Abstract
Introduction:
Decreased brain-derived neurotrophic factor (BDNF) is associated with poor sleep. This study examined the effects of acupuncture versus cognitive-behavioral therapy for insomnia (CBT-I) on serum BDNF and sleep outcomes in cancer survivors with insomnia.
Methods:
This was an exploratory analysis of a randomized clinical trial (N=160) comparing acupuncture versus CBT-I for cancer survivors with insomnia. Interventions were delivered over 8 weeks. Outcomes were assessed at baseline and week 8. Serum BDNF was evaluated with ELISA. Sleep was evaluated with Insomnia Severity Index and Consensus Sleep Diary. Pearson correlations between BDNF and sleep outcomes were calculated. Data analysis was limited to 87 survivors who provided serum samples.
Results:
Among 87 survivors, the mean age was 61.9 (SD 11.4) years, 51.7% were women, and 24.1% were non-white. Mean serum BDNF did not significantly increase in acupuncture (N=50) or CBT-I (N=37) groups. When analysis was restricted to patients with low baseline BDNF (i.e. levels below the sample median of 47.1 ng/ml), the acupuncture group (N=22) demonstrated a significant 7.2 ng/ml increase in mean serum BDNF (P=0.03), whereas the CBT-I group (N=21) demonstrated a non-significant 2.9 ng/ml increase (P=0.28). Serum BDNF was not significantly correlated with sleep outcomes (all P>0.05).
Conclusion:
Among cancer survivors with insomnia and low baseline BDNF, acupuncture significantly increased serum BDNF levels; however, the clinical significance of this finding requires further investigation.
Keywords: Insomnia, Cancer, Brain-Derived Neurotrophic Factor, Cognitive Behavioral Therapy, Acupuncture, Comparative Effectiveness
INTRODUCTION
Over half of patients with cancer suffer from insomnia, leading to harmful consequences for their physical and mental quality of life.1 Medications are commonly used to treat insomnia; however, their potential side effects, including drowsiness, impaired cognition, or increased fall risk, highlight that non-pharmacological modalities are important treatment options, particularly as polypharmacy becomes a growing concern in the aging cancer population.2, 3 In our recently published comparative effectiveness trial (N=160), both acupuncture and cognitive-behavioral therapy for insomnia (CBT-I) produced clinically meaningful improvements in insomnia among diverse cancer survivors across various disease stages.4 However, the biological mechanisms of these two non-pharmacological modalities may differ and have not been fully elucidated.
Brain-derived neurotrophic factor (BDNF) is a neuropeptide that plays an important role in neuronal survival, differentiation, plasticity, growth, and long-term potentiation.5–7 BDNF has been widely studied in the context of stress-related mood disorders8, 9 and some evidence suggests that sleep may be implicated in the relationship between BDNF and stress.10 Research from animal studies points to a potential role of BDNF in sleep homeostasis.11 In human studies, decreased serum BDNF levels have been associated with greater severity of subjective insomnia.12, 13 A recent study also demonstrated that serum BDNF levels were significantly lower among insomnia patients with objective short sleep duration (<6 hours of total sleep time) compared with those with normal sleep duration (≥6 hours of total sleep time).14 Limited research to date has explored these associations between BDNF and sleep in cancer populations or the responsiveness of BDNF to treatments for cancer-related insomnia.
Acupuncture has been shown to increase hippocampal BDNF expression in animal models of cognitive dysfunction.15, 16 A randomized controlled trial (N=80) demonstrated that acupuncture increased serum BDNF levels among breast cancer patients relative to no-treatment controls; however, this study lacked sleep measures and thus was unable to evaluate the association between BDNF and sleep.17 To the best of our knowledge, the effects of CBT-I on BDNF have not been studied in cancer survivors with insomnia. To address gaps in the mechanistic understanding of these two effective non-pharmacological insomnia treatments, the current study examined the effects of acupuncture versus CBT-I on serum BDNF in cancer survivors with insomnia. Guided by prior literature,12–14 we also sought to characterize the relationship between BDNF, subjective insomnia severity, and total sleep time in the context of insomnia treatment.
METHODS
Study Design, Participants, and Procedures
The current study is an exploratory analysis of a dual-center, parallel-group, 2-arm, randomized comparative effectiveness trial evaluating acupuncture versus CBT-I for the treatment of insomnia in cancer survivors.4 Interventions were delivered over 8 weeks. Outcomes were assessed at baseline and week 8 (end of intervention). Recruitment and interventions occurred from March 2015 to April 2017. The primary findings of the comparative effectiveness trial have been published previously.4 The study was approved by the institutional review boards at the University of Pennsylvania (IRB #: 821497) and Memorial Sloan Kettering Cancer Center (IRB #: 16–947). The study was conducted in accordance with the Declaration of Helsinki.
Inclusion criteria included: 1) English-speaking adult patients of any cancer type and stage; 2) completion of active cancer treatment with surgery, chemotherapy, and/or radiotherapy at least one month prior to study initiation; 3) score ≥8 on the Insomnia Severity Index;18 and 4) meeting criteria for insomnia disorder as defined by the Diagnostic and Statistical Manual of Mental disorders, 5th Edition (DSM-5).19 Exclusion criteria included: 1) presence of another sleep disorder not adequately treated (e.g. delayed/advanced sleep phase syndrome, obstructive sleep apnea, restless leg syndrome); 2) previous insomnia treatment with acupuncture or CBT-I; 3) presence of psychiatric disorder not adequately treated (e.g. major depressive disorder, bipolar disorder, schizophrenia, generalized anxiety disorder, post-traumatic stress disorder, dementia); and 4) employment in shift work that would impair ability to establish a regular sleep schedule. Research staff conducted a diagnostic interview to confirm study eligibility.
After eligibility was confirmed, patients completed written informed consent. Patients were sequentially randomized in a 1:1 ratio to one of the two treatment conditions using permuted block randomization with a secure computer system that ensures full allocation concealment. The study investigators, including outcome assessors, were blinded to treatment assignment. The complete study protocol has been described in detail separately.20
All participants were invited to provide serum samples for exploratory analyses. The provision of biospecimens was voluntary and was not required for study participation. The current study includes only patients who provided complete serum samples at all study timepoints (N=87).
Interventions
Acupuncture, a therapeutic modality derived from Traditional Chinese Medicine (TCM), involves the insertion of thin, sterile, single-use, metallic needles into the body surface.21 It is considered safe with few side effects.22 Four licensed acupuncturists with 11–14 years of experience delivered the intervention following a semi-fixed, manualized protocol. Informed by TCM principles, the protocol consisted of standardized points to address insomnia (Heart-7, Spleen-6, Du-20, Du-24, Auricular Shen-Men, Auricular Sympathetic) as well as supplementary points to treat co-morbid symptoms (i.e. psychological distress, fatigue, pain). Licensed acupuncturists inserted a total of 8 to 16 needles with sizes of 0.16–0.25 mm × 15–40 mm (manufactured by SEIRIN, Weymouth, MA). Needles were inserted at appropriate angles to indicated depths, based on body type and point location, then manually manipulated to achieve De Qi (a sensation of aching and soreness).23 Needles remained in place for 30 minutes. Participants received acupuncture treatments a total of ten treatments over eight weeks, i.e. twice per week for the first two weeks, then weekly for the six remaining weeks.
CBT-I is a manualized multi-component intervention that includes sleep restriction, stimulus control, cognitive restructuring, relaxation training, and sleep hygiene education.24 Four licensed therapists and five psychology trainees delivered the CBT-I intervention. Patients received a total of seven sessions over eight weeks, i.e. five weekly sessions of CBT-I followed by two bi-weekly sessions. The details of the acupuncture and CBT-I treatment protocols are available in Supplementary Materials.
Outcomes
BDNF
Most human studies measure BDNF peripherally due to the infeasibility of collecting brain-derived samples. BDNF readily crosses the blood-brain barrier,25 and circulating BDNF levels in peripheral blood have been shown in several species to correlate with levels in brain tissue.26 Given that plasma BDNF is sensitive to acute changes in circulating levels and is strongly influenced by pre-analytical conditions, measurement of serum BDNF is preferable in clinical studies.27, 28
For this study, we collected blood samples in serum separator tubes (SST) at baseline and week 8. Samples were allowed to clot for 30 minutes then centrifuged before sera were isolated, aliquoted and cryopreserved at −80°C until batch testing. Sera were diluted at 1:200 for all but one batch of samples (which was diluted at 1:100). Sera were tested in duplicates with the Human BDNF ELISA Kit (Aviscera-Bioscience, Santa Clara, CA). This kit demonstrated acceptable intra- and inter-assay variation, detection range, sensitivity, and processing time, in a study that compared six different kits.29
All samples fell within the range of detection. To determine testing variance and consistency across testing plates in this study, we used aliquots from the positive control included in the kit as well as aliquots of an internal laboratory control serum (i.e., serum control). The mean intraplate coefficient of variation (CV) in this study was 20.6% for the positive control and 8.8% for the serum control. The mean interplate CV was 13.1% for the positive control and 41.7% for the serum control. To maximize the detection of technical or procedural errors and minimize false rejections, quality control data points were plotted on Levey-Jennings and Westgard rules applied. No plate-runs were found to be in violation of these rules, i.e. values remained within the mean +/− 3 SD.
Insomnia Severity
The Insomnia Severity Index (ISI) provides a reliable measure of insomnia that has been validated in cancer populations with Cronbach’s α of 0.90.30 This 7-item instrument evaluates the subjective symptoms and consequences of insomnia as well as the degree of associated distress. Items are scored on a five-point scale (0–4), and total ISI scores range from 0–28 with higher scores indicating more severe insomnia symptoms.
Total Sleep Time
Consensus Sleep Diary (CSD) is a standardized measure that provides a night-by-night self-report of sleep continuity, including sleep latency, number of awakenings, duration of awakenings, total sleep time, and sleep efficiency.31 Values are averaged across the week to produce a single value for each CSD variable. Participants completed the CSD for a one-week period at baseline and week 8. Given that prior research had demonstrated significant association between BDNF and sleep duration,14 total sleep time was selected as the variable used in the current analyses.
Statistical Analyses
The analyses conducted in this study were post-hoc and exploratory with the goal of generating hypotheses for future research. To explore the effects of acupuncture and CBT-I on BDNF, we used paired t-tests to evaluate within-group changes in serum BDNF from baseline to week 8 by treatment group; between-group differences were evaluated with a 2-sample t-test. To explore the relationship between BDNF and sleep outcomes in the context of insomnia treatment, we examined Pearson correlations between serum BDNF and sleep outcomes (ISI and total sleep time) among the total sample and by treatment group. Given that prior research has demonstrated larger magnitude of BDNF response in those with lower baseline levels,32 we also conducted separate analyses restricted to patients with low serum BDNF, which we defined as patients with baseline BDNF levels below the sample median. The sample size was pre-determined by the parent study.4 All statistical tests were two-sided. Statistical significance was set at P<0.05. All statistical analyses were conducted using STATA (version 12.0; STATA Corporation, College Station, TX).
RESULTS
Between February 2015 to March 2017, we screened 604 patients for eligibility. Among these, 444 were excluded due to ineligibility, lack of interest, lack of time, or inability to travel to study appointments. The remaining 160 patients were randomly assigned to receive acupuncture (N=80) or CBT-I (N=80) in the parent study. Of these 160 patients, 87 (54%) provided complete serum samples and were included the current study: 50 were assigned to receive acupuncture and 37 were assigned to receive CBT-I. No patients withdrew from the study between baseline and week 8. In the acupuncture group, 50 (100%) patients received all ten treatments. In the CBT-I group, 31 (83.8%) patients received all seven treatments, and 37 (100%) received six out of seven treatments. Figure 1 summarizes participant flow through the study.
Figure 1.
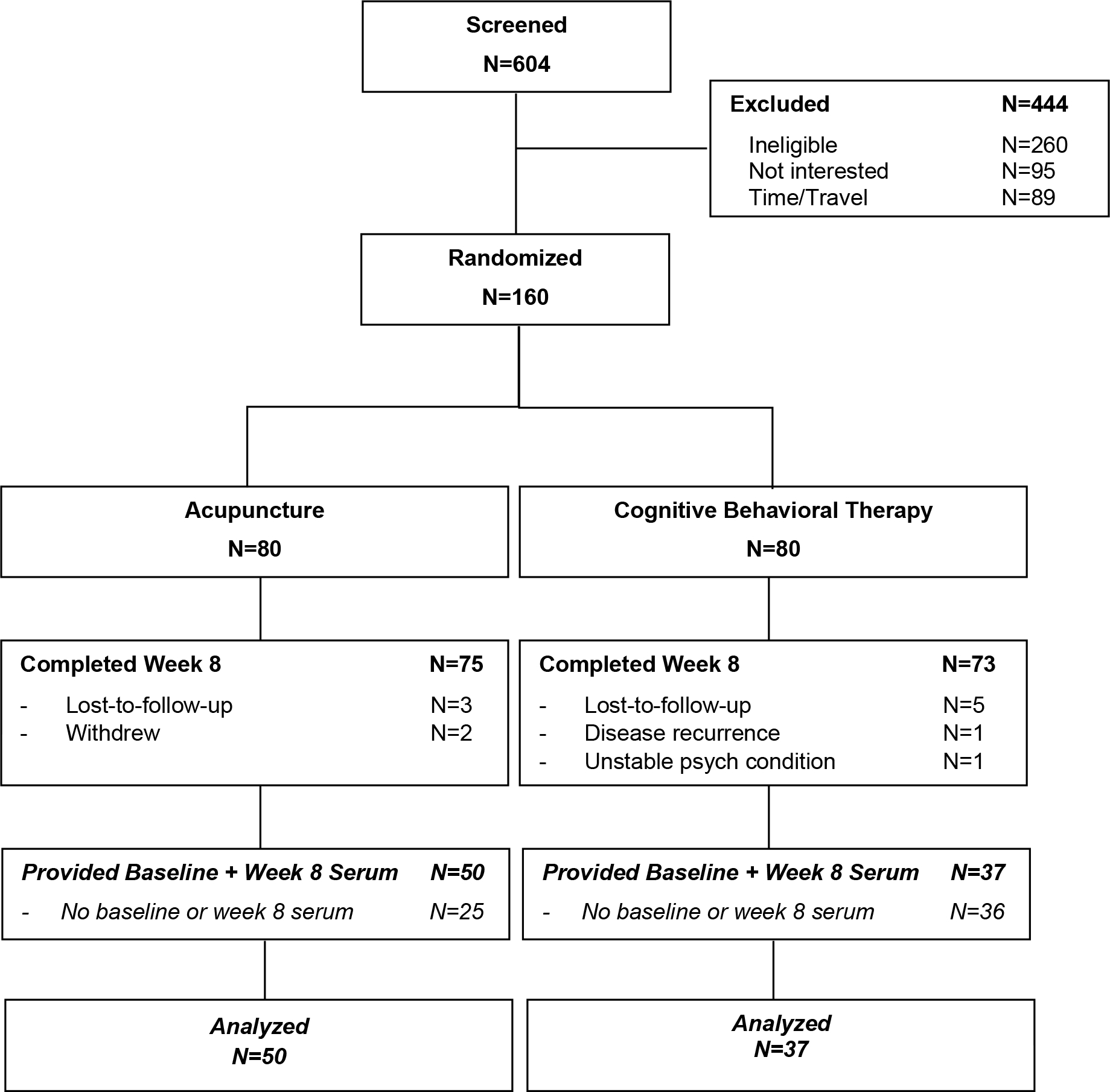
CONSORT Diagram. Italicized sections denote the current study.
Baseline sociodemographics and clinical characteristics of patients are shown in Table 1. The mean (SD) age was 61.9 (11.4) years, 51.7% were women, and 24.1% were non-white. The most common cancer types were breast (31.0%) and prostate (23.0%). The median time since cancer diagnosis was 4.6 years (interquartile range 3.0–7.0).
Table 1.
Sociodemographic and Clinical Characteristics.
| Total | Acupuncture | CBT-I | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
|
| ||||||
| 87 | 100.0 | 50 | 57.5 | 37 | 42.5 | |
|
| ||||||
| Age (Mean, SD), years | 61.9 (11.4) | 62.7 (10.6) | 60.8 (12.4) | |||
|
| ||||||
| Gender | ||||||
|
| ||||||
| Male | 42 | 48.3 | 26 | 52.0 | 16 | 43.2 |
| Female | 45 | 51.7 | 24 | 48.0 | 21 | 56.8 |
|
| ||||||
| Race | ||||||
|
| ||||||
| White | 66 | 75.9 | 37 | 74.0 | 28 | 78.4 |
| Non-white | 21 | 24.1 | 13 | 26.0 | 8 | 21.6 |
|
| ||||||
| Education | ||||||
|
| ||||||
| Elementary school | 1 | 1.2 | 1 | 2 | 0 | 0 |
| High school graduate | 6 | 6.9 | 5 | 10 | 1 | 2.7 |
| Some college or trade school | 13 | 14.9 | 6 | 12 | 7 | 18.9 |
| College graduate | 24 | 27.6 | 13 | 26 | 11 | 29.7 |
| Graduate school degree | 43 | 49.4 | 25 | 50 | 18 | 48.7 |
|
| ||||||
| Employment | ||||||
|
| ||||||
| Full-time | 33 | 37.9 | 21 | 42 | 12 | 32.4 |
| Part-time | 14 | 16.1 | 7 | 14 | 7 | 18.9 |
| Not currently employed | 40 | 46.0 | 22 | 44 | 18 | 48.7 |
|
| ||||||
| Cancer Type * | ||||||
|
| ||||||
| Breast | 27 | 31.0 | 15 | 30.0 | 12 | 32.4 |
| Prostate | 20 | 23.0 | 13 | 26.0 | 7 | 18.9 |
| Other | 40 | 46.0 | 22 | 44.0 | 18 | 48.7 |
|
| ||||||
| Cancer Stage | ||||||
|
| ||||||
| Stage 0 | 3 | 3.5 | 0 | 0 | 3 | 8.1 |
|
| ||||||
| Stage I | 41 | 47.1 | 24 | 48.0 | 17 | 46.0 |
| Stage II | 16 | 18.4 | 8 | 16.0 | 8 | 21.6 |
| Stage III | 16 | 18.4 | 10 | 20.0 | 6 | 16.2 |
| Stage IV | 8 | 9.2 | 6 | 12.0 | 2 | 5.4 |
| Unknown | 3 | 3.5 | 2 | 4.0 | 1 | 2.7 |
|
| ||||||
| Cancer Treatments ** | ||||||
|
| ||||||
| Surgery | 70 | 80.5 | 42 | 84.0 | 28 | 75.7 |
| Chemotherapy | 42 | 48.3 | 24 | 48.0 | 18 | 48.7 |
| Radiation | 49 | 56.3 | 29 | 58.0 | 20 | 54.1 |
| Hormonal | 20 | 23.0 | 12 | 24.0 | 8 | 21.6 |
|
| ||||||
| Years since Cancer Diagnosis (Median, IQR) | 4.6 (3.0–7.0) | 4.9 (2.9–7.0) | 4.2 (1.4–6.4) | |||
Other cancer types include Colorectal, Head/Neck, Hematologic, Gynecologic, Skin, Lung, Other Gastrointestinal, Other Genitourinary, and >1 cancer type.
Subjects can have more than 1 type of cancer treatments
Serum BDNF levels and sleep profile of patients at baseline are shown in Table 2. Median BDNF at baseline was 47.1 ng/ml (interquartile range 26.0 to 78.6 ng/ml). The mean years since insomnia onset was 9.8 (SD 9.9). The mean ISI total score was 17.8 (SD 4.2). The mean total sleep time was 360 (SD 71.6) minutes.
Table 2.
Baseline BDNF, Insomnia Symptom, and Sleep Continuity Profile.
| Total N=87 |
Acupuncture N=50 |
CBT-I N=37 |
|
|---|---|---|---|
|
| |||
| BDNF Levels at Baseline | |||
|
| |||
| Median (ng/ml) | 47.1 | 50.9 | 44.9 |
| Inter-Quartile Range (ng/ml) | 26.0 – 78.6 | 27.6–67.8 | 28.3–69.2 |
|
| |||
| Insomnia Symptom Profile at Baseline | |||
|
| |||
| Years since insomnia onset, mean (SD) | 9.8 (9.9) | 10.0 (10.5) | 9.6 (9.0) |
| ISI total score, mean (SD) | 17.8 (4.2) | 17.5 (4.2) | 18.2 (4.1) |
|
| |||
| Sleep Continuity Profile at Baseline | |||
|
| |||
| Minutes of total sleep time, mean (SD) | 360.0 (71.6) | 362.5 (62.6) | 356.6 (83.0) |
|
| |||
| Minutes of sleep onset latency, mean (SD) | 33.0 (33.6) | 30.4 (30.4) | 36.5 (37.6) |
|
| |||
| Number of awakenings, mean (SD) | 2.6 (1.3) | 2.6 (1.4) | 2.5 (1.2) |
|
| |||
| Minutes awake after sleep onset, mean (SD) | 53.2 (34.8) | 52.2 (32.2) | 54.5 (38.4) |
|
| |||
| Sleep efficiency percentage, mean (SD) | 75.9 (12.1) | 77.3 (9.2) | 74.0 (15.1) |
Notes: BDNF, brain-derived neurotrophic factor; CBT-I, cognitive-behavioral therapy for insomnia; SD, standard deviation; ISI, Insomnia Severity Index
Effects on BDNF
Among patients treated with acupuncture (N=50), mean BDNF increased non-significantly from 49.5 to 52.7 ng/ml (3.2 ng/ml, 95% CI −0.5 to 7.0, P=0.09). Among patients treated with CBT-I (N=37), mean BDNF increased non-significantly from 46.8 to 49.2 ng/ml (2.4 ng/ml, 95% CI −1.3 to 6.0, P=0.19). Between-group difference was not statistically significant (P=0.74). These findings are depicted in Figure 2.
Figure 2.
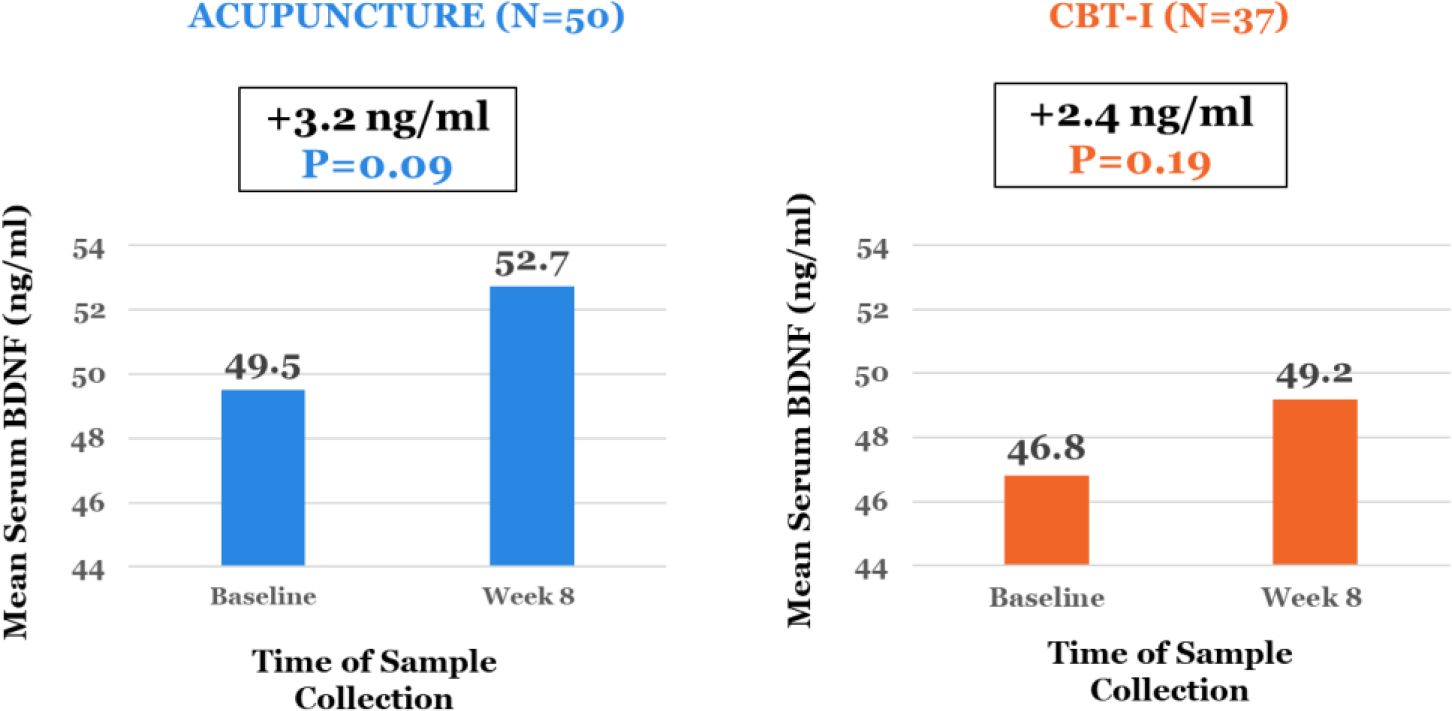
Change in Mean Serum BDNF by Treatment Group.
When analysis was restricted to patients with low baseline BDNF (i.e. <47.1 ng/ml), those who received acupuncture (N=22) demonstrated a significant increase in mean BDNF from 37.2 to 44.4 ng/ml (7.2 ng/ml, 95% CI 0.6 to 13.9, P=0.03), whereas those who received CBT-I (N=21) demonstrated a non-significant increase from 35.9 to 38.8 ng/ml (2.9 ng/ml, 95% CI −2.6 to 8.4, P=0.28). The between-group difference was not statistically significant (P=0.30). These findings are depicted in Figure 3.
Figure 3.
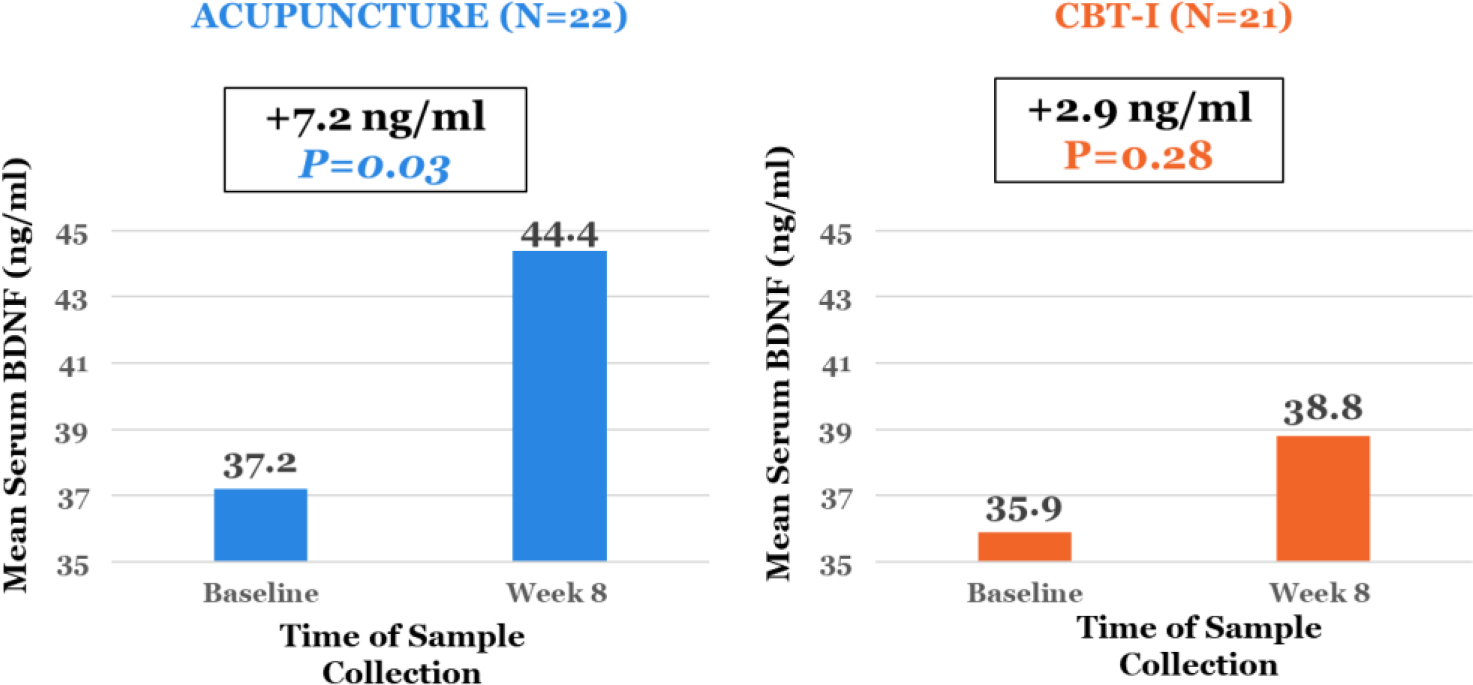
Change in Mean Serum BDNF among Patients with Low Baseline BDNF by Treatment Group. These analyses were restricted to patients whose baseline BDNF levels were below the sample median of 47.1 ng/ml.
Relationship between BDNF, Insomnia, and Sleep Continuity
Among the total sample (N=87), BDNF was not significantly associated with ISI scores or total sleep time at baseline (all P>0.05). Both acupuncture and CBT-I produced statistically significant reduction in ISI scores at week 8 compared to baseline. Acupuncture reduced by 8.7 points (95% CI 6.9 to 10.5, P<0.001), whereas CBT-I reduced by 12.4 points (95% CI 10.6 to 14.1, P<0.001); the between-group difference was statistically significant, favoring CBT-I (P=0.005). Acupuncture and CBT-I also produced statistically significant increases in total sleep time at week 8 compared to baseline. Acupuncture increased by 53.5 minutes (95% CI 36.1 to 70.9, P<0.001), whereas CBT-I increased by 35.4 minutes (95% CI 10.0 to 60.1, P=0.008); the between-group difference was not statistically significant (P=0.26). Changes in serum BDNF were not significantly associated with changes in ISI score and total sleep time in either treatment group (all P>0.05).
When analyses were restricted to patients with low BDNF at baseline (N=43), BDNF was not significantly associated with ISI scores or total sleep time at baseline (all P>0.05). Among those with low baseline BDNF, acupuncture significantly reduced the ISI score by 8.0 points (95% CI 5.0 to 11.0, P<0.001) from baseline to week 8, whereas CBT-I significantly reduced the ISI score by 13.1 points (95% CI 10.7 to 15.6, P<0.001); the between-group difference was statistically significant, favoring CBT-I (P=0.008). Among those with low baseline BDNF, acupuncture increased total sleep time by 57.6 minutes (95% CI 37.0 to 78.2, P<0.001) from baseline to week 8, whereas CBT-I increased by 48.2 minutes (95% CI 6.7 to 89.8, P=0.03); the between-group difference was not statistically significant (P=0.66). Changes in serum BDNF were not significantly associated with changes in ISI score and total sleep time among those with low baseline BDNF in either treatment group (all P>0.05).
DISCUSSION
Insomnia is a prevalent, disabling, and costly condition among cancer survivors.33 Acupuncture and CBT-I represent two effective, non-pharmacological treatments, but their biological mechanisms have not been clearly defined. In this exploratory analysis, we demonstrate that acupuncture significantly increased serum BDNF in cancer survivors with insomnia and low baseline BDNF levels, although the clinical significance of this finding remains unclear. Further research is required to determine whether acupuncture targets certain aspects of sleep through a mechanism involving BDNF.
Our findings align with other basic and clinical studies demonstrating that acupuncture increases serum BDNF levels and its expression in the brain.17, 34 Notably, one acupuncture trial did not demonstrate a significant BDNF increase after treatment;35 however, the study enrolled healthy, community-dwelling older adults and excluded patients with medical or psychiatric conditions (e.g. insomnia, depression, or dementia), which are typically associated with low BDNF levels.9, 36 Prior research has shown that patients with lower BDNF levels demonstrate a greater BDNF increase in response to interventions,32 as suggested by our current study. Future studies should evaluate whether patients with insomnia are more likely to respond to acupuncture if they have lower BDNF levels at baseline. If confirmed, BDNF has potential clinical utility as a biomarker to identify individuals more likely to benefit from acupuncture, helping to guide more personalized approaches to insomnia treatment.
In our comparative effectiveness trial, CBT-I was more effective at improving subjective insomnia symptoms, whereas acupuncture was more effective at improving self-reported total sleep time.4 Our current study did not demonstrate a significant correlation between BDNF and self-reported sleep duration. However, others have reported associations between BDNF and objective measures of sleep time; specifically, serum BDNF levels were found to be significantly lower among insomnia patients with <6 hours of total objective sleep time compared to those with longer sleep duration.14 Given that acupuncture has been shown to significantly increased objective total sleep time as measured by actigraphy or polysomnography,37, 38 BDNF warrants further investigation as a candidate biological mechanism by which acupuncture may increase total sleep time. If confirmed, acupuncture may be a good treatment option for insomnia with objective short sleep duration, which others have identified as a biologically severe insomnia phenotype that may be less responsive to CBT-I.39, 40
Our findings must be considered in the context of several limitations. First, our analysis of serum BDNF levels are hypothesis-generating and require confirmation in rigorously designed, adequately powered studies. Second, total serum BDNF was measured with an ELISA kit that lacks the sensitivity to quantify the precursor form of BDNF (i.e. pro-BDNF); thus, in practice, our current study reports on the mature, most abundant form of BDNF (i.e. mBDNF). The balance between mBDNF and pro-BDNF in the context of insomnia is potentially important to characterize, as others have previously demonstrated the differential activity of mBDNF and proBDNF.41 We plan to investigate both forms of BDNF in a future study. Third, given the lack of usual-care or no-treatment controls, regression to the mean and natural fluctuation of BDNF levels must also be considered. Fourth, our study population was comprised of cancer survivors, the majority of whom were well-educated and white, thus limiting the generalizability of our findings; this could potentially explain why our study did not observe a significant association between insomnia severity and BDNF levels, which had previously been demonstrated in non-cancer populations.12, 13 Lastly, our study used self-reported sleep outcomes and did not evaluate the relationship between serum BDNF and objective sleep parameters. This is a potential reason that we did not find a correlation between BDNF and total sleep time at baseline, in contrast to other studies that demonstrated a significant association with objective measures of sleep duration.14 Given that discrepancies between self-reported and objectively measured sleep are well-documented,42 future studies should incorporate both types of sleep outcomes to better characterize the relationship between BDNF and sleep.
Despite these limitations, this is the first study to characterize the effects of acupuncture and CBT-I on serum BDNF in cancer survivors with insomnia. We found preliminary evidence that acupuncture may increase serum BDNF in cancer patients with insomnia and low baseline BDNF levels. Confirmation of these findings could potentially lead to novel clinical applications of BDNF to guide personalized management of cancer-related insomnia.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank the patients, oncologists, nurses, and clinical staff at all study sites for their contributions to this study. They would also like to thank Jessica Kenney for her assistance with handling and aliquoting serum samples.
Funding:
This research was funded by a Patient-Centered Outcomes Research Institute (PCORI) Award (CER-1403-14292), a grant from the National Institutes of Health/National Cancer Institute (P30 CA008748), a grant from the American Cancer Society (RSG-14-167-01 ACS), and the Translational and Integrative Medicine Research Fund at Memorial Sloan Kettering Cancer Center.
Footnotes
DISCLOSURE STATEMENTS
Research reported in this paper was funded in part by a Patient-Centered Outcomes Research Institute (PCORI) Award (CER-1403-14292). This manuscript is also supported in part by a grant from the National Institutes of Health/National Cancer Institute (P30 CA008748), a grant from the American Cancer Society (RSG-14-167-01 ACS), and the Translational and Integrative Medicine Research Fund at Memorial Sloan Kettering Cancer Center. The statements presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the PCORI, its Board of Governors, or its Methodology Committee; the National Institutes of Health; or the American Cancer Society. The funders did not have any role in the study design, in the collection, analysis and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication. Dr. Mao reports grants from Tibet CheeZheng Tibetan Medicine Co. Ltd. and Zhongke Health International LLC, outside the submitted work.
Trial Registration: ClinicalTrials.gov Identifier NCT02356575
REFERENCES
- 1.Savard J, Ivers H, Villa J, et al. Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2011; 29: 3580–3586. 2011/08/10. DOI: 10.1200/jco.2010.33.2247. [DOI] [PubMed] [Google Scholar]
- 2.Lees J and Chan A. Polypharmacy in elderly patients with cancer: clinical implications and management. The Lancet Oncology 2011; 12: 1249–1257. 2011/07/12. DOI: 10.1016/s1470-2045(11)70040-7. [DOI] [PubMed] [Google Scholar]
- 3.Murphy CC, Fullington HM, Alvarez CA, et al. Polypharmacy and patterns of prescription medication use among cancer survivors. Cancer 2018; 124: 2850–2857. 2018/04/13. DOI: 10.1002/cncr.31389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garland SN, Xie SX, DuHamel K, et al. Acupuncture Versus Cognitive Behavioral Therapy for Insomnia in Cancer Survivors: A Randomized Clinical Trial. Journal of the National Cancer Institute 2019; 111: 1323–1331. 2019/05/14. DOI: 10.1093/jnci/djz050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu B, Nagappan G and Lu Y. BDNF and synaptic plasticity, cognitive function, and dysfunction. Handbook of experimental pharmacology 2014; 220: 223–250. 2014/03/29. DOI: 10.1007/978-3-642-45106-5_9. [DOI] [PubMed] [Google Scholar]
- 6.Park H and Poo MM. Neurotrophin regulation of neural circuit development and function. Nature reviews Neuroscience 2013; 14: 7–23. 2012/12/21. DOI: 10.1038/nrn3379. [DOI] [PubMed] [Google Scholar]
- 7.Zagrebelsky M and Korte M. Form follows function: BDNF and its involvement in sculpting the function and structure of synapses. Neuropharmacology 2014; 76 Pt C: 628–638. 2013/06/12. DOI: 10.1016/j.neuropharm.2013.05.029. [DOI] [PubMed] [Google Scholar]
- 8.Polyakova M, Stuke K, Schuemberg K, et al. BDNF as a biomarker for successful treatment of mood disorders: a systematic & quantitative meta-analysis. Journal of affective disorders 2015; 174: 432–440. 2015/01/02. DOI: 10.1016/j.jad.2014.11.044. [DOI] [PubMed] [Google Scholar]
- 9.Sen S, Duman R and Sanacora G. Serum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implications. Biological psychiatry 2008; 64: 527–532. 2008/06/24. DOI: 10.1016/j.biopsych.2008.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giese M, Unternaehrer E, Brand S, et al. The interplay of stress and sleep impacts BDNF level. PloS one 2013; 8: e76050. 2013/10/23. DOI: 10.1371/journal.pone.0076050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faraguna U, Vyazovskiy VV, Nelson AB, et al. A causal role for brain-derived neurotrophic factor in the homeostatic regulation of sleep. The Journal of neuroscience : the official journal of the Society for Neuroscience 2008; 28: 4088–4095. 2008/04/11. DOI: 10.1523/jneurosci.5510-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giese M, Unternahrer E, Huttig H, et al. BDNF: an indicator of insomnia? Molecular psychiatry 2014; 19: 151–152. 2013/02/13. DOI: 10.1038/mp.2013.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mikoteit T, Brand S, Eckert A, et al. Brain-derived neurotrophic factor is a biomarker for subjective insomnia but not objectively assessable poor sleep continuity. Journal of psychiatric research 2019; 110: 103–109. 2019/01/08. DOI: 10.1016/j.jpsychires.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 14.Fan TT, Chen WH, Shi L, et al. Objective sleep duration is associated with cognitive deficits in primary insomnia: BDNF may play a role. Sleep 2019; 42 2018/10/23. DOI: 10.1093/sleep/zsy192. [DOI] [PubMed] [Google Scholar]
- 15.Yun SJ, Park HJ, Yeom MJ, et al. Effect of electroacupuncture on the stress-induced changes in brain-derived neurotrophic factor expression in rat hippocampus. Neuroscience letters 2002; 318: 85–88. 2002/02/14. [DOI] [PubMed] [Google Scholar]
- 16.Lin R, Chen J, Li X, et al. Electroacupuncture at the Baihui acupoint alleviates cognitive impairment and exerts neuroprotective effects by modulating the expression and processing of brain-derived neurotrophic factor in APP/PS1 transgenic mice. Molecular medicine reports 2016; 13: 1611–1617. 2016/01/08. DOI: 10.3892/mmr.2015.4751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tong T, Pei C, Chen J, et al. Efficacy of Acupuncture Therapy for Chemotherapy-Related Cognitive Impairment in Breast Cancer Patients. Medical science monitor : international medical journal of experimental and clinical research 2018; 24: 2919–2927. 2018/05/08. DOI: 10.12659/msm.909712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bastien CH, Vallieres A and Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep medicine 2001; 2: 297–307. 2001/07/05. [DOI] [PubMed] [Google Scholar]
- 19.American Psychiatric A, American Psychiatric A and Force DSMT. Diagnostic and statistical manual of mental disorders : DSM-5. Arlington, VA: American Psychiatric Association, 2017. [Google Scholar]
- 20.Garland SN, Gehrman P, Barg FK, et al. CHoosing Options for Insomnia in Cancer Effectively (CHOICE): Design of a patient centered comparative effectiveness trial of acupuncture and cognitive behavior therapy for insomnia. Contemporary clinical trials 2016; 47: 349–355. 2016/03/10. DOI: 10.1016/j.cct.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Mao JJ and Kapur R. Acupuncture in primary care. Primary care 2010; 37: 105–117. 2010/03/02. DOI: 10.1016/j.pop.2009.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White A A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupuncture in medicine : journal of the British Medical Acupuncture Society 2004; 22: 122–133. [DOI] [PubMed] [Google Scholar]
- 23.Mao JJ, Farrar JT, Armstrong K, et al. De qi: Chinese acupuncture patients’ experiences and beliefs regarding acupuncture needling sensation--an exploratory survey. Acupuncture in medicine : journal of the British Medical Acupuncture Society 2007; 25: 158–165. [DOI] [PubMed] [Google Scholar]
- 24.Trauer JM, Qian MY, Doyle JS, et al. Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis. Annals of internal medicine 2015; 163: 191–204. 2015/06/09. DOI: 10.7326/m14-2841. [DOI] [PubMed] [Google Scholar]
- 25.Pan W, Banks WA, Fasold MB, et al. Transport of brain-derived neurotrophic factor across the blood-brain barrier. Neuropharmacology 1998; 37: 1553–1561. 1999/01/14. [DOI] [PubMed] [Google Scholar]
- 26.Klein AB, Williamson R, Santini MA, et al. Blood BDNF concentrations reflect brain-tissue BDNF levels across species. The international journal of neuropsychopharmacology 2011; 14: 347–353. 2010/07/08. DOI: 10.1017/s1461145710000738. [DOI] [PubMed] [Google Scholar]
- 27.Teche SP, Nuernberg GL, Sordi AO, et al. Measurement methods of BDNF levels in major depression: a qualitative systematic review of clinical trials. The Psychiatric quarterly 2013; 84: 485–497. 2013/04/09. DOI: 10.1007/s11126-013-9261-7. [DOI] [PubMed] [Google Scholar]
- 28.Polyakova M, Schlogl H, Sacher J, et al. Stability of BDNF in Human Samples Stored Up to 6 Months and Correlations of Serum and EDTA-Plasma Concentrations. International journal of molecular sciences 2017; 18 2017/06/08. DOI: 10.3390/ijms18061189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polacchini A, Metelli G, Francavilla R, et al. A method for reproducible measurements of serum BDNF: comparison of the performance of six commercial assays. Scientific reports 2015; 5: 17989. 2015/12/15. DOI: 10.1038/srep17989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Savard MH, Savard J, Simard S, et al. Empirical validation of the Insomnia Severity Index in cancer patients. Psycho-oncology 2005; 14: 429–441. 2004/09/18. DOI: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- 31.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 2012; 35: 287–302. 2012/02/02. DOI: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hakansson K, Ledreux A, Daffner K, et al. BDNF Responses in Healthy Older Persons to 35 Minutes of Physical Exercise, Cognitive Training, and Mindfulness: Associations with Working Memory Function. Journal of Alzheimer’s disease : JAD 2017; 55: 645–657. 2016/10/08. DOI: 10.3233/jad-160593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gonzalez BD, Grandner MA, Caminiti CB, et al. Cancer survivors in the workplace: sleep disturbance mediates the impact of cancer on healthcare expenditures and work absenteeism. Support Care Cancer 2018. 2018/06/06. DOI: 10.1007/s00520-018-4272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Manni L, Albanesi M, Guaragna M, et al. Neurotrophins and acupuncture. Autonomic neuroscience : basic & clinical 2010; 157: 9–17. 2010/05/11. DOI: 10.1016/j.autneu.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 35.Zuppa C, Prado CH, Wieck A, et al. Acupuncture for sleep quality, BDNF levels and immunosenescence: a randomized controlled study. Neuroscience letters 2015; 587: 35–40. 2014/12/17. DOI: 10.1016/j.neulet.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 36.Laske C, Stransky E, Leyhe T, et al. BDNF serum and CSF concentrations in Alzheimer’s disease, normal pressure hydrocephalus and healthy controls. Journal of psychiatric research 2007; 41: 387–394. 2006/03/24. DOI: 10.1016/j.jpsychires.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 37.Fu C, Zhao N, Liu Z, et al. Acupuncture Improves Peri-menopausal Insomnia: A Randomized Controlled Trial. Sleep 2017; 40 2017/10/14. DOI: 10.1093/sleep/zsx153. [DOI] [PubMed] [Google Scholar]
- 38.Yin X, Gou M, Xu J, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep medicine 2017; 37: 193–200. 2017/09/14. DOI: 10.1016/j.sleep.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 39.Vgontzas AN, Fernandez-Mendoza J, Liao D, et al. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep medicine reviews 2013; 17: 241–254. 2013/02/20. DOI: 10.1016/j.smrv.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bathgate CJ, Edinger JD and Krystal AD. Insomnia Patients With Objective Short Sleep Duration Have a Blunted Response to Cognitive Behavioral Therapy for Insomnia. Sleep 2017; 40 2017/04/02. DOI: 10.1093/sleep/zsw012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lu B, Pang PT and Woo NH. The yin and yang of neurotrophin action. Nature reviews Neuroscience 2005; 6: 603–614. 2005/08/03. DOI: 10.1038/nrn1726. [DOI] [PubMed] [Google Scholar]
- 42.Kay DB, Buysse DJ, Germain A, et al. Subjective-objective sleep discrepancy among older adults: associations with insomnia diagnosis and insomnia treatment. Journal of sleep research 2015; 24: 32–39. 2014/09/16. DOI: 10.1111/jsr.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


