Abstract
A dog was examined because of acute onset of respiratory distress following a cervical dog bite. Physical examination revealed a deep ventral cervical bite wound associated with localized mild subcutaneous emphysema. Thoracic radiographs showed moderate pneumomediastinum. Medical management consisting of oxygen therapy, antibiotics, and anti-inflammatories was initiated. After 2 days, respiratory distress suddenly worsened. Tracheoscopy showed a discontinuity between the tracheal rings of the cervical trachea; however, the inner tracheal wall appeared intact. Computed tomography scan revealed a ~3-cm complete rupture of all layers of the trachea. Surgical resection and anastomosis of the trachea were performed successfully. Follow-up 15 days after surgery showed complete resolution of respiratory signs, as well as subcutaneous emphysema. A mild ventral angulation of the trachea at the surgical site was noticed on thoracic radiographs.
This is the first case report of a pseudotrachea in a dog. Persistence of a pseudotrachea may initially result in only minor clinical signs responsive to medical therapy despite tracheal rupture. In the presence of a pseudotrachea, tracheal rupture may be difficult to identify with tracheoscopy alone. Therefore, CT scan should be proposed in every patient with suspected tracheal trauma.
Key clinical message:
This case report highlights the importance of including a tracheal rupture in the differential diagnosis of cervical subcutaneous emphysema, even if the amount is small and not associated with significant respiratory signs. The presence of a pseudotrachea may result in less severe clinical signs than expected based on the actual degree of tracheal injury; however, the clinical status may rapidly deteriorate and become life-threatening.
This case report also underlines the importance of a CT scan as a complement to tracheoscopy, which may not be sufficient to identify a tracheal rupture in the presence of a pseudotrachea.
Résumé
Rupture trachéale cervicale avec persistance d’une pseudotrachée chez un chien. Un chien a été présenté pour une dyspnée aiguë modérée consécutive à des morsures cervicales par un autre chien. L’examen clinique révéla une plaie cervicale ventrale profonde associée à un emphysème sous-cutané localisé léger. Les radiographies thoraciques ont montré un pneumomédiastin modéré. Un traitement médical consistant en une oxygénothérapie, des antibiotiques et des anti-inflammatoires a été initié. Après deux jours, la dyspnée s’aggrava brutalement. Une trachéoscopie révéla une discontinuité entre les anneaux trachéaux malgré la persistance d’une paroi trachéale interne intègre. L’examen par tomodensitométrie montra une rupture trachéale cervicale complète dans toute son épaisseur, sur 3 cm de long. Une chirurgie de résection-anastomose de la trachée a été réalisée avec succès.
Il s’agit de la première description de pseudotrachée chez un chien. La persistance d’une pseudotrachée peut initialement ne provoquer que des signes cliniques mineurs, notamment un emphysème sous-cutané léger et une dyspnée répondant au traitement médical, malgré une lésion trachéale en réalité importante. Par conséquent, un examen par tomodensitométrie de la trachée doit être envisagé chez tous les patients pour lesquels un traumatisme trachéal est suspecté.
Message clinique clé :
Ce cas souligne l’importance d’inclure une rupture trachéale dans le diagnostic différentiel de l’emphysème souscutané cervical, et cela même s’il n’est présent qu’en petite quantité et associé à faibles signes cliniques respiratoires. La persistance d’une pseudotrachée peut entraîner des signes cliniques moins importants qu’une rupture trachéale complète, cependant l’état respiratoire de l’animal peut rapidement s’aggraver et devenir une urgence vitale.
Ce cas souligne de plus l’importance de l’examen par tomodensitométrie en complément de la trachéoscopie, qui peut parfois s’avérer insuffisante pour le diagnostic des ruptures trachéales, en particulier en présence d’une pseudotrachée.
(Traduit par les auteurs)
Several types of traumatic tracheal injuries, ranging from small lacerations to complete tracheal rupture, have been reported in the literature (1–12). Tracheal rupture has been identified in the cervical and thoracic trachea and is considered uncommon in small animals. Dog bites and motor vehicle accidents are the most common causes of tracheal rupture in dogs (1,5,11,13).
Complete tracheal rupture is life-threatening and is characterized by acute onset of respiratory signs including respiratory distress and stridor (2–8,9,10). Generalized subcutaneous emphysema and pneumomediastinum are usually associated with tracheal rupture (1,5,9). However, smaller tears may result in minor clinical signs which typically resolve with medical treatment (4,11).
Surgical and medical management of tracheal injuries has been described (2–9,10,12,14,15) with options dependent upon the extent of the lesion, the severity and the progression of the associated clinical signs. Medical management typically consists of oxygen therapy, sedation, cage rest, as well as anti-inflammatory and antibiotic therapy. Surgical treatment, such as resection and anastomosis, is recommended for patients with extensive tracheal lesions associated with severe clinical signs (1–3,5,7,8,12,16). Animals with tracheal rupture may only show mild clinical signs at initial presentation with acute deterioration occurring several days later (1,2,12,15). The reasons for this deterioration remain unclear. Some authors (1,2,11) hypothesize that the presence of a pseudotrachea, which later ruptures, could explain this clinical course.
Pseudotrachea has been defined as a persistent structure providing the continuity of the trachea in cases of tracheal rupture, leading to less severe clinical signs than would be expected based on the extent of the tracheal injury (1,3,6,10,17).
In cats, pseudotrachea has been described as a persistence of the external layer, i.e., adventitia, of the trachea in cases of rupture of the extra-thoracic trachea; or as inflammatory tissue of the mediastinum in cases of avulsion of the intra-thoracic trachea (1–3,6,17). To the authors’ knowledge, this is the first report of a pseudotrachea in a dog with tracheal rupture.
Case description
A 7-year-old male French bulldog presented to the emergency department of the National Veterinary School of Toulouse for respiratory distress and stridor, as well as multiple bite wounds after being attacked by another dog a few hours earlier. The animal’s only known history was a moderate brachycephalic syndrome.
Initial physical examination revealed tachypnea at 48 breaths/min, moderate respiratory distress, and inspiratory stridor. The animal had multiple superficial wounds over its entire body and a small but deep ventral cervical wound associated with localized mild subcutaneous emphysema. The remainder of the physical examination was unremarkable. Initial diagnostic tests, including pulse oximetry (applied to the lip), microhematocrit, total protein, blood glucose, lactates, non-invasive arterial blood pressure measurement (Doppler; Parks Medical Electronics, Aloha, Oregon, USA), abdominal and thoracic Focused Assessment with Sonography in Trauma (FAST) ultrasound did not reveal any abnormalities. A complete serum biochemistry profile showed no abnormalities. Complete blood (cell) count (CBC) and blood cell differential examination revealed a leukocyte count within the reference interval [10.65 × 109/L WBC, reference interval (RI): 5.05 to 16.76 × 109/L] with a left shift and presence of toxic neutrophils on the blood smear.
Initial management consisted of oxygen therapy via unilateral nasopharyngeal tube (1.5 L/min), intravenous fluids (Ringer Lactate; B. Braun, Melsungen, Germany), antibiotic therapy with ampicillin-sulbactam (UNACIM; Pfizer, New York, USA), 20 mg/kg, IV, q8h, and anti-inflammatory treatment with meloxicam (METACAM; Boehringer Ingelheim, Ingelheim am Rhein, Germany), 0.2 mg/kg, IV, q24h. Intravenous injections of butorphanol (BUTADOR; Boehringer Ingelheim), 0.2 mg/kg were administrated as needed to sedate the patient and prevent agitation that would lead to worsening of respiratory status.
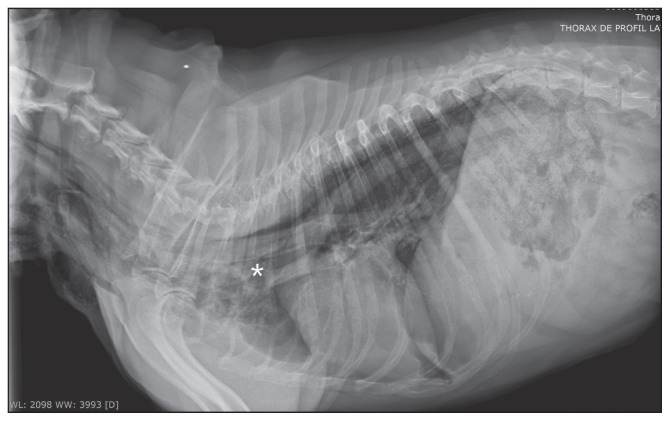
After initial stabilization, 3-view thoracic radiographs were taken, which showed moderate pneumomediastinum and moderate subcutaneous emphysema in the cervical area (Figure 1). These findings were suggestive of a perforation of the trachea or esophagus. Entry of air through the deep cervical bite wound had to be considered as well.
Figure 1.
Right-lateral radiographic image of the thorax 5 h after initial presentation. Heterogeneous radiolucent appearance of the cranial aspect of the mediastinum, and increased visualization of the walls of the esophagus, trachea, and great vessels, indicating a pneumomediastinum. Presence of moderate ventral cervical subcutaneous emphysema.
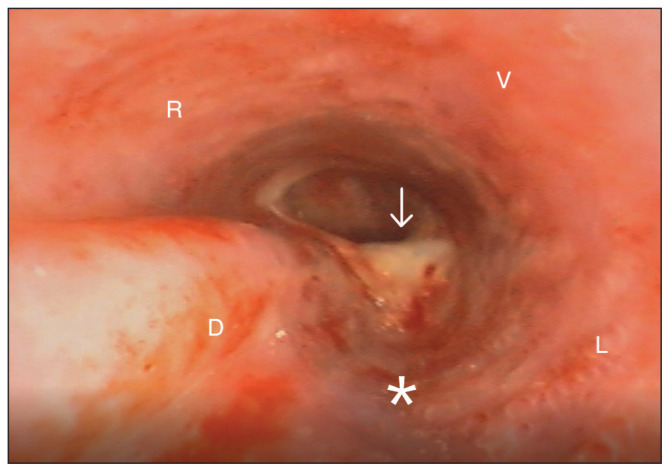
Since the respiratory status of the dog remained stable for 48 h and the subcutaneous emphysema did not worsen, medical management was continued. Oxygen therapy was discontinued 24 h after presentation. Two days after initial presentation, the dog developed acute inspiratory distress, associated with marked inspiratory stridor, a respiratory rate of 120 breaths/min, and discrete worsening of the subcutaneous emphysema. Pulse oximetry (applied to the lip) remained at 100% oxygen. The decision to perform a tracheoscopy (bronchoscope, Olympus BF-P190; Olympus, Shinjuku, Japan) was made to evaluate the integrity of the trachea and esophagus. After premedication with acepromazine (CALMIVET; Vétoquinol, Magny-Vernois, France), 15 μg/kg, IV and butorphanol (BUTADOR; Boehringer Ingelheim), 0.4 mg/kg, IV, the dog was anesthetized with propofol IV (PROPOVET; Zoetis, Parsippany-Troy Hills, USA) given to effect with a total dose of 25 mg/kg over 90 min. Endotracheal intubation was not performed; oxygen therapy was provided through bilateral nasal tubes. Esophagoscopy revealed no abnormalites. Tracheoscopy revealed edema of the arytenoid cartilages and altered motion of the laryngeal folds suggestive of laryngeal paresis. The proximal third of the tracheal wall was severely hyperemic, and a substantial amount of serohemorrhagic secretion was present within the tracheal lumen. An irregular depression of the dorsal tracheal wall approximately 1 cm in length with protrusion of fatty tissue, presumably representing a small tracheal perforation, was identified about 10 cm caudal to the larynx (Figure 2). Further caudally the tracheal path abruptly deviated dorsally, and the tracheal mucosa showed hemorrhagic and necrotic lesions. These findings were highly suggestive of a rupture between the tracheal rings, with persistence of at least the mucosal inner layer of the trachea. A focal breach of the mucosal layer with protrusion of cervical fatty tissue into the tracheal lumen was suspected. The proximal third of the trachea down to the bifurcation of the main stem bronchi was normal.
Figure 2.
Endoscopic image of the trachea. Significant tracheal inflammation (asterisk) and a small amount of what appeared to be fatty tissue attached to the tracheal wall (arrow), suggesting a tracheal perforation. Just caudally to this lesion, an abrupt dorsal deviation of the trachea is seen, consistent with disjunction of the tracheal rings. D — Dorsal; V — Ventral; R — Right; L — Left.
During recovery from anesthesia, the dog developed severe respiratory distress associated with a drop in oxygen saturation to below 80% (normal reference range: 93 to 100%). An emergency endotracheal intubation was initiated using an endotracheal tube of a smaller diameter than the dog’s trachea (5.5 mm), while paying close attention not to exacerbate the tracheal lesions. Anesthesia was maintained with 2% isoflurane, and the dog was manually ventilated at inspiratory pressures less than 10 cm H2O until the oxygen saturation stabilized above 95%.
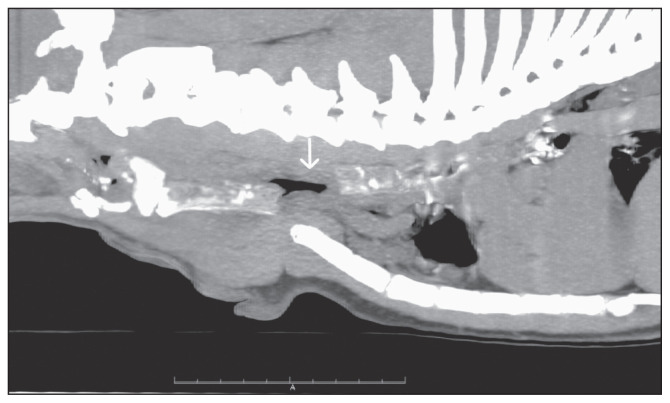
In order to better assess the type, extent, and location of the tracheal anomalies visualized on tracheoscopy, and to identify the cause for the sudden deterioration in respiratory status post-tracheoscopy, a cervical and thoracic computed tomography (CT) scan (GE BrightSpeed, 16-slice helical system; General Electric Healthcare, Medical Systems, Boston, USA), slice thickness 1.25 mm, rotation speed 0.6 s, helical pitch of 0.53, matrix 512 × 512) was performed. During the CT scan, the dog was in sternal recumbency and maintained under a constant rate perfusion of dexmedetomidine (0.5 μg/kg per hour). The dog was not intubated.
The CT scan revealed a 3-cm complete rupture of the caudal cervical trachea (Figure 3) involving all layers of the trachea, associated with local pneumomediastinum and subcutaneous emphysema.
Figure 3.
Sagittal computed tomographic image of the thorax, helical acquisition, tissue window without contrast injection. Discontinuity of 3 cm in the ventral and dorsal wall of the caudal cervical trachea (arrow), just cranially to the thoracic inlet.
Following the CT scan, resection and anastomosis surgery of the trachea was performed using a cervical ventral approach and a split-cartilage technique, without complication. Tracheal ends were anastomosed with 3-0 monofilament absorbable sutures. Post-surgical management consisted of analgesia with Fentanyl (FENTADON; Eurovet, Dechra Veterinary Products, Bladel, The Netherlands), continuous rate infusion (CRI) of 2 μg/kg per hour, sedation with dexmedetomidine (CRI: 0.35 μg/kg per hour), antibiotic therapy with ampicillin-sulbactam (UNACIM; Pfizer), 20 mg/kg, IV, q6h, and anti-inflammatory therapy with prednisolone (DERMIPRED; Ceva, Paris, France), 0.4 mg/kg, PO, q24h to prevent cough and reduce tracheal inflammation. Recovery after surgery was uneventful.
Follow-up thoracic radiographs 2 d after surgery showed a marked reduction in the size of the pneumomediastinum and the subcutaneous emphysema. The dog was discharged from the hospital 5 d after surgery.
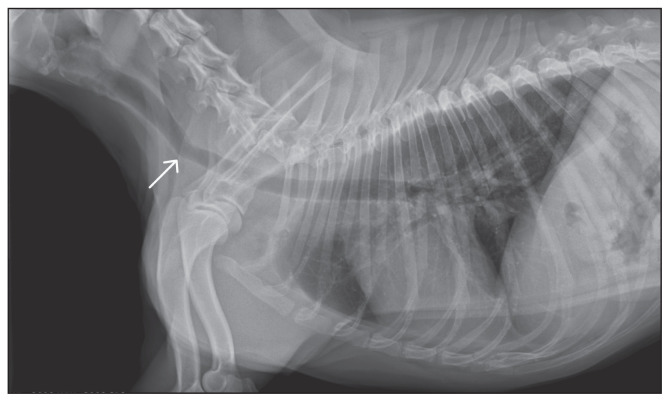
On recheck examination 2 wk after surgery, the dog was reported to be clinically normal. He had no respiratory signs, and the subcutaneous emphysema had completely resolved. Thoracic radiographs showed resolution of the pneumomediastinum; however, there was a moderate ventral deviation and mild stenosis of the trachea at the surgical site (Figure 4). Additional rechecks could not be performed because the dog was lost to follow-up.
Figure 4.
Right-lateral radiographic image of the thorax 14 d after surgery. Angulation (arrow) of the trachea in the caudal cervical region, corresponding to the resection/anastomosis site. Absence of previously noted subcutaneous emphysema.
Discussion
Tracheal rupture is an uncommon condition and has been reported less frequently in dogs than in cats (2,3,6,8,10,13,15). The main causes of tracheal rupture in dogs are bites or road traffic accidents (1,5), whereas iatrogenic causes such as endotracheal intubation are more common in cats (3,4).
Clinical signs reported in the literature are primarily respiratory in nature, including inspiratory distress of varying degrees and stridor. Respiratory symptoms may improve with sedation, especially in patients with minor tracheal injuries (4,11). Subcutaneous emphysema is typically present, and may be severe and generalized, or localized over the cervical region in cases of a small perforation of the cervical trachea (5). The dog reported in this case had moderate respiratory signs on initial examination, which improved markedly with sedation. Although the mild cervical subcutaneous emphysema may have been due to a tracheal rupture, an esophageal injury or penetration of air from the outside through the bite wound in the neck had to be considered as well. The pneumomediastinum could have developed due to tracheal or esophageal rupture, or secondary to air extension from the subcutaneous emphysema into the mediastinum. Tracheoscopy and esophagoscopy were therefore conducted to identify possible lesions. Although a tracheal perforation was suspected in this dog, clinical signs including moderate inspiratory distress responding to sedation and mild localized subcutaneous emphysema were suggestive of a small tracheal defect.
Given the findings on CT scan, which showed a complete rupture of the entire tracheal wall over several centimeters, more severe respiratory signs and subcutaneous emphysema would have been expected.
The authors hypothesize that the initial presence of a pseudotrachea allowed the airway to remain patent and therefore resulted in only mild to moderate clinical signs. This hypothesis is supported by the findings on tracheoscopy, which showed what appeared to be only a small rupture of the dorsal tracheal wall through which fatty tissue protruded. The remaining internal wall of the trachea was intact. However, a rupture between the tracheal rings manifested by the abnormal abrupt deviation of the trachea, and the irregularity of the tracheal diameter was suspected.
The dog developed acute and severe inspiratory distress following tracheoscopy, necessitating emergency endotracheal intubation. Possible causes for this acute inspiratory distress included laryngeal edema, worsening of an already existing brachycephalic syndrome, pulmonary atelectasis, or rupture of the pseudotrachea. The cause of the respiratory distress could not be identified definitively; however, signs improved markedly after endotracheal intubation.
The CT scan undertaken after tracheoscopy and following emergency endotracheal intubation revealed a complete rupture of the entire thickness of the tracheal wall. The authors suspect that the pseudotrachea ruptured post-tracheoscopy or during emergency endotracheal intubation even though tracheoscopy was performed by an experienced operator, and guidelines for endotracheal intubation of patients with tracheal injury, as described below, were strictly followed (2,10,15).
Pseudotrachea has been described in cats with an intrathoracic tracheal rupture following endotracheal intubation and is most often located just cranial to the carina. The pseudotrachea is described to be composed of tracheal adventitial tissue or mediastinal tissue (1,3,6,10,17). Thoracic radiographs may show an air-filled structure adjacent to the tracheal rupture which is called a diverticulum or a “balloon sign” (3,6,9). In the dog reported here, the focal subcutaneous emphysema masked the area around the tracheal rupture and may have prevented the visualization of this radiographic sign. Thoracic radiographs showed moderate pneumomediastinum (Figure 1), which has been reported in most cases of tracheal rupture (1,2,5,9,12).
Anesthetic management of dogs and cats with tracheal injuries can be challenging (2,6,10,15). If endotracheal intubation is necessary, it should be done using an endotracheal tube of a smaller diameter than that of the trachea. The balloon of the endotracheal tube should not be inflated and manual ventilation, but if it cannot be avoided, airway pressures should not exceed 10 cm H2O (6,8). In the dog herein, tracheoscopy and CT scan were completed without endotracheal intubation using intravenous anesthesia and sedation, respectively, with administration of oxygen via bilateral nasal tubes. Tracheoscopy (8,14) or CT scan (3,7,8,12) has been used to identify tracheal rupture in dogs and cats. In cases of severe tracheal trauma, tracheoscopy can aggravate the lesions and may not be recommended as a first-choice diagnostic test (5). In this case, the initial presentation did not suggest severe tracheal trauma, but a breach of the esophagus, although unlikely, could not be ruled out completely. Therefore, tracheoscopy and esophagoscopy were carried out early during examination.
A CT scan was performed following tracheoscopy to definitively diagnose the type and extent of the tracheal injury as previously reported in a case with an intrathoracic tracheal tear in a dog which also required CT scan in addition to tracheoscopy (12). In addition, given the clinical deterioration of the patient after the tracheoscopy, worsening of the tracheal injury had to be suspected and a second tracheoscopy couldn’t be considered.
Surgical and medical management of tracheal rupture have both been reported in the literature (2–8,10,12–15). The treatment decision is generally based on the severity of the clinical signs, the response to medical therapy, and the extent of the tracheal lesion. Medical management can be effective for small tracheal perforations that do not involve the tracheal rings (1,4). In a study of 20 cats with presumptive tracheal rupture caused by endotracheal intubation, 15 cats recovered completely with medical treatment consisting of oxygen therapy, sedation, and cage rest (4).
Surgical resection and anastomosis are recommended in patients with a large tracheal rupture. These procedures carry an excellent prognosis regardless of the location and extent of the rupture (2–6,8,12,14). Post-operative complications including suture dehiscence, infection or stenosis at the anastomosis site (1,8), dysphonia (5), self-resolving unilateral laryngeal paralysis (2), and rarely death (4) have been reported in the literature.
The dog reported here developed an asymptomatic focal stenosis and ventral angulation of the trachea at the surgical site identified on thoracic radiographs 14 d after surgery. This complication after resection and anastomosis of the trachea secondary to tracheal rupture has never been reported in the veterinary literature. However, cases of tracheal narrowing have been reported in dogs undergoing surgery for other causes (18,19). This is assumed to be a consequence of the healing process (20).
Follow-up radiographs are recommended in animals undergoing resection and anastomosis to evaluate for post-surgical tracheal stenosis even though this may be asymptomatic in mild cases as in the dog reported here.
To the authors’ knowledge this is the first report of a pseudotrachea after traumatic tracheal rupture in a dog. In the presence of a pseudotrachea, clinical signs may not be relied upon exclusively to assess the extent of the tracheal lesion.
Considering that a pseudotrachea can be present in the dog, a mild pneumomediastinum or a small amount of subcutaneous emphysema after possible tracheal trauma warrants further diagnostic evaluation of tracheal injuries.
In these dogs, tracheoscopy is of limited value in the assessment of tracheal rupture. A CT scan is therefore recommended in dogs with suspected tracheal trauma to optimize patient management and improve outcome. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Holt D. Tracheal trauma. In: Silverstein DC, Hopper K, editors. Small Animal Critical Care Medicine. 2nd ed. Ames, Iowa: Blackwell Publishing; 2014. pp. 107–110. [Google Scholar]
- 2.White RN, Burton CA. Surgical management of intrathoracic tracheal avulsion in cats: Long-term results in 9 consecutive cases. Vet Surg. 2000;29:430–435. doi: 10.1053/jvet.2000.9138. [DOI] [PubMed] [Google Scholar]
- 3.Moreau C, Blanchot D, Jacques D. Rupture trachéale intrathoracique chez un chat. Pratique médicale et chirurgicale de l’animal domestique. 2010;45:73–77. [Google Scholar]
- 4.Mitchell SL, McCarthy R, Rudloff E, Pernell RT. Tracheal rupture associated with intubation in cats: 20 cases (1996–1998) J Am Vet Med Assoc. 2000;216:1592–1595. doi: 10.2460/javma.2000.216.1592. [DOI] [PubMed] [Google Scholar]
- 5.Basdani E, Papazoglou LG, Patsikas MN, Kazakos GM, Adamama-Moraitou KK, Tsokataridis I. Upper airway injury in dogs secondary to trauma: 10 dogs (2000–2011) J Am Hosp Assoc. 2016;52:291–296. doi: 10.5326/JAAHA-MS-6067. [DOI] [PubMed] [Google Scholar]
- 6.Barletta M, Shaikh LS, Schmiedt CW, Secrest SA. Anesthesia case of the month. J Am Vet Med Assoc. 2015;247:488–491. doi: 10.2460/javma.247.5.488. [DOI] [PubMed] [Google Scholar]
- 7.Bhandal J, Kuzma A. Tracheal rupture in a cat: Diagnosis by computed tomography. Can Vet J. 2008;49:595–597. [PMC free article] [PubMed] [Google Scholar]
- 8.Morath U, Gendron K, Revés NV, Adami C. Perioperative and anesthetic management of complete tracheal rupture in one dog and one cat. J Am Anim Hosp Assoc. 2015;51:36–42. doi: 10.5326/JAAHA-MS-6022. [DOI] [PubMed] [Google Scholar]
- 9.Hayward N, Schwarz T, Weisse C. The trachea. In: Schwarz T, Johnson V, editors. BSAVA Manual of Canine and Feline Thoracic Imaging. Quedgeley, UK: British JSAP; 2008. pp. 213–227. [Google Scholar]
- 10.Griffiths LG, Sullivan M, Lerche P. Intrathoracic tracheal avulsion and pseudodiverticulum following pneumomediastinum in a cat. Vet Rec. 1998;142:693–696. doi: 10.1136/vr.142.25.693. [DOI] [PubMed] [Google Scholar]
- 11.Clarke DL. Tracheobronchial injury and collapse. In: Drobatz KJ, Hopper K, Rozanski EA, Silvertein DC, editors. Textbook of Small Animal Emergency Medicine. Ames, Iowa: Blackwell Publishing; 2018. pp. 196–205. [Google Scholar]
- 12.Dancer SC, Van der zee J, Kirkberger RM. Computed tomographic findings in a bluetick coonhound with a longitudinal thoracic tracheal tear. Vet Radiol Ultrasound. 2020;61:E12–E16. doi: 10.1111/vru.12607. [DOI] [PubMed] [Google Scholar]
- 13.Halfacree ZJ, Tivers MS, Jordan CJ. Airway injury associated with cervical bite wounds in dogs and cats: 56 cases. Vet Comp Orthop Traumatol. 2013;26:89–93. doi: 10.3415/VCOT-12-01-0013. [DOI] [PubMed] [Google Scholar]
- 14.Nikahval B, Foroud M, Raayat Jahromi A, Ahrari-Khafi MS. Generalized subcutaneous emphysema caused by concurrent cricoid cartilage fracture and cricotracheal detachment in a German Shepherd dog. Iran J Vet Res. 2015;16:226–228. [PMC free article] [PubMed] [Google Scholar]
- 15.White RN, Milner HR. Intrathoracic tracheal avulsion in three cats. J Small Anim Pract. 1995;36:343–347. doi: 10.1111/j.1748-5827.1995.tb02945.x. [DOI] [PubMed] [Google Scholar]
- 16.Sura P, Durant A. Trachea and bronchi. In: Tobias KM, Johnston SA, editors. Veterinary Surgery Small Animal. Vol. 2. St. Louis, Missouri: Saunders, Elsevier; 2012. pp. 1734–1751. [Google Scholar]
- 17.Sparkes A. Tracheal disease. In: Norsworthy GD, Restine LM, editors. The Feline Patient. 5th ed. Hoboken, New Jersey: John Wiley & Sons; 2018. pp. 635–641. [Google Scholar]
- 18.Lau RE, Schwarz A, Buergelt CD. Tracheal resection and anastomosis in dogs. J Am Vet Med Assoc. 1980;176:134–139. [PubMed] [Google Scholar]
- 19.Hedlund CS. Tracheal resection and reconstruction. Probl Vet Med. 1991;3:210–228. [PubMed] [Google Scholar]
- 20.Tobias KM. Manual of Small Animal Soft Tissue Surgery Hoboken. New Jersey: Wiley-Blackwell; 2011. pp. 1734–1751. [Google Scholar]