Abstract
Background:
Minimally invasive approaches to intra/extraforaminal lumbar disc herniations offer the benefit of less bone removal and reduced nerve root manipulation at the L5-S1 level. Moreover, the potential to better preserve stability.
Methods:
Here, we summarized the efficacy of the contralateral approach to intraforaminal/extraforaminal lumbar disc herniations particularly focusing on the L5-S1 level. Variables studied included the level of these disc herniations, their locations within the foramina, and the anatomy of the facet joints.
Results:
A major “pro” for the contralateral interlaminar procedure at the L5-S1 level is that it does not require facet joint removal, or with a spondylotic facet, <30% joint excision, to directly visualize the intraforaminal/ extraforaminal nerve root. It, therefore, reduces the risk of creating iatrogenic instability, while offering a higher certitude of adequate nerve root visualization, decompression, and safer disc removal.
Conclusion:
The contralateral interlaminar approach is more suitable for all types of intra/extraforaminal disc herniations at the L5/S1 level. The most specific benefit of this approach is its avoidance of disruption/significant removal (i.e., <30%) of the facet joint to adequately expose the foraminal L5 nerve root, and more safely remove the intra/extraforaminal disc herniation.
Keywords: Contralateral approach, Crossover technique, Intraforaminal lumbar disc herniation, Minimally invasive spine surgery, Over-the-top access, Spinal stability

INTRODUCTION
There is a 7–12% incidence of intra/extraforaminal lumbar disc herniations (IELDH).[1] One out of five patients will require surgery. Multiple operative approaches have been suggested for resection of IELDH. These include the unilateral interlaminar approach (warranting varying degrees of facet joint removal),[2,6,8] the transmuscular extraforaminal procedure,[4] various endoscopic approaches,[7] the endoscopic transiliac procedure, and the contralateral interlaminar approach.[8] Here, we have specifically focused on the safety/efficacy of the contralateral interlaminar approach to L5-S1 intra/extraforaminal L5-S1 disc herniations that critically avoid disrupting/removing none of a normal facet, or <30% of a spondylotic facet joint, thus averting instability. We treated all patients with FELDH at the L5-S1 level, with preforaminal discs with/without extension into the spinal canal, or for patients with purely intraforaminal discs, utilizing the contralateral interlaminar approach [Figures 1-4].
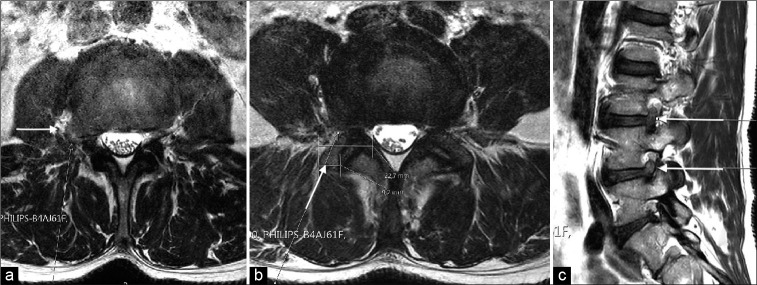
Figure 1:
(a) The presurgical T2 axial MRI arrow showed an extraforaminal disc herniation at the L5-S1 level with compression of the L5 root (white arrow). (b) The postsurgical T2 axial MRI images showed the disc herniation removed without violation of the facet joint (white arrow).
Figure 4:
(a) On the presurgical axial T2 MRI images at the L3-L4 level, the white arrow showed the correct extraforaminal trajectory indicating there would be no need for facet joint drilling, (b) the presurgical axial T2 MRI images at the L4-L5 level that included measurement of the facet joint complex, indicated possible facet joint removal, would be necessitated with an extraforaminal approach (i.e., 22.7 mm and 9.2 mm). Note, the white arrow indicated the appropriate extraforaminal trajectory, (c) on the presurgical sagittal T2 MRI, the white arrows pointed to an intraforaminal disc herniation at the L3-L4 and L4-L5 levels.
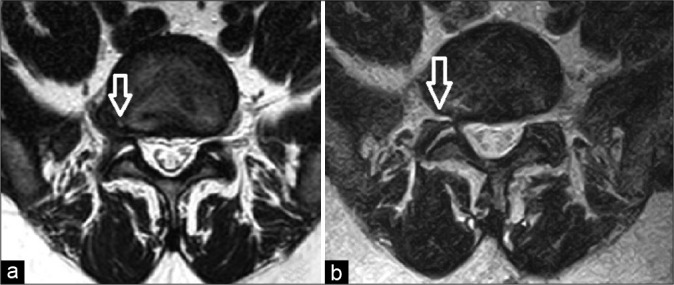
Figure 2:
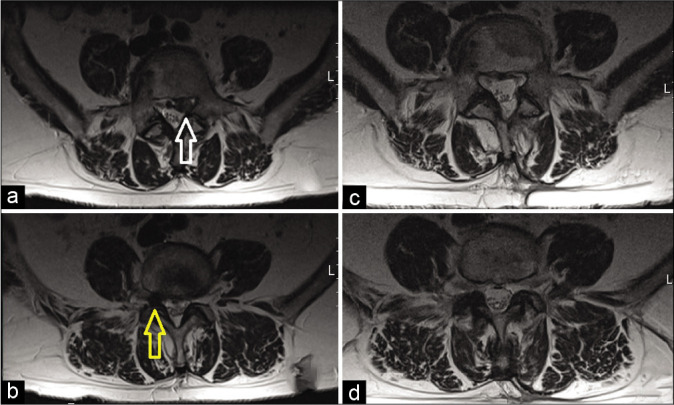
(a) The presurgical T2 axial MRI image and white arrow pointed to the left extruded disc herniation and (b) the presurgical T2 axial MRI showed a yellow arrow pointing to a purely intraforaminal disc herniation. (c) The postsurgical axial T2 MRI images showed removal of the left extruded disc herniation and (d) the postsurgical axial T2 MRI images showed the right intraforaminal disc herniation removed without facet violation.
Figure 3:
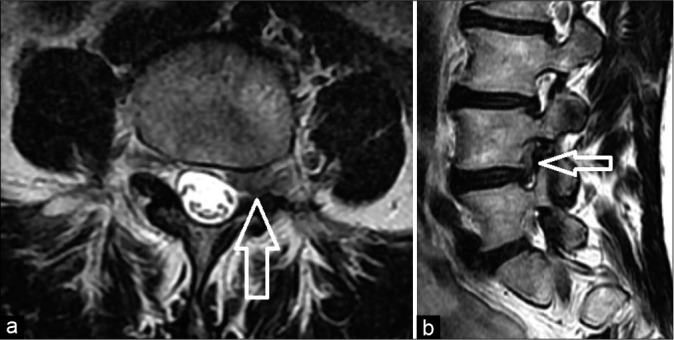
(a) The axial MRI images show a preforaminal and intraforaminal disc herniation (white arrow). (b) The sagittal T2 MRI showed cranial extension of the disc herniation (white arrow).
Results of the contralateral interlaminar approach
As noted, contralateral IELDHs at L5-S1 typically require no facet resection, or <30% of facet joint removal if significant spondylosis is present. This procedure affords adequate decompression of the foraminal/far lateral nerve root, thus enabling safer removal of the extrinsically compressing disc herniation without damaging the nerve root itself [Table 1]. [2,8] Therefore, in summary, this approach at the L5-S1 level to IELDH provides adequate exposure of the L5 intraforaminal/extraforaminal nerve root for the careful removal of these disc herniations without risking damage to the nerve root, or significantly compromising the ipsilateral facet joint and, thus, stability, compared to the ipsilateral approach [Figures 5 and 6].
Table 1:
Focused literature review for surgical techniques to remove intraforaminal/extraforaminal lumbar disc herniations.

Figure 5:
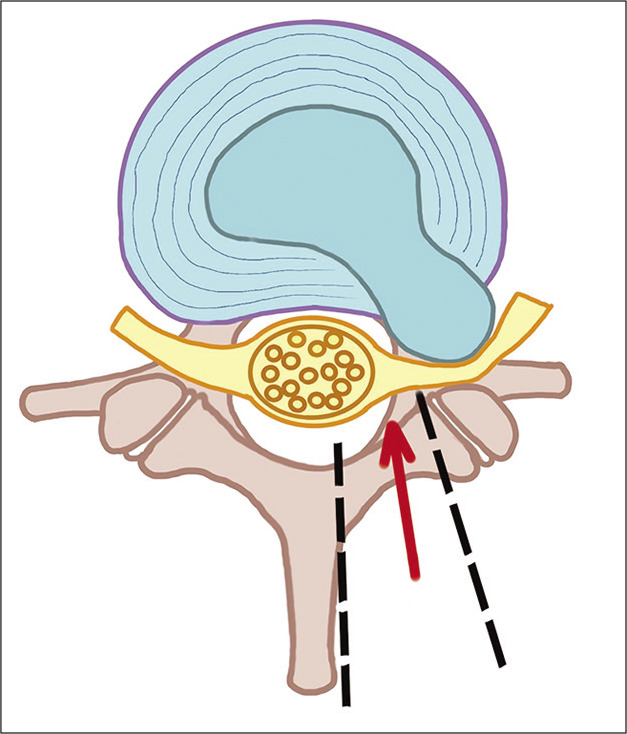
The ipsilateral approach to an intraforaminal herniated lumbar disk does not require exposure below the spinous process. However, it is limited laterally by the facet joints, thus making part of the disc herniation not directly/readily accessible. The red arrow indicated the surgical trajectory. The black lines delimitate the initial surgical exposition to approach the hernia. (Figure 5 by Dr-Andrea Ciuffi).
Figure 6:
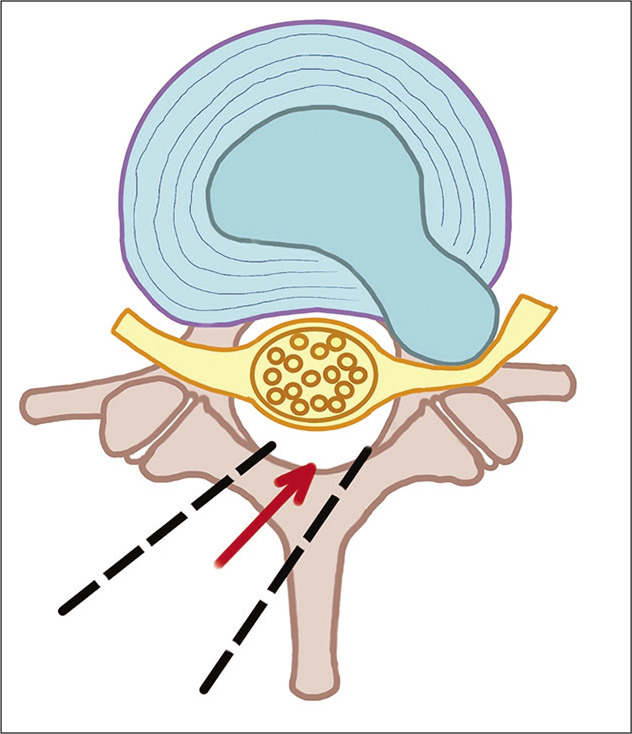
The contralateral approach allows for the development of a surgical corridor below the spinous process that with appropriate angulation between the dural sac and the distal facet joints, allows for direct access to the intraforaminal herniated disk. The red arrow indicated the surgical trajectory. The black lines delimitate the initial surgical exposition to approach the hernia. (Figure 6 by Dr. Andrea Ciuffi).
ALTERNATIVE APPROACHES TO INTRAFORAMINAL/EXTRAFORAMINAL LUMBAR DISC HERNIATIONS
Results of unilateral interlaminar approaches
Three studies advocated utilizing the unilateral interlaminar approach to intraforaminal/extraforaminal lumbar disc herniations [Table 1].[1,5,6] In Abdullah et al., 138 patients underwent unilateral interlaminar approaches to intraforaminal/extraforaminal lumbar disc herniations; 113 experienced complete pain resolution, while 20 observed good relief of pain.[1] With the same approach, 26 patients in Kunogi and Hasue (1991) series demonstrated 14.4 points of postoperative improvement on the JOA.[5] Further, in 1999, at 3 postoperative months, Postacchini et al., 43 patients exhibited an 89% incidence of sustained excellent/good outcomes.[6]
Results of complete facetectomy, unilateral laminotomy, and intertransverse approaches
In 1995, Epstein reported the results of utilizing three different techniques to resect 170 intraforaminal/extraforaminal lumbar disc herniations at multiple levels [Table 1].[3] For those undergoing complete facetectomy, unilateral laminotomy with partial facetectomy, or the intertransverse approaches, 73 demonstrated excellent, 51 good, 21 fair, and 20 poor outcomes. Interestingly, few of those treated with any of these procedures, including full facetectomy, later required fusions.
Results of transmuscular extraforaminal approaches
In Hodges et al. (1999), the 25 patients undergoing transmuscular extraforaminal approaches to intraforaminal/ extraforaminal lumbar disc herniations exhibited 3.5 points of improvement on the visual analog scale, and 16% on the Oswestry disability index scales [Table 1].[4]
CONCLUSION
There are multiple pros and cons for the different alternative approaches to resect IELDH. The ipsilateral interlaminar or the unilateral full facetectomy approaches, respectively, require partial versus total facet joint resection, and increase the risk of postoperative spinal instability.[7,8] The intertransverse route often requires too much medial/lateral facet removal that weakens the pars interarticularis making it more susceptible to fracture, and therefore, instability. Wiltse’s purely extraforaminal approach does not typically adequately access more proximal foraminal discs herniations, and thus has more limited applicability. As discussed here, uniquely for L5-S1 intraforaminal/extraforaminal discs herniations, the contralateral interlaminar approach is optimal. It either warrants no facet resection, or at most in the presence of significant spondylosis <30% medial facet removal. The resultant adequate visualization foraminally/ far laterally exiting nerve root allows for safer exposure and removal of the IELDH.
Footnotes
How to cite this article: Zekaj E, Saleh C, Iess G, Ciuffi A, Jaszczuk P, Galbiati TF, et al. Pros of the contralateral (over-the-top) approach to intra/extraforaminal lumbar disc herniations at the L5-S1 level. Surg Neurol Int 2022;13:243.
Contributor Information
Edvin Zekaj, Email: ezekaj@yahoo.com.
Christian Saleh, Email: chs12us75010@yahoo.com.
Guglielmo Iess, Email: guglielmoiess@gmail.com.
Andrea Ciuffi, Email: andreciuffi@hotmail.it.
Phillip Jaszczuk, Email: philja.ja@gmail.com.
Tommaso Francesco Galbiati, Email: tommaso.galbiati@unimi.it.
Domenico Servello, Email: servello@libero.it.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Abdullah AF, Wolber PG, Warfield JR, Gunadi IK. Surgical management of extreme lateral lumbar disc herniations: Review of 138 cases. Neurosurgery. 1988;22:648–53. doi: 10.1227/00006123-198804000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Berra LV, Foti D, Ampollini A, Faraca G, Zullo N, Musso C. Contralateral approach for far lateral lumbar disc herniations: A modified technique and outcome analysis of nine patients. Spine (Phila Pa 1976) 2010;35:709–13. doi: 10.1097/BRS.0b013e3181bac710. [DOI] [PubMed] [Google Scholar]
- 3.Epstein NE. Evaluation of varied surgical approaches used in the management of 170 far-lateral lumbar disc herniations: Indications and results. J Neurosurg. 1995;83:648–56. doi: 10.3171/jns.1995.83.4.0648. [DOI] [PubMed] [Google Scholar]
- 4.Hodges SD, Humphreys SC, Eck JC, Covington LA. The surgical treatment of far lateral L3-L4 and L4-L5 disc herniations. A modified technique and outcomes analysis of 25 patients. Spine (Phila Pa 1976) 1999;24:1243–6. doi: 10.1097/00007632-199906150-00012. [DOI] [PubMed] [Google Scholar]
- 5.Kunogi J, Hasue M. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine (Phila Pa 1976) 1991;16:1312–20. doi: 10.1097/00007632-199111000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Postacchini F, Cinotti G, Gumina S. Microsurgical excision of lateral lumbar disc herniation through an interlaminar approach. J Bone Joint Surg Br. 1998;80:201–7. doi: 10.1302/0301-620x.80b2.8163. [DOI] [PubMed] [Google Scholar]
- 7.Yue JJ, Scott DL, Han X, Yacob A. The surgical treatment of single level multi-focal subarticular and paracentral and/or far-lateral lumbar disc herniations: The single incision full endoscopic approach. Int J Spine Surg. 2014;8:16. doi: 10.14444/1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zekaj E, Menghetti C, Saleh C, Isidori A, Bona AR, Aimar E, et al. Contralateral interlaminar approach for intraforaminal lumbar degenerative disease with special emphasis on L5-S1 level: A technical note. Surg Neurol Int. 2016;7:88. doi: 10.4103/2152-7806.191024. [DOI] [PMC free article] [PubMed] [Google Scholar]