Abstract
Purpose
We report the case of a 32-year-old woman with orbital myositis prior to onset of Behcet's disease (BD).
Observations
A 32-year-old woman was referred to our hospital for a complaint of right eyelid swelling, eye pain, and diplopia. Her best-corrected visual acuity was 20/32 on the right, and 20/16 on the left. She was diagnosed as idiopathic orbital inflammation, and received two pulses of intravenous administration of methylprednisolone, followed by oral prednisolone. Three months later, she developed bilateral orbital myositis, and received one more pulse therapy, followed by oral prednisolone and cyclosporin. About one year after the first visit, oral aphthae, genital ulcers, and folliculitis-like skin rash appeared, and the physician diagnosed incomplete type BD. The patient had no uveitis during the disease course. Orbital inflammation and systemic manifestations of BD were ultimately well controlled with small doses of prednisolone.
Conclusion and importance
BD may develop during the course of orbital inflammation.
Keywords: Orbital inflammation, Behcet's disease
1. Introduction
The systemic manifestations of Behcet's disease (BD) include recurrent oral aphthae, followed in frequency by genital ulcers, variable skin lesions, arthritis, uveitis, thrombophlebitis, and gastrointestinal and central nervous system disorders.1
Ocular manifestations of BD cause retinal vasculitis and uveitis, which are important as causative diseases of visual impairment.2 Ocular adnexal involvement is rare in BD, but there have been several reports.3, 4, 5, 6, 7, 8 In this report, we describe a case of orbital myositis diagnosed with diplopia and ocular pain as the initial symptoms, with BD developing during the course of the disease.
2. Case report
A 32-year-old woman was referred to the eye center of Toyama University Hospital, complaining of eye pain, redness, and eyelid swelling in the right eye that had persisted for a month. Best-corrected visual acuity was 20/32 on the right, and 20/16 on the left.
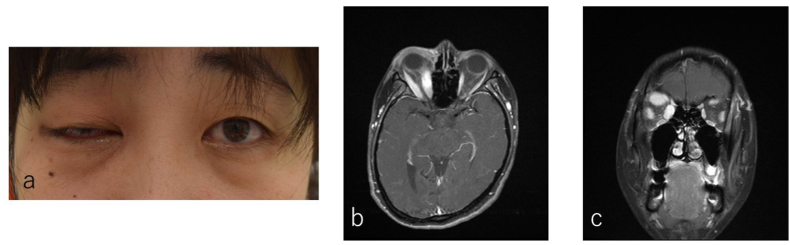
The patient's eyelid swelling on the right (Fig. 1a) was accompanied by ocular motility disorder in all directions. Conjunctival hyperemia was present, but there was no other finding of uveitis. Blood tests showed elevated complement titer, CRP, and platelet count, but no other specific abnormalities. Serum thyroid hormone levels, thyroid autoantibodies and IgG4 were also normal. Orbital contrast magnetic resonance imaging (MRI) showed enlargement and contrast effects in the eyelid and the superior, medial, lateral, and inferior rectus muscles of the right eye (Fig. 1b and c). We therefore diagnosed her as idiopathic orbital inflammation.
Fig. 1.
Imaging tests at initial examination. a. Photo of face. b,c. Orbital contrast magnetic resonance imaging (MRI).
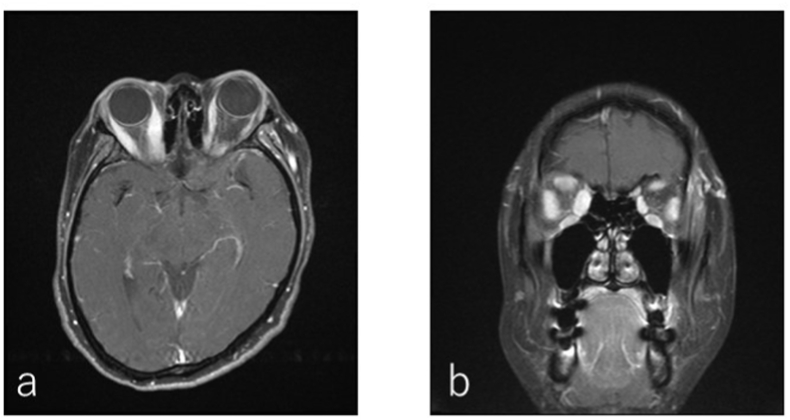
Two pulses of intravenous methylprednisolone therapy (mPSL, 1000 mg/day for 3 consecutive days) were performed for right eye pain due to orbital inflammation. During tapering of prednisolone (PSL) to 15 mg/day, the patient complained of steroid-induced full-moon appearance. MRI images taken after a two pulses treatment showed not only mild inflammation of the superior rectus muscle, but also orbital myositis in both eyes (Fig. 2a and b). Three months later, when the PSL dose was tapered to 10 mg/day, she had severe pain in the left eye and MRI contrast effects in the rectus muscles of both eyes. She received one more mPSL pulse therapy, followed by administration of PSL and cyclosporine. After 18 months, dose of PSL could be reduced to 5 mg/day in combination with cyclosporine.
Fig. 2.
MRI images after two courses of intravenous methylprednisolone pulse.
At the same time, oral aphthae, genital ulcers, and folliculitis-like skin rash appeared, and the patient was diagnosed with incomplete BD by internal medicine. She never experienced uveitis at any point during the course of the disease. Human leukocyte antigen was A26, A26, B7, B62, DR1, DR4. Although she had no abdominal symptoms, gastrointestinal endoscopy revealed an ulcer at the ileum, and intestinal BD was suspected.
We tried to increase the dose of cyclosporine and to change to methotrexate and tacrolimus, however, the effect was not sufficient and the drugs were discontinued due to side effects such as nausea. The dose of PSL was temporarily increased to 10 mg/day, eventually tapered to 6 mg/day. The recurrence of orbital inflammation was suppressed.
3. Discussion
Orbital myositis is a subtype of idiopathic orbital inflammation, in which inflammation of the external ocular muscles causes symptoms such as proptosis, periocular pain, and diplopia.9,10 Typical cases of orbital inflammation include sudden onset, unilateral, painful, non-infectious orbital inflammation, which is more common in women in their 30s and 40s.9 Systemic corticosteroid administration is the first choice of treatment.11, 12, 13 In this case, the patient was refractory to corticosteroid treatment and the side effects made it difficult to continue treatment. It has been reported that recurrence of orbital inflammation and side effects during tapering of PSL dose can make corticosteroid therapy difficult,12, 13, 14 and immunosuppressive agents may be used in combination.15, 16, 17 In this case, the combination of cyclosporine and tacrolimus allowed us to reduce the dose of PSL, and the orbital inflammation did not recur, suggesting a relatively good course.
The mechanism of idiopathic orbital inflammation has not been elucidated, but it has been suggested that it may be an autoimmune disorder.18, 19, 20 Orbital inflammation has been reported to be secondary to systemic diseases such as sarcoidosis,21 granulomatosis with polyangiitis,22 and Crohn's disease.23 In addition, there are several reports of orbital inflammation associated with BD.3, 4, 5 These systemic inflammatory diseases are thought to cause inflammatory infiltration into the orbit, including the external ocular muscle.22 The histologic findings of orbital inflammation vary widely, include vasculitis.18 The vasculitis is characteristic of BD, not only in the retina but also throughout the body. So it may be difficult to distinguish between the two diseases histopathologically. HLA-B * 51 and increased IL-17 response seems to have an important role in BD.24 On the other hand, Chen and colleagues reported that patients with orbital inflammation exhibited obvious increases of Tregs in peripheral blood and affected orbital tissues.25 They also described that circulating Tregs from patients were significantly more polarized to a Th17-like phenotype. Although there are still many unknowns between BD and orbital inflammation, the two diseases may share a common etiology.
The four main features of BD are recurrent oral aphthae, genital ulcers, skin lesions, and uveitis. In this case, there was no finding of uveitis, and the patient was diagnosed as incomplete type with the three main features. In the International Criteria for Behçet's Disease (ICBD), ocular lesions are also important in the diagnosis.26 It may be necessary to consider whether orbital inflammation should be included in the diagnosis of ocular lesions. Considering the reports on combined cases of BD and orbital inflammation,3, 4, 5, 6, 7, 8 we believe that this is a case of orbital inflammation that has come to the fore rather than retinal vasculitis or uveitis, against a background of systemic vasculitis in BD.
In addition, this case was diagnosed as idiopathic orbital inflammation due to the lack of systemic symptoms at the time of initial diagnosis, and administration of systemic corticosteroid was initiated. However, the patient was refractory to corticosteroid therapy, and symptoms appeared in both eyes during the course of treatment. This is considered to be an atypical case of idiopathic orbital inflammation, and further investigation of inflammatory and autoimmune diseases, including BD, was necessary at that time. The efficacy of immunosuppressive agents and infliximab has been reported for BD-related orbital inflammation.4,5 Therefore, early treatment with these agents is considered necessary for symptom relief.
In conclusion, orbital inflammation, including orbital myositis, may be the first symptom of BD. The risk of developing BD should be considered, especially when a case presents with atypical orbital inflammation.
Patient consent
The patient gave her written informed consent to publish the case (including publication of images).
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: SA, TY, AH.
Acknowledgments
None.
References
- 1.Yurdakul S., Yazici H. Behcet's syndrome. Best Pract Res Clin Rheumatol. 2008 Oct;22(5):793–809. doi: 10.1016/j.berh.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Tugal-Tutkun I., Gupta V., Cunningham E.T. Differential diagnosis of behçet uveitis. Ocul Immunol Inflamm. 2013 Oct;21(5):337–350. doi: 10.3109/09273948.2013.795228. [DOI] [PubMed] [Google Scholar]
- 3.Hammami S., Yahia S.B., Mahjoub S., Khairallah M. Orbital inflammation associated with Behcet's disease. Clin Exp Ophthalmol. 2006 Mar;34(2):188–190. doi: 10.1111/j.1442-9071.2006.01181.x. [DOI] [PubMed] [Google Scholar]
- 4.Dursun D., Akova Y., Yücel E. Myositis and scleritis associated with Behcet's disease: an atypical presentation. Ocul Immunol Inflamm. 2004 Dec;12(4):329–332. doi: 10.1080/092739490500264. [DOI] [PubMed] [Google Scholar]
- 5.Garrity J.A., Coleman A.W., Matteson E.L., et al. Treatment of recalcitrant idiopathic orbital inflammation (chronic orbital myositis) with infliximab. Am J Ophthalmol. 2004 Dec;138(6):925–930. doi: 10.1016/j.ajo.2004.06.077. [DOI] [PubMed] [Google Scholar]
- 6.Chebbi W., Jerbi S., Ammari W., et al. Orbital myositis in Behçet's disease. Joint Bone Spine. 2014 May;81(3):264. doi: 10.1016/j.jbspin.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Bouomrani S., Farah A., Bouassida N., et al. [Orbital inflammatory pseudotumor with optic neuritis in Behçet's disease] J Fr Ophtalmol. 2012 Jun;35(6) doi: 10.1016/j.jfo.2011.08.018. 439.e1-6. Article in French. [DOI] [PubMed] [Google Scholar]
- 8.Roh J.H., Koh S.B., Kim J.H. Orbital myositis in Behçet's disease: a case report with MRI findings. Eur Neurol. 2006;56(1):44–45. doi: 10.1159/000095142. [DOI] [PubMed] [Google Scholar]
- 9.Montagnese F., Wenninger S., Schoser B. Orbiting around" the orbital myositis: clinical features, differential diagnosis and therapy. J Neurol. 2016 Aapr;263(4):631–640. doi: 10.1007/s00415-015-7926-x. [DOI] [PubMed] [Google Scholar]
- 10.Kennerdell J.S., Dresner S.C. The nonspecific orbital inflammatory syndromes. Surv Ophthalmol. 1984 Sep-Oct;29(2):93–103. doi: 10.1016/0039-6257(84)90166-8. [DOI] [PubMed] [Google Scholar]
- 11.Siatkowski R.M., Capó H., Byrne S.F., et al. Clinical and echographic findings in idiopathic orbital myositis. Am J Ophthalmol. 1994 Sep 15;118(3):343–350. doi: 10.1016/s0002-9394(14)72959-9. [DOI] [PubMed] [Google Scholar]
- 12.Mombaerts I., Koornneef L. Current status in the treatment of orbital myositis. Ophthalmology. 1997 Mar;104(3):402–408. doi: 10.1016/s0161-6420(97)30301-7. [DOI] [PubMed] [Google Scholar]
- 13.Yan J., Wu P. Idiopathic orbital myositis. J Craniofac Surg. 2014 May;25(3):884–887. doi: 10.1097/SCS.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 14.Avni-Zauberman N., Tripathy D., Rosen N., et al. Relapsing migratory idiopathic orbital inflammation: six new cases and review of the literature. Br J Ophthalmol. 2012 Feb;96(2):276–280. doi: 10.1136/bjo.2010.191866. [DOI] [PubMed] [Google Scholar]
- 15.Smith J.R., Rosenbaum J.T. A role for methotrexate in the management of non-infectious orbital inflammatory disease. Br J Ophthalmol. 2001 Oct;85(10):1220–1224. doi: 10.1136/bjo.85.10.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gori S., Lucchesi C., Calabrese R., et al. Inferior rectus myositis: a rare cause of painful ophthalmoplegia and a therapeutic challenge. Neurol Sci. 2013 May;34(5):789–791. doi: 10.1007/s10072-012-1128-4. [DOI] [PubMed] [Google Scholar]
- 17.Spindle J., Narang S., Purewal B., et al. Atypical idiopathic orbital inflammation in a young girl. Ophthalmic Plast Reconstr Surg. 2013 May-Jun;29(3):e86–e88. doi: 10.1097/IOP.0b013e318275b649. [DOI] [PubMed] [Google Scholar]
- 18.Espinosa G.M. Orbital inflammatory pseudotumors: etiology, differential diagnosis, and management. Curr Rheumatol Rep. 2010 Dec;12(6):443–447. doi: 10.1007/s11926-010-0128-8. [DOI] [PubMed] [Google Scholar]
- 19.Harris G.J. Idiopathic orbital inflammation: a pathogenetic construct and treatment strategy: the 2005 ASOPRS Foundation Lecture. Ophthalmic Plast Reconstr Surg. 2006 Mar-Apr;22(2):79–86. doi: 10.1097/01.iop.0000203734.52333.93. [DOI] [PubMed] [Google Scholar]
- 20.Dalakas M.C. Therapeutic targets in patients with inflammatory myopathies: present approaches and a look to the future. Neuromuscul Disord. 2006 Apr;16(4):223–236. doi: 10.1016/j.nmd.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Mavrikakis I., Rootman J. Diverse clinical presentations of orbital sarcoid. Am J Ophthalmol. 2007 Nov;144(5):769–775. doi: 10.1016/j.ajo.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 22.Salam A., Meligonis G., Malhotra R. Superior oblique myositis as an early feature of orbital Wegener's granulomatosis. Orbit. 2008;27(3):203–206. doi: 10.1080/01676830701854268. [DOI] [PubMed] [Google Scholar]
- 23.Verma S., Kroeker K.I., Fedorak R.N. Adalimumab for orbital myositis in a patient with Crohn's disease who discontinued infliximab: a case report and review of the literature. BMC Gastroenterol. 2013 Apr 4;13:59. doi: 10.1186/1471-230X-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leccese P., Alpsoy E. Behçet's disease: an overview of etiopathogenesis. Front Immunol. 2019 May 10;10:1067. doi: 10.3389/fimmu.2019.01067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen J., Ye H., Xiao W., et al. Increased dysfunctional and plastic regulatory T cells in idiopathic orbital inflammation. Front Immunol. 2021 May 3;12 doi: 10.3389/fimmu.2021.634847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.International team for the revision of the international criteria for Behçet's disease (ITR-ICBD). The international criteria for Behçet's disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014 Mar;28(3):338–347. doi: 10.1111/jdv.12107. [DOI] [PubMed] [Google Scholar]