Abstract
Autism Spectrum Disorders (ASD) are neurodevelopmental disorders whose diagnosis relies on deficient social interaction and communication together with repetitive behavior. To date, no pharmacological treatment has been approved that ameliorates social behavior in patients with ASD. Based on the excitation/inhibition imbalance theory of autism, we hypothesized that bromide ions, long used as an antiepileptic medication, could relieve core symptoms of ASD. We evaluated the effects of chronic sodium bromide (NaBr) administration on autistic-like symptoms in three genetic mouse models of autism: Oprm1−/−, Fmr1−/− and Shank3Δex13-16−/− mice. We showed that chronic NaBr treatment relieved autistic-like behaviors in these three models. In Oprm1−/− mice, these beneficial effects were superior to those of chronic bumetanide administration. At transcriptional level, chronic NaBr in Oprm1 null mice was associated with increased expression of genes coding for chloride ions transporters, GABAA receptor subunits, oxytocin and mGlu4 receptor. Lastly, we uncovered synergistic alleviating effects of chronic NaBr and a positive allosteric modulator (PAM) of mGlu4 receptor on autistic-like behavior in Oprm1−/− mice. We evidenced in heterologous cells that bromide ions behave as PAMs of mGlu4, providing a molecular mechanism for such synergy. Our data reveal the therapeutic potential of bromide ions, alone or in combination with a PAM of mGlu4 receptor, for the treatment of ASDs.
Subject terms: Autism spectrum disorders, Pharmacology
Introduction
Autism Spectrum Disorders (ASD) are neurodevelopmental diseases whose diagnosis relies on the detection of impaired social communication and interaction together with a restricted, repetitive repertoire of behaviors, interests and activities [1]. Alongside core symptoms, ASD are often associated with neurobehavioral comorbidities, such as high anxiety, cognitive and motor deficits or epilepsy [2–5]. Despite the identification of vulnerability genes and environmental risk factors [6–8], the etiology of ASD remains essentially unknown, making difficult the development of pharmacological treatments.
Excitation/inhibition (E/I) imbalance appears as a common mechanistic feature in ASD [9, 10]. The heuristic hypothesis of excessive E/I ratio in ASD was initially formulated by Rubenstein and Merzenich [11] and accounted well for reduced GABAergic signaling [12, 13] and high prevalence of epilepsy (10–30%) [3] in these pathologies. Indeed, epilepsy is one of the most frequent comorbid medical condition in autism [5, 14], suggesting shared risk factors and/or pathophysiological mechanisms [15, 16]. However, the excessive E/I hypothesis in ASD has been challenged by studies in animal models showing instead decreased excitation, which led to a more general concept of altered E/I homeostasis [10, 17].
Compromised E/I balance in ASD may result from several neuropathological mechanisms. On the excitation side, glutamatergic transmission was found altered both in patients and animal models, although in different directions depending on genetic mutations/models [9, 18, 19]. On the inhibition side, decreased levels of GABA [20] and expression of GABAA and GABAB receptors (postmortem analyses, [21, 22]), as well as genetic polymorphisms in GABAA receptor subunits [23, 24], have been detected in patients with autism. Accordingly, decreased GABAergic neurotransmission has been reported in several ASD models [25–29]. Alternatively, it was proposed that GABA neurons remain immature in ASD, maintaining high intracellular concentrations of chloride ion (Cl−) whose efflux through activated GABAA receptor induced neuronal depolarization [30]. Intracellular Cl− concentration is under the control of the main Cl− importer NKCC1 (Na+-K+-2Cl− cotransporter) and its main exporter KCC2. Therefore blocking NKCC1 using the loop diuretic and antiepileptic drug [31, 32] bumetanide appeared a promising therapeutic approach in ASD. Accordingly, bumetanide improved autistic-like phenotype in rodent models of ASD [33] and relieved autistic behavior in small cohorts of patients [34, 35].
Bromide ion (Br−) was the first effective treatment identified for epilepsy [36] and long used as anxiolytic and hypnotic [37]. With the advent of novel antiepileptic and anxiolytic drugs, its use was progressively dropped down, although it remains a valuable tool to treat refractory seizures [38, 39]. At molecular level, Br− shares similar chemical and physical properties with Cl−, allowing it substituting Cl− in multiple cellular mechanisms. These include anion influx through activated GABAA receptor, with higher permeability to Br− compared to Cl− resulting in neuronal hyperpolarization [40], and transport through the NKCC and KCC cotransporters [41, 42]. In view of the E/I imbalance theory, these properties point to Br− as an interesting candidate for ASD treatment.
Here we assessed the effects of chronic sodium bromide administration on core autistic-like symptoms: social deficit and stereotypies, and a frequent comorbid symptom: anxiety, in three genetic mouse models of autism with different etiologies: Oprm1−/−, Fmr1−/− (preclinical model of Fragile X syndrome) and Shank3Δex13-16−/− mice, lacking the gene coding the mu opioid receptor or the FMRP protein for the formers, or the exons 13−16 of the Shank3 gene, coding for the PDZ domain of the SHANK3 protein, for the later. Altered E/I balance and/or modified expression of involved genes have been reported for these three models [28, 43–47]; the Oprm1 knockout model presents the advantage of limited impact on learning performance [44]. We evidenced that Br− treatment alleviates behavioral deficits in these three models and increases expression of various genes within the social brain circuit of Oprm1 null mice. We unraveled that Br− not only increases mGlu4 receptor gene expression but also potentiates the effects of the positive allosteric modulator (PAM) of mGlu4 VU0155041, in Oprm1−/− mice and in heterologous cells. Our data reveal the therapeutic potential of Br− administration and its combination with a PAM of mGlu4 receptor for the treatment of ASD.
Materials and methods
Animals
The Oprm1−/− (B6.129S2-Oprm1tm1Kff/J) [48] and Shank3Δex13-16−/− (B6.129-Shank3tm2Gfng/J, so called Shank3B−/−, lacking the PDZ domain) [47] mouse lines were acquired from Jackson Laboratories (Farmington, USA) and bred on a hybrid background: 50% 129SVPas - 50% C57BL/6 J. Fmr1-KO(2) mice [49] were generously provided by R. Willemsen (Erasmus University Medical Center, Rotterdam, The Netherlands) and bred on a C57BL/6 J background. Equivalent numbers of male and female mice were generated in-house from homozygous parents (F2), bred from heterozygous animals (F1), to prevent genetic derivation. Mice in the same cage were of the same genotype: this breeding scheme and housing conditions likely favored social deficits in mutant mice by maintaining them together during early post-natal development [50]. For similar reasons, mice in a same cage received the same pharmacological treatment. No statistical methods were used to predetermine sample size, which was based on prior experience with the assays used. Mice were aged 8−12 weeks at the beginning of experiments. Except otherwise stated, animals were group-housed and maintained on a 12 h light/dark cycle (lights on at 7:00 AM) at controlled temperature (21 ± 1 °C); food and water were available ad libitum. Cardboard igloos and laying (Dietex®, Argenteuil, France) were provided in each cage as enrichment. Each experimental mouse was weighed on the morning of each drug treatment, to calculate dose by body weight. All experimental procedures were conducted in accordance with the European Communities Council Directive 2010/63/EU and approved by the Comité d’Ethique en Expérimentation animale Val de Loire (C2EA-19).
Drugs
Mice were treated with vehicle (NaCl 0.9%; ip, 10 or 20 ml/kg), NaBr (Sigma-Aldrich, Saint-Quentin Fallavier, France) administered either chronically (once a day, 10, 30, 70, 125, 250 and 500 mg/kg; i.p. or per os, in a volume of 20 ml/kg – except for combination with VU0155041: 10 mg/kg) or acutely (250 mg/kg, 20 ml/kg), KBr (Sigma-Aldrich, Saint-Quentin Fallavier, France; 145 mg/kg; i.p., 20 ml/kg), bumetanide (R&D systems, Minneapolis, USA, 0.5 and 2 mg/kg; i.p., 20 ml/kg) or VU0155041 (Cayman Chemical, Ann Arbor, USA, once a day, i.p., 1 mg/kg, 10 ml/kg). Doses of bumetanide were chosen based on previous studies [33, 51]; liminal dose of VU0155041 was set based on previous studies [43, 52] and a pilot experiment showing no detectable effect in the social interaction test. When treatment was given chronically, behavioral testing started 8 days after beginning of daily administration. Treatment was maintained for 8−18 consecutive days (see timelines in Figs. 1, 4 and 5), allowing thorough behavioral phenotyping. On testing days, or when treatment was given acutely, drugs were administered 30 min before behavioral assays.
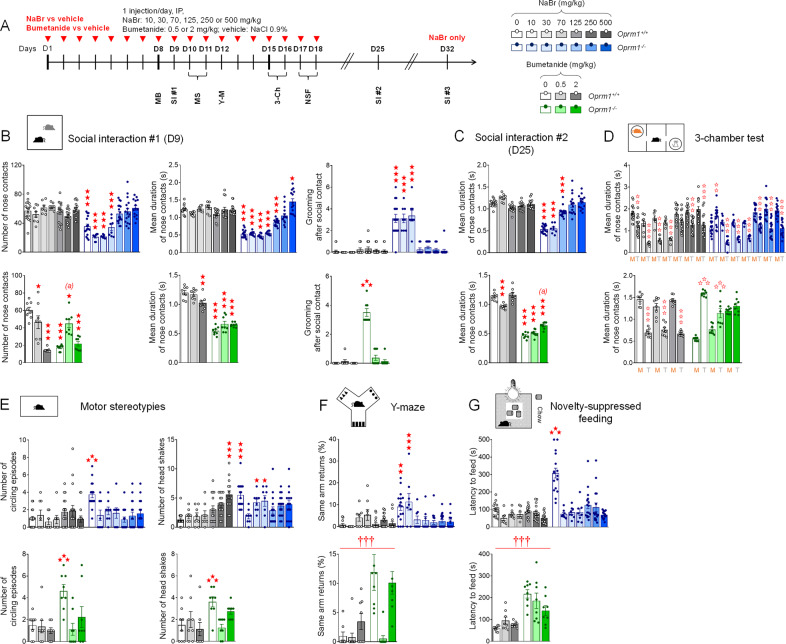
Fig. 1. Chronic sodium bromide dose-dependently relieved social behavior deficits in Oprm1−/− mice, demonstrating superior effects to chronic bumetanide.
A Oprm1+/+ and Oprm1−/− mice were treated either with NaBr (0, 125−500 mg/kg: n = 14−20 mice per genotype and dose; 10−70 mg/kg: n = 8 mice per genotype and dose) or with bumetanide (0, 0.5 and 2 mg/kg: n = 8−10 mice per genotype and dose) once daily for 18 days. Behavioral testing started on D8; social interaction was retested 1 week and 2 weeks after cessation of chronic administration. B In the direct social interaction test (D9, 10 min), chronic NaBr administration relieved social deficits of Oprm1 null mice in a dose-dependent manner for doses over 125 mg/kg; it had no detectable effect in Oprm1+/+ mice. Bumetanide had only partial effects, increasing the number of nose contacts (low dose) and suppressing grooming after social contact; at the highest dose, it impaired social interaction in wild-type controls. C One week after cessation of treatment, beneficial effects of bromide administration were preserved for doses over 125 mg/kg; bumetanide-treated mutants displayed longer nose contacts (high dose). D In the three-chamber test (10 min/phase), NaBr treatment rescued social preference in Oprm1 mutants since the dose of 10 mg/kg, while bumetanide increased their interest for the mouse without reducing their abnormal interest for the object. E Chronic NaBr administration suppressed stereotypic circling episodes in Oprm1−/− mice since the dose of 10 mg/kg and less consistently reduced the number of head shakes (doses over 125 mg/kg) during a 10 min observation session. In wild-type controls, NaBr at 500 mg/kg increased the frequency of grooming episodes and head shakes. Bumetanide suppressed stereotypic circling and head shakes. F In the Y-maze (5 min), NaBr suppressed perseverative same arm returns from the dose of 70 mg/kg; bumetanide had not significant effect despite a tendency for the dose of 0.5 mg/kg to relieve perseveration. G In the novelty-suppressed feeding test (<15 min), sodium bromide normalized the latency to feed in Oprm1 null mice to wild-type levels since the lowest dose tested in all mice; bumetanide had no significant effect in this test. Results are shown as scatter plots and mean ± sem. Daggers: genotype effect, asterisks: treatment effect, solid stars: genotype x treatment interaction (comparison to wild-type vehicle condition), open stars: genotype x treatment x stimulus interaction (mouse versus object comparison), (a) genotype x treatment interaction (comparison with knockout vehicle condition, p < 0.001) (two-way ANOVA or three-way ANOVA with stimulus as repeated measure, followed by Newman-Keuls post-hoc test). One symbol: p < 0.05, two symbols: p < 0.01; three symbols: p < 0.001. More behavioral parameters in Figs. S2, S3 and S4. 3-Ch 3-chamber test, M Mouse, MB Marble burying, MS Motor stereotypies, NSF Novelty-suppressed feeding, SI Social interaction, T Toy, Y-M Y-maze.
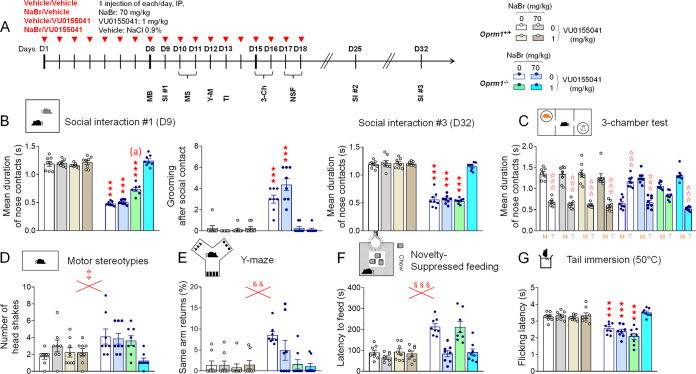
Fig. 4. Sodium bromide and VU0155041, a positive allosteric modulator of mGlu4 receptors, show synergistic effects in Oprm1−/− mice.
A Oprm1+/+ and Oprm1−/− mice were treated either with vehicle, NaBr (70 mg/kg), VU0155041 (1 mg/kg) or NaBr and VU0155041 (70 and 1 mg/k, respectively; 8 mice per genotype and dose) once daily for 18 days. Behavioral testing started on D8; social interaction was retested 1 week and 2 weeks after cessation of chronic administration. B In the direct social interaction test (10 min), NaBr and VU0155041 treatments demonstrated synergistic effects in restoring the duration of nose contacts in Oprm1−/− mice. VU0155041 at 1 mg/kg, however, was sufficient to suppress grooming after social contact. Beneficial effects of combined NaBr/VU0155041 were fully maintained two weeks after cessation of treatment. C In the 3-chamber test (10 min/phase), VU0155041 at 1 mg/kg increased the duration of nose contacts with the mouse to that of the toy in Oprm1−/− mice; NaBr at 70 mg/kg and combined NaBr/VU0155041 treatment fully restored longer nose contacts with the mouse. D Combined NaBr/VU0155041 administration reduced head shakes in Oprm1−/− and Oprm1+/+ mice during a 10 min observation session. E VU0155041 treatment was sufficient to suppress perseverative same arm returns in Oprm1−/− mice exploring the Y-maze (5 min) and (F) NaBr administration was sufficient to normalize their latency to feed in the novelty-suppressed feeding test (<15 min). G In the tail immersion test at 50 °C, only combined NaBr/VU0155041 treatment restored flicking latency of Oprm1−/− mice to wild-type levels. Results are shown as scatter plots and mean ± sem. Solid stars: genotype x NaBr x VU0155041 interaction (comparison to wild-type vehicle condition), open stars: genotype x stimulus x NaBr x VU0155041 interaction (mouse versus object comparison), (a) genotype x NaBr x VU0155041 interaction (comparison with knockout vehicle condition, p < 0.001), double dagger: NaBr x VU0155041 interaction, ampersand: genotype x VU0155041 interaction, section: genotype x NaBr interaction (three-way or four-way ANOVA followed by Newman-Keuls post-hoc test). One symbol: p < 0.05, two symbols: p < 0.01; three symbols: p < 0.001. 3-Ch 3-chamber test, M Mouse, MB Marble burying, MS Motor stereotypies, NSF Novelty-suppressed feeding, SI Social interaction, T Toy, TI Tail immersion, Y-M Y-maze. More behavioral parameters in Figs. S10 and S11.
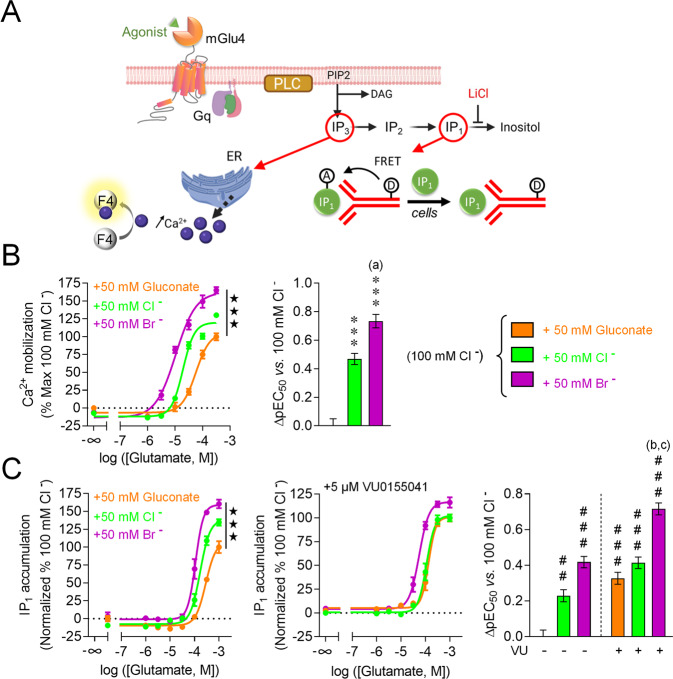
Fig. 5. Bromide ions behave as PAMs of the mGlu4 receptor and shows synergistic effects with the mGlu4 PAM VU0155041.
A Signaling cascade of mGlu4 receptor when coupled with the chimeric G-protein Gαqi9 (to allow the recruitment of the phosphoinositide pathway) and experimental principles of the calcium mobilization (B) and IP1 accumulation assays (C). B In the calcium mobilization assay, bromide ions behave as PAM of mGlu4, demonstrating broader effects than chloride ions on both pEC50 and Emax. C In the IP1 accumulation assay, bromide confirmed its PAM effects; when supplemented with VU0155041, facilitation of mGlu4 signaling was even increased, as seen by a further rise in ∆pEC50. Results are shown as mean ± SEM of three independent experiments realized in triplicates. Solid stars: effect of ion concentration on Emax; asterisks: effect of ion concentration on ∆pEC50, comparison with physiological conditions (100 mM Cl− + 50 mM gluconate); (a): comparison with high chloride condition (150 mM Cl−, p < 0.0001); hashtags: effect of ion concentration and VU0155041 on ∆pEC50, comparison with physiological conditions (100 mM Cl− + 50 mM gluconate); (b) and (c): comparison with bromide conditions (100 mM Cl− + 50 mM Br−) with or without VU0155041 (p < 0.0001) (One-way ANOVA, followed by Tukey’s post-hoc test). Two symbols: p < 0.001, three symbols: p < 0.0001. DAG Diacylglycerol, ER Endoplasmic reticulum, F4 Fluo4 calcium probe, FRET Fluorescence resonance energy transfer, PLC Phospholipase C, IP1/2/3 Inositol mono/di/triphosphate.
Behavioral experiments
When assessing effects of chronic administration, experiments were performed successively (timelines in Figs. 1, 4, and 5) [1, 2]. Testing order was chosen to minimize the incidence of anxiety. Experiments were conducted and analyzed blind to genotype and experimental condition.
Social abilities
Direct social interaction test
On testing day, a pair of unfamiliar mice (not cage mates, age-, sex-, genotype- and treatment-matched) was introduced in one of 4 square arenas (50 × 50 cm, separated by 35cm-high opaque grey Plexiglas walls) over a white infrared floor (View Point, Lyon, France) for 10 min (15 lx). Each arena received a black plastic floor (transparent to infrared) to minimize anxiety levels. The total amount of time spent in nose contact (nose-to-nose, nose-to-body and nose-to-anogenital region), the number of these contacts, the time spent in paw contact and the number of these contacts, grooming episodes (allogrooming), notably ones occurring immediately (<5 s) after a social contact, as well as the number of following episodes were scored a posteriori on video recordings (infrared light-sensitive video camera) using an ethological keyboard (Labwatcher®, View Point, Lyon, France) by trained experimenters, and individually for each animal [1, 2]. The mean duration of nose and paw contacts was calculated from previous data [3–5].
Three-chamber social preference test
The test apparatus consisted of a transparent acrylic box (exterior walls blinded with black plastic film); partitions divided the box into three equal chambers (40 × 20 x 22.5 cm). Two sliding doors (8 × 5 cm) allowed transitions between chambers. Cylindrical wire cages (18 × 9 cm, 0.5 cm diameter-rods spaced 1 cm apart) were used to contain the mouse interactor and object (soft-toy mouse). The test was performed in low-light conditions (15 lx) to minor anxiety. Stimulus wild-type mice were habituated to wire cages for 2 days before the test (20 min/day). On testing day, the experimental mouse was introduced to the middle chamber and allowed to explore the whole apparatus for a 10-min habituation phase (wire cages empty). The experimental mouse was then confined back in the middle chamber while the experimenter introduced an unfamiliar wild-type age and sex-matched mouse (8-14-week-old, grouped housed) into a wire cage in one of the side-chambers and a soft toy mouse (8 × 10 cm) in the second wire cage. Then the experimental mouse was allowed to explore the apparatus for a 10-min interaction phase. The time spent in each chamber, the time spent in nose contact with each wire cage, as well as the number of these nose contacts were scored a posteriori on video recordings using an ethological keyboard (Labwatcher®, View Point, Lyon, France) by trained experimenters. The mean duration of nose contacts was calculated from these data [3–5]. The relative position of stimulus mice was counterbalanced between groups.
Protocols for assessing stereotyped behavior and anxiety, gene expression (qRT-PCR, see dissection in Fig. S1) and for in cellulo pharmacology can be found in Supplement 1.
Statistics
Statistical analyses were performed using Statistica 9.0 software (StatSoft, Maisons-Alfort, France). For all comparisons, values of p < 0.05 were considered as significant. Statistical significance in behavioral experiments was assessed using one or two-way analysis of variance (drug, stimulus and treatment effects) followed by Newman-Keuls post-hoc test. Significance of quantitative real-time PCR (qRT-PCR) results was assessed after transformation using a two-tailed t-test, as previously described [52]; an adjusted p value was calculated using Benjamin-Hochberg correction for multiple testing. Unsupervised clustering analysis was performed on transformed qRT-PCR data using complete linkage with correlation distance (Pearson correlation) for genotype and treatment (Cluster 3.0 and Treeview software) [43, 52]. When used for clustering analysis (Fig. 3B), behavioral data were normalized to vehicle-vehicle condition and transformed using the same formula as qRT-PCR data. As regards in vitro experiments, statistical differences between pEC50, ∆pEC50 and Emax were determined using a one-way analysis of variance followed by Tukey’s post-test.
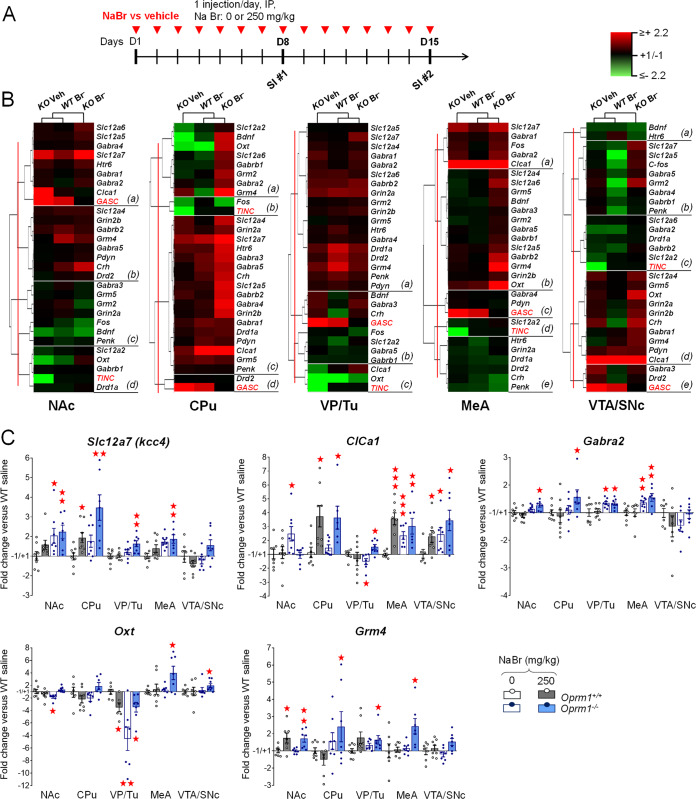
Fig. 3. Chronic sodium bromide treatment induced transcriptional modifications in the reward/social circuit of Oprm1−/− mice.
A Oprm1+/+ and Oprm1−/− mice were treated for 2 weeks with either vehicle or NaBr (250 mg/kg, i.p. once a day). They undergone two sessions of direct social interaction (10 min), at D8 and D15, the latter 45 min before sacrifice for qRT-PCR experiment. We evaluated the expression of 27 genes of interest in 5 regions of the reward/social circuit: the NAc, CPu, VP/Tu, MeA and VTA/SNc. B Clustering analysis revealed that the most contrasted transcriptional profiles were observed in Oprm1−/− mice under NaBr versus vehicle treatment; mRNA levels, however, were poorly correlated with behavioral parameters (red characters, GASC: grooming after social contact, TINC: time in nose contact). Bromide treatment induced rather than normalized gene expression in Oprm1 null mice, most remarkably in the CPu. C Focusing on candidate genes, we unraveled an upregulation of the chloride transporters Slc12a7, coding for KCC4, and Clca1, coding for the calcium-activated chloride channel regulator 1 (CLCA1), as well as Gabra2, coding for the α2 subunit of the GABAA receptor, in mutant mice under NaBr treatment. Finally, chronic NaBr in mutant mice increased the levels of Oxt and Grm4, coding respectively for oxytocin and mGlu4 receptor, across brain regions. Gene (n = 8 per group) expression data are expressed as fold change versus Oprm1+/+ - vehicle group (scatter plots and mean ± SEM). Comparison to Oprm1+/+ - vehicle group (two-tailed t-test): One star p < 0.05, two stars p < 0.01, three stars p < 0.001. qRT-PCR data used for clustering are displayed in Table S2.
Results
Chronic sodium bromide relieved autistic-like symptoms in Oprm1−/− mice more efficiently than bumetanide
We first assessed the effects of NaBr administration over a wide range of doses (10−500 mg/kg, i.p.) in Oprm1−/− mice and their WT counterparts and compared with bumetanide administration (0.5 and 2 mg/kg, i.p.) (Fig. 1A). Treatment was given chronically to mimic clinical conditions.
Social interaction was evaluated after 9 days of chronic NaBr treatment (Fig. 1B, more parameters in Fig. S2A). Oprm1−/− mice exhibited a severe decrease in social interaction; chronic NaBr administration from the dose of 125 mg/kg dose-dependently relieved this deficit in mutant mice, as evidenced by restored number (genotype [G] x treatment [T]: F6,163 = 13.2, p < 0.0001) and mean duration (G x T: F6,163 = 31.6, p < 0.0001) of nose contacts. Chronic NaBr also normalized the frequency of grooming after social contact in mutants, since the dose of 70 mg/kg (G x T: F6,163 = 32.2, p < 0.0001). In contrast, acute NaBr administration (250 mg/kg) had little effect on social interaction, increasing partially the number of nose contacts but not their duration, and suppressing grooming, including those occurring after a social contact (Fig. S2B). When given chronically, NaBr (over 125 mg/kg) produced relieving effects that were still detectable one week after cessation of treatment, as evidenced by preserved restoration of the duration of nose contacts (G x T: F6,134 = 53.3, p < 0.0001) (Fig. 1C) as well as most interaction parameters in this test (Fig. S3A). These beneficial effects had mostly vanished after two weeks (Fig. S3B).
In contrast, chronic bumetanide increased the number of nose contacts at the dose of 0.5 mg/kg (G x T: F2,42 = 22.6, p < 0.0001) but failed to significantly increase their duration (G x T: F2,42 = 22.6, p < 0.0001) and finally suppressed grooming episodes occurring after social contact at both tested doses (G x T: F2,42 = 80.7, p < 0.0001). Of note, chronic bumetanide showed deleterious effects on social interaction in WT controls, reducing the number and duration of nose contacts at high dose. One week after cessation of treatment, partial effects of bumetanide were still detectable on the duration of nose contacts for the dose of 2 mg/kg (G x T: F2,42 = 9.3, p < 0.0001) (Figs.1C and S3A).
In the 3-chamber test (Figs. 1D and S2C), Oprm1−/− mice showed a severe impairment in social preference, as evidenced by longer nose contacts made with the toy over the mouse. Chronic NaBr completely restored this preference in mutant mice, which displayed longer nose contacts with the mouse since the lowest dose of bromide administered (G x T x stimulus [S]: F6,160 = 8.9, p < 0.0001). Chronic bumetanide in mutant mice dose-dependently increased the duration of nose contacts with the mouse without reducing the duration of contacts with the toy (G x T x S: F2,42 = 32.5, p < 0.0001).
Regarding stereotypic behavior, Oprm1−/− mice displayed spontaneous stereotypic circling and head shakes (Fig. 1E, see also Fig. S4A) that were decreased under NaBr treatment since the lowest dose (circling: G x T: F6,161 = 4.6, p < 0.001; shakes: G x T: F6,161 = 7.0, p < 0.0001). In Oprm1+/+ mice, NaBr dose-dependently increased the number of head shakes (G x T: F6,161 = 7.0, p < 0.0001). Bumetanide suppressed circling (G x T: F2,42 = 7.4, p < 0.01) and head shakes (G x T: F2,42 = 5.4, p < 0.01) in mutant mice. NaBr and bumetanide treatments failed to normalize marble burying (Fig. S4B). However, in the Y-maze test (Figs. 1F and S4C), bromide decreased the number of perseverative same arm returns in Oprm1 null mice to wild-type levels since the dose of 30 mg/kg (G x T: F6,161 = 6.7, p < 0.0001), while bumetanide at 0.5 mg/kg tended to suppress same arm returns (G: F2,46 = 19.7, p < 0.001).
We assessed anxiety levels in Oprm1−/− mice and their WT counterparts using the novelty suppressed feeding test (Figs. 1G and S4D). Mutant mice displayed exaggerated anxiety in this test, with increased latency to eat. Chronic bromide normalized eating latency (G x T: F6,160 = 6.7, p < 0.0001) to wild-type levels in Oprm1 knockout mice since the lowest dose tested. Chronic bumetanide had no detectable effect on this parameter (G: F2,42 = 27.1, p < 0.0001).
In a next series of experiments, we tested the effects of NaBr administered sub-chronically (4–5 days, Fig. S5A) via oral route (gavage, 250 mg/kg once per day) in Oprm1 null mice and their wild-type counterparts. Oral NaBr suppressed stereotyped circling and head shakes in Oprm1−/− mice (Fig. S5B). In the direct social interaction test, repeated oral NaBr treatment normalized nose and paw contacts, as well as following and grooming episodes of Oprm1 null mice in a similar way as it did after intra-peritoneal injection (Fig. S5C). Also, we assessed the behavioral effects of chronic administration (Fig. S6A) of another bromide salt, KBr. A dose of KBr equivalent to 250 mg/kg NaBr being toxic in pilot experiments, we thus lowered the dose to 145 mg/kg KBr (i.p.), equivalent to 125 mg/kg NaBr. KBr treatment normalized social interaction parameters in Oprm1−/− mice (Fig. S6B), with carry-over effects (Fig. S6C), and social preference in the 3-chamber test (Fig. S6D). KBr administration did not suppress excessive marble burying in mutant mice (Fig. S6E) but normalized their spontaneous circling and head shakes (Fig. S6F), perseverative same arm entries in the Y-maze (Fig. S6G) and latency to eat in the novelty-suppressed feeding test (Fig. S6H). Beneficial effects of NaBr treatment in Oprm1−/− mice were thus fully replicated by KBr.
We monitored activity in several behavioral tests: vertical activity (rearing) in the direct social interaction test and during the scoring of motor stereotypies, and horizontal activity in the 3-chamber (entries in chambers) and Y-maze (entries in arms) test. Oprm1 null mice did not show any modification of activity; bromide administration increased vertical activity at low doses (Fig. S2A) and horizontal activity at high doses (Figs. S2C and S4C).
Chronic sodium bromide relieved social behavior deficits, stereotypies and excessive anxiety in Fmr1−/− and Shank3∆ex13-16−/− mice
We then questioned whether beneficial effects of NaBr on autistic-like symptoms may generalize to the Fmr1 null and Shank3∆ex13-16 knockout mouse lines. To this purpose, we evaluated the effects of chronic NaBr administration at the dose of 250 mg/kg (i.p.) on autism-sensitive behaviors in these lines (Fig. 2A).
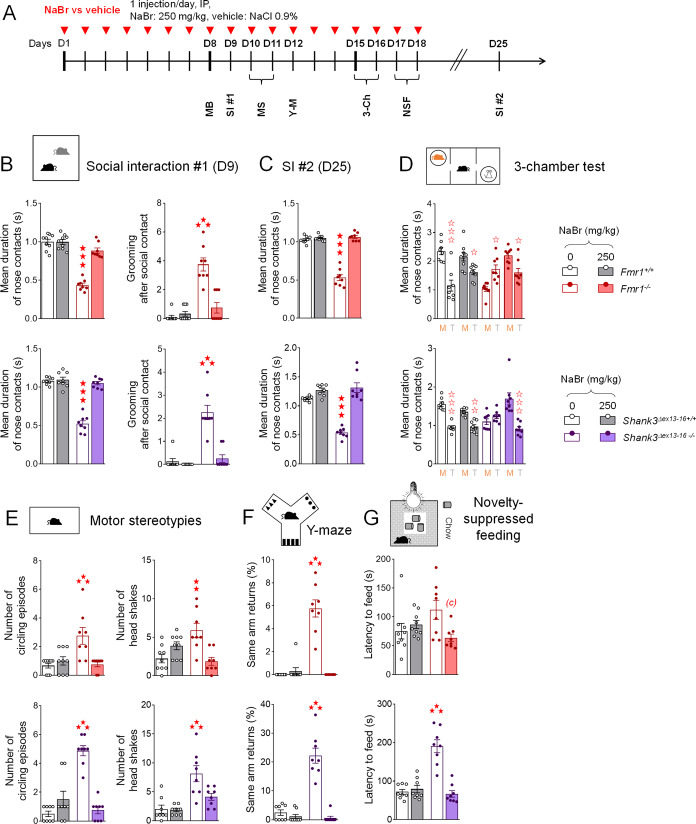
Fig. 2. Chronic sodium bromide administration relieved social behavior deficits, stereotypies and exacerbated anxiety in Fmr1−/− and Shank3∆ex13-16−/− mice.
A Fmr1−/− or Shank3∆ex13-16−/− and their respective wild-type counterparts were treated with NaBr (0 or 250 mg/kg; n = 8 mice per genotype and treatment) once daily for 18 days. Behavioral testing started on D8; social interaction was retested 1 week (D25) after cessation of chronic administration. B In the direct social interaction test (10 min), chronic NaBr treatment normalized interaction parameters to wild-type levels in both Fmr1 and Shank3 mutant lines. C One week after cessation of treatment, beneficial effects on nose contact duration were maintained. D In the 3-chamber test (10 min/phase), chronic NaBr administration rescued preference for making longer nose contacts with the mouse in both mutant mouse lines. E Chronic sodium bromide treatment suppressed stereotypic circling and head shakes in Fmr1−/− and Shank3∆ex13-16−/− mice during a 10 min observation session. F During Y-maze exploration (5 min), chronic NaBr suppressed perseverative same arm returns in both Fmr1 and Shank3 mutant lines. G Finally, in the novelty-suppressed feeding test (<15 min), sodium bromide-treated Fmr1−/− or Shank3∆ex13-16−/− mice displayed reduced or normalized latency to feed, respectively. Results are shown as scatter plots and mean ± sem. Daggers: genotype effect, solid stars: genotype x treatment interaction (comparison to wild-type vehicle condition), open stars: genotype x treatment x stimulus interaction (mouse versus object comparison), (a) genotype x treatment interaction (comparison with knockout vehicle condition, p < 0.001), (c) genotype x treatment interaction (comparison to knockout vehicle condition, p < 0.05) (two-way ANOVA or three-way ANOVA with stimulus as repeated measure, followed by Newman-Keuls post-hoc test). One symbol: p < 0.05, two symbols: p < 0.01; three symbols: p < 0.001. More behavioral parameters in Figs. S7 and S8. 3-Ch 3-chamber test, AAR Alternate arm returns, M Mouse, MB Marble burying, MS Motor stereotypies, NSF Novelty-suppressed feeding, SAR Same arm returns, SPA Spontaneous alternation, SI Social interaction, T Toy, Y-M Y-maze.
As concerns social behavior (Figs. 2B and S7A), chronic bromide in Fmr1−/− as well as Shank3∆ex13-16−/− mice restored direct social interaction, as illustrated by rescued duration of nose contacts (G x T – Fmr1: F1,30 = 49.5, p < 0.0001; Shank3∆ex13-16: F1,28 = 73.0, p < 0.0001) and suppressed grooming after social contact (G x T- Fmr1: F1,30 = 30.1, p < 0.0001; Shank3∆ex13-16: F1,28 = 25.0, p < 0.0001). One week after interruption of NaBr treatment (Figs. 2C and S7B), significant beneficial effects were still detected, notably on the duration of nose contacts (Fmr1: G x T: F1,30 = 128.9, p < 0.0001; Shank3∆ex13-16: F1,28 = 42.3, p < 0.0001).
We further assessed social behavior under chronic bromide exposure using the 3-chamber test (Figs. 2D and S7C). Fmr1 knockout mice made longer nose contacts with the object than with the living congener in this test, demonstrating disrupted social preference. Chronic NaBr treatment restored a preference for making longer nose contacts with the mouse (G x T x S: F1,29 = 18.4, p < 0.001). Likewise, Shank3∆ex13-16−/− mice treated with vehicle made nose contacts of equivalent duration with the mouse and the object, and NaBr restored preference for making longer nose contacts with the mouse (G x T x S: F1,28 = 26.9, p < 0.0001). Thus, NaBr treatment rescued social preference in both models.
Regarding stereotypic behavior, chronic NaBr normalized the number of circling episodes (Fmr1, G x T: F1,30 = 11.9, p < 0.01; Shank3∆ex13-16, G x T: F1,28 = 48.4, p < 0.0001) and head shakes (Fmr1, G x T: F1,30 = 68.0, Shank3∆ex13-16, G x T: F1,28 = 5.3, p < 0.05) in both mutant lines (Figs. 2E and S8A). NaBr treatment did not normalize marble burying (Fig. S8B) but suppressed perseverative same arm returns (Figs. 2F and S8C) of Fmr1 null (G x T: F1,30 = 61.9, p < 0.0001) and Shank3∆ex13-16 knockout (G x T: F1,28 = 47.5, p < 0.0001) mice during Y-maze exploration.
As regards anxiety, a tendency for Fmr1 null mice for increased latency to eat in the novelty-suppressed feeding test (Figs. 2G and S8D) did not reach significance; however chronic bromide reduced this latency (G x T: F1,30 = 6.7, p < 0.05). Shank3∆ex13-16−/− mice took longer to eat in the open field and NaBr administration normalized this latency (G x T: F1,28 = 35.0, p < 0.0001).
Vertical activity was not modified in Fmr1−/− and Shank3∆ex13-16−/− mice; the latter showed decreased horizontal activity in the Y-maze (Fig. S8C) which, together with impaired burying during scoring of spontaneous stereotypies (Fig. S8A) and in the marble burying test (Fig. S8B), points to altered motor function/coordination. Bromide ions have no effect on activity and burying behavior in Fmr1−/− as well as Shank3∆ex13-16−/− mice.
Chronic sodium bromide modulates transcription in the reward circuit of Oprm1−/− mice
To shed light on the molecular mechanism involved in beneficial effects of chronic sodium bromide administration, we assessed the effects of a 2-week NaBr treatment (vehicle versus 250 mg/kg, i.p.) on gene expression in Oprm1 null mice across five regions of the brain reward/social circuit: NAc, CPu, VP/Tu, MeA and VTA/SNc. Mice underwent a first session of social interaction after one week under treatment and a second 45 min before sacrifice for qRT-PCR experiment (Fig. 3A). We focused primarily on genes coding for chloride transporters (Slc12a2 [NKCC1], Slc12a4,5,6,7 [KCC1,2,3,4, respectively], ClCa1), GABAA receptor subunits (Gabra1,2,3,4,5, Gabrb1,2) and glutamate receptors (Grm2,4,5) and subunits (Grin2a,2b). In addition, we evaluated the expression of marker genes of neuronal expression and plasticity (Fos, Bdnf), social behavior (Oxt) and striatal projection neurons (SPNs; Crh, Drd1a, Drd2, Htr6, Pdyn, Penk).
We performed hierarchical clustering analysis of qRT-PCR data for each brain region to visualize the influence of NaBr treatment on gene expression (Fig. 3B, Table S2). Overall, transcriptional profiles in Oprm1−/− mice under vehicle and NaBr treatment differed the most, while mRNA levels correlated poorly with social interaction parameters (displayed in Fig. S9). These results indicate that bromide induced transcriptional changes on its own rather than it normalized gene expression in Oprm1 knockouts (as observed for behavioral parameters). This was particularly true in the CPu, where Oprm1−/− mice under bromide treatment displayed predominant up-regulated gene expression (clusters a and c).
This overall profile was confirmed when focusing on candidate genes (Fig. 3C). We ought to acknowledge here that the sample number of mice allocated to each experimental condition was low to address the complex influences of genotype and pharmacological treatment, which may have limited the statistical power. For this reason, we focused our attention on gene expression regulations affecting either several brain regions for the same gene, or several genes of the same family. Chronic NaBr up regulated the expression of Slc12a7 in the NAc, CPu, VP/Tu and MeA. ClCa1 mRNA levels were increased in the NAc, MeA and VTA/SNc while reduced in the VP/Tu of mutant mice; they were normalized by NaBr treatment in the NAc, increased in the VP/Tu and maintained high in the MeA and VTA/SNc. In the CPu, bromide increased ClCa1 transcription in mice of both genotypes. As regards the GABAergic system, chronic NaBr in Oprm1−/− mice stimulated the expression of Gabra2, coding for the α2 subunit of the GABAA receptor, in the NAc and CPu and left this expression high in the VP/TU and MeA. Remarkably, bromide consistently upregulated the expression of Gabra3, Gabra4, Gabra5, Gabrg1 and Gabrb2 in the CPu of mutant mice (Table S2). Oxt (coding for oxytocin) mRNA levels were decreased in the NAc and VP/Tu of Oprm1−/− mice and normalized by NaBr in the former and partially in the latter; bromide induced Oxt expression in the MeA and VTA/SNc. Finally, chronic NaBr upregulated the expression of Grm4, coding for the metabolic glutamate receptor mGlu4, in all brain regions but the VTA/SNc of mutant mice, and in the NAc of wild-type controls. Transcriptional results indicate that bromide regulated the expression of Cl− transporters; it also modulated the expression genes related to the GABA system or involved in the control of social behavior.
Synergistic effects of chronic bromide and mGlu4 receptor facilitation in Oprm1 null mice
Intrigued by increased Grm4 transcription in Oprm1−/− mice under bromide treatment, whose autistic-like symptoms were relieved when stimulating mGlu4 activity [43], we studied the effects of combined administration of chronic liminal doses of NaBr (70 mg/kg, i.p.) and VU0155041 (1 mg/kg, i.p.) in Oprm1−/− and Oprm1+/+ mice (Fig. 4A).
In the direct social interaction test (Figs. 4B and S10A), NaBr at 70 mg/kg had no effect in Oprm1−/− mice (see also Fig. 1B); VU0155041 partially rescued the duration of their nose contacts (G x VU0155041[V]: F1,56 = 157.1, p < 0.0001) and suppressed grooming episodes after a social contact (G x VU0155041[V]: F1,56 = 83.3, p < 0.0001). Combined treatments normalized the duration of nose contacts (G x bromide [B] x VU0155041[V]: F1,56 = 31.1, p < 0.0001) and number of grooming episodes after social contact (G x B x V: F1,56 = 5.8, p < 0.05) in these mice. Restoration of the mean duration of nose contacts was fully preserved two weeks after cessation of treatment (G x B x V: F1,56 = 57.3, p < 0.0001) (see also Fig. S10B, C). Synergistic effects were not observed in the 3-chamber test (Figs. 4C and S11A), where NaBr at 70 mg/kg was notably sufficient to restore longer nose contacts with the mouse versus the toy in Oprm1−/− mice (G x B x S: F1,55 = 61.6, p < 0.0001).
As regards stereotypic behavior (Figs. 4D and S11B), combined NaBr and VU0155041 treatments reduced the number of head shakes in Oprm1−/− and Oprm1+/+ mice (B x V: F1,56 = 4.1, p < 0.05). Chronic VU0155041 was sufficient to suppress perseverative same arm returns during Y-maze exploration in Oprm1 null mice (G x V: F1,56 = 11.3, p < 0.01) (Figs. 4E and S11C). In the novelty-suppressed feeding test, chronic NaBr was similarly sufficient to normalize the latency to feed (G x V: F1,56 = 11.3, p < 0.01) (Figs. 4F and S11D). Finally, we tested the effects of bromide and VU0155041 on nociceptive thresholds in Oprm1 null mice. At 50 °C, combined NaBr and VU0155041 treatment normalized flicking latency (lowered in mutants), while each compound given alone was ineffective (G x B x V: F1,56 = 20.5, p < 0.0001) (Figs. 4G and S11E). Together, these results indicate that bromide administration and facilitation of mGlu4 activity exert synergistic beneficial effects on autistic-like behavior in Oprm1−/− mice.
Combined liminal doses of bromide ions and VU0155041 increased vertical activity of Oprm1 null mice during the direct social interaction test. This effect disappeared progressively after cessation of treatment (Fig. S11).
Bromide ions behave as positive allosteric modulators of the mGlu4 glutamate receptor
Chloride ions have been shown to facilitate mGlu4 signaling and ligand binding [53, 54]. Here we assessed whether synergistic in vivo effects of bromide treatment and VU0155041 administration may result from a modulation of mGlu4 activity by bromide ions, in addition to their ability to upregulate Grm4 expression (see Fig. 3).
We measured mGlu4 signaling under glutamate stimulation in HEK293T cells transiently expressing mGlu4 receptors and Gαqi9, a Gi/Gq chimeric G-protein [55] that allows mGlu4 to activate the phosphoinositide pathway. Receptor activation was then evaluated by measuring intracellular Ca2+ release or inositol monophosphate (IP1, Fig. 5A). The experiments were performed in buffers containing either a physiological concentration of chloride ions (100 mM, supplemented with 50 mM gluconate to maintain equivalent osmolarity between mediums), 150 mM of chloride ions (classical buffer for cell culture studies) or 100 mM of chloride ions and 50 mM of bromide ions, to compare the effects of modulating chloride and bromide concentrations within a physiological range on mGlu4 activity.
Compared with physiological concentration of chloride, addition of 50 nM bromide significantly improved glutamate potency, showing a 0.73 ± 0.05 log increase in pEC50 (left panel; ion concentration: F2,6 = 104.2, p < 0.0001) in the Ca2+ assay (Fig. 5B). Compared with an equivalent concentration of chloride ( + 50 mM Cl−), bromide showed a higher efficacy (∆pEC50: 0.27 ± 0.04) (right panel; ion concentration: F2,6 = 66.7, p < 0.0001). Further, bromide increased glutamate efficacy, with a 65 ± 9% rise in maximal mGlu4-triggered calcium release (Emax, left panel; ion concentration: F2,21 = 56.2, p < 0.0001).
When measuring IP1 production (Fig. 5C), bromide increased glutamate efficacy (Emax, maximal IP1 production) within a similar range (60 ± 10%) as observed when measuring Ca2+ release (left panel; ion concentration: F2,24 = 22.1, p < 0.0001). pEC50 was consistently increased in presence of bromide ions (left panel; ion concentration: F2,6 = 104.2, p < 0.0001; ∆pEC50 between physiological Cl− concentration and after addition of 50 nM Br−: 0.42 ± 0.03) though to a lower extend as those measured in the Ca2+ assay. When 5 µM of VU0155041 were added, bromide significantly increased glutamate potency compared with physiological concentration of chloride (∆pEC50: 0.72 ± 0.03). Bromide and VU0155041 in combination were also more effective in increasing glutamate potency than VU0155041 (∆pEC50: 0.39 ± 0.03) or bromide (∆pEC50: 0.30 ± 0.03) alone (ion concentration and VU0155041: F5,12 = 49.4, p < 0.0001). These results indicate that sodium bromide behaves as a PAM of mGlu4 receptors. They thus provide a molecular mechanism for synergistic effects of bromide and VU0155041 in Oprm1 null mice and suggest that benefits of bromide treatment in mouse models of ASD involved a facilitation of mGlu4 activity.
Discussion
In the current study, we tested whether bromide ions would relieve autistic-like symptoms in mouse models of ASD. We first assessed bromide effects in the Oprm1−/− mouse model of ASD. In this model, chronic bromide dose-dependently rescued social behavior, at doses (over 125 mg/kg) in the lower range for acute anticonvulsant effects in rodents (0.2–2 g/kg) [56, 57] and slightly superior to those required for antiepileptic effects in dogs (20–100 mg/kg/day; initial dose up to 500 mg/kg) [58, 59] and humans (30–100 mg/kg/day) [60, 61]. At these doses, and for the duration of our experiments, we did not observe toxic effects of bromide administration (except for KBr at 250 mg/kg). In the 3-chamber test, however, beneficial effects of chronic NaBr were detected since the dose of 10 mg/kg, indicating that low doses of bromide can improve social behavior. Effects on social behavior were unlikely the result from increased activity under bromide treatment, as such increase was unevenly observed across doses, time points, bromide salts and models, while the relief of social behavior deficits remained consistent. Acute administration of NaBr had only minor effects on social interaction in Oprm1 null mice, showing that bromide needed to accumulate to reach therapeutic efficacy, as observed in the clinics [61]. Consistent with this, blood concentrations of bromide ions are known to progressively increase upon chronic treatment [62, 63]. As its clearance is slow, bromide has a rather long half-life, about 8–14 days in human adults [61, 64]. In the clinics, such an atypical pharmacokinetic profile implies that bromide blood levels are monitored closely, to avoid toxic accumulation. This profile may account for the carry-over effects of NaBr treatment detected in Oprm1−/− mice. NaBr also reduced stereotypic and perseverative behaviors in Oprm1 knockouts, indicating benefit on the second diagnostic criteria for ASD. Behavioral improvements were replicated after repeated oral administration of NaBr, in agreement with previous reports of oral bioavailability [64]. Further, bromide, known as anxiolytic [37], consistently decreased anxiety levels, often high in ASD [3, 5]. Beneficial effects of chronic NaBr administration in Oprm1−/− mice were replicated using KBr. Convergent effects of NaBr and KBr salts demonstrate that bromide ions are indeed the active compound to relieve ASD-like symptoms.
Effects of chronic NaBr administration were compared to those of the NKCC1 inhibitor bumetanide. Although the most promising drug developed based on the E/I balance hypothesis, bumetanide has been scarcely tested in animal models of ASD. We observed partial beneficial effects of chronic bumetanide on autistic-like behavior in Oprm1−/− mice. In contrast, previous studies have reported a complete rescue of autistic-like social deficits following bumetanide treatment in animal models of ASD, but under conditions where bumetanide was administered preventively rather than curatively [33, 51]. In present study, bumetanide was given in adult Oprm1−/− mice, when neurodevelopmental deficits were fully installed, which may account for partial improvements. These effects were consistent with clinical reports of beneficial effects of the NKCC1 antagonist on social abilities in children and adults with ASD diagnosis [34, 35], maybe too subtle however to be confirmed in larger cohorts, except for a reduction of stereotypies [65]. Importantly, such consistency confers predictive value to the Oprm1 null mouse model, boding well for clinical translation of bromide effects.
After comprehensive testing in Oprm1 null mice, we extended our observation of beneficial effects of bromide administration to Fmr1−/− and Shank3Δex13-16−/− mice, with longer-lasting effects in the former. Interestingly, the three models of ASD used in this study differed in their genetic cause and E/I profile. As regards excitatory neurotransmission, Fmr1 mutants display more frequent miniature excitatory postsynaptic currents (mEPSCs) in the hippocampus [33], persistent activity states in the somatosensory cortex [66] and excessive mGluR1/5-dependent signaling [66, 67], suggesting a global facilitation of glutamatergic transmission. Mutations in Shank3 lead to reduced frequency and amplitude of mEPSCs in the striatum [47, 68] and hippocampus [69], where they also reduced long-term potentiation (LTP) [70, 71]; in Oprm1−/− mice, hippocampal LTP is decreased [44] and the morphology of asymmetrical synapses is altered in the striatum while the expression of key glutamate-related genes is reduced [43]. These data point to impaired glutamatergic neurotransmission in the latter models. On the inhibition side, multiple alterations of the GABAergic system have been documented in Fmr1 null mice [72, 73]. Such deficit, however, is not observed in the striatum, where GABA release is increased [74], possibly a consequence of impaired endocannabinoid-mediated long-term depression (LTD) that represses the activity of D2 dopamine receptor-expressing striatal projection neurons (D2-SPNs) [45]. Remarkably, endocannabinoid-mediated LTD is also deficient in Shank3∆ex13-16 mice, and consequent excessive D2-SPN tone has been linked to stereotyped behavior [75]. In Oprm1−/− mice, facilitating the activity of mGlu4 receptor, which represses D2-SPN activity [76], relieved autistic-like behavior [43]. Together, these data suggest that GABAergic D2-SPNs may represent a common target for bromide effects on the E/I balance across mouse models.
Transcriptional effects of chronic bromide treatment in Oprm1−/− versus Oprm1+/+ mice are consistent with an influence on the E/I balance. NaBr administration tended to restore or increase the expression of all genes coding for Cl− co-transporters tested in these mice, notably the exporters KCC2-4 and CLCA1 (a modulator of the calcium-activated Cl− channel Anoctamine-1/TMEM16A [77]). These transporters have been related to autistic-like features in mouse models [33, 78, 79]. Increased expression of Cl− transporters under chronic NaBr treatment may have been a regulatory response triggered by Br− accumulation, to maintain the extracellular/intracellular gradient of anion concentrations. Cl− and Br− sharing similar physicochemical properties, this increase likely favored a high turnover of both anion species and, thus, depolarizing effects of GABA [80]. Moreover, chronic bromide increased the transcription of genes coding for several GABAA receptor subunits. Previous studies in the field of epilepsy have evidenced a facilitating influence of bromide on GABAergic inhibition [40, 81]. Together, these data suggest that NaBr treatment increased GABA-mediated inhibition.
Besides effects on E/I balance, bromide treatment in Oprm1−/− mice stimulated the expression of Oxt, coding for the social neuropeptide oxytocin, notably in the NAc, where it plays a key role in modulating social reward [82]. Oprm1−/− mice that undergone an appetitive social conditioning displayed similar restoration [50]. Moreover, oxytocin administration rescued social ultrasonic vocalizations in Oprm1 null mice [83]. Thus, restored Oxt mRNA levels in mutants may have contributed to behavioral improvements under bromide administration. Finally, although Grm4 mRNA levels were not low in the striatum of Oprm1−/− mice as in previous studies [43, 50], maybe due to different experimental conditions, chronic NaBr increased its expression in most brain regions studied. By facilitating mGlu4 expression, bromide may thus have relieved autistic-like symptoms, as observed under VU0155041 treatment [43, 84]. Consistent with this, liminal doses of bromide and VU0155041 to Oprm1−/− mice exerted synergistic effects when co-administered. This synergy was observed for core autistic-like symptoms (social and repetitive behaviors) as well as for comorbid anxiety and lowered nociceptive thresholds. Moreover, in heterologous cells, bromide ions behave as better mGlu4 PAMs than it was previously shown for chloride ions [53]. Interestingly, we previously evidenced an upregulation of Grm4 expression in mice under mGlu4 PAM treatment [52]; we thus cannot exclude that increased Grm4 transcription in NaBr-treated mice resulted from mGlu4 PAM effects of bromide ions. Together, our finding suggests that beneficial effects of Br− in ASD models involve a facilitation of mGlu4 signaling. The PAM effect of bromide synergizes with that of VU0155041, providing a molecular mechanism for synergy in vivo. Yet, this mechanism may not have been the only one. At cellular level, VU0155041 represses the activity of D2-SPNs [76], found disinhibited in Fmr1−/− and Shank3Δex13-16−/− mice, while bromide promotes GABAergic transmission. Thus, synergistic action of bromide and mGlu4 PAM may also lie in their common inhibition of a neuronal population, D2-SPNs. Hence, bromide ions act at multiple levels, on chloride gradient, GABA-mediated neurotransmission, mGlu4 signaling and, through these different mechanisms, on gene expression, all these effects converging towards facilitated neuronal inhibition.
We should here consider limitations of this study. First, the benefit of bromide treatment that we detected in social tests may have resulted not only from improvements in the social dimension but also from ameliorated motor, cognitive or somatosensorial processes, altered in mouse models of autism [85, 86]. Further investigations will explore the effects of bromide on such functions. Also, we tested the effects of bromide treatment in adult mice whilst autism is diagnosed early in life and early behavioral/cognitive interventions have proven to be more efficient in relieving autistic features [87, 88]. In future studies, we will administer bromide at young age in mouse models of ASD to delineate the optimal developmental window for its therapeutic action.
In conclusion, the present study reports the therapeutic potential of chronic bromide treatment, alone or in combination with a PAM of mGlu4 receptor, to relieve core symptoms of ASD. Beneficial effects of bromide were observed in three mouse models of ASD with different genetic causes, supporting high translational value. Moreover, bromide has a long history of medical use, meaning that its pharmacodynamics and toxicity are well known, which, combined with long-lasting effects as well as excellent oral bioavailability and brain penetrance, are strong advantages for repurposing.
Supplementary information
Acknowledgements
We thank Dr. Thierry Plouvier for inspiring initial discussions on this project, Pr Frédérique Bonnet-Brilhault for critical reading of the manuscript, Yannick Corde for technical support, and Drs. Jorge Gandía and Sébastien Roux for assistance in performing behavioral experiments. We thank the Experimental Unit PAO-1297 (EU0028, Animal Physiology Experimental Facility, 10.15454/1.5573896321728955E12) from the INRAE-Val de Loire Centre for animal breeding and care.
Author contributions
Conceptualization: CD, JK, JPP, JLM, JAJB; Methodology: JK, JPP, JLM, JAJB; Investigation: CD, AL, AB, DJ, CT, JLM, JAJB; Visualization: CD, AB, CT, JLM, JAJB; Funding acquisition: JPP, JLM, JAJB; Project administration: JK, JPP, JLM, JAJB; Supervision: JK, JPP, JLM, JAJB; Writing: CD, JLM, JAJB.
Funding
We acknowledge the following funding sources: C-VaLo, Cisbio Bioassays, Perkin Elmer (IP1 FRET), European Regional Development Fund (ERDF), Inserm Transfert (CoPOC), Région Centre (ARD2020 Biomédicament – GPCRAb) and ERA-NET NEURON. This work was supported by the Institut National de la Santé et de la Recherche Médicale (Inserm), Centre National de la Recherche Scientifique (CNRS), Institut National de Recherche pour l’Agriculture, l’Alimentation et l’Environnement (INRAe) and Université de Tours.
Data availability
All data that support the findings of this study are available from the corresponding author upon request.
Competing interests
JLM and JAJB are co-inventors of the patent WO2018096184: “Use of bromides in the treatment of autistic spectrum disorder”, US Patent App. 16/464,403, 2021 and patent application EP 21 194 699: “Methods for treating autism spectrum disorders”. CD, AL, AB, DJ, CT, JPP, and JK report no biomedical financial interests or potential conflicts of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Julie Le Merrer, Jerome A. J. Becker.
Contributor Information
Julie Le Merrer, Email: julie.le-merrer@inserm.fr.
Jerome A. J. Becker, Email: Jerome.becker@inserm.fr
Supplementary information
The online version contains supplementary material available at 10.1038/s41386-022-01317-1.
References
- 1.APA. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC; 2013.
- 2.Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120:1183–215.. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- 3.Lai MC, Lombardo MV, Baron-Cohen S. Autism. Lancet. 2014;383:896–910. doi: 10.1016/S0140-6736(13)61539-1. [DOI] [PubMed] [Google Scholar]
- 4.Mazurek MO, Vasa RA, Kalb LG, Kanne SM, Rosenberg D, Keefer A, et al. Anxiety, sensory over-responsivity, and gastrointestinal problems in children with autism spectrum disorders. J Abnorm Child Psychol. 2013;41:165–76. doi: 10.1007/s10802-012-9668-x. [DOI] [PubMed] [Google Scholar]
- 5.Fombonne E, Green Snyder L, Daniels A, Feliciano P, Chung W, Consortium S. Psychiatric and medical profiles of autistic adults in the SPARK cohort. J Autism Dev Disord. 2020;50:3679–98.. doi: 10.1007/s10803-020-04414-6. [DOI] [PubMed] [Google Scholar]
- 6.Satterstrom FK, Kosmicki JA, Wang J, Breen MS, De Rubeis S, An JY, et al. Large-scale exome sequencing study implicates both developmental and functional changes in the neurobiology of autism. Cell. 2020;180:568–84 e23. doi: 10.1016/j.cell.2019.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanders SJ, Murtha MT, Gupta AR, Murdoch JD, Raubeson MJ, Willsey AJ, et al. De novo mutations revealed by whole-exome sequencing are strongly associated with autism. Nature. 2012;485:237–41.. doi: 10.1038/nature10945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park HR, Lee JM, Moon HE, Lee DS, Kim BN, Kim J, et al. A short review on the current understanding of autism spectrum disorders. Exp Neurobiol. 2016;25:1–13. doi: 10.5607/en.2016.25.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee E, Lee J, Kim E. Excitation/Inhibition imbalance in animal models of autism spectrum disorders. Biol Psychiatry. 2017;81:838–47.. doi: 10.1016/j.biopsych.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Nelson SB, Valakh V. Excitatory/Inhibitory balance and circuit homeostasis in autism spectrum disorders. Neuron. 2015;87:684–98.. doi: 10.1016/j.neuron.2015.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubenstein JL, Merzenich MM. Model of autism: Increased ratio of excitation/inhibition in key neural systems. Genes Brain Behav. 2003;2:255–67. doi: 10.1034/j.1601-183X.2003.00037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cellot G, Cherubini E. GABAergic signaling as therapeutic target for autism spectrum disorders. Front Pediatr. 2014;2:70. doi: 10.3389/fped.2014.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robertson CE, Ratai EM, Kanwisher N. Reduced GABAergic action in the autistic brain. Curr Biol: CB. 2016;26:80–5. doi: 10.1016/j.cub.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 14.Muhle R, Trentacoste SV, Rapin I. The genetics of autism. Pediatrics. 2004;113:e472–86. doi: 10.1542/peds.113.5.e472. [DOI] [PubMed] [Google Scholar]
- 15.Jeste SS, Tuchman R. Autism spectrum disorder and epilepsy: Two sides of the same coin? J Child Neurol. 2015;30:1963–71. doi: 10.1177/0883073815601501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strasser L, Downes M, Kung J, Cross JH, De, Haan M. Prevalence and risk factors for autism spectrum disorder in epilepsy: A systematic review and meta-analysis. Dev Med Child Neurol. 2018;60:19–29. doi: 10.1111/dmcn.13598. [DOI] [PubMed] [Google Scholar]
- 17.O’Donnell C, Goncalves JT, Portera-Cailliau C, Sejnowski TJ. Beyond excitation/inhibition imbalance in multidimensional models of neural circuit changes in brain disorders. eLife. 2017;6:e26724. [DOI] [PMC free article] [PubMed]
- 18.Rinaldi T, Kulangara K, Antoniello K, Markram H. Elevated NMDA receptor levels and enhanced postsynaptic long-term potentiation induced by prenatal exposure to valproic acid. Proc Natl Acad Sci USA. 2007;104:13501–6. doi: 10.1073/pnas.0704391104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi R, Redman P, Ghose D, Hwang H, Liu Y, Ren X, et al. Shank proteins differentially regulate synaptic transmission. eNeurology. 2017;4:ENEURO.0163-15.2017. [DOI] [PMC free article] [PubMed]
- 20.Fung LK, Flores RE, Gu M, Sun KL, James D, Schuck RK, et al. Thalamic and prefrontal GABA concentrations but not GABAA receptor densities are altered in high-functioning adults with autism spectrum disorder. Mol Psychiatry. 2020;26:1634–46. doi: 10.1038/s41380-020-0756-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fatemi SH, Reutiman TJ, Folsom TD, Thuras PD. GABA(A) receptor downregulation in brains of subjects with autism. J Autism Dev Disord. 2009;39:223–30. doi: 10.1007/s10803-008-0646-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oblak AL, Gibbs TT, Blatt GJ. Decreased GABA(B) receptors in the cingulate cortex and fusiform gyrus in autism. J Neurochem. 2010;114:1414–23. doi: 10.1111/j.1471-4159.2010.06858.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sesarini CV, Costa L, Granana N, Coto MG, Pallia RC, Argibay PF. Association between GABA(A) receptor subunit polymorphisms and autism spectrum disorder (ASD) Psychiatry Res. 2015;229:580–2. doi: 10.1016/j.psychres.2015.07.077. [DOI] [PubMed] [Google Scholar]
- 24.Mahdavi M, Kheirollahi M, Riahi R, Khorvash F, Khorrami M, Mirsafaie M. Meta-analysis of the association between GABA receptor polymorphisms and Autism Spectrum Disorder (ASD) J Mol Neurosci: MN. 2018;65:1–9. doi: 10.1007/s12031-018-1073-7. [DOI] [PubMed] [Google Scholar]
- 25.Adusei DC, Pacey LK, Chen D, Hampson DR. Early developmental alterations in GABAergic protein expression in fragile X knockout mice. Neuropharmacology. 2010;59:167–71.. doi: 10.1016/j.neuropharm.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Banerjee A, Garcia-Oscos F, Roychowdhury S, Galindo LC, Hall S, Kilgard MP, et al. Impairment of cortical GABAergic synaptic transmission in an environmental rat model of autism. Int J Neuropsychopharmacol. 2013;16:1309–18. doi: 10.1017/S1461145712001216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chao HT, Chen H, Samaco RC, Xue M, Chahrour M, Yoo J, et al. Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes. Nature. 2010;468:263–9. doi: 10.1038/nature09582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curia G, Papouin T, Seguela P, Avoli M. Downregulation of tonic GABAergic inhibition in a mouse model of fragile X syndrome. Cereb Cortex. 2009;19:1515–20.. doi: 10.1093/cercor/bhn159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Han S, Tai C, Jones CJ, Scheuer T, Catterall WA. Enhancement of inhibitory neurotransmission by GABAA receptors having alpha2,3-subunits ameliorates behavioral deficits in a mouse model of autism. Neuron. 2014;81:1282–89.. doi: 10.1016/j.neuron.2014.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ben-Ari Y, Khalilov I, Kahle KT, Cherubini E. The GABA excitatory/inhibitory shift in brain maturation and neurological disorders. Neuroscientist. 2012;18:467–86. doi: 10.1177/1073858412438697. [DOI] [PubMed] [Google Scholar]
- 31.Eftekhari S, Mehvari Habibabadi J, Najafi Ziarani M, Hashemi Fesharaki SS, Gharakhani M, Mostafavi H, et al. Bumetanide reduces seizure frequency in patients with temporal lobe epilepsy. Epilepsia. 2013;54:e9–12. doi: 10.1111/j.1528-1167.2012.03654.x. [DOI] [PubMed] [Google Scholar]
- 32.Soul JS, Bergin AM, Stopp C, Hayes B, Singh A, Fortuno CR, et al. A pilot randomized, controlled, double-blind trial of bumetanide to treat neonatal seizures. Ann Neurol. 2020;89:327–40.. doi: 10.1002/ana.25959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tyzio R, Nardou R, Ferrari DC, Tsintsadze T, Shahrokhi A, Eftekhari S, et al. Oxytocin-mediated GABA inhibition during delivery attenuates autism pathogenesis in rodent offspring. Science. 2014;343:675–9. doi: 10.1126/science.1247190. [DOI] [PubMed] [Google Scholar]
- 34.Lemonnier E, Degrez C, Phelep M, Tyzio R, Josse F, Grandgeorge M, et al. A randomised controlled trial of bumetanide in the treatment of autism in children. Transl Psychiatry. 2012;2:e202. doi: 10.1038/tp.2012.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernell E, Gustafsson P, Gillberg C. Bumetanide for autism: Open-label trial in six children. Acta Paediatrica. 2020;110:1548–53.. doi: 10.1111/apa.15723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pearce JM. Bromide, the first effective antiepileptic agent. J Neurol, Neurosurg, Psychiatry. 2002;72:412. doi: 10.1136/jnnp.72.3.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uhr L, Pollard JC, Miller JG. Behavioral effects of chronic administration of psychoactive drugs to anxious patients. Psychopharmacologia. 1959;1:150–68.. doi: 10.1007/BF00409114. [DOI] [PubMed] [Google Scholar]
- 38.Almeida AC, Scorza FA, Rodrigues AM, Arida RM, Carlesso FN, Batista AG, et al. Combined effect of bumetanide, bromide, and GABAergic agonists: an alternative treatment for intractable seizures. Epilepsy Behav. 2011;20:147–9. doi: 10.1016/j.yebeh.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 39.Woody RC. Bromide therapy for pediatric seizure disorder intractable to other antiepileptic drugs. J Child Neurol. 1990;5:65–7. doi: 10.1177/088307389000500116. [DOI] [PubMed] [Google Scholar]
- 40.Suzuki S, Kawakami K, Nakamura F, Nishimura S, Yagi K, Seino M. Bromide, in the therapeutic concentration, enhances GABA-activated currents in cultured neurons of rat cerebral cortex. Epilepsy Res. 1994;19:89–97. doi: 10.1016/0920-1211(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 41.Gagnon KB, Adragna NC, Fyffe RE, Lauf PK. Characterization of glial cell K-Cl cotransport. Cell Physiol Biochem: Int J Exp Cell Physiol, Biochem, Pharmacol. 2007;20:121–30.. doi: 10.1159/000104160. [DOI] [PubMed] [Google Scholar]
- 42.Kinne R, Kinne-Saffran E, Scholermann B, Schutz H. The anion specificity of the sodium-potassium-chloride cotransporter in rabbit kidney outer medulla: studies on medullary plasma membranes. Pflug Arch: Eur J Physiol. 1986;407(Suppl 2):S168–73. doi: 10.1007/BF00584947. [DOI] [PubMed] [Google Scholar]
- 43.Becker JA, Clesse D, Spiegelhalter C, Schwab Y, Le Merrer J, Kieffer BL. Autistic-like syndrome in mu opioid receptor null mice is relieved by facilitated mGluR4 activity. Neuropsychopharmacology. 2014;39:2049–60.. doi: 10.1038/npp.2014.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jamot L, Matthes HW, Simonin F, Kieffer BL, Roder JC. Differential involvement of the mu and kappa opioid receptors in spatial learning. Genes Brain Behav. 2003;2:80–92. doi: 10.1034/j.1601-183X.2003.00013.x. [DOI] [PubMed] [Google Scholar]
- 45.Jung KM, Sepers M, Henstridge CM, Lassalle O, Neuhofer D, Martin H, et al. Uncoupling of the endocannabinoid signalling complex in a mouse model of fragile X syndrome. Nat Commun. 2012;3:1080. doi: 10.1038/ncomms2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Michalon A, Sidorov M, Ballard TM, Ozmen L, Spooren W, Wettstein JG, et al. Chronic pharmacological mGlu5 inhibition corrects fragile X in adult mice. Neuron. 2012;74:49–56. doi: 10.1016/j.neuron.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Peca J, Feliciano C, Ting JT, Wang W, Wells MF, Venkatraman TN, et al. Shank3 mutant mice display autistic-like behaviours and striatal dysfunction. Nature. 2011;472:437–42. doi: 10.1038/nature09965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matthes HW, Maldonado R, Simonin F, Valverde O, Slowe S, Kitchen I, et al. Loss of morphine-induced analgesia, reward effect and withdrawal symptoms in mice lacking the mu-opioid-receptor gene. Nature. 1996;383:819–23.. doi: 10.1038/383819a0. [DOI] [PubMed] [Google Scholar]
- 49.Mientjes EJ, Nieuwenhuizen I, Kirkpatrick L, Zu T, Hoogeveen-Westerveld M, Severijnen L, et al. The generation of a conditional Fmr1 knock out mouse model to study Fmrp function in vivo. Neurobiol Dis. 2006;21:549–55.. doi: 10.1016/j.nbd.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 50.Pujol CN, Pellissier LP, Clément C, Becker JAJ, Le Merrer J. Back-translating behavioral intervention for autism spectrum disorders to mice with blunted reward restores social abilities. Transl Psychiatry. 2018;8:197. doi: 10.1038/s41398-018-0247-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holmes GL, Tian C, Hernan AE, Flynn S, Camp D, Barry J. Alterations in sociability and functional brain connectivity caused by early-life seizures are prevented by bumetanide. Neurobiol Dis. 2015;77:204–19. doi: 10.1016/j.nbd.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Becker JAJ, Pellissier LP, Corde Y, Laboute T, Leaute A, Gandia J, et al. Facilitating mGluR4 activity reverses the long-term deleterious consequences of chronic morphine exposure in male mice. Neuropsychopharmacology. 2021;46:1373–85.. doi: 10.1038/s41386-020-00927-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tora AS, Rovira X, Dione I, Bertrand HO, Brabet I, De Koninck Y, et al. Allosteric modulation of metabotropic glutamate receptors by chloride ions. Faseb J. 2015;29:4174–88. [DOI] [PubMed]
- 54.Kuang D, Hampson DR. Ion dependence of ligand binding to metabotropic glutamate receptors. Biochem Biophys Res Commun. 2006;345:1–6. doi: 10.1016/j.bbrc.2006.04.064. [DOI] [PubMed] [Google Scholar]
- 55.Conklin BR, Farfel Z, Lustig KD, Julius D, Bourne HR. Substitution of three amino acids switches receptor specificity of Gq alpha to that of Gi alpha. Nature. 1993;363:274–6. doi: 10.1038/363274a0. [DOI] [PubMed] [Google Scholar]
- 56.Goldstein DB. Sodium bromide and sodium valproate: effective suppressants of ethanol withdrawal reactions in mice. J Pharm Exp Ther. 1979;208:223–7. [PubMed] [Google Scholar]
- 57.Hayashi K, Ueshima S, Ouchida M, Mashimo T, Nishiki T, Sendo T, et al. Therapy for hyperthermia-induced seizures in Scn1a mutant rats. Epilepsia. 2011;52:1010–7. doi: 10.1111/j.1528-1167.2011.03046.x. [DOI] [PubMed] [Google Scholar]
- 58.Charalambous M, Shivapour SK, Brodbelt DC, Volk HA. Antiepileptic drugs’ tolerability and safety-a systematic review and meta-analysis of adverse effects in dogs. BMC Vet Res. 2016;12:79. doi: 10.1186/s12917-016-0703-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Trepanier LA, Babish JG. Pharmacokinetic properties of bromide in dogs after the intravenous and oral administration of single doses. Res Vet Sci. 1995;58:248–51. doi: 10.1016/0034-5288(95)90111-6. [DOI] [PubMed] [Google Scholar]
- 60.Steinhoff BJ, Kruse R. Bromide treatment of pharmaco-resistant epilepsies with generalized tonic-clonic seizures: a clinical study. Brain Dev. 1992;14:144–9. doi: 10.1016/S0387-7604(12)80253-1. [DOI] [PubMed] [Google Scholar]
- 61.Vidaurre J, Gedela S, Yarosz S. Antiepileptic drugs and liver disease. Pediatr Neurol. 2017;77:23–36. doi: 10.1016/j.pediatrneurol.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 62.Pavelka S, Babicky A, Vobecky M, Lener J, Svandova E. Bromide kinetics and distribution in the rat. I. Biokinetics of 82Br-bromide. Biol trace Elem Res. 2000;76:57–66. doi: 10.1385/BTER:76:1:57. [DOI] [PubMed] [Google Scholar]
- 63.Rauws AG. Pharmacokinetics of bromide ion-an overview. Food Chem Toxicol: Int J published Br Ind Biol Res Assoc. 1983;21:379–82.. doi: 10.1016/0278-6915(83)90091-1. [DOI] [PubMed] [Google Scholar]
- 64.Vaiseman N, Koren G, Pencharz P. Pharmacokinetics of oral and intravenous bromide in normal volunteers. J Toxicol Clin Toxicol. 1986;24:403–13.. doi: 10.3109/15563658608992603. [DOI] [PubMed] [Google Scholar]
- 65.Sprengers JJ, van Andel DM, Zuithoff NPA, Keijzer-Veen MG, Schulp AJA, Scheepers FE, et al. Bumetanide for Core Symptoms of Autism Spectrum Disorder (BAMBI): A single center, double-blinded, participant-randomized, placebo-controlled, Phase-2 superiority trial. J Am Acad Child Adolesc Psychiatry. 2020;S0890-8567:31290–9. doi: 10.1016/j.jaac.2020.07.888. [DOI] [PubMed] [Google Scholar]
- 66.Hays SA, Huber KM, Gibson JR. Altered neocortical rhythmic activity states in Fmr1 KO mice are due to enhanced mGluR5 signaling and involve changes in excitatory circuitry. J Neurosci. 2011;31:14223–34. doi: 10.1523/JNEUROSCI.3157-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bear MF, Huber KM, Warren ST. The mGluR theory of fragile X mental retardation. Trends Neurosci. 2004;27:370–7. doi: 10.1016/j.tins.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 68.Yoo T, Cho H, Lee J, Park H, Yoo YE, Yang E, et al. GABA neuronal deletion of Shank3 Exons 14-16 in mice suppresses striatal excitatory synaptic input and induces social and locomotor abnormalities. Front Cell Neurosci. 2018;12:341. doi: 10.3389/fncel.2018.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bozdagi O, Sakurai T, Papapetrou D, Wang X, Dickstein DL, Takahashi N, et al. Haploinsufficiency of the autism-associated Shank3 gene leads to deficits in synaptic function, social interaction, and social communication. Mol Autism. 2010;1:15. doi: 10.1186/2040-2392-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yang M, Bozdagi O, Scattoni ML, Wohr M, Roullet FI, Katz AM, et al. Reduced excitatory neurotransmission and mild autism-relevant phenotypes in adolescent Shank3 null mutant mice. J Neurosci. 2012;32:6525–41. doi: 10.1523/JNEUROSCI.6107-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jaramillo TC, Speed HE, Xuan Z, Reimers JM, Escamilla CO, Weaver TP, et al. Novel Shank3 mutant exhibits behaviors with face validity for autism and altered striatal and hippocampal function. Autism Res. 2017;10:42–65. doi: 10.1002/aur.1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Paluszkiewicz SM, Martin BS, Huntsman MM. Fragile X syndrome: The GABAergic system and circuit dysfunction. Dev Neurosci. 2011;33:349–64. doi: 10.1159/000329420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Van der Aa N, Kooy RF. GABAergic abnormalities in the fragile X syndrome. Eur J Paediatr Neurol. 2020;24:100–04. doi: 10.1016/j.ejpn.2019.12.022. [DOI] [PubMed] [Google Scholar]
- 74.Centonze D, Rossi S, Mercaldo V, Napoli I, Ciotti MT, De Chiara V, et al. Abnormal striatal GABA transmission in the mouse model for the fragile X syndrome. Biol Psychiatry. 2008;63:963–73. doi: 10.1016/j.biopsych.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 75.Wang W, Li C, Chen Q, van der Goes MS, Hawrot J, Yao AY, et al. Striatopallidal dysfunction underlies repetitive behavior in Shank3-deficient model of autism. J Clin Invest. 2017;127:1978–90.. doi: 10.1172/JCI87997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Niswender CM, Johnson KA, Weaver CD, Jones CK, Xiang Z, Luo Q, et al. Discovery, characterization, and antiparkinsonian effect of novel positive allosteric modulators of metabotropic glutamate receptor 4. Mol Pharmacol. 2008;74:1345–58. doi: 10.1124/mol.108.049551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sala-Rabanal M, Yurtsever Z, Nichols CG, Brett TJ. Secreted CLCA1 modulates TMEM16A to activate Ca(2+)-dependent chloride currents in human cells. eLife. 2015;4:e05875. doi: 10.7554/eLife.05875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Seo KH, Jin Y, Jung SY, Lee SH. Comprehensive behavioral analyses of anoctamin1/TMEM16A-conditional knockout mice. Life Sci. 2018;207:323–31.. doi: 10.1016/j.lfs.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 79.Tang X, Kim J, Zhou L, Wengert E, Zhang L, Wu Z, et al. KCC2 rescues functional deficits in human neurons derived from patients with Rett syndrome. Proc Natl Acad Sci USA. 2016;113:751–6. doi: 10.1073/pnas.1524013113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Doyon N, Vinay L, Prescott SA, De, Koninck Y. Chloride regulation: A dynamic equilibrium crucial for synaptic inhibition. Neuron. 2016;89:1157–72.. doi: 10.1016/j.neuron.2016.02.030. [DOI] [PubMed] [Google Scholar]
- 81.Meierkord H, Grunig F, Gutschmidt U, Gutierrez R, Pfeiffer M, Draguhn A, et al. Sodium bromide: Effects on different patterns of epileptiform activity, extracellular pH changes and GABAergic inhibition. Naunyn-Schmiedeberg’s Arch Pharmacol. 2000;361:25–32. doi: 10.1007/s002109900162. [DOI] [PubMed] [Google Scholar]
- 82.Dolen G, Darvishzadeh A, Huang KW, Malenka RC. Social reward requires coordinated activity of nucleus accumbens oxytocin and serotonin. Nature. 2013;501:179–84.. doi: 10.1038/nature12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gigliucci V, Leonzino M, Busnelli M, Luchetti A, Palladino VS, D’Amato FR, et al. Region specific up-regulation of oxytocin receptors in the opioid oprm1 (−/−) mouse model of autism. Front Pediatr. 2014;2:91. doi: 10.3389/fped.2014.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dunn HA, Zucca S, Dao M, Orlandi C, Martemyanov KA. ELFN2 is a postsynaptic cell adhesion molecule with essential roles in controlling group III mGluRs in the brain and neuropsychiatric behavior. Mol Psychiatry. 2019;24:1902–19.. doi: 10.1038/s41380-019-0512-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Argyropoulos A, Gilby KL, Hill-Yardin EL. Studying autism in rodent models: Reconciling endophenotypes with comorbidities. Front Hum Neurosci. 2013;7:417. doi: 10.3389/fnhum.2013.00417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Silverman JL, Yang M, Lord C, Crawley JN. Behavioural phenotyping assays for mouse models of autism. Nat Rev Neurosci. 2010;11:490–502. doi: 10.1038/nrn2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hadders-Algra M. Early diagnostics and early intervention in neurodevelopmental disorders-age-dependent challenges and opportunities. J Clin Med. 2021;10:861. doi: 10.3390/jcm10040861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Smith T, Klorman R, Mruzek DW. Predicting outcome of community-based early intensive behavioral intervention for children with autism. J Abnorm Child Psychol. 2015;43:1271–82.. doi: 10.1007/s10802-015-0002-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data that support the findings of this study are available from the corresponding author upon request.