Abstract
Objective:
Knee osteoarthritis (KOA) is the most common degenerative disease of the joints caused by articular cartilage injury, degeneration of joint edges and hyperplasia of subchondral bone. The purpose of this study is to investigate the efficacy and safety of clinical therapy of platelet-rich plasma vs hyaluronic acid injections in patients with KOA.
Methods:
We systematically investigated Pubmed, Embase, and the Cochrane Library for all related articles published through May 2020. Any study was included that compared the effect of platelet-rich plasma (PRP) and hyaluronic acid (HA) in patients with KOA. The search terms included “platelet-rich plasma,” “PRP,” “hyaluronic acid,” “HA,” “knee,” “osteoarthritis,” “arthritis,” “KOA”. Review Manager 5.3 was used to analyze and calculate data regarding these outcome indicators.
Results:
In this study,
-
1.
Six randomized double-blind controlled trials were included, including 338 patients in the PRP group and 323 patients in the HA group.
-
2.
Meta-analysis results showed that the Western Ontario and MacMaster Universities Osteoarthritis Index (WOMAC) Total Score was differed significantly between the PRP and HA groups at the 1, 6, 12 months follow-up (MD = 3.39, 95% CI: 2.85–3.92, P < .05). In a comparison of Physical function scores at the 12 months follow-up, PRP improved knee function scores more than HA (MD = 3.28; 95% CI: 2.13–4.43; P < .05). However, International Knee Documentation Committee (IKDC), Tegner Activity scores, EuroQol visual analogue scale (EQ-VAS), and Adverse Events (AEs) were all not significantly different (P > .05).
-
3.
Results showed that compared with HA, PRP had significant advantages in relevant improving knee function and quality of life.
Conclusion:
In improving knee function and quality of life, PRP showed superiority over HA in long-term follow-up from well-designed double-blind trials, but a large number of high-quality multi-center studies are still needed to provide more sufficient evidence.
Keywords: hyaluronic acid, knee osteoarthritis, meta-analysis, platelet-rich plasma, systematic review
1. Introduction
Knee osteoarthritis (KOA) is a very common chronic degenerative disease, and its characterized by varying degrees of cartilage degeneration, cartilage exfoliation, and subchondral bone hyperplasia.[1] In addition, the degeneration of cartilage is mainly manifested with pain, stiffness, swelling, restriction of joint motion.[2] Moreover, this disease has a significantly impact on patient's quality of life and loss of function, and it has become the most common public health issue in the elderly.[3] According to the Osteoarthritis Society International, non-surgical treatment rather than surgery as the first recommendation therapeutics for KOA. Non-surgical treatment includes oral anti-inflammatory drugs, exercise, physical therapy, and intra-articular injections, depending on the severity and compliance of articular cartilage.[4] The relevant literatures report[5–6] that its can relieve pain symptoms and improve joint function in patients with KOA, which emphasizes the importance of conservative therapeutics in the treatment of KOA.
Although the above non-surgical therapies are beneficial to a certain degree of arthritis, there are no non-surgical or surgical interventions proven to alter the process of degenerative joint.[7] In recent years, platelet-rich plasma (PRP) or hyaluronic acid (HA) are the most extensive applications for intra-articular injection in alleviating pain and improving function.[8] However, a recent systematic review could not recommend the use of HA, which remains a matter of debate for effectiveness of hyaluronic acid.[9] Compared to HA, many systematic reviews suggest that injection of PRP can reduce inflammatory factors and synovial fluid in an arthritic joint. Moreover, several studies have shown PRP injections represent an effective and safe therapy, without increased risk of adverse events (AEs) in the treatment of osteoarthritis of the knee.[10] PRP is described as an autologous blood product, including multiple growth factors and concentration of platelets. It had been used to treat different degeneration diseases, which included the bone, cartilage, and soft tissues injury. In some randomized prospective studies, anti-inflammatory and tissue regeneration effects of PRP on joint cartilage, tissues recovery have been shown, especially treatment option in mild to moderate stage KOA.[11–12]
There exist considerable controversy with regard to the application of PRP or HA injections. Many studies have focused on the comparion of PRP with HA for KOA to determine which was more effective, and have not achieved consensus in terms of their mechanisms.[13] In some experimental studies comparing the effective of proliferation and differentiation of cartilage cells in PRP and HA treatment have shown that PRP can significantly improve cell mobility, but there is no systematically evidence-based demonstrate any advantage when compared with HA. Therefore, the aim of this study is to investigate the efficacy and safety of intra-articular injection of PRP compared with HA. A large sample of clinical studies will be conducted in the future to providing an evidence-based clinical guidance for the treatment of KOA. At the same time, we hope to strengthen the health education for the elderly, especially for the patients with knee osteoarthritis, and develop good living habits, to reduce the incidence of osteoarthritis.
2. Materials and methods
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement criteria, we performed strictly a prospective protocol to ensure a more precise conclusion could be made and accepted as a means to guide decision.
2.1. Search strategy
To identify all possible articles, Pubmed, Cochrane library, Embase, and Medline were investigated until May 2020 according to the Cochrane Collaboration guidelines. The following keywords were used in the search “platelet-rich plasma” or “PRP” and “hyaluronic acid” or “HA” and “knee osteoarthritis” or “KOA” or “knee” or “osteoarthritis” or “arthritis”. No language exclusions were applied. Two reviewers independently assessed the identified articles according to the title and abstract. They resolved any disagreement through discussion.
2.2. Inclusion and exclusion criteria
Studies were included based on the following inclusion criteria
-
1.
double-blind randomized clinical study with knee osteoarthritis and
-
2.
compared platelet-rich plasma and hyaluronic acid alone.
Exclusion criteria were
-
1.
retrospective and nonrandomized studies and
-
2.
unable to obtain results and relevant data.
2.3. Outcome measures
The primary important outcome were the Western Ontario and MacMaster Universities Osteoarthritis Index (WOMAC), Physical function scores. The secondary outcomes were the International Knee Documentation Committee (IKDC), EuroQol visual analogue scale (EQ-VAS), Tegner Activity scores, and AEs.
2.4. Quality assessment
According to the Cochrane Collaboration “Risk of bias,” we assessed the quality of the studies using the following 8 items: adequate sequence generation, allocation concealment, blinding of participants, blinding of investigators, blinding of assessors, incomplete outcome data inexistent or addressed, free of selective reporting, and free of other bias. The 2 reviewers independently assessed each study and determined whether there was a high, low, or uncertain risk of bias. A third reviewer resolved any disagreements when consensus was insufficient to do so.
2.5. Data extraction
Two reviewers independently extracted the general data in this study, including author, year, sample size, PRP or HA interventions, patient age, sex, and body mass index (BMI), and follow-up periods, radiographic classification, and clinical items such as WOMAC, Physical function, IKDC, EQ-VAS and Tegner scores, and AEs. If the relevant data had not been reported, the authors may be contacted by email or in other means to try to obtain the missing contents.
2.6. Statistic analysis
All included data were analyzed using the Review Manager 5.3 software, with risk ratios and 95% confidence intervals being determined for binary variables. The relative risk (RR) was used to evaluate the effects of binary variables, the effect size was calculated with mean difference (MD) when the same outcome was measured by the same scale at the end of intervention. In addition, for homogeneous data sets, I2 < 50% were used as the test standards. When the above statistical conditions were met, a fixed-effects model was used for the meta-analysis because the pooled effect sizes were relatively homogenous. If the above standards did not conform, the homogeneity of the pooled effect size was not ideal, and a random effects model was applied. P < .05 would be considered statistically significant.[14]
2.7. Grading the quality of evidence
The grading of recommendations assessment, development, and evaluation (GRADE) method was used to evaluate the quality of meta-analysis. Levels of quality of evidence were defined as high, moderate, low, and very low. All operations are on this page: https://gradepro.org/.
3. Results
3.1. Literature search and study characteristics
A total of 1056 potential studies were identified with the first search strategy. The titles of 698 studies were investigated, and 695 studies were not related to this topic and were excluded. Of these, 43 studies were included according to the eligibility criteria, and 6 studies[15–20] were selected in final quality assessment and data extraction. The process of selection and inclusion studies are shown in Figure 1. Analysing the basic characteristics of the included studies, all studies clearly stated that they were double-blind randomized clinical study, for a total of 661 patients (338 participants in PRP group and 323 participants in HA group). The ratio of patients included in the study was 1:1. The studies that were included had been conducted from 2012 through 2019 years. It was found that the ages were mainly in the 45 to 65 years range, the Kellgrenand Lawrence grading scale grading scale was I to IV, and the follow-up period was 6 to 24 months. In the 6 studies, baseline materials of the patients were comparable, both P > .05. The features of the 6 studies that were included are shown in Table 1.
Figure 1.
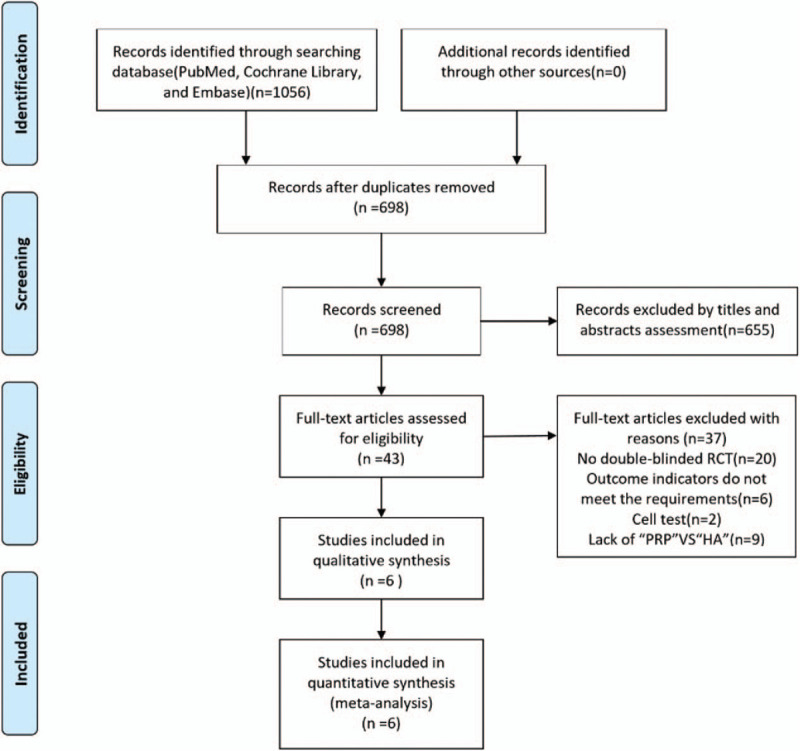
Flow diagram of study selection.
Table 1.
Characteristics of the included studies.
| Author (Year) | Study | Sex (M/F) | Age, Mean (SD) | Groups and interventions | BMI (kg/m2) | K–L Grade | Clinical outcomes | Follow-up |
| Kuan–Yu Lin 2019 | DB-RCT | 29/58 | PRP:61.17 (13.08); HA: 62.53 (9.9); NS: 62.23 (11.71) | PRP:31;HA:29;NS:27 | PRP:23.98 (2.62); HA:26.26 (2.99); NS: 24.98 (3.12) | I,II,III | WOMAC, IKDC | 12 mo |
| Wen-xing Yu 2018 | DB-RCT | 148/140 | PRP+HA:46.5 (7.5); PRP: 46.2 (8.6); HA:51.5 (9.3) | PRP+HA:96;PRP:104;HA:88 | NC | I,II,III,IV | WOMAC, Physical function, AEs | 12 mo |
| Ke Su 2018 | DB-RCT | 33/49 | PRPA:50.67 (8.70); PRPB:54.16 (6.56); HA:53.13 (6.41) | PRPA:27;PRPB:25;HA:30 | PRPA:28.19 (1.31); PRPB:28.17 (1.43); HA:28.69 (1.13) | II,III | WOMAC, Physical function, VAS, AEs | 18 mo |
| Gökay Görmeli 2015 | DB-RCT | 72/90 | PRP3:53.7 (13.1); PRP1:53.8 (13.4); HA:53.5 (14); NS:52.8 (12.8) | PRP3:39;PRP1:44;HA:39; NS:40 | PRP3:28.7 (4.8); PRP1:28.4 (4.4); HA:29.7 (3.7); NS:29.5 (3.2) | I,II,III,IV | EQ-VAS, IKDC | 6 mo |
| Di Martino 2019 | DB-RCT | 100/67 | PRP:52.7 (13.2); HA:57.5 (11.7) | PRP:85;HA:82 | PRP:27.2 (7.6); HA:26.8 (4.3) | PRP:2.0 (1.1); HA:2.0 (1.0) | EQ-VAS,IKDC, Tegner, AEs | 24 mo |
| Giuseppe Filardo 2012 | DB-RCT | 68/41 | PRP:55;HA:58 | PRP:54;HA:55 | PRP:27;HA:26 | PRP:2.2; HA:2.1 | IKDC, Tegner | 12 mo |
AE = adverse events, BMI = body mass index, DB-RCT = double-blind randomized control trial, EQ-VAS = EuroQol visual analogue scale, HA = hyaluronic acid, IKDC = International Knee Documentation Committee, K-L = Kellgrenand Lawrence grading scale, NC = not clear, NS = normal saline, PRP = platelet-rich plasma, Tegner = Tegner Activity Score, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index score.
3.2. Quality assessment
All included studies were double-blind randomized controlled trials.[15–20] However, there were no detailed descriptions on other biases. In 2 of the trials, there was incomplete outcome data provided with respect to participant or personnel information, resulting in a high risk of performance bias.[18–20] In total, 4 trails lost some patients during follow-up.[15,17–19] All the results of the quality assessment are shown in Figures 2 and 3.
Figure 2.
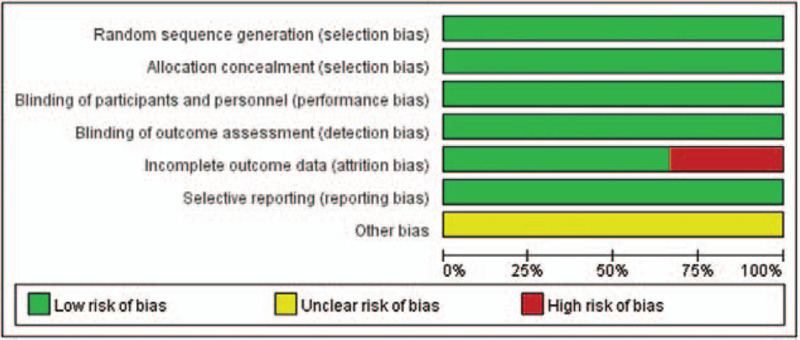
Risk of bias assessment.
Figure 3.
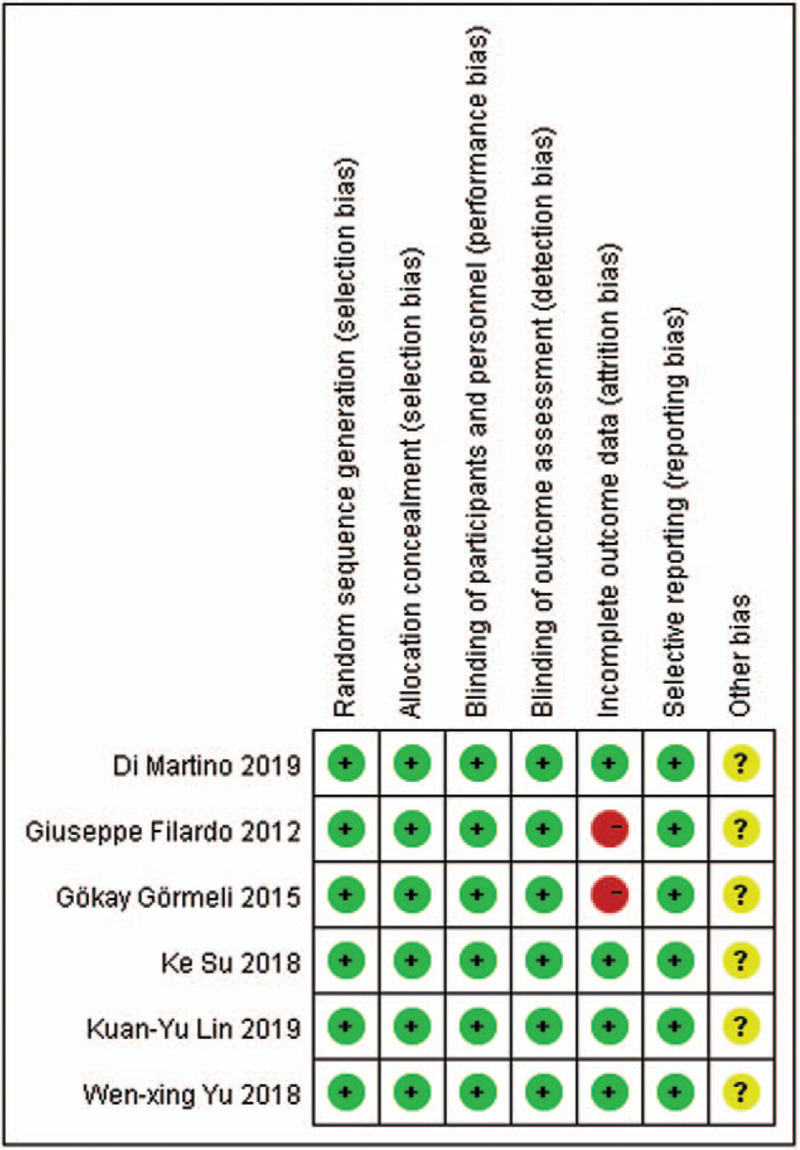
Risk of bias summary.
3.3. GRADE level of evidence
The GRADE level of evidence was low for each outcome. As shown in Table 2, the main reasons for a reducing level were high heterogeneity and possible publication bias.
Table 2.
Grading the quality of evidence.
| Certainty assessment | No of patients | Effect | ||||||||||
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | exercise group | control group | Relative (95% CI) | Absolute (95% CI) | Certainty | Importance |
| Physical function total score | ||||||||||||
| 2 | randomized trials | not serious | not serious | not serious | serious | publication bias strongly suspected† | 129 | 118 | – | MD 3.28 higher (2.13 higher to 4.43 higher) |

|
CRITICAL |
| EQ-VAS score | ||||||||||||
| 2 | randomized trials | not serious | not serious | not serious | serious∗ | publication bias strongly suspected† | 124 | 121 | – | MD 6.26 higher (2.76 lower to 15.27 higher) |

|
IMPORTANT |
| Tegner Activity score | ||||||||||||
| 2 | randomized trials | not serious | not serious | not serious | serious∗ | publication bias strongly suspected† | 139 | 137 | – | MD 0.1 higher (0.23 lower to 0.43 higher) |

|
IMPORTANT |
| adverse events score | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | serious∗ | publication bias strongly suspected† | 36/214 (16.8%) | 37/200 (18.5%) | RR 0.88 (0.60 to 1.29) | 22 fewer per 1000 (from 74 fewer to 54 more) |

|
IMPORTANT |
| WOMAC total score | ||||||||||||
| 3 | randomised trials | not serious | not serious | not serious | serious | publication bias strongly suspected† | 272 | 265 | – | MD 3.39 higher (2.85 higher to 3.92 higher) |

|
CRITICAL |
| IKDC score | ||||||||||||
| 4 | randomized trials | not serious | not serious | not serious | serious∗ | publication bias strongly suspected† | 379 | 373 | – | MD 3.73 higher (0.95 lower to 8.41 higher) |

|
IMPORTANT |
Statistical heterogeneity.
Potential publication bias.
CI = confidence interval, MD = mean difference.
4. Outcomes of the meta-analysis
4.1. WOMAC total scores
A total of 2 studies[15,17] reported WOMAC Total scores at 1 month after treatment. The heterogeneity test indicated that the homogeneity was good (I2 = 0%, MD = 1.33, 95% CI: 0.43–2.23, P = .004 < .05); 2 studies[15,17] reported WOMAC total scores at 6 months after treatment. The heterogeneity test indicated heterogeneity (I2 = 0%, MD = 4.79, 95% CI: 4.00–5.59, P < .05); 3 studies[15–17] reported WOMAC Total scores at 12 months after treatment. The heterogeneity test suggested a low degree of homogeneity (I2 = 0%, MD = 3.85, 95% CI: 2.66–5.04, P < .05). A fixed-effects model was used for meta-analysis. The subgroup analysis results showed that the WOMAC Total Score of the group receiving PRP compared with HA was statistically significantly different at 1, 6, 12 months after treatment. (Fig. 4).
Figure 4.
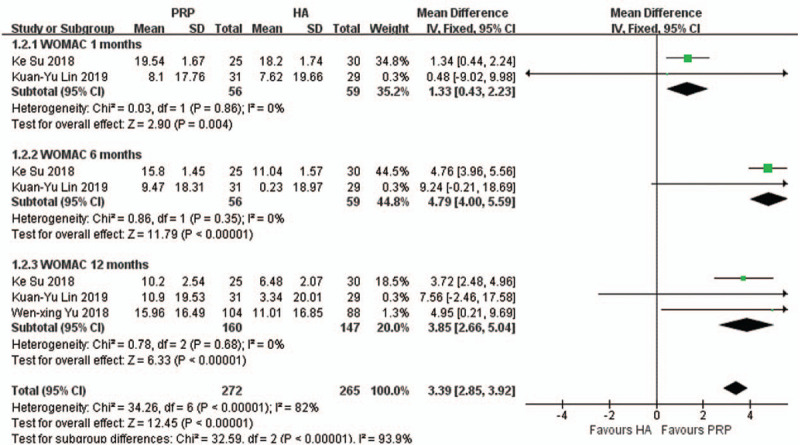
Forest plot and meta-analysis of WOMAC Total score (1, 6, and 12 months).
4.2. WOMAC physical function total score
A total of 2 studies[15,16] reported comparisons of the WOMAC Physical function Total Scores at 12 months after treatment. The heterogeneity test indicated that the homogeneity was good (I2 = 0%), and a fixed-effects model was used for meta-analysis. There was significant difference between these 2 groups, and the results showed that the score improvements of PRP was better than HA (MD: 3.28, 95% CI: 2.13–4.43, P < .05) (Fig. 5).
Figure 5.
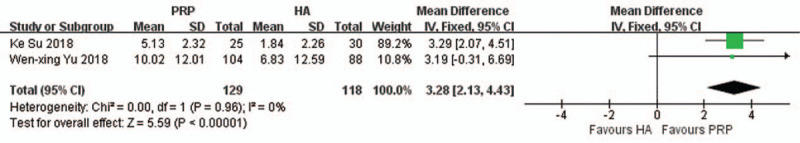
Forest plot and meta-analysis of Physical function total score (12 months).
4.3. IKDC score
Several studies[15,18–20] reported the subjective IKDC scores. The heterogeneity test suggested a high degree of homogeneity (I2 = 56%, 75%, 79%), and a random-effects model was used for meta-analysis. We can find that patients in the PRP group showed no significant difference in these scores than those in the HA group at 2 months (MD = −0.58, 95% CI: −5.78–4.62, P = .83), 6 months (MD = 6.51, 95% CI: −0.01–13.03; P = .05), and 12 months (MD = 5.72, 95% CI: −5.16–16.59, P = .30) (Fig. 6).
Figure 6.
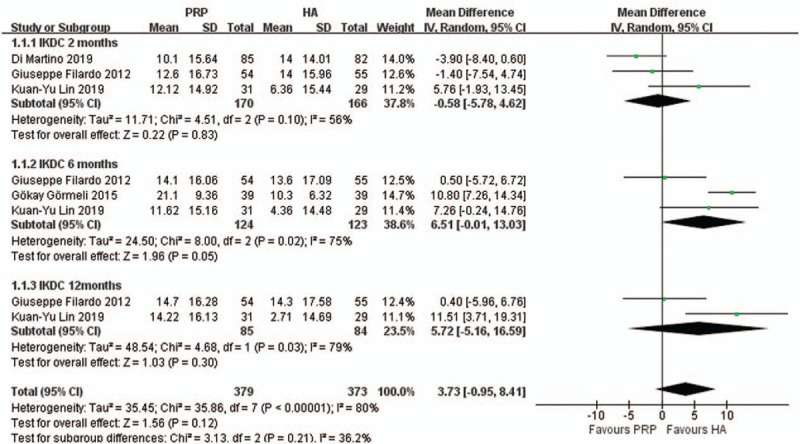
Forest plot and meta-analysis of IKDC score (2, 6, and 12 months).
4.4. EQ-VAS score
Two studies[18,19] reported the EQ-VAS at 6 months after treatment. The heterogeneity test suggested a high degree of homogeneity (I2 = 91%), and a random-effects model was used for meta-analysis. There was no significant difference between these 2 groups, and the results demonstrated that the PRP injections and HA injections were similar in treatment KOA (MD = 6.26, 95% CI: −2.76–15.27, P = .17) (Fig. 7).
Figure 7.
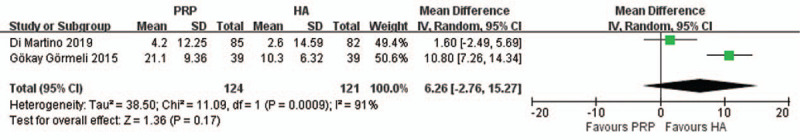
Forest plot and meta-analysis of EQ-VAS score (6 months).
4.5. Tegner activity score
Tegner Activity Score was reported in 2 studies[19,20] and showed that recovery of patients treated with PRP injections and HA injections had no significant difference after treatment (MD = −0.10, 95% CI: −0.23–0.43, P = .55, I2 = 0%). However, there was no a significant of heterogeneity, and a fixed-effects model was used for meta-analysis. (Fig. 8)
Figure 8.
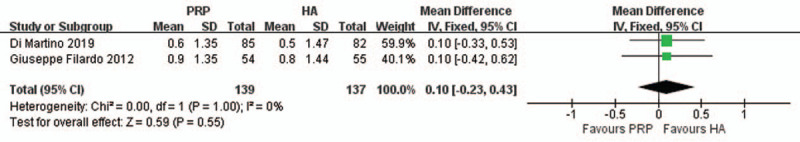
Forest plot and meta-analysis of Tegner Activity score.
4.6. Adverse events
Three studies[16,17,19] reported the comparison of AEs of PRP injections and HA injections on KOA. The heterogeneity test showed that the homogeneity was a low degree (I2 = 45%), and a fixed-effects model was used for meta-analysis. The results demonstrated no significant difference between PRP compared with HA (RR: 0.88, 95% CI: 0.60–1.29, P = .52), concluded that PRP and HA had similar safety profiles. The main types of adverse reactions were hypertension, diarrhea, vomiting, rash, proteinuria, fatigue, and worsening of pain and swelling, without serious adverse events reported. (Fig. 9)
Figure 9.
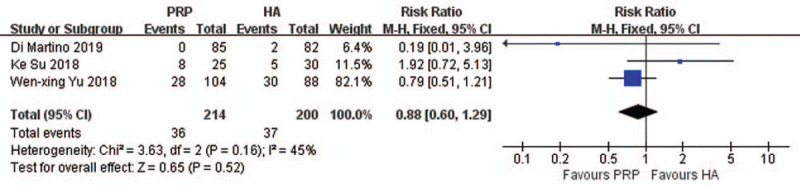
Forest plot and meta-analysis of adverse events score.
5. Discussion
Due to the increase in the average age of the active population, knee arthritis is the most common degenerative joint disorder in the elderly, which has a significant impact on society and economy. The main symptoms are pain and disability, which greatly reduces the quality of life of patients.[21] As a chronic degenerative joint disease, the incidence of KOA is increasing because of the increase in activities, ages, BMI, and trauma.[22] The etiology and pathogenesis of KOA are still not clear, and the main pathologic change is hyperosteogeny, articular cartilage degeneration and decrease of the number of cells in cartilage.[23] At present, there are many non-surgical and surgical treatments for KOA, which only relieve symptoms and improve the quality of life, but they can not completely cure the disease. Currently, non steroidal anti-inflammatory drugs are widely used in the treatment of knee osteoarthritis, and it has potential negative effects and lacks clear clinical efficacy data, which limits its application.[24] Therefore, finding a suitable treatment to relieve pain and improve the state of cartilage has been the focus and difficulty of clinical research.
Degeneration of articular cartilage is the fundamental reason for the development of KOA. The focus of current treatment is how to repair damaged cartilage and prevent further injury.[25] Relevant literature finds that growth factors play a decisive role in the expression of chondrocytes, such as transforming growth factorβ, platelet derived growth factor, insulin-like growth factors, and fibroblast growth factor, et al.[26] PRP is a kind of blood product with high concentration of platelets, leukocytes and a large number of growth factors, which can play an important role in stimulating cell proliferation and differentiation, promoting angiogenesis and accelerating tissue repair. PRP can be converted into a large number of collagen fibers, forming fibrin network scaffolds, which can maintain the number of platelets and ensure high growth factor in the knee joint.[12] At the same time, it comes from the patients themselves, does not have immune rejection and disease infection, and has a low degree of damage. It has become an important treatment for the KOA.[27] However, it takes a long time for PRP to promote cartilage regeneration and repair, and different amounts of leukocytes can be produced during PRP preparation, so PRP injection may aggravate the inflammatory response of knee joint.[28] Recently, HA injections have proven effective for maintaining adequate nutrition and characteristics for cartilage, lubricating joints to reduce and prevent inflammatory reactions, without increasing the risk of intra-articular infection, which can provide adequate nutrition for cartilage. With the passage of time, the decrease of the dosage in the joint cavity and the continuous disintegration of the joint matrix will reduce the clinical effect of HA.[29] As shown by previous studies, although they have been widely used and recognized in the treatment of KOA, there also exist considerable controversies with regard to the application of PRP injections and HA. Most of the previous studies have shown that PRP is superior to HA for patients with KOA.[30] PRP is an effective and safe alternative therapy for long-term pain relief and functional improvement in patients with KOA. However, the previous conclusions were reached on the basis of the inappropriate selection strategies, a limitation number of trials; Consequently, we hypothesized that PRP may influence pain and function better than HA as a ways of treating KOA, and as such, we performed a best-evidence synthesis of meta-analysis to ensure a more reliable conclusion.
To enhance the reliability of our conclusion, all of the studies we included in this meta-analysis were double-blind, randomized, and clinical trials. In this study, the primary outcome were the WOMAC, Physical function scores, and the secondary outcomes were IKDC, EQ-VAS, Tegner scores, AEs. This subgroups outcome showed PRP can reduce WOMAC scores more than HA for KOA at 1 month, 6 months, and 12 months after treatment. In terms of the improved Physical function score, PRP compared with HA, showed that there was no significant difference after treatment, which may suggest that PRP compared with HA may be a better treatment for patients with long-term knee joint pain and function improvement in the future. Ke et al[17] conducted an RCT investigating the effect of PRP injections and HA injections suggested that there were significant improvements, and PRP patients had significantly superior WOMAC and Physical function scores than were observed in HA, which showed PRP injections improve clinical outcomes more effectively than HA injections. From the results of IKDC scores, of the 6 studies comparing PRP with HA, 4 provided the IKDC score, it was found that there was no significant difference between PRP compared with HA for KOA at 2 month, 6 months, and 12 months after treatment. In terms of the improved EQ-VAS Score, PRP injections compared with HA, both can improve patients’ health-related quality of life, showed that there no significant difference between them after treatment. Görmeli et al[18] compared the effectiveness of PRP injections as well as HA injections in different stages of KOA, and found PRP injections was useful in achieving better clinical results for patients with early OA. The meta-analysis results showed that no significant difference was found in the Tegner scores and AEs, whether PRP or HA was applied for KOA, indicating that the side effects of the 2 treatments was not different. Alessandro et al[19] reported an RCT investigating of the adverse events and patient satisfaction of PRP injections and HA injections, few patients showed nausea, vomiting, and knee of pain and swelling, without serious adverse events reported, which indicated both treatments were safety in the treatment of KOA over time. In this meta-analysis, we included 6 studies, including the longest follow-up time of 1 article was 24 months, and the shortest follow-up time of 1 article was 6 months. Given the long follow-up period, this suggested that the results of meta-analysis were more reliable.
A large number of basic, preclinical and clinical studies have been carried out in the early stage, which showed that PRP was effective in the treatment of KOA. Platelet rich plasma can promote trauma, skeleton and muscles to repair, and have antibacterial properties, which contributes to prevent infection.[31] Raeissadat et al[32] reviewed the effects of PRP injection compared to HA for KOA in a one-year randomized clinical trial performed in 2014. The study showed that PRP led to significant pain score and SF-36 improvement in patients with poor quality of life, at the 12-month follow-up. Compared to HA, PRP was more efficacious and a therapeutic option in select patients with KOA. Similar results were obtained in a randomized prospective study. Kavadar et al[33] found the PRP was an effective and reliable treatment for functional status and pain in moderate knee osteoarthritis. In another study by Spakova et al[34] in 2012, 120 patients in 2 groups underwent PRP injections or HA injections and were followed up at 2, 6 months after the treatment. At the end of the follow-up, similar improvements were observed in WOMAC and Numeric Rating Scale scores in both groups, and no severe AEs were observed. However, there were no statistically meaningful differences advocating that PRP was better than HA in efficiency or safety for KOA. Although most of the previous clinical studies have shown that PRP was superior to HA for PRP injections in pain relief and functional improvement in patients with KOA. there was no consensus in terms of pain relief and function recovery, which was better, and lack of systematic evaluation of high quality trials.[35] The role of HA should not be underestimated in reducing pain and improving the viscoelasticity of synovial fluid, which was helpful to improve the viscoelasticity of the synovial fluid, reduce the inflammatory reaction, antioxidation and promote the synthesis and metabolism of cartilage. In previous years, there have been an increasing number of experimental studies on the mechanisms of PRP and HA for KOA, which have been discussed in depth and showed that PRP was more effective in improving cell mobility.[36]
5.1. Strengths and limitations
This study is the first systematic evaluation of high quality of the efficacy and safety of PRP compared with HA for KOA. A strengths of this investigation is that trails included are all randomized double-blinded design. The results of this study may have promising effects for the clinical application of PRP. Nevertheless, this quality of meta-analysis has some certain limitations. First, the number of included trials with double-blinded design was relatively small, which may increase the heterogeneity and affect our results. Second, the results of studies failed to directly compare the efficacy of the PRP injections and HA injections. Third, the sample size and indicators of the each study was insufficient, which had the potential to increase the significant heterogeneity. Lastly, a funnel plot could not be drawn to analyze the publication bias, and it weakened our ability to draw a precise conclusion.
6. Conclusions
Based on this systematic evaluation and meta-analysis, compared with HA injections, PRP injections can improve WOMAC Total Scores and Physical Function Scores. However, in terms of the incidence of IKDC, Tegner scores, EQ-VAS Scores, and AEs, PRP injections is not significantly different from HA injections, which makes our hypothesis appearing not to be confirmed. In future research, more long-term, multicenter, large sample sizes will be conducted to confirm the efficacy and safety of the PRP injections in relieving pain and function improvement. In general, the results need to be further verified by a larger high-qulity study at a later stage.
Author contributions
Hao Gong, Kaiming Li, and Rui Xie participated in the design of the study; Jinyu Gu, Jing Yin and Xiaozhou Hou carried out data curation; Ming Chen and Ping Wang performed the statistical analysis; Shangquan Wang and Guoqing Du carried out supervision; Hao Gong and Kaiming Li wrote the manuscript; Hao Gong and Rui Xie plotted the manuscript; Guoqing Du and Linghui Li revised the manuscript; All authors approved the final version of the manuscript.
Data curation: Jing Yin, Jinyu Gu, Xiaozhou Hou.
Formal analysis: Ping Wang, Ming Chen.
Funding acquisition: Guoqing Du, Linghui Li, Shangquan Wang.
Supervision: Shangquan Wang.
Writing – original draft: Kaiming Li, Hao Gong.
Writing – review & editing: Rui Xie, Guoqing Du, Linghui Li.
Footnotes
Abbreviations: AEs = adverse events, BMI = body mass index, DB-RCT = double-blind randomized controlled trail, EQ-VAS = EuroQol visual analogue scale, HA = hyaluronic acid, IKDC = International Knee Documentation Committee, KOA = knee osteoarthritis, MD = mean difference, PRP = platelet-rich plasma, RR = relative risk, WOMAC = Western Ontario and McMaster Universities Arthritis Index.
How to cite this article: Gong H, Li K, Xie R, Du G, Li L, Wang S, Yin J, Gu J, Wang P, Chen M, Hou X. Clinical therapy of platelet-rich plasma vs hyaluronic acid injections in patients with knee osteoarthritis: a systematic review and meta-analysis of randomized double-blind controlled trials. Medicine. 2021;100:12(e25168).
HG, KL, and RX contributed equally to this work.
The study was supported by National Natural Science Foundation of China (No.81904230, 81704103, 81674005, 81804120); Scientific Research Project of Chinese Academy of Traditional Chinese Medicine: Research on Rehabilitation-related Diagnosis and Treatment Technology of Characteristic Traditional Chinese Medicine (No.ZZ10-015).
Ethical Review Committee Statement was not necessary because this study is a meta-analysis of previous RCTs, the need for consent to participate is not applicable.
All data analyzed during this study were included in the manuscript. The raw data used and analyzed during the current study are available from the corresponding author upon reasonable request.
This review is registered in PROSPERO: CRD42020182571.
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Larsson S, Englund M, Struglics A, et al. Interleukin-6 and tumor necrosis factor alpha in synovial fluid are associated with progression of radiographic knee osteoarthritis in subjects with previous meniscectomy. Osteoarthritis Cartilage 2015;23(11):1906–14. [DOI] [PubMed] [Google Scholar]
- [2].Buhr M, Siekmann W. Intra-articular injection of platelet rich plasma for the treatment of cartilage damage. Orthopa Dische Praxis 2009;45(1):10–6. [Google Scholar]
- [3].Tammachote N, Kanitnate S, Yakumpor T, et al. Intra-articular, single shot hylan G-F 20 hyaluronic acid injection compared with corticosteroid in knee osteoarthritis: a double-blind, randomized controlled trial. J Bone Joint Surg Am 2016;98(11):885–92. [DOI] [PubMed] [Google Scholar]
- [4].Rodriguez-Merchan EC. Topical therapies for knee osteoarthritis. Postgrad Med 2018;130(7):607–12. [DOI] [PubMed] [Google Scholar]
- [5].Galluccio F, Barskova T, Cerinic MM. Short-term effect of the combination of hyaluronic acid, chondroitin sulphate, and keratin matrix on early symptomatic knee osteoarthritis. Eur J Rheumatol 2015;2(3):106–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int 2010;107(9):152–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Altman RD, Devji T, Bhandari M, et al. Clinical benefit of intra-articular saline as a comparator in clinical trials of knee osteoarthritis treatments: a systematic review and meta-analysis of randomized trials. Semin Arthritis Rheum 2016;46(2):151–9. [DOI] [PubMed] [Google Scholar]
- [8].Duymus TM, Mutlu S, Dernek B, et al. Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee Surg Sports Traumatol Arthrosc 2017;25(2):485–92. [DOI] [PubMed] [Google Scholar]
- [9].Foster TE, Puskas BL, Mandelbaum BR, et al. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med 2009;37(11):2259–72. [DOI] [PubMed] [Google Scholar]
- [10].Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop 2014;5(3):351–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Perdisa F, Filardo G, Di Matteo B, et al. Platelet rich plasma: a valid augmentation for cartilage scaffolds? A systematic review. Histol Histopathol 2014;29(7):805–14. [DOI] [PubMed] [Google Scholar]
- [12].Mifune Y, Matsumoto T, Takayama K, et al. The effect of platelet-rich plasma on the regenerative therapy of muscle derived stem cells for articular cartilage repair. Osteoarthritis Cartilage 2013;21(1):175–85. [DOI] [PubMed] [Google Scholar]
- [13].McArthur BA, Dy CJ, Fabricant PD, et al. Long term safety, efficacy, and patient acceptability of hyaluronic acid injection in patients with painful osteoarthritis of the knee. Patient Prefer Adherence 2012;6:905–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kuanyu L, Chiachi Y, Chienjen H, et al. Intra-articular injection of platelet-rich plasma is superior to hyaluronic acid or saline solution in the treatment of mild to moderate knee osteoarthritis: a randomized, double-blind, triple-parallel, placebo-controlled clinical trial. J Arthroscopic Related Surg 2019;35(1):106–17. [DOI] [PubMed] [Google Scholar]
- [16].Yu W, Xu P, Huang G, Liu L, et al. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med 2018;16(3):2119–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ke S, Yuming B, Jun W, et al. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol 2018;37(5):1341–50. [DOI] [PubMed] [Google Scholar]
- [18].Görmeli G, Görmeli CA, Ataoglu B, et al. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc 2017;25:958–65. [DOI] [PubMed] [Google Scholar]
- [19].Alessandro DM, Berardo DM, Tiziana P, et al. Platelet-rich plasma versus hyaluronic acid injections for the treatment of knee osteoarthritis: results at 5 years of a double-blind, randomized controlled trial. Am J Sports Med 2019;47(2):347–54. [DOI] [PubMed] [Google Scholar]
- [20].Filardo G, Kon E, Di Martino A, et al. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial. BMC Musculoskelet Disord 2012;13:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Van Manen MD, Nace J, Mont MA. Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners. J Am Osteopath Assoc 2012;112(11):709–15. [PubMed] [Google Scholar]
- [22].Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil 2006;85(11):S2–11. [DOI] [PubMed] [Google Scholar]
- [23].Rayegani SR. Does intra articular platelet rich plasma injection improve function, pain and quality of life in patients with osteoarthritis of the knee? A randomized clinical trial. Orthop Rev 2014;6(5405):112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jevsevar D. Treatment of osteoarthritis of the knee: evidence-based guideline. Second nd edition. J Am Acad Orthop Surg 2013;21(9):571–6. [DOI] [PubMed] [Google Scholar]
- [25].Bendinelli P, Matteucci E, Dogliotti G, et al. Molecular basis of antiinflammatory action of platelet-rich plasma on human chondrocytes: mechanisms of NF-κB inhibition via HGF. J Cell Physiol 2010;225(3):757–66. [DOI] [PubMed] [Google Scholar]
- [26].Sampson S, Reed M, Silvers H, et al. Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis a pilot study. Am J Phys Med Rehabil 2010;89(12):961–9. [DOI] [PubMed] [Google Scholar]
- [27].Buhr M, Siekmann W. Intra-articular injection of platelet rich plasma for the treatment of cartilage damage. Orthopadische Praxis 2009;45(1):10–6. [Google Scholar]
- [28].Gobbi A, Karnatzikos G, Mahajan V, et al. Platelet-rich plasma treatment in symptomatic patients with knee osteoarthritis preliminary results in a group of active patients. Sports Health 2012;4(2):162–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Iannitti T, Lodi D, Palmieri B. Intra-articular injections for the treatment of osteoarthritis: focus on the clinical use of hyaluronic acid. Drugs R D 2011;11(1):13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Miller LE, Block JE. US-approved intra-articular hyaluronic acid injections are safe and effective in patients with knee osteoarthritis: systematic review and meta-analysis of randomized, saline-controlled trials. Clin Med Arthritis Musculoskelet Disord 2013;6:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Alsousou J, Thompson M, Halley P, et al. The biology of platete-rich plasma and its application in trauma and orthopaedic surgery. J Bone Joint Surg Br 2009;91(8):987–96. [DOI] [PubMed] [Google Scholar]
- [32].Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet-Rich Plasma (PRP) vs Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights 2015;8:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kavadar G, Demircioglu DT, CeliK MY, et al. Effectiveness of platelet-rich plasma in the treatment of moderate knee osteoarthritis: a randomized prospective study. J Phys Ther 2015;12(27):3863–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Spakova T, Rosocha J, Lacko M, et al. Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am J Phys Med Rehabil 2012;91:411–7. [DOI] [PubMed] [Google Scholar]
- [35].Wernecke C, Braun HJ, Dragoo JL. The effect of intra-articular corticosteroids on articular cartilage: a systematic review. Orthop J Sports Med 2015;3(5):2325967115581163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kon E, Mandelbaum B, Buda R, et al. Platelet-rich plasma intraarticular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: from early degeneration to osteoarthritis. Arthroscopy 2011;27(11):1490–501. [DOI] [PubMed] [Google Scholar]


