Abstract
Background
Current guidelines recommend assessing the prognosis in high-risk upper tract urothelial carcinoma patients (UTUC) after surgery. However, no specific method is endorsed. Among the various prognostic models, nomograms represent an easy and accurate tool to predict the individual probability for a specific event. Therefore, identifying the best-suited nomogram for each setting seems of great interest to the patient and provider.
Objectives
To identify, summarize and compare postoperative UTUC nomograms predicting oncologic outcomes. To estimate the overall performance of the nomograms and identify the most reliable predictors. To create a reference tool for postoperative UTUC nomograms, physicians can use in clinical practice.
Design
A systematic review was conducted following the recommendations of Cochrane’s Prognosis Methods Group. Medline and EMBASE databases were searched for studies published before December 2021. Nomograms were grouped according to outcome measurements, the purpose of use, and inclusion and exclusion criteria. Random-effects meta-analyses were performed to estimate nomogram group performance and predictor reliability. Reference tables summarizing the nomograms’ important characteristics were created.
Results
The systematic review identified 26 nomograms. Only four were externally validated. Study heterogeneity was significant, and the overall Risk of Bias (RoB) was high. Nomogram groups predicting overall survival (OS), recurrence-free survival (RFS), and intravesical recurrence (IVR) had moderate discrimination accuracy (c-Index summary estimate with 95% confidence interval [95% CI] and prediction interval [PI] > 0.6). Nomogram groups predicting cancer-specific survival (CSS) had good discrimination accuracy (c-Index summary estimate with 95% CI and PI > 0.7). Advanced pathological tumor stage (≥ pT3) was the most reliable predictor of OS. Pathological tumor stage (≥ pT2), age, and lymphovascular invasion (LVI) were the most reliable predictors of CSS. LVI was the most reliable predictor of RFS.
Conclusions
Despite a moderate to good discrimination accuracy, severe heterogeneity discourages the uninformed use of postoperative prognostic UTUC nomograms. For nomograms to become of value in a generalizable population, future research must invest in external validation and assessment of clinical utility. Meanwhile, this systematic review serves as a reference tool for physicians choosing nomograms based on individual needs.
Systematic Review Registration
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=282596, identifier PROSPERO [CRD42021282596].
Keywords: UTUC, upper tract urothelial carcinoma, nomograms, prognostic models, oncologic outcome
1 Introduction
Upper tract urothelial carcinoma (UTUC) is a rare and biologically heterogeneous disease that accounts for less than five percent of all urothelial tumors (1). Given the disease’s heterogeneity, risk stratification leads the patient’s management.
Preoperative risk assessment guides the selection of treatment strategies in patients with localized disease, recommending kidney sparing surgery for low-risk (2) and radical nephroureterectomy for high-risk patients (3–6). Postoperative risk stratification decides on the administration of adjuvant chemotherapy and defines the follow-up strategy (7). For this purpose, the European Association of Urology guideline recommends using prognostic models (7). However, no specific model has been endorsed yet.
Improvements in postoperative patient counseling regarding adjuvant treatment are urgently needed. The POUT trial and Checkmate-274 provided evidence for a disease-free-survival benefit of adjuvant therapy (platin-based chemotherapy, nivolumab) (8–10). Conversely, IMvigor010, evaluating adjuvant immunotherapy with atezolizumab, failed to demonstrate any benefit (11). Patient risk stratification might explain these differences. The supplementary analysis of IMvigor010 showed that TNM-based risk stratification was insufficient in identifying patients in need of adjuvant treatment (12).
Among the various prognostic models, nomograms represent a user-friendly tool to predict a patient’s individual probability for a specific event, such as tumor recurrence or death (13–15). This information helps to individualize medical care and counsel patients based on evidence.
Over the past decades, various nomograms have been developed for postoperative UTUC patient counseling. However, there is no comprehensive overview to guide potential users regarding the utility or accuracy of these tools. It is, indeed, necessary to summarize the most reliable nomograms for clinical practice, identify those applicable for further research, and give suggestions for individual patient settings.
We performed a systematic review and meta-analyses on multivariable postoperative prognostic UTUC nomograms predicting oncological outcomes. Our secondary objectives were to outline and compare the nomograms, investigate their overall performance, identify the most reliable predictors, and provide physicians with a reference tool for clinical practice.
2 Material and Methods
We performed this review following the recommendations of the Cochrane Prognosis Methods Group (16). The review protocol was prospectively registered in PROSPERO (registration number: CRD42021282596).
2.1 Search Strategy
We used the CHARMS checklist for systematic reviews of prediction modeling studies and the PICOTS scheme to define the review question (17). We searched for all studies that included UTUC patients (P), where a multivariable prognostic nomogram was investigated (I), to predict the oncologic outcome (O) (overall survival [OS], cancer-specific survival [CSS], recurrence-free survival [RFS], or intravesical recurrence [IVR]) in a one, three, or five years period (T), and that can be used after surgery or at a specific time point along the further course of the disease (postoperative) (S). Surgery was defined as any surgery intended to remove the tumor entirely.
Studies were eligible if (I) they matched the research question and (II) presented data on the development and internal or external validation of a multivariable prognostic nomogram. The studies also had to present data on (III) the nomogram’s prediction accuracy and calibration. (IV) Only full-text manuscripts published in English were included.
We searched the electronic databases Medline and EMBASE for studies published before December 2021. The search string used is listed on the PROSPERO website.
2.2 Data Collection
2.2.1 Study Inclusion and Exclusion
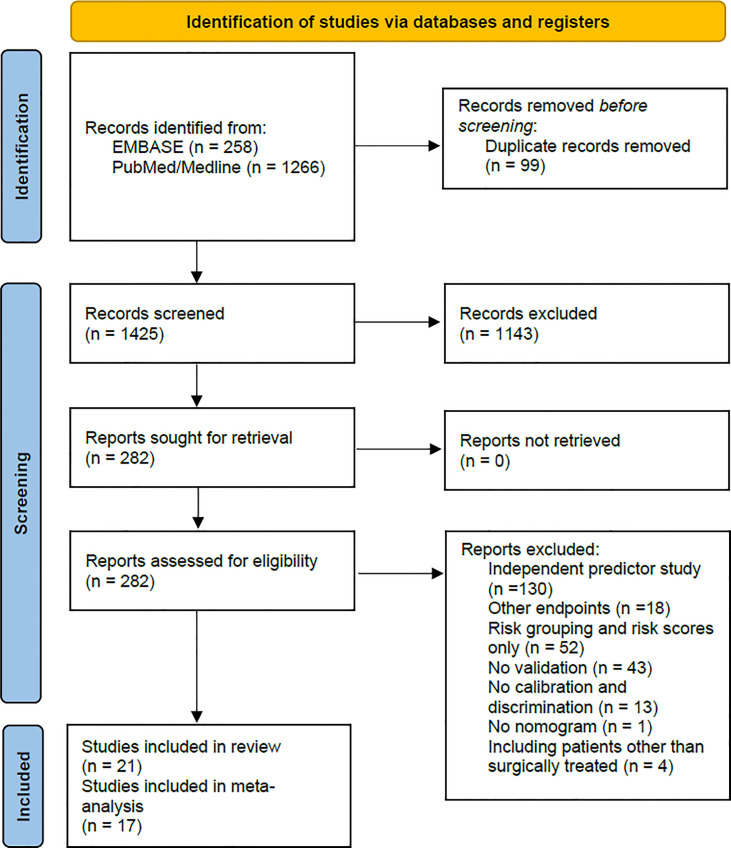
Two reviewers independently screened the titles and abstracts to identify eligible publications and performed a full-text review based on the inclusion criteria. Disagreements between the two reviewers were resolved in consensus with the co-authors. Figure 1 shows the PRISMA flow chart (18).
Figure 1.
This figure shows the PRISMA flow chart of the study selection process. From: Page et al. (18).
2.2.2 Data Extraction and Management
Two reviewers independently extracted the data to a predefined datasheet, and a third reviewer verified the accuracy of the extraction process. We extracted data from the following domains: overall information, paper information, source data, participant information, outcomes to be predicted, model development, model validation, sample size, predictors, model performance, internal validation, and external validation. Supplementary Table 1 lists the data extracted in detail.
2.2.3 Model Performance Measures to be Extracted
We assessed the performance of each nomogram by extracting the measures for discrimination (c-Index with 95% confidence intervals [CIs] and standard error [SE], area under the receiver operating curve) and calibration (calibration plot interpretation, observed/expected ratio) presented without validation, and on internal and external validation. We assessed the independent effect of each predictor by extracting the hazard ratio (HR) or the coefficient Beta with 95% CIs and SE presented in the final model.
2.2.4 Dealing With Missing Data
We calculated missing data of performance measures as recommended by Cochrane (16). The predictor’s Beta and Beta’s and HR’s SE were calculated with the given HR and the 95% CIs. Missing 95% CIs of HRs were calculated either with the SE or with the HR and its p-value (19). Missing 95% CIs and SE of the c-Index were calculated with the c-Index and the number of patients with and without events (20). All the corresponding authors were contacted in case of missing data.
2.3 Quality Assessment
2.3.1 Assessment of Risk of Bias
Two reviewers independently assessed the risk of bias (RoB) of the included studies, using the dedicated Prediction model Risk Of Bias ASessment Tool (PROBAST) (21), which considered four potential sources of bias and three of applicability. The results of the PROBAST analysis were reported for each domain (bias: low risk, high risk, unclear; applicability: low concern, high concern, unclear), and an overall score for RoB and applicability was given.
2.3.2 Assessment of Nomogram Heterogeneity
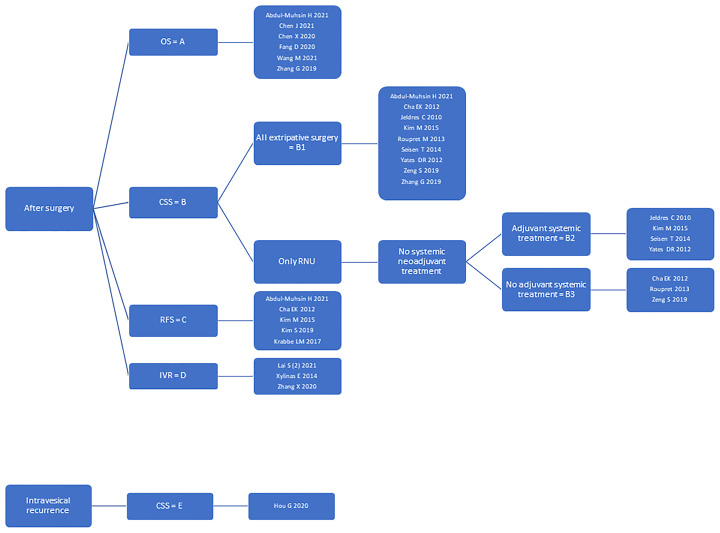
To account for nomogram heterogeneity, we stratified them into groups (A, B, C, D, E) regarding the purpose of use (after surgery or at the time of intravesical recurrence) and the outcomes to be predicted (OS or CSS or RFS or IVR). Group A included nomograms predicting OS, group B: CSS, group C: RFS, and group D: IVR after surgery. Group E included nomograms predicting CSS at the time of intravesical recurrence. We further stratified the nomograms from group B according to the surgical treatment (all types of surgery or radical nephroureterectomy only) and the patients’ baseline inclusion and exclusion criteria (neoadjuvant systemic treatment, adjuvant systemic treatment). Group B1 included nomograms for all types of surgery, whereas groups B2 and B3 included radical nephroureterectomy nomograms without systemic neoadjuvant treatment. Further, group B2 included nomograms with adjuvant and B3 without adjuvant systemic treatment. The nomogram groups were used for further statistical analysis. Figure 2 highlights the nomogram group stratification process and lists the nomograms within each group.
Figure 2.
This figure shows the nomogram group stratification process. Further, it lists all nomograms within each group.
2.4 Data Synthesis
2.4.1 Summary of Nomograms
We summarized the key findings of the included studies by giving (I) general information on the publication, (II) the nomogram’s purpose of use, (III) predicted outcomes, (IV) validation types, (V) inclusion and exclusion criteria of the study, (VI) essential patient characteristics, (VII) nomogram predictors, (VIII) nomogram performance (without validation, on internal validation, on external validation), (IX) and the RoB and applicability of the publication/nomogram.
2.4.2 Meta-Analysis Approach
We conducted the meta-analyses by nomogram groups due to the lack of validation studies and nomogram heterogeneity.
We investigated the overall performance of the nomogram groups by pooling the c-Index, which is a measure of discrimination accuracy. It accounts for censored data and is frequently used with survival data. Its value ranges between zero and one, with a value of 0.5 indicating prediction by chance (22). We set the cut-off values 0.6, 0.7, and 0.8 for moderate, good, and excellent nomogram discrimination accuracy. We included the c-Index that accounted best for the risk of overfitting in development studies: 1. Validation with an internal split cohort, 2. Validation with resampling by bootstrapping or cross-validation, 3. Development cohort without validation. We included the c-Index of all external validation studies.
We identified the most reliable predictors within each nomogram group by pooling Beta for predictors with a similar definition. The coefficient Beta is a measure of the predictor’s effect, and its value is independent of the measurement scale and therefore comparable among different variables. Positive values indicate a determinate effect, whereas negative values indicate a beneficial effect (23).
The number of three measurements (c-Index, Beta) was set as the lower limit for pooling. Therefore, we did not pool Beta within nomogram groups D and E and the c-Index for nomogram group E.
We used a Frequentist approach random-effects meta-analysis with the restricted maximum likelihood estimation and the Hartung-Knapp correction for calculating confidence intervals. If less than five studies were included, we additionally conducted a Bayesian approach random-effects meta-analysis. The meta-analyses results were plotted on a forest plot. The significance of the pooled summary estimate was assessed with the 95% CI, and the prediction interval (PI) verified its consistency. We used the statistical software R (v.4.0.5/2021) using the packages’ meta’ (24), ‘metafor’ (25), and ‘metamisc’ (20).
3 Results
3.1 Nomogram Search and Study Characteristics
From the 1524 records identified, we performed a full-text review of 282 articles and finally included 21 studies (26–46) for the systematic review and 17 studies (26–30, 32–35, 38–41, 43–46) for the meta-analyses. The full-text review excluded four studies that presented prognostic nomograms for UTUC patients receiving various treatments (surgery and/or radiotherapy and/or chemotherapy) (47–50). Nineteen studies presented nomogram development and internal validation data (26–35, 37, 39–46), of which two additionally presented external validation data of a separate nomogram (37, 44). Two studies presented external nomogram validation data only (36, 38). The development cohorts included 21,610 patients, and the internal split and external validation cohorts included 14167 patients. Patient data were collected in Asia in 11 (28–30, 33, 34, 36–38, 41, 44, 46), in North America in seven (26, 30–32, 41, 42, 45), in Europe in three (40, 42, 43), and worldwide in three (27, 35, 39) studies.
We identified 26 postoperative prognostic nomograms. All nomograms had been developed based on a cox-regression model. Table 1 gives a detailed overview of the studies and nomograms, taking study inclusion and exclusion criteria into consideration. Supplementary Table 2 lists the patient characteristics of development and validation studies in detail.
Table 1.
This table summarizes the publications included in the systematic review, highlighting nomogram prediction outcome, nomogram validation, and patient inclusion and exclusion criteria.
| GENERAL INFORMATION | ENDPOINTS | VALIDATION | INCLUSION / EXCLUSION CRITERIA | COMMENTS | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First author | Year | Purpose (FS = following surgery, IV = intravesical recurrence, V = validation) | Overall Survival | OS timeframe (years) | Cancer Specific Surival | CSS timeframe (years) | Recurrence Free Survival | RFS timeframe (years) | Intravesical Recurrence | IVR timeframe (months) | Internal Validation Bootstrapp-/Resampling | Internal Validation Split Cohort / 2nd Cohort | External Validation Paper | External Validation Paper Author / Year | I/E Radical Nephroureterectomy | I/E Surgery other than RNU | I/E Systemic Neoadjuvant Treatment | I/E Systemic Adjuvant Treatment | I/E Intravesical Adjuvant Treatment | I/E Systemtic Palliative Treatment | I/E Badder Cancer~ | I/E Contralateral UTUC~ | I/E Other Malignancy or Systemtic Disaese | other important I/E | Nomogram groups | Y = yes N = no NI = no information ~if specifically named / otherwise other malignancy |
| Abdul-Muhsin H | 2021 | FS | Y | 5 | Y | 5 | Y | 5 | N | N | Y | N | I | E | I | I | NI | NI | NI | NI | NI | E: no currative intent | A, B1, C | |||
| Cha EK | 2012 | FS | N | Y | 2; 5 | Y | 2; 5 | N | N | Y | Y | Zeng S 2019 | I | E | E | E | NI | NI | E* | NI | NI | B1, B3, C | *no previous MIBC | |||
| Chen J | 2021 | FS | Y | 3; 5 | N | N | N | N | Y | N | I | E | E | I | NI | NI | NI | NI | E | A | ||||||
| Chen X | 2020 | FS | Y | 3; 5 | N | N | N | Y | N | N | I | E | NI | NI | NI | NI | I | NI | E | A | ||||||
| Fang D | 2020 | FS | Y | 3; 5; 10 | N | N | N | N | Y | N | I | I | E | E | NI | NI | NI | E | NI | E: solitary kidney | A | |||||
| Hou G | 2020 | IV | N | Y | 1; 3; 5 | N | N | Y | N | N | I | E | NI | NI | NI | NI | E* | E | NI | E: systemic recurrence before intravesical recurrence; more than one intravesical recurrence | E | *no bladder cancer before RNU | ||||
| Jeldres C | 2010 | FS | N | Y | 5 | N | N | N | Y | N | I | E | NI | NI | NI | NI | NI | NI | NI | B1, B2 | ||||||
| Kim M | 2015 | FS | N | Y | 2; 5 | Y | 2; 5 | N | Y | N | N | I | E | E | I | NI | NI | E* | NI | E | B1, B2, C | *no previous MIBC | ||||
| Kim S | 2019 | FS | N | N | Y | 3 | N | Y | Y | N | I | E | E | I | NI | NI | I | E | NI | E: previous or concurrent radical cystectomy | C | |||||
| Krabbe LM | 2017 | FS | N | N | Y | 5 | N | Y | Y | N | I | I | NI | NI | NI | NI | I | NI | NI | E: low grade UTUC | C | |||||
| Ku J | 2013 | V | I | E | E | I | NI | NI | NI | NI | NI | E: previous or concurrent cystectomy | ||||||||||||||
| Lai S 1 | 2021 | V | I | E | E | I | NI | NI | E* | E | NI | *no previous or conocmittant muscle invasive bladder cancer | ||||||||||||||
| Lai S 2 | 2021 | FS | N | N | N | Y | 12; 36; 60 | Y | Y | N | I | E | NI | I | I | NI | E* | E | NI | D | *no synchronous baldder cancer, previous bladder cancer possible | |||||
| Roupret M | 2013 | FS | N | Y | 5 | N | N | Y | Y | N | I | E | E | E | NI | NI | E* | NI | NI | E: pT0 | B1, B3 | *exclusion history of muscle invasive bladder cancer | ||||
| Seisen T | 2014 | FS | N | Y | 5 | N | N | Y | Y | N | I | E | E | NI | NI | NI | E* | NI | NI | E: pTa, pT4, N 1-2, M1 | B1, B2 | *exclusion history of muscle invasive bladder cancer | ||||
| Wang M | 2021 | FS | Y | 1; 3; 5 | N | N | N | N | Y | N | I | I | I | I | I | I | E | NI | NI | Nomogram I: HG only, Nomogram II: LG only | A | |||||
| Xylinas E | 2014 | FS | N | N | N | Y | 3; 6; 12; 18; 24; 36 | N | Y | Y | Lai S 1 2021 Lai S 2 2021 | I | E | E | I | NI | NI | E* | NI | NI | D | *no previous muscle invasive bladder cancer and high grade non muscle invasive bladder cancer | ||||
| Yates DR | 2012 | FS | N | Y | 3; 5 | N | N | Y | Y | Y | Ku J 2013 | I | E | NI | NI | NI | NI | NI | NI | NI | B1, B2 | |||||
| Zeng S | 2019 | FS | N | Y | 3; 5 | N | N | Y | Y | N | I | E | E | E | NI | NI | I | NI | NI | B1, B3 | ||||||
| Zhang G | 2019 | FS | Y | 3; 5 | Y | 3; 5 | N | N | N | Y | N | I | I | NI | NI | NI | NI | NI | NI | E | A, B1 | |||||
| Zhang X | 2020 | FS | N | N | N | Y | 24; 48 | N | Y | N | I | E | E | I | I | NI | I | E | NI | E: pTa, pT4, N1-2, M1 | D | |||||
3.2 Nomogram Predictors
The median number of predictors used in the nomograms was 5.5 (Range 2-9). The most frequent predictors were pathological T-stage (n=21), age (n=17), pathological N-stage (n=16), tumor grade (n=12), and lymphovascular invasion (LVI) (n=11). In four nomograms, the reported HRs of the multivariable analysis and the assigned weights of the nomogram predictors did not match (42–44). Supplementary Table 3 gives the predictors of each nomogram in detail. Supplementary Table 4 summarizes the predictors most frequently used within each nomogram group.
3.3 Nomogram Performance Measures
The c-Index of development studies ranged from 0.657 (95% CI 0.560-0.755) (34) to 0.825 (95% CI 0.648-1) (41). Calibration plots of development studies showed moderate to good nomogram calibration, except for one nomogram (43).
The c-Index of external validation studies ranged from 0.683 (38, 42) to 0.742 (36, 43). A calibration plot of external validation was presented for only three nomograms (36–38, 42, 43). Nomogram calibration was good for two nomograms (37, 38, 42) but poor for the other (36, 43).
Neither development studies nor validation studies reported the observed/expected ratio. Table 2 outlines the performance measures reported for the nomograms.
Table 2.
This table gives a detailed overview of the performance of the nomograms (discrimination = c-Index, and calibration = interpretation of the calibration plot) on development and validation studies.
| INFORMATION | Abdul-Muhsin H | Cha EK | Chen J | Chen X | Fang D | Hou G | Jeldres C | Kim M | Kim S | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2021 | 2012 | 2021 | 2020 | 2020 | 2020 | 2010 | 2015 | 2019 | ||||||||||||||
| OUTCOME / GROUP | Overall survival | Cancer Specific Survival | Metasatasis Free Survival | Cancer Specific Surival | Recurrence Free Survival | Overall Survival | Overall Survival | Overall Survival | Cancer Specific Survival | Cancer Specific Survival | Cancer Specific Survival | Recurrence Free Survival | Recurrence Free Survival | |||||||||
| A | B1 | C | B1, B3 | C | A | A | A | E | B1, B2 | B1, B2 | C | C | ||||||||||
| RESULTS | c-Index Development Paper¹ | 0.784 | 0.714 | 0.753 | 0.815 | 0.768 | 0,804 (95%CI 0,713-0,895) | 0.82 | 0,698 0,724 | NI | 0,753 | 0,802 (95%CI 0,752-0,851) | 0,788 (95%CI 0,73-0,826) | 0,657 (95%CI 0,560-0,755) | ||||||||
| c-Index External Validation | NI | NI | NI | 0,69 0,7 | NI | NI | NI | NI | NI | NI | NI | NI | NI | |||||||||
| Calibration Plot Development Paper Interpretation Authors 3 years / 5 years (+/~/-)1,2 | NI / + | NI / + | NI / + | NI / + | NI / + | NI / + | + / + | ~ / NI | + / + | NI / + | NI / + | NI / + | + / NI | |||||||||
| Calibration Plot External Validation Interpretation Authors 3 years / 5 years (+/~/-)² | NI | NI | NI | NI / NI | NI | NI | NI | NI | NI | NI | NI | NI | NI | |||||||||
| INFORMATION | Krabbe LM | Lai S 2 | Roupret M | Seisen T | Wang M | Xylinas E | Yates DR | Zeng S | Zhang G | Zhang X | ||||||||||||
| 2017 | 2021 | 2013 | 2014 | 2021 | 2014 | 2012 | 2019 | 2019 | 2020 | |||||||||||||
| OUTCOME / GROUP | Recurrence Free Survival | Intravesical Recurrence | Cancer Specific Survival | Cancer Specific Survival | HG Group Overall Survival | LG Group Overall Survival | Intravesical Recurrence Full Model | Intravesical Recurrence Reduced Modell | Cancer Specific Survival | Cancer Specific Survival | Overall Survival | Cancer Specific Survival | No Intravesical Recurrence | |||||||||
| C | D | B1, B3 | B1, B2 | A | A | D | D | B1, B2 | B1, B3 | A | B1 | D | ||||||||||
| RESULTS | c-Index Development Paper¹ | 0,76 (±0,012) | NI | 0,79 (95% CI 0,75-0,83) | 0,8 (95%CI 0,76-0,84) | 0,729 (95%CI 0,707-0,750) 0,763 (95% CI 0,656-0,869) | 0,731 (95%CI 0,67-0,791) 0,825 (95%CI 0,648-1) | 0.69 | 0.678 | 0.78 | 0,73 (95%CI 0,59-0,87) | 0,702 (95%CI 0,684-0,720) | 0,771 (95%CI 0,746-0,796) | 0,678 (95%CI 0,583-0,772) | ||||||||
| c-Index External Validation | NI | NI | NI | NI | NI | NI | 0.684 | 0.683 | 0.742 | NI | NI | NI | NI | |||||||||
| Calibration Plot Development Paper Interpretation Authors 3 years / 5 years (+/~/-)1,2 | NI / ~ | + / NI + / NI | NI / ~ | NI / + | + / + | + / + | + / NI | + / NI | + / - | ~ / ~ | + / + | + / + | + / NI | |||||||||
| Calibration Plot External Validation Interpretation Authors 3 years / 5 years (+/~/-)² | NI | NI | NI | NI | NI | NI | + / NI + / NI | + / NI | - / - | NI | NI | NI | NI | |||||||||
¹We only report the c-Index/calibration plot accounting best for overfitting (split cohort validation > bootstrapping/resample validation > development cohort).
²If calibration plot was given but without interpretation from the authors, the reviewers interpreted the calibration plot. NI, no information given.
3.4 Nomogram Reference Tool
Figure 2 , Tables 1 , 2 , and Supplementary Tables 2 , 3 represent a reference tool for postoperative UTUC nomograms. As a first step, Figure 2 shall be used to identify nomograms predicting the outcome of interest. As a second step, Table 1 needs to be checked for inclusion and exclusion criteria to be considered. If more than one nomogram is applicable, Table 2 can be used to compare the nomogram’s diagnostic accuracy and calibration presented on internal and external validation cohorts. As the last step, Supplementary Tables 2 , 3 can be checked to evaluate whether the patient’s characteristics align with the nomogram’s development and validation cohort and whether the predictors are readily available. Using this stepwise approach, physicians can choose a nomogram that fits the individual patient’s needs.
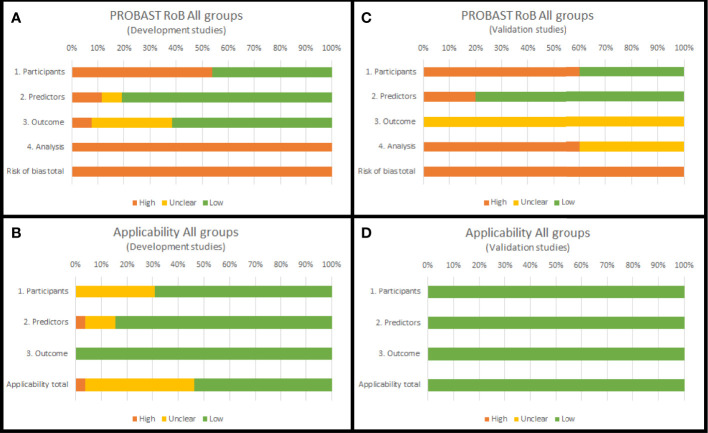
3.5 Risk of Bias Assessment of Included Studies
For development studies, overall RoB was high in 100% of the studies. RoBs mainly were due to inconsistencies in the analysis (100%) and participants domains (54%). Most predictors were selected based on the results of a univariable analysis, and the complexity of the data was not considered. Moreover, the data source and patient inclusion and exclusion criteria had a high RoB. Overall applicability of development studies was unclear in 42% of the studies, mainly due to inconsistencies in the participants (31%) and predictors (11%) domains.
For validation studies, overall RoB was high in 100% of the studies. RoBs mainly were due to inconsistencies in the analysis (60%) and participants (60%) domains. All studies validated the nomograms with retrospective cohorts, and in most cases, this resulted in a high RoB. Furthermore, most validation studies did not report handling of missing data and did not update the nomograms. Overall, the applicability of the validation studies was good.
Figure 3 summarizes the PROBAST assessment of nomogram development and validation studies. Supplementary Table 5 reports the PROBAST assessment of all nomograms.
Figure 3.
PROBAST summary (RoB domains and applicability domains) for all nomogram development (A, B) and validation studies (C, D) included in this systematic review.
3.6 Meta-Analyses
3.6.1 Pooled Predictor Coefficient Beta
Advanced pathological T-stage (≥ pT3) was a significant and consistent negative predictor (Beta summary estimate with 95%CI and PI > 0) of OS (Nomogram group A). Age, pathological T-stage (≥ pT2), and LVI were significant negative predictors (Beta summary estimate with 95%CI and PI > 0) of CSS (Nomogram group B1). LVI was a significant and consistent negative predictor (Beta summary estimate with 95%CI and PI > 0) of RFS (Nomogram group C). CSS subgroups B2 and B3 had no significant and consistent predictors. The maximum number of coefficients pooled per predictor was six. See Supplementary Figures 1 – 5 .
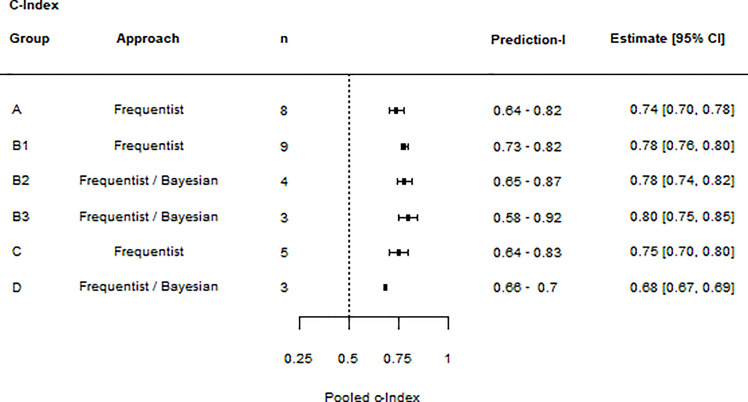
3.6.2 Pooled c-Index
Nomograms predicting OS (Nomogram group A), RFS (Nomogram group C), and IVR (Nomogram group D) had a significant and consistent moderate discrimination accuracy (c-Index with 95%CI and PI > 0.6). Nomograms predicting CSS (Nomogram group B1) had a significant and consistent good discrimination accuracy (c-Index with 95%CI and PI >0.7). CSS subgroup B2, but not B3, had a significant and consistent moderate discrimination accuracy (c-Index with 95%CI and PI >0.6). The maximum number of c-Indexes pooled per nomogram group was nine. See Figure 4 .
Figure 4.
Summary forest plot of c-Index meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the nomogram group, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
4 Discussion
The discrepancy between nomogram development and external validation studies was high. Out of 26 nomograms, only four had been externally validated with a maximum of two validation cohorts. Indeed, the lack of external validation is a significant drawback for generalizability and discourages the uninformed use of nomograms in clinical practice. A common problem seen for prognostic model studies, as their five-year validation rate was shown to be only 16% (51).
We found that patients’ baseline characteristics varied widely between the studies. Patients had been recruited across different periods and continents and received varying treatment regimens. The increasing incidence of primary metastatic disease might have influenced nomograms’ predictions (52, 53). However, oncologic outcomes remained unchanged throughout the last decades (52). Further, the extent of surgical treatment can impact oncologic outcomes, either by increasing the risk of incomplete tumor resection or by selecting patients with favorable pathology (2). This is of particular importance, as previous studies highlighted the inaccuracy of preoperative staging (54). Even patients with relatively small tumors are at risk of muscle-invasive or even non–organ-confined disease (55). Similarly, excluding perioperative chemotherapy might select patients with favorable pathology or those unfit to receive the treatment. More importantly, it directly impacts the outcome (56). Heterogeneity in patient characteristics and its impact on oncologic outcomes is also a major drawback for the generalizability of these nomograms.
There were critical methodological weaknesses in the nomogram development studies. The data source mainly was from retrospective cohorts, which bears the risk of selection bias. Moreover, all development studies had a high RoB in the analysis domain. The nomograms might have been fitted to the characteristics of the development cohorts instead of a generalizable patient collective. In addition, no nomogram considered competing risks, which can cause an overestimation of the true event rate (57). Unfortunately, these limitations affect the reliability of the nomograms’ outcomes.
The meta-analyses identified several reliable nomogram predictors. Advanced pathological T-stage (≥pT3) predicted OS. Pathological T-stage (≥pT2), age, and LVI predicted CSS. LVI predicted RFS. These predictors were already known as individual risk factors (3, 58, 59). However, we elaborated that they retain their validity when combined, such as in a nomogram. Integrating novel biomarkers, reflecting the biological and clinical behavior of the tumor’s environment, could further improve the nomograms’ accuracy. So far, they have barely been considered.
The meta-analyses identified moderate discrimination accuracy for nomograms predicting OS, RFS, and IVR. Further, it identified good discrimination accuracy for nomograms predicting CSS. Because it was impossible to pool the c-Index of each nomogram separately, we could not identify the most accurate nomogram to be used in clinical practice. Instead, our analyses demonstrated the overall potential of postoperative prognostic UTUC nomograms, which justifies the effort for further research.
This systematic review highlights the critical absence of external validation studies, limiting nomograms’ applicability and uninformed use. Furthermore, it outlines that information on the clinical utility is scarce. Whether patients benefit from using nomograms remains unreported. However, improvements in postoperative risk stratification are urgently needed. Although the POUT trial and, most recently, Checkmate-274 demonstrated improved disease-free survival with adjuvant systemic therapy (platinum-based chemotherapy; nivolumab) in high-risk patients (10, 56), IMvigor010 failed to demonstrate any benefit (atezolizumab) (11). Further, the study raised concerns about postoperative TNM-based risk stratification (12). Therefore, future studies should focus on assessing the nomograms’ clinical utility and whether they can identify patients most suitable for adjuvant treatment.
This systematic review outlined similarities and differences between postoperative prognostic UTUC nomograms. Further, it provides physicians with a reference tool, enabling them to choose nomograms based on their individual needs and easily implement nomograms into clinical practice. For example, when searching for a nomogram predicting the five-year CSS following RNU, physicians can decide between the nomograms of Cha EK et al. (27) and Yates DR. et al. (43), as both have been externally validated. Further, they can decide whether to choose a nomogram taking the effects of adjuvant chemotherapy into account. As the last step, they can check whether the patient’s characteristics align with the patient cohort used for nomogram development or validation and whether the predictors are readily available. The reference tool will promote the widespread use of nomograms in postoperative UTUC patient counseling.
This study is the first systematic review summarizing postoperative prognostic UTUC nomograms. We set a standard for study quality, excluding all without internal validation data nor presenting discrimination and calibration accuracy. Although we used this most rigorous method, the approach could have missed potential nomograms. We estimated the nomograms’ and predictors’ overall predictive value by summarizing the c-Index and the coefficient Beta. Nevertheless, we could not estimate the overall nomogram calibration because the observed/expected rates were missing. However, calibration is essential to assess the benefit for clinical practice (60). We accounted for heterogeneity within the meta-analyses by stratifying nomograms into distinct groups. As a result, the number of studies included per analysis was low. Moreover, despite contacting all the corresponding authors in case of lacking results descriptions, our analyses were limited by missing values.
5 Conclusions
Despite a moderate to good discrimination accuracy, severe heterogeneity discourages the uninformed use of postoperative prognostic UTUC nomograms. For nomograms to become of value in a generalizable population, future research must invest in external validation and assessment of clinical utility. Meanwhile, this systematic review serves as a reference tool for physicians choosing nomograms based on individual needs.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Author Contributions
MP contributed to protocol/project development/management, data collection and management, data analysis and interpretation, and manuscript writing/editing. FK contributed to data collection and management, data interpretation, and manuscript writing/editing. AA, DD, EL, EX, FS, FQ, HM, LL, MRi, MRo, NS, PIK, PR, RSM, TK, TY, VM, and YL contributed to data interpretation and manuscript writing/editing. SFS contributed to protocol/project development/management, data interpretation, and manuscript writing/editing. BP contributed to protocol/project development/management, data collection and management, data interpretation, and manuscript writing/editing. All authors contributed to the article and approved the submitted version.
funding
The author PR is supported by a EUSP Scholarship from the European Association of Urology.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer DE declared a shared affiliation with the author EL to the handling editor at the time of review.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.907975/full#supplementary-material
Supplementary Table S1 lists the data extracted from the original publications.
Supplementary Table S2 lists the patient characteristics of nomogram development and validation cohorts in detail.
Supplementary Table S3 lists the predictors included within each nomogram in detail.
Supplementary Table S4 summarizes the predictors most frequently used with each nomogram group
Supplementary Table S5 gives a detailed overview of the nomograms’/studies’ RoB, giving RoB and applicability for each domain.
Summary forest plot of nomogram group A predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group B1 predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group B2 predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group B3 predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group C predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Abbreviations
CI, Confidence Interval; CSS, Cancer-Specific Survival; HR, Hazard Ratio; IVR, Intravesical Recurrence; LVI, Lymphovascular Invasion; OS, Overall Survival; PI, Prediction Interval; PROBAST, Prediction model Risk Of Bias ASessment Tool; RFS, Recurrence-Free Survival; RoB, Risk of Bias; SE, Standard Error; UTUC, Upper Tract Urothelial Carcinoma.
References
- 1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin (2021) 71(1):7–33. doi: 10.3322/caac.21654 [DOI] [PubMed] [Google Scholar]
- 2. Seisen T, Peyronnet B, Dominguez-Escrig JL, Bruins HM, Yuan CY, Babjuk M, et al. Oncologic Outcomes of Kidney-Sparing Surgery Versus Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma: A Systematic Review by the EAU Non-Muscle Invasive Bladder Cancer Guidelines Panel. Eur Urol (2016) 70(6):1052–68. doi: 10.1016/j.eururo.2016.07.014 [DOI] [PubMed] [Google Scholar]
- 3. Margulis V, Shariat SF, Matin SF, Kamat AM, Zigeuner R, Kikuchi E, et al. Outcomes of Radical Nephroureterectomy: A Series From the Upper Tract Urothelial Carcinoma Collaboration. Cancer (2009) 115(6):1224–33. doi: 10.1002/cncr.24135 [DOI] [PubMed] [Google Scholar]
- 4. Favaretto RL, Shariat SF, Savage C, Godoy G, Chade DC, Kaag M, et al. Combining Imaging and Ureteroscopy Variables in a Preoperative Multivariable Model for Prediction of Muscle-Invasive and non-Organ Confined Disease in Patients With Upper Tract Urothelial Carcinoma. BJU Int (2012) 109(1):77–82. doi: 10.1111/j.1464-410X.2011.10288.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chromecki TF, Cha EK, Fajkovic H, Margulis V, Novara G, Scherr DS, et al. The Impact of Tumor Multifocality on Outcomes in Patients Treated With Radical Nephroureterectomy. Eur Urol (2012) 61(2):245–53. doi: 10.1016/j.eururo.2011.09.017 [DOI] [PubMed] [Google Scholar]
- 6. Favaretto RL, Shariat SF, Chade DC, Godoy G, Adamy A, Kaag M, et al. The Effect of Tumor Location on Prognosis in Patients Treated With Radical Nephroureterectomy at Memorial Sloan-Kettering Cancer Center. Eur Urol (2010) 58(4):574–80. doi: 10.1016/j.eururo.2010.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur Urol (2021) 79(1):62–79. doi: 10.1016/j.eururo.2020.05.042 [DOI] [PubMed] [Google Scholar]
- 8. Birtle A, Johnson M, Chester J, Jones R, Dolling D, Bryan RT, et al. Adjuvant Chemotherapy in Upper Tract Urothelial Carcinoma (the POUT Trial): A Phase 3, Open-Label, Randomised Controlled Trial. Lancet (2020) 395(10232):1268–77. doi: 10.1016/S0140-6736(20)30415-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Birtle AJ, Chester JD, Jones RJ, Jenkins B, Johnson M, Catto JW, et al. Updated Outcomes of POUT: A Phase III Randomized Trial of Peri-Operative Chemotherapy Versus Surveillance in Upper Tract Urothelial Cancer (UTUC). J Clin Oncol (2021) 39(6_suppl):455–5. doi: 10.1200/JCO.2021.39.6_suppl.455 [DOI] [Google Scholar]
- 10. Bajorin DF, Witjes JA, Gschwend JE, Schenker M, Valderrama BP, Tomita Y, et al. Adjuvant Nivolumab Versus Placebo in Muscle-Invasive Urothelial Carcinoma. N Engl J Med (2021) 384(22):2102–14. doi: 10.1056/NEJMoa2034442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bellmunt J, Hussain M, Gschwend JE, Albers P, Oudard S, Castellano D, et al. Adjuvant Atezolizumab Versus Observation in Muscle-Invasive Urothelial Carcinoma (IMvigor010): A Multicentre, Open-Label, Randomised, Phase 3 Trial. Lancet Oncol (2021) 22(4):525–37. doi: 10.1016/S1470-2045(21)00004-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Powles T, Assaf ZJ, Davarpanah N, Banchereau R, Szabados BE, Yuen KC, et al. ctDNA Guiding Adjuvant Immunotherapy in Urothelial Carcinoma. Nature (2021) 595(7867):432–7. doi: 10.1038/s41586-021-03642-9 [DOI] [PubMed] [Google Scholar]
- 13. Iasonos A, Schrag D, Raj GV, Panageas KS. How to Build and Interpret a Nomogram for Cancer Prognosis. J Clin Oncol (2008) 26(8):1364–70. doi: 10.1200/JCO.2007.12.9791 [DOI] [PubMed] [Google Scholar]
- 14. Lughezzani G, Briganti A, Karakiewicz PI, Kattan MW, Montorsi F, Shariat SF, et al. Predictive and Prognostic Models in Radical Prostatectomy Candidates: A Critical Analysis of the Literature. Eur Urol (2010) 58(5):687–700. doi: 10.1016/j.eururo.2010.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shariat SF, Kattan MW, Vickers AJ, Karakiewicz PI, Scardino PT. Critical Review of Prostate Cancer Predictive Tools. Future Oncol (2009) 5(10):1555–84. doi: 10.2217/fon.09.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Debray TP, Damen JA, Snell KI, Ensor J, Hooft L, Reitsma JB, et al. A Guide to Systematic Review and Meta-Analysis of Prediction Model Performance. BMJ (2017) 356:i6460. doi: 10.1136/bmj.i6460 [DOI] [PubMed] [Google Scholar]
- 17. Moons KG, de Groot JA, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical Appraisal and Data Extraction for Systematic Reviews of Prediction Modelling Studies: The CHARMS Checklist. PloS Med (2014) 11(10):e1001744. doi: 10.1371/journal.pmed.1001744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ (2021) 372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Altman DG, Bland JM. How to Obtain the Confidence Interval From a P Value. BMJ (2011) 343:d2090. doi: 10.1136/bmj.d2090 [DOI] [PubMed] [Google Scholar]
- 20. Debray TP, Damen JA, Riley RD, Snell K, Reitsma JB, Hooft L, et al. A Framework for Meta-Analysis of Prediction Model Studies With Binary and Time-To-Event Outcomes. Stat Methods Med Res (2019) 28(9):2768–86. doi: 10.1177/0962280218785504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moons KGM, Wolff RF, Riley RD, Whiting PF, Westwood M, Collins GS, et al. PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann Intern Med (2019) 170(1):W1–W33. doi: 10.7326/M18-1377 [DOI] [PubMed] [Google Scholar]
- 22. Harrell FE, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the Yield of Medical Tests. JAMA (1982) 247(18):2543–6. doi: 10.1001/jama.247.18.2543 [DOI] [PubMed] [Google Scholar]
- 23. George B, Seals S, Aban I. Survival Analysis and Regression Models. J Nucl Cardiol (2014) 21(4):686–94. doi: 10.1007/s12350-014-9908-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Balduzzi S, Rücker G, Schwarzer G. How to Perform a Meta-Analysis With R: A Practical Tutorial. Evidence-Based Ment Health (2019) 22:153–60. doi: 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Viechtbauer W. Conducting Meta-Analyses in R With the Metafor Package. J Stat Software (2010) 36(3):1–48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 26. Abdul-Muhsin H, De Lucia N, Singh V, Faraj K, Rose K, Cha S, et al. Outcome Prediction Following Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma. Urol Oncol (2021) 39(2):133.e9–133.e16. doi: 10.1016/j.urolonc.2020.08.021 [DOI] [PubMed] [Google Scholar]
- 27. Cha EK, Shariat SF, Kormaksson M, Novara G, Chromecki TF, Scherr DS, et al. Predicting Clinical Outcomes After Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma. Eur Urol (2012) 61(4):818–25. doi: 10.1016/j.eururo.2012.01.021 [DOI] [PubMed] [Google Scholar]
- 28. Chen J, Zhong W, Yang M, Hou W, Wang X, Xia K, et al. Development and Validation of a PD-L1/PD-1/CD8 Axis-Based Classifier to Predict Cancer Survival of Upper Tract Urothelial Carcinoma After Radical Nephroureterectomy. Cancer Immunol Immunother (2021) 70(9):2657–68. doi: 10.1007/s00262-020-02827-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen X, Ji H, Wang J, Zhao G, Zheng B, Niu Z, et al. Prognostic Value of the Preoperative Plasma D-Dimer Levels in Patients With Upper Tract Urothelial Carcinoma in a Retrospective Cohort Study. Onco Targets Ther (2020) 13:5047–55. doi: 10.2147/OTT.S254514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fang D, Singla N, Bao Z, Jafri SM, Su X, Cao Z, et al. The Significance of Preoperative Serum Sodium and Hemoglobin in Outcomes of Upper Tract Urothelial Carcinoma: Multi-Center Analysis Between China and the United States. Cancer Manag Res (2020) 12:9825–36. doi: 10.2147/CMAR.S267969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hou G, Zheng Y, Zhang L, Lai D, Wang F, Li X, et al. Development and Validation of a Prognostic Nomogram for Patients With Intravesical Recurrence After Radical Nephroureterectomy for Non-Metastatic Upper Tract Urothelial Carcinoma. World J Urol (2020) 38(8):1969–75. doi: 10.1007/s00345-019-02985-3 [DOI] [PubMed] [Google Scholar]
- 32. Jeldres C, Sun M, Lughezzani G, Isbarn H, Shariat SF, Widmer H, et al. Highly Predictive Survival Nomogram After Upper Urinary Tract Urothelial Carcinoma. Cancer (2010) 116(16):3774–84. doi: 10.1002/cncr.25122 [DOI] [PubMed] [Google Scholar]
- 33. Kim M, Moon KC, Choi WS, Jeong CW, Kwak C, Kim HH, et al. Prognostic Value of Systemic Inflammatory Responses in Patients With Upper Urinary Tract Urothelial Carcinoma. World J Urol (2015) 33(10):1439–57. doi: 10.1007/s00345-015-1484-9 [DOI] [PubMed] [Google Scholar]
- 34. Kim SH, Song MK, Hong B, Kang SH, Jeong BC, Ku JH, et al. Developing a Prediction Model for Disease-Free Survival From Upper Urinary Tract Urothelial Carcinoma in the Korean Population. Cancer Med (2019) 8(11):4967–75. doi: 10.1002/cam4.2382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Krabbe LM, Eminaga O, Shariat SF, Hutchinson RC, Lotan Y, Sagalowsky AI, et al. Postoperative Nomogram for Relapse-Free Survival in Patients With High Grade Upper Tract Urothelial Carcinoma. J Urol (2017) 197(3 Pt 1):580–9. doi: 10.1016/j.juro.2016.09.078 [DOI] [PubMed] [Google Scholar]
- 36. Ku JH, Moon KC, Jung JH, Jeong SH, Kwak C, Kim HH. External Validation of an Online Nomogram in Patients Undergoing Radical Nephroureterectomy for Upper Urinary Tract Urothelial Carcinoma. Br J Cancer (2013) 109(5):1130–6. doi: 10.1038/bjc.2013.462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lai S, Long X, Wu P, Liu J, Seery S, Hou H, et al. Developing a Nomogram for Predicting Intravesical Recurrence After Radical Nephroureterectomy: A Retrospective Cohort Study of Mainland Chinese Patients. Jpn J Clin Oncol (2021) 51(7):1132–41. doi: 10.1093/jjco/hyab017 [DOI] [PubMed] [Google Scholar]
- 38. Lai S, Wu P, Diao T, Seery S, Liu J, Hou H, et al. Does Xylinas' Nomogram Accurately Predict Intravesical Recurrence Risk After Radical Nephroureterectomy for Primary Upper Urinary Tract Urothelial Carcinoma When Applied to Asian Populations? Jpn J Clin Oncol (2021) 51(3):469–77. doi: 10.1093/jjco/hyaa138 [DOI] [PubMed] [Google Scholar]
- 39. Rouprêt M, Hupertan V, Seisen T, Colin P, Xylinas E, Yates DR, et al. Prediction of Cancer Specific Survival After Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma: Development of an Optimized Postoperative Nomogram Using Decision Curve Analysis. J Urol (2013) 189(5):1662–9. doi: 10.1016/j.juro.2012.10.057 [DOI] [PubMed] [Google Scholar]
- 40. Seisen T, Colin P, Hupertan V, Yates DR, Xylinas E, Nison L, et al. Postoperative Nomogram to Predict Cancer-Specific Survival After Radical Nephroureterectomy in Patients With Localised and/or Locally Advanced Upper Tract Urothelial Carcinoma Without Metastasis. BJU Int (2014) 114(5):733–40. doi: 10.1111/bju.12631 [DOI] [PubMed] [Google Scholar]
- 41. Wang M, Ren X, Wang G, Sun X, Tang S, Zhang B, et al. Construction of a Survival Prediction Model for High-And Low -Grade UTUC After Tumor Resection Based on "SEER Database": A Multicenter Study. BMC Cancer (2021) 21(1):999. doi: 10.1186/s12885-021-08742-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Xylinas E, Kluth L, Passoni N, Trinh QD, Rieken M, Lee RK, et al. Prediction of Intravesical Recurrence After Radical Nephroureterectomy: Development of a Clinical Decision-Making Tool. Eur Urol (2014) 65(3):650–8. doi: 10.1016/j.eururo.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 43. Yates DR, Hupertan V, Colin P, Ouzzane A, Descazeaud A, Long JA, et al. Cancer-Specific Survival After Radical Nephroureterectomy for Upper Urinary Tract Urothelial Carcinoma: Proposal and Multi-Institutional Validation of a Post-Operative Nomogram. Br J Cancer (2012) 106(6):1083–8. doi: 10.1038/bjc.2012.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zeng S, Dai L, Yang J, Gao X, Yu X, Ren Q, et al. Development and External Validation of a Nomogram Predicting Prognosis of Upper Tract Urothelial Carcinoma After Radical Nephroureterectomy. Urol Oncol (2019) 37(4):290.e17–290.e24. doi: 10.1016/j.urolonc.2018.12.027 [DOI] [PubMed] [Google Scholar]
- 45. Zhang GL, Zhou W. A Model for the Prediction of Survival in Patients With Upper Tract Urothelial Carcinoma After Surgery. Dose Response (2019) 17(4):1559325819882872. doi: 10.1177/1559325819882872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhang X, Bu R, Liu Z, Wu B, Bai S. Development and Validation of a Model for Predicting Intravesical Recurrence in Organ-Confined Upper Urinary Tract Urothelial Carcinoma Patients After Radical Nephroureterectomy: A Retrospective Study in One Center With Long-Term Follow-Up. Pathol Oncol Res (2020) 26(3):1741–8. doi: 10.1007/s12253-019-00748-4 [DOI] [PubMed] [Google Scholar]
- 47. Li C, Yang J, Xu F, Han D, Zheng S, Kaaya RE, et al. A Prognostic Nomogram for the Cancer-Specific Survival of Patients With Upper-Tract Urothelial Carcinoma Based on the Surveillance, Epidemiology, and End Results Database. BMC Cancer (2020) 20(1):534. doi: 10.1186/s12885-020-07019-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Li C, Han D, Huang Q, Xu F, Zheng S, Li X, et al. Competing-Risks Nomogram for Predicting Cancer-Specific Death in Upper Tract Urothelial Carcinoma: A Population-Based Analysis. BMJ Open (2021) 11(7):e048243. doi: 10.1136/bmjopen-2020-048243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Qi F, Wei X, Zheng Y, Sha Y, Lu Y, Li X. Nomograms to Predict Overall and Cancer-Specific Survival in Patients With Upper Tract Urothelial Carcinoma: A Large Population-Based Study. Transl Androl Urol (2020) 9(3):1177–91. doi: 10.21037/tau.2020.03.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wu J, Chen S, Wu X, Mao W, Wang Y, Xu B, et al. Trends of Incidence and Prognosis of Upper Tract Urothelial Carcinoma. Bosn J Basic Med Sci (2021) 21(5):607–19. doi: 10.17305/bjbms.2020.5345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Siontis GC, Tzoulaki I, Castaldi PJ, Ioannidis JP. External Validation of New Risk Prediction Models Is Infrequent and Reveals Worse Prognostic Discrimination. J Clin Epidemiol (2015) 68(1):25–34. doi: 10.1016/j.jclinepi.2014.09.007 [DOI] [PubMed] [Google Scholar]
- 52. van Doeveren T, van der Mark M, van Leeuwen PJ, Boormans JL, Aben KKH. Rising Incidence Rates and Unaltered Survival Rates for Primary Upper Urinary Tract Urothelial Carcinoma: A Dutch Population-Based Study From 1993 to 2017. BJU Int (2021) 128(3):343–51. doi: 10.1111/bju.15389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Collà Ruvolo C, Nocera L, Stolzenbach LF, Wenzel M, Cucchiara V, Tian Z, et al. Incidence and Survival Rates of Contemporary Patients With Invasive Upper Tract Urothelial Carcinoma. Eur Urol Oncol (2021) 4(5):792–801. doi: 10.1016/j.euo.2020.11.005 [DOI] [PubMed] [Google Scholar]
- 54. Shiga M, Nagumo Y, Chihara I, Nitta S, Kojo K, Kimura T, et al. Discrepancy Between Clinical and Pathological T Stages in Upper Urinary Tract Urothelial Carcinoma: Analysis of the Hospital-Based Cancer Registry Data in Japan. Int J Urol (2021) 28(8):814–9. doi: 10.1111/iju.14583 [DOI] [PubMed] [Google Scholar]
- 55. Collà Ruvolo C, Nocera L, Stolzenbach LF, Wenzel M, Califano G, Tian Z, et al. Tumor Size Predicts Muscle-Invasive and Non-Organ-Confined Disease in Upper Tract Urothelial Carcinoma at Radical Nephroureterectomy. Eur Urol Focus (2021) S2405–4569. doi: 10.1016/j.euf.2021.03.003 [DOI] [PubMed] [Google Scholar]
- 56. Leow JJ, Chong YL, Chang SL, Valderrama BP, Powles T, Bellmunt J. Neoadjuvant and Adjuvant Chemotherapy for Upper Tract Urothelial Carcinoma: A 2020 Systematic Review and Meta-Analysis, and Future Perspectives on Systemic Therapy. Eur Urol (2021) 79(5):635–54. doi: 10.1016/j.eururo.2020.07.003 [DOI] [PubMed] [Google Scholar]
- 57. Kim HT. Cumulative Incidence in Competing Risks Data and Competing Risks Regression Analysis. Clin Cancer Res (2007) 13(2 Pt 1):559–65. doi: 10.1158/1078-0432.CCR-06-1210 [DOI] [PubMed] [Google Scholar]
- 58. Petrelli F, Yasser Hussein MI, Vavassori I, Barni S. Prognostic Factors of Overall Survival in Upper Urinary Tract Carcinoma: A Systematic Review and Meta-Analysis. Urology (2017) 100:9–15. doi: 10.1016/j.urology.2016.07.036 [DOI] [PubMed] [Google Scholar]
- 59. Liu W, Sun L, Guan F, Wang F, Zhang G. Prognostic Value of Lymphovascular Invasion in Upper Urinary Tract Urothelial Carcinoma After Radical Nephroureterectomy: A Systematic Review and Meta-Analysis. Dis Markers (2019) 2019:7386140. doi: 10.1155/2019/7386140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Moons KG, Altman DG, Reitsma JB, Ioannidis JP, Macaskill P, Steyerberg EW, et al. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD): Explanation and Elaboration. Ann Intern Med (2015) 162(1):W1–73. doi: 10.7326/M14-0698 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1 lists the data extracted from the original publications.
Supplementary Table S2 lists the patient characteristics of nomogram development and validation cohorts in detail.
Supplementary Table S3 lists the predictors included within each nomogram in detail.
Supplementary Table S4 summarizes the predictors most frequently used with each nomogram group
Supplementary Table S5 gives a detailed overview of the nomograms’/studies’ RoB, giving RoB and applicability for each domain.
Summary forest plot of nomogram group A predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group B1 predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group B2 predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group B3 predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Summary forest plot of nomogram group C predictor meta-analyses: The forest plot lists the results of individual meta-analyses. For each meta-analysis, the predictor’s name, the statistical approach, the number of values included (n), the prediction interval (lower limit – upper limit), and the c-Index summary estimate (estimate and 95% CIs) are given.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.