Abstract
Objectives
Contact tracing applications are technological solutions that can quickly trace and notify users of their potential exposure to the Covid-19 virus and help contain the spread of the disease. However, extant research delineating the various factors predicting the adoption of contact tracing apps is scant. The study's primary objective is to develop and validate a research model based on the unified theory of acceptance and use of technology (UTAUT), health belief model (HBM), perceived privacy risk and perceived security risk to understand the adoption of contact tracing application.
Methods
An online survey was carried out among users of the ‘Aarogya Setu’ contact tracing app in India. The partial least squares structural equation modelling (PLS-SEM) tool was employed to analyze data from 307 respondents.
Results
The results showed that performance expectancy, social influence, and facilitating conditions positively influenced users’ intention to adopt the app. In contrast, perceived privacy and security risks were significant barriers to app adoption. Perceived disease threat as a moderator mitigated the adverse impact of perceived privacy risk on users' intention to adopt contact tracing apps.
Conclusions
The current study gives insights on both drivers and barriers to the adoption of contract tracing applications. Various theoretical and practical implications of significance are provided for academicians and practitioners to effectively promote app adoption to tackle the Covid-19 pandemic.
Keywords: Contact tracing application, UTAUT, Health belief model, Privacy risk, Security risk, Perceived disease threat
Introduction
The worldwide outburst of the Coronavirus disease (Covid-19) pandemic has forced extended lockdowns, strained the public health care system and negatively impacted the global economy. At the time of writing this (July 2020), global Coronavirus infections have crossed 14 million, while India has seen more than one million disease cases [1]. Since the inception of the Covid-19 disease, governments around the globe have taken initiatives to implement smartphone-based contact tracing apps to quickly identify infected individuals and contain the spread of the disease. The digital contact tracing system depends mainly on mobile devices and technology to track and trace contact between an infected patient and the user. The ubiquitous nature of smartphones, laced with location tracking via GPS and WiFi, and the built-in Bluetooth interface make them suitable for automated and reliable contact tracing. Some of the contact tracing apps deployed in various countries across the world are: CovidTrace (Australia), Covid Alert (Canada), Corona-Warn-App (Germany), Immuni (Italy), NHS COVID-19 (United Kingdom), GuideSafe, Covid Watch and COVID Alert (United States). The Indian government has also launched its own Covid-19 tracing app named, ‘Aarogya Setu’ for Android and iOS users on 2nd of April 2020. According to a recent report, the adoption rate of the Aarogya Setu app has been low, despite achieving the highest number of downloads globally, crossing 127 million till July 2020 [2].
Recognising the importance and urgency, researchers have started investigating challenges, issues, benefits, and costs related to Covid-19 contact tracing apps use [3,4]. It has been noted that the effectiveness of contact tracing depends on the widespread adoption of these apps among users [5]. Thus, it is highly essential to identify factors that influence users’ intention to adopt digital contact tracing apps. Few studies have tried to analyze users’ perspectives to delineate factors influencing the adoption of contact tracing apps in the European context [6, 7]. But there is a shortage of studies investigating the adoption of contact tracing apps from the perspective of theories related to information systems (IS) like the technology acceptance model (TAM), unified theory of acceptance and use of technology (UTAUT) and others. We opine that UTAUT variables like performance expectancy (PE), effort expectancy (EE), social influence (SI), and facilitating conditions (FC) would be relevant in the context of this research. Hence, the UTAUT framework is applied as the base model to develop and test a theoretical model to elucidate the adoption of contact tracing applications in India.
Researchers have taken note of privacy and security issues as critical inhibitors of largescale adoption of contact tracing apps among users. Kaptchuk et al. [8] have mentioned that the degree of privacy risk may adversely affect the willingness to install Covid-19 contact tracing apps. Likewise, Baumgärtner et al. [9] have discussed how the use of contact tracing apps may raise security risks for individuals and all the stakeholders involved and make it vulnerable to cyber-attacks. Taking cognizance of the same, we have extended the UTAUT framework by conjoining perceived privacy risk (PPR) and perceived security risk (PSR) in our model. As UTAUT mainly entails a set of factors driving adoption of technology, additions of these perceived risk barriers augment the predictive power and validity of our model.
Kokolakis [10] has mentioned about the privacy paradox when an individual is in a dilemma of choosing between data privacy and freedom and health. The ongoing threat of Covid-19 presents an apt scenario where we may value our privacy, but we are ready to trade it for something else. The adoption of contact tracing apps may reduce the risk of infection and bring higher safety for individuals and society. Hence, we propose that under a scenario of high disease threat, users may ignore the privacy and security breaches related to contact tracing applications vis-à-vis their prospective benefits. So, the perceived disease threat (PDT) construct from the health belief model has been incorporated as a moderator in this study.
Based on the key issues identified, the author seeks to address the following research questions (RQs) in this study. They are RQ1. What are the key predictors of adoption intention of Covid-19 contact tracing app? RQ2. Does user perception about privacy and security risk act as significant inhibitors of adoption of contact tracing app? And RQ3. Does perceived disease threat act as a moderator to attenuate the adverse effects of perceived privacy and security risks on users’ intention to adopt a contact tracing app?
The current study makes multiple contributions toward enhancing knowledge related to the adoption of contact tracing apps in particular. Firstly, it applies and validates the UTAUT model in predicting adoption of contact tracing app in India. Secondly, it extends the UTAUT model by integrating privacy risk and security risk constructs and furnishes empirical evidence of their deleterious effects on adoption of contact tracing app. Thirdly, it is one of the earliest attempts to combine the health belief model (HBM) with the technology use approach of UTAUT and perceived risks in a scholarly work to understand the adoption of contact tracing applications. Fourthly, it contributes significantly towards a finer cognizance of the manifestation and impact of perceived disease threat (PDT) as a moderator on adoption of contact tracing apps, thereby yielding higher explanatory power to the model. Lastly, it provides vital strategic inputs for app developers, government agencies, and administrators to further enhance the adoption of contact tracing applications.
The following sections of the paper are structured in the following manner. The next section presents a comprehensive assessment of the extant literature and the theoretical background. It is followed by the conceptual model and development of hypotheses in section 3. Next, the research design is presented in section 4, followed by the analytical results in section 5. Section 6 discusses the primary findings, theoretical and managerial implications, limitations and future research directions. To end, the last section presents the concluding remarks.
Literature review and theoretical background
A synopsis of studies on adoption of contact tracing apps
Academic research on the adoption of contact tracing applications has gained traction on account of the current outbreak of Covid-19 disease around the globe. In a study in America, it was observed that accuracy, privacy, and individual benefits are key drivers of individuals willingness to adopt contact tracing apps [8]. Applying a choice-based conjoint analysis approach, Wiertz et al. [11] performed a study in the United Kingdom. Their findings indicated that different app configurations could influence the adoption rates in a distinct manner. Blom et al. [7] investigated barriers to large scale adoption of contact tracing app in Germany and found that lack of willingness and access were major hurdles to participants app adoption. Based on the findings of a simulated research among French citizens, Lopez et al. [6] suggested that adopting a digital contact tracing app can significantly reduce the incidence of Covid-19. Saw et al. [12] conducted a survey in Singapore to investigate factors predicting adoption of contact tracing mobile applications. They noted that people using hand sanitizers and avoiding public transport were more likely to use the app, whereas demographics were weak predictors of app usage. In an experimental study by Trang et al. [13], societal-benefit appeal, privacy and convenience were identified as key determinants of installation intention of contact tracing app. In another study, Kaspar [14] employed the protection motivation theory to examine the effects of various health-related and technology-related variables on adoption of contact tracing app in Germany. Despite few notable works mentioned, there is enormous potential to indulge in further research on this topic, keeping in mind its importance and the severity of the current situation. Moreover, research following an information system (IS) oriented theoretic approach to uncover drivers of adoption of contact tracing apps are barely sufficient.
The unified theory of acceptance and use of technology (UTAUT) model
Venkatesh et al. [15] came up with the unified theory of acceptance and use of technology (UTAUT) by integrating various IT adoption models to predict an individual's behavioral intention and use behavior of technology. Performance expectancy, effort expectancy, social influence and facilitating conditions were proposed as the exogenous variable in the model. It is one of the most popular theoretical approaches to explain the adoption and use of various technologies. Performance expectancy, effort expectancy and social influence were identified as key UTAUT variables influencing adoption of mobile health services among the elderly [16]. Similarly, Petersen et al. [17] employed the UTAUT model to analyze the acceptance of mobile health apps among people with diabetes in South Africa. Further, UTAUT has been found to be an excellent predictive model to explain adoption of mobile health among generation Y in Bangladesh [18]. UTAUT framework has also been applied and validated to delineate factors aiding in acceptance of mobile-based smoking cessation service application [19]. The various studies mentioned above have endorsed the efficacy and superiority of UTAUT model over other models.
Venkatesh et al. [20] have advocated extending or modifying a single model while applying to a specific IT context. Thus, it is appropriate to extend or refine a model, congruent with changing technological applications. Zhou [21] extended the UTAUT model with privacy risk construct to investigate the use of location-based services (LBS) among Chinese mobile users. Similarly, Chopdar et al. [22] have confirmed the unfavorable impact of security risk on mobile app shoppers in India. In a recent study, Kukuk [23] modified the UTAUT framework to investigate users’ adoption of contact tracing app in Germany and the Netherlands. Similarly, Tomczyk et al. [24] have used the theory of planned behavior and UTAUT to predict users’ adoption of contact tracing applications. As governments worldwide are trying to uncover and contain the spread of new cases of Covid-19, contact tracing apps present serious privacy and cybersecurity concerns among users [25]. Hence, it is believed that individuals’ risk perceptions may play a significant role in the adoption of mobile-based digital contact tracing apps.
Perceived risks
The concept of perceived risk was equated with uncertainty and consequences of consumers’ actions by Bauer [26]. It was later conceptualized as the amount that would be lost if consequences are not favorable, and the subjective feeling that the consequences will be unfavourable [27]. Numerous studies have examined perceived risk as a multidimensional construct that includes various facets of users’ risk perceptions [28, 29]. Privacy risk and security risk have been proposed as a type of information-related risks in web shopping scenario [30]. Both privacy and security risks have been found to negatively influence users’ acceptance of mobile-based services like location-based mobile commerce, mobile shopping, and health informatics [31, 22, 32]. Despite its immense potential to add value to businesses and society, location-based mobile services are beset with risks related to sharing personal and location information [33]. Rowe [34] noted that adopting contact tracing apps presents severe privacy and security challenges for both users and service providers. Kaspar [14] have also noted that perceived data misuse is a key barrier to adoption of contact tracing app. Notwithstanding the growing concern about privacy and security regarding the adoption of contact tracing apps to curb Covid-19 worldwide, there is limited empirical evidence to validate their negative effects on citizens’ intention to use the app. Thus, it will be interesting to find out whether privacy and security risks act as significant barriers towards adoption of contact tracing applications.
Health belief model
Besides technological factors, health-related factors also play a crucial role in influencing users’ decisions to adopt digital technologies [35]. The health belief model advocates that “an individual's health-related activities depend on his/her consideration of perceived threat of health problems, and the benefits of taking an action in reducing it” [36]. Perceived threat is a function of perceived susceptibility and severity, whereas perceived benefits and barriers determine net benefits. Various researchers in the past have integrated technology acceptance theories with health belief model to investigate users’ attitude and intention towards health-related digital technologies. The extant literature is replete with research which has combined the health belief model (HBM) with technology acceptance model (TAM) and unified theory of acceptance and use of technology (UTAUT) to investigate adoption of health technologies like personal health information systems, health-related internet, and mobile fitness app [37,38,39].
In a recent empirical research in Belgium, perceived benefit of the contact tracing app was noted to be the strongest predictor of its adoption, followed by self-efficacy and perceived barriers [40]. Similarly, in another study in the Netherlands, Jonker et al. [41] observed that the perception of severity of health conditions correlated strongly with an increased preference for contact tracing apps among users. Past research has also indicated that self-efficacy, perceived threats, benefits and barriers are critical determinants of individuals’ engagement in health behaviors [42]. Based on the health belief model, Guillon and Kergall [43] have explored the attitudes of French citizens towards quarantine and contact tracing app use during Covid-19. In the context of this study, the authors believe that the probability of adoption of a contact tracing app may be influenced by an individual's perceived consequences of Covid-19 and perceived benefits they can derive from the app use. Hence, the health belief model has been integrated with the UTAUT framework to furnish a more comprehensive understanding of the phenomenon under study.
Research model and hypotheses development
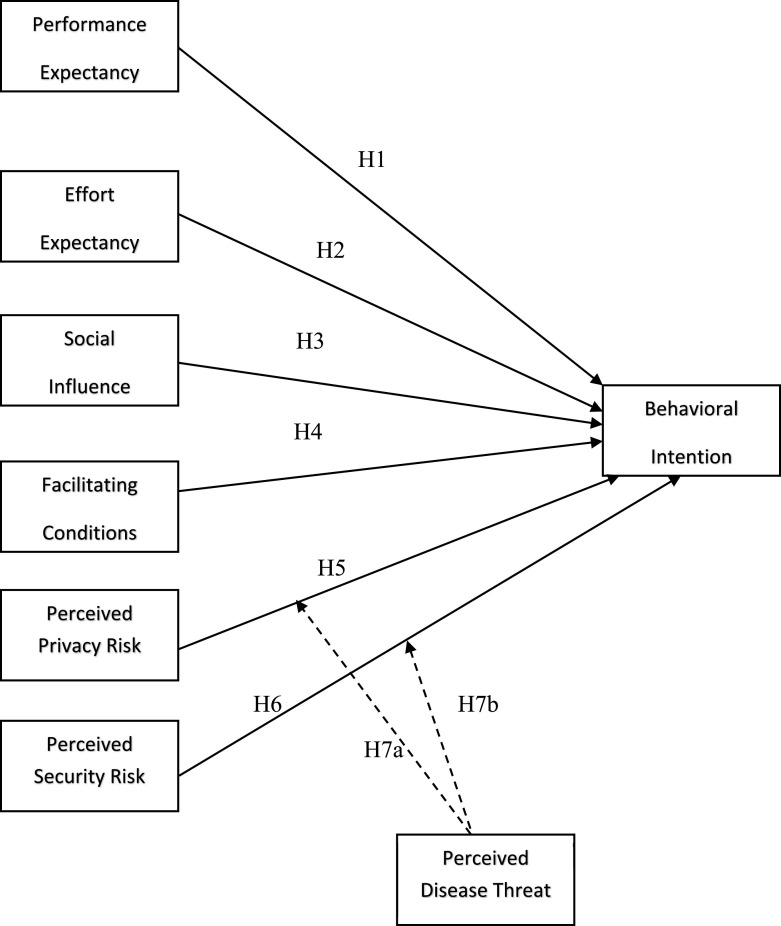
The proposed theoretical framework for this research is depicted in Fig. 1 below. Performance expectancy, effort expectancy, social influence and facilitating conditions are key UTAUT antecedent variables. We have extended the UTAUT model to assess the impact of perceived risks, namely perceived privacy risk and perceived security risk, on the adoption of contact tracing app among Indian users. All the UTAUT constructs are posited to influence users’ intention to adopt contact tracing app positively, whereas privacy risk and security risk constructs are hypothesized to negatively affect the outcome variable in our model. The moderating effect of perceived disease threat (PDT) is further examined in the model. Age, gender and marital status are the control variables in this study.
Fig. 1.
Research model Notes: → Direct effect → Moderating effect.
Performance expectancy (PE)
Performance expectancy is defined as “the degree to which user perceives that adopting technology will help them in performing a particular task more effectively” [15,44]. In the context of health-related technology, PE has been identified as one of the strongest drivers of user's adoption intention [45,39]. Performance expectancy was found to be a salient construct that influenced individuals’ behavioral intention to use health information systems in Ghana [46]. Similarly, PE substantially influenced the adoption of wearable healthcare technology among Chinese citizens [47]. In the current study, PE has been operationalized as the extent to which users believe that contact tracing apps can provide useful, real-time information and help them effectively deal with Covid-19 disease. It is argued that when users have a favorable perception of the usefulness of contact tracing app, they will exhibit a greater intention to adopt it. Hence, it is posited that:
H1. Performance expectancy (PE) positively affects the behavioral intention (BI) to use contact tracing app
Effort expectancy (EE)
Effort expectancy is defined as “the degree of easiness associated with the use of a technology” [15]. EE has been noted to be a favorable factor influencing behavioral intention of users to adopt a specific technology in numerous past studies. EE was noted to be a crucial predictor of acceptance of smartphone fitness app with Indian users [48]. In another study, Quaosar et al. [49] ratified EE as a critical factor that influences users to adopt mobile health services. A convenient design of the contact tracing app, which reduces time and effort and makes it easy to use, was observed to increase the intention to install the app among German citizens [13]. Simple and easy to use interface, convenient installation and updation process with the app may be a significant determinant of adoption among its prospective users. Based on the above arguments, the next hypothesis is postulated:
H2. Effort expectancy (EE) positively affects the behavioral intention (BI) to use contact tracing app.
Social influence (SI)
Social influence is “the extent to which a user perceives that other important members of the society (e.g., family and friends) believe they should use a certain technology” [15]. Prior studies have presented rich affirmation of the positive effect of social influence on user adoption of mobile-based technologies. Social influence was noted to be positively correlated with an individual's intention to use mobile health services in Bangladesh [50]. Likewise, empirical findings from Bettiga et al. [51] confirm that subjective norm plays a significant role in strengthening users' intention to adopt mobile health applications. In a recent study in Singapore, Cho et al. [52] affirmed that social pressure may help gain widespread adoption of contact tracing apps. Walrave et al. [53] have also shown that social influence has a positive impact on users’ intention to adopt contact tracing app. Based on the above findings, it is assumed that individuals embedded in a social context may get influenced by friends, family members, and peer groups to adopt and use a contact tracing application. Thus, we propose:
H3. Social influence (SI) positively affects the behavioral intention (BI) to use contact tracing app.
Facilitating conditions (FC)
Facilitating conditions relate to “an individual's perception regarding the availability of resources, and support facilities to engage in the desired activity or behavior” [15]. Conducting an experimental study, Mahardika et al. [54] observed that low facilitating conditions may act as an impediment to consumers’ new technology adoption, such as mobile applications. On the contrary, a favorable perception regarding facilitating conditions resulted in a higher intention to adopt fitness wearables among Mexican users [55]. Facilitating conditions were found to be a prime enabler of adoption of information and communication technology (ICT) for self-care among diabetics [17]. Walrave et al. [53] have noted that facilitating conditions are one of the crucial factors that promote contact tracing app-uptake intention among Belgians. In a developing country like India, we believe that favorable facilitating conditions like availability of internet-enabled smartphones, supporting information, and assistance will stimulate users' intention to adopt digital contact tracing apps on a large scale. Based on the above logic, it is hypothesized that:
H4. Facilitating conditions (FC) positively affects the behavioral intention (BI) to use contact tracing app.
Perceived privacy risk (PPR)
Individuals are more sensitive toward their personal health-related information in comparison to other demographic information [56]. Further, the potential misuse of personal health information may worsen individuals’ privacy concerns about various health-related technologies [57]. Thus, when a user perceives a greater privacy risk/loss compared to the benefits, they are less likely to adopt a health information technology. It is evident from the findings of Gao et al. [58], which showed that privacy risk is a significant barrier towards adoption of healthcare wearable devices. As noted by Rowe [34], the adoption of Covid-19 contact tracing applications presents a privacy paradox scenario, where users want the immediate benefits from the app but are deeply concerned about their data privacy. Xia and Lee [59] have also echoed similar views by suggesting app developers and government agencies to develop mechanisms to preserve privacy of individuals to promote higher adoption of digital contact tracing apps. In the current study, PPR is conceptualized as the user's perception regarding risk associated with their personal health information, unauthorized use, and sharing to third parties without their consent while using contact tracing app. It is believed that a higher level of PPR will attenuate their intention to adopt contact tracing application. Hence, the next hypothesis is proposed:
H5. Perceived privacy risk (PPR) negatively affects the behavioral intention (BI) to use contact tracing app.
Perceived security risk (PSR)
Security risk deals with users’ perception about modes of payment, storage and transfer of information in an online context [60]. It can also be described as “protecting the integrity, confidentiality, authentication, and non-recognition of relationships” [61]. In a study in the healthcare industry, high degree of security risk resulted in a lesser intention among medical practitioners to use mobile device [62]. Along similar lines, Zhou et al. [63] have noted that lack of security features was a key barrier towards adoption of mobile health apps. We consider perceived security risk with contact tracing applications as users’ perception about the lack of protection of information and chances of hacking and security breaches related to app usage. Mbunge [64] has observed that various Covid-19 contact tracing apps present serious security threats on account of concurrent access to personal health and location data. In a cross-country study on the acceptability of app-based contact tracing, it was observed that countries with higher security concerns are less supportive of adopting the technology [65]. Thus, to substantiate the unfavorable impact of perceived security risk on adoption of contact tracing app, the next hypothesis is offered:
H6. Perceived security risk (PSR) negatively affects the behavioral intention (BI) to use contact tracing app.
Perceived disease threat (PDT) as moderator
Perceived disease threat (PDT) includes “perceived susceptibility and severity, which refers to one's subjective perception of the risk of contracting a health condition and the seriousness of contracting an ailment or of leaving it untreated” [66]. In this research, PDT refers to a person's awareness of Covid-19 condition and apprehension about its potential consequences. The health belief model (HBM) suggests that, “individuals do not engage in taking health-related action unless they feel susceptible to or experience severity of a disease” [67]. PDT has been found to be a significant predictor of health behavioral intention in numerous past researches. PDT was observed to positively influence the adoption of diabetes management apps among patients in China [68]. In another study among hypertension patients, the intensity of perceived health threat favorably impacted their intention to use smartphone health technology [69]. Built on the above findings, it is deduced that PDT strengthens users’ intention to adopt a health-related technology. Based on the review of prior literature on severe acute respiratory syndrome, swine flu, and pandemics, Bish and Michie [70] have also advocated using a theory-driven perspective on health behavior to furnish more clarity on the role of PDT on user behavior.
When the perceived threat of a disease is high, people tend to engage in behavior related to threat reduction strategies [71,72]. Most digital contact tracing apps are designed to identify and inform users about their probable contact with an infected person, thus limiting the spread of the disease [73]. On account of the dual benefits to both individuals and society, adoption of such apps depicts a manifestation of self-beneficial and/or pro-social behavior [74]. Hence, an individual is more likely to adopt a mobile-based contact tracing app to protect oneself from the health threat posed by Covid-19. The current study brings PDT as a moderator into the research model to examine whether the relationship between perceived risks (PPR and PSR) and behavioral intention to adopt contact tracing app varies as a function of PDT. In a study examining computer security behavior, Ng et al. [75] have noted that when the perceived disease threat is high, it will outweigh the cost of inconvenience caused due to other perceived barriers in performing the desired behavior. Likewise, Johnston et al. [76] have endorsed that individuals perceive threats directed at themselves more severely than threats to their personal information. In a recent study, Tran and Nguyen [77] have noted that users may engage in a risk-risk trade-off, where specific type of risk (Privacy) may be accepted to lower other risk (Health) in using Covid-19 contact tracing apps. Grounded on the findings from the past studies, it is argued that under conditions of high disease threat perceived by individuals, the adverse effects of PPR and PSR on adoption of contact tracing app would be attenuated. Accordingly, the following hypotheses are proposed:
H7a. The negative effect of perceived privacy risk (PPR) on behavioral intention (BI) to use contact tracing app will be weaker for individuals scoring high on perceived disease threat (PDT).
H7b. The negative effect of perceived security risk (PSR) on behavioral intention (BI) to use contact tracing app will be weaker for individuals scoring high on perceived disease threat (PDT).
Controlling for demographic variables
Demographic differences among individuals play a critical role with regard to their divergent behavioral intention. Prior studies have observed the significant effect of gender on adoption of mobile health applications [78]. In a meta-analysis of previous literature on mobile health services, the adoption rate of mobile health services was found to be different for various age groups of users [79]. A recent study in Japan noted that a digital contact tracing app is more likely to be adopted by married people [80]. On account of the novelty of the Covid-19 pandemic and the use of contact tracing apps, in particular, we have included gender, age, and marital status as controls in the current study.
Research methodology
A descriptive research approach was preferred for the study based on the insights gleaned from extant literature and proposed hypotheses. The process of questionnaire development, sampling and data collection, and analytical tools employed are presented next.
Instrument development
All the scales employed for measuring the core constructs in this research were adapted from past literature. 28 scale items were used to cover all the core constructs used in our conceptual framework. A seven-point Likert type scale (1= Strongly disagree, 7= Strongly agree) was chosen for measuring all the items. The survey questionnaire was adjusted to attain a better fit with the context of our study, based on the suggestions from two domain experts. In addition, various questions were asked to gather information about respondents’ demographic details. About the control variables, gender, age, and marital status are measured as categorical variables in this study and presented in Table 1 . Appendix A shows details of all the measured variables along with their respective sources.
Table 1.
Respondent demographics (N= 307)
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Gender | Male | 183 | 59.6 |
| Female | 124 | 40.4 | |
| Age | 18-24 | 63 | 20.6 |
| 25-34 | 83 | 27.0 | |
| 35-44 | 112 | 36.5 | |
| 45-54 | 29 | 9.4 | |
| 55-64 | 19 | 6.2 | |
| More than 64 | 1 | 0.3 | |
| Education | Completed school | 11 | 3.6 |
| Diploma | 40 | 13.0 | |
| Graduate | 137 | 44.6 | |
| Post-graduate | 112 | 36.5 | |
| Others | 7 | 2.3 | |
| Marital Status | Single | 47 | 15.3 |
| In a relationship | 59 | 19.2 | |
| Married | 192 | 62.5 | |
| Separated | 2 | 0.7 | |
| Divorced | 3 | 1.0 | |
| Widow/widower | 4 | 1.3 | |
| Profession | Free lancer | 9 | 2.9 |
| Govt. employee | 38 | 12.4 | |
| Home maker | 13 | 4.2 | |
| Private jobs | 129 | 42.0 | |
| Self employed | 54 | 17.6 | |
| Students | 63 | 20.6 | |
| Retired | 1 | 0.3 |
Sampling and data collection
Data was collected through an online questionnaire survey method. We obtained a database of verified mobile app users from a private market research firm. The target population for our study were users of mobile contact tracing apps in India. A representative sample belonging to members from different age groups and locations across India was chosen to boost the validity of our findings.
First, we furnished a brief description of the objectives of our study and highlighted the anonymity and confidentiality of the data collection process. At the beginning of the survey, the participants were clearly informed that the personal information obtained would be solely used for research purposes. Three thousand five hundred e-mails were sent containing the online survey form in the second week of May 2020. Informed consent was obtained from all the participants before data collection. A screening question was employed at the start of the data collection process to exclude non-users of contact tracing app. We received a total of 355 responses at the end of ten days of data collection. The response rate for our survey was quite good at 10.14 %. Eighteen responses were eliminated who were non-users of the app. Moreover, few cases were removed due to missing data and non-engaged responses. Finally, 307 data points were kept for the next stage of analysis. The demographics of our sample members are presented in Table 1. It can be observed that the data are comparable in terms of the gender distribution of respondents.
Data Analysis
The partial least square structural equation modelling (PLS-SEM) approach recommended by Chin [81] was employed to estimate the path models proposed in our study. This is appropriate to research settings which are in the early stages of development and involve testing a theory for prediction purpose [82]. Further, it needs fewer assumptions about the data distributions. The SmartPLS version 3.2.9 software was availed to assess the path model [83]. Moreover, the PLS approach produces robust result when concurrently analyzing moderating effects with direct effects [84].
Results
Adhering to the two-step approach proposed by Anderson and Gerbing [85], the reliability and validity of measures were assessed to validate the factor structure, followed by structural model analysis.
Measurement model evaluation
First, the internal consistency reliability of all the measures are checked by observing the Cronbach's alpha values. They were found to be in the range 0.80-0.90. Jöreskog's [86] composite reliability (CR) values also indicated higher levels of reliability of all the constructs. Next, the average variance extracted (AVE) criterion is assessed to substantiate the convergent validity of constructs. The AVE values were in the range of 0.67-0.79, thus demonstrating an adequate level of convergent validity. Table 2 shows the item loadings, Cronbachs alpha, CR, and AVE estimates of all the latent constructs. Fornell and Larcker [87] proposed that the shared variance among all the constructs in the model should be lower than their AVEs to confirm discriminant validity. It can be inferred from Table 3 that all the measures of constructs are not highly related. Recent studies have indicated that Fornell and Larcker criterion is not suitable when there are only slight differences in the indicator loadings [88]. Table 4 presents the heterotrait-monotrait (HTMT) ratio, with all the values lower than 0.85, thus signifying discriminant validity.
Table 2.
Item loadings, Cronbach's alpha, CR and AVE
| Construct | Number of items | Item loadings | Cronbach's alpha | Composite reliability (CR) | Average variance extracted (AVE) |
|---|---|---|---|---|---|
| Performance expectancy | 4 | 0.77-0.85 | 0.84 | 0.89 | 0.67 |
| Effort expectancy | 4 | 0.80-0.88 | 0.88 | 0.91 | 0.72 |
| Social influence | 4 | 0.73-0.90 | 0.87 | 0.92 | 0.71 |
| Facilitating conditions | 3 | 0.87-0.89 | 0.87 | 0.92 | 0.79 |
| Perceived privacy risk | 3 | 0.87-0.91 | 0.86 | 0.92 | 0.79 |
| Perceived security risk | 3 | 0.83-0.90 | 0.85 | 0.91 | 0.77 |
| Perceived disease threat | 4 | 0.84-0.90 | 0.89 | 0.92 | 0.75 |
| Behavioral intention | 3 | 0.85-0.92 | 0.87 | 0.92 | 0.79 |
Table 3.
Construct correlation matrix and square root of AVE in the diagonal
| BI | EE | FC | PDT | PE | PPR | PSR | SI | |
|---|---|---|---|---|---|---|---|---|
| BI | 0.891 | |||||||
| EE | 0.137 | 0.851 | ||||||
| FC | 0.328 | 0.327 | 0.888 | |||||
| PDT | 0.412 | 0.033 | 0.118 | 0.868 | ||||
| PE | 0.481 | 0.191 | 0.308 | 0.172 | 0.820 | |||
| PPR | -0.426 | 0.054 | -0.077 | 0.027 | -0.132 | 0.887 | ||
| PSR | -0.366 | 0.028 | 0.003 | 0.138 | -0.085 | 0.528 | 0.880 | |
| SI | 0.338 | 0.055 | 0.216 | 0.145 | 0.428 | -0.077 | -0.058 | 0.846 |
Notes: BI = behavioral intention; EE = effort expecatancy; FC = facilitating conditions; PDT = perceived disease threat; PE = performance expectancy; PPR = perceived privacy risk; PSR = perceived security risk; SI = social influence.
Table 4.
HTMT ratio
| BI | EE | FC | PDT | PE | PPR | PSR | SI | |
|---|---|---|---|---|---|---|---|---|
| BI | ||||||||
| EE | 0.138 | |||||||
| FC | 0.376 | 0.392 | ||||||
| PDT | 0.459 | 0.073 | 0.130 | |||||
| PE | 0.555 | 0.223 | 0.360 | 0.194 | ||||
| PPR | 0.478 | 0.071 | 0.087 | 0.068 | 0.148 | |||
| PSR | 0.418 | 0.090 | 0.122 | 0.160 | 0.105 | 0.617 | ||
| SI | 0.372 | 0.103 | 0.247 | 0.174 | 0.479 | 0.090 | 0.074 |
Notes: BI = behavioral intention; EE = effort expectancy; FC = facilitating conditions; PDT = perceived disease threat; PE = performance expectancy; PPR = perceived privacy risk; PSR = perceived security risk; SI = social influence.
The variance inflation factor (VIF) is calculated to explore the likelihood of multicollinearity among the independent variables of the model. The highest VIF value was noted to be 2.83, which is well below the threshold value of 5 [89]. Hence, it rules out any possibility of multicollinearity in this study.
Owing to the self-reported data gathered from respondents through subjective measures, common method bias (CMB) may affect our findings. First, following the guidelines of Podsakoff et al. [90], Harman's single factor analysis was performed to find the variance explained by a single factor. It was observed to be 22.5 percent, thus rejecting the prevalence of CMB issues. Second, it can be noted from Table III that, the largest inter-construct correlation is 0.52 and the correlation values are below the upper limit of 0.90 [91]. Thus, based on the above process suggested by Pavlou et al. [92], it is confirmed that CMB is not a significant issue.
Structural model assessment
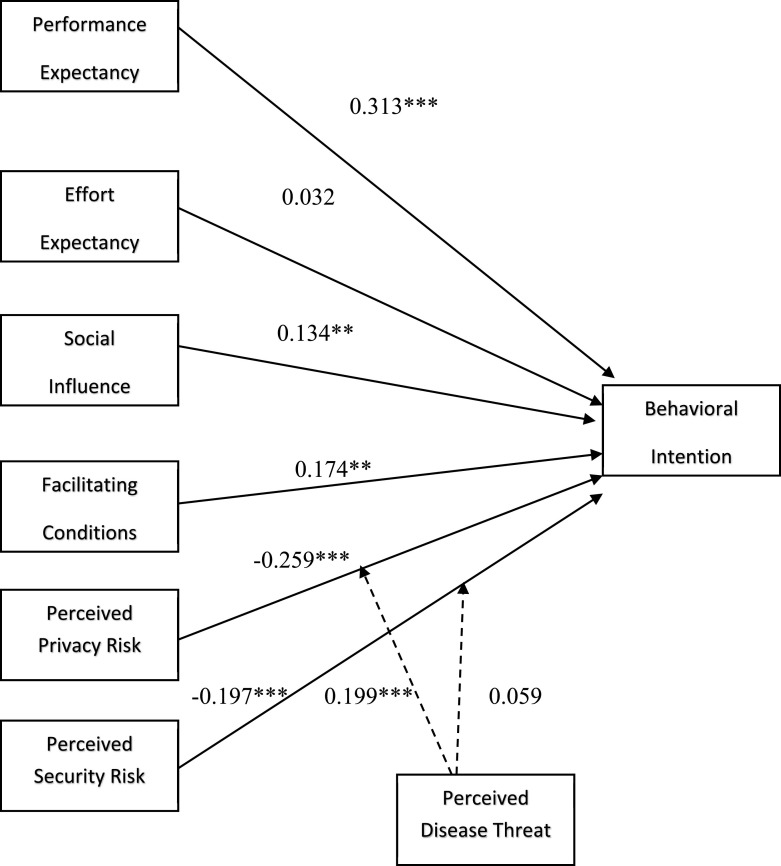
Next, 5000 bootstrap samples were employed to estimate the PLS path model for estimating the significance of path coefficients. Most of the results presented in Table 5 supported our hypothesized model. Apart from effort expectancy (β= 0.03, p= 0.52), all other direct paths were found to be statistically significant. Among all, performance expectancy was observed to be the strongest driver of users’ intention to adopt mobile contact tracing apps (β= 0.31, p= 0.000). Further, perceived privacy risk (β= -0.25, p= 0.000), and perceived security risk (β= -0.19, p= 0.000) were noted to be significant barriers towards the adoption of contact tracing applications among the users.
Table 5.
Hypotheses testing results
| Hypothesized paths | Coefficients | T-values | Results |
|---|---|---|---|
| Main effects | 0.313*** | 5.856 | Supported |
| PE → BI | |||
| EE → BI | 0.032 | 0.643 | Not Supported |
| SI → BI | 0.134** | 2.621 | Supported |
| FC → BI | 0.174** | 3.041 | Supported |
| PPR → BI | -0.259*** | 5.756 | Supported |
| PSR → BI | -0.197*** | 3.902 | Supported |
| Control variables | |||
| Age → BI | -0.138 | 1.628 | |
| Gender → BI | 0.056 | 1.002 | |
| Marital status → BI | -0.073 | 1.002 | |
| Moderation effects | 0.199*** | 4.102 | Supported |
| PPR x PDT → BI | |||
| PSR x PDT → BI | 0.059 | 1.280 | Not Supported |
| Main effects | R2 on BI | ||
| Full model | 0.439 | ||
| 0.620 |
Notes: **p < .01; ***p < .001 (two-tailed), degrees of freedom of t-value= sample size- number of parameters-1.
The moderating effects of perceived disease threat (PDT) were also examined in the model. The two-stage approach was preferred for modelling the interaction term, as it engenders more statistical power [93]. The interaction between perceived privacy risk and PDT on behavioral intention was found to be significant (β= 0.19, p= 0.000). Whereas the impact of PDT on the relationship between perceived security risk and behavioral intention was not significant (β= 0.05, p= 0.201). Overall, hypothesis H1, H3, H4, H5, H6 and H7a were validated, whereas H2 and H7b were not substantiated. The base model explained 43.9% variance in behavioral intention of users. The R2 value for the full model was found to be 62%, which validates the importance of PDT in this research. The impact of control variables, age, gender and marital status on the intention to adopt contact tracing app was found to be insignificant. Overall, the empirical results indicate good model fit for the proposed framework, with standardized root mean square residual (SRMR) value of 0.06, below the threshold of 0.08 [94]. Regarding effect size, an f2 value of 0.02, 0.15, and 0.35 shows small, medium, and large effect sizes, respectively [95]. Among all the predictor variables, the impact of PE was the strongest (f2 =0.13), whereas EE had a negligible effect on adoption (f2= 0.002). Fig. 2 shows the outcomes of the structural model evaluation for the study.
Fig. 2.
Structural model results Notes: → Direct effect → Moderating effect **p < 0.01; ***p < 0.001 (two-tailed)
Discussion
Responding to the current global crisis on Covid-19 pandemic and the insufficiency of research on adoption of contact tracing applications, we utilized the UTAUT and HBM framework along with perceived risks constructs to develop and validate a model for an in-depth cognizance of factors influencing adoption of contact tracing app in India.
Primary findings
Out of all, PE had the strongest impact on users’ behavioral intention to adopt contact tracing app, which is similar to the findings of Kukuk [23]. When users perceive that the contact tracing app benefits them by providing relevant information on Covid-19 and notifying them of probable contacts with infected individuals quickly, their intention to adopt it becomes higher. Contrary to our proposed hypothesis, EE did not significantly affect the adoption of contact tracing app among the respondents. It may happen because smartphone users are accustomed to using so many app-based technologies for messaging, social media, shopping, news etc. Hence, they perceive that they can use digital contact tracing apps without much effort. Similar findings were observed in mobile health applications, where EE was a key predictor of app adoption only for older men, not for younger users [96]. Next, SI was noted to be a significant predictor of app adoption, which suggests that users get influenced by their friends, family members, and peers and look for their approval in adopting contact tracing applications. The effect of SI on adoption intention was not as strong as PE, which is similar to the findings of Walrave et al. [53]. Facilitating conditions, as expected, was observed to have a strong positive effect on behavioral intention of app users. It is analogous to the findings of Zhang et al. [68] study among users of Diabetes management apps. Availability of the technology, necessary infrastructure related to smartphones and the internet, and other information positively influences the adoption of contact tracing apps. Tomczyk et al. [24] have examined the role of additional constructs like hedonic motivation, price value, and habit from the UTAUT 2 framework on adoption and use of contact tracing application. Hedonic motivation was found to be a strong predictor of both intention and frequency of use of contact tracing apps, whereas price value, and habit were significantly associate with intention, and use frequency respectively.
Next, it was noted that PPR and PSR were potent inhibitors of adoption of contact tracing apps among Indian users. It manifests the significant risk perceptions of users with regard to the privacy and security of their personal, health and location-related information shared on platform like a contact tracing application. It is comparable to findings from previous researches on use of mobile apps [97, 22]. In their recent empirical investigation among Irish citizens, O'Callaghan et al. [98] have also discerned the detrimental effect of privacy risk and security risk on the large-scale adoption of contact tracing apps. Even though users are aware of the utilities derived from the contact tracing apps, they hesitate to adopt them due to fears of privacy and security of their information. Further, the insignificant impact of control variables: age, gender and marital status in the model lessens their potential role in confounding the study findings. Although statistically insignificant, age was found to negatively affect the adoption intention for contact tracing app. One plausible justification may be that elderly users find these apps less beneficial or have low confidence in using them effectively [40]. Notwithstanding the insignificant effects of demographic variables like age, gender, and marital status on adoption of contact tracing app in the current study, other variable like past experience may influence users’ behavioral intention. Prior experience with related technology was found to influence users’ intention to adopt mobile health apps [99]. Moreover, Yun [100] has noted that societies with prior experience with pandemics like MERS/SARS1 will be more willing to adopt contact tracing apps. Therefore, prior user experience in influencing the adoption of contact tracing apps cannot be refuted. Hence, it is advisable to examine the role of users' prior experience with similar technology on the adoption of contact tracing applications in future research for a more nuanced understanding of the phenomenon.
Another noteworthy finding of this study deals with the moderating effect of PDT on the relationship between PPR and behavioral intention to adopt contact tracing app. It was noted that perceived disease threat dampens the negative impact of perceived privacy risk on adoption of contact tracing app. We can see that despite a high PPR level, users exhibit a greater level of intention to adopt contact tracing apps when perceived disease threat is high. It indicates that when users perceive they have an increased risk of getting Covid-19 which may make them seriously ill, they tend to disregard the privacy concern related to the app. This is a novel finding of our study, which may help strategists in mitigating users’ risk concerns about contact tracing app adoption. Previously, Bish and Michie [70] had observed that greater levels of perceived susceptibility to and perceived severity of the diseases are important predictors of protective behavior in a pandemic.
In addition, our findings depict the interaction result of PSR and PDT on adoption intention of users. Notwithstanding the insignificant moderating effect, it is evident that users show a greater intention to adopt contact tracing app when perceived disease threat is high compared to low level of threats, despite of high security risk perception. The above empirical findings on moderation aid in developing theory, as such results are not easy to attain frequently [101]. The mixed findings on moderation warrants further studies to uncover other alternate variables and measures. While few scholars have suggested technological solution like encryption-based protocol and centralized app architecture to preserve users’ privacy and security [102,103], others have argued that centralized data storage may promote increased surveillance and infringement on the privacy of individuals [34]. Our study findings unveil a subtle way to minimize users risk perceptions about contact tracing apps by highlighting the moderating role of PDT.
Theoretical and practical implications
This empirical work makes significant contributions to the academic literature on adoption of digital contact tracing app for Covid-19. It is one of the earliest attempts to model and explain adoption of contact tracing app by employing the UTAUT framework. The significant effects of most of the UTAUT variables and moderate level of variance explained indicate potency and relevance of the framework in the research context. We further contribute to the knowledge base by extending the UTAUT framework with privacy risk and security risk as two critical barriers of adoption of contact tracing applications. The current study is a pioneering effort in theorizing and examining the moderating influence of perceived disease threat on the adoption process revealed by users of contact tracing apps. By merging both UTAUT and health belief model, our study not only examines technological drivers of adoption, but also probes the role of health-related beliefs of users in adoption of contact tracing app, thereby contributing to a holistic understanding of the phenomenon.
Along with the theoretical contributions, various practical implications of significance are outlined. PE, being the foremost predictor of adoption of contact tracing applications, app developers should focus on providing better functionalities to augment the usefulness of mobile-based contact tracing systems. Even though EE had a negligible effect on the adoption of digital contact tracing app, developing a simplified version of the app with an easy-to-use interface may hasten adoption among the elderly population. As social influence is a key factor driving adoption in India, the government at the central and state level should strive to leverage the power of social systems to promote ‘Aarogya Setu’ app among the larger population. As a matter of fact, the concerned ministries have requested various social media platforms in India to promote the installation of ‘Aarogya Setu’ app among their vast user base. Using celebrities from sports and entertainment fields at the national and regional level and other social media influencers, could further amplify penetration of the app among the general public. The government should further facilitate the use of contact tracing app by developing low-bandwidth version for rural areas with less connectivity. Making provisions to install the app in old feature phones could enable millions of rural users to adopt it, thereby increasing the effectiveness of contact tracing in containing community spread of Covid-19. As most users perceive a high degree of privacy and security risk in using the contact tracing app, app developers should provide proper data encryption and knowledge sharing mechanisms to minimize potential threats. Additionally, government should communicate and make all users aware of the privacy and security policies related to the ‘Aarogya Setu’ app. Measures should be taken to rectify errors and improvise the app environment through an evolving process to deliver a safer and more effective tracking mechanism. The moderating effect of PDT reveals alternate ways to reduce risk perception of users to further expedite adoption of contact tracing application. Public health agencies across the country should communicate with people with correct and timely information about the risk and severity of Covid-19. Priorities should be given to vulnerable segment of the population and geographical areas with greater chances of infection to make them realise the threats of Covid-19 and its negative consequences. Effective communication guidelines from the government will help citizens in better understanding of the disease and garnering support for health interventions like use of contact tracing apps to reduce the impact of Covid-19.
Limitations and future research
Despite multifarious contributions to both theory and practice, the current study is not without several limitations. First, our sample respondents are limited to Indian users which limits the generalizability of the findings. We recommend replication of this research model with samples from different nationalities. Cross-cultural studies may help uncover the possible role of culture in influencing the adoption of contact tracing applications across nations. Second, behavioral intention was the key dependent variable in this study, as it is difficult to measure the actual usage behavior in a cross-sectional design [104]. Hence, future studies can opt for longitudinal design to capture actual usage data to explore the post-adoption behavior of users of contact tracing applications. Third, our conceptual framework has borrowed constructs from UTAUT and HBM along with privacy and security risk. Future works can utilize other theoretical frameworks and constructs like social cognitive theory, protection motivation theory, technology anxiety, and trust to capture a higher share of variance in the dependent construct and offer alternative explanations of the phenomenon. Fourth, our study reported mixed findings on the moderating role of perceived disease threat. Therefore, future researches may opt for larger sample size and alternate variables to test moderation. Exploring moderating impacts of prior experience, occupation, family size, location, and situational variables in the model would be interesting to observe in future studies.
Conclusions
While digital contact tracing applications for Covid-19 provide a faster way to trace a user's likelihood of contact with infected people and guide them for further actions, its effectiveness is largely dependent on a significant portion of the population installing the app [73]. This research is a pioneering effort to identify various factors that influence the adoption of digital contact tracing applications in India by integrating UTAUT, HBM and perceived risks (Privacy and security) into a theoretical model. The findings vindicate the positive effects of UTAUT variables: performance expectancy, social influence, and facilitating conditions, alongside the adverse impact of user's privacy and security risk on behavioral intention to adopt contact tracing apps. Apart from effort expectancy, all other direct effects posited in the conceptual model were significant. Further, the moderating effect of perceived disease threat aids in extending the theoretical confines and manifests alternate ways to lessen the adverse effects of privacy risk on adoption of contact tracing apps. The research findings contribute to the body of knowledge related to developing and implementing digital contact tracing apps to maximize adoption in a developing country context.
Public interest summary
Countries worldwide are looking at digital contract tracing applications as a major tool to contain the spread of the Covid-19 disease. This study analyzes the various factors that may motivate or dissuade individuals to use contract tracing applications through their mobile devices. We found that the app's effectiveness, social influence, and other facilitating conditions can encourage more people to use them. But people are concerned about the safety and security of their private information, which makes it challenging to popularize this technology among the masses. Governments should make citizens aware of the Covid-19 disease and its threat by disseminating accurate and timely information. Moreover, appropriate measures should be taken to reduce cybersecurity risks for effectively dealing with this pandemic by advocating the use of contract tracing applications.
Patient Consent
Not required.
Ethical approval
Not required, informed consent was obtained from all respondents before the survey.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None declared.
Appendix A. Construct measures with sources
| Construct | Items | Sources |
|---|---|---|
| Performance expectancy (PE) | I feel contact tracing app is useful in collecting Covid-19 related information. | Wang et al. [104] |
| Using contact tracing app enables me to obtain Covid-19 information quickly. | ||
| Using contact tracing app provides me with Covid-19 information that I need. | ||
| If I use contact tracing app, I will increase my chances of dealing with Covid-19. | ||
| Effort expectancy (EE) | Learning how to use mobile contact tracing app is easy for me. | Venkatesh et al. [44] |
| My interaction with mobile contact tracing app is clear and understandable. | ||
| I find this mobile contact tracing app easy to use. | ||
| It is easy for me to become skilful at using mobile contact tracing app. | ||
| Social influence (SI) | People who are important to me think that I should use mobile contact tracing app. | Venkatesh et al. [44] and San martin and Herrero [105] |
| People who influence my behavior think that I should use mobile contact tracing app. | ||
| People whose opinions that I value, prefer that I use mobile contact tracing app. | ||
| People around me consider, it is appropriate to use mobile contact tracing app. | ||
| Facilitating conditions (FC) | I have the resources necessary to use mobile contact tracing app. | Venkatesh et al. [15] and Venkatesh et al. [44] |
| I have the knowledge necessary to use mobile contact tracing app. | ||
| Mobile contact tracing app is compatible with other technologies I use. | ||
| Perceived privacy risk (PPR) | I am concerned that mobile contact tracing app will collect too much personal information from me. | Kyriakidis et al. [106] and Zhang, Tao, Qu, Zhang, Lin, and Zhang [107] |
| I am concerned that mobile contact tracing app will use my personal information for other purposes without my authorization. | ||
| I am concerned that mobile contact tracing app will share my personal information with other entities without my authorization. | ||
| Perceived security risk (PSR) | Using a mobile contact tracing app could allow other people or companies to use my personal information without my knowledge. | Klobas et al. [108] |
| The security systems built into mobile contact tracing app are not strong enough to protect my information. | ||
| Internet hackers (Criminals) might take control of my information if I use mobile contact tracing app. | ||
| Perceived disease threat (PDT) | I find that I can contract Covid-19 easier than others. | Rosenstock [109, 110] |
| I find that I can suffer from Covid-19 disease in the future. | ||
| I find that my health is deteriorating. | ||
| I find that I can suffer from Covid-19 disease in the future and become severely ill. | ||
| Behavioral intention (BI) | Assuming I had access to mobile contact tracing app, I intend to use it. | Venkatesh and Bala [111] and Venkatesh et al. [44] |
| Given that I had access to mobile contact tracing app, I predict that I would use it. | ||
| I intend to continue using mobile contact tracing app in the future. |
References
- 1.xxx https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200717-covid-19-sitrep-179.pdf?sfvrsn=2f1599fa_2. [Accessed 28.07. 2020].
- 2.xxx https://www.indiatoday.in/technology/news/story/aarogya-setu-now-world-s-most-downloaded-covid-19-tracking-app-1701273-2020-07-16. [Accessed 16.08. 2020].
- 3.Ahmed N, Michelin RA, Xue W, Ruj S, Malaney R, Kanhere SS, et al. A survey of COVID-19 contact tracing apps. IEEE access. 2020;8:134577–134601. 2020. [Google Scholar]
- 4.Barrat A, Cattuto C, Kivelä M, Lehmann S, Saramäki J. Effect of manual and digital contact tracing on COVID-19 outbreaks: a study on empirical contact data. Journal of the Royal Society Interface. 2020;18(178) doi: 10.1098/rsif.2020.1000. Jul 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kleinman RA, Merkel C. Digital contact tracing for COVID-19. CMAJ. 2020;192(24):E653–E656. doi: 10.1503/cmaj.200922. Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.López JA, García BA, Bentkowski P, Bioglio L, Pinotti F, Boëlle PY, Barrat A, Colizza V, Poletto C. Anatomy of digital contact tracing: Role of age, transmission setting, adoption, and case detection. Science advances. 2021;7(15):eabd8750. doi: 10.1126/sciadv.abd8750. Apr 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blom AG, Wenz A, Cornesse C, Rettig T, Fikel M, Friedel S, Möhring K, Naumann E, Reifenscheid M, Krieger U. Barriers to the large-scale adoption of the COVID-19 contact-tracing app in Germany: Survey study. Journal of Medical Internet Research: JMIR. 2021;23(3):e23362. doi: 10.2196/23362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaptchuk G, Goldstein DG, Hargittai E, Hofman J, Redmiles EM. t. 2020. How good is good enough for COVID19 apps? The influence of benefits, accuracy, and privacy on willingness to adop. arXiv preprint arXiv:2005.04343May 9. [Google Scholar]
- 9.Baumgärtner L, Dmitrienko A, Freisleben B, Gruler A, Höchst J, Kühlberg J, Mezini M, Mitev R, Miettinen M, Muhamedagic A, Nguyen TD. In2020 IEEE 19th International Conference on Trust, Security and Privacy in Computing and Communications (TrustCom) IEEE; 2020. Mind the GAP: Security & privacy risks of contact tracing apps; pp. 458–467. Jun. [Google Scholar]
- 10.Kokolakis S. Privacy attitudes and privacy behaviour: A review of current research on the privacy paradox phenomenon. Computers & security. 2017;64:122–134. Jan 1. [Google Scholar]
- 11.Wiertz C, Banerjee A, Acar OA, Ghosh A. Predicted adoption rates of contact tracing app configurations-insights from a choice-based conjoint study with a representative sample of the UK population. Available at SSRN 3589199. 2020 Apr 28.
- 12.Saw YE, Tan EY, Liu JS, Liu JC. Towards a digital solution: Predicting public take-up of Singapore′ s contact tracing application during the COVID-19 crisis. medRxiv. 2020 Jan 1. (Pre-print version).
- 13.Trang S, Trenz M, Weiger WH, Tarafdar M, Cheung CM. One app to trace them all? Examining app specifications for mass acceptance of contact-tracing apps. European Journal of Information Systems. 2020;29(4):415–428. Jul 3. [Google Scholar]
- 14.Kaspar K. Motivations for social distancing and app use as complementary measures to combat the COVID-19 pandemic: quantitative survey study. Journal of medical Internet research. 2020;22(8):e21613. doi: 10.2196/21613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: Toward a unified view. MIS quarterly. 2003:425–478. Sep 1. [Google Scholar]
- 16.Hoque R, Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. International journal of medical informatics. 2017;101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002. May 1. [DOI] [PubMed] [Google Scholar]
- 17.Petersen F, Baker A, Pather S, Tucker WD. Impact of socio-demographic factors on the acceptance of information communication and technology (ICT) for diabetes self-care. Responsible Design, Implementation and Use of Information and Communication Technology. 2020;12067:73. Apr 6. [Google Scholar]
- 18.Alam MZ, Hoque MR, Hu W, Barua Z. Factors influencing the adoption of mHealth services in a developing country: A patient-centric study. International Journal of Information Management. 2020;50:128–143. Feb 1. [Google Scholar]
- 19.Ghorai K, Ray P. Factors Affecting the Acceptance of Mobile Based Multi-Feature Service For Smoking Cessation Using UTAUT. European Journal of Biomedical Informatics. 2019 [Google Scholar]
- 20.Venkatesh V, Thong JY, Chan FK, Hu PJ, Brown SA. Extending the two-stage information systems continuance model: Incorporating UTAUT predictors and the role of context. Information Systems Journal. 2011;21(6):527–555. Nov. [Google Scholar]
- 21.Zhou T. Examining location-based services usage from the perspectives of unified theory of acceptance and use of technology and privacy risk. Journal of Electronic Commerce Research. 2012;13(2):135. May 1. [Google Scholar]
- 22.Chopdar PK, Korfiatis N, Sivakumar VJ, Lytras MD. Mobile shopping apps adoption and perceived risks: A cross-country perspective utilizing the Unified Theory of Acceptance and Use of Technology. Computers in Human Behavior. 2018;86:109–128. Sep 1. [Google Scholar]
- 23.Kukuk L. University of Twente); 2022. Analyzing adoption of contact tracing apps using UTAUT (Bachelor's thesis. [Google Scholar]
- 24.Tomczyk S, Barth S, Schmidt S, Muehlan H. Utilizing Health Behavior Change and Technology Acceptance Models to Predict the Adoption of COVID-19 Contact Tracing Apps: Cross-sectional Survey Study. Journal of medical Internet research. 2021;23(5):e25447. doi: 10.2196/25447. May 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newyorktimes, 2020. Virus-Tracing Apps Are Rife With Problems. Governments Are Rushing to Fix Them. Available online: https://www.nytimes.com/2020/07/08/technology/virus-tracing-apps-privacy.html. [Accessed 17.09.2020].
- 26.Bauer RA. InProceedings of the 43rd National Conference of the American Marketing Assocation, June 15, 16, 17, Chicago, Illinois, 1960 1960. American Marketing Association; 2022. Consumer behavior as risk taking. [Google Scholar]
- 27.Cunningham MS. The major dimensions of perceived risk. Risk taking and information handling in consumer behavior. 1967.
- 28.Featherman MS, Pavlou PA. Predicting e-services adoption: a perceived risk facets perspective. International journal of human-computer studies. 2003;59(4):451–474. Oct 1. [Google Scholar]
- 29.Forsythe S, Liu C, Shannon D, Gardner LC. Development of a scale to measure the perceived benefits and risks of online shopping. Journal of interactive marketing. 2006;20(2):55–75. Mar. [Google Scholar]
- 30.Bhatnagar A, Misra S, Rao HR. On risk, convenience, and Internet shopping behavior. Communications of the ACM. 2000;43(11):98–105. Nov 1. [Google Scholar]
- 31.Lee JM, Rha JY. Personalization–privacy paradox and consumer conflict with the use of location-based mobile commerce. Computers in Human Behavior. 2016;63:453–462. Oct 1. [Google Scholar]
- 32.Xu Z. An empirical study of patients' privacy concerns for health informatics as a service. Technological Forecasting and Social Change. 2019;143:297–306. Jun 1. [Google Scholar]
- 33.Pee LG. 2022 Attenuating perceived privacy risk of location-based mobile services.
- 34.Rowe F. Contact tracing apps and values dilemmas: A privacy paradox in a neo-liberal world. International Journal of Information Management. 2020;55 doi: 10.1016/j.ijinfomgt.2020.102178. Dec 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo X, Han X, Zhang X, Dang Y, Chen C. Vol. 21. Telemedicine and e-Health; 2015. pp. 661–669. (Investigating m-health acceptance from a protection motivation theory perspective: gender and age differences). Aug 1. [DOI] [PubMed] [Google Scholar]
- 36.Becker MH. The health belief model and personal health behavior. Health education monographs. 1974;2:324–473. [Google Scholar]
- 37.Hsieh PJ, Lai HM. Exploring peoples intentions to use the health passbook in self-management: An extension of the technology acceptance and health behavior theoretical perspectives in health literacy. Technological Forecasting and Social Change. 2020;161 Dec 1. [Google Scholar]
- 38.Ahadzadeh AS, Sharif SP, Ong FS, Khong KW. Integrating health belief model and technology acceptance model: an investigation of health-related internet use. Journal of medical Internet research. 2015;17(2):e3564. doi: 10.2196/jmir.3564. Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wei J, Vinnikova A, Lu L, Xu J. Understanding and predicting the adoption of fitness mobile apps: evidence from China. Health communication. 2021;36(8):950–961. doi: 10.1080/10410236.2020.1724637. Jul 3. [DOI] [PubMed] [Google Scholar]
- 40.Walrave M, Waeterloos C, Ponnet K. Adoption of a contact tracing app for containing COVID-19: a health belief model approach. JMIR public health and surveillance. 2020;6(3):e20572. doi: 10.2196/20572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jonker M, de Bekker-Grob E, Veldwijk J, Goossens L, Bour S, Rutten-Van Mölken M. COVID-19 contact tracing apps: predicted uptake in the Netherlands based on a discrete choice experiment. JMIR mHealth and uHealth. 2020;8(10):e20741. doi: 10.2196/20741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McArthur LH, Riggs A, Uribe F, Spaulding TJ. Health belief model offers opportunities for designing weight management interventions for college students. Journal of nutrition education and behavior. 2018;50(5):485–493. doi: 10.1016/j.jneb.2017.09.010. May 1. [DOI] [PubMed] [Google Scholar]
- 43.Guillon M, Kergall P. Attitudes and opinions on quarantine and support for a contact-tracing application in France during the COVID-19 outbreak. Public health. 2020;188:21–31. doi: 10.1016/j.puhe.2020.08.026. Nov 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Venkatesh V, Thong JY, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS quarterly. 2012:157–178. Mar 1. [Google Scholar]
- 45.Duarte P, Pinho JC. A mixed methods UTAUT2-based approach to assess mobile health adoption. Journal of Business Research. 2019;102:140–150. Sep 1. [Google Scholar]
- 46.Owusu Kwateng K, Appiah C, Atiemo KA. Adoption of health information systems: health professionals perspective. International Journal of Healthcare Management. 2021;14(2):517–533. Apr 3. [Google Scholar]
- 47.Talukder MS, Sorwar G, Bao Y, Ahmed JU, Palash MA. Predicting antecedents of wearable healthcare technology acceptance by elderly: A combined SEM-Neural Network approach. Technological Forecasting and Social Change. 2020;150 Jan 1. [Google Scholar]
- 48.Dhiman N, Arora N, Dogra N, Gupta A. Consumer adoption of smartphone fitness apps: an extended UTAUT2 perspective. Journal of Indian Business Research. 2019 Nov 17. [Google Scholar]
- 49.Quaosar GA, Hoque MR, Bao Y. Vol. 24. Telemedicine and e-Health; 2018. pp. 309–314. (Investigating factors affecting elderly's intention to use m-health services: an empirical study). Apr 1. [DOI] [PubMed] [Google Scholar]
- 50.Alam MZ, Hu W, Barua Z. Using the UTAUT model to determine factors affecting acceptance and use of mobile health (mHealth) services in Bangladesh. Journal of Studies in Social Sciences. 2018;17(2) Dec 1. [Google Scholar]
- 51.Bettiga D, Lamberti L, Lettieri E. Individuals’ adoption of smart technologies for preventive health care: a structural equation modeling approach. Health care management science. 2020 Jun;23(2):203-14. [DOI] [PubMed]
- 52.Cho H, Ippolito D, Yu YW. Contact tracing mobile apps for COVID-19: Privacy considerations and related trade-offs. arXiv preprint arXiv:2003.11511. 2020 Mar 25.
- 53.Walrave M, Waeterloos C, Ponnet K. Ready or not for contact tracing? Investigating the adoption intention of COVID-19 contact-tracing technology using an extended unified theory of acceptance and use of technology model. Cyberpsychology, Behavior, and Social Networking. 2021;24(6):377–383. doi: 10.1089/cyber.2020.0483. Jun 1. [DOI] [PubMed] [Google Scholar]
- 54.Mahardika H, Thomas D, Ewing MT, Japutra A. Experience and facilitating conditions as impediments to consumers’ new technology adoption. The International Review of Retail, Distribution and Consumer Research. 2019;29(1):79–98. Jan 1. [Google Scholar]
- 55.Reyes-Mercado P. Adoption of fitness wearables: Insights from partial least squares and qualitative comparative analysis. Journal of Systems and Information Technology. 2018 Mar 12. [Google Scholar]
- 56.Bansal G, Gefen D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decision support systems. 2010;49(2):138–150. May 1. [Google Scholar]
- 57.Li H, Gupta A, Zhang J, Sarathy R. Examining the decision to use standalone personal health record systems as a trust-enabled fair social contract. Decision Support Systems. 2014;57:376–386. Jan 1. [Google Scholar]
- 58.Gao Y, Li H, Luo Y. An empirical study of wearable technology acceptance in healthcare. Industrial Management & Data Systems. 2015 Oct 19.
- 59.Xia Y, Lee G. How to return to normalcy: fast and comprehensive contact tracing of COVID-19 through proximity sensing using mobile devices. arXiv preprint arXiv:2004.12576. 2020 Apr 27.
- 60.Kolsaker A, Payne C. Engendering trust in e-commerce: a study of gender-based concerns. Marketing intelligence & planning. 2002 Jul 1.
- 61.Flavián C, Guinalíu M. Consumer trust, perceived security and privacy policy: three basic elements of loyalty to a web site. Industrial management & data Systems. 2006 Jun 1.
- 62.Alexandrou A, Chen LC. A security risk perception model for the adoption of mobile devices in the healthcare industry. Security Journal. 2019;32(4):410–434. Dec. [Google Scholar]
- 63.Zhou L, Bao J, Watzlaf V, Parmanto B. Barriers to and facilitators of the use of mobile health apps from a security perspective: mixed-methods study. JMIR mHealth and uHealth. 2019;7(4):e11223. doi: 10.2196/11223. Apr 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mbunge E. Integrating emerging technologies into COVID-19 contact tracing: Opportunities, challenges and pitfalls. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(6):1631–1636. doi: 10.1016/j.dsx.2020.08.029. Nov 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Altmann S, Milsom L, Zillessen H, Blasone R, Gerdon F, Bach R, Kreuter F, Nosenzo D, Toussaert S, Abeler J. Acceptability of app-based contact tracing for COVID-19: Cross-country survey study. JMIR mHealth and uHealth. 2020;8(8):e19857. doi: 10.2196/19857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deng Z. Understanding public users’ adoption of mobile health service. International Journal of Mobile Communications. 2013;11(4):351–373. [Google Scholar]
- 67.Janz NK, Becker MH. The health belief model: A decade later. Health education quarterly. 1984 Mar;11(1):1-47. [DOI] [PubMed]
- 68.Zhang Y, Liu C, Luo S, Xie Y, Liu F, Li X, Zhou Z. Factors influencing patients’ intentions to use diabetes management apps based on an extended unified theory of acceptance and use of technology model: web-based survey. Journal of medical Internet research. 2019;21(8):e15023. doi: 10.2196/15023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dou K, Yu P, Deng N, Liu F, Guan Y, Li Z, Ji Y, Du N, Lu X, Duan H. Patients’ acceptance of smartphone health technology for chronic disease management: a theoretical model and empirical test. JMIR mHealth and uHealth. 2017;5(12):e7886. doi: 10.2196/mhealth.7886. Dec 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British journal of health psychology. 2010;15(4):797–824. doi: 10.1348/135910710X485826. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hogg MA, Mullin BA. Joining groups to reduce uncertainty: Subjective uncertainty reduction and group identification. 1999.
- 72.Van den Bos K. Uncertainty management: the influence of uncertainty salience on reactions to perceived procedural fairness. Journal of personality and social psychology. 2001;80(6):931. Jun. [PubMed] [Google Scholar]
- 73.Ferretti L, Wymant C, Kendall M, Zhao L, Nurtay A, Abeler-Dörner L, Parker M, Bonsall D, Fraser C. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368(6491) doi: 10.1126/science.abb6936. May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.White K, Habib R, Hardisty DJ. How to SHIFT consumer behaviors to be more sustainable: A literature review and guiding framework. Journal of Marketing. 2019;83(3):22–49. May. [Google Scholar]
- 75.Ng BY, Kankanhalli A, Xu YC. Studying users' computer security behavior: A health belief perspective. Decision Support Systems. 2009;46(4):815–825. Mar 1. [Google Scholar]
- 76.Johnston AC, Warkentin M, Siponen M. An Enhanced Fear Appeal Rhetorical Framework. MIS quarterly. 2015;39(1):113–134. Mar 1. [Google Scholar]
- 77.Tran CD, Nguyen TT. Health vs. privacy? The risk-risk tradeoff in using COVID-19 contact-tracing apps. Technology in Society. 2021;67 doi: 10.1016/j.techsoc.2021.101755. Nov 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Garavand A, Samadbeik M, Nadri H, Rahimi B, Asadi H. Effective factors in adoption of mobile health applications between medical sciences students using the UTAUT model. Methods of information in medicine. 2019 Nov;58(04/05):131-9. [DOI] [PubMed]
- 79.Zhao Y, Ni Q, Zhou R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. International Journal of Information Management. 2018;43:342–350. Dec 1. [Google Scholar]
- 80.Ishimaru T, Ibayashi K, Nagata M, Tateishi S, Hino A, Tsuji M, Ando H, Muramatsu K, Fujino Y. Factors associated with acceptance of a digital contact tracing application for COVID-19 in the Japanese working-age population. medRxiv. 2021 Jan 1. [DOI] [PMC free article] [PubMed]
- 81.Chin WW. The partial least squares approach to structural equation modeling. Modern methods for business research. 1998;295(2):295–336. Jan 1. [Google Scholar]
- 82.Hair JF, Risher JJ, Sarstedt M, Ringle CM. When to use and how to report the results of PLS-SEM. European business review. 2019 Jan 14.
- 83.Ringle CM, Wende S, Becker JM. Bönningstedt; Germany: 2015. SmartPLS 3. SmartPLS GmbH. [Google Scholar]
- 84.Yoon C. The effects of national culture values on consumer acceptance of e-commerce: Online shoppers in China. Information & Management. 2009;46(5):294–301. Jun 1. [Google Scholar]
- 85.Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological bulletin. 1988;103(3):411. May. [Google Scholar]
- 86.Jöreskog KG. Simultaneous factor analysis in several populations. Psychometrika. 1971;36(4):409–426. Dec 1. [Google Scholar]
- 87.Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. Journal of marketing research. 1981;18(1):39–50. Feb. [Google Scholar]
- 88.Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the academy of marketing science. 2015;43(1):115–135. Jan. [Google Scholar]
- 89.Hair JF, Ringle CM, Sarstedt M. PLS-SEM: Indeed a silver bullet. Journal of Marketing theory and Practice. 2011;19(2):139–152. Apr 1. [Google Scholar]
- 90.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. Journal of applied psychology. 2003;88(5):879. doi: 10.1037/0021-9010.88.5.879. Oct. [DOI] [PubMed] [Google Scholar]
- 91.Bagozzi RP, Yi Y, Phillips LW. Assessing construct validity in organizational research. Administrative science quarterly. 1991:421–458. Sep 1. [Google Scholar]
- 92.Pavlou PA, Liang H, Xue Y. Understanding and mitigating uncertainty in online exchange relationships: A principal-agent perspective. MIS quarterly. 2007:105–136. Mar 1. [Google Scholar]
- 93.Hair JF, Jr, Hult GT, Ringle CM, Sarstedt M. Sage publications; 2021. A primer on partial least squares structural equation modeling (PLS-SEM) Jun 30. [Google Scholar]
- 94.Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological methods. 1998;3(4):424. Dec. [Google Scholar]
- 95.Cohen J. Academic press; 2013. Statistical power analysis for the behavioral sciences. Sep 3. [Google Scholar]
- 96.Nunes A, Limpo T, Castro SL. Acceptance of mobile health applications: examining key determinants and moderators. Frontiers in psychology. 2019;10:2791. doi: 10.3389/fpsyg.2019.02791. Dec 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Balapour A, Nikkhah HR, Sabherwal R. Mobile application security: Role of perceived privacy as the predictor of security perceptions. International Journal of Information Management. 2020;52 Jun 1. [Google Scholar]
- 98.Balapour A, Reychav I, Sabherwal R, Azuri J. Mobile technology identity and self-efficacy: Implications for the adoption of clinically supported mobile health apps. International Journal of Information Management. 2019;49:58–68. Dec 1. [Google Scholar]
- 99.Yun M. How Taiwan is containing coronavirus–despite diplomatic isolation by China. The Guardian [online]. 2020 Mar;13. [Accessed 18.11.2021].
- 100.Podsakoff PM, MacKenzie SB, Ahearne M, Bommer WH. Searching for a needle in a haystack: Trying to identify the illusive moderators of leadership behaviors. Journal of Management. 1995;21(3):423–470. Jan 1. [Google Scholar]
- 101.Berke A, Bakker M, Vepakomma P, Larson K, Pentland AS. Assessing disease exposure risk with location data: A proposal for cryptographic preservation of privacy. arXiv preprint arXiv:2003.14412. 2020 Mar 31.
- 102.Li T, Faklaris C, King J, Agarwal Y, Dabbish L, Hong JI. Decentralized is not risk-free: Understanding public perceptions of privacy-utility trade-offs in COVID-19 contact-tracing apps. arXiv preprint arXiv:2005.11957. 2020 May 25.
- 103.Wang H, Tao D, Yu N, Qu X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. International journal of medical informatics. 2020;139 doi: 10.1016/j.ijmedinf.2020.104156. Jul 1. [DOI] [PubMed] [Google Scholar]
- 104.San Martín H, Herrero Á. Influence of the user's psychological factors on the online purchase intention in rural tourism: Integrating innovativeness to the UTAUT framework. Tourism Management. 2012;33(2):341–350. Apr 1. [Google Scholar]
- 105.Kyriakidis M, Happee R, de Winter JC. Public opinion on automated driving: Results of an international questionnaire among 5000 respondents. Transportation research part F: traffic psychology and behaviour. 2015;32:127–140. Jul 1. [Google Scholar]
- 106.Zhang T, Tao D, Qu X, Zhang X, Lin R, Zhang W. The roles of initial trust and perceived risk in public's acceptance of automated vehicles. Transportation research part C: emerging technologies. 2019;98:207–220. Jan 1. [Google Scholar]
- 107.Klobas JE, McGill T, Wang X. How perceived security risk affects intention to use smart home devices: A reasoned action explanation. Computers & Security. 2019;87 Nov 1. [Google Scholar]
- 108.Rosenstock IM. Why people use health services Milbank meml Fund. Q. Bull. 1966;4:94. [PubMed] [Google Scholar]
- 109.Rosenstock IM. Historical origins of the health belief model. Health education monographs. 1974;2(4):328–335. doi: 10.1177/109019817800600406. Dec. [DOI] [PubMed] [Google Scholar]
- 110.Venkatesh V, Bala H. Technology acceptance model 3 and a research agenda on interventions. Decision sciences. 2008;39(2):273–315. May. [Google Scholar]