Abstract
Background:
Breast cancer is one of the common malignant tumors in women, which seriously affects women's physical and mental health and even life-threatening. The occurrence and development of breast cancer are closely related to genetic factors. Many studies have shown that human leukocyte antigen DRB1 is associated with the development of breast cancer, but lack evidence. This study aims to systematically evaluate the relationship between HLA-DRB1 gene polymorphism and breast cancer.
Methods:
The retrieval time of this study was from the establishment of the database to February 2021. The retrieval databases included CNKI, Wanfang, VIP and China Biomedical Database, PubMed, Embase, Web of Science, and the Cochrane Library. The retrieval objects were observational studies on the relationship between HLA-DRB1 gene polymorphism and breast cancer (including case--control studies, cross-sectional studies, and cohort studies). The language restrictions were English and Chinese. Two researchers independently extracted the data and assessed the quality of the included studies, and Stata 16.0 software was used for statistical analysis.
Results:
This study will systematically evaluate the relationship between HLA-DRB1 gene polymorphism and breast cancer based on existing studies.
Conclusion:
This study will explore the early warning signal of breast cancer genetic susceptibility, and provide evidence-based medical evidence for clarifying the role of HLA-DRB1 gene polymorphism in breast cancer.
OSF Registration number:
DOI 10.17605/OSF.IO/847FQ
Keywords: breast cancer, gene polymorphism, human leucocyte antigen DRB1, protocol, systematic review
1. Introduction
Breast cancer is one of the common malignant tumors in women. According to the 2012 global cancer report data[1] released by International Agency for Research on Cancer (IARC), breast cancer accounts for the first place in the incidence of female cancer. There are about 1.671 million new cases of breast cancer in the world each year, and about 5.22 million cases die of breast cancer each year, which seriously endangers women's health. The epidemiological characteristics of breast cancer have obvious regional differences, ethnic and ethnic differences, and family history, which are similar to the genetic characteristics of human leukocyte antigen (HLA).[2] About 5% to 10% of breast cancer cases have familial genetic tendency, and the first-degree relatives have a high incidence of breast cancer.[3] Under the same environmental exposure level, people with different genetic backgrounds have different responses to the exposure environment, indicating that different genetic backgrounds may be protective or hazardous factors for the occurrence of breast cancer in individuals. HLA allele polymorphism is an essential genetic factor that determines the ability of immune response, and different HLA allele polymorphism will affect the degree of individual immune response.[4]
HLA system is the major histocompatibility complex (MHC), the system is located in human chromosome 6, is the decisive factor of immune response.[5]HLA-DRB1 gene has the most abundant polymorphism in HLA-II gene, which is the decisive factor of immune antigen polymorphism. It is mainly involved in the immune process of tumor body and affects the occurrence and development of various tumor diseases.[6]
At present, the association between HLA-DRB1 allele polymorphism and breast cancer has attracted many scholars’ attention. Many studies have explored the relationship between HLA-DRB1 allele polymorphism and breast cancer.[7–10] However, as HLA-DRB1 is rich in polymorphism, there are both correlations and differences among people of different races, nationalities, and regions, the conclusions obtained by different studies are not identical or even opposite. Therefore, we adopted the meta-analysis method to comprehensively analyze the existing data in order to provide evidence-based medicine evidence for clarifying the relationship between HLA-DRB1 allele polymorphism and breast cancer genetic susceptibility.
2. Methods
2.1. Protocol register
This protocol of systematic review and meta-analysis has been drafted under the guidance of the preferred reporting items for systematic reviews and meta-analyses protocols (PRISMA-P).[11] Moreover, it has been registered on open science framework (OSF) (Registration number: DOI 10.17605/OSF.IO/847FQ).
2.2. Ethics
As the protocol did not require patient recruitment and the collection of personal information, it did not require approval from an ethics committee.
2.3. Eligibility criteria
-
(1)
Studies where the relationship between HLA-DRB1 gene polymorphism and breast cancer was studied and evaluated;
-
(2)
Observational studies (including case--control studies, cross-sectional studies, cohort studies);
-
(3)
Studies with allele or genotype distribution frequency data available;
-
(4)
Studies with the distribution frequency of genotypes conformed to Hardy--Weinberg law.
2.4. Exclusion criteria
-
(1)
Republished studies;
-
(2)
Published literatures for summary or review, articles with incomplete data or data errors, and contact the author cannot get complete data of the article;
-
(3)
Failure to provide detailed genotype frequency data;
-
(4)
Literatures without related outcome indicators;
-
(5)
The research object is not from human.
2.5. Search strategy
“HLA-DRB1,” “ gene polymorphism,” and “ breast cancer” were used as Chinese search terms to search in Chinese databases, including CNKI, Wanfang Data Knowledge Service Platform, VIP Chinese Journal Service Platform and Chinese Biomedical Database; “HLA antigen,” “HLA-DRB1,” “polymorphism,” “breast cancer,” “breast tumor,” etc, were searched in English databases, including PubMed, EMBASE, Web of Science, the Cochrane Library. All the domestic and foreign literatures on the relationship between HLA-DRB1 gene polymorphism and breast cancer were collected from the establishment of database to February 2021. Taking PubMed as an example, the search strategy is shown in Table 1.
Table 1.
Search strategy in PubMed database.
| Number | Search terms |
| #1 | HLA antigen [Title/Abstract] |
| #2 | HLA-DRB1 [Title/Abstract] |
| #3 | Human leucocyte antigen DRB1 [Title/Abstract] |
| #4 | #1 OR #2 OR #3 |
| #5 | polymorphism [Title/Abstract] |
| #6 | variant [Title/Abstract] |
| #7 | #4 OR #5 |
| #8 | Breast cancer [MeSH] |
| #9 | Breast Neoplasm [Title/Abstract] |
| #10 | Breast Tumor [Title/Abstract] |
| #11 | Mammary Cancer [Title/Abstract] |
| #12 | Malignant Neoplasm of Breast [Title/Abstract] |
| #13 | Malignant Tumor of Breast [Title/Abstract] |
| #14 | Cancer of Breast [Title/Abstract] |
| #15 | Mammary Carcinoma, Human [Title/Abstract] |
| #16 | Human Mammary Neoplasm [Title/Abstract] |
| #17 | Breast Carcinoma [Title/Abstract] |
| #18 | #7 OR #8 OR #9 OR #10 OR #11 |
| #19 | #4 AND #7 AND #18 |
2.6. Data screening and extraction
Two researchers independently completed literature screening. After excluding the studies that obviously did not meet the inclusion criteria, they further read the abstract and full text to determine whether they met the inclusion criteria. Data from the included literatures were extracted and cross-checked. In case of disagreement, consult with the third researcher and reach a consensus. The extracted data include the first author, publishing year, publishing country, ethnicity of the study population, basic characteristics of the study population (including age, sex, disease, etc), distribution of each gene phenotype (whether it complies with Hardy-Weinberg equilibrium law), and detection method of gene polymorphism. The literature screening process is shown in Figure 1.
Figure 1.
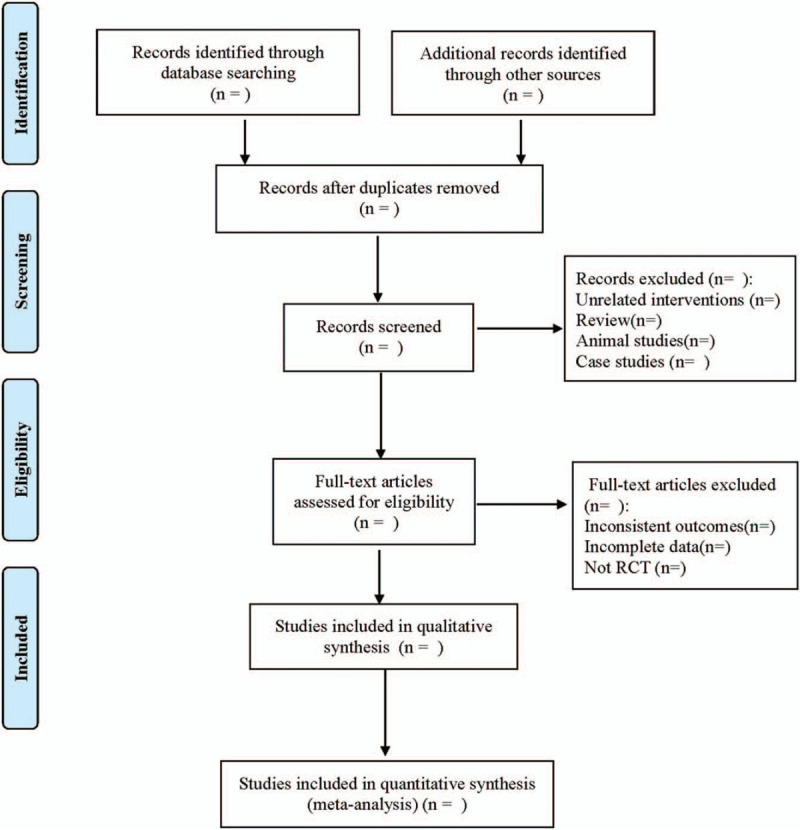
Flow diagram.
2.7. Literature quality assessment
The quality of case--control and cohort studies was evaluated by the Newcastle--Ottawa Scale (NOS),[12] including 3 columns and 8 items with a total score of 9, and the evaluation criteria ≥6 was high quality; The cross-sectional studies were evaluated using 11 standard entries from the evaluation cross-sectional studies recommended by the U.S. Agency for Healthcare Research and Quality (AHRQ); 0 ∼ 3 is low quality, 4 ∼ 7 is medium quality, and 8 ∼ 11 is high quality.[13]
2.8. Statistical analysis
2.8.1. Data analysis and processing
Before evaluating the correlation between gene polymorphism and breast cancer, the genotype distribution of each control group was tested for Hardy--Weinberg genetic balance (P ≥ .05). The software STATA.16 was used for meta-analysis, continuity variables were expressed as standard mean difference (SMD) and 95% confidence interval (CI), while binary variables were expressed as odds ratio (OR) and 95% CI. Q test and I2 were used for heterogeneity analysis, and I2 value was used to evaluate the magnitude of heterogeneity. If P > .1 and I2 < 50%, it indicated that the heterogeneity among included studies was small, and the fixed effect model was used for analysis. If P < .1 and I2 ≥ 50%, it suggested obvious heterogeneity among included studies. The source of heterogeneity was analyzed and the random effect model was used for analysis.
2.8.2. Dealing with missing data
If the data are incomplete or not reported in the study, the researcher will contact the first author or other authors of these studies by telephone or email. If we cannot get the required data, we will use descriptive analysis instead of meta-analysis, if necessary, eliminate these studies.
2.8.3. Subgroup analysis
In order to address the heterogeneity between studies, subgroup analyses were conducted according to race (e.g., yellow, white, etc), region (e.g., European, Asian, etc) and population (high-risk populations with hypertension, diabetes, heart disease, and healthy low-risk populations).
2.8.4. Sensitivity analysis
To test the stability of meta-analysis results, we use Stata 16.0 to perform sensitivity analysis using one-by-one exclusion.
2.8.5. Assessment of reporting biases
We will use funnel plot to qualitatively identify publication bias, and use Egger and Begg test to quantitatively evaluate publication bias. If the funnel plot is asymmetric and P < .05, it is considered to have obvious publication bias.
2.8.6. Evidence quality evaluation
For studies that can achieve meta-analysis, we will use the Grading of Recommendation Assessment, Development and Evaluation (GRADE) scoring method to grade the evidence of its outcome indicators.[14] Evaluation includes risk of bias, indirectness, inconsistency, inaccuracy, publication bias, and the quality of evidence will be rated as high, medium, low, or very low.
3. Discussion
Breast cancer is the most common cancer among women, and the incidence of breast cancer is increasing globally due to factors that are not fully understood. The pathogenesis of breast cancer is complex, and the relationship between gene polymorphism and the risk of breast cancer has attracted extensive attention. Precision therapy is the direction of breast cancer treatment at present. With the increasing attention of HLA in tumor immunity, we can find suitable tumor specific antigen peptide as tumor vaccine, and provide new methods and ideas for the prevention and treatment of breast cancer.[15]
HLA is the most complex and polymorphic gene in human, which is related to the occurrence of many kinds of tumors, and has always been a hot in tumor immunity research.[16,17] HLA consists of closely linked I, II, III genes. HLA-DRB1 is the most polymorphic locus of HLA-II genes, it is mainly involved in the immune process of tumor body,[18] mainly expressed on the surface of APC cells (macrophages, dendritic cells, and B cells). It presents exogenous antigens to CD4+ regulatory T cells, helper T cells (Th) and inhibitory T cells (Ts) and participates in the immune response process.[19] HLA-DRB1, as an immune effector molecule, plays an important role in the occurrence and development of breast cancer. By studying the association of HLA-DRB1 and breast cancer, it is helpful for early diagnosis, early treatment, and prognosis of breast cancer.
At present, there have been studies on the correlation between HLA-DRB1 gene polymorphism and breast cancer. Because of the different genetic background, environmental factors, and research methods, the regional differences are also great. Studies suggest that DRB1∗12, DRB1∗1801, and DRB1∗1501 are highly expressed in breast cancer populations in Iran, Mexico, Istanbul, and Greece, respectively.[20] Studies have also found that DRB1∗01, DRB1∗13, and DRB1∗15 are not associated with risk of breast cancer in Jordan.[21] Ghaderi et al[22] have found that HLA-DRB1∗12 are susceptible genes to breast cancer, while Gun et al[23] found that HLA-DRB1 ∗ 03 is a protective gene of breast cancer. The reason for inconsistency is that the protocol itself is still affected by population characteristics or other factors. This study will explore the relationship between HLA-DRB1 gene polymorphism and breast cancer by systematic review and meta-analysis.
Due to the limitation of language retrieval, we only included Chinese and English literature in this study, and may ignore the research of other languages. Factors such as race, skin color, and disease may cause some clinical heterogeneity.
Author contributions
Data collection: Linlin Liu and Xu Sun
Data curation: Linlin Liu, Xu Sun.
Funding acquisition: Huaimin Liu.
Funding support: Huaimin Liu
Resources: Xu Sun and Chenxi Yuan
Software operating: Chenxi Yuan and Huaimin Liu
Software: Chenxi Yuan, Huaimin Liu.
Supervision: Chenxi Yuan.
Writing – original draft: Linlin Liu and Xu Sun
Writing – review & editing: Linlin Liu and Huaimin Liu
Footnotes
Abbreviations: AHRQ = Agency for Healthcare Research and Quality, CI = confidence interval, GRADE = Grading of Recommendation Assessment, Development and Evaluation, HLA = human leukocyte antigen, IARC = International Agency for Research on Cancer, MHC = major histocompatibility complex, NOS = Newcastle-Ottawa Scale, OR = odds ratio, OSF = open science framework, PRISMA-P = preferred reporting items for systematic reviews and meta-analyses protocols, SMD = standard mean difference, Th = helper T cells, Ts = inhibitory T cells.
How to cite this article: Liu L, Sun X, Yuan C, Liu H. Relationship between HLA-DRB1 gene polymorphism and breast cancer: a protocol for systematic review and meta-analysis. Medicine. 2021;100:12(e25078).
This work is supported by the Joint Project of National Natural Science Foundation of China (No. U2004105) and The Natural Science Foundation of Henan Province is a face-to-face project (No. 202300410450)
The authors have no conflicts of interest to disclose.
Private information from individuals will not be published. This systematic review also does not involve endangering participant rights. Ethical approval will not be required. The results may be published in a peer-reviewed journal or disseminated at relevant conferences.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87–108. [DOI] [PubMed] [Google Scholar]
- [2].Huang CX, Cheng LH, Liu YZ, et al. A study on the relationship between allele polymorphism of HLA-DRB1 seat and genetic susceptibility to breast cancer. Int J Lab Med 2011;32:728–30. +33. [Google Scholar]
- [3].Madigan MP, Ziegler RG, Benichou J, et al. Proportion of breast cancer cases in the United States explained by well-established risk factors. J Natl Cancer Inst 1995;87:1681–5. [DOI] [PubMed] [Google Scholar]
- [4].de Andrade DR, Jr, de Andrade DR. The influence of the human genome on chronic viral hepatitis outcome. Rev Inst Med Trop Sao Paulo 2004;46:119–26. [PubMed] [Google Scholar]
- [5].Halloran PF, Reeve JP, Pereira AB, et al. Antibody-mediated rejection, T cell-mediated rejection, and the injury-repair response: new insights from the Genome Canada studies of kidney transplant biopsies. Kidney Int 2014;85:258–64. [DOI] [PubMed] [Google Scholar]
- [6].Ji SZ, Mu NR, Mu SJ. Advances in HLA-DRB1 and common tumor susceptibility. Chongqing Med 2016;45:831–3. [Google Scholar]
- [7].Chaudhuri S, Cariappa A, Tang M, et al. Genetic susceptibility to breast cancer: HLA DQB∗03032 and HLA DRB1∗11 may represent protective alleles. Proc Natl Acad Sci U S A 2000;97:11451–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mahmoodi M, Nahvi H, Mahmoudi M, et al. HLA-DRB1,-DQA1 and -DQB1 allele and haplotype frequencies in female patients with early onset breast cancer. Pathol Oncol Res 2012;18:49–55. [DOI] [PubMed] [Google Scholar]
- [9].Baccar Harrath A, Yacoubi Loueslati B, Troudi W, et al. HLA class II polymorphism: protective or risk factors to breast cancer in Tunisia? Pathol Oncol Res 2006;12:79–81. [DOI] [PubMed] [Google Scholar]
- [10].Cantú de León D, Pérez-Montiel D, Villavicencio V, et al. High resolution human leukocyte antigen (HLA) class I and class II allele typing in Mexican mestizo women with sporadic breast cancer: case-control study. BMC Cancer 2009;9:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2016;354:i4086. [DOI] [PubMed] [Google Scholar]
- [12].Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [13].Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 2015;8:2–10. [DOI] [PubMed] [Google Scholar]
- [14].Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014;349:g5630. [DOI] [PubMed] [Google Scholar]
- [15].Jin Y, Liu ZY, Gao P, et al. Recent developments and development directions on breast cancer. Chin J Pract Surg 2021;41:80–4. [Google Scholar]
- [16].Aureli A, Canossi A, Del Beato T, et al. HLA-DRB1∗13:01 allele in the genetic susceptibility to colorectal carcinoma. Int J Cancer 2015;136:2464–8. [DOI] [PubMed] [Google Scholar]
- [17].Nunes LM, Ayres FM, Francescantonio IC, et al. Association between the HLA-G molecule and lymph node metastasis in papillary thyroid cancer. Hum Immunol 2013;74:447–51. [DOI] [PubMed] [Google Scholar]
- [18].Ji SZ, Gulizhareye A, Zhu XL, et al. Analysis polymorphism of breast cancer and HLA-DRB1 in Xinjiang Uygur and Han. Chin J Cancer Prev Treat 2015;22:1791–6. [Google Scholar]
- [19].Taneja V, David CS. Role of HLA class II genes in susceptibility/resistance to inflammatory arthritis: studies with humanized mice. Immunol Rev 2010;233:62–78. [DOI] [PubMed] [Google Scholar]
- [20].Anagnostouli M, Anagnostoulis G, Katsavos S, et al. HLA-DRB1 15:01 and Epstein-Barr virus in a multiple sclerosis patient with psoriasis, nasopharyngeal and breast cancers: lessons for possible hidden links for autoimmunity and cancer,. J Neurol Sci 2014;339:26–31. [DOI] [PubMed] [Google Scholar]
- [21].Atoum MF, Tanashat RQ, Mahmoud SA. Negative association of the HLA-DQB1∗02 allele with breast cancer development among Jordanians. Asian Pacific J Cancer Prev 2013;14:7007–10. [DOI] [PubMed] [Google Scholar]
- [22].Ghaderi A, Talei A, Gharesi-Fard B, et al. HLA-DBR 1 alleles and the susceptibility of Iranian patients with breast cancer. Pathol Oncol Res 2001;7:39–41. [DOI] [PubMed] [Google Scholar]
- [23].Gun FD, Ozturk OG, Polat A, et al. HLA class-II allele frequencies in Turkish breast cancer patients. Med Oncol 2012;29:466–71. [DOI] [PubMed] [Google Scholar]


