Abstract
The COVID-19 pandemic has exacerbated inequalities related to the digital divide. With wide adoption of remote working and learning, telehealth, and virtual events and social activities, the technology have-nots and know-nots experienced substantial marginalization and elevated risks of COVID-19 exposure in daily lives. This study discusses the pathways through which digital exclusion could aggravate the impacts of the pandemic and explored the linkage between digital access and COVID-19 outcomes in U.S. counties. It finds that counties with higher percentages of digitally excluded populations have seen higher COVID-19 case and death rates throughout the pandemic and lower vaccination rates by January 2022.
Keywords: Digital divide, Internet access, Digital exclusion, Health disparities, COVID-19
1. Introduction
The digital divide, or the gap between those who can and those who cannot use and benefit from modern information and communication technologies (ICTs), has been a long-standing social and policy issue since we entered the information age. As Internet services, computers, and mobile phones become more prevalent and affordable, focus on the digital divide has extended from physical access to digital literacy and skills (Bodie and Dutta, 2008; Thomas et al., 2018; Van Deursen and Mossberger, 2018; Yu et al., 2018). Nevertheless, the first-level digital divide – the unequal access to Internet, especially broadband connections, and devices such as home computers and mobile phones – persists even in the most developed countries and regions (Thomas et al., 2018; Winslow, 2019). Moreover, as the society as a whole is more accustomed to and dependent on digital technologies in all aspects of daily life, the consequences of being on the wrong side of the gap can be more pronounced in these countries and regions.
The digital divide is often closely associated with socioeconomic status (Fang et al., 2019; Forenbacher et al., 2019) and hence easily overlooked when the latter is seen as a more universal indicator of social inequalities. Being disconnected in an increasingly interconnected network society and consequently excluded from employment, education, and other opportunities, however, could replicate and perpetuate existing inequalities. Interventions that address the digital divide directly and extend access to and utilization of ICTs among marginalized communities, on the other hand, have the potential of alleviating poverty, closing the achievement gap, and reducing health disparities (Azzopardi-Muscat and Sørensen, 2019; Kim, 2018; Mitchell et al., 2019; Rotondi et al., 2020; Soriano, 2007). Studying the digital divide as an additional dimension of social exclusion and better understanding its impacts can therefore have important policy implications.
The COVID-19 pandemic has exacerbated the inequalities associated with digital exclusion and brought renewed attention to the digital divide (Lai & Widmar, 2021; Watts, 2020). With much of the world swiftly turning to working from home, remote learning, and virtual activities ranging from concerts and church services to weddings and funerals following the initial COVID-19 outbreaks in 2020, individuals and households without reliable, high-speed Internet or any of the hardware, software, and subscriptions needed to stay connected increasingly find themselves left out of the plan forward. The significance of digital inclusion as a social determinant of health has also multiplied: more extensive adoption of telehealth widens the gap between technology haves and have-nots (Clare, 2021; Ramsetty and Adams, 2020); lockdowns and social isolation take a heavier toll on the mental health and well-being of those unable to participate in online gatherings and social activities (Cho and Kim, 2022; Martins Van Jaarsveld, 2020); not to mention the indirect effects of the digital divide through magnifying inequalities in other social determinants of health (Alkureishi et al., 2021; Sostero et al., 2020).
There has been limited discussion and little evidence, however, on the impact of the digital divide on COVID-19 infections and deaths (Eruchalu et al., 2021), two of the most relevant health outcomes of the pandemic, despite the established linkages between race (Bhala et al., 2020; Gold et al., 2020; Hamidian Jahromi and Hamidianjahromi, 2020; Van Holm, Wyczalkowski and Dantzler, 2021) or socioeconomics (Mena et al., 2021; Sy et al., 2021) and COVID-19 outcomes. Apart from the aforementioned influences of the digital divide on general health and telehealth access, there are multiple reasons to believe that digital exclusion may contribute to the spread of COVID-19 and more adverse outcomes:
-
1.
Digital exclusion limits individuals' ability to “shelter in place” and adhere to quarantine and isolation guidelines, especially in the early stages of the pandemic and during periods of high transmission in the subsequent waves. Having to work in person as opposed to remotely, for example, can substantially increase one's exposure to and risk of contracting COVID-19. While the ability to telecommute is largely determined by the nature of the occupation (Sostero et al., 2020), the technology have-nots and know-nots are essentially precluded from opportunities of telework or participating in the new digital economy and therefore restricted to occupations and industries that require in-person work. Likewise, inability to substitute other trips with digital technologies, such as virtual doctor visits, leads to more in-person contact and multiplies the risk of COVID-19 exposure and transmission.
-
2.
Digital exclusion slows down the dissemination of information and knowledge, which can be crucial for timely responses and taking precautionary measures in a rapidly evolving pandemic. In digitally marginalized communities, the awareness and understanding of local pandemic situations, public health guidelines and policies could lag behind the most up-to-date information, leading to delays in social distancing, masking, sanitation and ventilation upgrades, testing and early treatment, etc.
-
3.
Many of the pandemic response measures – from testing and contact tracing to treatment and vaccines, including the more recent distribution of home test kits and masks – depend on digital platforms and technologies. As a result, even when digitally disadvantaged individuals are aware of COVID-19 outbreaks in their communities or seek to take precautions, they may face additional difficulties in locating and accessing the needed resources. The more effective N95 and KN95 respirators, for example, have been in short supply during much of the pandemic and often only found online. Apart from the cost factor, access to Internet and skills to identify and verify online stores are necessary to acquire such personal protective equipment (PPE) that offers the most protection. Similarly, in the first few months of the vaccine rollout, vaccination appointments could be extremely difficult to secure in some regions and require persistent searching, refreshing, and filling in scheduling forms online (Fowler, 2021; Santhanam, 2021). These technological barriers amplified the challenges facing the digitally marginalized in fighting COVID-19.
-
4.
Digital exclusion could potentially distort perceptions of the pandemic and related issues, leading to more risky behavior and increased COVID-19 transmission. Although the COVID-19 pandemic is, first and foremost, a public health crisis, it has also become a crisis of public opinion and trust in the United States as well as many other parts of the world, complicating the public health efforts to contain the pandemic and its impacts (Algan et al. 2021; Devine et al., 2021; Gualano et al., 2022). Mistrust in government, public health agencies, and scientists are associated with incompliance with public health measures, vaccine hesitancy, and mortality rates (Devine et al., 2021; Palamenghi et al., 2020). The role of digital technologies in the public trust crisis is a complex one. On the one hand, digital platforms, especially social media, have greatly facilitated the spread of misinformation, the maintenance of information silos, and reinforcement of existing misbeliefs (Auxier, 2020; Chou et al., 2020; Vicario et al., 2016). On the other hand, misinformation can be countered by exposure to contradicting content, active consumption of information (e.g., through Internet search instead of social media feeds), and fact checking (Ferreira and Borges, 2020; Nekmat, 2020; Wittenberg et al., 2020), most of which depend on advanced access to and knowledge of digital technologies. For instance, someone with only mobile Internet access on a limited data plan is more likely to rely on Facebook feeds as their main source of information and less likely to look up and fact check the information through credible sources or search engines as compared to someone with broadband Internet access on a home computer. While the digital divide per se is not necessarily aligned with the ideological divide that often dictate COVID-19 perceptions, lack of access to or proficiency in digital technologies could restrict one's exposure to diverse information sources and ability to actively seek and verify information, making digitally disadvantaged individuals more vulnerable to misinformation about COVID-19 (Ferreira and Borges, 2020; Seo et al., 2021).
-
5.
Moreover, digital exclusion could indirectly affect COVID-19 outcomes through exacerbating the pandemic's negative impacts on mental health. Many have suffered from different degrees of anxiety and depression related to the pandemic (Panchal et al., 2021), though the digitally disadvantaged could disproportionately experience social isolation, loneliness, and stress as online activities, services, and social interactions substituted for in-person ones (Cheshmehzangi et al., 2022; Cho and Kim, 2022; Martins Van Jaarsveld, 2020). With known linkages between mental health and the immune system, these psychological impacts may subject the digitally excluded to a higher risk of severe COVID-19 outcomes (Vasile, 2020; World Health Organization, 2022).
These theoretical considerations motivated this study to explore the linkage between the digital divide and COVID-19 outcomes in the United States. I formulate the following hypotheses:
H1
Access to digital technologies is negatively associated with COVID-19 infection and death rates.
H2
Access to digital technologies is positively associated with COVID-19 vaccination rates.
The following section describes the data and the analytical model. Section 3 presents the results, and Section 4 concludes the study with a discussion of the findings and policy implications.
2. Data and methods
This study uses three data sources: 1) county-level digital access and socio-demographic data from the American Community Survey (ACS), 2015–2019; 2) COVID-19 data from the CDC, compiled over time by the Opportunity Insights Economic Tracker (Chetty et al. 2020); and 3) 2020 presidential election returns to control for political attitudes (MIT Election Data and Science Lab, 2018). The three key COVID-19 outcome variables are confirmed case, death, and vaccination rates. These metrics are available daily since January 2020, as seven day moving averages, in the Opportunity Insights Economic Tracker database. I converted the data to monthly series, using the last Sunday of each month, from 2/28/2020 to 1/30/2022. After verifying the data with the CDC Data Tracker,1 the COVID-19 dashboard by Johns Hopkins University,2 and state pandemic reports, I adjusted the dataset to remove obvious inconsistencies and recalculated COVID-19 case and death rates based on confirmed case and death numbers and county population from 2015-2019 ACS. The states of Alaska and Hawaii, as well as 9 counties in California and Texas, are excluded from the study due to missing or inaccurate vaccination data. I also excluded 7 small counties with populations below 500 in the regression analysis, leaving 3101 counties in the 48 contiguous states and the District of Columbia.
Fig. 1 displays the case, death, and full vaccination rates in contiguous United States by 1/30/2022. While COVID-19 mortality is a direct result of COVID-19 infections, the geographic correlation between COVID-19 incidence and death rates is less straightforward. As Fig. 1 shows, some of the areas with the highest death rates, such as Georgia, Montana, and parts of South Dakota and Texas, are not necessarily higher in case rates than neighboring regions. Similarly, while a negative correlation between vaccination and case/death rates can be seen along the east and west coasts, other regions with high vaccination rates, such as Arizona, New Mexico, southern Texas, and northern Michigan are also some of the hardest hit areas by COVID-19. A two-way relationship could be at play: while communities with higher vaccination rates may be better protected against future outbreaks, those that have seen higher levels of COVID-19 incidence and mortality may take a more aggressive approach to vaccination campaigns or have more people motivated to get the vaccine, leading to higher vaccination rates. The net relationship between vaccination rate and COVID-19 case/death rate, therefore, can be either negative or positive.
Fig. 1.
COVID-19 case, death, and full vaccination rates on 1/30/2022.
The independent variable, digital exclusion/access, also consists of three measures: the share of households with no Internet access, the share of individuals who have no computer at home, and the share of individuals who have broadband Internet subscription. The first two variables measure digital exclusion – without a computer or Internet plan, individuals and households are simply excluded from most resources or opportunities available online. The third variable measures digital access at a more advanced level, as a broadband connection is usually necessary for more intensive Internet use like streaming and video/audio meeting, essential for activities like telehealth, remote learning, and working from home. I expect the first two measures of digital exclusion (% no Internet and % no computer) to be positively associated with COVID-19 case and death rates and negatively associated with vaccination rates, and the opposite relationships between the third variable (% broadband) and the outcome variables.
Fig. 2 shows the distribution of digitally excluded and broadband connected populations across the lower 48 states. Compared with the three COVID-19 outcome variables, these measures are more closely related, especially the first two measures of digital exclusion, though the prevalence of home computers is much higher than that of the Internet. A substantial number of the U.S. counties have more than 20% of the households with no Internet access, with some as high as 40%. Some of these regions with the highest share of digitally excluded population, such as southern Texas along the U.S.-Mexico border and the Black Belt states, are also among the regions hardest hit by COVID-19 in Fig. 1.
Fig. 2.
Percentages of households with no Internet, individuals with no home computer, and individuals with broadband subscriptions from ACS 2015–2019.
A simple comparison of the outcome variables among counties with different levels of Internet access, as shown in Table 1 , supports the hypothesized relationship between the digital divide and COVID-19 outcomes: COVID-19 death rates in counties with the lowest level of digital access almost triple those in counties with the highest level of access. However, since digital access is highly correlated with urban/rural status, demographics and socioeconomic factors, many of which may also influence COVID-19 outcomes, the relationship in Table 1 may be a spurious one reflecting association with a common third factor. Therefore, the multivariate analysis controls for population density, age, race, housing tenure, poverty, income, political attitudes, as well as state fixed effects to account for different state-level responses to the pandemic. The regression models assume the following forms:
| (1) |
| (2) |
| (3) |
where are the three outcome variables described above; is one of the three measures of the digital divide; and are the COVID-19 case and full vaccination rates, lagged by one month, to account for the relationships between the three outcome variables; is a vector of control variables; represents the state fixed effects; and is the error term.
Table 1.
COVID-19 outcomes in U.S. counties with different levels of Internet access.
| % No Internet | # of counties | COVID-19 cases per 100,000 people | COVID-19 deaths per 100,000 people | Full vaccine series per 100 people |
|---|---|---|---|---|
| 0–10% | 236 | 20,192 | 161 | 62.7 |
| 11–20% | 1401 | 21,975 | 288 | 52.2 |
| 21–30% | 1096 | 22,412 | 381 | 44.9 |
| 31–40% | 297 | 22,526 | 412 | 44.9 |
| >40% | 78 | 22,881 | 458 | 49.7 |
Despite the use of lagged variables, Models 1 to 3 are not panel data or time series models. Instead, they are estimated as a series of cross-sectional models examining the cumulative rates of COVID-19 cases, deaths, and vaccinations at different time points. This is because 1) this study is more interested in exploring the inter-county relationship between digital access and COVID-19 outcomes, and 2) both the independent variables and the control variables were measured before the pandemic, and while the monthly COVID-19 metrics are available, there is not sufficient temporal variation in digital access or socio-demographics to explore during the two years of the pandemic. The lagged vaccination rate is only included in time periods when vaccines were available, i.e., after December 2020.
As OLS regression can be biased by spatial autocorrelation, I also test a spatial lag model and a spatial error model, with the assumption that the outcome variable (COVID-19 case, death, or vaccination rates) is correlated across neighboring counties, or that the error term is correlated across neighboring counties, respectively. The R package ‘spatialreg’ is used to estimate the spatial autoregressive models.
Table 2 presents the descriptive statistics of the dependent, independent, and control variables. COVID-19 case, death, and vaccination rates in Table 2 represents latest updates from the last week of January 2022. Due to the Omicron surge in the U.S., there had been a sharp increase in COVID-19 cases in January 2022 compared to November and December 2021. Considering the delay between surges in cases and deaths, we may see a similar change in the death rate in February 2022 or subsequent periods. The maximum value of the full vaccination rate exceeds 100, representing a small number of counties that have administered more vaccine series than their residents, likely due to non-residents from adjacent jurisdictions taking vaccines in the county.
Table 2.
Descriptive statistics of key variables.
| Variable | Mean | SD | Min | Max | Description |
|---|---|---|---|---|---|
| Case rate | 22,062 | 4601 | 5218 | 62,983 | Confirmed COVID-19 cases per 100,000 people |
| Death rate | 327 | 143 | 0 | 1089 | Confirmed COVID-19 deaths per 100,000 people |
| Full vaccination rate | 49.7 | 11.7 | 1.6 | 106 | Full vaccination series completed per 100 people |
| % No Internet | 20.6 | 8.2 | 2.5 | 59.6 | % of households with no Internet access |
| % No computer | 9.9 | 5.2 | 0.8 | 46.5 | % of population with no computer at home |
| % Broadband | 80.2 | 8.3 | 34.7 | 97.5 | % of population with broadband Internet subscription |
| Population density | 274 | 1802 | 0 | 71,485 | Population density (persons per square mile, log transformed in model) |
| % Under 18 | 22.2 | 3.5 | 7.3 | 41.8 | % of population under 18 |
| % 65 and over | 18.8 | 4.6 | 3.2 | 56.7 | % of population 65 and over |
| % Black | 9.2 | 14.6 | 0.0 | 87.2 | % of population Black |
| % Hispanic | 9.4 | 13.9 | 0.0 | 99.2 | % of population Hispanic |
| % Renter | 28.3 | 8.2 | 6.9 | 80.3 | % of housing units renter occupied |
| Poverty rate (%) | 15.1 | 6.3 | 2.4 | 55.5 | % of population living in poverty |
| % Democrat votes | 33.3 | 15.9 | 3.1 | 92.1 | % of votes for the Democrat candidate in 2020 presidential election |
| Median income ($) | 53,310 | 14,101 | 21,504 | 142,299 | Median income, 2019 dollars (log transformed in model) |
| N | 3101 |
3. Results
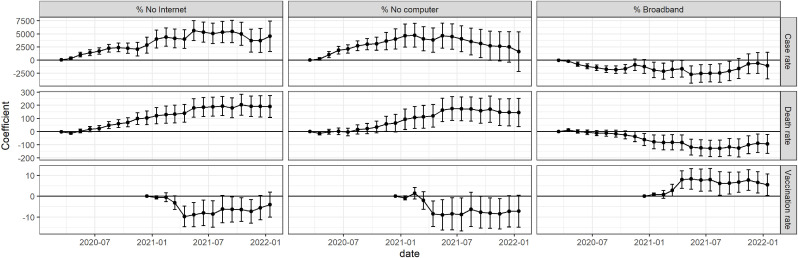
The three models are estimated for each of the three independent variables (% no Internet, % no computer, and % broadband), resulting in nine models per time period. Fig. 3 summarizes the main coefficients of interest (i.e., the association between the measure of digital divide and the COVID-19 outcome) and 95% confidence intervals over time for each of the nine models.3 Overall, Fig. 3 supports the hypotheses that higher levels of digital exclusion (% no Internet and % no computer) are associated with higher COVID-19 infection and death rates and lower vaccination rates, and higher levels of digital access (% broadband) are associated with lower case and death rates and higher vaccination rates. Among the three outcome variables, cumulated COVID-19 death rates demonstrate the most persistent linkage with digital access over time and across all measures of the digital divide, although the relationship only became significant after mid-to-late 2020, while the association between the digital divide and COVID-19 case rates appeared in the first few months of the pandemic and persisted until fall 2021, when waves of new variants likely changed the picture. Nevertheless, the basic measure of digital exclusion (% no Internet) remains a strong predictor of cumulated COVID-19 case rates, even as the Omicron surge caused a leap in case numbers in most counties by the end of the study period.
Fig. 3.
Estimates of the association between digital access and COVID-19 outcomes over time, March 2020 to January 2022.
Note: error bars represent 95% confidence intervals.
The relationship between digital access and cumulated vaccination rates also took a few months to show, mostly after April 2022, when all U.S. adults became eligible for COVID-19 vaccines per President Biden's deadline. There is, however, a small but significant relationship between broadband Internet access and vaccination rates in January 2021 (0.843, p = 0.011), when vaccines were first made available to frontline healthcare workers and people with increased risk due to age or existing conditions. The corresponding coefficients for % no Internet and % no computer are negative but not statistically significant (−0.588 and −0.792, respectively, with p values of 0.123 and 0.107). A possible explanation is that not just home computers with any Internet subscription, but high-speed, stable connections were often required to secure vaccination appointments in the early phase of vaccine rollout when many jurisdictions faced vaccine shortages. Broadband Internet access also has the most consistent association with vaccination rates throughout the study period (Fig. 3).
Table 3 presents the full OLS model results for January 2022, the last time period in the dataset. As already shown in Fig. 3, some coefficients between digital access and COVID-19 case/vaccination rates, while maintaining the expected signs, had become statistically insignificant by late 2021 or early 2022. All three digital divide measures, nevertheless, stayed strong predictors of cumulated COVID-19 deaths. Most of the control variables behave as expected. Notably, the Democrat candidate's (Joe Biden) vote share in 2020 presidential election is strongly associated with lower COVID-19 case and death rates and higher vaccination rates, which is consistent with the partisan divide on COVID-19 attitudes, behaviors, and outcomes (Gollwitzer et al., 2020). Median income is negatively related to COVID-19 case and death rates and positively related to vaccination rates, corroborating the observation that lower-income communities tend to experience more severe COVID-19 outcomes (Mena et al., 2021). Poverty rate, unsurprisingly, has coefficients of the opposite signs, though only those in the death rate models (columns 4–6) are statistically significant.
Table 3.
Digital access and COVID-19 outcomes, January 2022.
| Dependent Variable | Cases per 100,000 people |
Deaths per 100,000 people |
Full vaccination series per 100 people |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| % No Internet | 4541*** (1484) | 190.8*** (42.47) | −4.064 (3.048) | ||||||
| % No computer | 1604 (1913) | 144.6*** (54.74) | −7.179* (3.917) | ||||||
| % Broadband | −1053 (1292) | −93.83** (36.94) | 5.481** (2.638) | ||||||
| Case rate (t – 1) | 0.011*** (0.001) | 0.012*** (0.001) | 0.012*** (0.001) | 0.000*** (0.000) | 0.000*** (0.000) | 0.000*** (0.000) | |||
| Full vaccination rate (t – 1) | 108.9*** (8.913) | 108.5*** (8.927) | 108.6*** (8.932) | −0.429* (0.259) | −0.444* (0.260) | −0.437* (0.260) | |||
| Population density (logged) | 649.7*** (72.96) | 603.0*** (71.94) | 604.6*** (72.46) | 12.47*** (2.108) | 11.04*** (2.079) | 11.16*** (2.092) | −0.427*** (0.152) | −0.428*** (0.149) | −0.444*** (0.150) |
| % Under 18 | −1943 (2767) | −1238 (2776) | −1190 (2770) | 646.5*** (79.09) | 661.2*** (79.40) | 665.8*** (79.23) | 3.760 (5.698) | 4.269 (5.708) | 4.232 (5.692) |
| % 65 and over | −31992*** (2439) | −31826*** (2447) | −31790*** (2445) | 1024*** (71.65) | 1027*** (71.95) | 1031*** (71.85) | 51.03*** (5.058) | 51.43*** (5.066) | 51.29*** (5.057) |
| % Black | 3586*** (933.8) | 3900*** (929.3) | 3899*** (929.5) | 148.1*** (26.75) | 158.6*** (26.65) | 158.4*** (26.66) | −25.75*** (1.859) | −25.85*** (1.846) | −25.78*** (1.848) |
| % Hispanic | 6075*** (792.2) | 6324*** (789.0) | 6293*** (790.1) | 40.13* (22.93) | 49.76** (22.87) | 46.81** (22.91) | 3.245** (1.642) | 3.039* (1.635) | 3.214** (1.637) |
| % Renter | 2177* (1223) | 1492 (1208) | 1496 (1210) | −15.43 (34.97) | −36.85 (34.56) | −36.642 (34.606) | 2.736 (2.509) | 2.803 (2.472) | 2.652 (2.476) |
| Poverty rate | 1183 (2354) | 1741 (2379) | 1741 (2381) | 190.0*** (67.26) | 195.5*** (68.02) | 195.8*** (68.10) | −3.067 (4.840) | −2.251 (4.882) | −1.972 (4.887) |
| % Democrat votes | −14924*** (981.2) | −14849*** (984.2) | −14853*** (984.7) | −162.2*** (29.79) | −160.1*** (29.89) | −159.8*** (29.89) | 64.27*** (1.798) | 64.37*** (1.800) | 64.38*** (1.798) |
| Median income (logged) | −3248*** (730.0) | −3904*** (702.1) | −3901*** (704.1) | −95.97*** (21.00) | −116.6*** (20.26) | −116.3*** (20.33) | 10.66*** (1.513) | 10.77*** (1.453) | 10.64*** (1.457) |
| Intercept | 58863*** (8420) | 66823*** (8050) | 67774*** (7871) | 794.7*** (243.8) | 1047*** (234.1) | 1131*** (229.4) | −101.3*** (17.56) | −102.8*** (16.79) | −106.5*** (16.42) |
| N | 3093 | 3093 | 3093 | 3093 | 3093 | 3093 | 3084 | 3084 | 3084 |
| R Squared | 0.45 | 0.45 | 0.45 | 0.54 | 0.54 | 0.53 | 0.65 | 0.65 | 0.65 |
***: p < 0.01; **: p < 0.05; *: p < 0.1. All models include state fixed effects. Figures in parentheses are standard errors.
Some coefficients, however, run contrary to popular hypotheses or findings in earlier studies. The positive association between % under 18 and COVID-19 death rates, for example, likely reflects some unobserved factor that correlates with both the percentage of children in a county and COVID-19 deaths instead of suggesting that children are more likely to die from the coronavirus. Interestingly, after controlling for political attitudes, population density and % Black are both negatively associated with the vaccination rate, indicating that urban counties and majority-Black counties are not necessarily more successful in their vaccination campaigns but for the preferences of their residents. These two variables are positively associated with case and death rates, consistent with the evidence showing that densely populated areas and minority communities are more vulnerable to COVID-19 transmission and severe outcomes (Gold et al., 2020; Van Holm et al., 2021). The percentage of Hispanic population is positively associated with all three COVID-19 outcomes, further showing how racial/ethnic segregation and marginalization can lead to increased risks for minority communities in a pandemic.
Nevertheless, it should be noted that the relationships between % Hispanic and COVID-19 death and vaccination rates are not consistently positive over time. In a temporal comparison like Fig. 3, the relationship between % Hispanic and the vaccination rate has been significantly negative until October 2021, similar to that of % Black. The coefficients on death rates (Models 4–6) are also negative in some time periods and statistically insignificant in some others, though the positive association between % Hispanic and COVID-19 cases remains consistent throughout the study period. Similarly, while % renter does not seem to be a strong predictor in the January 2022 model (Table 3), it is positively related to COVID-19 case and vaccination rates from the beginning of the pandemic to late 2021.
Another oft-mentioned COVID-19 risk factor, the percentage of population age 65 and over, is positively associated with death and vaccination rates but negatively associated with the case rate. These coefficients are largely consistent over time, with the exception of positive coefficients on COVID-19 case rate in March and April 2020. It is likely that after the first few months of the pandemic, as it became apparent that age and underlying conditions were among the leading predictors of severe COVID cases and deaths, older adults were offered extra protection by policy measures, communities, and family members, as well as taking additional precaution to protect themselves and avoid infections, including the higher likelihood of getting a COVID vaccine. Still, the heightened risk of severe outcomes when older people are infected could have led to the strong positive association between % 65 and over and COVID-19 death rate.
Table 3 also shows a positive relationship between COVID-19 cases and vaccinations. As discussed earlier, this could reflect the effect of higher infection rates on vaccination rollouts, as well as the potential confounding effects of more testing. The Opportunity Insights Economic Tracker dataset does not contain county-level COVID-19 test rates, though it seems probable that the case rate models (Models 1 to 3) may be partly explained by different levels of testing across counties, which could well be correlated with the same socio-demographic factors. Meanwhile, the protective effects of vaccines are clearly reflected in Models 4, 5, and 6, where vaccination rates are significantly negatively related to COVID-19 death rates (Table 3).
In addition to the OLS regression models, spatial lag and spatial error models are fitted to account for spatial autocorrelation between adjacent counties. As spatial autoregressive models on a large dataset are computationally intensive, instead of estimating all nine models across all 23 periods in Fig. 3, I estimated the models with COVID-19 case and death rates as the dependent variable for five representative periods (March 2020, August 2020, February 2021, August 2021, and January 2022) and the models with vaccination rates as the dependent variable, which only became available after January 2021, for four periods (February 2021, April 2021, August 2021, and January 2022). Table 4 summarizes the key coefficients from these models. The results are consistent with those from the OLS models. Digital exclusion, after the first several months of the pandemic, has been positively associated with COVID-19 case and death rates and negatively associated with vaccination rates.
Table 4.
Spatial regression models on digital access and COVID-19 outcomes.
| DV | IV | March 2020 | August 2020 | February 2021 | August 2021 | January 2022 | |
|---|---|---|---|---|---|---|---|
| Case rate | Spatial lag | % No Internet | 23.70*** (8.05) | 1910*** (350.8) | 4059*** (851.6) | 4937*** (995.4) | 4153*** (1269) |
| % No computer | 20.16* (10.33) | 2408*** (451.2) | 4249*** (1097) | 3173** (1255) | 1130 (−)a | ||
| % Broadband | −17.49** (6.97) | −1518*** (304.5) | −2052*** (741.5) | −2249*** (858.5) | −902.1 (843.4) | ||
| Spatial error | % No Internet | 29.66*** (8.64) | 1990*** (370.1) | 4507*** (902.3) | 5243*** (1052) | 4093*** (1497) | |
| % No computer | 24.64** (11.03) | 2398*** (473.9) | 4067*** (1157) | 3055** (1316) | 301.1 (1919) | ||
| % Broadband | −22.23*** (7.47) | −1493*** (320.8) | −2070*** (783.9) | −1995** (903.0) | −167.2 (1297) | ||
| Death rate | Spatial lag | % No Internet | −0.863 (0.607) | 32.73** (12.82) | 129.12*** (32.11) | 185.01*** (36.11) | 208.4*** (40.67) |
| % No computer | −0.574 (0.780) | 6.235 (16.49) | 98.83** (41.39) | 153.18*** (45.41) | 150.3*** (52.46) | ||
| % Broadband | 0.661 (0.526) | −3.424 (11.13) | −82.37*** (27.88) | −117.44*** (31.03) | −101.8*** (35.34) | ||
| Spatial error | % No Internet | −0.796 (0.629) | 34.81** (13.71) | 128.26*** (33.72) | 187.34*** (38.06) | 209.3*** (42.97) | |
| % No computer | −0.496 (0.806) | 6.86 (17.59) | 98.52** (43.28) | 154.59*** (47.57) | 151.7*** (55.13) | ||
| % Broadband | 0.563 (0.544) | −3.03 (11.88) | −79.56*** (29.21) | −113.29*** (32.57) | −99.59*** (37.23) | ||
| February 2021 | April 2021 | August 2021 | January 2022 | ||||
| Full vaccination rate | Spatial lag | % No Internet | −0.355 (1.051) | −7.638*** (2.147) | −8.933*** (3.157) | −6.904** (2.918) | |
| % No computer | 1.275 (1.352) | −7.953*** (2.764) | −9.172** (3.960) | −9.503** (3.746) | |||
| % Broadband | 0.894 (0.910) | 6.606*** (1.860) | 8.371*** (2.705) | 7.233*** (2.523) | |||
| Spatial error | % No Internet | −0.171 (1.119) | −7.194*** (2.289) | −7.082** (3.386) | −4.683 (3.104) | ||
| % No computer | 1.881 (1.429) | −7.015** (2.926) | −7.220* (4.210) | −7.608* (3.972) | |||
| % Broadband | 0.906 (0.965) | 6.728*** (1.975) | 7.469*** (2.883) | 5.985** (2.680) |
***: p < 0.01; **: p < 0.05; *: p < 0.1. All models include state fixed effects. Figures in parentheses are standard errors.
This model needs a smaller tol.solve parameter in the lagsarlm function to obtain the standard error for % no computer. The coefficient is not statistically significant. To keep the results in Table 4 consistent, here the coefficient using the same tol.solve value as other models is reported without a standard error.
4. Conclusion
The digital divide is becoming a more prominent driver of social exclusion and inequalities in the age of the COVID-19 pandemic. As researchers reexamine the digital divide and digital exclusion as a social determinant of health (Clare, 2021; Ramsetty and Adams, 2020), this study argues that digital exclusion could have direct and indirect impacts on pandemic outcomes such as COVID-19 incidence, mortality, and vaccination. Digital exclusion could limit individuals' and communities’ awareness and understanding of public health measures, obstruct preventative measures, and encourage or necessitate risky activities that lead to more coronavirus exposure. Using county-level data on digital access and COVID-19 case, death, and vaccination rates in the United States, I demonstrate that counties with a higher percentage of digitally excluded population have seen higher COVID-19 case and death rates throughout the pandemic and lower vaccination rates by late 2021 and early 2022, which can lead to increased vulnerability to future waves.
Using a series of monthly cross-sectional models, the study finds that the relationship between digital access and COVID-19 outcomes, especially the death rate, only appeared after the first few months of the pandemic and became stronger over time. Similarly, the vaccination rate did not show a clear linkage with home access to computer or Internet until April 2021, when the vaccines were first made available to all U.S. adults, though there was a small but statistically significant association between the percentage of population with broadband Internet subscriptions and the vaccination rate in January 2021, when vaccines were in short supply and often required high-speed Internet to locate and book even for eligible individuals. A number of other socio-demographic factors, such as the percentage of Hispanic population or renter occupied housing, are also shown to have changing relationships with COVID-19 outcomes over time. The temporal variation in these relationships reflect an evolving landscape of the pandemic, suggesting that understandings of the neighborhood determinants of COVID-19 incidence and mortality based on early data may need an update.
One of the first to empirically examine the linkage between the digital divide and COVID-19 outcomes, this study employs temporal analysis and spatial econometrics to provide robust evidence on how digital exclusion is related to disparities in health outcomes in the COVID-19 pandemic. Moreover, it proposes a theoretical framework on the pathways through which digital exclusion can lead to such disparities which is not only relevant to the U.S. under the current pandemic, but also pertinent to other parts of the world or to a future pandemic or epidemic. In a country with one of the highest prevalence of digital access, there remain substantial gaps between counties that are well connected and those that are poorly connected, with the latter experiencing much higher COVID-19 incidence and mortality and lagging behind in vaccination. These findings highlight the importance of digital inclusion and equity in bridging the widening health disparities in the U.S., as well as the pressing need to expand digital access and digital literacy in countries and regions with a greater digital divide.
Limited by data availability, the study does not account for different levels of testing or inconsistencies in reporting COVID-19 cases or deaths. Like other studies using COVID-19 metrics, findings regarding confirmed COVID-19 cases may be affected by testing rates (Omori et al., 2020). Furthermore, with the data sources and methodology used, this study cannot pinpoint which of the five predicted pathways played more important roles in shaping the linkage between the digital divide and COVID-19 outcomes. Nevertheless, the results do lend support to certain hypotheses. The strong association between digital exclusion and COVID-19 infections, for example, appeared very early in the pandemic, supporting the theory of increased exposure due to the inability to substitute face-to-face contact with remote options, the theory of lagged response due to lack of timely information or awareness, or the theory of challenges in acquiring PPE offline. The consistent negative relationship between digital exclusion and the vaccination rate, even after COVID vaccines were widely available and abundant in the U.S., may suggest that vulnerability to misinformation related to dependence on single, homogeneous sources of information could be at work. The relationship between digital exclusion and COVID-19 deaths, with case and vaccination rates controlled for, may suggest limited information of or access to treatment, misinformation regarding ineffective treatments, or the indirect effects of digital marginalization and isolation via impacting mental and overall health. Better understanding of the pathways would require more targeted studies designed specifically to test these hypotheses, including studies in different geographical contexts, on smaller spatial scales, or at the individual level.
Despite these limitations, the study raises important policy questions and points to directions for future research and practice. It calls upon governments, public health agencies, and healthcare providers to recognize the significant implications of digital exclusion and marginalization in a pandemic and direct more targeted effort and resources to digitally disadvantaged individuals and communities. For example, offline channels of education and outreach, including programs that distribute PPE, test kits, and early treatments should be expanded in communities with lower levels of digital access. It calls upon legislatures, regulators, and providers to reform digital platforms, especially those that often serve as the primary source of information for people with limited digital access and/or literacy, such as social media, to mitigate misinformation and information silos. More importantly, it calls for reforms and investments, through the Infrastructure Investment and Job Act and future actions, in more accessible and equitable Internet infrastructure and digital literacy education that close the gaps between the technology haves and have-nots, allowing every citizen to take full advantage of the technology progress to obtain accurate, timely information, acquire goods and services, maintain social and emotional support, and mitigate health risks in a pandemic.
Even as the current waves of new Omicron variants recede and governments relax containment measures, the impacts of the COVID-19 pandemic on vulnerable populations and communities are far from over. Further research is direly needed to better understand the implications of the digital divide on pandemic impacts and resilience, as well as timely actions to address the immediate challenges faced by the digitally disconnected. However, to reduce health disparities related to digital exclusion in the long term requires addressing the digital divide itself. Policy makers must recognize broadband Internet has become an essential service and critical infrastructure in the digital era and make the essential technologies accessible and affordable to all.
Footnotes
Full results available in the supplemental tables.
References
- Algan Y., Cohen D., Davoine E., Foucault M., Stantcheva S. Trust in scientists in times of pandemic: panel evidence from 12 countries. Proc. Natl. Acad. Sci. USA. 2021;118(40) doi: 10.1073/pnas.2108576118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkureishi M.A., Choo Z.-Y., Rahman A., Ho K., Benning-Shorb J., Lenti G.…Lee W.W. Digitally disconnected: qualitative study of patient perspectives on the digital divide and potential solutions. JMIR Hum. Factors. 2021;8(4) doi: 10.2196/33364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auxier B. 64% of Americans say social media have a mostly negative effect on the way things are going in the U.S. today. 2020. https://www.pewresearch.org/fact-tank/2020/10/15/64-of-americans-say-social-media-have-a-mostly-negative-effect-on-the-way-things-are-going-in-the-u-s-today/ Retrieved from.
- Azzopardi-Muscat N., Sørensen K. Towards an equitable digital public health era: promoting equity through a health literacy perspective. Eur. J. Publ. Health. 2019;29(Suppl. 3):13–17. doi: 10.1093/eurpub/ckz166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhala N., Curry G., Martineau A.R., Agyemang C., Bhopal R. Sharpening the global focus on ethnicity and race in the time of COVID-19. Lancet. 2020;395(10238):1673–1676. doi: 10.1016/S0140-6736(20)31102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodie G.D., Dutta M.J. Understanding health literacy for strategic health marketing: eHealth literacy, health disparities, and the digital divide. Health Market. Q. 2008;25(1-2):175–203. doi: 10.1080/07359680802126301. [DOI] [PubMed] [Google Scholar]
- Cheshmehzangi A., Zou T., Su Z. The digital divide impacts on mental health during the COVID-19 pandemic. Brain Behav. Immun. 2022;101:211–213. doi: 10.1016/j.bbi.2022.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R., Friedman J.N., Hendren N., Stepner M. 2020. The Economic Impacts of COVID-19: Evidence from a New Public Database Built Using Private Sector Data. Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho M., Kim K.M. Effect of digital divide on people with disabilities during the COVID-19 pandemic. Disabil. Health J. 2022;15(1) doi: 10.1016/j.dhjo.2021.101214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.-Y.S., Gaysynsky A., Cappella J.N. Where we go from here: health misinformation on social media. Am. J. Publ. Health. 2020;110(S3):S273–S275. doi: 10.2105/ajph.2020.305905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clare C.A. Telehealth and the digital divide as a social determinant of health during the COVID-19 pandemic. Netw. Model. Anal. Health Inf. Bioinf. 2021;10(1):26. doi: 10.1007/s13721-021-00300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine D., Gaskell J., Jennings W., Stoker G. Trust and the coronavirus pandemic: what are the consequences of and for trust? An early review of the literature. Polit. Stud. Rev. 2021;19(2):274–285. doi: 10.1177/1478929920948684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eruchalu C.N., Pichardo M.S., Bharadwaj M., Rodriguez C.B., Rodriguez J.A., Bergmark R.W.…Ortega G. The expanding digital divide: digital health access inequities during the COVID-19 pandemic in New York City. J. Urban Health. 2021;98(2):183–186. doi: 10.1007/s11524-020-00508-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang M.L., Canham S.L., Battersby L., Sixsmith J., Wada M., Sixsmith A. Exploring privilege in the digital divide: implications for theory, policy, and practice. Gerontol. 2019;59(1):e1–e15. doi: 10.1093/geront/gny037. [DOI] [PubMed] [Google Scholar]
- Ferreira G.B., Borges S. Media and misinformation in times of COVID-19: how people informed themselves in the days following the Portuguese declaration of the state of emergency. Journal. Media. 2020;1(1):108–121. https://www.mdpi.com/2673-5172/1/1/8 Retrieved from. [Google Scholar]
- Forenbacher I., Husnjak S., Cvitić I., Jovović I. Determinants of mobile phone ownership in Nigeria. Telecommun. Pol. 2019;43(7) [Google Scholar]
- Fowler G.A. Your best tips for hunting vaccine appointments online. Wash. Post. 2021 https://www.washingtonpost.com/technology/2021/02/12/covid-vaccine-appointment-websites/ Retrieved from. [Google Scholar]
- Gold J.A.W., Rossen L.M., Ahmad F.B., Sutton P., Li Z., Salvatore P.P.…Jackson B.R. Race, ethnicity, and age trends in persons who died from COVID-19 - United States, May-August 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(42):1517–1521. doi: 10.15585/mmwr.mm6942e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollwitzer A., Martel C., Brady W.J., Pärnamets P., Freedman I.G., Knowles E.D., Van Bavel J.J. Partisan differences in physical distancing are linked to health outcomes during the COVID-19 pandemic. Nat. Human Behav. 2020;4(11):1186–1197. doi: 10.1038/s41562-020-00977-7. [DOI] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Is the pandemic leading to a crisis of trust? Insights from an Italian nationwide study. Publ. Health. 2022;202:32–34. doi: 10.1016/j.puhe.2021.10.015. [DOI] [PubMed] [Google Scholar]
- Hamidian Jahromi A., Hamidianjahromi A. Why African Americans are a potential target for COVID-19 infection in the United States. J. Med. Internet Res. 2020;22(6) doi: 10.2196/19934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. ICT and the UN's sustainable development goal for education: using ICT to boost the math performance of immigrant youths in the US. Sustainability. 2018;10(12):4584. [Google Scholar]
- Lai J., Widmar N.O. Revisiting the digital divide in the COVID-19 era. Appl. Econ. Perspect. Pol. 2021;43(1):458–464. doi: 10.1002/aepp.13104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins Van Jaarsveld G. The effects of COVID-19 among the elderly population: a case for closing the digital divide. Front. Psychiatr. 2020:1211. doi: 10.3389/fpsyt.2020.577427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mena G.E., Martinez P.P., Mahmud A.S., Marquet P.A., Buckee C.O., Santillana M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science. 2021;372(6545) doi: 10.1126/science.abg5298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MIT Election Data and Science Lab County presidential election returns 2000-2020. 2018. Retrieved from: [DOI]
- Mitchell U.A., Chebli P.G., Ruggiero L., Muramatsu N. The digital divide in health-related technology use: the significance of race/ethnicity. Gerontol. 2019;59(1):6–14. doi: 10.1093/geront/gny138. [DOI] [PubMed] [Google Scholar]
- Nekmat E. Nudge effect of fact-check alerts: source influence and media skepticism on sharing of news misinformation in social media. Soc. Media Soc. 2020;6(1) doi: 10.1177/2056305119897322. [DOI] [Google Scholar]
- Omori R., Mizumoto K., Chowell G. Changes in testing rates could mask the novel coronavirus disease (COVID-19) growth rate. Int. J. Infect. Dis. 2020;94:116–118. doi: 10.1016/j.ijid.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020;35(8):785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal N., Kamal R., Cox C., Garfield R. The implications of COVID-19 for mental health and substance use. 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ Retrieved from.
- Ramsetty A., Adams C. Impact of the digital divide in the age of COVID-19. J. Am. Med. Inf. Assoc. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotondi V., Kashyap R., Pesando L.M., Spinelli S., Billari F.C. Leveraging mobile phones to attain sustainable development. Proc. Natl. Acad. Sci. USA. 2020;117(24):13413–13420. doi: 10.1073/pnas.1909326117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santhanam L. These ‘vaccine hunters’ are chasing down appointments for people who need them most. PBS. 2021 https://www.pbs.org/newshour/health/these-vaccine-hunters-are-chasing-down-appointments-for-people-who-need-them-most (Mar 24, 2021). Retrieved from. [Google Scholar]
- Seo H., Blomberg M., Altschwager D., Vu H.T. Vulnerable populations and misinformation: a mixed-methods approach to underserved older adults' online information assessment. New Media Soc. 2021;23(7):2012–2033. doi: 10.1177/1461444820925041. [DOI] [Google Scholar]
- Soriano C.R.R. Exploring the ICT and rural poverty reduction link: Community telecenters and rural livelihoods in Wu'an, China. Electron. J. Inf. Syst. Dev. Ctries. 2007;32(1):1–15. [Google Scholar]
- Sostero M., Milasi S., Hurley J., Fernandez-Macías E., Bisello M. Teleworkability and the COVID-19 crisis: a new digital divide? JRC working papers series on labour, education and technology. 2020 https://www.econstor.eu/bitstream/10419/231337/1/jrc-wplet202005.pdf Retrieved from. [Google Scholar]
- Sy K.T.L., Martinez M.E., Rader B., White L.F. Socioeconomic disparities in subway use and COVID-19 outcomes in New York City. Am. J. Epidemiol. 2021;190(7):1234–1242. doi: 10.1093/aje/kwaa277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas J., Barraket J., Wilson C.K., Cook K., Louie Y.M., Holcombe-James I.…MacDonald T. 2018. Measuring Australia's Digital Divide: the Australian Digital Inclusion Index 2018. [Google Scholar]
- Van Deursen A.J., Mossberger K. Any thing for anyone? A new digital divide in internet‐of‐things skills. Pol. Internet. 2018;10(2):122–140. [Google Scholar]
- Van Holm E.J., Wyczalkowski C.K., Dantzler P.A. Neighborhood conditions and the initial outbreak of COVID-19: the case of Louisiana. J. Publ. Health. 2021;43(2):219–224. doi: 10.1093/pubmed/fdaa147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasile C. Mental health and immunity (Review) Exp. Ther. Med. 2020;20(6):211. doi: 10.3892/etm.2020.9341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicario M.D., Bessi A., Zollo F., Petroni F., Scala A., Caldarelli G.…Quattrociocchi W. The spreading of misinformation online. Proc. Natl. Acad. Sci. USA. 2016;113(3):554–559. doi: 10.1073/pnas.1517441113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts G. COVID-19 and the digital divide in the UK. Lancet Digit. Health. 2020;2(8):e395–e396. doi: 10.1016/S2589-7500(20)30169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winslow J. America's digital divide. Trust Mag. 2019 https://www.pewtrusts.org/en/trust/archive/summer-2019/americas-digital-divide (September 2019). Retrieved from. [Google Scholar]
- Wittenberg C., Berinsky A.J., Persily N., Tucker J.A. Misinformation and its correction. Soc. Media Democr.: The state of the field, prospects for reform. 2020;163 [Google Scholar]
- World Health Organization COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. 2022. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide [Press release]. Retrieved from.
- Yu B., Ndumu A., Mon L.M., Fan Z. E-inclusion or digital divide: an integrated model of digital inequality. J. Doc. 2018 [Google Scholar]