Sir,
Syringomas are benign tumors of eccrine sweat gland origin that occur more frequently in women. Clinically, they appear as multiple, tiny, firm, skin-colored papules. The sites of predilection are the eyelids, malar regions, neck, and chest. Syringomas in the vulva are rare and asymptomatic and therefore overlooked.
A 32-year-old female presented to us with skin lesions over genitalia for 2 years, not associated with itching. There was a history of similar lesions near both eyes. There was no history of similar complaints in the family.
Examination of the vulva revealed the presence of multiple discrete dome-shaped skin-colored papules present over labia majora, measuring about 0.5–0.8 mm in diameter [Figure 1]. The lesions were nontender and symmetrically distributed. Similar lesions were present below both lower eyelids.
Figure 1.

Multiple dome-shaped skin-colored papules present over the labia majora
Punch biopsy was done from vulvar lesion and histopathological features were studied. Section showed epidermis with hyperkeratosis and increase in basal pigmentation [Figure 2]. Dermis showed multiple tubular ductal structures in dense collagenous stroma, lined by 2 layers of epithelial cells. Few ducts showed comma-like extensions, histological features consistent with syringoma [Figure 3].
Figure 2.
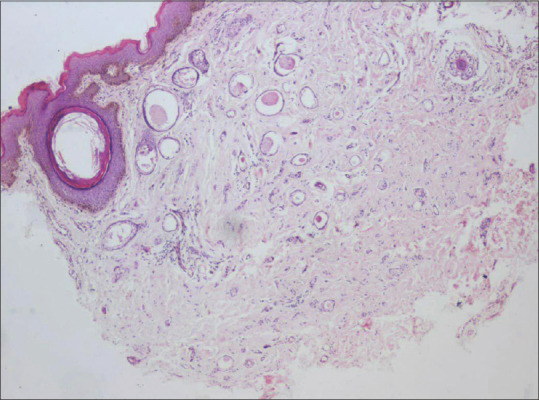
Epidermis showing hyperkeratosis and increase in basal pigmentation (×10)
Figure 3.
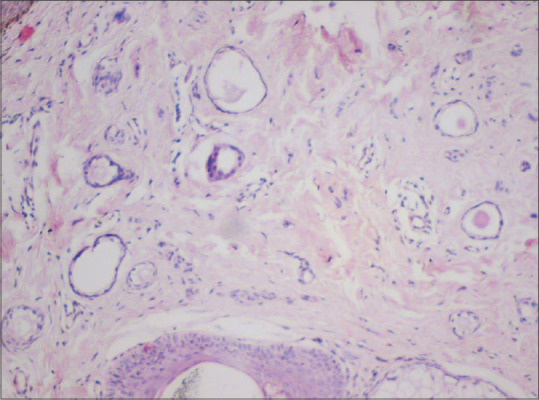
Dermis showing multiple tubular ductal structures with commalike extensions (×100)
Syringoma is a common benign tumor of eccrine sweat gland origin. It is more common in females. The characteristic presentations are multiple tiny skin-colored or yellowish papules over eyelids and may also involve neck, chest, axillae, and abdomen. Genital involvement is rare. Zalla and Perry in 1971 described syringomas confined to penis. Carnerio et al. were the first to report cases of vulval syringomas.[1]
About 34 cases have been reported till 2015.[2] The incidence of vulvar syringoma is approximately 1:1100–1500 as evaluated in large gynecological collections.[3]
Syringomas have been associated with Down syndrome, Marfan syndrome, and Ehlers–Danlos syndrome. Case of vulvar syringoma aggravated during pregnancy was reported by Bal et al.[4] Hormones may play a role in the development of syringomas. Wallace and Smoller demonstrated estrogen and progesterone receptor in syringomas.[5]
Clinically vulvar syringomas should be differentiated from Fox–Fordyce disease, multiple small epidermal cysts, senile angiomas, condyloma acuminata, and lymphangioma circumscriptum. Histopathologically, syringoma must be differentiated from microcystic adnexal carcinoma and desmoplastic trichoepithelioma. Treatment of syringoma is usually done for cosmetic issues.
Treatment modalities include surgical excision, electrodessication, cryotherapy, CO2 laser, and argon laser.[3] Topical treatments such as atropine sulfate and tretinoin have been successfully tried in pruritic syringoma to reduce pruritus. Our patient was counseled about the nature of the condition and its treatment modalities but the patient refused any treatment since it was asymptomatic. Syringomas over vulva is rare but it should be a part of differential diagnosis of multiple, papular lesions of the vulva.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zalla JA, Perry HO. An unusual case of syringoma. Arch Dermatol. 1971;103:215–7. [PubMed] [Google Scholar]
- 2.Ozdemir O, Sari ME, Sen E, Ozcanli G, Atalay C. Vulvar Syringoma in a Postmenopausal Woman. J Reprod Med. 2015;60(9-10):452–4. [PubMed] [Google Scholar]
- 3.Kopera D, Soyer HP, Cerroni L. Vulvar syringoma causing pruritus and carcinophobia: Treatment by argon laser. J Cutan Laser Ther. 1999;1:181–3. doi: 10.1080/14628839950516850. [DOI] [PubMed] [Google Scholar]
- 4.Bal N, Aslan E, Kayaselcuk F, Tarim E, Tuncer I. Vulvar syringoma aggravated by pregnancy. Pathol Oncol Res. 2003;9:196–7. doi: 10.1007/BF03033738. [DOI] [PubMed] [Google Scholar]
- 5.Wallace ML, Smoller BR. Progesterone receptor positivity supports hormonal control of syringomas. J Cutan Pathol. 1995;22:442–5. doi: 10.1111/j.1600-0560.1995.tb00760.x. [DOI] [PubMed] [Google Scholar]


