Abstract
Objectives
The Interdisciplinary Cardiac Arrest Research Review (ICARE) group was formed in 2018 to conduct an annual search of peer‐reviewed literature relevant to cardiac arrest. Now in its third year, the goals of the review are to highlight annual updates in the interdisciplinary world of clinical cardiac arrest research with a focus on clinically relevant and impactful clinical and population‐level studies from 2020.
Methods
A search of PubMed using keywords related to clinical research in cardiac arrest was conducted. Titles and abstracts were screened for relevance and sorted into 7 categories: Epidemiology & Public Health Initiatives; Prehospital Resuscitation, Technology & Care; In‐Hospital Resuscitation & Post‐Arrest Care; Prognostication & Outcomes; Pediatrics; Interdisciplinary Guidelines & Reviews; and a new section dedicated to the coronavirus disease 2019 (COVID‐19) pandemic. Screened manuscripts underwent standardized scoring of methodological quality and impact on the respective fields by reviewer teams lead by a subject matter expert editor. Articles scoring higher than 99 percentiles by category were selected for full critique. Systematic differences between editors’ and reviewers’ scores were assessed using Wilcoxon signed‐rank test.
Results
A total of 3594 articles were identified on initial search; of these, 1026 were scored after screening for relevance and deduplication, and 51 underwent full critique. The leading category was Prehospital Resuscitation, Technology & Care representing 35% (18/51) of fully reviewed articles. Four COVID‐19 related articles were included for formal review that was attributed to a relative lack of high‐quality data concerning cardiac arrest and COVID‐19 specifically by the end of the 2020 calendar year. No significant differences between editor and reviewer scoring were found among review articles (P = 0.697). Among original research articles, section editors scored a median 1 point (interquartile range, 0–3; P < 0.01) less than reviewers.
Conclusions
Several clinically relevant studies have added to the evidence base for the management of cardiac arrest patients including methods for prognostication of neurologic outcome following arrest, airway management strategy, timing of coronary intervention, and methods to improve expeditious performance of key components of resuscitation such as chest compressions in adults and children.
Keywords: cardiopulmonary resuscitation, emergency medical services, epidemiology, heart arrest, out‐of‐hospital cardiac arrest, sudden cardiac death
1. INTRODUCTION
1.1. Background
Recent estimates of the global burden of out‐of‐hospital cardiac arrest report an annual incidence of 14–147 per 100,000 persons with considerable variability across global regions and age groups. 1 Ongoing improvements in the form of novel approaches to care for these patients are continually being presented from social, clinical, and pharmacologic perspectives to reduce the significant morbidity and mortality of cardiac arrest.
1.2. Importance
Given the broad scope of cardiac arrest research across multiple disciplines, the Interdisciplinary Cardiac Arrest Research Review (ICARE) Group was created in 2018. This review, now in its third iteration, systematically gathers and summarizes articles in multiple disciplines with relevance or value to the realm of cardiac arrest research in keeping with the PRISMA‐ScR guidelines. As a scoping review rather than a systematic review focused on a specific research question, this review looks to serve as an annual update on clinically relevant cardiac arrest research.
1.3. Goals of this investigation
This manuscript focuses on the major updates in epidemiologic and clinical cardiac arrest research. The intent of the ICARE review is to be a resource both for clinicians and academic researchers by referencing the most clinically relevant developments from the previous year.
2. METHODS
The methods for the 2020 ICARE edition are adopted from the Global Emergency Medicine Literature Review group's methodology as detailed in the procedure manual (Supporting Information 1) and are consistent with PRISMA‐ScR guidelines and the 2019 review published previously. 2 , 3 Additional manual screening to prevent inadvertent omissions was also performed. The 2020 ICARE working group is comprised of 67 members, including 54 reviewers, 9 editors, and 4 senior editors. All editors have previously published cardiac arrest research. The working group consists of physicians, scientists, medical students, and graduate students from multiple disciplines and educational backgrounds relevant to the field of cardiac arrest. All working group members are unpaid and selected through an application process before literature search. As a scoping review, this review was registered on OSFHome as protocol osf.io/4gzbw.
2.1. Literature search
Publications pertaining to cardiac arrest were searched on PubMed in 2 phases: the first included publications between January and August 2020 and was conducted in October 2020, and the second included publications between September and December 2020 and was conducted in January 2021. Queries were limited to PubMed due to the clinical focus of PubMed and the sheer number of articles returned. To filter by article publication dates, both literature searches were performed using the “[PDAT]” PubMed/MEDLINE field description tag. Therefore, articles with either an “Electronic Date of Publication” and/or “Print Date of Publication” in 2020 were included. Articles that were included in prior iterations were manually excluded by technical and section editors. Inclusion and exclusion criteria were consistent with previous ICARE reviews. 2 , 4 Only articles that were available in English were included. Publications that were commentaries, editorials, case reports, study design protocols, data releases, and letters to the editor were excluded. The full PubMed/MEDLINE search query is presented in Supporting Information 2. We continued to use the search string used for the 2019 edition. 2
2.2. Article screening
The titles and abstracts of articles identified were screened by the technical and section editors independently based on detailed inclusion and exclusion criteria (Supporting Information 1). The kappa statistic for agreement on article inclusion at this stage was calculated to determine consistency in the screening process. Full texts of selected articles for scoring were classified as either Original Research or Review according to the study design. The articles were classified into 7 thematic categories: Epidemiology & Public Health; Prehospital Resuscitation, Technology & Care Processes; In‐Hospital Resuscitation & Post‐Arrest Care Processes; Prognostication & Outcomes; Pediatrics; Interdisciplinary Guidelines & Reviews; and the Coronavirus disease 2019 (COVID‐19) pandemic. Results pertaining to basic science and pharmacology studies are available as a supplement on request.
2.3. Article scoring
The scoring scale originally adapted from the annual Global Emergency Medicine Literature Review and used in both prior ICARE reviews was again used according to the study type—original research or review. 2 , 3 , 4 Each article was scored independently by reviewers, and scores were verified by each section editor. Scoring scales for original research and review articles are presented in Tables 1 and 2. In addition to the reviewers’ scoring, each article's “Impact” and “Importance” was graded independently by the section editor. Total scores ranged between 0 and 22 points and were calculated using the reviewer's “Clarity” and “Design” scores and the section editor's “Importance” and “Impact” scores. To ensure scoring reliability among the working group, random articles were selected and the reviewer and editor scores of each were compared for quality control. Systematic differences between editor and reviewer scores for each of the quality control articles were assessed using Wilcoxon signed‐rank test.
TABLE 1.
Scoring of original research articles
| Quality measure | Question | Points | |
|---|---|---|---|
| Design A | Select one | Descriptive studies (including case studies and case series, natural observation studies and descriptive surveys) | 1 ‐or‐ |
| Correlation studies (case control studies, prospective observational studies, retrospective studies) | 2 ‐or‐ | ||
| Non‐randomized or non‐blinded experimental studies | 3 ‐or‐ | ||
| Randomized, blinded experimental studies | 4 | ||
| Design B | Study design is appropriate to answer the authors’ hypothesis | 1 | |
| Design C | Correct statistical tests are used to analyze the data | 1 | |
| Design D | Results are presented accurately and without bias | 1 | |
| Design E | Limitations are clearly described, and the conclusions are supported by data | 1 | |
| Design total | 8/out of max score 8 | ||
| Ethics A | The study was approved by an institutional review board (IRB)/institutional animal use and care committee, ethics committee, community group, as required by local laws | 1 | |
| Ethics B | Informed consent was obtained or consent was waived by the IRB (give point if not applicable, e.g., animal study) | 1 | |
| Ethics C | The authors declare their conflicts of interest or declare that none exist | 2 | |
| Ethics total | 4/out of a max of 4 | ||
| Importance A | The study results are not specific to one certain patient population but are broadly generalizable to a variety of settings | 2 | |
| Importance B | The topic being studied is an important one, in that it advances the field of cardiac arrest research or care | 2 | |
| Importance C | The study is clearly relevant to the realm of cardiac arrest research or care | 1 | |
| Importance total | 5/out of a max of 5 | ||
| Impact | The findings or recommendations of this study may be feasibly implemented by practitioners a of cardiac arrest care | ||
| Impact A | Practitioners a would likely change their practice if they were aware of this study | 2 | |
| Impact B | The authors of this study raise interesting questions that may stimulate further research | 2 | |
| Impact C | The findings or recommendations of this study may be feasibly implemented by practitionersa of cardiac arrest care | 1 | |
| Impact total | 5/out of a max of 5 | ||
aPractitioner: reader practicing in the category of the article (physician, epidemiologist, pharmacist etc).
TABLE 2.
Scoring of review articles
| Quality measure | Question | Points |
|---|---|---|
| Clarity A | The review has a clearly stated hypothesis or purpose | 2 |
| Clarity B | The authors provide sufficient background to put the results of the review into context | 1 |
| Clarity C | The review can be understood by someone with general medical or public health training | 1 |
| Clarity D | The authors use clear language and appropriate graphs, tables, and figures throughout the article | 1 |
| Clarity total | 5/out of max score 5 | |
| Design A | This is a formal meta‐analysis or a systematic review that only includes studies with a control group | 3 |
| Design B | There is a clear, reproducible method for the selection of studies included in this review | 2 |
| Design C | Articles for this review were selected by at least 2 authors blinded to each other's selection | 1 |
| Design D | The data was aggregated and/or analyzed appropriately | 1 |
| Design total | 7/out of max score 7 | |
| Importance A | The review is not specific to one certain patient population but is broadly generalizable to a variety of settings | 2 |
| Importance B | The topic being reviewed is an important one, in that it advances the field of cardiac arrest research or care | 2 |
| Importance C | This is clearly relevant to the realm of cardiac arrest research or care | 1 |
| Importance total | 5/out of max score 5 | |
| Impact A | The findings or recommendations of this review appear to have applicability toward improving cardiac arrest research or care | 2 |
| Impact B | Practitioners a would likely change their practice if they were aware of this review | 2 |
| Impact C | The authors of this review raise interesting questions that may stimulate further research | 1 |
| Impact total | 5/out of max score 5 |
aPractitioner: reader practicing in the category of the article (physician, epidemiologist, pharmacist etc).
2.4. Formal article review
Articles scoring in the 99th percentile by category and type were evaluated for a formal review with accompanying summary. To reduce the likelihood of imperfect but high‐impact articles unintentionally being excluded from formal summarization, articles that scored one point below the 99th percentile score were discussed in a committee consisting of 3 editorial members. Reviewers then summarized these articles with attention to the objective, key findings, and strengths/limitations of each study. Section editors then reviewed summaries for content, accuracy, and style according to each category.
3. RESULTS
The screening, scoring, and full article review process is presented in Figure 1. A total of 3594 articles were identified on initial search; of these, 1026 were scored after screening for relevance and deduplication, and 51 scored in the 99th percentile for their respective sections and underwent full critique and summarization. A further 45 articles that scored 1 point below the 99th percentile threshold for their given sections were also reviewed for inclusion and full review by the Editorial board. Full summaries of the top scoring cardiac arrest articles of 2020 identified by our review are available as Supporting Information 3. Inter‐rater reliability between the screening editors revealed a Cohen's κ score of 0.83 (95% confidence interval [CI], 0.78–0.87). Article scoring statistics for each article category are summarized in Table 3. Table 4 summarizes the articles reviewed. The scores for all Original Research and Review articles are presented in Supporting Information 4 and 5, respectively. The leading category was Prehospital Resuscitation, Technology & Care representing 35% (18/51) of fully reviewed articles. No significant differences between editor and reviewer scoring were found among review articles (P = 0.697). Among original research articles, section editors scored a median 1 point (interquartile range [IQR], 0–3; P < 0.01) less than reviewers. The median and IQR of scores by reviewer and editors for each category are presented in Supporting Information 6. The threshold for 99th percentile for each section was a total score over 17 for Epidemiology & Public Health, over 18 for Prehospital Resuscitation, Technology & Care Processes, over 16 for In‐Hospital Resuscitation & Post‐Arrest Care Processes, over 17 for Prognostication & Outcomes, over 16 for Pediatrics, over 14 for Interdisciplinary Guidelines & Reviews, and over 16 for COVID‐19‐related articles.
FIGURE 1.
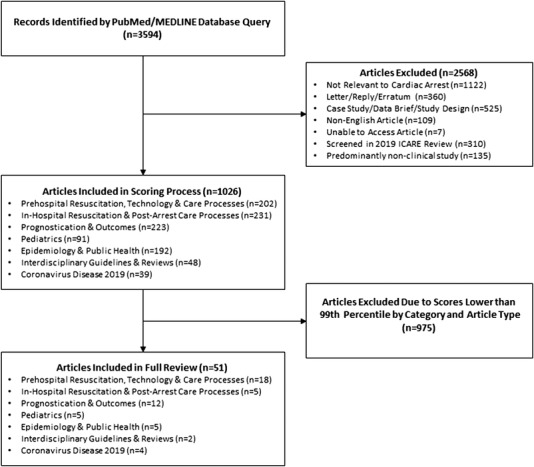
Flowchart of screening and scoring process
TABLE 3.
2020 summary statistics of reviewer scoring by category and article type
| Article category | Original research | Review | ||
|---|---|---|---|---|
| Count (%) | Median (IQR) | Count (%) | Median (IQR) | |
| Epidemiology and Public Health | 171 (17.8) | 15 (13–17) | 21 (10.6) | 12 (9–16) |
| Prehospital Resuscitation, Technology, and Care Processes | 177 (18.4) | 16 (15–18) | 25 (12.6) | 16 (14–19) |
| In‐Hospital Resuscitation and Post‐Arrest Care Processes | 186 (19.3) | 16 (15–18) | 45 (22.7) | 16 (13–19) |
| Prognostication and Outcomes | 205 (21.3) | 16 (14–18) | 18 (9.1) | 17 (16–19) |
| Pediatrics | 77 (8.0) | 16 (15–17) | 14 (7.1) | 16 (13–21) |
| Coronavirus Disease 2019 | 29 (3.0) | 16 (14–16) | 10 (5.1) | 15.5 (14–16) |
| Interdisciplinary Guidelines and Reviews | — | — | 48 (24.2) | 14 (13–18) |
| Totals | 845 (100.0) | 16 (14–18) | 181 (100.0) | 16 (13–19) |
TABLE 4.
Brief summaries of articles by category
| First author, journal | Title | Type | Summary |
|---|---|---|---|
| Prehospital Resuscitation, Technology and Care Processes | |||
| Bartos J, Circulation | Improved Survival with Extracorporeal Cardiopulmonary Resuscitation Despite Progressive Metabolic Derangement Associated with Prolonged Resuscitation | OR | Transport of out‐of‐hospital cardiac arrest patients with shockable rhythms and ongoing CPR to a cardiac catheterization laboratory for ECPR improved neurologically favorable survival at all CPR durations <60 min |
| Chou E, Resuscitation | Association of Ultrasound‐Related Interruption during Cardiopulmonary Resuscitation with Adult Cardiac Arrest Outcomes: A Video‐Reviewed Retrospective Study | OR | This retrospective cohort study finds that brief echocardiography (ECHO)‐related interruption, ≤2 ECHO‐related interruptions, and ECHO‐related no‐flow time between 77–122 s during cardiopulmonary resuscitation (CPR) are associated with improved outcomes in cardiac arrest |
| Cournoyer A, Resuscitation | Can a Shockable Initial Rhythm Identify Out‐of‐Hospital Cardiac Arrest Patients with a Short No‐flow Time? | OR | Presence of an initial shockable rhythm in out‐of‐hospital cardiac arrest does not correlate with a short no‐flow time |
| Coute R, Am J Emerg Med | The Association Between Scene Time Interval and Neurologic Outcome Following Adult Bystander Witnessed Out‐of‐Hospital Cardiac Arrest | OR | Longer scene time intervals by Emergency Medical Services is positively correlated with poorer neurological outcomes in bystander‐witnessed out‐of‐hospital cardiac arrest patients |
| Felder S, Can J Emerg Med | Decreasing Time to First Shock: Routine Application of Defibrillation Pads in Prehospital STEMI | OR | This retrospective study finds that routine application of defibrillation pads to patients with prehospital ST‐elevation myocardial infarction (STEMI) reduces time to initial defibrillation in out‐of‐hospital cardiac arrest (OHCA) |
| Grunau B, JAMA | Association of Intra‐arrest Transport vs Continued On‐Scene Resuscitation with Survival to Hospital Discharge Among Patients with Out‐of‐Hospital Cardiac Arrest | OR | Continued on‐scene resuscitation was associated with higher probability of survival to hospital discharge and more favorable neurologic outcomes than patients transported intra‐arrest |
| Kedan I, Cardiovasc Ultrasound | Prognostic value of point‐of‐care ultrasound during cardiac arrest: a systematic review | RE | Cardiac motion detected by ultrasound during cardiac arrest resuscitation is correlated with return of spontaneous circulation |
| Lee SGW, Am J Emerg Med | Time to First Defibrillation and Survival Outcomes of Out‐of‐Hospital Cardiac Arrest with Refractory Ventricular Fibrillation | OR | Shorter times to first defibrillation attempt led to significantly improved neurological outcomes in OHCA patients with refractory ventricular fibrillation |
| Sarkisian L, Resuscitation | Global Positioning System Alerted Volunteer First Responders Arrive Before Emergency Medical Services in More Than Four Out of Five Emergency Calls | OR | Use of a GPS smartphone application to reach out to volunteer first responders during out‐of‐hospital cardiac arrest could have benefit on time of arrival of a first responder with an automated external defibrillator |
| Sinden S, Resuscitation | The Association of Scene‐Access Delay and Survival with Favourable Neurological Status in Patients with Out‐of‐Hospital Cardiac Arrest | OR | The curb‐to‐care time—time from EMS arrival to patient attendance—showed improved OHCA outcomes when reduced, suggesting there should be further effort to improve quick EMS access to OHCA patients on‐scene |
| Stangenes R, Resuscitation | Delays in Recognition of the Need for Telephone‐Assisted CPR Due to Caller Descriptions of Chief Complaint | OR | Caller description of chief complaints affects the time taken to recognize the need for telephone‐assisted CPR |
| Szarpak L, Am J Emerg Med | Survival, Neurological and Safety Outcomes after Out‐of‐Hospital Cardiac Arrests Treated by Using Prehospital Therapeutic Hypothermia: A Systematic Review and Meta‐Analysis | RE | Prehospital therapeutic hypothermia did not demonstrate any improvement in survival or neurologic outcome |
| Tan BKK, Resuscitation | Clinical Evaluation of Intravenous Alone Versus Intravenous or Intraosseous Access for Treatment of Out‐of‐Hospital Cardiac Arrest | OR | Attempting intraosseous access after intravenous access failure led to an improved rate of vascular success and earlier epinephrine administration, but was not associated with improved survival outcomes in EMS‐treated OHCA patients |
| Wagner P, BMJ Open | In Out‐of‐Hospital Cardiac Arrest, Is the Positioning of Victims by Bystanders Adequate for CPR? A Cohort Study | OR | Approximately one‐third of bystanders position victims of cardiac arrest in a suitable position for CPR; victims placed in the “supine position” with effective chest compressions were found to have better neurologic outcomes |
| Wang CH, Ann Emerg Med | Comparing Effectiveness of Initial Airway Interventions for Out‐of‐Hospital Cardiac Arrest: A Systematic Review and Network Meta‐analysis of Clinical Controlled Trials | RE | Supraglottic airway devices proved to be the most effective at attaining ROSC; supraglottic airway devices, intubation, and bag‐valve masks were equally effective with survival to hospital discharge and neurologic outcome at discharge |
| Zalewski R, J Thoracic Dis | The Use of Prefilled Adrenaline Syringes Improves Cardiopulmonary Resuscitation Quality—High‐Fidelity Simulator‐Based Study | OR | Simplification of cardiopulmonary resuscitation by prefilling syringes with medications instead of using glass ampoules may significantly improve the quality of CPR by a 2‐person team |
| Zhang Y, Resuscitation | Intravenous Versus Intraosseous Adrenaline Administration in Out‐of‐Hospital Cardiac Arrest: A Retrospective Cohort Study | OR | With regard to ROSC, survival and favorable neurologic outcome, IV administration of epinephrine appears to be superior to IO administration during OHCA resuscitations |
| In‐Hospital Resuscitation and Post‐Arrest Care Processes | |||
| Ameloot K, J Am Coll Cardiol | Optimum Blood Pressure in Patients with Shock after Acute Myocardial Infarction and Cardiac Arrest | OR | In patients experiencing acute myocardial infarction (AMI) and cardiac arrest with shock, targeting a mean arterial pressure (MAP) goal between 80/85 and 100 mm Hg with vasopressors and inotropes during the initial 36 h in the ICU resulted in lower hs‐cTnT values, indicating smaller myocardial injury |
| Liao X, Critical Care |
Effects of Endovascular and Surface Cooling on Resuscitation in Patients with Cardiac Arrest and a Comparison of Effectiveness, Stability, and Safety: A Systematic Review and Meta‐Analysis. |
RE |
This meta‐analysis compared endovascular cooling with surface cooling for the induction of therapeutic hypothermia in adult patients with cardiac arrest |
| Liu B, J Int Med Res | Steroid Use after Cardiac Arrest Is Associated with Favourable Outcomes: A Systematic Review and Meta‐Analysis | RE | This systematic review found treatment with steroids after all causes of cardiac arrest significantly increased both rate of ROSC and survival to discharge |
| Orso D, Respir Care | Mechanical Ventilation Management During Mechanical Chest Compressions | RE | This review discusses multiple invasive ventilation strategies that have been employed in the mechanical ventilation of cardiac arrest patients |
| Verma B, JACC‐Cardiovasc Interv | Coronary Angiography in Patients with Out‐of‐Hospital Cardiac Arrest without ST‐Segment Elevation: A Systematic Review And Meta‐Analysis | RE | This meta‐analysis showed that in patients who have experienced out‐of‐hospital cardiac arrest without ST‐segment elevation, there is no 30‐day neurological or mortality benefit with early coronary angiography when compared to non‐early |
| Prognostication and Outcomes | |||
| Admiraal MM, Neurology | EEG Reactivity Testing for Prediction of Good Outcome in Patients after Cardiac Arrest | OR | EEG background reactivity, when assessed twice a day using a rigorous protocol, holds additional prognostic value in distinguishing patients with higher chances of achieving independence by 6 months post‐arrest |
| Barbella G, Neurology | Prediction of Regaining Consciousness Despite an Early Epileptiform EEG after Cardiac Arrest | OR | In a retrospective cohort comprised of comatose anoxic brain injury patients with epileptiform activity on EEG, a cutoff of 2 in the NEC2RAS score—a combined 6‐point score of electroencephalographic features—was 100% sensitive in predicting consciousness recovery with an AUC of 0.96 |
| Barbella G, Resuscitation | Prognostic Role of EEG Identical Bursts in Patients after Cardiac Arrest: Multimodal Correlation | OR | Burst suppression with identical bursts on EEG remained 100% specific in predicting poor outcome in hypoxic‐ischemic brain injured patients; however, it did not add to the predictive performance when incorporated in a multimodal model |
| Beuchat I, Neurology | MRI‐EEG Correlation for Outcome Prediction in Postanoxic Myoclonus | OR | Post‐anoxic myoclonus is prevalent following cardiac arrest and is traditionally, yet not universally, associated with a poor prognosis |
| Düring J, Critical Care | Copeptin as a Marker of Outcome after Cardiac Arrest: a Sub‐Study of the TTM Trial | OR | Copeptin, a surrogate biomarker of vasoregulatory status, holds promise identifying patients with severe post‐cardiac arrest syndrome at risk for cardiovascular deterioration and early death |
| Ebner F, Resuscitation | Serum GFAP and UCH‐L1 for the Prediction of Neurological Outcome in Comatose Cardiac Arrest Patients | OR | Serial serum GFAP and UCH‐L1 combined measurements are more sensitive than neuron specific enolase in predicting poor outcome following out of hospital cardiac arrest |
| Guy A, Resuscitation | The Relationship Between No‐Flow Interval and Survival with Favourable Neurological Outcome in Out‐of‐Hospital Cardiac Arrest: Implications for Outcomes and ECPR Eligibility | OR | In witnessed cardiac arrests without bystander CPR, the duration of no‐flow time carries important prognostic ability discriminating patients in whom a functional state is achievable |
| Moseby‐Knappe M, Intensive Care Med | Performance of a Guideline‐Recommended Algorithm for Prognostication of Poor Neurological Outcome after Cardiac Arrest | OR | The 2015 European Resuscitation Council and European Society of Intensive Care Medicine algorithm for post‐cardiac arrest prognostication, maintained 100% specificity for a poor outcome prediction when applied to the TTM 1 cohort, albeit with low sensitivity at 38.7% |
| Reynolds JC, Resuscitation | Prognostication with Point‐of‐Care Echocardiography During Cardiac Arrest: A Systematic Review | RE | Insufficient evidence exists supporting the use of point‐of‐care echocardiography as a prognostic tool, unveiling the need for high‐quality research with standardized timepoints and definitions for outcomes, as well as control for sources of biases on this topic |
| Sandroni C, Intensive Care Med | Prediction of Poor Neurological Outcome in Comatose Survivors of Cardiac Arrest: A Systematic Review | RE | False‐positive rates of 0% for poor outcome were retained by bilaterally absent ocular reflexes after day 4 post‐arrest, high titers of neuron specific enolase after 24 h post‐arrest, diffusion restriction on brain MRI from 2–5 days post‐arrest, diffuse cerebral edema on head CTH after 2 h post‐arrest, unequivocal seizures or bilaterally absent cortical potentials on somatosensory evoked potentials at any point post‐arrest |
| Scarpino M, Resuscitation | Does a Combination of ≥2 Abnormal Tests vs. the ERC‐ESICM Stepwise Algorithm Improve Prediction of Poor Neurological Outcome after Cardiac Arrest? A Post‐Hoc Analysis of the ProNeCA Multicentre Study | OR | A prognostication strategy combining ≥2 among bilateral absence of pupillary light reflex, cortical peaks on somatosensory evoked potentials, malignant features on EEG, diffuse cerebral edema on CT and status myoclonus |
| Wang CH, Resuscitation | Neuroprognostic Accuracy of Blood Biomarkers for Post‐Cardiac Arrest Patients: A Systematic Review and Meta‐Analysis | RE | In this systematic review and meta‐analysis of 42 studies with a total of 4806 patients, neuron‐specific enolase (NSE) and S‐100B demonstrated comparably high specificities for predicting poor neurologic outcome after cardiac arrest |
| Pediatrics | |||
| Chang CY, Int J Environ Res Pu | Analysis of Chest‐Compression Depth and Full Recoil in Two Infant Chest‐Compression Techniques Performed by a Single Rescuer: Systematic Review and Meta‐Analysis | RE | Results of this review and meta‐analysis of randomized controlled trials demonstrate that the 2‐thumb technique surpasses the 2‐finger technique in the outcome of chest compression depth whereas the 2‐finger technique is superior to the 2‐thumb technique in achieving complete chest recoil |
| Chang C, Int J Environ Res Pu | Two‐Thumb or Two‐Finger Technique in Infant Cardiopulmonary Resuscitation by a Single Rescuer? A Meta‐Analysis with GOSH Analysis. | RE | This meta‐analysis compares the 2 techniques available for infant chest compressions: 2‐thumb vs. 2‐finger |
| Lee W, PLoS ONE | Differences in the Performance of Resuscitation According to the Resuscitation Guideline Terminology During Infant Cardiopulmonary Resuscitation: “Approximately 4 cm” Versus “At Least One‐Third of the Anterior‐Posterior Diameter of the Chest” | OR | Current guidelines for infants recommend a chest compression depth (CCD) of “approximately 4 cm” or “at least one‐third the anterior‐posterior diameter of the chest” simultaneously |
| Siebert J, J Med Internet Res | The Impact of a Tablet App on Adherence to American Heart Association Guidelines During Simulated Pediatric Cardiopulmonary Resuscitation: Randomized Controlled Trial | OR | In simulated cases of pediatric pulseless ventricular tachycardia, this blinded randomized controlled trial showed that using a PALS guiding application increased adherence to AHA guidelines in comparison to the traditional PALS pocket card |
| Topjian A, Circulation | Part 4: Pediatric Basic and Advanced Life Support‐2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care | RE | This review examines the American Heart Association's newest cardiopulmonary resuscitation (CPR guidelines); the guidelines expand on the Chain of Survival and the sequence of resuscitation while reaffirming evidence‐based CPR components |
| Epidemiology and Public Health | |||
| Baldi E, Simul Healthc | A Multicenter International Randomized Controlled Manikin Study on Different Protocols of Cardiopulmonary Resuscitation for Laypeople: The MANI‐CPR Trial | OR | 30c2s (30 compressions and 2s pause) and 50c5s (50 compression and 5s pause) cardiopulmonary resuscitation (CPR) protocols utilized by laypeople in out‐of‐hospital cardiac arrest (OHCA) events offer better quality CPR compared to continuous compressions |
| Feng D, Intern Emerg Med | Gender Differences and Survival after an Out‐of‐Hospital Cardiac Arrest: A Systematic Review and Meta‐Analysis | RE | In a meta‐analysis, women are more likely to have significant survival benefit after cardiac arrest compared to men even though women are less likely to have shockable initial rhythm, witnessed arrest, and have CPR performed |
| Kalra R, Am J Cardiol | Cardiac Function and Sudden Cardiac Death in Heart Failure with Preserved Ejection Fraction (from the TOPCAT Trial) | OR | Left ventricular global longitudinal strain may be an independent predictor of sudden cardiac death and aborted cardiac arrest |
| Liu J, Heart Rhythm | Improvement in Sudden Cardiac Death Risk Prediction by the Enhanced American College of Cardiology/American Heart Association Strategy in Chinese Patients with Hypertrophic Cardiomyopathy | OR | When compared to the 2011 ACC/AHA and 2014 ESC guidelines, the 2019 enhanced ACC/AHA strategy had the best predictive utility of cardiac arrest risk in a Chinese cohort |
| Scquizzato T, Resuscitation | Enhancing Citizens Response to Out‐of‐Hospital Cardiac Arrest: A Systematic Review of Mobile‐Phone Systems to Alert Citizens As First Responders | RE | This systematic review and meta‐analysis explored research that utilized mobile technology to alert citizens to act as first responders for patients experiencing out‐of‐hospital cardiac arrest (OHCA) |
| Interdisciplinary Guidelines and Review | |||
| Olasveengen TM, Circulation | Adult Basic Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations | RE | The 2020 Basic Life Support (BLS) guidelines provide a comprehensive update to BLS treatment recommendations |
| Holmberg MJ, Resuscitation | Oxygenation and Ventilation Targets after Cardiac Arrest: A Systematic Review and Meta‐Analysis | RE | The optimal oxygenation and ventilation targets in survivors of cardiac arrest remain unclear, though evidence continues to support targeting normoxemia and normocapnia in post‐arrest patients |
| Coronavirus Disease 2019 | |||
| Gruneau B, Resuscitation Plus | Bystanders Are Less Willing to Resuscitate Out‐of‐Hospital Cardiac Arrest Victims During the COVID‐19 Pandemic | OR | Members of the general public are less likely to check for pulses/breathing, and less likely to perform resuscitative measures on out‐of‐hospital cardiac arrest victims during the COVID‐19 pandemic, as compared to before the pandemic onset; however, willingness to intervene increases when personal protective equipment is made available |
| Latsios G, Hellenic J Cardiol | Cardiopulmonary Resuscitation in Patients with Suspected or Confirmed COVID‐19. A Consensus of the Working Group on Cardiopulmonary Resuscitation of the Hellenic Society of Cardiology | RE | The COVID‐19 pandemic presented unprecedented challenges in performing cardiopulmonary resuscitation (CPR) safely both in and out of clinical settings; this review incorporates the needed adjustments to basic and advanced life support to ensure provider safety and patient survivorship |
| Zheng JL, Resuscitation | Incidence and Outcome of Out‐of‐Hospital Cardiac Arrests in the COVID‐19 Era: A Systematic Review and Meta‐Analysis | RE | Evaluation of how the COVID‐19 pandemic affected the incidence and outcomes of Out of Hospital Cardiac Arrests (OHCA); it was found that OHCA rates were increased during the COVID‐19 pandemic and this may be due to a lack of optimization in pre‐ and in‐hospital resuscitation methods |
Abbreviations: OR, Original Research; RE, Review.
The following sections highlight the critical findings of the top‐scoring articles. More in‐depth discussions and summaries of the data from each study are available in Supporting Information 3.
3.1. Epidemiology and public health initiatives
Provision of high‐quality bystander cardiopulmonary resuscitation (CPR) is a crucial link in the chain of survival for patients with out‐of‐hospital cardiac arrest. There is ongoing work to encourage improved access to effective bystander CPR, with several articles focusing on this topic specifically. 5 , 6 , 7 Additional work to identify the best recommendations for chest compressions found that pausing for 2 seconds after 50 compressions generated the most reliable proportion of adequate compressions among lay volunteers. 6 This is an increase in the number of chest compressions from current American Heart Association (AHA) Basic Life Support (BLS) guidelines for healthcare providers. 8
In predicting cardiac arrest among specific populations, impaired left ventricular ejection fraction and left ventricular global longitudinal strain were both associated with an increased risk of sudden cardiac death. 9 , 10 Specifically, global longitudinal strain was most predictive and had an increased hazard ratio of 58% with each increasing unit of strain. 9 In a validation of existing predictive models developed with Western patients, a study of Chinese patients with hypertrophic cardiomyopathy found the 2019 combined American College of Cardiology/American Heart Association model to have a positive predictive value of 66% for cardiac arrest during the observational period compared to other guidelines. 10
3.2. Prehospital resuscitation, technology and care processes
A common theme of the prehospital literature from 2020 was the focus on timeliness in cardiac arrest management. Times to specific endpoints were the primary outcomes of interest in 9 articles. 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 Endpoints included time elapsed until recognition of cardiac arrest, contact with first responders, defibrillation, establishment of vascular access, epinephrine administration, resumption of chest compressions after pulse check, and definitive care in a hospital. 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 Overall, although a reduced time to each intervention during resuscitation was not uniformly shown to improve survival or neurologic outcome, no harms from more rapid intervention for each of the parameters listed above were noted. Moreover, delays in arrival or in initiation of a given therapy continued to demonstrate increased odds of poor outcomes as measured by cerebral performance category (CPC). 15 Mean scene time was 19 minutes for survivors with CPC 1 or 2 and 23 minutes for those with CPC 3 or 4 (P < 0.001). Two regression models showed that for every 1‐minute increase in scene time, the adjusted odds for a poor outcome (death or CPC of 3 or 4) increased by 3.5% (P < 0.001) with an inflection point at 20 minutes. 15 Variability in resources and response strategies worldwide limits direct comparison between separate emergency response systems; the ideal strategy for responding to out‐of‐hospital cardiac arrest should be tailored to each region's unique capabilities.
Another study emphasizing the importance of high‐quality chest compressions found that when echocardiogram‐related interruptions in chest compressions were limited to less than 3 events, rates of return of spontaneous circulation (ROSC) (odds ratio [OR], 5.55; 95% CI, 2.44–12.61; P < 0.001) and survival to hospital discharge improved (OR, 7.31; 95% CI, 1.59–33.59; P = 0.01). 18 Patients with non‐echocardiogram‐related interruptions totaling less than 43 seconds also had significantly increased rates of ROSC and survival, in keeping with current AHA recommendations to limit interruptions in chest compressions. 18 , 21 A separate meta‐analysis found that cardiac motion detected on ultrasound was positively associated with ROSC, especially in patients with shockable initial rhythms, although no specific or objective threshold was identified. 22
Other studies sought to describe the significance of a shockable initial rhythm, patient positioning, choice of airway device, and prehospital temperature reduction techniques on survival and neurologic outcomes. 20 , 23 , 24 , 25 Patient positioning by lay rescuers was found to be non‐ideal (ie, not supine on a firm surface) most of the time, and the presence of an initial shockable rhythm was found to be a poor predictor of no‐flow time, the time elapsed between onset of cardiac arrest and CPR initiation, with 36% sensitivity and 66% specificity. 23 , 24
Two systematic reviews with meta‐analyses comparing initial airway strategy and prehospital targeted temperature management with patient survival and neurologic outcomes found no difference in mortality or outcome among airway and temperature interventions. 12 , 25 , 26 These findings further support the recommendations of the International Liaison Committee on Resuscitation from 2019 and findings of the PRINCESS trial. 12 , 27 , 28 , 29 Interpreting these data in a clinical context, the ICARE group believes that supraglottic airway devices may be a viable alternative in areas with infrequent airway experience or relatively lower first‐pass intubation success rates and that targeted temperature management with chilled intravenous fluids may lead to harm from pulmonary edema or fluid overload.
A statistically significant 16% absolute increase in discharge with favorable neurologic outcome (CPC 1 or 2) was found in 39% (n = 52) of patients in a historically controlled, descriptive retrospective study with refractory ventricular fibrillation receiving extracorporeal therapy. 30 These findings, although limited by indication bias, suggest the potential benefits of extracorporeal support for patients in prolonged resuscitation. The open‐label, randomized ARREST trial by the same group did show a survival benefit with extracorporeal support in refractory ventricular fibrillation. 31
3.3. In‐hospital resuscitation and post‐arrest care
A systematic review and meta‐analysis comparing endovascular and surface cooling for survival and favorable neurologic outcome defined by CPC 1 or 2 found endovascular cooling methods achieve goal temperature sooner and more reliably without significant effects on survival or neurologic outcome compared to surface cooling. 26
A narrative review of mechanical ventilation for patients receiving mechanical CPR advocated for maintaining high FiO2, but heterogeneity in the compared models (a mix of pre‐clinical animal models and clinical studies) invites further study of other ventilation parameters. 32
Data regarding objective targets for goal‐directed pharmacologic therapy remains mixed. 33 Pooled data from 2 separate randomized controlled trials found higher blood pressure goals through vasopressor use corresponded with lower troponin levels suggesting the presence of smaller infarcts, without an increased risk of repeat arrest or atrial fibrillation. 34 Survival and rates of favorable neurologic outcome as determined by CPC were similar between cohorts, which suggest the benefits of titration to markers of end‐organ perfusion rather than specific blood pressure goals. Another systematic review and meta‐analysis studied steroid administration after cardiac arrest with pooled data from 5 randomized controlled trials and 2 cohort studies and found steroid use correlated with a statistically significant increased survival to hospital discharge (relative risk [RR], 1.67; 95% CI, 1.16–2.40; P < 0.005). 35
Optimal timing for cardiac catheterization after cardiac arrest remains controversial in patients without ST‐segment elevation. 36 , 37 A meta‐analysis found no improvement in outcomes despite shorter intervals to catheterization after arrest, which comports with the relatively low percentage of intervenable lesions for non‐ST‐segment elevation arrests identified in the COACT trial. 36 Together, these studies suggest that catheterization for non‐ST‐segment elevation cardiac arrests is less time‐sensitive than for patients with ST‐segment elevations.
3.4. Prognostication and outcomes
Several methods for predicting patient outcomes during and after cardiac arrest have been proposed, guiding ongoing resuscitative efforts.
The time from onset of arrest to the initiation of CPR in witnessed arrests was investigated, retrospectively; the probability of achieving a favorable outcome, defined as modified Rankin scale (mRS) scores of 0–3, decreased by 13% (adjusted RR, 0.87; 95% CI, 0.85–0.90) for each minute of delay. 38 Further, no favorable outcomes were observed in patients with no‐flow times longer than 10 minutes. 38
Magnetic resonance imaging (MRI), ultrasound, and electroencephalography (EEG) have also been proposed as methods to determine the likelihood of a patient regaining neurologic function following cardiac arrest. A retrospective cohort study found that despite epileptiform activity, patients with background continuity ≥50%, absence of epileptiform abnormalities, preserved reactivity on initial and/or repeat EEG, normal background amplitude, and stimulus‐induced rhythmic, periodic, or ictal discharges on subsequent EEG had favorable outcome (CPC 1–3 within 3 months of arrest), whereas burst suppression with identical bursts on EEG were 100% specific in predicting poor outcome. 39 , 40 Preserved EEG reactivity specifically following cardiac arrest predicted functional independence at 6 months after arrest. 41 The combination of MRI and EEG for determining outcome for patients with post‐anoxic myoclonus found that absence of injury on MRI and preserved EEG background continuity had a positive predictive value of 91% for ability to follow commands and negative predictive value of 99% for coma recovery. 42 A brain death determination strategy that combined at least 2 findings among bilaterally absent pupillary light reflex, bilaterally absent cortical potentials on somatosensory evoked potentials, malignant features on EEG, diffuse cerebral edema on computed tomography (CT), and status myoclonus achieved higher specificity than the 2015 European Resuscitation Council‐European Society of Intensive Care Medicine (ERC‐ESICM) prognostication algorithm when predicting death or dependence at 6 months post‐cardiac arrest. Although ERC‐ESICM algorithm demonstrated higher sensitivity (63[56–71]% vs 49[41–57]%; P < 0.0001), the strategy of any combination of 2 or more abnormal tests had lower false‐positive rates (0[0–8]% vs 7[1–18]%; P < 0.0001). 43 Although post‐arrest brain imaging and EEG were predictive of neurologic outcome using CPC, intra‐arrest echocardiographic findings were not predictive. 44
Neuron‐specific enolase (NSE), glial fibrillary acidic proteins (GFAP), ubiquitin C‐terminal hydrolase (UCH‐L1), and S‐100B were among the biomarkers most tested for their prognostic significance after cardiac arrest. 45 , 46 , 47 , 48 A systematic review and meta‐analysis of NSE and S‐100B as prognostic markers following cardiac arrest found that each had high specificity with NSE pooled specificity of 0.99 (95% CI, 0.98–1.00) and S‐100B pooled specificity of 0.97 (95% CI, 0.92–1.00). 46 The 2015 ERC‐ESICM guidelines included NSE as part of a multi‐modal assessment of mental status but noted that NSE levels did not affect the specificity of the assessment. 49 GFAP and UCH‐L1 were evaluated as a pair in the initial 72 hours among patients enrolled in the international target temperature management (TTM) trial, and this combined measurement was more specific for poor neurologic function defined by CPC at 6 months following cardiac arrest than NSE alone. 45
A systematic review of the heterogenous field of neuroprognostication research found no false‐positives for prediction of poor outcome (defined as severe neurologic disability, persistent vegetative state, or death, corresponding to a CPC of 3–5 or mRS score of 5–6) if patients had bilaterally absent ocular reflexes after 4 days post‐arrest, high titers of NSE after 24 hours post‐arrest, diffusion restriction on brain MRI from 2–5 days post‐arrest, diffuse cerebral edema on head CT after 2 hours post‐arrest, unequivocal seizures, or bilaterally absent cortical potentials on somatosensory evoked potentials at any point post‐arrest. 48
3.5. Pediatrics
Updating previous recommendations, the AHA reiterated the importance of high‐quality CPR and the equivalence of bag‐mask ventilation to advanced airway interventions in out‐of‐hospital cardiac arrest. 50 Other additions included administering epinephrine within 5 minutes of arrest, targeting higher respiratory rates (20–30 per minute) for infants and children, and promoting cuffed endotracheal tubes. 50 Cricoid pressure during bag‐mask ventilation and use of naloxone for patients suspected of ingestion were discouraged. 50 In a simulation study, an electronic application was found to enhance adherence to guidelines better than traditional pocket cards. 51 Another simulation trial found that the chest compression depth target of “at least one‐third the anterior‐posterior diameter of the chest” resulted in appropriately deep chest compressions and recoil compared to the target of “approximately 4 cm” as worded in current guidelines. 52 A systematic review and meta‐analysis demonstrated that the 2‐thumb technique surpassed the 2‐finger technique with respect to chest compression depth, whereas the 2‐finger technique was superior to the 2‐thumb technique in achieving complete chest recoil. 53
3.6. Interdisciplinary guidelines and reviews
The 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care with Treatment Recommendations (CoSTR) for BLS provide the most comprehensive update to BLS guidelines since 2015. Although the goal of guideline review committees was to produce new systematic review recommendations, the evidence for each of the recommendations was often noted by the guideline committee to be based largely on low‐certainty data.
Dispatcher assisted‐compression only CPR was strongly recommended for out‐of‐hospital cardiac arrest and is in keeping with specific research dedicated to the topic. 54 , 55 , 56 Compression only‐CPR was recommended over conventional CPR for lay rescuers, whereas conventional CPR was recommended for emergency medical services (EMS) personnel and in‐hospital cardiac arrest. Placement of patients on a firm surface and starting with chest compressions was recommended. 54 In the hospital, moving a patient from a hospital bed to the floor to improve chest compression quality was discouraged. 54 Immediate resumption of CPR after rhythm checks was recommended and in keeping with current advanced cardiac life support guidelines. 54 Audiovisual feedback devices during CPR were recommended as part of quality improvement programs, but not in isolation. 54 Back slaps followed by abdominal thrusts were recommended for foreign‐body airway obstructions in adults and children older than 1 year. 54 Chest thrusts were recommended for use in unconscious patients with airway obstruction. 54 Manual extraction of visible items and blind finger sweeps were recommended in airway obstruction. Magill forceps were recommended for skilled healthcare providers. 54 Stronger recommendations were made for lone bystanders with a mobile device to call EMS for help before starting CPR and to start CPR without concern of causing harm but the quality of evidence for these positions remained low. 54 Cough CPR and pre‐cordial thump were strongly recommended against. 54 The impact of COVID‐19 on these recommendations was not assessed. As with pediatric guidelines, screening for cognitive and emotional injury post discharge was recommended as part of the Chain of Survival. 57 This recommendation reflects a larger research emphasis on recovery and survivorship after cardiac arrest across all patient populations.
Another systematic review and meta‐analysis sought to identify the optimal targets for oxygenation and ventilation after cardiac arrest with the evidence supporting targeted normoxemia and normocapnia in post‐arrest patients. 58 Post‐arrest hyperoxia was associated with worse outcomes and moderate hypercapnia had similar outcomes when compared with normocapnia. 58
3.7. COVID‐19 and cardiac arrest
COVID‐19 significantly impacted many aspects of life and a significant proportion of the scientific output in 2020. Although research regarding the intersection between COVID‐19 and cardiac arrest was carried out by several groups around the world, relatively little COVID‐19 research was directed at cardiac arrest specifically. Many of the articles pertaining to COVID‐19 in the context of cardiac arrest were recommendations based on local practices, although some studies provided guidance for future research.
In one of the largest systematic reviews published in 2020, the incidence, prevalence, and mortality rates for all‐cause out‐of‐hospital cardiac arrest from 35,379 arrests during the pandemic found a 120% increase in out‐of‐hospital arrests and increased mortality rates since the COVID‐19 pandemic began. 59 Time from onset of arrest to ambulance arrival was noted to be longer, and supraglottic airway devices were used more often than endotracheal intubations. Automated external defibrillator use and rates of ROSC were both higher prior to the pandemic. Similarly, bystanders were less likely to participate in the assessment or resuscitation of a theoretical patient during the pandemic. The presence of personal protective equipment increased theoretical willingness to intervene, but willingness to intervene remained less than pre‐pandemic levels. 60 A unique simulation trial from Poland demonstrated increasing fatigue among rescuers performing chest compressions while wearing full protective equipment and recommended changing compressors every minute rather than every 2 minutes if mechanical CPR devices were not being used. 61
For resuscitating known COVID‐19 patients, the Hellenic Society of Cardiology recommended full PPE for staff, defibrillation as early as feasible, limitations of the personnel involved, and an emphasis on high‐quality chest compressions over ventilation when responders have already been in close contact with the victim, such as in nursing homes. 62 Authors in the state of Georgia reported disproportionately high mortality rates for COVID‐19‐positive patients experiencing cardiac arrest, leading some authors to suggest that CPR in these patients is futile. 63 A group in Colombia provided an ethical framework for addressing the dual risks of increased rates of cardiac arrest with increased risk of viral transmission though aerosol generation during resuscitation. 64
4. DISCUSSION
Cardiac arrest remains a leading cause of morbidity and mortality worldwide. Although, advances in research aim to improve our understanding of cardiac arrest medicine, there is an ever‐growing number of publications in the field of cardiac arrest medicine that makes staying apprised of current literature difficult, time‐consuming, and resource intensive.
General trends in clinical cardiac arrest research in the year 2020 included continued efforts to determine the ideal sequence and timing of resuscitation. The findings of improved chest compressions with an altered timing from that recommended by more recent guidelines warrants further study as improved quality of bystander CPR has been associated with improved outcomes of resuscitative efforts.
The ideal manner for prediction of functional outcomes continues to be an area of focus, and in the opinion of the authors, should be tailored to a given community's resources as certain biomarkers may or may not be available to all centers.
Although noted as a therapy to be considered in the most recent guidelines, extracorporeal support in cardiac arrest has undergone more direct study, with certain locales publishing impressive results, though certain geographic factors may limit the wider adoption of this strategy. 31 , 65
In medical management of resuscitation, there is strong evidence to suggest the inclusion of steroids in cardiac arrest management, which would be a notable change from current guidelines.
Work studying the influence of the global pandemic on cardiac arrest care is expected to be relevant for as long as COVID continues to impact medical facilities worldwide. The impact of potential future outbreaks on community emergency management may become more relevant than ever as different variants of the virus circulate.
In the first 2 iterations of ICARE reviewing cardiac arrest literature published in 2018 and 2019, our group reviewed 1214 and 1364 papers, respectively. 2 , 4 In this third iteration of the ICARE review, we reviewed 1026 cardiac arrest manuscripts. Although this number is less than prior years’, this number does not include the 135 studies dedicated to basic science and pharmacological research reported separately.
Moreover, we noted a decrease in the number and a temporal lag of published manuscripts during this year's iteration, likely due to various factors associated with the COVID‐19 pandemic. As indicated by the findings of Gao et al, 66 the COVID‐19 pandemic impacted the scientific research mission in many ways, especially disrupting research that did not specifically address the virus. The findings of this group suggest that researchers likely worked on existing projects, wrote manuscripts, revisited older topics, or wrote grants as opposed to pursuing new projects during the pandemic. 66 Without insight into each center's programming, this cannot be known with certainty, although the decline in research productivity was noted to be homogenous across the entire scientific community. 66
Despite the apparent decrease in published articles this iteration, the sheer volume of literature concerning cardiac arrest medicine is undeniable. There remains a need for a holistic and robust review that is not a narrow systematic review. This remains the objective of ICARE in seeking to provide a broad, multidisciplinary review for the clinician to be aware of the latest and most impactful updates.
We implemented several key methodological changes in this iteration of ICARE based on perceived deficiencies in previous iterations of ICARE. First, we noted that our screening and scoring protocol did not fully account for several impactful and clinically relevant articles during previous iterations of ICARE. In evaluating the source of these omissions, we realized that although the scoring of the articles was accurate and appropriate (eg, studies were not fully blinded or randomized, thereby losing points), nevertheless, the articles were landmark studies in resuscitation research. Because our objective is to provide clinicians with a broad update of impactful articles concerning cardiac arrest research, our protocol was modified and required all articles that scored within 1 point of the top 99th percentile of articles in a given section to be reviewed once more by the Section Editors and the Editorial Board. Of 22 articles that were nearly excluded from formal review, the Editorial Board elected to include 9 of these articles to perform a full critique.
Second, we recognized that the Importance and Impact sections are subjective, as opposed to the objective nature of the Design and Ethics categories. Therefore, the Importance and Impact sections require subject‐matter experts to provide a critical appraisal and score; therefore, we delegated the Importance and Impact scoring of each article to the section editors, who are subject‐matter experts.
5. LIMITATIONS
The 2020 Interdisciplinary Cardiac Arrest Research Review is not without limitations. First, the conclusions presented are descriptive of the current evidence for various aspects of cardiac arrest research but are insufficient to be considered comprehensive. The aim of this literature review is to highlight advances in the disparate fields of cardiac arrest medicine on an annual basis. An intrinsic shortcoming of this approach is that it does not provide extensive context, such as historical comparison as seen in a systematic review, or fully account for differences in systems of care. To address this concern, we provide article summaries and commentaries for additional context in Supporting Information 3. There is potential for bias in the inherently subjective “Impact” and “Importance” categories, although articles are screened and reviewed by multiple study team members to mitigate this risk. Additionally, while the methodology used to screen, select, and score articles is designed to capture the most relevant research, it is possible that other high‐quality publications may be inadvertently omitted. Last, to remain objective in this literature search, this review did not include letters to the editor, commentaries, and other editorials that can provide additional context when interpreting the impact of large studies.
6. CONCLUSION
In its third year, the Interdisciplinary Cardiac Arrest Research Review scored more than 1000 articles related to cardiac arrest, and after a rigorous scoring process, the group fully summarized 51 articles in 7 different categories. Although COVID‐19 dominated scientific literature and discussion throughout 2020, relatively little was directed at cardiac arrest specifically and many of the articles pertaining to COVID‐19 in the context of cardiac arrest were recommendations based on local practices with high‐quality data only recently being released. The impact of COVID‐19 on the epidemiology and treatment of cardiac arrest continues to be a subject of much interest. The top‐scoring articles from 2020 were focused on the prognostication of outcomes and trials of novel interventions to influence outcomes following cardiac arrest. The total number of articles relevant to cardiac arrest continues to demonstrate the need for an accessible guide that summarizes findings of clinically relevant research articles and serves as a reference for clinicians and scientists. ICARE's goal is to further the development of the field of cardiac arrest medicine by highlighting clinically relevant and impactful articles each year.
Supporting information
Supporting Information, Additional supporting information may be found online in the Supporting Information section at the end of the article.
Supporting Information
Supporting Information
Supporting Information
Supporting Information
Supporting Information
APPENDIX A.
A.1.
Interdisciplinary Cardiac Arrest Research Review (ICARE) 2020 Managing Editors, Editors, and Reviewers
Murphy TW, Cohen SA, Hwang CW, et al. Cardiac arrest: An interdisciplinary scoping review of clinical literature from 2020. JACEP Open. 2022;3:e12773. 10.1002/emp2.12773
Dr. Murphy, Dr. Hwang, and Mr. Cohen contributed equally to this manuscript.
The Interdisciplinary Cardiac Arrest Research Review (ICARE) group members who contributed to this manuscript are listed in Appendix A.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: David Wampler, PhD, LP.
REFERENCES
- 1. Wong CX, Brown A, Lau DH, et al. Epidemiology of sudden cardiac death: global and regional perspectives. Hear Lung Circ. 2019;28:6‐14. 10.1016/j.hlc.2018.08.026 [DOI] [PubMed] [Google Scholar]
- 2. Murphy TW, Cohen SA, Avery KL, et al. Cardiac arrest: an interdisciplinary scoping review of the literature from 2019. Resusc Plus. 2020;4:100037. 10.1016/j.resplu.2020.100037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schroeder ED, Jacquet G, Becker TK, et al. Global emergency medicine: a review of the literature from 2011. Acad Emerg Med. 2012. 10.1111/j.1553-2712.2012.01447.x [DOI] [PubMed] [Google Scholar]
- 4. Gul SS, Cohen SA, Avery L, et al. Cardiac arrest: an interdisciplinary review of the literature from 2018. Resuscitation. 2020;148:66‐82. 10.1016/j.resuscitation.2019.12.030 [DOI] [PubMed] [Google Scholar]
- 5. Scquizzato T, Pallanch O, Belletti A, et al. Enhancing citizens response to out‐of‐hospital cardiac arrest: a systematic review of mobile‐phone systems to alert citizens as first responders. Resuscitation. 2020;152:16. 10.1016/J.RESUSCITATION.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baldi E, Contri E, Burkart R, et al. A multicenter international randomized controlled manikin study on different protocols of cardiopulmonary resuscitation for laypeople. Simul Healthc. 2021;16:239‐245. 10.1097/sih.0000000000000505 [DOI] [PubMed] [Google Scholar]
- 7. Feng D, Li C, Yang X, Wang L. Gender differences and survival after an out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. Intern Emerg Med. 2021;16:765‐775. 10.1007/s11739-020-02552-4 [DOI] [PubMed] [Google Scholar]
- 8. Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S366‐S468. 10.1161/CIR.0000000000000916 [DOI] [PubMed] [Google Scholar]
- 9. Kalra R, Gupta K, Sheets R, et al. Cardiac function and sudden cardiac death in heart failure with preserved ejection fraction (from the TOPCAT Trial). Am J Cardiol. 2020;129:46‐52. 10.1016/j.amjcard.2020.04.038 [DOI] [PubMed] [Google Scholar]
- 10. Liu J, Wu G, Zhang C, et al. Improvement in sudden cardiac death risk prediction by the enhanced American College of Cardiology/American Heart Association strategy in Chinese patients with hypertrophic cardiomyopathy. Hear Rhythm. 2020;17:1658‐1663. 10.1016/j.hrthm.2020.04.017 [DOI] [PubMed] [Google Scholar]
- 11. Sarkisian L, Mickley H, Schakow H, et al. Global positioning system alerted volunteer first responders arrive before emergency medical services in more than four out of five emergency calls. Resuscitation. 2020;152:170‐176. 10.1016/j.resuscitation.2019.12.010 [DOI] [PubMed] [Google Scholar]
- 12. Wang CH, Lee AF, Chang WT, et al. Comparing effectiveness of initial airway interventions for out‐of‐hospital cardiac arrest: a systematic review and network meta‐analysis of clinical controlled trials. Ann Emerg Med. 2020;75:627‐636. 10.1016/j.annemergmed.2019.12.003 [DOI] [PubMed] [Google Scholar]
- 13. Lee SGW, Park JH, Ro YS, Hong KJ, Song KJ, Shin SD. Time to first defibrillation and survival outcomes of out‐of‐hospital cardiac arrest with refractory ventricular fibrillation. Am J Emerg Med. 2021;40:96‐102. 10.1016/j.ajem.2020.12.019 [DOI] [PubMed] [Google Scholar]
- 14. Tan BKK, Chin YX, Koh ZX, et al. Clinical evaluation of intravenous alone versus intravenous or intraosseous access for treatment of out‐of‐hospital cardiac arrest. Resuscitation. 2021;159:129‐136. 10.1016/j.resuscitation.2020.11.019 [DOI] [PubMed] [Google Scholar]
- 15. Coute RA, Nathanson BH, Kurz MC, McNally B, Mader TJ. The association between scene time interval and neurologic outcome following adult bystander witnessed out‐of‐hospital cardiac arrest. Am J Emerg Med. 2021;46:628‐633. 10.1016/j.ajem.2020.11.059 [DOI] [PubMed] [Google Scholar]
- 16. Stangenes SR, Painter IS, Rea TD, Meischke H. Delays in recognition of the need for telephone‐assisted CPR due to caller descriptions of chief complaint. Resuscitation. 2020;149:82‐86. 10.1016/j.resuscitation.2020.02.013 [DOI] [PubMed] [Google Scholar]
- 17. Zalewski R, Puslecki M, Kłosiewicz T, Sip M, Perek B. The use of prefilled adrenaline syringes improves cardiopulmonary resuscitation quality‐high‐fidelity simulator‐based study. J Thorac Dis. 2020;12:2105‐2112. 10.21037/jtd.2020.04.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chou EH, Wang CH, Monfort R, et al. Association of ultrasound‐related interruption during cardiopulmonary resuscitation with adult cardiac arrest outcomes: a video‐reviewed retrospective study. Resuscitation. 2020;149:74‐80. 10.1016/j.resuscitation.2020.02.004 [DOI] [PubMed] [Google Scholar]
- 19. Felder S, Vanaarsen K, Davis M. Decreasing time to first shock: routine application of defibrillation pads in prehospital STEMI. Can J Emerg Med. 2019;22:82‐85. 10.1017/cem.2019.408 [DOI] [PubMed] [Google Scholar]
- 20. Grunau B, Kime N, Leroux B, et al. Association of intra‐arrest transport vs continued on‐scene resuscitation with survival to hospital discharge among patients with out‐of‐hospital cardiac arrest. JAMA ‐ J Am Med Assoc. 2020;324:1058‐1067. 10.1001/jama.2020.14185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S444‐S464. [DOI] [PubMed] [Google Scholar]
- 22. Kedan I, Ciozda W, Palatinus JA, Palatinus HN, Kimchi A. Prognostic value of point‐of‐care ultrasound during cardiac arrest: a systematic review. Cardiovasc Ultrasound. 2020;18:1. 10.1186/s12947-020-0185-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cournoyer A, de Montigny L, Potter BJ, et al. Can a shockable initial rhythm identify out‐of‐hospital cardiac arrest patients with a short no‐flow time? Resuscitation. 2021;158:57‐63. 10.1016/j.resuscitation.2020.11.012 [DOI] [PubMed] [Google Scholar]
- 24. Wagner P, Schloesser S, Braun J, Arntz HR, Breckwoldt J. In out‐of‐hospital cardiac arrest, is the positioning of victims by bystanders adequate for CPR? A cohort study. BMJ Open. 2020;10:e037676. 10.1136/bmjopen-2020-037676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Szarpak L, Filipiak KJ, Mosteller L, et al. Survival, neurological and safety outcomes after out of hospital cardiac arrests treated by using prehospital therapeutic hypothermia: a systematic review and meta‐analysis. Am J Emerg Med. 2021;42:168‐177. 10.1016/j.ajem.2020.02.019 [DOI] [PubMed] [Google Scholar]
- 26. Liao X, Zhou Z, Zhou M, et al. Effects of endovascular and surface cooling on resuscitation in patients with cardiac arrest and a comparison of effectiveness, stability, and safety: a systematic review and meta‐analysis. Crit Care 2020;24:27. 10.1186/s13054-020-2731-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Soar J, Maconochie I, Wyckoff MH, et al. 2019 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2019;140:e826‐e880. 10.1016/j.resuscitation.2019.10.016 [DOI] [PubMed] [Google Scholar]
- 28. Granfeldt A, Avis SR, Nicholson TC, et al. Advanced airway management during adult cardiac arrest: a systematic review. Resuscitation. 2019;139:133‐143. 10.1016/j.resuscitation.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 29. Nordberg P, Taccone FS, Truhlar A, et al. Effect of trans‐nasal evaporative intra‐arrest cooling on functional neurologic outcome in out‐of‐hospital cardiac arrest: the PRINCESS randomized clinical trial. JAMA 2019;321:1677‐1685. 10.1001/jama.2019.4149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bartos JA, Grunau B, Carlson C, et al. Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation. 2020;141:877‐886. 10.1161/CIRCULATIONAHA.119.042173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yannopoulos D, Bartos J, Raveendran G, et al. Advanced reperfusion strategies for patients with out‐of‐hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open‐label, randomised controlled trial. Lancet. 2020;396:1807‐1816. 10.1016/S0140-6736(20)32338-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Orso D, Vetrugno L, Federici N, et al. Mechanical ventilation management during mechanical chest compressions. Respir Care. 2021;66:334‐346. 10.4187/respcare.07775 [DOI] [PubMed] [Google Scholar]
- 33. Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post–cardiac arrest care. Circulation. 2010;122:S768‐S786. 10.1161/CIRCULATIONAHA.110.971002 [DOI] [PubMed] [Google Scholar]
- 34. Ameloot K, Jakkula P, Hästbacka J, et al. Optimum blood pressure in patients with shock after acute myocardial infarction and cardiac arrest. J Am Coll Cardiol. 2020;76:812‐824. 10.1016/j.jacc.2020.06.043 [DOI] [PubMed] [Google Scholar]
- 35. Liu B, Zhang Q, Li C. Steroid use after cardiac arrest is associated with favourable outcomes: a systematic review and meta‐analysis. J Int Med Res. 2020;48:300060520921670. 10.1177/0300060520921670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Verma BR, Sharma V, Shekhar S, et al. Coronary angiography in patients with out‐of‐hospital cardiac arrest without ST‐segment elevation: a systematic review and meta‐analysis. JACC Cardiovasc Interv. 2020;13:2193‐2205. 10.1016/j.jcin.2020.07.018 [DOI] [PubMed] [Google Scholar]
- 37. Barbarawi M, Zayed Y, Kheiri B, et al. Optimal timing of coronary intervention in patients resuscitated from cardiac arrest without ST‐segment elevation myocardial infarction (NSTEMI): a systematic review and meta‐analysis. Resuscitation. 2019;144:137‐144. 10.1016/j.resuscitation.2019.06.279 [DOI] [PubMed] [Google Scholar]
- 38. Guy A, Kawano T, Besserer F, et al. The relationship between no‐flow interval and survival with favourable neurological outcome in out‐of‐hospital cardiac arrest: implications for outcomes and ECPR eligibility. Resuscitation. 2020;155:219‐225. 10.1016/j.resuscitation.2020.06.009 [DOI] [PubMed] [Google Scholar]
- 39. Barbella G, Novy J, Marques‐Vidal P, Oddo M, Rossetti AO. Prognostic role of EEG identical bursts in patients after cardiac arrest: multimodal correlation. Resuscitation. 2020;148:140‐144. 10.1016/j.resuscitation.2020.01.017 [DOI] [PubMed] [Google Scholar]
- 40. Barbella G, Lee JW, Alvarez V, et al. Prediction of regaining consciousness despite an early epileptiform EEG after cardiac arrest. Neurology. 2020;94:E1675‐E1683. 10.1212/WNL.0000000000009283 [DOI] [PubMed] [Google Scholar]
- 41. Admiraal MM, Horn J, Hofmeijer J, et al. EEG reactivity testing for prediction of good outcome in patients after cardiac arrest. Neurology. 2020;95:e653‐e661. 10.1212/WNL.0000000000009991 [DOI] [PubMed] [Google Scholar]
- 42. Beuchat I, Sivaraju A, Amorim E, et al. MRI‐EEG correlation for outcome prediction in postanoxic myoclonus: a multicenter study. Neurology. 2020;95:E335‐E341. 10.1212/WNL.0000000000009610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Scarpino M, Lolli F, Lanzo G, et al. Does a combination of ≥2 abnormal tests vs. the ERC‐ESICM stepwise algorithm improve prediction of poor neurological outcome after cardiac arrest? A post‐hoc analysis of the ProNeCA multicentre study. Resuscitation. 2021;160:158‐167. 10.1016/j.resuscitation.2020.12.003 [DOI] [PubMed] [Google Scholar]
- 44. Reynolds JC, Issa MS, Nicholson TC, et al. Prognostication with point‐of‐care echocardiography during cardiac arrest: a systematic review. Resuscitation. 2020;152:56‐68. 10.1016/j.resuscitation.2020.05.004 [DOI] [PubMed] [Google Scholar]
- 45. Ebner F, Moseby‐Knappe M, Mattsson‐Carlgren N, et al. Serum GFAP and UCH‐L1 for the prediction of neurological outcome in comatose cardiac arrest patients. Resuscitation. 2020;154:61‐68. 10.1016/j.resuscitation.2020.05.016 [DOI] [PubMed] [Google Scholar]
- 46. Wang CH, Chang WT, Su KI, et al. Neuroprognostic accuracy of blood biomarkers for post‐cardiac arrest patients: a systematic review and meta‐analysis. Resuscitation. 2020;148:108‐117. 10.1016/j.resuscitation.2020.01.006 [DOI] [PubMed] [Google Scholar]
- 47. Düring J, Annborn M, Cronberg T, et al. Copeptin as a marker of outcome after cardiac arrest: a sub‐study of the TTM trial. Crit Care. 2020;24:185. 10.1186/s13054-020-02904-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sandroni C, D'Arrigo S, Cacciola S, et al. Prediction of poor neurological outcome in comatose survivors of cardiac arrest: a systematic review. vol. 46. Springer; 2020. 10.1007/s00134-020-06198-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Moseby‐Knappe M, Westhall E, Backman S, et al. Performance of a guideline‐recommended algorithm for prognostication of poor neurological outcome after cardiac arrest. Intensive Care Med. 2020;46:1852‐1862. 10.1007/s00134-020-06080-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Topjian AA, Raymond TT, Atkins D, et al. Part 4: pediatric basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S469‐E523. 10.1161/CIR.0000000000000901 [DOI] [PubMed] [Google Scholar]
- 51. Siebert JN, Lacroix L, Cantais A, Manzano S, Ehrler F. The impact of a tablet app on adherence to American Heart Association Guidelines During Simulated Pediatric Cardiopulmonary Resuscitation: randomized controlled trial. J Med Internet Res 2020;22:e17792. 10.2196/17792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lee W, Yang D, Oh JH. Differences in the performance of resuscitation according to the resuscitation guideline terminology during infant cardiopulmonary resuscitation: “approximately 4 cm” versus “at least onethird the anterior‐posterior diameter of the chest.” PLoS One 2020;15:e0230687. 10.1371/journal.pone.0230687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chang CY, Lin PC, Chien YJ, Chen CS, Wu MY. Analysis of chest‐compression depth and full recoil in two infant chest‐compression techniques performed by a single rescuer: systematic review and meta‐analysis. Int J Environ Res Public Health. 2020;17:1‐17. 10.3390/ijerph17114018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Olasveengen TM, Mancini ME, Perkins GD, et al. Adult basic life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142:S41‐S91. 10.1161/CIR.0000000000000892 [DOI] [PubMed] [Google Scholar]
- 55. Chen KY, Ko YC, Hsieh MJ, Chiang WC, Ma MHM. Interventions to improve the quality of bystander cardiopulmonary resuscitation: a systematic review. PLoS One. 2019;14:e0211792. 10.1371/journal.pone.0211792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lewis M, Stubbs BA, Eisenberg MS. Dispatcher‐assisted cardiopulmonary resuscitation. Circulation. 2013;128:1522‐1530. 10.1161/CIRCULATIONAHA.113.002627 [DOI] [PubMed] [Google Scholar]
- 57. Sawyer KN, Camp‐Rogers TR, Kotini‐Shah P, et al. Sudden cardiac arrest survivorship: a scientific statement from the American Heart Association. Circulation. 2020;141:E654‐E685. 10.1161/CIR.0000000000000747 [DOI] [PubMed] [Google Scholar]
- 58. Holmberg MJ, Nicholson T, Nolan JP, et al. Oxygenation and ventilation targets after cardiac arrest: a systematic review and meta‐analysis. Resuscitation. 2020;152:107‐115. 10.1016/j.resuscitation.2020.04.031 [DOI] [PubMed] [Google Scholar]
- 59. Lim ZJ, Ponnapa Reddy M, Afroz A, Billah B, Shekar K, Subramaniam A. Incidence and outcome of out‐of‐hospital cardiac arrests in the COVID‐19 era: a systematic review and meta‐analysis. Resuscitation. 2020;157:248‐258. 10.1016/j.resuscitation.2020.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Grunau B, Bal J, Scheuermeyer F, et al. Bystanders are less willing to resuscitate out‐of‐hospital cardiac arrest victims during the COVID‐19 pandemic. Resusc Plus. 2020;4:100034. 10.1016/j.resplu.2020.100034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Małysz M, Smereka J, Jaguszewski M, et al. An optimal chest compression technique using personal protective equipment during resuscitation in the COVID‑19 pandemic: a randomized crossover simulation study. Kardiol Pol. 2020;78:1254‐1261. 10.33963/KP.15643 [DOI] [PubMed] [Google Scholar]
- 62. Latsios G, Synetos A, Mastrokostopoulos A, et al. CardioPulmonary resuscitation in patients with suspected or confirmed Covid‐19. A consensus of the working group on cardiopulmonary resuscitation of the Hellenic society of cardiology. Hell J Cardiol. 2021;62:24‐28. 10.1016/j.hjc.2020.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Shah P, Smith H, Olarewaju A, et al. Is cardiopulmonary resuscitation futile in coronavirus disease 2019 patients experiencing in‐hospital cardiac arrest? Crit Care Med. 2021;49:201‐208. 10.1097/CCM.0000000000004736 [DOI] [PubMed] [Google Scholar]
- 64. Rueda EA, Suárez E, Gempeler FE, et al. Ethical guidelines on cardiopulmonary resuscitation in the context of the COVID‐19 pandemic in Colombia. Biomedica. 2020;40:180‐187. 10.7705/BIOMEDICA.5762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hsu CH, Meurer WJ, Domeier R, et al. Extracorporeal cardiopulmonary resuscitation for refractory out‐of‐hospital cardiac arrest (EROCA): results of a randomized feasibility trial of expedited out‐of‐hospital transport. Ann Emerg Med. 2021;78:92‐101. 10.1016/J.ANNEMERGMED.2020.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gao J, Yin Y, Myers KR, Lakhani KR, Wang D. Potentially long‐lasting effects of the pandemic on scientists. Nat Commun. 2021;12:1‐6. 10.1038/s41467-021-26428-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information, Additional supporting information may be found online in the Supporting Information section at the end of the article.
Supporting Information
Supporting Information
Supporting Information
Supporting Information
Supporting Information


