Since the beginning of the current coronavirus disease 2019 (COVID-19) pandemic, it has been highly debated whether hypertension, as a preexisting disease, affects the clinical course of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Early studies reported that hypertension was commonly observed in patients hospitalized with COVID-19 [1–5]. However, because the severity of COVID-19 has consistently been shown to be increased in older people, it is likely that the finding was confounded by age and related factors. In addition, other risk factors for severe COVID-19, such as obesity, chronic kidney disease, and cardiovascular disease, are commonly observed in patients with hypertension [6, 7]. In June 2021, the World Health Organization (WHO) released a report that hypertension, along with other cardiovascular diseases, can increase the risk of severe COVID-19, defined as admission to the intensive care unit, clinically defined severity, or mortality [8]. However, the statement also noted that whether the increased risk observed in hypertensive patients was independent of other risk factors has not been fully elucidated. It was also noted that the statement was based on the literature published before August 2020. Therefore, uncertainty remains regarding whether preexisting hypertension worsens the clinical outcome of COVID-19, independent of age and other risk factors.
In May 2022 issue of Hypertension Research, McFarlane et al. examined the risk of preexisting hypertension on in-hospital mortality in patients with COVID-19 in unadjusted and multivariate-adjusted analyses using data from the CAPACITY-COVID patient registry [9]. This registry was founded on the Case Record Form released by the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) and WHO in response to the outbreak of COVID-19, with an extension of ~400 data fields to collect detailed information on cardiovascular history, the use of cardiovascular medication, and cardiovascular outcomes [10, 11]. Adult patients (aged ≥18 years) with laboratory-confirmed or highly suspected SARS-CoV-2 infection who required hospitalization were eligible for inclusion. The study by McFarlane et al. included a total of 9197 patients from the registry who were admitted to the hospital between March 1st, 2020, and April 18th, 2021, with documentation on preexisting hypertension status and known outcomes at discharge in their records. Among the 9197 patients, nearly 50% (4443 patients) had preexisting hypertension. As expected, subjects with preexisting hypertension were older and had a higher burden of comorbid conditions such as cardiovascular disease, chronic kidney disease, chronic lung disease, obesity, and diabetes mellitus, all of which are known risk factors for severe COVID-19 [6, 7]. Approximately 80% of the participants with preexisting hypertension were taking antihypertensive medications, with RAS inhibitors being the most common, followed by beta-blockers, diuretics, and calcium-channel blockers. Conversely, ten percent of those without preexisting hypertension were taking antihypertensive medications, likely prescribed for comorbid conditions other than hypertension (such as chronic heart failure).
For the primary outcome of the study, the authors found that preexisting hypertension was associated with increased odds for in-hospital mortality in unadjusted analysis; however, adjustment for age and sex substantially attenuated the association, and the influence of preexisting hypertension was no longer observed (adjusted odds ratio (aOR) 1.06, 95% CI 0.95–1.18). Similarly, the aOR was 0.97 (95% CI 0.87–1.10) after further adjustment for diabetes, chronic kidney disease, chronic lung disease, obesity, and heart failure [9]. Thus, the association between preexisting hypertension and in-hospital mortality in COVID-19 patients was not significant after appropriate adjustment for confounding factors in the CAPACITY-COVID registry data. The results were consistent when the authors performed sensitivity analyses, in which individuals who did not have a laboratory-confirmed SARS-CoV-2 infection (10.3%) or those who were taking antihypertensive medications without documented preexisting hypertension (10.7%) were excluded.
As a secondary analysis, the study by McFarlene et al. [9] also addressed whether the type of antihypertensive medication affects the severity of COVID-19. Given that SARS-CoV-2 uses angiotensin converting enzyme 2 (ACE-2) as the cell-entry receptor, providing a link between COVID-19 and the renin-angiotensin system (RAS), it has been discussed whether antihypertensive agents, particularly RAS inhibitors, influence the course of COVID-19. Although unadjusted analysis found that the prescription of antihypertensive medications was associated overall with an increased probability of in-hospital mortality, no association was found between any medications and increased mortality. When ACE inhibitors and ARBs were pooled, the use of these agents was associated with reduced in-hospital mortality (aOR 0.88, 95% CI 0.78–0.99).
The influence of RAS inhibitors on the clinical course in patients with COVID-19 has been addressed by several randomized clinical trials. In the BRACE CORONA trial, 659 hospitalized patients with COVID-19 were assigned to the continuation of ACEi/ARB treatment or temporary suspension of the therapy for 30 days. The study found no significant differences in the primary outcome of the numbers of days alive and out of hospital at 30 days [12]. In the REPLACE COVID trial, 152 patients were randomly assigned to two groups, the RAS inhibitor continuation group or the discontinuation group. The results showed no effects on the risk of intensive care unit admission, invasive mechanical ventilatory support or death [13]. In the ACEI-COVID trial, 204 patients chronically treated with ACEIs or ARBs were randomly assigned to continuation and discontinuation groups for 30 days. There were no significant differences among the groups in the primary outcome of the maximum sequential organ failure assessment (SOFA) score within 30 days. In addition, the randomized clinical trial by Najmeddin et al. found no difference between the continuation of RAS blockers or substitution with a calcium channel blocker in the primary outcome of the length of stay in the hospital and in the intensive care unit [14]. In a recent meta-analysis of seven randomized controlled trials, the use of ACEIs/ARBs was not associated with a higher risk of mortality [15]. In sum, these data support the statements and reports from hypertension communities that usual antihypertensive therapy should be continued during COVID-19 [16–18].
The major strength of the study by McFarlane et al. [9]. lies in the large number of patients participating in the study and in the fact that the CAPACITY-COVID registry was specifically designed to collect information on cardiovascular history and complications in patients with COVID-19. Given that the clinical course of COVID-19 can vary across the world and that the study mostly enrolled patients from Europe, whether the findings of the study also apply to Asian and other populations needs to be tested in future studies. It also needs to be considered that the study was based on the data obtained by April 2021, which was before the emergence of the Omicron variant. Finally, because the study was based on the information of the documentation of preexisting hypertension in the data records, the contribution of blood pressure levels at baseline (before SARS-CoV-2 infection) and the duration of preexisting hypertension were not considered, which is an area requiring further investigation.
In summary, the study by McFarlane et al. demonstrated that the apparent association of in-hospital mortality with preexisting hypertension or with antihypertensive medication use in patients with COVID-19 was almost entirely explained by cosegregation with known risk factors, including older age and comorbidities such as obesity, diabetes, cardiovascular disease, and chronic kidney disease. Whether and how the duration, quality of control, and severity of hypertension affect the clinical course of COVID-19 independent of other risk factors merit future analysis (Fig. 1).
Fig. 1.
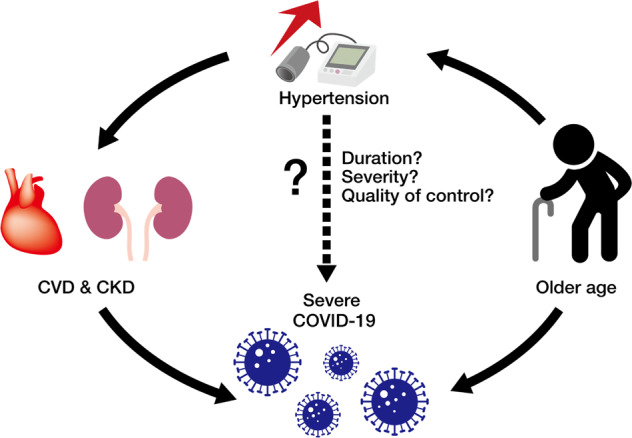
Hypertension and associated factors that potentially influence the severity of COVID-19
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Karina W, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–59. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–8. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. Prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28:1195–99. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M. Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS Study of the Italian Society of Hypertension. Hypertension. 2020;76:366–72. doi: 10.1161/HYPERTENSIONAHA.120.15324. [DOI] [PubMed] [Google Scholar]
- 7.Semenzato L, Botton J, Drouin J, Cuenot F, Dray-Spira R, Weill A, et al. Chronic diseases, health conditions and risk of COVID-19-related hospitalization and in-hospital mortality during the first wave of the epidemic in France: a cohort study of 66 million people. Lancet Reg Health Eur. 2021;8:100158. doi: 10.1016/j.lanepe.2021.100158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Hypertension and COVID-19: Scientific Brief. 2021. https://apps.who.int/iris/bitstream/handle/10665/341848/WHO-2019-nCoV-Sci-Brief-Hypertension-2021.1-eng.pdf Accessed May 2022.
- 9.McFarlane E, Linschoten M, Asselbergs FW, Lacy PS, Jedrzejewski D, Williams B. The impact of pre-existing hypertension and its treatment on outcomes in patients admitted to hospital with COVID-19. Hypertension Res. 2022;45:834–45. doi: 10.1038/s41440-022-00893-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linschoten M, Asselbergs FW. CAPACITY-COVID: a European Registry to determine the role of cardiovascular disease in the COVID-19 pandemic. Eur Heart J. 2020;41:1795–96. doi: 10.1093/eurheartj/ehaa280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CAPACITY-COVID Collaborative Consortium and LEOSS Study Group. Clinical presentation, disease course, and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease: a cohort study across 18 countries. Eur Heart J. 2022;43:1104–20. doi: 10.1093/eurheartj/ehab656. [DOI] [PubMed] [Google Scholar]
- 12.Lopes RD, Macedo AVS, de Barros E Silva PGM, Moll-Bernardes RJ, Dos Santos TM, Mazza L, et al. Effect of discontinuing vs continuing angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on days alive and out of the hospital in patients admitted with COVID-19: a randomized clinical trial. JAMA. 2021;325:254–64. doi: 10.1001/jama.2020.25864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen JB, Hanff TC, William P, Sweitzer N, Rosado-Santander NR, Medina C, et al. Continuation versus discontinuation of renin-angiotensin system inhibitors in patients admitted to hospital with COVID-19: a prospective, randomised, open-label trial. Lancet Respir Med. 2021;9:275–84.. doi: 10.1016/S2213-2600(20)30558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Najmeddin F, Solhjoo M, Ashraf H, Salehi M, Rasooli F, Ghoghaei M, et al. Effects of Renin-Angiotensin-Aldosterone Inhibitors on Early Outcomes of Hypertensive COVID-19 Patients: A Randomized Triple-Blind Clinical Trial. Am J Hypertens 2021 (e-pub ahead of print. 10.1093/ajh/hpab111). [DOI] [PMC free article] [PubMed]
- 15.Yin J, Wang C, Song X, Li X, Miao M. Effects of renin-angiotensin system inhibitors on mortality and disease severity of COVID-19 patients: a meta-analysis of randomized controlled trials. Am J Hypertens. 2022;35:462–9. doi: 10.1093/ajh/hpac001. [DOI] [PubMed] [Google Scholar]
- 16.ESC position statement, https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang Accessed May 2022.
- 17.ISH statement, https://ish-world.com/a-statement-from-the-international-society-of-hypertension-on-covid-19/ Accessed May 2022.
- 18.Shibata S, Arima H, Asayama K, Hoshide S, Ichihara A, Ishimitsu T, et al. Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19. Hypertens Res. 2020;43:1028–46. doi: 10.1038/s41440-020-0515-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


