bair TL, Anderson JL, Crandall BG, Cutler M, et al . Dementia and stroke rates were lower among patients receiving long-term anticoagulation therapy with novel oral anticoagulants compared to warfarin. American Journal of Cardiology 2015;118(2):210-4. [DOI: 10.1016/j.amjcard.2016.04.039] [PMID: 27236255] [DOI] [PubMed] [Google Scholar]
Kwok 2015 {published data only}
- Kwok CS, Shoamanesh A, Copley HC, Myint PK, Loke YK, Benavente OR. Efficacy of antiplatelet therapy in secondary prevention following lacunar stroke pooled analysis of randomised trials. Stroke 2015;46(4):1014. [DOI: 10.1161/STROKEAHA.114.008422] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kwon 2016 {published data only}
- Kwon HM, Lynn MJ, Turan TN, Derdeyn CP, Fiorella D, Lane BF, et al, Sammpris Investigators. Frequency, risk factors, and outcome of coexistent small vessel disease and intracranial arterial stenosis: results from the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial. JAMA Neurology 2016;73:36-42. [DOI: 10.1001/jamaneurol.2015.3145.] [PMID: ] [DOI] [PMC free article] [PubMed]
LACI‐1 {published data only}
- Blair GW, Appleton JP, Flaherty K, Doubal F, Sprigg N, Dooley R, et al. Tolerability, safety and intermediary pharmacological effects of cilostazol and isosorbide mononitrate, alone and combined, in patients with lacunar ischaemic stroke: the LACunar Intervention-1 (LACI-1) trial, a randomised clinical trial. Lancet EClinical Medicine 2019;11:34-43. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shinod‐Tagawa 2002 {published data only}
- Shindo-Tagawa T, Yamasaki Y, Yoshida S, Kajimoto Y, Tsujino T, Hakui N, et al. A phosphodiesterase inhibitor, cilostazol, prevents the onset of silent brain infarction in Japanese subjects with type II diabetes. Diabetologia 2002;45:188-94. [DOI] [PubMed] [Google Scholar]
Xu 2020 {published data only}
- Xu YY, Zong L, Zhang C, Pan Y, Jing J, Meng X, et al, on behalf of the CHANCE Investigators. The association of white matter hyperintensities with stroke outcomes and antiplatelet therapy in minor stroke patients. Annals of Translational Medicine 2020;8:331. [DOI: 10.21037/atm.2020.02.137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2014 {published data only}
- Zhang Y, Zhang Z, Yang B, Li Y, Zhang Q, Qu Q, et al. Effects of antiplatelet agents on functional outcome and cognitive status in patients with acute ischaemic stroke. International Journal of Gerontology 2014;8(4):189-92. [DOI: 10.1016/j.ijge.2013.12.005] [DOI] [Google Scholar]
References to studies awaiting assessment
CAVAD {published data only}
- NCT00847860. Cilostazol verse aspirin for vascular dementia in poststroke patients with white matter lesions (CAVAD). clinicaltrials.gov/ct2/show/NCT00847860 (first received 19 February 2009).
References to ongoing studies
CAF {published data only}
- NCT03061006. Impact of anticoagulation therapy on the cognitive decline and dementia in patients with non-valvular atrial fibrillation (CAF). clinicaltrials.gov/ct2/show/NCT03061006 (first received 23 February 2017).
CHALLENGE {published data only}
- NCT01932203. Efficacy study of cilostazol and aspirin on cerebral small vessel disease (Challenge). clinicaltrials.gov/ct2/show/NCT01932203 (first received 30 August 2013).
ChiCTR‐TCS‐14005054 {unpublished data only}
- ChiCTR-TCS-14005054. Cilostazol in retarding progression of cerebral white matter hyperintensities. www2.ccrb.cuhk.edu.hk/registry/public/269/history/1495 (first received 21 January 2014).
ECISBI {published data only}
- NCT04698031. Efficacy of Clopidogrel on Incidence of Silent Brain Infarction (ECISBI). clinicaltrials.gov/ct2/show/NCT04698031 (first received 6 January 2021).
LACI‐2 {published data only}
- NCT03451591. LACunar Intervention (LACI-2) Trial-2 (LACI-2). clinicaltrials.gov/ct2/show/NCT03451591 (first received 2 March 2018).
NCT01932203 {unpublished data only}
- NCT01932203. Efficacy study of cilostazol and aspirin on cerebral small vessel disease (Challenge). clinicaltrials.gov/ct2/show/NCT01932203 (first received 30 August 2013).
PICASSO‐Cog {published data only}
- Yu KH, Hong KS, Oh MS, Lee J, Lee JS, Kwon Su. Design and rationale for a cognitive outcome substudy in ischemic stroke patients with high risk of cerebral hemorrhage. Journal of Stroke and Cerebrovascular Diseases 2016;25(8):2061-6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Reid ENVIS‐ion 2012 {unpublished data only}
- Reid CM, Storey E, Budge MM. Aspirin for the prevention of cognitive decline in the elderly: rationale and design of a neuro-vascular imaging study (ENVIS-ion). BMC Neurology 2012;12(3):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Akinyemi 2013
- Akinyemi RO, Mukaetova-Ladinska EB, Attems J, Ihara M, Kalaria RN. Vascular risk factors and neurodegeneration in ageing related dementias: Alzheimer's disease and vascular dementia. Current Alzheimer Research 2013;10:642-53. [DOI] [PubMed] [Google Scholar]
Arba 2018
- Arba F, Quinn TJ, Hankey GJ, Lees KR, Wardlaw JM, Ali M, et al. Enlarged perivascular spaces and cognitive impairment after stroke and transient ischemic attack. International Journal of Stroke 2018;13:47-56. [DOI: 10.1177/1747493016666091] [DOI] [PubMed] [Google Scholar]
ATC 2002
- Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002;324:71-86. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Battle 2021
- Battle CE, Abdul-Rahimn AH, Shenkin SD, Hewitt J, Quinn TJ. Cholinesterase inhibitors for vascular dementia and other vascular cognitive impairments: a network meta-analysis. Cochrane Database of Systematic Reviews 2021, Issue 2. Art. No: CD013306. [DOI: 10.1002/14651858.CD013306.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beishuizen 2016
- Beishuizen CR, Stephan BC, Gool WA, Brayne C, Peters RJ, Andrieu S, et al. Web-based interventions targeting cardiovascular risk factors in middle-aged and older people: a systematic review and meta-analysis. Journal of Medical Internet Research 2016;18(3):e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blair 2019
- Blair GW, Appleton JP, Flaherty K, Doubal F, Sprigg N, Dooley R, et al. Tolerability, safety and intermediary pharmacological effects of cilostazol and isosorbide mononitrate, alone and combined, in patients with lacunar ischaemic stroke: the LACunar Intervention-1 (LACI-1) trial, a randomised clinical trial. EClinicalMedicine 2019;11:34-43. [DOI: 10.1016/j.eclinm.2019.04.001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boutet 2016
- Boutet C, Rouffiange-Leclair L, Schneider F, Camdessanché JP, Antoine JC, Barral FG. Visual assessment of age-related white matter hyperintensities using FLAIR images at 3T: inter- and intra-rater agreement. Neurodegenerative Diseases 2016;16:279-83. [DOI: 10.1159/000441420] [DOI] [PubMed] [Google Scholar]
Cameron 2014
- Cameron C, Coyle D, Richter T, Kelly S, Gauthier K, Steiner S, et al. Systematic review and network meta-analysis comparing antithrombotic agents for the prevention of stroke and major bleeding in patients with atrial fibrillation. British Medical Journal Open 2014;4:e004301. [DOI: 10.1136/bmjopen-2013-004301] [DOI] [PMC free article] [PubMed] [Google Scholar]
Crum 1993
- Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA 1993;269:2386-91. [PMID: ] [PubMed] [Google Scholar]
Del Brutto 2015
- Del Brutto OH, Mera RM, Zambrano M, Lama J, Del Brutto VJ, Castillo PR. Poor sleep quality and silent markers of cerebral small vessel disease: a population-based study in community-dwelling older adults (the Atahualpa Project). Sleep Medicine 2015;16:428-31. [DOI: 10.1016/j.sleep.2014.10.023] [DOI] [PubMed] [Google Scholar]
Diener 2008
- Diener HC, Sacco RL, Yusuf S, Cotton D, Ounpuu S, Lawton WA, et al. Effects of aspirin plus extended-release dipyridamole versus clopidogrel and telmisartan on disability and cognitive function after recurrent stroke in patients with ischaemic stroke in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial: a double-blind, active and placebo-controlled study. Lancet Neurology 2008;7:875-84. [DOI: 10.1016/S1474-4422(08)70198-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 1991
- Fisher CM. Lacunar infarcts – a review. Cerebrovascular Diseases 1991;1:311-20. [DOI: 10.1159/000108861] [DOI] [Google Scholar]
Geeganage 2010
- Geeganage C, Wilcox R, Bath PM. Triple antiplatelet therapy for preventing vascular events: a systematic review and meta-analysis. BMC Medicine 2010;8:36. [DOI: 10.1186/1741-7015-8-36] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), accessed 1 December 2021. Available at gradepro.org.
Grammas 2011
- Grammas P. Neurovascular dysfunction, inflammation and endothelial activation: implications for the pathogenesis of Alzheimer's disease. Journal of Neuroinflammation 2011;8:26. [DOI: 10.1186/1742-2094-8-26] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grau‐Olivares 2009
- Grau-Olivares M, Arboix A. Mild cognitive impairment in stroke patients with ischaemic cerebral small-vessel disease: a forerunner of vascular dementia? Expert Review of Neurotherapeutics 2009;9:1201-17. [DOI: 10.1586/ern.09.73] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Iadecola 2010
- Iadecola C. The overlap between neurodegenerative and vascular factors in the pathogenesis of dementia. Acta Neuropathology 2010;120:287-96. [DOI: 10.1007/s00401-010-0718-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ishida 2014
- Ishida K, Messé SR. Antiplatelet strategies for secondary prevention of stroke and TIA. Current Atherosclerosis Report 2014;16:449. [DOI: 10.1007/s11883-014-0449-6] [DOI] [PubMed] [Google Scholar]
Jack 2010
- Jack CR Jr, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurology 2010;9:119-28. [DOI: 10.1016/S1474-4422(09)70299-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jordan 2020
- Jordan F, Quinn TJ, McGuinness B, Passmore P, Kelly JP, Tudur Smith C, et al. Aspirin and other non-steroidal anti-inflammatory drugs for the prevention of dementia. Cochrane Database of Systematic Reviews 2020, Issue 4. Art. No: CD011459. [DOI: 10.1002/14651858.CD011459.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kwan 2016
- Kwan JS, Mak SF, Hui R, So K, Har WY, Azman R, et al. Prevalence and clinical impact of white matter hyperintensities, cerebral microbleeds, and medial temporal lobe atrophy on short- and long-term outcomes after stroke rehabilitation. Hong Kong Medical Journal 2016;22(Suppl 1):28. [hdl.handle.net/10722/225697] [Google Scholar]
Lip 2015
- Lip GY, Lane DA. Stroke prevention in atrial fibrillation: a systematic review. JAMA 2015;313:1950-62. [DOI: 10.1001/jama.2015.4369] [DOI] [PubMed] [Google Scholar]
McNeil 2018
- McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. Effect of aspirin on disability-free survival in the healthy elderly. New England Journal of Medicine 2018;379:1499-508. [DOI: 10.1056/NEJMoa1800722] [DOI] [PMC free article] [PubMed] [Google Scholar]
McShane 2019
- McShane R, Westby MJ, Roberts E, Minakaran N, Schneider L, Farrimond L, et al. Memantine for dementia. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No: CD003154. [DOI: 10.1002/14651858.CD003154.pub6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moffitt 2016
- Moffitt P, Lane DA, Park H, O'Connell J, Quinn TJ. Thromboprophylaxis in atrial fibrillation and association with cognitive decline: systematic review. Age Ageing 2016;45(6):767-75. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mok 2015
- Mok V, Kim JS. Prevention and management of cerebral small vessel disease. Journal of Stroke 2015;17:111-22. [DOI: 10.5853/jos.2015.17.2.111] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mortamais 2013
- Mortamais M, Artero S, Ritchie K. Cerebral white matter hyperintensities in the prediction of cognitive decline and incident dementia. International Review of Psychiatry 2013;25:686-98. [DOI: 10.3109/09540261.2013.838151] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norrving 2015
- Norrving B. Evolving concept of small vessel disease through advanced brain imaging. Journal of Stroke 2015;17:94-100. [DOI: 10.5853/jos.2015.17.2.94] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peng 2019
- Peng D. Clinical practice guideline for cognitive impairment of cerebral small vessel disease. Aging Medicine (Milton) 2019;2:64-73. [DOI: 10.1002/agm2.12073] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prince 2013
- Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and meta-analysis. Alzheimer's & Dementia 2013;9:63-75.e2. [DOI: 10.1016/j.jalz.2012.11.007] [DOI] [PubMed] [Google Scholar]
Richard 2012
- Richard E, Andrieu S, Solomon A, Mangialasche F, Ahtiluoto S, Moll van Charante EP, et al. Methodological challenges in designing dementia prevention trials – the European Dementia Prevention Initiative (EDPI). Journal of Neurological Sciences 2012;322(1):64-70. [DOI] [PubMed] [Google Scholar]
Safouris 2015
- Safouris A, Psaltopoulou T, Sergentanis TN, Boutati E, Kapaki E, Tsivgoulis G. Vascular risk factors and Alzheimer's disease pathogenesis: are conventional pharmacological approaches protective for cognitive decline progression? CNS & Neurological Disorders Drug Targets 2015;14:257-69. [DOI] [PubMed] [Google Scholar]
Schünemann 2008
- Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008;336:1106-10. [DOI: 10.1136/bmj.a139] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shinoda‐Tagawa 2002
- Shinoda-Tagawa T, Yamasaki Y, Yoshida S, Kajimoto Y, Tsujino T, Hakui N, et al. A phosphodiesterase inhibitor, cilostazol, prevents the onset of silent brain infarction in Japanese subjects with Type II diabetes. Diabetologia 2002;45:188-94. [DOI: 10.1007/s00125-001-0740-2] [DOI] [PubMed] [Google Scholar]
Smith 2017
- Smith EE, Saposnik G, Biessels GJ, Doubal FN, Fornage M, Gorelick PB, et al, American Heart Association Stroke Council, Council on Cardiovascular Radiology and Intervention, Council on Functional Genomics and Translational Biology, and Council on Hypertension. Prevention of stroke in patients with silent cerebrovascular disease: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017;48(6):e44-e71. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wardlaw 2013
- Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al, STandards for ReportIng Vascular changes on nEuroimaging (STRIVE v1). Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurology 2013;12:822-38. [DOI: 10.1016/S1474-4422(13)70124-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wardlaw 2019
- Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurology 2019;18:684-96. [DOI: 10.1016/S1474-4422(19)30079-1] [DOI] [PubMed] [Google Scholar]
Wardlaw 2021
- Wardlaw JM, Debette S, Jokinen H, De Leeuw FE, Pantoni L, Chabriat H, et al. ESO Guideline on covert cerebral small vessel disease. European Stroke Journal 2021;6(2):111-62. [DOI: 10.1177/23969873211012132] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
Wimo 2013
- Wimo A, Jönsson L, Bond J, Prince M, Winblad B, Alzheimer Disease International. The worldwide economic impact of dementia 2010. Alzheimers Dementia 2013;9:1-11.e3. [DOI: 10.1016/j.jalz.2012.11.006] [DOI] [PubMed] [Google Scholar]
Wong 2020
- Wong CK, Huang D, Zhou M, Hai J, Yue WS, Li WH, et al. Antithrombotic therapy and the risk of new-onset dementia in elderly patients with atrial fibrillation. Postgraduate Medicine Journal 2020;12:1-6. [DOI: 10.1136/postgradmedj-2020-137916] [DOI] [PubMed] [Google Scholar]
World Alzheimer Report 2015
- Prince M, Wimo A, Guerchet M, Ali GC, Wu YT, Prina M. World Alzheimer Report 2015. London (UK): Alzheimer's Disease International (ADI), 2015. [Google Scholar]
References to other published versions of this review
Kwan 2016b
- Kwan JS, Myint PK, Wong A, Mok V, Lau GK, Mak KF. Antithrombotic therapy to prevent cognitive decline in people with small vessel disease on neuroimaging but without dementia. Cochrane Database of Systematic Reviews 2016, Issue 7. Art. No: CD012269. [DOI: 10.1002/14651858.CD012269] [DOI] [PMC free article] [PubMed] [Google Scholar]


