Abstract
This cohort study uses data from the Atherosclerosis Risk in Communities (ARIC) Study to investigate whether the increase in metabolic syndrome severity is more pronounced in women than men and whether the sex difference varies by race.
Introduction
The mechanism underlying women's higher risk of cardiovascular disease (CVD) associated with diabetes is not fully elucidated but may be related to greater metabolic risk deterioration before diabetes in women than men.1 The sex disparity in diabetic CVD varies by race. Non-Hispanic Black (Black) women with diabetes have a higher prevalence of CHD and stroke than Black men, while in non-Hispanic White (White) individuals, there is a male predominance in diabetic CVD.2 In this study, we investigated whether the increase in metabolic syndrome severity, a continuous biomarker of the severity of metabolic derangement, during prediabetes is more pronounced in women than in men and whether the sex difference varies by race.
Methods
In this cohort study, we used data from the Atherosclerosis Risk in Communities (ARIC) Study visits 1 to 4 from 1987 to 1998. ARIC is a prospective study of middle-aged adults in the US.3 We reported findings according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. This analysis involved secondary, deidentified data that did not require review from the institutional review board at Tulane University.
Our primary outcome was the metabolic syndrome severity score derived from waist circumference, triglycerides, systolic blood pressure (SBP), high-density lipoprotein (HDL), and fasting glucose (FG), accounting for the weight of the contribution of each component by sex and race.4 Race was self-reported, and the categories included non-Hispanic Black and non-Hispanic White. Ethnicity was not considered in this study because only a small portion of ARIC participants self-reported as Hispanic, which did not provide sufficient power for statistical testing. Race was considered in this study because sex differences in diabetes progression has rarely been reported in Black and White individuals separately, and the sex disparity in diabetic cardiovascular disease varies by race.
The score was calculated for participants at visits 1 to 4 with a 3-year interval between visits. We performed linear mixed regressions to model the metabolic syndromescore and components over time among men and women across FG levels (normoglycemia, <100 mg/dL; prediabetes, 100-125 mg/dL; diabetes, ≥126 mg/dL, or with a diabetes diagnosis; to convert glucose to mmol/L, multiply by 0.0555), including a random intercept and a random slope to account for the within-subject correlation. We adjusted for age, education, smoking, and antihypertensive, lipid-lowering, and antidiabetes medications. We also adjusted for body mass index (calculated as weight in kilograms divided by height in meters squared) for outcomes of SBP, HDL, triglycerides, and FG. The SAS statistical software, version 9.4 (SAS Institute) was used for statistical analysis. Statistical significance was set at P < .05.
Results
This study included 13 412 individuals, with 7414 women (55%) and 9983 White individuals (75%) (Table). During a median follow-up of 9 years, women had a significantly greater increase in mean (SD) metabolic syndrome severity vs men (0.098 [0.004] vs 0.074 [0.004]) in the prediabetes state, while men experienced a greater increase in the diabetes state (0.055 [0.005] vs women 0.04 [0.005]) (Figure, Table). Metabolic syndrome severity increased at a greater rate among White women vs White men in the prediabetes state (0.12 [0.004] vs 0.054 [0.004]) and diabetes state (0.06 [0.006] vs 0.043 [0.006]); however, in Black individuals, there were no significant changes in metabolic syndrome severity across FG levels (Figure, Table). Women had a greater increase in waist circumference vs men in prediabetes and diabetes states for White individuals and the prediabetes state for Black individuals (Figure, Table). Compared with Black men, Black women had a greater increase in triglycerides across FG levels (Figure, Table) and a greater increase in SBP in the prediabetes state (Figure, Table). Men had a greater adverse change in HDL vs women across FG levels in white individuals (Figure, Table). No significant sex difference was observed in the change of FG in the prediabetes state. During diabetes, men showed a greater increase in FG (Figure, Table).
Table. Characteristics and Changes of Metabolic Risk Factors by Sex and Race.
| Characteristics and changes | All (n = 13 412) | White (n = 9983) | Black (n = 3429) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men (n = 5998) | Women (n = 7414) | P valuea | Men (n = 4643) | Women (n = 5340) | P valuea | Men (n = 1355) | Women (n = 2074) | P valuea | |
| Characteristics | |||||||||
| Age, mean (SD), y | 54.4 (5.8) | 53.7 (5.7) | <.001 | 54.5 (5.7) | 53.9 (5.7) | <.001 | 53.8 (6) | 53.2 (5.8) | .007 |
| High school education or less, No. (%) | 2988 (49.9) | 4404 (59.5) | <.001 | 2134 (46) | 3121 (58.5) | <.001 | 854 (63.2) | 1283 (62.0) | .49 |
| Current smoking, No. (%) | 1662 (27.7) | 1823 (24.6) | <.001 | 1143 (24.6) | 1325 (24.8) | .80 | 519 (38.3) | 498 (24.0) | <.001 |
| Antihypertensive medications, No. (%) | 1206 (20.1) | 1734 (23.4) | <.001 | 783 (16.7) | 895 (16.8) | .90 | 423 (31.2) | 839 (40.5) | <.001 |
| Lipid lowering medications, No. (%) | 1102 (18.6) | 1755 (23.8) | <.001 | 803 (17.4) | 1127 (21.2) | <.001 | 299 (22.6) | 628 (30.7) | <.001 |
| Antidiabetic medications, No. (%) | 264 (5.6) | 377 (5.7) | .90 | 136 (3.6) | 145 (3.0) | .10 | 128 (14.3) | 232 (13.3) | .50 |
| Metabolic syndrome z-score, mean (SD) | 0.4 (0.9) | 0.3 (1.3) | <.001 | 0.36 (0.8) | 0.1 (1.1) | <.001 | 0.34 (1.4) | 0.7 (1.7) | <.001 |
| BMI, mean (SD) | 27.4 (4.2) | 27.6 (6) | .009 | 27.3 (3.9) | 26.4 (5.4) | <.001 | 27.6 (4.9) | 30.7 (6.5) | <.001 |
| Waist circumference, mean (SD), cm | 98.8 (10.9) | 94.7 (15.4) | <.001 | 99.4 (10.3) | 92.6 (14.5) | <.001 | 96.8 (12.9) | 100.2 (16.3) | <.001 |
| Triglycerides, mean (SD), mg/dL | 133.2 (71.1) | 118.5 (63.5) | <.001 | 138.9 (71.8) | 123.1 (67) | <.001 | 113.8 (64.9) | 106.7 (51.8) | <.001 |
| SBP, mean (SD), mmHg | 122.3(17.7) | 119.9 (19.4) | <.001 | 120 (15.9) | 116.8 (17.7) | <.001 | 130.2 (21.3) | 128.2 (21.1) | .005 |
| HDL cholesterol, mean (SD), mg/dL | 45.1 (13.9) | 58.0 (16.9) | <.001 | 43.3 (12.1) | 57.9 (16.9) | <.001 | 51.4 (17.3) | 58.1 (17.1) | <.001 |
| Fasting glucose, mean (SD), mg/dL | 108.7 (35.1) | 106.8 (40.6) | .003 | 106.6 (27.9) | 102 (28.5) | <.001 | 116.1 (52.3) | 119 (60) | .10 |
| Annual change of metabolic risk factors across visits (SD)b | |||||||||
| Metabolic syndrome z-score | |||||||||
| Normoglycemia | 0.07 (0.02) | 0.09 (0.02) | .001 | 0.04 (0.02) | 0.1 (0.02) | .80 | 0.07 (0.05) | 0.08 (0.04) | .40 |
| Prediabetes | 0.07 (0.004) | 0.1 (0.004) | <.001 | 0.05 (0.004) | 0.1 (0.004) | <.001 | 0.07 (0.01) | 0.09 (0.01) | .10 |
| Diabetes | 0.06 (0.01) | 0.04 (0.01) | <.001 | 0.04 (0.01) | 0.06 (0.01) | <.001 | 0.09 (0.01) | 0.03 (0.01) | .20 |
| Waist circumference | |||||||||
| Normoglycemia | 0.6 (0.2) | 1.4 (0.3) | .46 | 0.7 (0.2) | 1.7 (0.4) | .10 | 0.3 (0.5) | 1.6 (0.6) | .91 |
| Prediabetes | 0.7 (0.05) | 1.8 (0.06) | <.001 | 0.8 (0.05) | 2.1 (0.07) | <.001 | 0.5 (0.1) | 1.8 (0.1) | .01 |
| Diabetes | 0.7 (0.07) | 1.5 (0.09) | <.001 | 0.7 (0.08) | 1.8 (0.1) | <.001 | 0.6 (0.1) | 1.7 (0.2) | .07 |
| Triglyceridesc | |||||||||
| Normoglycemia | 0.03 (0.01) | 0.09 (0.01) | <.001 | 0.04 (0.001) | 0.1 (0.01) | <.001 | 0.02(0.03) | 0.07 (0.02) | <.001 |
| Prediabetes | 0.04 (0.002) | 0.09 (0.002) | <.001 | 0.05 (0.002) | 0.1 (0.002) | .10 | 0.02 (0.01) | 0.07 (0.004) |
.07 |
| Diabetes | 0.03 (0.003) | 0.08 (0.003) | .03 | 0.04 (0.004) | 0.1 (0.004) | <.001 | 0.03 (0.01) | 0.07 (0.004) | <.001 |
| SBP | |||||||||
| Normoglycemia | 1 (0.47) | 0.9 (0.5) | <.001 | 1.1 (0.5) | 0.6 (0.5) | <.001 | 2.2 (1.2) | 2.51 (0.9) | .06 |
| Prediabetes | 1 (0.08) | 0.8 (0.08) | .90 | 1.1 (0.08) | 0.4 (0.08) | .10 | 2 (0.2) | 2.44 (0.2) | .80 |
| Diabetes | 0.8 (0.1) | 0.7 (0.1) | .20 | 0.8 (0.1) | 0.3 (0.1) | .004 | 2 (0.3) | 2.39 (0.2) | .20 |
| HDL cholesterol | |||||||||
| Normoglycemia | −0.7 (0.4) | 0.5 (0.4) | <.001 | −0.3 (0.4) | 0.6 (0.5) | <.001 | −0.9 (0.9) | −0.01 (0.7) | .04 |
| Prediabetes | −0.7 (0.06) | 0.4 (0.07) | <.001 | −0.4 (0.06) | 0.4 (0.08) | <.001 | −1 (0.2) | −0.02 (0.2) | .07 |
| Diabetes | −0.9 (0.09) | 0.5 (0.1) | <.001 | −0.4 (0.1) | 0.5 (0.1) | <.001 | −1.3 (0.2) | 0.27 (0.2) | .40 |
| Fasting glucose | |||||||||
| Normoglycemia | 2.2 (0.6) | 0.8 (0.5) | .005 | 1.1 (0.5) | 0.6 (0.4) | .08 | 3.3 (2.2) | 0.3 (1.7) | .07 |
| Prediabetes | 2.3 (0.1) | 0.8 (0.1) | .90 | 1.2 (0.1) | 0.7 (0.09) | .40 | 3.3 (0.5) | 0.3 (0.4) | .80 |
| Diabetes | 2.4 (0.2) | 0.4 (0.2) | .02 | 1.5 (0.2) | 1 (0.2) | .30 | 3.2 (0.8) | −0.9 (0.6) | .10 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HDL, high-density lipoprotein; SBP, systolic blood pressure.
SI conversion factor: To convert triglycerides to mmol/L, multiply by 0.0113; HDL cholesterol to mmol/L, multiply by 0.0259; glucose to mmol/L, multiply by 0.0555.
P for sex differences.
Atherosclerosis Risk in Communities Study visits 1 to 4 (1987 to 1998).
Log-transformed.
Figure. Annual Change of Metabolic Risk Factors Across Atherosclerosis Risk in Communities Visits.
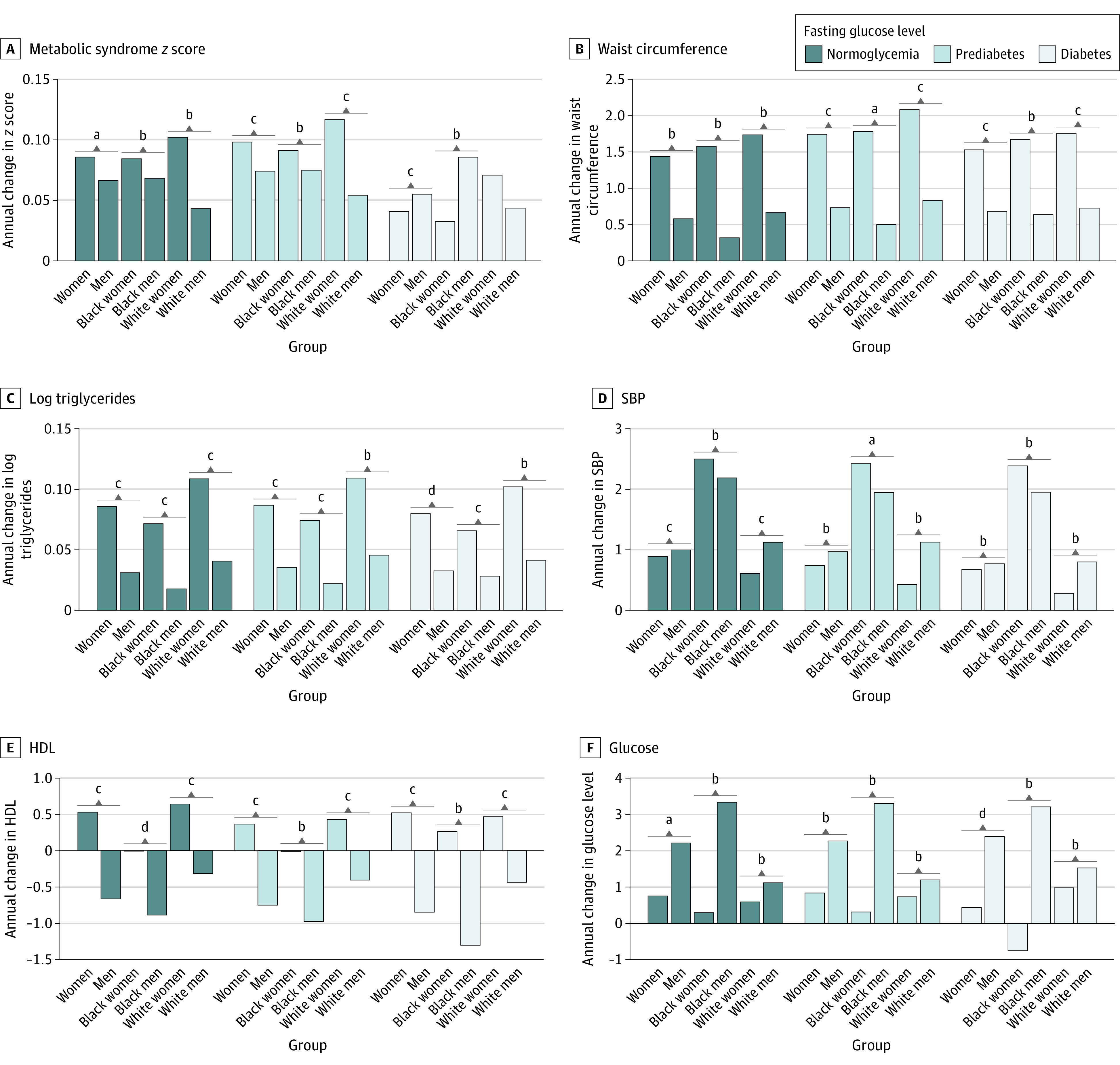
HDL indicates high-density lipoprotein; SBP, systolic blood pressure.
aP < .01.
bNot significant.
cP < .001.
dP < .05.
Discussion
In this study, women were associated with experiencing a greater increase in metabolic syndrome severity, central adiposity, and triglycerides than men in the prediabetes state, potentially explaining women's disadvantage in diabetic CVD risk. We extended prior cross-sectional evidence5,6 and highlighted women's worse metabolic risk profiles vs men before diabetes, and the sex difference varied by race. However, this study was limited because of the study’s short follow-up (9 years), so we cannot capture all individuals' 3-stage diabetes development (normoglycemia to prediabetes to diabetes). Sex and race-specific strategies for metabolic risk monitoring and control during prediabetes should be considered.
References
- 1.Peters SA, Huxley RR, Sattar N, Woodward M. Sex differences in the excess risk of cardiovascular diseases associated with type 2 diabetes: potential explanations and clinical implications. Curr Cardiovasc Risk Rep. 2015;9(7):36. doi: 10.1007/s12170-015-0462-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Diabetes Statistics Report. Centers for Disease Control and Prevention . 2020. Accessed June 9, 2022. https://www.cdc.gov/diabetes/data/statistics-report/index.html
- 3.The ARIC investigators . The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129(4):687-702. doi: 10.1093/oxfordjournals.aje.a115184 [DOI] [PubMed] [Google Scholar]
- 4.DeBoer MD, Gurka MJ, Golden SH, et al. Independent associations between metabolic syndrome severity and future coronary heart disease by sex and race. J Am Coll Cardiol. 2017;69(9):1204-1205. doi: 10.1016/j.jacc.2016.10.088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Ritter R, Sep SJS, van der Kallen CJH, et al. Adverse differences in cardiometabolic risk factor levels between individuals with pre-diabetes and normal glucose metabolism are more pronounced in women than in men: the Maastricht Study. BMJ Open Diabetes Res Care. 2019;7(1):e000787. doi: 10.1136/bmjdrc-2019-000787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wannamethee SG, Papacosta O, Lawlor DA, et al. Do women exhibit greater differences in established and novel risk factors between diabetes and non-diabetes than men: The British Regional Heart Study and British Women’s Heart Health Study. Diabetologia. 2012;55(1):80-87. doi: 10.1007/s00125-011-2284-4 [DOI] [PubMed] [Google Scholar]


