Abstract
Introduction
Olecranon fractures are a common fracture of the upper extremity. The primary aim was to investigate the evolution of olecranon fractures and fixation method over a period of 12 years. The secondary aim was to compare complication rates of Tension Band Wiring (TBW) and Plate Fixation (PF).
Materials and Methods
Retrospective Study for all patients with surgically treated olecranon fractures from 1 January 2005 to 31 December 2016 from a tertiary trauma center. Records review for demographic, injury characteristics, radiographic classification and configuration, implant choices and complications. Results grouped into three 4-year intervals, analyzed comparatively to establish significant trends over 12 years.
Results
262 patients were identified. Demographically, increasing mean age (48.7 to 58.9 years old, p value 0.004) and higher ASA scores (7.1% ASA 3 to 21.0% ASA 3 p value 0.001). Later fractures were more oblique (fracture angle 86.1–100.0 degrees, p value 0.001) and comminuted (Schatzker D type 10.4–30.0%, p value 0.025, single fracture line 94.0–66.0%, p value 0.001). Implant choice, sharp increase in PF compared to TBW (PF 16.0% to PF 80.2%, p value 0.001). Complication-wise, TBW had higher rates of symptomatic implant, implant and bony failures and implant removal.
Conclusion
Demographic and fracture characteristic trends suggest that olecranon fractures are exhibiting fragility fracture characteristics (older age, higher ASA scores, more unstable, oblique and comminuted olecranon fractures). Having a high index of suspicion would alert surgeons to consider use of advanced imaging, utilize appropriate fixation techniques and manage the underlying osteoporosis for secondary fracture prevention. Despite this, trends suggest a potential overutilization of PF particularly for stable fracture patterns and the necessary precaution should be exercised.
Keywords: Olecranon fracture, Evolution, Osteoporosis, Fragility fracture, Tension band wiring, Plate fixation
Introduction
Olecranon fractures represent 10% of all upper extremity fractures [1] and 18% of all proximal forearm fractures [2]. It represents a loss of extensor mechanism of the elbow and is commonly treated surgically [3]. Indications for surgery include displacement leading to articular incongruity, loss of extensor mechanism, and comminution, and the goals of treatment include anatomic reduction to restore articular congruity, restoration of the extensor mechanism and stable fixation to allow for early range of motion postoperatively. There are several methods of fixation, most commonly tension band wiring (TBW) or plate fixation (PF).
TBW is a technique that converts the tensile distraction force of the triceps on the posterior surface into a compressive force at the articular surface [4]. The ideal indication for such a construct is a simple, transverse olecranon fracture with no comminution. Comminution of the articular surface, unstable fractures and complex fracture involving other areas, such as the coronoid process or radial head, are not generally amenable to the tension band technique. PF is indicated in unstable, oblique or comminuted fracture patterns where TBW would not be able to provide an adequately stable fixation [5].
While commonly recognized fragility fractures include the hip, proximal humerus, distal radius and vertebral fractures, we have noticed a trend for more comminuted olecranon fractures occurring in older patients in the osteoporotic age group. We therefore hypothesized that with an increasing prevalence of osteoporosis in an aging population, the incidence of older patients presenting with unstable comminuted olecranon fractures has been increasing, necessitating the increased use of PF. The primary aim was to look at the evolution of olecranon fractures and fixation method over a period of 12 years. The secondary aim was to compare the complication rates between TBW and PF.
Patients and Methods
This was a retrospective study looking at all olecranon fractures treated with surgical fixation in a single tertiary trauma center from 1 January 2005 to 31 December 2016. Ethics approval was obtained prior to the initiation of the study. The STROBE guidelines were used to ensure comprehensive reporting of this study [6].
Surgical records from 2005 to 2016 were reviewed from an electronic surgical database through the use of surgical procedures codes and the cases were identified based on the inclusion and exclusion criteria. The inclusion criteria were surgical-treated olecranon fractures (AO/OTA 2U1B1 [7]) for patients who were 16 years or older. The exclusion criteria were pathological fractures or peri-implant fractures. The radiographs and clinical notes were analyzed.
Variables collected included demographic data, medical history, injury factors, surgery details and clinical outcomes. Injury factors included proportion of low-energy trauma or poly-trauma, incidence of open fractures, associated elbow fractures, such as coronoid or radial head fractures, or use of CT scans for fracture purposes.
Clinical outcomes included complications and re-operation rates. Complications that were collected included failure (implant and bony), infection, wound complications, non-union, malunion, ulnar neuritis, heterotopic ossification and symptomatic implant (with or without implant failure). Implant failure was defined as implant migration or breakage with no loss of reduction such as K wire backing out in TBW or screw backing out in plate fixation. Bony failure in contrast was defined as a loss of reduction due to the failure of the fixation construct. Heterotopic ossification was defined by the formation of extra-skeletal bone in the elbow. Fracture union was defined as bridging cortices on at least 3 of the 4 cortices.
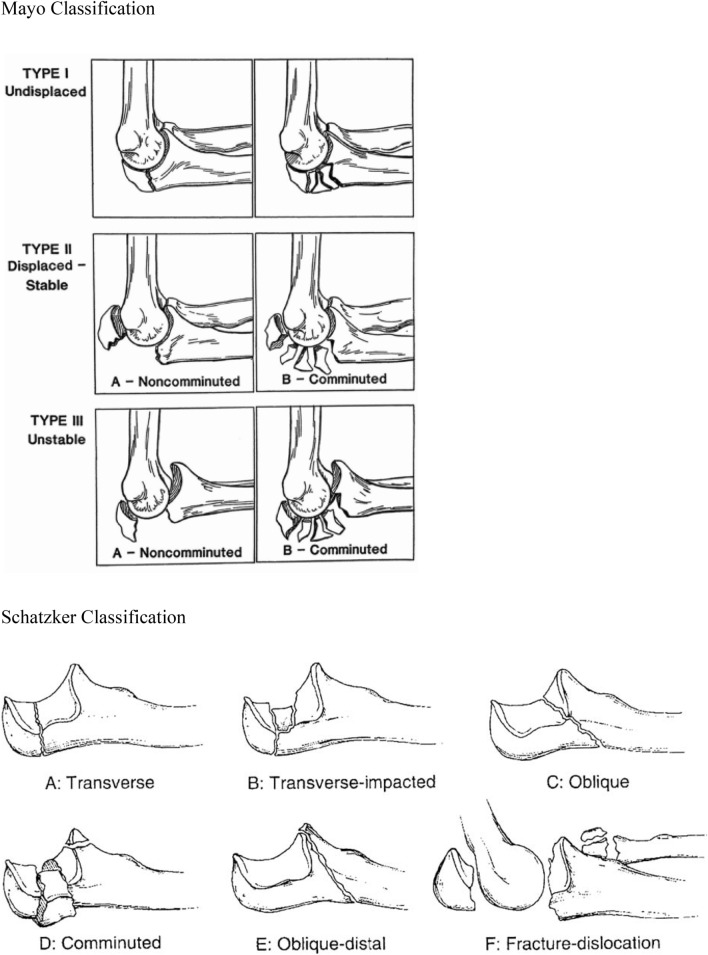
In terms of radiological assessment, the Mayo [8] and Schatzker [9] classifications (Fig. 1) were used to categorize the fractures. The Mayo classification examines three main factors, namely the stability, displacement and comminution. Type 1 is un-displaced, type 2 is displaced and stable, type 3 is displaced and unstable. Each type is further divided into A and B depending on presence of absence of comminution. The Schatzker classification is a biomechanical-based classification that progressively moves from a stable transverse fracture (Type A, B) to increasingly unstable oblique fracture (Type C) or comminuted fracture (Type D) or oblique-distal fracture (Type E) to the highly unstable fracture dislocation (Type F).
Fig. 1.
Mayo and Schatzker Classification
Beyond the radiological classification, 2 additional radiological features, namely fracture angle and number of fracture lines, were included to provide a further basis for comparison. Fracture angle as a representation of fracture obliquity (Fig. 2) was defined as the distal angle obtained from a line drawn along the ulnar shaft to a line drawn along the most prominent fracture line of the distal fragment. Building from the Schatzker classification, the more oblique the fracture, the more unstable it was deemed to be. In the event of multiple fracture lines, the most prominent fracture line was taken for measurement. Fracture angles were grouped (< 60 degrees, 61–80 degrees, 81–100 degrees, 101–120 degrees, > 121 degrees) in addition to mean fracture angle to facilitate comparisons. The number of fracture lines was identified as a measure of comminution.
Fig. 2.
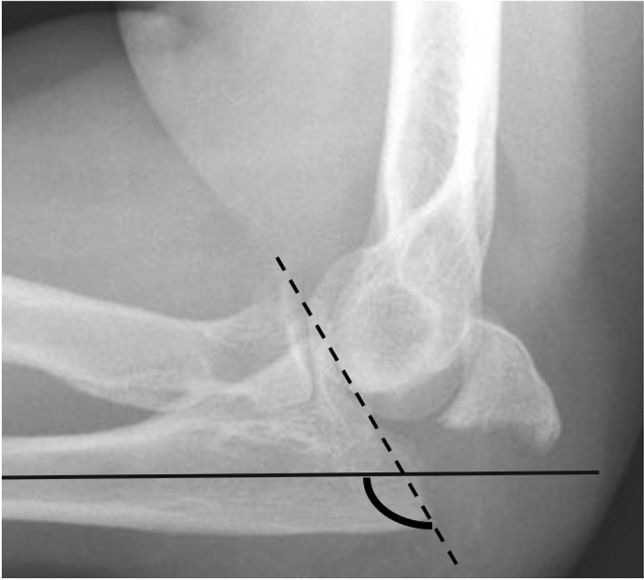
Fracture Angle to Ulnar Shaft Axis. Figure showing the calculation of the fracture angle. The solid line represents the line drawn along the ulnar shaft. The dashed line represents the line drawn along the most prominent fracture line of the distal fragment. The fracture angle is represented by the distal angle subtended between these two lines
Results were grouped into three 4-year intervals to demonstrate a trend of differences across a 12-year period. Group 1 were olecranon fractures that were surgically treated from 2005 to 2008, group 2 from 2009 to 2012 and group 3 from 2013 to 2016. Each group was analyzed separately and compared against each other.
Statistical Analysis
Data were entered and analyzed using the IBM SPSS Statistics for Windows (IBM Corp, Released 2010, Version 19, Armonk, NY: IBM Corp). For continuous variables, the descriptive statistics were presented in counts, minimum, maximum, mean (standard deviation), and median (interquartile range). As for the binary and ordinal/categorical variables, proportions and percentage were presented.
Comparisons among the three periods (2005–2008, 2009–2012, 2013–2016) were done using the chi-square test for categorical variables and ANOVA test for continuous variables. Results were presented in tabular format showing the change across the three period and the p value. A p value of less than 0.05 was considered to be significant. Data with missing information were excluded from the analysis.
Results
Demographic and Injury Characteristics
A total of 262 patients were identified according to the inclusion and exclusion criteria. The average follow-up time was 30.2 weeks (1–90 weeks). The patient demographics are shown in Table 1. There were statistically significant trends from Group 1 to Group 3 of increasing mean age (48.7 years old in Group 1 to 58.9 in Group 3, p value 0.004) and higher ASA score (7.1% ASA 3 in Group 1 to 21.0% ASA 3, p value 0.001).
Table 1.
Patient demographics
| Variable | Group 1 2005–2008 | Group 2 2009–2012 | Group 3 2013–2016 | P value |
|---|---|---|---|---|
| Gender (%) | 0.328 | |||
| Male | 20 (40) | 52 (49) | 42 (39) | |
| Female | 30 (60) | 54 (51) | 65 (61) | |
| Age | ||||
| Mean (SD) | 48.7 (19.5) | 53.1 (18.4) | 58.9 (18.5) | 0.004 |
| Median (IQR) | 49.0 (32.0) | 55.0 (26.0) | 61.5 (23.0) | |
| Past medical history (%) | ||||
| Hypertension | 10 (20.0) | 25 (23.6) | 36 (34.0) | 0.107 |
| Hyperlipidemia | 10 (20.0) | 18 (17.0) | 27 (25.5) | 0.310 |
| Diabetes Mellitus | 6 (12.0) | 13 (12.3) | 14 (13.2) | 0.969 |
| Osteoporosis | 1 (2.1) | 10 (9.4) | 8 (7.5) | 0.266 |
| Ischemic Heart Disease | 0 (0.0) | 5 (4.7) | 5 (4.7) | 0.293 |
| Renal disease | 0 (0.0) | 1 (0.9) | 2 (1.1) | 0.568 |
| No of past medical hx (%) | 0.281 | |||
| None | 35 (70.0) | 67 (63.2) | 55 (51.9) | |
| One | 6 (12.0) | 17 (16.0) | 22 (20.8) | |
| Two | 5 (10.0) | 13 (12.3) | 16 (15.1) | |
| Three | 3 (6.0) | 5 (4.7) | 9 (8.5) | |
| Four | 1 (2.0) | 1 (0.9) | 4 (3.8) | |
| Five or more | 0 (0.0) | 3 (2.8) | 0 (0.0) | |
| American Society of Anesthesiologist (ASA) Score (%) | 0.001 | |||
| 1 | 13 (46.4) | 30 (29.1) | 10 (9.5) | |
| 2 | 13 (46.4) | 58 (56.3) | 73 (69.5) | |
| 3 | 2 (7.1) | 15 (14.6) | 22 (21.0) |
In terms of injury characteristics, there were no significant changes in the proportions of low-energy trauma or poly-trauma, incidence of open fractures, associated elbow fractures, such as coronoid or radial head fractures, or use of CT scans across the 12-year period.
Radiological Assessment
The mean time to radiological union was 9 weeks. Preoperative X-rays for 9 patients were not available for analysis. Table 2 shows the distribution of fractures in the Mayo and Schatzker classifications and the fracture configurations for the 3 time periods. Overall, there was an increasing incidence of more oblique and comminuted fractures over the 12-year period. With regards to Schatzker classification, there was a statistically significant change (p value 0.025) most notably in a decrease in proportion of type A (transverse) (45.8% in Group 1–28.0% in Group 3) and increase in proportion of type D (comminuted) (10.4% in Group 1–30.0% in Group 3). In terms of the Mayo classification, there was an increased number of 2B type (comminuted) (14.9% in Group 1–32.0% in Group 3) fractures compared to 2A type (non-comminuted) (77.1% in Group 1–55.0% in Group 3). However, this did not reach statistical significance (p value 0.100).
Table 2.
Fracture Classification and configuration
| Variable | Group 1 2005–2008 | Group 2 2009–2012 | Group 3 2013–2016 | P value |
|---|---|---|---|---|
| Schatzker classification (%) | 0.025 | |||
| A | 22 (45.8) | 29 (27.6) | 28 (28.0) | |
| B | 1 (2.1) | 0 (0) | 1 (1.0) | |
| C | 19 (39.6) | 45 (42.9) | 33 (33.0) | |
| D | 5 (10.4) | 30 (28.6) | 30 (30.0) | |
| E | 0 (0) | 0 (0) | 1 (1.0) | |
| F | 1 (2.1) | 1 (1.0) | 7 (7.0) | |
| Mayo classification (%) | 0.100 | |||
| 1A | 3 (6.25) | 2 (2.0) | 5 (5.0) | |
| 1B | 0 (0) | 1 (1.0) | 2 (2.0) | |
| 2A | 37 (77.1) | 71 (67.6) | 55 (55.0) | |
| 2B | 7 (14.9) | 30 (28.6) | 32 (32.0) | |
| 3A | 0 (0) | 1 (1.0) | 2 (2.0) | |
| 3B | 1 (2.1) | 0 (0) | 4 (4.0) | |
| Number of fracture lines (%) | 0.001 | |||
| One | 47 (94.0) | 64 (60.4) | 68 (66.0) | |
| Two | 1 (2.0) | 28 (26.4) | 26 (25.2) | |
| More than two | 2 (4.0) | 14 (13.2) | 9 (8.7) | |
| Fracture angle of ulnar shaft axis (degree) | 0.001 | |||
| Mean (SD) | 86.1(26.2) | 79.8 (28.1) | 100.0 (27.5) | |
| Fracture angle of ulnar shaft axis (degree) (%) | 0.001 | |||
| < 60 | 8 (16.0) | 28 (26.4) | 12 (11.7) | |
| 61–80 | 17 (34.0) | 23 (21.7) | 16 (15.5) | |
| 81–100 | 11 (22.0) | 32 (30.2) | 21 (20.4) | |
| 101–120 | 9 (18.0) | 18 (17.0) | 29 (28.2) | |
| > 121 | 5 (10.0) | 5 (4.7) | 25 (24.3) |
In terms of fracture configuration, there was a statistically significant reduction in the proportion of single fracture lines (94.0% in Group 1–66.0% in Group 3, p value 0.001), a higher mean fracture angle (86.1 degrees in Group 1–100.0 degrees in Group 3, p value 0.001) and a lower incidence of fractures presenting with fractures angles between 80 and 100 degrees (22.0% in Group 1–20.4% in Group 3, p value 0.001).
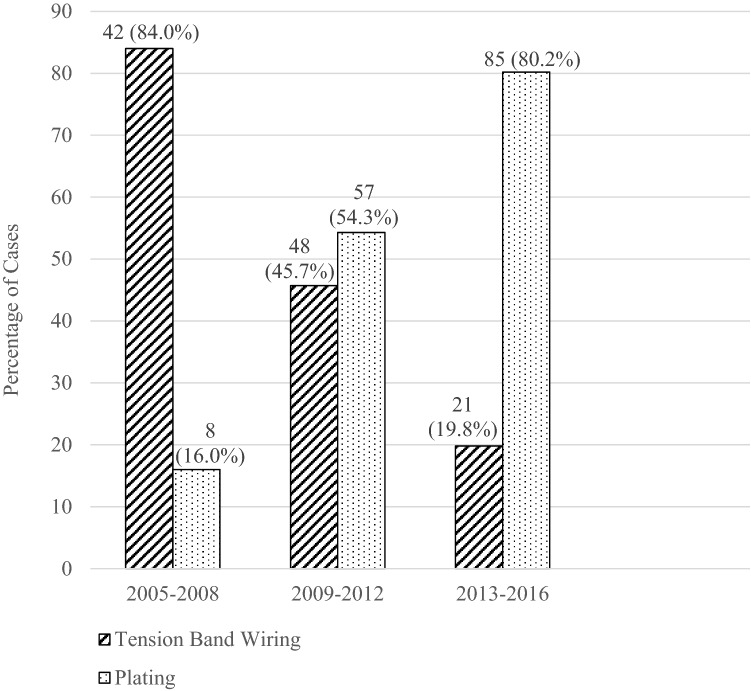
Implant Choice
A total of 111 patients underwent TBW and 150 patients underwent PF. 1 patient underwent intramedullary nailing. There was a statistically significant increase in the number of PF and correspondingly a decrease in the number of TBW across the 12-year period (TBW 84.0% PF 16.0% in Group 1 to TBW 19.8% PF 80.2% in Group 3, p value 0.001). Figure 3 illustrates the shift in implant choices.
Fig. 3.
Distribution of Implant Choice
Looking closer at the differences in fracture classification and configuration that underwent both TBW and PF, patients who underwent PF had statistically more comminuted and unstable fracture patterns (Schatzker D 38.3–7.3%, Mayo 2B 40.9–7.3%, single fracture 48.7–97.3%). Table 3 illustrates the significant demographic and fracture configurations variables for TBW and PF separately.
Table 3.
Fracture classification and configuration between tension band wiring and plate fixation
| Variable | Tension band wiring (n = 111) | Plate fixation (n = 150) | P value |
|---|---|---|---|
| Schatzker Classification (%) | 0.001 | ||
| A | 49 (45.0) | 26 (22.6) | |
| B | 0 (0) | 1 (0.9) | |
| C | 52 (47.7) | 36 (31.3) | |
| D | 8 (7.3) | 44 (38.3) | |
| E | 0 (0) | 1 (0.9) | |
| F | 0 (0) | 7 (6.1) | |
| Mayo Classification (%) | 0.001 | ||
| 1A | 2 (1.8) | 6 (5.2) | |
| 1B | 1 (0.9) | 2 (1.7) | |
| 2A | 98 (90.0) | 54 (47.0) | |
| 2B | 8 (7.3) | 47 (40.9) | |
| 3A | 0 (0) | 2 (1.7) | |
| 3B | 0 (0) | 4 (3.5) | |
| Number of fracture lines (%) | 0.001 | ||
| One | 108 (97.3) | 58 (48.7) | |
| Two | 2 (1.8) | 43 (36.1) | |
| More than two | 1 (0.9) | 18 (15.1) | |
| Fracture angle of ulnar shaft axis (degree) (%) | 0.001 | ||
| < 60 | 22 (18.5) | 17 (15.3) | |
| 61–80 | 19 (16.0) | 35 (31.5) | |
| 81–100 | 25 (21.0) | 31 (27.9) | |
| 101–120 | 29 (24.4) | 24 (21.6) | |
| > 121 | 24 (20.2) | 4 (3.6) |
Complications
Table 4 shows the complications of the TBW and PF techniques. TBW was associated with more symptomatic implant issues, implant and bony failures. TBW was associated with a statistically significant higher incidence of removal of implant compared to PF (34.0–18.4%, p value 0.023).
Table 4.
Complications of tension band wiring and plate fixation
| Variable | Tension band wiring (n = 111) | Plate fixation (n = 150) | P value |
|---|---|---|---|
| Failure | 0.001 | ||
| Implant failure (%) | 17 (18.1) | 0 (0) | |
| Bony failure (%) | 5 (5.3) | 3 (4.0) | |
| Symptomatic implant (with or without implant failure) (%) | 20 (21.3) | 8 (10.5) | 0.06 |
| Ulnar neuritis (%) | 3 (3.2) | 4 (5.3) | 0.499 |
| Deep Infection (%) | 2 (2.1) | 2 (2.6) | 0.829 |
| Heterotopic Ossification (%) | 2 (2.1) | 1 (1.3) | 0.689 |
| Superficial Wound Infection (%) | 1 (1.1) | 1 (1.3) | 0.88 |
| Total | 94 | 76 |
Discussion
Olecranon Fracture: A New Fragility Fracture?
Over a 12-year period, demographic and fracture characteristic trends from our study suggest that patients are presenting at an older age, have higher ASA scores with a more unstable, oblique and comminuted type of olecranon fracture.
With a rapidly aging population, osteoporosis has become an increasingly important public health problem [10]. The prevalence of osteoporosis is likely to increase as the population ages. While the primary focus has traditionally been on the more commonly recognized osteoporosis-related fragility fractures, such as hip and vertebral fracture [11], many other fractures throughout the body including olecranon fractures will be impacted by this growing osteoporosis epidemic.
Wellman et al. in their 2015 study reporting the use of 2.4–2.7 mm PF technique demonstrated occult fracture comminution on CT scans of olecranon fractures that were initially thought to be simple on initial radiographs [12]. The authors suggested that the extent of fracture comminution was underappreciated leading to the inappropriate use of the TBW for such fractures. In view of such concerns, TBW was no longer being performed in their institution.
Park et al. in 2017 performed a cross-sectional study on 114 patients with acute olecranon fractures with the use of elbow CT scans looking for osteoporotic features [13]. The authors reported several osteoporotic features in their findings including age-dependent low bone attenuation and low-energy trauma as the predominant cause of injury. It was recommended that osteoporosis evaluation should be considered for patients more than 50 years old presenting with olecranon fractures.
While we were not able to definitively demonstrate significant trends in certain variables (incidence of osteoporosis history at presentation, proportion of low-energy trauma), building from the findings from Park et al. which provided CT evidence, results from our study provide further demographic trends and radiographic evidence to further suggest that olecranon fractures have evolved over time to exhibit many of the characteristics of osteoporotic fractures. Raising awareness of other non-traditional fragility fractures such as olecranon fractures would have two key benefits. First, this would alert the surgeon to have a high index of suspicion for comminuted, unstable fracture pattern presentations in poor bone stock, to consider the use of advance imaging such as CT scans for further evaluation and to employ appropriate fixation techniques such as PF. Second, this would prompt the surgeon to recognize, investigate and manage the underlying osteoporosis potentially as part of a fracture liaison service which is key to the prevention of future fractures [10]. Of note, only 34 out of 262 patients (13.0%) in our study had any record of bone mineral densitometry (BMD) done either prior to or within 1 year of the olecranon fracture presentation.
Olecranon Plate Fixation: Have We Gone Too Far?
Our study demonstrated a very dramatic increase in usage of PF as compared to TBW over the 12-year period. While this could be partially attributed to an evolution in the fracture pattern becoming more unstable and comminuted as demonstrated in our findings, the trend demonstrated did not appear strong enough to explain the five-fold increase in proportion of PF compared to TBW.
While our study suggested that PF was being used more often in the correct fracture configuration with more fracture lines and oblique type fracture compared to TBW, it was also used in a significant proportion of situations where there was a single fracture line that was within a 70–90 degrees angle to the ulnar shaft i.e., transverse fracture configuration. These fractures may have been amenable to TBW. There can be many possible reasons for this ranging from industry influence, wider availability of contoured plates to surgeon preferences.
Though proponents cite superior biomechanical properties and lower complication rates for the plate fixation technique, questions about the routine use of PF for more stable e.g., Mayo 2A olecranon fractures remain, particularly due to the higher cost of this technique [5, 14, 15]. Our study demonstrated significantly higher complication rates with TBW especially in terms of wire migration and symptomatic implant prominence requiring the need for revision or removal of implant which is consistent with literature [16, 17].
A recent prospective randomized control trial by Duckworth et al. compared treatment of PF versus TBW for Mayo 2A fractures in active patients and showed no difference in patient-reported outcome measures at 1 year following surgery [18]. A balance between the higher implant cost of PF compared to the higher risk of symptomatic implant necessitating implant removal with TBW must be weighed against each other. Tan et al. looked at the cost effectiveness of PF compared to TBW in Mayo 2A olecranon fractures concluded that TBW was ideal from an economic analysis; however, the local implant removal rates and cost have to be taken into account for each patient [19].
Strengths and Limitations
To the best of our knowledge, this is the largest study to date examining the evolution of olecranon fractures in a comprehensive manner ranging from the demographics shift, changes in fracture morphology, to the implant choices. Adding to existing literature, the study provides evidence that recent trends of olecranon fractures are demonstrating certain features of osteoporotic fragility fractures. Raising awareness among orthopedic surgeons can have potentially far-reaching effects not only in dealing with the index presentation but in prevention of subsequent fractures through the early treatment of osteoporosis.
There are several limitations for this study. First, this is a retrospective nature of the study. Second, patient-reported outcomes (PROMs) were not collected. Third, the implants used for olecranon fracture PF have changed over the study period. PF has evolved from non-contoured locking plate to locking, pre-contoured plates and more recently variable angle, locking, pre-contoured plates. This limits the generalizability of our conclusions to current practice using the latest plate designs. Fourth, only 13% of our population had BMD results, the gold standard diagnostic tool for osteoporosis. While this has impacted the ability to definitely establish osteoporosis and its severity, the evidence presented in this study suggested support the key message that osteoporosis was likely under recognized and under investigated in many of these fractures.
Conclusion
Over a 12-year period, our study found a trend of older patients with higher ASA scores presenting with more comminuted, oblique and unstable olecranon fractures. With the understanding that these fractures may represent fragility fractures in the elderly, the surgeon should consider the use of advanced imaging, utilize appropriate fixation techniques and manage the underlying osteoporosis for secondary fracture prevention.
While there was a clear demographical and fracture pattern trend demonstrated, this was coupled with a disproportionate rise in the use of plate fixation. Given its significantly higher cost compared to TBW, the use of plating particularly in stable fracture patterns is an area for future research.
Acknowledgements
The authors would like to acknowledge the contributions of Dr Thach Thuan Quoc and Dr Yoko Wong Kin Yoke in assisting with the statistical analysis.
Abbreviations
- TBW
Tension band wiring
- PF
Plate fixation
- ASA
American Society of Anesthesiologist
- PROM
Patient-reported outcome measure
Authors Contributions
BYJT: Conceptualization, Methodology Data curation, Formal analysis, Methodology, and Writing (original draft). JN and WXN: Methodology, Data curation, Formal analysis, and Writing (review and editing). YW: Data curation, Formal analysis, and Writing (review and editing). EBKK: Conceptualization, Data curation, Resources, Supervision, and Writing (review and editing). The authors read and approved the final manuscript.
Funding
No funding was received for this project.
Availability of Data and Materials
The data used and analyzed during the current study are available in anonymized form from the corresponding author on reasonable request.
Declarations
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics Approval
Ethics approval was obtained prior to the initiation of the study (National Healthcare Group Domain Specific Review Board Reference: 2015/00988).
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Veillette CJ, Steinmann SP. Olecranon fractures. The Orthopedic Clinics of North America. 2008;39(2):229–36. doi: 10.1016/j.ocl.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. 2012;43(3):343–346. doi: 10.1016/j.injury.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Wiegand L, Bernstein J, Ahn J. Fractures in brief: Olecranon fractures. Clinical orthopaedics and related research. 2012;470(12):3637–3641. doi: 10.1007/s11999-012-2393-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instructional Course Lectures. 1995;44:175–185. [PubMed] [Google Scholar]
- 5.Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. The Journal of bone and joint surgery American volume. 2009;91(10):2416–2420. doi: 10.2106/JBJS.H.01419. [DOI] [PubMed] [Google Scholar]
- 6.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Journal of Clinical Epidemiology. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Meinberg E, Agel J, Roberts C, Karam M, Kellam J. Fracture and dislocation classification compendium—2018. Journal of Orthopaedic Trauma. 2018;32:S1–S10. doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 8.Bernstein J, Monaghan BA, Silber JS, DeLong WG. Taxonomy and treatment–a classification of fracture classifications. The Journal of bone and joint surgery British volume. 1997;79(5):706–7. doi: 10.1302/0301-620X.79B5.0790706. [DOI] [PubMed] [Google Scholar]
- 9.Schatzker J, Tile M, editors. J S Fractures of the olecranon. The rationale of operative fracture care. New York: Springer; 1996. [Google Scholar]
- 10.Compston JE, McClung MR, Leslie WD. Osteoporosis. The Lancet. 2019;393(10169):364–376. doi: 10.1016/S0140-6736(18)32112-3. [DOI] [PubMed] [Google Scholar]
- 11.Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, et al. Major osteoporotic fragility fractures: Risk factor updates and societal impact. World Journal of Orthopedics. 2016;7(3):171–181. doi: 10.5312/wjo.v7.i3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wellman DS, Lazaro LE, Cymerman RM, Axelrad TW, Leu D, Helfet DL, et al. Treatment of olecranon fractures with 2.4- and 2.7-mm plating techniques. Journal of Orthopaedic Trauma. 2015;29(1):36–43. doi: 10.1097/BOT.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 13.Park SC, Gong HS, Kim K, Lee SH, Kim S, Baek GH. Olecranon fractures have features of osteoporotic fracture. Journal of Bone Metabolism. 2017;24(3):175–181. doi: 10.11005/jbm.2017.24.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hak DJ, Golladay GJ. Olecranon fractures: Treatment options. The Journal of the American Academy of Orthopaedic Surgeons. 2000;8(4):266–275. doi: 10.5435/00124635-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. The Journal of Bone and Joint Surgery American Volume. 1985;67(9):1396–1401. doi: 10.2106/00004623-198567090-00015. [DOI] [PubMed] [Google Scholar]
- 16.Ren YM, Qiao HY, Wei ZJ, Lin W, Fan BY, Liu J, et al. Efficacy and safety of tension band wiring versus plate fixation in olecranon fractures: A systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research. 2016;11(1):137. doi: 10.1186/s13018-016-0465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koziarz A, Woolnough T, Oitment C, Nath S, Johal H. Surgical Management for olecranon fractures in adults: A systematic review and meta-analysis. Orthopedics. 2019;42(2):75–82. doi: 10.3928/01477447-20190221-03. [DOI] [PubMed] [Google Scholar]
- 18.Duckworth AD, Clement ND, White TO, Court-Brown CM, McQueen MM. Plate versus tension-band wire fixation for olecranon fractures: A prospective randomized trial. The Journal of Bone and Joint Surgery American volume. 2017;99(15):1261–1273. doi: 10.2106/JBJS.16.00773. [DOI] [PubMed] [Google Scholar]
- 19.Tan BYJ, Pereira MJ, Ng J, Kwek EBK. The ideal implant for Mayo 2A olecranon fractures? An economic evaluation. Journal of Shoulder and Elbow Surgery. 2020;29(11):2347–2352. doi: 10.1016/j.jse.2020.05.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used and analyzed during the current study are available in anonymized form from the corresponding author on reasonable request.