INTRODUCTION
Hospital at Home (HaH) has been demonstrated to be effective in a variety of settings and patient populations.1, 2 However, it is unknown whether HaH is feasible or effective for socioeconomically disadvantaged patients. Our aim is to determine whether HaH services were received by disadvantaged patients, and if so, whether effectiveness differs for patients depending on socioeconomic status (SES) using two indicators of SES.
METHODS
Patient Selection
In a previous Center for Medicare and Medicaid Innovation (CMMI) demonstration of HaH, we recruited patients ages ≥18 years with fee-for-service Medicare or coverage from a private insurer that contracted for HaH services.1 Patients with Medicaid were dually eligible or had Medicaid Managed Care. All participants required inpatient admission for medical diagnoses from one of four New York City hospitals from November 2014 through August 2017. Patients were ineligible if they required intensive care, surgery, or telemetry monitoring. Additionally, program eligibility required a suitable home environment. Participation in HaH consisted of acute hospital-level care at home and a 30-day period of post-acute transitional care. Control patients were identified using identical eligibility criteria, but either chose traditional inpatient care instead of HaH, were admitted to inpatient units on nights and weekends when HaH was unavailable, or were admitted before HaH was implemented at one hospital.
Analysis
Primary outcomes and subgroups were selected prior to conducting the analysis. Primary outcomes were duration of acute hospital-level length of stay (LOS), 30-day all-cause hospital readmissions and 30-day all-cause emergency department (ED) visits not leading to hospitalization. We examined whether primary outcomes differ for subgroups using two indicators of SES: 1) Medicaid enrollment status; 2) binary SES residential indicator (i.e., whether patient lived in public housing3 or a census block group where 20% or more of the households had incomes below the federal poverty level). We compared outcomes of HaH and control patients within subgroups. To limit potential bias from non-random assignment to HaH, we used entropy balancing weighted regression. Models for Medicaid status subgroups were adjusted for age, race and ethnicity, education, ADL impairment, and general health; models for the SES residential indicator were only adjusted for age, race and ethnicity due to cell size limitations. Standard errors were adjusted for clustering of HaH admissions among individual patients.
RESULTS
A total of 477 hospital episodes across 443 unique subjects were included in this analysis (289 [60.6%] HaH and 188 [39.4%] controls). Medicaid status and low SES residential indicator was prevalent at similar rates in the two groups: 41.9% in HaH vs. 39.4% in controls had Medicaid (p=0.59); 55.0% of HaH and 60.8% of controls were associated with the low SES residential indicator (p=0.18). The Medicaid and the low SES residential indicator had substantial but incomplete overlap; 42.7% of those linked to the low SES residential indicator did not have Medicaid status, and 18.7% of those linked to the higher SES residential indicator had Medicaid.
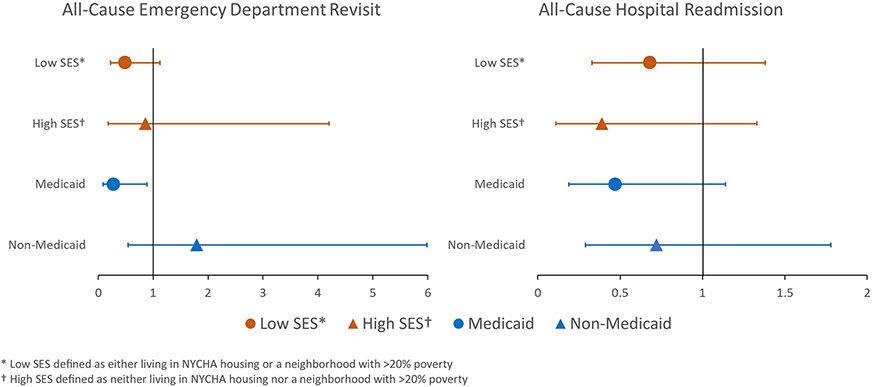
Primary outcomes by subgroups are shown in Table 1. Unadjusted and adjusted analyses demonstrate that the duration of acute care was shorter in HaH compared to hospital inpatient controls regardless of SES. The 30-day ED revisits not leading to hospitalization were significantly reduced in patients with Medicaid (AOR 0.28, 95% CI 0.09, 0.88; p=0.03) favoring HaH. There were no other statistically significant differences in hospital readmission and ED revisit outcomes between HaH and controls. However, the point estimates favored HaH (see Figure 1) except in the case of 30-day ED revisits in the non-Medicaid subgroup.
Table 1.
Raw and adjusted patient outcomes among hospital at home patients and inpatient controls, stratified by socioeconomic status and by Medicaid status.
| Acute Length of Stay | All-Cause Hospital Readmission |
All-Cause Emergency Department Revisit |
|||||
|---|---|---|---|---|---|---|---|
| Raw | Adjustedc | Raw | Adjustedc | Raw | Adjustedc | ||
| Subgroup | n | Mean (SD) | Difference | 30-Day Rate (%) |
Odds Ratio (CI) | 30-Day Rate (%) |
Odds Ratio (CI) |
| Low SESa | |||||||
| Hospital at Home | 159 | 3.17 (2.30)** | 1.97** | 13.21 | 0.68 (0.33, 1.38) | 6.92 | 0.49 (0.22, 1.12) |
| Inpatient Control | 115 | 5.05 (2.94) | 17.39 | 13.91 | |||
| High SESb | |||||||
| Hospital at Home | 130 | 3.26 (1.87)** | 1.92** | 5.38* | 0.39 (0.11, 1.33) | 4.62 | 0.86 (0.18, 4.20) |
| Inpatient Control | 73 | 5.64 (3.21) | 15.07 | 6.85 | |||
| Medicaid | |||||||
| Hospital at Home | 121 | 3.33 (2.46)** | 2.85** | 9.92 | 0.47 (0.19, 1.14) | 4.96* | 0.28 (0.09, 0.89)* |
| Inpatient Control | 74 | 5.81 (3.74) | 20.27 | 16.22 | |||
| Non-Medicaid | |||||||
| Hospital at Home | 168 | 3.13 (1.82)** | 1.59** | 9.52 | 0.72 (0.29, 1.78) | 6.55 | 1.79 (0.54, 5.99) |
| Inpatient Control | 114 | 4.94 (2.46) | 14.04 | 7.89 | |||
Statistically significant at the 0.05 level
Statistically significant at the 0.01 level
Low SES defined as either living in NYCHA housing or a neighborhood with >20% poverty
High SES defined as neither living in NYCHA housing nor a neighborhood with >20% poverty
Adjusted for patient mix based on age and race/ethnicity in analysis of SES, and adjusted for patient mix based on age, sex, education, race/ethnicity, ADL impairment and general health in analysis of Medicaid status
Figure 1.
Distribution of adjusted odds ratios comparing the outcomes of hospital at home patients to controls in four subgroups. Adjusted for patient mix based on age and race/ethnicity in analysis of low and high socioeconomic status (SES). Adjusted for patient mix based on age, sex, education, race/ethnicity, activities of daily living impairment and general health in analysis of Medicaid status.
DISCUSSION
There is a dearth of research on issues related to healthcare equity in the provision of HaH.4 This is important to address now, as the model is expanding due to Medicare’s Acute Hospital Care at Home waiver for hospital reimbursement for the duration of the pandemic.5, 6 Our data suggest that HaH is feasible for economically disadvantaged patients and that these patients may even have greater benefit from HaH. We hypothesize that better outcomes for low SES patients may result from the ability of HaH providers to directly observe and provide care to patients in their homes, where they can address social determinants of health (e.g, food insecurity, medical equipment needs, management of chronic diseases in real-world situations). Study limitations include the use of retrospective data and proxy indicators of SES status, and limited ability to adjust for potential confounders due to cell size constraints. More research on HaH and healthcare equity needs to be performed, including routine measurement of multiple dimensions of SES, to better understand how this expanding model of care supports these populations.
ACKNOWLEGEMENTS
As corresponding author, I affirm that I have listed everyone who contributed significantly to the work. There are no other contributors who are not co-authors.
Sponsor’s Role
The Hospitalization at Home (HaH) clinical project described was supported by grant number 1C1CMS331334 from the US Department of Health and Human Services, Centers for Medicare & Medicaid Services. Research reported in this publication was supported by the National Institute on Aging, Claude D. Pepper Older Americans Independence Center (3P30AG028741), and the John A. Hartford Foundation (2014-0158). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest
Dr. Leff serves as a clinical advisor to Medically Home, Dispatch Health, and the Chartis Group. He serves as a volunteer member of the Humana Multidisciplinary Advisory Board. In the early 2000s Dr. Leff developed Hospital at Home technical assistance tools that were licensed by Johns Hopkins to several entities and, as a result of these license agreements, both the University and its inventors received royalty income; there has been no royalty income for several years. Dr. Leff’s arrangements and relationships have been reviewed and approved by the Johns Hopkins University in accordance with its conflicts of interest policy. Dr. Leff serves as a consultant to the Kenes Group as a member of the planning committee of the World Hospital at Home Congress. Drs. Siu, DeCherrie and Leff are leaders of the Hospital at Home Users Group, which focuses on Hospital at Home technical assistance and is supported by grants from the John A. Hartford Foundation. Dr. DeCherrie is a full-time employee of the Medically Home Group. Dr. Siu, Mr. Zhao, Mr. Bollens-Lund, Ms. Lubetsky, Ms. Schiller, Dr. Saenger, Dr. Ornstein, and Dr. Federman are full-time employees of the Icahn School of Medicine, which in turn has an ownership interest in a joint venture with Contessa Health, a venture that manages acute care services provided to patients in their homes through prospective bundled payment arrangements. No authors have a personal financial interest in the joint venture.
Preliminary results of this research were presented as a poster:
Schiller GS, DeCherrie LV, Federman AD, Lubetsky S, Saenger P, Siu AL. Comparing Post-Acute Health Service Utilization for Medicaid versus non-Medicaid Patients Treated in Hospital-at-Home. Poster presented at: 2021 Hospital at Home Users Group Annual Meeting; October 28; Online.
REFERENCES
- 1.Federman AD, Soones T, DeCherrie LV, Leff B, Siu AL. Association of a Bundled Hospital-at-Home and 30-Day Postacute Transitional Care Program With Clinical Outcomes and Patient Experiences. JAMA Intern Med. Aug 1 2018;178(8):1033–1040. doi: 10.1001/jamainternmed.2018.2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Augustine MR, Siu AL, Boockvar KS, DeCherrie LV, Leff BA, Federman AD. Outcomes of Hospital at Home for Older Adults with and without High Levels of Social Support. Home Healthc Now. Sep-Oct 01 2021;39(5):261–270. doi: 10.1097/nhh.0000000000000980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yim B, Howland RE, Culp GM, Zhilkova A, Barbot O, Tsao TY. Disparities in Preventable Hospitalizations Among Public Housing Developments. Am J Prev Med. Feb 2019;56(2):187–195. doi: 10.1016/j.amepre.2018.08.019 [DOI] [PubMed] [Google Scholar]
- 4.Leff B D L, Montalto M, Levine DM. A Research Agenda for Hospital at Home. J Am Geriatr Soc. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levine DM, DeCherrie LV, Siu AL, Leff B. Early Uptake of the Acute Hospital Care at Home Waiver. Ann Intern Med. Dec 2021;174(12):1772–1774. doi: 10.7326/m21-2516 [DOI] [PubMed] [Google Scholar]
- 6.Clarke DV, N J, Olson DP, Adams D, Wolfe AJ, Fleisher LA. Acute Hospital Care at Home: the CMS Waiver Experience. NEJM Catal Innov Care Deliv. Published online December 7, 2021;doi: 10.1056/CAT.21.0338 [DOI] [Google Scholar]