Abstract
This study assessed the relationship between ethnicity, social determinants of health (SDH), and measures of health outcomes for children during the COVID-19 pandemic. This retrospective study reviewed electronic medical records of 1234 in-person well child visits (WCVs for age <18 years) at a single academic primary care clinic in a Chicago suburb for the results of SDH screening in the domains of food, financial, and transportation insecurity. The association between ethnicity, unmet SDH domains, routine medical care delay, vaccine delays, and utilization of acute and emergency department (ED) visits were evaluated. Patients with unmet SDH were more likely to be non-White (P < .001), ≥3 years of age (P < .001) and have Medicaid coverage (P < .001). Unmet social needs were also associated with more acute visits (P < .001), ED visits (P < .001), and WCV delays (P < .001). The results suggest that the COVID-19 pandemic has disproportionately affected patients with unmet SDH in obtaining routine pediatric well child care.
Keywords: access to care, children, community health, health promotion, pediatrics, underserved communities
Background
The coronavirus disease 2019 (COVID-19) global pandemic has had significant impacts upon health care outcomes for minority and socioeconomically disadvantaged families. A complex interplay exists between ethnicity, socioeconomic background, and social determinants of health (SDH). SDH are defined by the World Health Organization (WHO) as the “conditions in which people are born, grow, work, live, and age, and the wide set of forces and systems shaping the conditions of daily life.”1,2 Unmet social needs are associated with a variety of adverse outcomes including increased frequency of hospitalization, slower recovery time, and a higher infant mortality rate.2,3
Individuals belonging to ethnic minorities or living in low-income households are more likely to have pre-existing conditions that are associated with increased risk of illness from COVID-19 compared to those from White or more affluent households. 4 These disparities are exacerbated by structural inequities in access to medical insurance and medical care, as well as wealth variability and income volatility. Additional factors impacting the risk of developing COVID-19-related illness include work in essential industries that remained open during the early portion of the pandemic, habitation in crowded conditions, and membership in multigenerational households.4 –8 These factors both increase exposure risks, limit ability to quarantine and isolate, and restrict access to necessary preventative care. 4
The Centers for Disease Control and Prevention (CDC) posted guidelines on March 24, 2020 emphasizing the importance of routine pediatric well child care and immunizations in the midst of the pandemic. 5 In making these guidelines, the CDC cited concern about how missed primary care visits have led to immunization delays contributing to the spread of communicable disease, later recognition of new onset medical conditions, and worse chronic disease management. 6 Previous studies have shown a cumulative deficit in pediatric primary visits and vaccination rates nationwide.7 –9 However, there is still limited data on differentiating the pandemic’s impact on the heterogeneous pediatric population. This study aims to identify and quantify specific socioeconomic risk factors for delayed pediatric primary care.
Methods
The data from this qualitative retrospective chart review is presented to further demonstrate the healthcare disparities that were exacerbated by the COVID-19 pandemic. The retrospective chart review of a single academic primary care pediatric clinic was approved by the hospital system’s Institutional Review Board (IRB). The academic clinic is in Maywood, Illinois, which is a suburb of Chicago. The academic clinic is predominantly a resident-run primary care clinic with some attending-physician only visits. The population served is ethnically diverse with a significant portion of families on Medicaid. The insurance status is approximately 60% Medicaid, 35% private insurance, and 5% self-pay or uninsured. The population mix is approximately 30% White, 30% Hispanic, 30% Black, and 10% other. These demographics show that the clinic serves a diverse population with a large percentage living at or below 200% of the federal poverty level.
Screening for SDH was implemented for all the families who presented to the clinic starting in August 2020 as a pilot quality improvement project (Appendices A and B). 14 The voluntary SDH screening questionnaires included questions in the domains of food, financial, and transportation insecurity, and were offered to all families presenting for well child visits (WCVs). The timeline for implementation was planned prior to the COVID-19 pandemic but coincided with the pandemic.
The association between ethnicity, unmet SDH domains, routine medical care delay, vaccine delays, and utilization of acute and emergency department (ED) visits were evaluated using electronic medical records. There were 1234 in-person WCVs among children ≤18 years old from August 2020 through February 2021 with completed SDH screening utilized in this study. Since the protocol was for all families to receive SDH screening, there were some repeat screens for multiple visits by the same families within the time frame observed. The opportunity to have repeat screens for families provided additional opportunities to address dynamic socioeconomic transitions, such as job losses that accelerated during the pandemic. There were also families who refused to answer screening questions if they had done it on a recent visit or if they chose not to answer. Patients with repeat screens (n = 130) accounted for 25% (n = 310) of the visits.
Data Analysis
To ascertain relationships between socio-demographics and health utilization markers, multiple quantitative data analysis methodologies were utilized. For quantitative data, Chi-square, Kruskal-Wallis test, Fisher exact test, and Spearman correlation were computed. Comparisons of groups and health utilization markers were determined for statistical significance.
Results
Table 1 shows the breakdown of SDH positivity rates separated based upon ethnicity. The screening rates reflect the largely non-White population served by the clinic. Unmet SDH needs were associated with non-White ethnicity (P-value < .001). Among positive screens, 89.3% (n = 486/544) identified as non-White (American Indian, Asian, Black, Hispanic/Latino, and mixed) and 7.2% (n = 39/544) identified as White. Among negative screens, 77.1% (n = 532/690) identified as non-White and 19.1% (n = 132/690) identified as White.
Table 1.
Social Determinants of Health Screening Positivity Rates by Ethnicity.
| Positive SDH screen (%) | Negative SDH screen (%) | |
|---|---|---|
| American Indian | 1 (100) | 0 (0.0) |
| Asian | 8 (42.1) | 11 (57.9) |
| Black | 174 (48.9) | 182 (51.1) |
| Hispanic/Latino | 299 (47.2) | 334 (52.8) |
| Mixed | 2 (28.6) | 5 (71.4) |
| White | 39 (22.8) | 132 (77.2) |
| Unknown | 19 (42.2) | 26 (57.8) |
| P-value (Fisher) | <.001 | |
Among positive screens, 71.1% (n = 387/544) were enrolled in Medicaid, 23.5% (n = 128/544) private insurance, and 5.3% (n = 29/544) self-pay. Among negative screens, 53.5% (n = 369/690) were enrolled in Medicaid, 40.3% (n = 278/690) private insurance, 4.5% (n = 31/690) self-pay, and 1.7% (n = 12/690) military insurance.
There were statistically significant differences in health care utilization markers among positive and negative screens. The median number of days of delay in WCVs was 33.0 for positive screens versus 8.0 for negative screens (P < .001). Patients with positive screens were more likely to have attended acute care visits (P < .001) and ED visits (P < .001) compared to their negative-screened counterparts.
Two utilization markers without statistical significance were being up to date (UTD) on vaccinations (P = .85) and delay in vaccinations if not UTD (P = .055).
Table 2 presents additional demographics and health care utilization data. Any ED utilization was consistently statistically significant for age range (P < .001), ethnicity (P < .01), and insurance status (P < .01). School age children, Hispanic or Latino ethnicity, and Medicaid coverage were associated with having any ED visit during the timeframe reviewed.
Table 2.
Outcomes Measurement.
| Delay WCV in days (mean) | Vaccine delay in months (mean) | Acute care visits (mean) | Any acute visits (%) | ED visits (mean) | Any ED visits (%) | Hospitalization (mean) | Any hospitalization (%) | |
|---|---|---|---|---|---|---|---|---|
| SDH screen negative | 145.0 | 6.29 | 0.68 | 33.7 | 0.19 | 12.8 | 0.06 | 5.6 |
| SDH screen positive | 97.8 | 7.75 | 0.97 | 43.5 | 0.33 | 21.5 | 0.06 | 4.7 |
| P-value | <.01* | .20 | .02* | <.001* | <.01* | <.001* | .60 | .60 |
Statistically significant with P < .05.
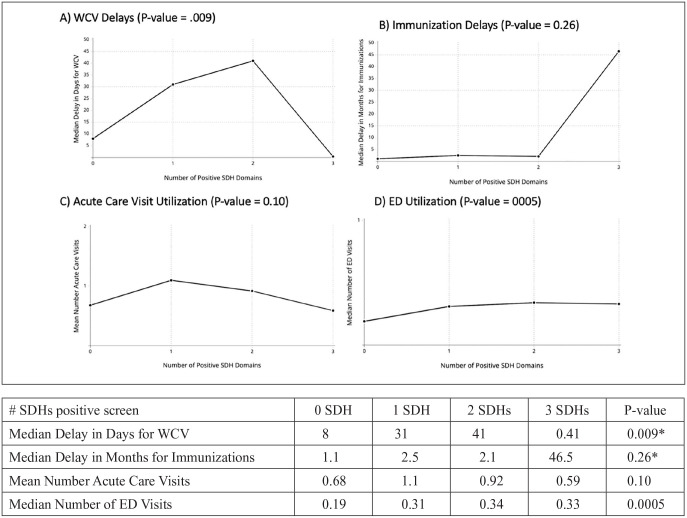
In Figure 1, the association with the number of positive SDH domains and health care utilization are presented. There was a statistically significant relationship between the number of SDH domains that screened positive and WCV delays (Kruskal-Wallis, P = .009) as well as the number of ED visits (P = .0005). There was no association between the number of positive SDH domains and delays in vaccinations or number of acute care visits. Although it appeared that vaccine delays in months increased with the number of SDH domains with positive screens, it was not statistically significant (Kruskal-Wallis, P-value = .26) since there were only 3 patients with 3 positive SDH domains.
Figure 1.
Number of SDH positives and health care utilization. Positive screens for social determinants: financial insecurity, food insecurity, transport, and other social determinants. (A) Association between delays in median well child visit (WCV) based upon number of positive social determinants of health (SDH) domains. Statistically significant relationship between number of SDHs screened positive and WCV delays (Kruskal-Wallis, P = .001). (B) Association between median delay in months for immunizations based upon number of positive SDH domains. There are only 3 subjects with 3 positive SDHs, resulting in a divergent and non-significant result for median delay in months for immunizations UTD. (C) Association between mean number of acute care visits based upon number of positive SDH domains. Relationships between number of positive SDHs and number of acute care visits are not significant. (D) Association between median number of acute emergency department (ED) visits based upon number of positive SDH domains. Statistically significant relationship between number of SDHs screened positive and number of ED visits (P = .0005).
In Figure 2, data reviewing delays in WCVs based on age and SDH screen results are presented. Among positive screens, 57.5% (n = 313/544) were among children ≥3 years of age. Among negative screens, 58.1% (n = 401/690) were among children <3 years of age. There is a positive relationship with increase in delays of WCVs for patients with positive SDH screens and patient age with more delays associated in higher age groups up to school age (Spearman correlation, Kruskal-Wallis P < .001).
Figure 2.
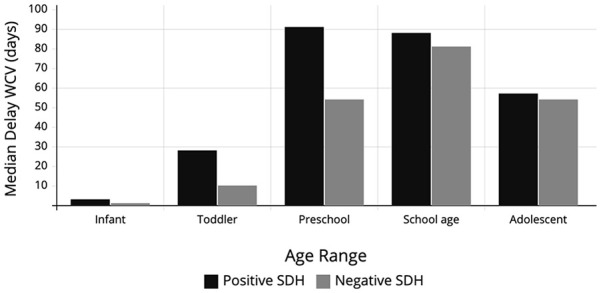
Delay in WCV based on age and positive SDH. Both age and age-range are associated with delays in WCVs. Significant Spearman correlation with age and significant increase in delayed WCV in patient age up to School Age. Kruskal-Wallis P < .001.
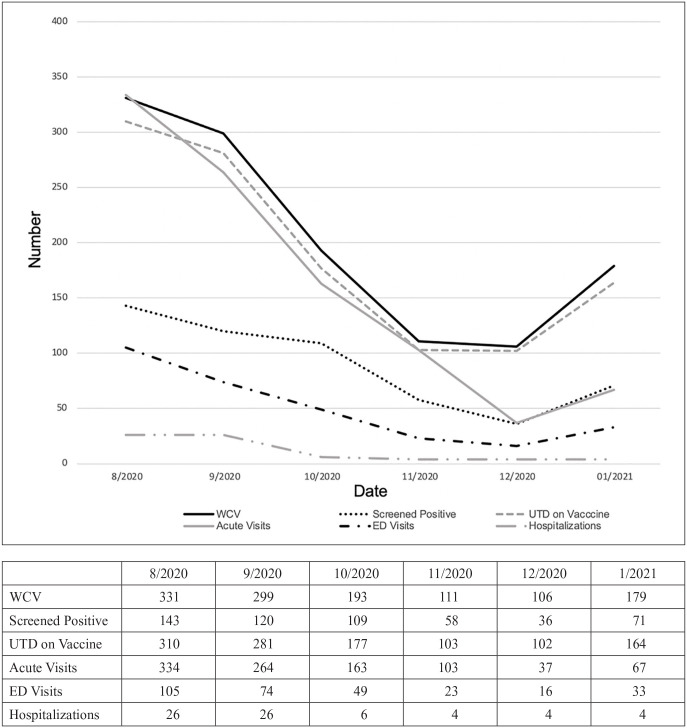
In Figure 3, health care utilization of the time period of the project was reviewed. February 2021 was excluded since only part of the month was included in the data collection period for comparison purposes. WCVs, acute visits, ED visits, and hospitalizations decreased from the beginning of the time period and reached their nadir around the winter months. WCVs, acute visits, and ED visits show increases in utilization by January 2021.
Figure 3.
Time-related data. Comparing monthly rates of WCV, positive SDH screening, UTD on vaccines, number of acute visits, number of ED visits, and number of hospitalization rates during study period.
Discussion
This retrospective chart review illustrates that there are distinguishable differences among pediatric primary care markers based upon ethnicity and self-reported unmet social needs during the COVID-19 pandemic in this patient cohort. The ethnically diverse population in this cohort provides insight into the complex interplay between various factors contributing to health care utilization during the COVID-19 pandemic. The association of ethnicity with SDH was strongly correlated. Non-White background was associated with increased likelihood of self-reporting an unmet SDH domain. Positive SDH screens for unmet needs were associated with a greater likelihood of acute care and ED visits. Increasing numbers of unmet SDH domains were positively correlated with increased WCV delays and number of ED visits. This is consistent with the existing literature regarding structural health disparities among those from ethnic minority backgrounds and those living in poverty.4,10 –13
Raifman and Raifman completed a survey of >400 000 adults which found that those “who were black, American Indian, or live in low-income households are more likely to have conditions associated with increased risk of illness from COVID-19 relative to those who are white or are living in higher-income household.” 4 Although the Raifman and Raifman study looked at adults only, it is consistent with our findings that ethnicity and income levels translate to inequities in risk also for children.
A study comparing pediatric primary care visits (n = 120 230) in April 2020 compared to April 2019 in the Carolinas found overall fewer well and acute visits in April 2020. 6 The study by Brown et al 6 found lower odds of attending well visits compared to acute visits in 2020. Their study also found differences in visits for chronic conditions that varied among ethnic groups and insurance type. For example, non-Hispanic black and Hispanic patients had lower odds of attending visits for ADHD, depression, and anxiety compared to white patients. 6 Also, children insured by private insurance had higher odds of attending well visits and visits for certain chronic conditions (such as depression and anxiety). 6 This study only compared 2 months (April 2019 and April 2020), but also found disparities in access to pediatric primary care based upon ethnicity and insurance type.
There were some differences between our findings and existing literature as well. A study by Lebrun-Harris et al 9 reviewed US Census Bureau’s Household Pulse Survey data from April to May 2021. The sample of 48 824 households with ≥1 child or adolescent <18 years found that 26.4% of households reported at least 1 child or adolescent had missed or delayed a preventative visit due to COVID-19. 9 This survey found an association between unmet social needs and prevalence of missed or delayed preventative visits, but no association between health insurance or income levels and missed or delayed preventative visits. The most common reasons were related to concern about visiting a health care provider, limited appointment availability, and provider office being closed. 9 This population sample does vary from our own significantly. Our population size was limited to a patient population who were able to make at least 1 in-person well child appointment, our captured time frame was earlier in the pandemic (April 2020-February 2021), and our study was limited to a single clinical site.
Our study contributes knowledge about the disruption of routine pediatric care that has been uneven during the time frame reviewed. Although much of the literature focuses on aggregate data, our study is noteworthy in its ability to identify and quantify the impacts of specific socioeconomic factors on access to routine pediatric care. This data shows greater specificity involving the pandemic’s disruption of routine pediatric care that has been uneven during the time frame reviewed.
Many of the public health interventions regarding primary care have lacked specificity in targeting particularly vulnerable subgroups. For instance, in March 2020, after the WHO declared a global pandemic and the United States declared a National Emergency due to COVID-19, the Centers for Disease Control (CDC) recommended that outpatient medical providers prioritize urgent visits, delay elective care, and convert clinic visits to telehealth encounters.15,16 Despite the CDC and the American Academy of Pediatrics (AAP) recommending that routine vaccinations continue to be delivered especially for younger children, many families were fearful of entering a clinic or assumed that the primary care office was closed. 17 This, combined with extraordinarily high levels of economic distress faced by many families, contributed to delays in care. 9 Our study reflects that access to care was more influenced by SDH and other socioeconomic factors, which is mirrored by national data. Nationwide, routine pediatric visits and childhood vaccination adherence dramatically decreased in March and April of 2020 during the pandemic.5,17,18
Upon initial analysis, our study’s data appears to show discordance with national rates of pediatric ED and acute care visits. A marked decrease in pediatric ED visits was also noted during the pandemic.7,19 Upon more thorough analysis, our study shows greater specificity for shifts in pediatric healthcare utilization based on socioeconomic factors. The results of this study indicate that children from ethnic minority backgrounds and children with unmet social needs experienced greater delays in WCVs and increased reliance on acute and ED visits during the pandemic.
Limitations
Several limitations of this study should be noted. First, the cohort studied was limited to a single primary care center in the Midwest. The cohort only included those who were able to attend in-person WCVs during the time frame studied. Many children and families opted out of in-person visits during the pandemic. Therefore, this may not be a representative sample of the entire population served by the clinic. Second, the screening tool used to categorize the cohort into positive versus negative SDH screens was entirely self-reported and subjective, which raises the possibility of response bias. Additionally, the completion of SDH screening was voluntary, so there may have been patients who refused to answer the screening questions. Finally, the health care utilization measures were limited to those which were documented within the electronic medical record. If patients received outside care that was not captured in the record, then that data was inevitably excluded.
Conclusion
Findings from this retrospective study indicate that the COVID-19 pandemic has had an uneven impact upon routine well child care. Children already at risk for poorer health outcomes due to disparities and inequities, such as those from minority and lower socioeconomic backgrounds, were disproportionately impacted. Non-White ethnicity was associated with self-reported unmet social needs in the domains studied. Health care utilization in turn varied. Those with unmet social needs were more likely to be delayed in routine WCVs compared to those with no reported SDH needs. However, those with unmet social needs were more likely to utilize acute care and ED visits due to gaps in receiving timely health care needs. These variations may have negative implications for both immediate and long-term effects on the health of children from these vulnerable backgrounds.
Acknowledgments
The authors would like to thank and acknowledge the support of the Loyola University Medical Center Quality Improvement (QI) team, specifically Beatrice D. Probst, MD; Stephanie Kendzior, BSN, RN; and Aurora Trnka, MSN, RN; as well as the Loyola Outpatient Center pediatric clinical coordinator, Mary Ellen Callaghan, RN and the other nursing and clinical staff at the Loyola Outpatient Center’s pediatric outpatient clinic.
Appendix A: SDH Screen (English)
Name: ___________________________________ DOB: ____________
Changes have happened during the pandemic. We care about your child and family, so we are asking all families these questions. Please answer the following questions.
□ No thanks □ Done at recent visit
Finances
How hard is it for you to pay for the very basics like food, housing, medical care, and heating?
| Not hard at all | Not very hard | Somewhat hard | Hard | Very hard | Prefer Not to Answer |
_______________________________________________________________________________________________________
Food
Within the past 12 months, you worried that your food would run out before you got money to buy more:
| Never True | Sometimes True | Often True | Prefer Not to Answer |
Within the past 12 months, the food you bought just did not last and you did not have money to get more:
| Never True | Sometimes True | Often True | Prefer Not to Answer |
_______________________________________________________________________________________________________
Transportation Needs
In the past 12 months, has lack of transportation kept you from medical appointments or from getting medications?
| Yes | No | Prefer Not to Answer |
In the past 12 months, has lack of transportation kept you from meetings, work, or getting things needed for daily living?
| Yes | No | Prefer Not to Answer |
Appendix B: SDH Screen (Spanish)
Nombre: ___________________________________ Fecha de nacimiento: ___________
Cambios han pasado durante la pandemia. Nos importa su hijo/a y su familia, entonces les hacemos estas preguntas a todas las familias. Favor de contestar las siguientes preguntas.
□ No gracias □ Hecho a otra visita recién
Finanzas
¿Para usted, cuán difícil es pagar para los gastos básicos como alimentos, alojamiento, atención médica, y calefacción?
| No es nada difícil | No muy difícil | Algo difícil | Difícil | Muy difícil | Prefiero no contestar |
_______________________________________________________________________________________________________
Alimentos
En los últimos 12 meses, le preocupaba que los alimentos se acabaran antes de que tuviera suficiente dinero para comprar más:
| Nunca verdad | A veces verdad | Frecuentemente verdad | Prefiero no contestar |
En los últimos 12 meses, los alimentos que compraba no duraron lo suficiente y no tenía dinero para comprar más:
| Nunca verdad | A veces verdad | Frecuentemente verdad | Prefiero no contestar |
_______________________________________________________________________________________________________
Necesidades de transporte
¿En los últimos 12 meses, le ha impedido la falta de transporte de asistir a citas médicas o de recoger medicinas?
| Sí | No | Prefiero no contestar |
¿En los últimos 12 meses, le ha impedido la falta de transporte de asistir a reuniones, a trabajo, o conseguir cosas necesarias para la vida diari?
| Sí | No | Prefiero no contestar |
Footnotes
Author Contributions: Pyone David, Julie O’Keefe, and Nadia K. Qureshi made substantial contributions to conception and design. Pyone David, Sarah Fracci, Jennifer Wojtowicz, Erin McCune, Katyln Sullivan made substantial contributions to acquisition of data. Pyone David, Garry Sigman, Julie O’Keefe, and Nadia K. Qureshi made substantial contributions to analysis and interpretation of data. Pyone David, Julie O’Keefe, and Nadia K. Qureshi completed the drafting and revisions of the article. All authors gave final approval of the version to be published.
Availability of data and material: Available upon appropriate request to Pyone David (pyone.david@uchospitals.edu).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: The Loyola Internal Review Board Committee (IRB) approved the study without need for ethical approval (reference # 213880).
ORCID iDs: Pyone David  https://orcid.org/0000-0003-3214-1628
https://orcid.org/0000-0003-3214-1628
Jennifer Wojtowicz  https://orcid.org/0000-0002-2087-099X
https://orcid.org/0000-0002-2087-099X
Erin McCune  https://orcid.org/0000-0001-5154-2043
https://orcid.org/0000-0001-5154-2043
Katyln Sullivan  https://orcid.org/0000-0003-1277-9085
https://orcid.org/0000-0003-1277-9085
Julie O’Keefe  https://orcid.org/0000-0003-3863-1257
https://orcid.org/0000-0003-3863-1257
References
- 1. Greater New York Hospital Association. Training primary care residents on social determinants of health. Accessed March 11, 2021. https://www.gnyha.org/tool/training-primary-care-residents-on-the-social-determinants-of-health
- 2. Narayan A, Raphael J, Rattler T, Bocchini C. Social determinants of health. Accessed March 11, 2021. https://www.texaschildrens.org/sites/default/files/uploads/documents/83176%20BRIEF%20Social%20Determinants%20of%20Health%20Policy%20Digital.pdf
- 3. Chung EK, Siegel BS, Garg A, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46(5):135-153. doi: 10.1016/j.cppeds.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137-139. doi: 10.1016/j.amepre.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Santoli JM, Lindley MC, DeSilva MB, et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(19):591-593. doi: 10.15585/mmwr.mm6919e2 [DOI] [PubMed] [Google Scholar]
- 6. Brown CL, Montez K, Amati JB, et al. Impact of COVID-19 on pediatric primary care visits at four academic institutions in the Carolinas. Int J Environ Res Public Health. 2021;18(11):5734. doi: 10.3390/ijerph18115734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schweiberger K, Patel SY, Mehrotra A, Ray KN. Trends in pediatric primary care visits during the coronavirus disease of 2019 pandemic. Acad Pediatr. 2021;21(8):1426-1433. doi: 10.1016/j.acap.2021.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Onimoe G, Angappan D, Chandar MCR, Rikleen S. Effect of COVID-19 pandemic on well child care and vaccination. Front Pediatr. 2022;10:873482. doi: 10.3389/fped.2022.873482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lebrun-Harris LA, Sappenfield OR, Warren MD. Missed and delayed preventive health care visits among US children due to the COVID-19 pandemic. Public Health Rep. 2022;137(2):336-343. doi: 10.1177/00333549211061322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Griffith K, Evans L, Bor J. The Affordable Care Act reduced socioeconomic disparities in health care access. Health Aff. 2017;36(8):1503-1510. doi: 10.1377/hlthaff.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. The Pew Charitable Trusts. How Income Volatility Interacts With American Families Financial Security. The Pew Charitable Trusts; 2017. Accessed April 6, 2022. www.pewtrusts.org/-/media/assets/2017/03/incomevolatility_and_financialsecurity.pdf [Google Scholar]
- 12. U.S. Bureau of Labor Statistics. BLS reports: a profile of the working poor, 2016. 2018. www.bls.gov/opub/reports/working-poor/2016/home.htm. Accessed April 6, 2022.
- 13. Adamkiewicz G, Zota AR, Fabian MP, et al. Moving environmental justice indoors: understanding structural influences on residential exposure patterns in low-income communities. Am J Public Health. 2011;101 Suppl 1(1):S238-S245. doi: 10.2105/AJPH.2011.300119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. David P, Qureshi NK, Ha L, et al. Social determinants of health screening at well child visits: a pilot program implemented during the COVID-19 pandemic. Glob Pediatr Health. 2021;8:2333794X2110609. doi: 10.1177/2333794x211060971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. Interim guidance for routine and influenza immunization services during the COVID-19 pandemic. Published 2020. Updated October 20, 2020. [Google Scholar]
- 17. Mehrotra M, Linetsky D, Hatch H, Cutler D. What impact has COVID-19 had on outpatient visits? The Commonwealth Fund. To the Point website. Published 2020. [Google Scholar]
- 18. O’Leary ST, Trefren L, Roth H, Moss A, Severson R, Kempe A. Number of childhood and adolescent vaccinations administered before and after the COVID-19 outbreak in Colorado. JAMA Pediatr. 2021;175(3):305-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DeLaroche AM, Rodean J, Aronson PL, et al. Pediatric emergency department visits at US children’s hospitals during the COVID-19 pandemic. Pediatrics. 2021;147(4):e2020039628. doi: 10.1542/peds.2020-039628 [DOI] [PubMed] [Google Scholar]