Abstract
Background
Femoral shaft fracture in patients of post-polio syndrome (PPS) represents an uncommon yet complex injury pattern. Poorly developed soft-tissue envelope, decreased muscle bulk, reduced vascularity, regional osteopenia, joint contractures, and altered bony anatomy impose significant surgical challenges. Thorough pre-operative planning is imperative as each case requires individualized approach and method of fixation. The aim of the study was to analyze the clinical outcomes in such patients following fracture fixation and to assess the surgical challenges encountered and provide solutions.
Materials and Methods
A retrospective case series of 33 patients with femoral shaft fracture in PPS limbs was undertaken. Mode of injury, method of fixation, surgical time, intra-operative blood loss, union time, and complications were recorded.
Results
Low-energy fall was the most common mechanism of injury (73%). Thirty-three patients underwent fixation with intramedullary nailing being the most common mode (79%). Femoral canal diameter, femoral bow, fracture location and morphology and clinical deformities of the patients are key governing factors that determine the choice of implant. Locking plates, pre-contoured anatomical plates, and titanium elastic nailing system offer an alternative in patients unsuitable for nailing. With no difference between various implants, average time for bone healing was 13.8 ± 4.4 weeks. All patients resumed full weight-bearing mobilization and returned to pre-injury activity status at the end of 6 months post-surgery.
Conclusion
With detailed pre-operative work-up, contemplating intra-operative difficulties, individualized surgical plan, careful handling of soft tissues, and availability of back-up implants, good clinical outcomes can be achieved in femur fractures in PPS patients.
Keywords: Post-polio syndrome, Femur shaft fracture, PPS, Intramedullary nailing
Introduction
Poliomyelitis is a viral disease primarily affecting the central nervous system and results in asymmetrical flaccid paralysis [1]. The sustained vaccination efforts by the WHO [2] have led to near eradication of the disease over the past few decades, the neuro-muscular sequelae of the illness still contribute to a major health care burden, especially in the developing countries. Polio virus predominantly affects the anterior horn cells [3] and leads to poor development of musculo-skeletal system ensuing weakness, wasting, and deformation of the affected limb. Post-polio syndrome as defined by the March of Dimes criteria is encompassed by muscular atrophy, gait disturbances, osteopenia, bony deformities, reduced joint stability, mobility and contractures, and functional disability affecting the activities of daily living. All these predispose to an increased tendency to fall and subsequently to sustain a fracture [4, 5].
Lean and thin limb along with deformed bones and joint contractures poses a technical challenge for the surgeons for operative intervention. Primarily, long bones are affected among which femur is commonly involved. Due to ill developed surrounding muscles and soft tissues, the bones develop regional osteoporosis [4, 6]. Osteoporosis combined with an increased tendency to fall and neuro-muscular imbalance multiply the chances to sustain a femur fracture despite trauma being trivial [7]. In patients with PPS, femoral morphology is usually altered begetting in a complex and uncommon pattern of fracture [8]. Although fracture can occur anywhere in PPS limb but low-energy proximal and distal shaft femur fractures are more common [9]. Thorough clinical evaluation and detailed pre-operative planning is imperative for operative management of such fractures. This retrospective case series was undertaken to evaluate (a) various technical challenges witnessed during surgical fixation, (b) functional and radiological outcomes following fixation, and (c) if any special requirements are to be considered while managing femoral fractures in PPS limbs.
Materials and Methods
After prior approval from Institutional Ethics Committee, the data of patients admitted for femoral fractures in PPS limbs between January, 2016 and December, 2019 with a minimum follow-up of 6 months was retrospectively reviewed from hospital records. All the patients were managed in a level I trauma center by an experienced orthopedic trauma team.
All cases who fulfilled these inclusion criteria of (1) age between 18 and 60 years, (2) femoral shaft fractures, and (3) fractures presenting to the emergency department within 48 h of injury were included for review while patients with (1) polytrauma, (2) traumatic brain injury, (3) > grade III open (Gustilo Anderson classification) fracture, (4) history of chronic smoking or alcohol intake, (5) pre-injury immunocompromised status, (6) femur fractures involving neck, intertrochanteric region, and intraarticular distal femur, and (7) those unfit for surgery were excluded from the study. Demographic data were recorded as per the standard norms and the comorbidities of the patient along with the associated injuries, past surgical history, mechanism of trauma, and pre-trauma mobility status including ability to sit cross legged, squat before injury, and whether walking aid was used prior to injury were documented.
Clinical examination was conducted to rule out other causes of limb weakness and assess deformities of hip and knee, comparative muscle bulk of the affected limb, motor power, and sensory status. Knee range of motion was checked under anesthesia prior to surgery.
X-rays of hip with thigh with knee (AP and Lat. views) of the affected limb were done to identify and classify the fracture. Pelvic anatomy, morphology of greater trochanter, and femoral bowing were noticed for any abnormal deviation from normal affecting the surgical plan. Femoral canal diameter was measured at the level of isthmus, and femur length was analyzed using the distance measuring tool of a picture archiving and communication system (PACS).
As per records, all patients were operated under regional anesthesia within 24 h after arrival in hospital. Retrograde intramedullary nailing (RIMN) with distal femoral nail (DFN) was done in supine position on a radiolucent table, while fixation with proximal femoral nail (PFN), plating, antegrade femoral nail (AFN), and titanium elastic nailing system (TENS) was done on fracture table. In all cases, adequacy of reduction and implant placement was confirmed under image intensifier. Surgical duration, blood loss, and any intra-operative difficulties encountered were noted from case records.
Single dose of intravenous antibiotic (Cefuroxime, 1.5 g) was given perioperatively as per the departmental protocol. Post-skeletal fixation, all patients received DVT prophylaxis and 1 dose of intravenous (Cefuroxime, 1.5 g) antibiotic. Routine analgesics were given as per requirement. Knee ROM exercises and toe-touch weight-bearing mobilization with walker was allowed on post-operative day 1 in all cases as per records. Post-operatively, radiographs (AP and lateral) were taken at day 0, 6 weeks, 12 weeks, and 6 months post-surgery. Full weight-bearing mobilization was permitted after clinical and radiographic evidence of union. The choice of implant, time to fracture union, and complications were noted and analyzed.
Results
A total of 33 patients comprising 26 males and 7 females with mean age of 34.7 ± 8.7 years (mean ± SD) years were included in the study (Table 1). Among 33 patients, 8 sustained subtrochanteric fractures, 10 distal femur fractures, and 15 endured mid-shaft femur fractures. Fall during activities of daily living was the most common injury mechanism (in 24 patients) seconded by high-energy trauma (RTA/ fall from > 10 feet height) in 9 patients. All patients had fixed flexion deformity (FFD) in knee preoperatively with mean range of motion (ROM) of 72 ± 11.9° and median FFD of 22.5°. No significant comorbidities were detected in any of the patients except type II diabetes in two patients and controlled hypertension in four patients.
Table 1.
Demographic details of patients and fracture characteristics
| S no. | Age | Sex | Fracture location | Canal diameter (mm) | Implant used | Union time (weeks) |
|---|---|---|---|---|---|---|
| 1 | 32 | M | Subtrochanteric | 9 | PFN | 12 |
| 2 | 21 | M | Shaft femur | 10 | AFN | 12 |
| 3 | 24 | M | Shaft femur | 10 | AFN | 12 |
| 4 | 25 | F | Shaft femur | 6 | Plating-LCP | 12 |
| 5 | 27 | M | Distal femur | 9 | DFN | 12 |
| 6 | 35 | M | Subtrochanteric | 11 | PFN | 12 |
| 7 | 46 | F | Distal femur | 9 | DFN | 12 |
| 8 | 28 | M | Shaft femur | 8 | Plating: LCP | 25 |
| 9 | 41 | M | Shaft femur | 9 | AFN | 12 |
| 10 | 40 | M | Subtrochanteric | 10 | PFN | 12 |
| 11 | 37 | M | Subtrochanteric | 9 | PFN | 24 |
| 12 | 33 | M | Shaft femur | 11 | AFN | 12 |
| 13 | 47 | F | Shaft femur | 8 | Plating: LCP | 12 |
| 14 | 28 | M | Distal femur | 10 | DFN | 12 |
| 15 | 36 | F | Shaft femur | 10 | AFN | 12 |
| 16 | 30 | F | Shaft femur | 9 | AFN | 24 |
| 17 | 43 | M | Shaft femur | 10 | AFN | 12 |
| 18 | 36 | M | Subtrochanteric | 7 | Plating-reverse DFLP | 12 |
| 19 | 32 | M | Distal femur | 19 | DFN | 12 |
| 20 | 30 | M | Shaft femur | 7 | TENS | 12 |
| 21 | 46 | M | Subtrochanteric | 10 | PFN | 12 |
| 22 | 21 | M | Distal femur | 9 | DFN | 12 |
| 23 | 51 | M | Shaft femur | 10 | AFN | 24 |
| 24 | 28 | M | Subtrochanteric | 9 | PFN | 12 |
| 25 | 34 | M | Distal femur | 11 | DFN | 12 |
| 26 | 39 | M | Shaft femur | 9 | AFN | 12 |
| 27 | 41 | M | Distal femur | 9 | Plating- DFLP | 24 |
| 28 | 30 | F | Shaft femur | 9 | AFN | 12 |
| 29 | 22 | M | Distal femur | 9 | DFN | 12 |
| 30 | 50 | M | Shaft femur | 10 | AFN | 12 |
| 31 | 37 | M | Distal femur | 9 | DFN | 12 |
| 32 | 53 | F | Distal femur | 9 | Plating-DFLP | 12 |
| 33 | 25 | M | Subtrochanteric | 11 | PFN | 12 |
DFN distal femoral nail, AFN antegrade femoral nailing, PFN proximal femoral nail, DFLP distal femur locking plate, LCP locking compression plate, TENS titanium elastic nailing system
Mean interval from injury to hospital presentation was 26.3 h, while average time to surgery was 15.6 ± 3.4 h. The mean duration of surgery was 87.45 ± 21.89 min and the average blood loss was 106.36 ± 25.99 ml. Average canal diameter measured preoperatively was 9.54 ± 2.04 mm. Closed reduction and intramedullary nailing was the preferred mode of fixation wherein 11 patients were managed with AFN (Fig. 1), 7 with PFN and 8 with DFN (Fig. 2) governed by the anatomic location of the fracture. Open reduction and internal fixation (ORIF) with locked compression plating (LCP) was employed in two patients due to excessive femoral bow (not amenable to nailing), while two patients underwent plating in view of narrow femoral canal (canal diameter < 9 mm). Additionally, TENS nailing was done in one patient due to narrow femoral canal. ORIF with distal femoral locking plate (DFLP) was done in two patients due to pre-operative FFD in knee precluding RIMN.
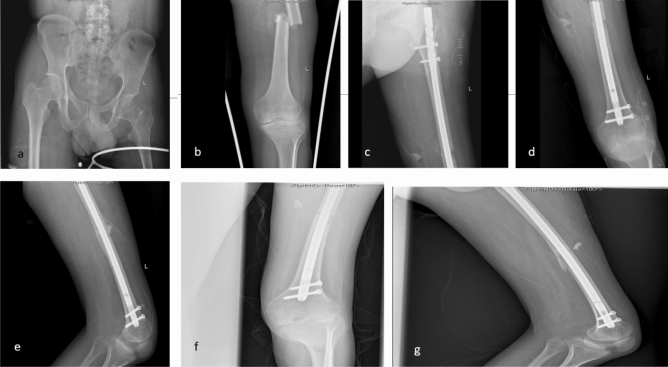
Fig. 1.
30-Year-old male suffered fall from > 15 feet height. a, b Pre-op radiograph demonstrates mid-shaft femur fracture. CRIF with AFN was done. c–e Immediate post-op radiographs depicting anatomic reduction and satisfactory implant placement. f, g 3-Month post-op X-ray depicts bony union
Fig. 2.
53-year-old female suffered fall from standing height and sustained a a–c right distal femoral shaft fracture. CRIF with DFN was done. d–f Post-op 6 month X-rays demonstrate complete bony union. Diffuse regional osteoporosis in femoral bone compared to healthy side
Mean duration of hospital stay was 3.66 ± 1.03 days. 1 patient, managed with ORIF and plating developed persistent discharge from surgical wound which was managed successfully with a course of suppressive antibiotic for 2 weeks. Average period for radiographic union was 13.8 ± 4.4 weeks. All patients achieved pre-operative knee ROM and mobility at 6 month follow-up. At final follow-up, all the patients had bony union with no evidence of any complications including non-union, mal-union, screw-cutout, implant failure, infection, or any neurovascular injury.
Discussion
Polio, a neurotropic virus, damages the anterior horn cells of spinal cord and results in flaccid paralysis of muscles supplied by the affected neurons [10] leading to widespread muscular atrophy. Over a period of time, this progresses to post-polio syndrome (PPS), which causes further weakness of the limbs despite collaterals being formed [11]. This leads to progressive muscle weakness, joint malalignment, and skeletal deformities which brings about severe handicap in activities of daily living.
Poliotic fractures encompass a rare injury pattern as poliomyelitis has been virtually eradicated from most of the countries, but as polio survivors are aging, number of people with residual PPS is on the rise [12]. 28–38% of patients with PPS are estimated to suffer from a fracture during their lifetime [5], while this increases to 48% after 40 years of age [6]. These fractures occur generally due to low-energy trauma in course of day-to-day activities because of higher incidence of fall [13] and osteoporotic bone, primarily a result of disuse atrophy [4]. Factors associated with recurrent fall include preponderance of lower limb affliction, quadriceps weakness, increased fear of falling, and frequent complaints of difficulty in maintaining balance. Also, the tendency or fear of fall increases with each successive fall and the incidence approaches as high as 79–82% over 5 years [5, 6, 14, 15]. Low-energy fall was the most common mode of injury in our case series (73%), paralleled by other studies too [13, 14]. Males are more frequently afflicted than females probably because poliomyelitis has a prevailing rate more in males compared to females.
Major impediments to surgical management of fractures in PPS bones are deformity and osteopenia. Only 4% of patients with PPS encounter normal bone mineral density [6]. While the remaining routinely develop osteoporosis, it is more pronounced in the poliotic limb compared to the healthy limb increasing the predilection to sustain a fracture [6]. Deformity of the bones results due to imbalanced muscle forces across bone. Non-paralyzed muscles exert increased muscular forces toward them compared to their counterpart paralyzed muscle groups precipitating abnormal bowing of bones. Imbalance in muscle forces also leads to joint laxity and subluxation emanating to joint contracture and decreased range of motion. Disuse atrophy, osteoporosis, and joint contractures combine to cause resultant wasting of the affected limb and subsequently loss of subcutaneous fat and thinning of skin.
Shaft femur fracture almost always require surgical fixation of the fractured bone and pre-operative planning forms the cornerstone, more so in cases with PPS. Pre-operative planning includes detailed history as well as clinical examination and radiological work-up. It is necessary to look for deformities of hip, knee and ankle as they can impose challenges in patient positioning and thus alter the management plan. Radiographic evaluation includes measurement of femoral canal diameter, assessment of femoral bow, greater trochanter, and neck geometry including version and length. Although intramedullary nailing is the gold standard fixation method for shaft femur fractures, but in cases with PPS, aforementioned factors dictate the choice of implant. Deformed greater trochanter can cause difficulty in identifying entry point for AFN. Varus or valgus neck causes eccentric lag screw placement in the femoral head. However, in our series, no case had deformed trochanter or excessive varus or valgus neck. To counter excessive bending of femur, an anterior entry point was preferred. In two patients with fractures in distal one-third of shaft femur amenable to AFN, DFN was chosen due to presence of hip and knee deformities precluding positioning over a fracture table or antegrade nailing in lateral position. Narrow femoral canal is another important parameter that needs to be measured preoperatively as it is encountered frequently and forbids intramedullary nailing with standard available implants. Authors set 9 mm canal diameter as the threshold precluding nailing. While one patient with mid-shaft fracture and narrow canal was managed with 4.5 mm narrow LCP, another patient with a subtrochanteric fracture received opposite side reversed DFLP (Fig. 3). Proximal femoral locking plate was attempted for the same patient but, broad profile and fixed direction of locking screws incoherent with the deformed femoral neck estopped its placement and opposite side DFLP was preferred. Long DHS as well as DCS have also been attempted successfully in management of such fractures as reported previously [16, 17], but they could also not be employed due to altered neck-shaft angle prohibiting their placement. One patient with 7 mm canal diameter and excessive femoral bow was managed with TENS as standard LCP could not be used intraoperatively. This prompted the authors to search for bent plates and in another two successive patients, pre-contoured ‘banana shaped’ LCP was used to accommodate for excessive femoral bow. This emphasizes the fact that additional back-up implants should always be kept ready while operating upon such fractures. Another peculiar issue faced in three patients was short femoral length of 300 mm. Standard antegrade femoral nails are usually available from size 320 mm and above. Authors had to cut the standard nail using a high-speed burr and a jumbo cutter through the distal most locking hole to address this problem (Fig. 4). Besides, short-length one patient also had excessive femoral bow, and thus, authors bent the AFN using a bench press bender to accommodate for the same (Fig. 5).
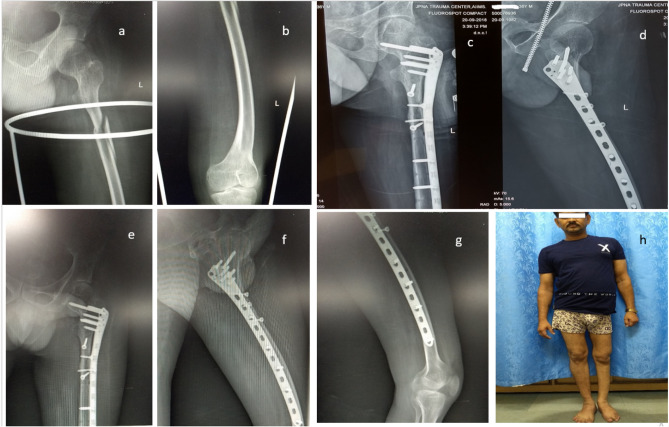
Fig. 3.
36-Year-old male suffered from RTA. a, b Pre-op radiograph demonstrates subtrochanteric femoral fracture. ORIF with opposite side reverse DFLP done due to narrow femoral canal diameter. c, d 3-Month post-op X-ray depicts union; e–g follow-up 6-month X-rays demonstrating complete bony union. h Clinical photograph depicting resumption of full weight-bearing mobilization
Fig. 4.

Antegrade femoral nail cut from distal dynamic locking hole to achieve the length of 300 mm
Fig. 5.
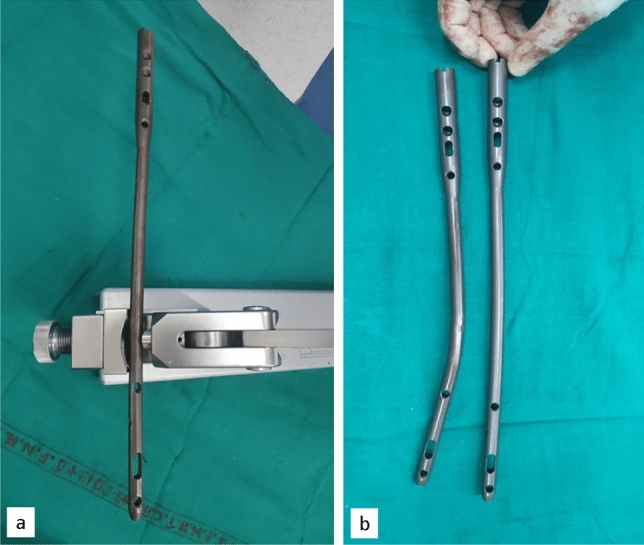
a Antegrade femoral nail bent using a bench press bender. b Note the difference in sagittal profile of the bent nail compared to the standard available femoral nail
Back-up implants including 3.5 and 4.5 mm LCPs, TENS must always be kept ready to treat poliotic femoral shaft fracture as affected bone usually has narrow profile, altered anatomy, and thin cortices. In an attempt to address these issues, various studies have demonstrated bankable results with several different implants. They include standard custom-made interlocking nails, tibial nail, humerus nail, adolescent nail, and LCP. Choice of implant depends upon diameter of femoral canal as well as expertise of operating surgeon. Park et al. [18] used humerus nail for fixing femoral shaft fractures. They used 6.7 mm- and 7.5 mm-diameter nail and bent it proximally by 5° to match the greater trochanter curvature; however, they did not bend it distally and reaming was not done. Expert tibia nail has also been used effectively for subtrochanteric femoral fracture with narrow canal [19]. We propound that standard femoral nail should only be used in cases with normal size of canal (> 9 mm) while being cautious about overzealous reaming of the canal and forceful hammering to insert the nail as this can lead to shattering of femur in the backdrop of regional osteopenia. Also, whenever possible, authors advocate additional reaming of the femoral canal by 0.5–1 mm over and above that described for standard nailing and/or using an undersized diameter nail. This helps to accommodate for increased femoral bow while avoiding forceful insertion. Adolescent femoral nail is a good choice in some of these cases as both nail length and diameter are available in suitable sizes, but were not employed in the series due to unavailability of the same. Fixation with locking plates has been frequently demonstrated to report favorable outcomes [9, 20], but these are also not free of complications. Application of plate leads to opening of fracture site, stripping of healthy periosteum as well as increased chances of infection. This may lead to increased chances of non-union or delayed union, especially taking into consideration the already compromised blood supply, poorly developed soft-tissue envelope, and osteoporotic nature of the affected bone in poliotic limbs. Careful soft-tissue handling, employing minimally invasive techniques for screw insertion and limited stripping of periosteum, is advised to minimize soft-tissue trauma and thereby to promote early healing [21]. Distal femoral fracture fixation was a bit tricky because of deformed geometry and stiffness of affected knee joint. It was difficult to identify the precise nail entry point. We used image intensifier and rotated affected limb in various directions to get true AP and lateral view to identify femoral inter-condylar sulcus [22]. Blocking screws have been described to aid reduction [23] as well as achieve good alignment and were employed in one of our case.
Average duration for radiographic union in poliotic femoral fracture is more as compared to normal femoral fractures. This stems from regional osteoporosis, compromised soft-tissue coverage, low vascularity, and low activity of osteoblasts. However, we registered that bone union progressed normally in all the patients with mean duration of 13.8 weeks and 85% uniting within 3 months without any increased complication rate as compared to 16 weeks reported in the other studies [9, 24]. Also, it was noted that bones united with minimal callus formation despite polio being a neuro-muscular disease [21]. Fractures in our study united earlier, probably because closed reduction and nailing was preferred in most of our cases (79%) as opposed to open reduction.
The aim of surgical management is not merely to achieve bony union, rather promote early mobilization and rehabilitation to prevent joint contractures and further muscle atrophy. Functional outcome was measured in terms of post-operative ambulation, knee range of motion achieved, use of walking aids, and restoration to occupation before trauma. All of our patients achieved good functional outcome at the end of 6 months wherein all reported return to pre-injury status. Knee ROM and ambulatory status was also comparable to pre-operative status [9, 20, 24].
Our study had certain limitations: (a) sample size comprised merely 33 patients and several types of implants were used, forbidding us to compare bone healing among various implants, and (b) bone mineral density (BMD) was not evaluated in our series as patients had fractured limbs and density values post implant fixation cannot be corroborated. Measurement of BMD could have aided in initiation of pharmacological agents (bisphosphonates) post-fixation that are reported to decrease risk of subsequent fractures in PPS patients [25].
Conclusion
Although rare, femoral fractures in PPS patients are not an uncommon case scenario, especially in developing countries. Altered anatomy, compromised soft-tissue coverage and joint contractures impose significant challenge for surgical fixation. Meticulous pre-operative work-up including clinical assessment as well as radiological evaluation to foresee possible intra-operative challenges forms the cornerstone of surgical management. Intramedullary nailing is the gold standard method for fixation; however, implant choice as well as method of fixation should be individualized on a case-to-case basis and additional back-up implants must always be kept available in operating room. With careful handling of soft tissue, maintenance of the fracture biology, and adherence to orthopedic principles, successful bone healing with good functional outcome can be achieved even in PPS limbs.
Declarations
Conflict of Interest
The authors (Suman Saurabh, Anupam Gupta, Tanya Trikha, Aashraya Karpe, and Samarth Mittal) declare that they have no conflict of interests. Authors also declare that no funding has been received from any source.
Ethical approval
All procedures performed in study were in accordance with the ethical standards of the institutional guidelines and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants involved in the study.
Footnotes
The original online version of this article was revised: It was erroneously stated in the Introduction that “Poliovirus predominantly affects the dorsal root ganglion …”.
The correct statement is: “Poliovirus predominantly affects the anterior horn cells …” [3].
References
3. Tiffreau V, Rapin A, Serafi R, Percebois-Macadré L, Supper C, Jolly D, Boyer FC. Post-polio syndrome and rehabilitation. Ann Phys Rehabil Med. 2010 Feb;53(1):42-50. doi: 10.1016/j.rehab.2009.11.007. Epub 2009 Dec 30. PMID: 20044320.
The original article has been corrected.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
11/29/2022
A Correction to this paper has been published: 10.1007/s43465-022-00764-8
References
- 1.Trojan DA, Cashman NR. Post-poliomyelitis syndrome. Muscle and Nerve. 2005;31(1):6–19. doi: 10.1002/mus.20259. [DOI] [PubMed] [Google Scholar]
- 2.Poliomyelitis (polio) [Internet]. [cited 2021 Jun 26]. https://www.who.int/westernpacific/health-topics/poliomyelitis. Accessed 26 June 2021
- 3.Tiffreau V, Rapin A, Serafi R, Percebois-Macadré L, Supper C, Jolly D, Boyer FC. Post-polio syndrome and rehabilitation. Annals of Physical and Rehabilitation Medicine. 2010;53(1):42–50. doi: 10.1016/j.rehab.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Haziza M, Kremer R, Benedetti A, Trojan DA. Osteoporosis in a postpolio clinic population. Archives of Physical Medicine and Rehabilitation. 2007;88(8):1030–1035. doi: 10.1016/j.apmr.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Silver JK, Aiello DD. Polio survivors: Falls and subsequent injuries. American Journal of Physical Medicine and Rehabilitation. 2002;81(8):567–570. doi: 10.1097/00002060-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Mohammad AF, Khan KA, Galvin L, Hardiman O, O’Connell PG. High incidence of osteoporosis and fractures in an aging post-polio population. European Neurology. 2009;62(6):369–374. doi: 10.1159/000242444. [DOI] [PubMed] [Google Scholar]
- 7.Goerss JB, Atkinson EJ, Windebank AJ, O’Fallon WM, Melton LJ. Fractures in an aging population of poliomyelitis survivors: A community-based study in Olmsted County. Minnesota. Mayo Clin Proc. 1994;69(4):333–339. doi: 10.1016/S0025-6196(12)62217-4. [DOI] [PubMed] [Google Scholar]
- 8.Mingo-Robinet J, Alonso JA, Moreno-Barrero M, González-García L, Garcia-Virto V, Aguado HJ. Aspectos técnicos y complicaciones en el tratamiento de las fracturas de los miembros inferiores con secuelas de poliomielitis. Rev Esp Cir Ortopédica Traumatol. 2018;62(4):257–266. doi: 10.1016/j.recot.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Wang W, Shi H, Chen D, Chen Y, Wang J, Wang S, et al. Distal femoral fractures in post-poliomyelitis patients treated with locking compression plates. Orthopaedic Surgery. 2013;5(2):118–123. doi: 10.1111/os.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehndiratta MM, Mehndiratta P, Pande R. Poliomyelitis. The Neurohospitalist. 2014;4(4):223–229. doi: 10.1177/1941874414533352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonzalez H, Khademi M, Borg K, Olsson T. Intravenous immunoglobulin treatment of the post-polio syndrome: Sustained effects on quality of life variables and cytokine expression after one year follow up. Journal of Neuroinflammation. 2012;9(9):167. doi: 10.1186/1742-2094-9-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gellman YN, Khoury A, Liebergall M, Mosheiff R, Weil YA. Outcome of femoral fractures in poliomyelitis patients. International Orthopaedics. 2019;43(11):2607–2612. doi: 10.1007/s00264-019-04285-2. [DOI] [PubMed] [Google Scholar]
- 13.Hill KD, Stinson AT. A pilot study of falls, fear of falling, activity levels and fall prevention actions in older people with polio. Aging Clinical and Experimental Research. 2004;16(2):126–131. doi: 10.1007/BF03324541. [DOI] [PubMed] [Google Scholar]
- 14.Bickerstaffe A, Beelen A, Nollet F. Circumstances and consequences of falls in polio survivors. Journal of Rehabilitation Medicine. 2010;42(10):908–915. doi: 10.2340/16501977-0620. [DOI] [PubMed] [Google Scholar]
- 15.Brogårdh C, Lexell J. Falls, fear of falling, self-reported impairments, and walking limitations in persons with late effects of polio. PM & R: The Journal of Injury, Function, and Rehabilitation. 2014;6(10):900–907. doi: 10.1016/j.pmrj.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Khallaf FGM, Al-Rowaih A, Abdul-Hamid HF. Results of subtrochanteric fractures treated with dynamic hip screw and dynamic condylar screw. Medical Principles and Practice. 1998;7(4):283–291. doi: 10.1159/000026056. [DOI] [Google Scholar]
- 17.Çevik HB. Management of femoral fractures in aging adult polio population: A retrospective review of 13 cases. South Clin Istanb Eurasia [Internet]. 2020 [cited 2021 Jul 6]. http://www.scie.online/jvi.aspx?un=SCIE-95967. Accessed 21 Aug 2019
- 18.Park H, Kim HW. Treatment of femoral shaft fracture with an interlocking humeral nail in older children and adolescents. Yonsei Medical Journal. 2012;53(2):408–415. doi: 10.3349/ymj.2012.53.2.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee, K.J., Min, B.W., Jung, J.H., Kang, M.K., Kim, M.J. (2015) Expert tibia nail for subtrochanteric femoral fracture to prevent thermal injury. International Journal of Surgery Case Reports, 10, 158–61. [DOI] [PMC free article] [PubMed]
- 20.El-Sayed KA. Locked plating for femoral fractures in polio patients. Archives of Orthopaedic and Trauma Surgery. 2010;130(10):1299–1304. doi: 10.1007/s00402-010-1126-z. [DOI] [PubMed] [Google Scholar]
- 21.Gupta M, Jain VK, Upadhyaya GK, Arya RK. Comprehensive review of challenges associated with management of lower limb fractures in poliomyelitis patients. Journal of Clinical Orthopaedics and Trauma. 2016;7(4):276–281. doi: 10.1016/j.jcot.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krupp RJ, Malkani AL, Goodin RA, Voor MJ. Optimal entry point for retrograde femoral nailing. Journal of Orthopaedic Trauma. 2003;17(2):100–105. doi: 10.1097/00005131-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Pettett BJ, Avery MC, Ostrum RF. Retrograde femoral nailing using percutaneous reduction techniques. Journal of Orthopaedic Trauma. 2017;31:S6. doi: 10.1097/BOT.0000000000000890. [DOI] [PubMed] [Google Scholar]
- 24.Assessment of bone geometry and its considerations in implant selection for polio affected femoral fractures: An outcome analysis [Internet]. ResearchGate. [cited 2019 Jan 19]. https://www.researchgate.net/publication/316019975_Assessment_of_bone_geometry_and_its_considerations_in_implant_selection_for_polio_affected_femoral_fractures_An_outcome_analysis. Accessed 6 Dec 2016
- 25.Alvarez A, Kremer R, Weiss DR, Benedetti A, Haziza M, Trojan DA. Response of postpoliomyelitis patients to bisphosphonate treatment. PM&R. 2010;2(12):1094–1103. doi: 10.1016/j.pmrj.2010.08.009. [DOI] [PubMed] [Google Scholar]