Abstract
Systemic inflammation has been suggested to have a pivotal role in atherothrombosis, but the factors that trigger systemic inflammation have not been fully elucidated. Lipopolysaccharide (LPS) is a component of the membrane of Gram-negative bacteria present in the gut that can translocate into the systemic circulation, causing non-septic, low-grade endotoxaemia. Gut dysbiosis is a major determinant of low-grade endotoxaemia via dysfunction of the intestinal barrier scaffold, which is a prerequisite for LPS translocation into the systemic circulation. Experimental studies have demonstrated that LPS is present in atherosclerotic arteries but not in normal arteries. In atherosclerotic plaques, LPS promotes a pro-inflammatory status that can lead to plaque instability and thrombus formation. Low-grade endotoxaemia affects several cell types, including leukocytes, platelets and endothelial cells, leading to inflammation and clot formation. Low-grade endotoxaemia has been described in patients at risk of or with overt cardiovascular disease, in whom low-grade endotoxaemia was associated with atherosclerotic burden and its clinical sequelae. In this Review, we describe the mechanisms favouring the development of low-grade endotoxaemia, focusing on gut dysbiosis and changes in gut permeability; the plausible biological mechanisms linking low-grade endotoxaemia and atherothrombosis; the clinical studies suggesting that low-grade endotoxaemia is a risk factor for cardiovascular events; and the potential therapeutic tools to improve gut permeability and eventually eliminate low-grade endotoxaemia.
Subject terms: Microbiota, Thrombosis
In this Review, the authors describe the mechanisms underlying lipopolysaccharide translocation from the gut to the systemic circulation and the ensuing low-grade endotoxaemia, discuss studies suggesting a role for low-grade endotoxaemia in atherothrombosis and cardiovascular complications, and highlight potential therapeutic strategies to improve gut permeability and eliminate low-grade endotoxaemia.
Key points
Gut permeability can be altered by gut microbiota dysbiosis, favouring lipopolysaccharide (LPS) translocation into the systemic circulation, with ensuing development of low-grade endotoxaemia.
Low-grade endotoxaemia induces an inflammatory state in the arterial wall that ultimately leads to initiation and progression of atherosclerosis.
Low-grade endotoxaemia has effects on several cell types, such as leukocytes, platelets and endothelial cells, shifting them to a procoagulant phenotype that contributes to thrombosis.
Gut permeability-derived low-grade endotoxaemia might contribute to atherosclerosis and be associated with cardiovascular events in patients at risk of or with overt cardiovascular disease.
Modulation of gut permeability-derived low-grade endotoxaemia is a potential tool to counteract inflammation-related atherothrombosis and its clinical sequelae.
Introduction
Atherosclerosis is a multifactorial disease associated with many risk factors, such as smoking, type 2 diabetes mellitus, obesity, hypertension and metabolic syndrome. Lipid-driven chronic inflammation is a typical feature of atherosclerosis that is initiated by LDL accumulation in the arterial wall and its modification by oxidative stress-mediated mechanisms1–4. LDL accumulation results in the recruitment of macrophages, dendritic cells and lymphocytes. The absence of tissue repair or a defect in the resolution of inflammation leads to atherosclerotic lesion progression, characterized by the formation of a central necrotic core and the presence of inflammatory cells5. Persistent inflammatory stimuli owing to continuous accumulation of LDL in the arterial intima, coupled with impaired efferocytosis and an inflammatory plaque phenotype leads to plaque instability and eventual thrombosis5. The central role of inflammation in the atherosclerotic process is supported by interventional studies performed in the past decade showing that the risk of cardiovascular disease can be attenuated with the use of anti-inflammatory therapies6,7. A more detailed definition of the mechanisms underlying inflammation-related cardiovascular disorders such as atherothrombosis could help identify novel therapeutic approaches to preventing atherosclerotic progression.
The gut microbiota comprises trillions of microbes, including bacteria, archaea and viruses, that colonize the entire gut from the stomach to the small intestine and, to a major extent, the colon8. Gut dysbiosis is an alteration of the gut microbiome characterized by a reduction in microbial diversity, with predominance of bacteria such as Bacteroidetes and Enterococcaceae and a reduction in Bifidobacterium and Firmicutes9. A growing body of evidence indicates that gut dysbiosis is implicated in the atherothrombotic process via increased translocation of viable bacteria or bacterial products such as lipopolysaccharides (LPS) and trimethylamine-N-oxide (TMAO) into the systemic circulation10.
Translocation of LPS into the systemic circulation has negative effects on body homeostasis, shifting the host immune defence to a pro-inflammatory state, which has been shown to predispose to atherosclerosis11,12 (Box 1). LPS is a pathogen-associated molecular pattern, and is recognized by innate immune system receptors, such as Toll-like receptors (TLRs), a family of highly conserved, membrane pattern-recognition receptors that are implicated in atherosclerotic and thrombotic processes13–15. For example, TLR2, TLR4 and TLR9 are involved in platelet activation and thrombus formation16,17.
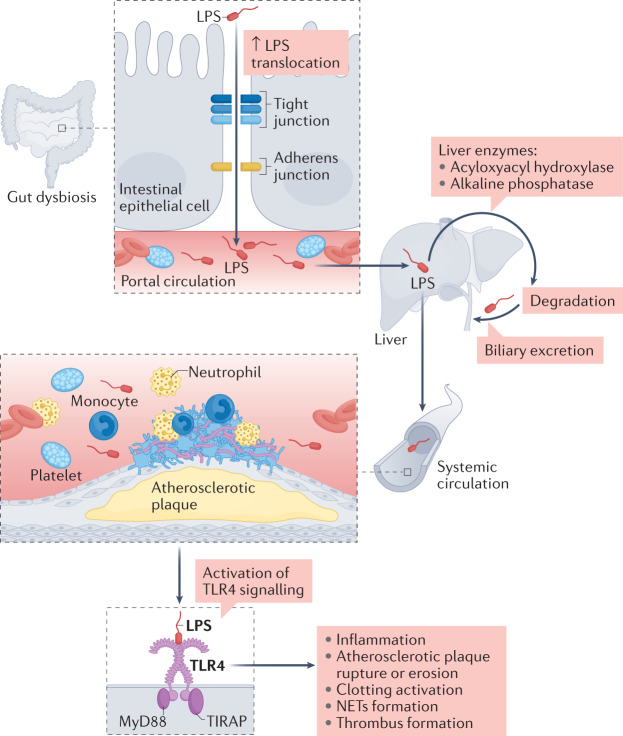
Together, these data indicate the existence of a gut–systemic circulation axis, which might contribute to atherothrombosis via a sequence of events including increased LPS translocation from the gut to the portal circulation and impaired degradation of LPS in the liver. The LPS can then reach the systemic circulation to induce arterial inflammation and ultimately thrombus growth via binding to TLR4 (Fig. 1). In this Review, we describe the mechanisms underlying LPS translocation from the gut to the systemic circulation and the ensuing low-grade endotoxaemia, the effect of low-grade endotoxaemia on the atherosclerotic and thrombotic processes, the clinical settings associated with low-grade endotoxaemia and cardiovascular complications, and the potential therapeutic tools to improve gut permeability and eventually eliminate low-grade endotoxaemia.
Fig. 1. Interplay between low-grade endotoxaemia and vascular disease.
Lipopolysaccharide (LPS) can translocate into the systemic circulation as a consequence of downregulation of intestinal adhesion proteins induced by gut dysbiosis. LPS is metabolized by liver cell enzymes and excreted through the bile. However, if degradation and biliary excretion are impaired, LPS can reach the systemic circulation. In the arteries, LPS can bind to Toll-like receptor 4 (TLR4) in leukocytes, endothelial cells and platelets. TLR4 activation leads to the recruitment of the TIRAP–MyD88 complex and downstream signalling, eliciting an inflammatory response that induces plaque instability (which can lead to rupture and erosion), leukocyte activation with the formation of neutrophil extracellular traps (NETs), clotting activation and thrombus formation.
Box 1 Sources of LPS and endotoxaemia.
Commensal microorganisms colonize all skin and mucosal surfaces in vertebrates. Distinct site-specific microbes reside in different body habitats, including the gastrointestinal tract, oral cavity, skin surface, genital and urinary tracts, and respiratory tract.
The majority of microbes are located in the gastrointestinal tract, which hosts approximately 100 trillion commensal organisms144, including Gram-negative bacteria. Lipopolysaccharide (LPS) is the major component of the outer membrane of Gram-negative bacteria, which makes the gut bacteria the major source of LPS, contributing to an enteric reservoir of up to 1 g of LPS145–147.
Microbial diversity, density and abundance increase steadily along the gastrointestinal tract according to the heterogeneity of each segment. Very few bacteria are resistant to the acidic milieu of the stomach (101 bacteria per gram of tissue), whereas the colon has higher bacterial density and diversity (1012 bacteria per gram of tissue)148. Most human gut microorganisms belong to the phyla Bacteroidetes, Firmicutes and Proteobacteria148. An abnormal expansion of the phylum Proteobacteria149 and the alteration of the Firmicutes to Bacteroidetes ratio150 compromises the gut microbiome, leading to gut dysbiosis and altered gut-barrier functionality.
The oral cavity has diverse microbial communities and is the second largest bacterial reservoir after the lower gastrointestinal tract151. Subgingival plaque is the niche in the oral cavity with the highest richness and diversity of species, which typically are Gram-negative Bacteroidetes, Fusobacterium, Proteobacteria, Saccharibacteria and Spirochaetes, and Gram-positive Firmicutes and Actinobacteria152. The oral microbiota is involved in the aetiology of local diseases, such as dental caries and periodontal disease153. However, endotoxin from oral bacteria can disseminate into the circulation through inflamed periodontium, resulting in chronic inflammatory diseases at distant sites, such as bacterial endocarditis154, atherosclerosis and diabetes mellitus155, and respiratory infection and diseases156,157.
The skin is a biologically active ecosystem of microbial communities. The composition of these microbial communities varies across different body sites and individuals, influenced by different host characteristics, including age, sex, diet and lifestyle factors. Healthy skin microbiota primarily consists of four phyla: Actinobacteria, Firmicutes, Proteobacteria and Bacteroidetes158. Several factors, such as infection and the use of antibiotics, can cause a shift in microbiome composition, altering the host immune response by promoting the production of pro-inflammatory cytokines. Inflammation in turn impairs skin homeostasis, facilitating immune cell infiltration and physical destruction of the skin barrier, which ultimately results in microbial escape from typical niches and penetration into sterile tissues159.
Microbial communities in the urinary tract (the urinary microbiome or ‘urobiome’) help in the maintenance of bladder homeostasis by ensuring the integrity of the urinary tract epithelium, protecting against infections and promoting the proper functioning of the immune system. The main phyla in the urinary tract are Proteobacteria, Firmicutes, Actinobacteria and Bacteroidetes160. Uropathogens, in particular uropathogenic Escherichia coli, express specific surface virulence factors, including adhesive fimbriae (by which bacteria adhere avidly to specific receptors on the urothelium, establishing infection in the urinary tract) and flagella (contributing to ascending E. coli infection to the kidney)161. Moreover, uropathogenic E. coli secrete toxins, such as the lipoprotein α-haemolysin, cytotoxic necrotizing factor 1 and autotransporter toxins, which disrupt the epithelial barrier and enable access to the underlying tissue162.
Low-grade endotoxaemia and gut permeability
Low-grade endotoxaemia
According to studies performed in healthy individuals, low-grade endotoxaemia is defined as circulating levels of LPS of >20 ng/ml15,18,19. Compared to patients with sepsis, low-grade endotoxaemia is characterized by at least twofold lower blood LPS levels13,20 and absence of a specific clinical picture. Low-grade endotoxaemia can occur as a consequence of gut microbiota dysbiosis and disruption of intestinal barrier function21.
LPS is a glycolipid component of the outer membrane of Gram-negative bacteria and is composed of carbohydrates and a lipid A portion. LPS levels in the peripheral circulation usually increase after food intake, coinciding with elevation in the levels of apolipoprotein B48, a protein synthetized by intestinal cells to transport chylomicrons in the peripheral circulation22. LPS is embedded in newly synthesized chylomicrons and passes across the intestinal barriers into the lymphatic system and then into the bloodstream23,24. In the bloodstream, LPS is transported by the LPS-binding protein, a specific 60-kDa acute-phase response glycoprotein, and cleared from the blood circulation by plasma lipoproteins including HDL, LDL and VLDL25,26. HDL is the main lipoprotein implicated in LPS transport and clearance by hepatic bile, and the HDL–LPS interaction directly protects against the toxic effect of LPS, as shown in vitro and in vivo27–29. In normal settings, LPS is transported to the liver, where it undergoes degradation by specific liver enzymes (such as acyloxyacyl hydroxylase and alkaline phosphatase) or excretion into the bile via scavenger receptors30. The inability of liver cells to completely metabolize or excrete LPS into the bile might have consequences not only in the establishment of low-grade endotoxaemia but also in inducing liver damage, such as non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH)31. The pro-inflammatory damage induced by LPS occurs via binding of its lipid moiety lipid A to TLR4 (ref.32), which binds LPS via the membrane-bound co-receptor CD14 (ref.33). LPS binding to TLR4 leads to the recruitment of the adaptor protein myeloid differentiation primary response protein 88 (MyD88) to the cytoplasmic domain of TLR4 (ref.34), resulting in activation of the transcription factor NF-κB35.
Gut barrier and permeability
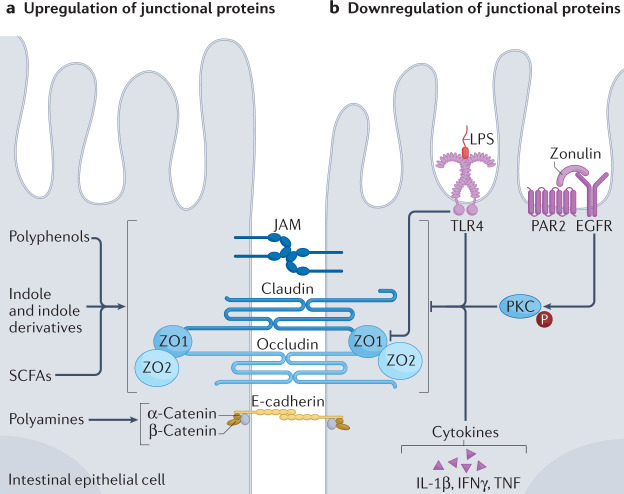
The human intestine has several lines of defence that protect against the translocation of microorganisms or microbial products into the bloodstream. This multilayer barrier constitutes the largest interface between the external environment and the host. The first line of defence consists of mucus that separates the gut microbiota from a single layer of different types of epithelial cells that forms the intestinal epithelial barrier36,37. The continuous intercellular barrier of intestinal epithelial cells tightly regulates the absorption, secretion and transport of water, ions and organic molecules across the epithelium38. The intestinal epithelial barrier consists of a physical barrier formed by the apical plasma membrane of enterocytes, which are held together by tight junction proteins, adherens junction proteins (cadherins and catenins), gap junction proteins (connexins) and desmosomes (desmoglein and desmocollins)39 (Fig. 2). Tight junction proteins are the most apical junctional complex regulating gut permeability and paracellular diffusion and, therefore, are crucial for maintaining cell-to-cell adhesion and gut barrier health40. The tight junction complex includes transmembrane proteins, such as claudins, occludin, tricellulin and junctional adhesion molecules, and intracellular scaffold proteins such as the zonula occludens proteins ZO1, ZO2 and ZO3 that bind the transmembrane structure to the cytoskeleton40,41 (Fig. 2). The gut–vascular barrier, an additional cellular barrier, is situated below the epithelial barrier and is also involved in controlling the translocation of microorganisms into the portal vein42,43.
Fig. 2. Mechanisms of gut permeability-mediated low-grade endotoxaemia.
The gut epithelial barrier consists of the apical plasma membrane of enterocytes, held together by tight junction proteins (claudin and occludin) and adherens junction proteins (E-cadherin and catenin), as well as the zonula occludens proteins ZO1 and ZO2, which are adaptor proteins necessary for the structural and regulatory functions of tight junctions. a | Upregulation of junctional proteins can be induced by microbiota metabolites including polyphenols, indole and indole derivatives, short-chain fatty acids (SCFAs) and polyamines. b | Downregulation of junctional proteins is mediated by: lipopolysaccharides (LPS) through binding to Toll-like receptor 4 (TLR4); by zonulin, a protein that activates the EGF receptor (EGFR) through transactivation of the proteinase-activated receptor 2 (PAR2), thereby inducing protein kinase C (PKC) phosphorylation; and by pro-inflammatory cytokines, including IL-1β, interferon-γ (IFNγ) and tumour necrosis factor (TNF). JAM, junctional adhesion molecules.
Gut barrier permeability is regulated by intrinsic and extrinsic mechanisms in the intestinal epithelial cells, and can be altered by exogenous factors, such as excessive alcohol intake and non-steroidal anti-inflammatory drugs, or endogenous factors, such as inflammation linked to systemic disease40. The gut microbiota has a protective role in the digestive mucosa by participating in the maintenance of the physiological integrity of tight junction proteins44. The gut microbiota generates a variety of metabolites from dietary products that have important effects on gut barrier function and immune responses45. Microbiota metabolites with a protective role for the gut barrier include short-chain fatty acids (SCFA), indole and indole derivatives (which are generated from tryptophan microbial digestion40), bile acid metabolites, polyamines and polyphenols (Fig. 2). Moreover, gut dysbiosis is a prerequisite for the modification of gut barrier functionality and the translocation of microorganisms or microbial products into the systemic circulation40. For example, in animal models of diabetes and obesity, treatment with a large spectrum of antibiotics reduced the levels of LPS in the systemic circulation coincidentally with a reduction in gut permeability via upregulation of tight junction proteins such as ZO1 and occludin20.
Diet is an important factor affecting gut permeability. In rats fed a high-fat diet, changes in gut microbiota are characterized by an imbalance in the ratio of Gram-negative to Gram-positive bacteria that might predispose to alterations in gut barrier defence21. The relationship between a high-fat diet, metabolic disease and blood LPS levels was first outlined by Cani and colleagues13,20. They demonstrated in mouse models that a 4-week high-fat diet chronically increased the plasma LPS concentration two to five times, corresponding to one to two orders of magnitude lower than the levels attained with infections46. The high-fat diet also affected gut barrier integrity by reducing the number of Bifidobacteria20, which have been shown to protect intestinal barrier integrity via upregulation of tight junction proteins such as ZO1 and occludin47. Finally, Cani and colleagues showed that chronic, experimental metabolic endotoxaemia induced by LPS infusion triggered the development of obesity, diabetes and liver insulin resistance, mimicking the negative effects elicited by a high-fat diet alone20.
Ageing is another important factor in gut barrier dysfunction, which in turn can promote low-grade systemic inflammation, a characteristic observed in older individuals48. A reduction in gut microbiota diversity and an imbalance between opportunistic and commensal bacteria (with increased numbers of opportunistic bacteria such as Enterobacteriaceae, Clostridium perfringens and Clostridium difficile, and decreased numbers of commensal bacteria such as Bacteroides, Bifidobacteria and Lactobacilli) have been reported in older individuals49,50. Age-related gut dysbiosis negatively influences gut barrier permeability and is responsible for translocation of microbial products into the systemic circulation, with ensuing systemic inflammation and ultimately impaired bacteria-killing immune responses51.
Together, these data indicate that diet-induced gut microbiota alterations are the primum movens of a sequence of events including dysbiosis-mediated increase in gut permeability, in which LPS has a key role in the disassembly of intestinal adhesion proteins (Fig. 2). LPS binding to TLR4 in intestinal cells begets an inflammatory process that ultimately downregulates the levels of tight junction proteins and favours the translocation of LPS into the systemic circulation. Several studies in experimental models using TLR4 inhibitors or Tlr4-knockout animals have demonstrated a crucial role for the LPS–TLR4 pathway in modulating gut barrier integrity52–55. Nevertheless, the intestinal barrier includes factors that can protect from LPS-induced damage. For example, intestinal alkaline phosphatase (IAP) removes one of the two phosphate groups of the LPS lipid A moiety, resulting in LPS degradation to monophosphoryl LPS, which can still bind to TLR4 but acts as antagonist56. In animals fed a high-fat diet, IAP overexpression improved intestinal function by maintaining the integrity of intestinal mucosa, thereby reducing LPS translocation into the systemic circulation and lipid accumulation in the liver, resulting in the attenuation of atherosclerotic plaque burden57. Biosynthesis of HDL subspecies, such as HDL3, by intestinal cells is another tool to counteract LPS pro-inflammatory activity, given that HDL3 can sequester LPS in the portal vein, thereby preventing its binding to TLR4 on liver macrophages and protecting against liver damage58.
Gut permeability and cardiovascular risk
Emerging evidence indicates that gut dysbiosis is a risk factor for cardiovascular disease in mice with type 1 diabetes mellitus59, obesity60 or hypertension10. Studies to assess gut permeability in patients at risk or with coronary heart disease have mostly been conducted by measuring serum levels of zonulin, which is an indirect marker of gut permeability. Zonulin is a 47-kDa protein released by epithelial cells of the small intestine after stimulation by gliadin or gut dysbiosis61. In interstitial epithelial cells, the signalling pathway downstream of zonulin leads to protein kinase C phosphorylation, which triggers the disassembly of tight junction proteins such as ZO1 (ref.62). Increased serum levels of zonulin together with elevated levels of LPS have been detected in individuals with type 2 diabetes, obesity63–65 or acute or chronic cardiovascular disease15 compared with the levels in healthy individuals. Increased gut permeability and low-grade LPS endotoxaemia related to gut dysbiosis have also been detected in patients with non-septic pneumonia19,66,67 or in the acute phase of myocardial infarction, as well as in experimental models of intestinal anoxia40,68 and systemic inflammation-associated overproduction of pro-inflammatory cytokines, such as interferon-γ and tumour necrosis factor (TNF)67 (Fig. 2).
Of note, given that analysis of serum zonulin levels is an indirect measure of gut permeability, other assays should be used to assess changes in gut permeability in humans. In this regard, analysis of d-lactate might be an alternative approach because an increase in d-lactate levels in the blood is considered to be a marker of increased intestinal permeability secondary to bacterial infection or experimentally induced gut injury69,70. However, measurement of urinary excretion of dextrose and mannitol after oral ingestion is likely to be a better approach for analysing gut burrier dysfunction because dextrose and mannitol are absorbed through the paracellular and transcellular pathways, respectively71, but such an analysis is cumbersome and requires specific expertise72. Nevertheless, the relationship between gut permeability and low-grade endotoxaemia in patients at risk of or with cardiovascular disease should be further investigated.
LPS and atherosclerosis
Atherogenesis is a complex process that is thought to be initiated by LDL crossing the arterial wall, where LDL is trapped in the subendothelial layer and undergoes oxidative changes that lead to the formation of oxidized LDL (oxLDL)73. OxLDL elicits recruitment of inflammatory cells, production of inflammatory cytokines and a shift in endothelial cells to a pro-atherogenic phenotype, all of which perpetuate the inflammation in the arterial intima74. The relevance of oxidative stress in atherogenesis has been supported by evidence of impaired macrophage uptake of oxLDL in patients undergoing carotid endarterectomy who received vitamin E (which has antioxidant properties) and injected with native radiolabelled LDL75.
Experimental studies have suggested that gut dysbiosis is involved in the aforementioned mechanisms of atherosclerosis by promoting the development of metabolic diseases that favour arterial inflammation, such as dyslipidaemia, obesity and hypertension10,76. Pathogenic gut microbiota are more frequent in patients with symptomatic atherosclerosis than in those with asymptomatic atherosclerosis, and are predictive of the risk of coronary heart disease76–78. Further support for the connection between gut microbiota and cardiovascular disease has been provided by studies in germ-free mouse models that have shown a causal link between gut dysbiosis, hypertension, vascular dysfunction, systemic inflammation and atherothrombosis10,51,79.
In this context, data on the role of LPS in atherosclerosis might provide insights into the mechanisms linking gut microbiota to atherosclerosis and its complications. LPS is a pro-atherogenic molecule through its pro-oxidant properties, which are mediated by the activation of NOX2 (ref.80), the catalytic core of NADPH oxidase, among the most important cellular producers of reactive oxygen species (ROS). LPS concentrations similar to those found in the plasma of individuals without sepsis amplified platelet responses in vitro to common agonists via TLR4-mediated, NOX2-derived ROS formation, which is a mechanism favouring LDL oxidation81–83. A significant correlation between the presence of low-grade endotoxaemia and elevated circulating levels of oxLDL has been found in patients with impaired fasting glucose84, which provides indirect evidence for the pro-oxidant properties of LPS.
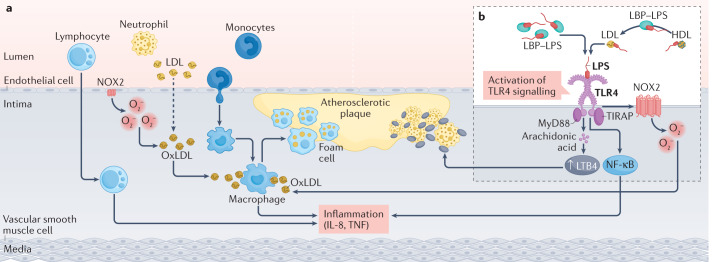
Support for the putative role of LPS in atherosclerosis has been provided by immunohistochemistry analysis of carotid atherosclerotic plaques from patients undergoing endarterectomy, which revealed the presence of LPS adjacent to plaque macrophages with high TLR4 levels85. By contrast, LPS was not detected in atherosclerosis-free thyroid arteries from the same patients85. In humans, LPS in circulation is mostly bound to lipoproteins (80–97%)86,87, with the highest concentration in LDL (35.7%) and the lowest in VLDL (13.9%)88. However, VLDL particles carry a higher number of LPS molecules88. The observation that circulating LPS is transported by pro-atherogenic lipoproteins, such as VLDL and LDL, might be relevant in the pathogenesis of atherosclerosis. LPS could enter the arterial wall bound to these pro-atherogenic lipoproteins, which would favour LDL oxidation89 and thereby contribute to propagation of arterial inflammation. A further contributor to the pro-atherogenic process is LPS-binding protein-mediated LPS transfer from HDL to LDL26 (Fig. 3).
Fig. 3. Mechanisms of LPS-mediated atherosclerosis.
a | LDL can cross into the arterial wall and undergo oxidation in the subendothelial space, leading to the formation of oxidized LDL (oxLDL). OxLDL is taken up by macrophages, inducing foam cell formation and inflammatory cytokine production. b | Lipopolysaccharides (LPS) can cross into the arterial wall, either together with LPS binding protein (LBP) or by LBP-mediated LPS transfer from HDL to LDL particles. LPS binds to Toll-like receptor 4 (TLR4) in several cell types, leading to phosphorylation of Toll–interleukin-1 receptor domain-containing adaptor protein (TIRAP) and recruitment of the myeloid differentiation primary response protein 88 (MyD88) to the cytoplasmic domain of TLR4. Downstream signalling induces the activation of the transcription factor nuclear factor-κB (NF-κB), which increases the production of pro-inflammatory cytokines, such as IL-8 and tumour necrosis factor (TNF); oxidative stress via upregulation of NADPH oxidase 2 (NOX2)-derived reactive oxygen species, which further promotes LDL oxidation; and destabilization of the atherosclerotic plaque via activation of the arachidonic acid pathway and biosynthesis of leukotriene B4 (LTB4), which attract leukocytes to the atherosclerotic lesion. O2−, superoxide.
Experiments in animal models have been conducted to substantiate the role of LPS as a trigger of atherosclerosis. One study found that a single LPS infusion induced a profound systemic inflammatory response without changes to the atherosclerotic plaque90. However, other experiments have consistently shown an association between LPS infusion and arterial injury91,92. Daily intravenous or intraperitoneal LPS infusions in animals accelerated atherosclerosis in the aorta, together with increased production of pro-inflammatory cytokines, such as IL-8 and TNF, and autoantibodies against oxLDL, and increased accumulation of activated lymphocytes and deposition of IgG and IgM in the arterial intima91,92. In isolated human saphenous vein samples, LPS at concentrations as low as 0.1 ng/ml increased the production of ROS and chemotactic cytokines, such as IL-8 and CCL2, via interaction with TLR4 (ref.93). These changes were mitigated by administration of statins, which are known to have antioxidant properties beyond their LDL-lowering effect94. The relevance of the LPS–TLR4 axis in atherogenesis is further supported by studies in mice. In atherosclerosis-prone hypercholesterolaemic Apoe−/− mice, LPS-induced TLR4 activation increased neointima formation, whereas lack of either the adaptor molecule MyD88 or its upstream receptor TLR4 reduced atherosclerotic burden95,96. Tlr4−/−Ldlr−/− mice fed a carbohydrate-rich diet or a control diet had markedly reduced aortic atherosclerotic lesion areas compared with Ldlr−/− mice97.
In accordance with these experiments, the analysis of human atherosclerotic plaques revealed TLR4 overexpression in several cells types, including macrophages, vascular smooth muscle cells and dendritic cells14,98. However, it is unclear whether TLR4 overexpression is mediated by LPS or other TLR4 ligands, such as oxLDL, cleaved fibrinogen or heparin sulfate proteoglycan. Furthermore, studies in patients with the Asp299Gly variant in the TLR4 region on chromosome 9, which is associated with impaired TLR4 signalling, have provided inconclusive results14.
LPS has also been shown to destabilize atherosclerotic lesions, which renders the atherosclerotic plaque more vulnerable to rupture or erosion. Intratracheal injection of LPS in Apoe−/− mice fed a Western diet99 induced progression from stable to unstable phenotypes in aortic arch atherosclerotic plaques; histological features of plaque vulnerability included reduced cap thickness, leukocyte infiltration, increased necrotic core and thrombus formation at the edges of atherosclerotic plaque99. Consistent with these findings, a marked increase in atherosclerotic plaque size was detected in hypercholesterolaemic mice after a single LPS infusion mimicking the acute endotoxaemia detectable during infections100. Plaque instability was caused by acute inflammation of the arterial wall via leukocyte infiltration and the ensuing formation of neutrophil extracellular traps (NETs)100. A potential mechanism for LPS-induced plaque instability is activation in atherosclerotic lesions of the arachidonic acid pathway that leads to biosynthesis of leukotrienes, such as leukotriene B4 (LTB4), which are potent attractants of leukocytes101. In Apoe−/− mice, injection of 1.5 mg/kg of LPS each day for 5 days resulted in overproduction of LTB4 in atherosclerotic plaques, infiltration of leukocytes into the subluminal area and plaque destabilization, as indicated by increased collagen digestion, increased necrotic core size and reduced cap thickness101. The relevance of LTB4 in leukocyte-mediated atherosclerotic plaque progression was indicated by attenuation of arterial inflammation in mice with a deficiency in polyunsaturated fatty acid 5-lipooxygenase, the enzyme that converts arachidonic acid to LTB4 (ref.101) (Fig. 3).
LPS and thrombosis
Studies have shown that gut microbiota might be implicated in the atherothrombotic process and suggested production of TMAO as a potential mechanism79,102. LPS translocation into the systemic circulation might be another pathway.
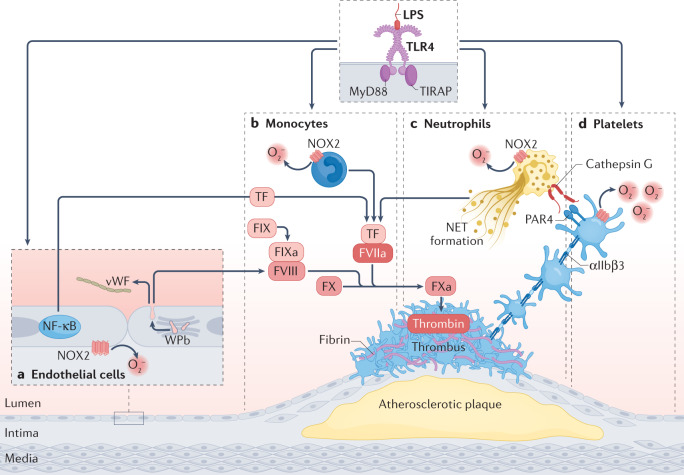
The relationship between low-grade endotoxaemia and thrombosis was first hypothesized based on observations in patients with advanced liver disease, who have an increased risk of bleeding and thrombotic complications in the portal and peripheral circulation103–105. Low-grade endotoxaemia was detected in both vascular trees in these patients and was associated with increased biosynthesis and activity of tissue factor in monocytes106, a glycoprotein that converts factor X to factor Xa after binding to factor VIIa107. Stimulation of human monocytes with LPS in vitro resulted in increased thrombin generation, an effect that was blunted by treatment with the antioxidant vitamin E108. In endothelial cells in vitro, LPS addition caused a shift to a prothrombotic phenotype characterized by overexpression of tissue factor and overproduction of thrombin-activatable fibrinolysis inhibitor (also known as carboxypeptidase B2) and plasminogen activator inhibitor 1 (refs.109,110). Overexpression of tissue factor by LPS-treated mouse endothelial cells in vitro was related to LPS binding to TLR4 because tissue factor activity and mRNA were significantly higher in wild-type endothelial cells than in Tlr4−/− endothelial cells111. Under the same experimental conditions, LPS-induced tissue factor activation was inhibited in wild-type endothelial cells by pre-treatment with an anti-TLR4 antibody111. Further evidence of the prothrombotic effects mediated by LPS comes from an in vitro study showing that stimulation of human endothelial cells with LPS induced the release of prothrombotic molecules, such as von Willebrand factor and factor VIII, via formation and secretion of Weibel–Palade bodies112 (Fig. 4). This phenomenon was blunted by pretreating the cells with a TLR4 inhibitor.
Fig. 4. Mechanisms of LPS-mediated thrombosis.
Low-grade endotoxaemia caused by lipopolysaccharide (LPS) promotes thrombus formation at the site of atherosclerotic plaque rupture or erosion by binding to Toll-like receptor 4 (TLR4) in different cell types, including endothelial cells, monocytes, neutrophils and platelets. a | In endothelial cells, TLR4 activation induces the release of von Willebrand factor (vWf) and factor VIII (FVIII) via formation and secretion of Weibel–Palade bodies (WPb) and the upregulation of tissue factor (TF) secretion, which converts factor X (FX) to activated factor X (FXa) to generate thrombin. b | In monocytes, TLR4 induces upregulation of TF release. c | In neutrophils, TLR4 signalling triggers the formation of neutrophil extracellular traps (NETs) and cathepsin G-mediated platelet activation. d | In platelets, LPS-mediated TLR4 signalling leads to platelet activation via NADPH oxidase 2 (NOX2)-mediated oxidative stress. FVIIa, activated factor VII; FIX, factor IX; FIXa, activated FIX; MyD88, myeloid differentiation primary response protein 88; NF-κB, nuclear factor-κB; PAR4, proteinase-activated receptor 4; O2−, superoxide; TIRAP, Toll–interleukin-1 receptor domain-containing adaptor protein.
Further support for a role of the LPS–TLR4 axis in thrombosis has been provided by immunohistochemistry analysis of coronary thrombi from patients with myocardial infarction15. The analysis revealed the presence of LPS within the thrombus alongside the overexpression in leukocytes of TLR4 and cathepsin G, a protein favouring leukocyte–platelet binding and activation113,114. The interplay between LPS and leukocytes might also contribute to thrombosis via release of NETs (Fig. 4), which comprise DNA and histones and are released upon neutrophil stimulation by pattern-recognition receptor activation or chemokines115. The release of NETs requires ROS formation and calcium mobilization into the neutrophil, which in turn activate protein–arginine deaminase type 4 (PAD4) to deaminate arginine residues on histones116. LPS stimulates NET formation in vitro in a dose-dependent manner117 and requires binding to TLR4 and increased NOX-generated ROS, as indicated by the observation that the TLR4 inhibitor TAK242 and the NOX inhibitor diphenyleneiodonium suppress LPS-mediated NETosis118.
To explore whether the prothrombotic effect of LPS could be recapitulated in vivo, we developed a mouse model of low-grade endotoxaemia that involved intraperitoneal LPS injection (0.5 mg/kg) at a concentration that corresponded with the LPS level detected in human thrombus (40 pg/ml)15. In LPS-treated animals, thrombus growth was accelerated and was associated with increased levels of systemic biomarkers of platelet activation15. Both changes were inhibited by co-administration of a TLR4 inhibitor, reinforcing the hypothesis that TLR4 has a pivotal role in the prothrombotic effect of LPS15. This finding is consistent with the significant correlation between platelet TLR4 upregulation and low-grade endotoxaemia detected in patients with coronary thrombosis119 (Fig. 4).
Other components of the TLR family are also implicated in the thrombotic process mediated by gut microbiota. For instance, TLR2 recognizes and is activated by lipoprotein components of Gram-positive or Gram-negative bacteria and has direct pro-thrombotic effects98. Germ-free or TLR2-deficient mice had reduced thrombus growth after carotid artery injury compared with controls, and this effect was counteracted by intestinal colonization with microbiota120. However, the interplay, if any, between LPS and TLR2 in this context remains to be established.
LPS and cardiovascular events
Circulating LPS levels have been assessed in the general population121,122, in patients at risk of cardiovascular events18,123 and in patients with metabolic diseases31,65,124,125, clinically overt cardiovascular disease (such as atrial fibrillation126,127 or myocardial infarction15,68) or acute infections19,66,128. The association between circulating LPS levels and atherosclerotic burden and the clinical sequelae of atherosclerosis have been assessed in cross-sectional studies and prospective analyses (Table 1).
Table 1.
Low-grade endotoxaemia in various clinical settings
| Study (year) | Study design | Study cohort (n) | Follow-up | Endotoxaemia evaluation | Main results | Ref. |
|---|---|---|---|---|---|---|
| Carpino et al. (2020) | Case–control study | NAFLD (n = 211); no NAFLD (n = 65) | NR | LPS | Increased serum LPS level and higher LPS localization in hepatocytes in patients with NAFLD versus patients without NAFLD; LPS was associated with liver inflammation | 31 |
| Simonsen et al. (2020) | Prospective study | Type 1 diabetes (n = 3,781) | 13.7 years | LAL | LPS activity increased in patients with type 1 diabetes and incident CHD | 125 |
| Wiedermann et al. (1999) | Prospective study | General population, cohort from the Bruneck study (n = 516) | 5 years | LAL | LPS >50 pg/ml in the plasma increased the risk of carotid artery atherosclerosis | 18 |
| Asada et al. (2019) | Prospective study | General population, cohort from Japan (n = 2,568) | 10 years | LBP | Serum LBP level was associated with cardiovascular events | 121 |
| Pussinen et al. (2007) | Prospective study | General population, cohort from FINRISK study (n = 7,927) | 10 years | LAL | The LPS to HDL-cholesterol ratio was associated with systemic inflammation and cardiovascular events | 123 |
| Leskelä et al. (2021) | Genome-wide association study | Three cohorts from Finnish studies (total n = 11,296): FinnDiane, type 1 diabetes (n = 4,242); FINRISK, general population (n = 6,323); Finnish Twin Cohort study, general population (n = 731) | NR | LAL | Five genetic loci were associated with serum endotoxin activity; the genetic risk score of endotoxaemia was associated with venous thromboembolism | 122 |
| Zhou et al. (2018) | Case–control, prospective study | STEMI (total n = 100): stable angina (n = 50); control group (n = 50) | 3 years | LAL | Serum LPS was increased in patients with STEMI and was associated with cardiovascular events | 68 |
| Carnevale et al. (2020) | Case–control study | STEMI (total n = 50): stable angina (n = 50); control group (n = 50) | NR | LPS | Serum LPS level was increased in patients with STEMI and correlated with serum zonulin levels; LPS localized in coronary thrombi from patients with STEMI | 15 |
| Pastori et al. (2017) | Prospective study | Atrial fibrillation (n = 912) | 3 years | LPS | Serum LPS > 100 pg/ml was associated with increased risk of MACE | 126 |
| Zhang et al. (2021) | Cross-sectional study | Atrial fibrillation (total n = 1,152): young participants (aged 18–44 years; n = 694); middle-aged participants (aged 45–64 years, n = 357); older participants (65–75 years, n = 101) | NR | LAL | Serum LPS levels were increased in older patients with atrial fibrillation | 127 |
| Cangemi et al. (2016) | Prospective, observational study | CAP (n = 278); control group (n = 50) | NR | LPS | Serum LPS levels increased in the acute phase of CAP and correlated with serum zonulin levels | 66 |
| Oliva et al. (2021) | Case–control, prospective study | COVID-19 (n = 81); control group (n = 81) | 18 days | LPS | Serum LPS level was associated with thrombotic events in patients with COVID-19 and correlated with serum zonulin level | 19 |
CAP, community-acquired pneumonia; CHD, coronary heart disease; COVID-19, coronavirus disease 2019; LAL, limulus amoebocyte lysate; LBP, lipopolysaccharide-binding protein; LPS, lipopolysaccharide; MACE, major adverse cardiovascular events; NAFLD, non-alcoholic fatty liver disease; NR, not reported; STEMI, ST-segment elevation myocardial infarction.
Wiedermann and colleagues were among the first to investigate the effect of low-grade endotoxaemia on the risk of atherosclerosis in a study that included 516 individuals with risk factors for atherosclerotic disease18. After 5 years of follow-up, individuals with LPS >50 pg/ml at baseline had a threefold increased risk of incident carotid artery atherosclerosis compared with individuals with LPS levels <50 pg/ml. These findings were supported and extended by a study that included 2,568 individuals without previous cardiovascular disease121. After 10 years of follow-up, baseline serum levels of LPS-binding protein were significantly associated with incident cardiovascular disease, after adjusting for conventional risk factors for cardiovascular disease121. This finding was corroborated by a study that analysed circulating LPS levels in 7,927 individuals from a population-based chronic disease risk factor survey123. The study found a significant association between the LPS to HDL cholesterol ratio and cardiovascular events after a follow-up of 10 years123. Evidence for a relationship between endotoxaemia and thrombosis was also provided by an analysis of the genetic profile linked to endotoxaemia and its association with thrombosis in participants of three Finnish cohorts122. The study identified single‐nucleotide polymorphisms at five genetic loci that were associated with serum endotoxin activity; several of the single‐nucleotide polymorphisms were associated with expression of nearby genes affecting the clotting system. Interestingly, a significant association between the genetic risk score of endotoxaemia and venous thromboembolism was also identified122.
Low-grade endotoxaemia has also been investigated in patients with stable or unstable cardiovascular disease in cross-sectional and prospective studies15,68. Elevated circulating levels of LPS and d-lactate, a marker of gut permeability, have been reported in patients in the early phase of acute myocardial infarction, suggesting that coronary ischaemia is a trigger for gut barrier dysfunction68. This hypothesis was corroborated by a study in an animal model of coronary ischaemia, in which coronary ischaemia was associated with increased gut permeability and downregulation of tight junction proteins68. Furthermore, in patients with myocardial infarction, a significant association was observed between circulating LPS levels detected during the acute phase of the disease and major adverse cardiovascular events after 3 years of follow-up68. Furthermore, elevated circulating LPS levels in the peripheral and coronary circulation have been observed in patients with myocardial infarction compared with the levels in patients with stable cardiovascular disease and healthy individuals15. Of note, circulating LPS levels correlated with the serum levels of zonulin and several markers of inflammation, such as IL-1β and TNF, reinforcing the hypothesis that coronary ischaemia is associated with intestinal barrier dysfunction15.
A growing body of evidence indicates that low-grade endotoxaemia occurs in patients with metabolic disease, such as type 2 diabetes, obesity, NAFLD and NASH31,65,124 (Box 2). A systematic review of studies in patients with diabetes and obesity found a significant association between circulating LPS levels and triglyceride and total cholesterol levels, fasting glycaemia, insulinaemia, HbA1c levels and C-reactive protein levels124. The elevation in circulating LPS levels was more marked in patients with macroalbuminuria and was reduced in patients taking hypoglycaemic drugs, and insulin therapy exacerbated endotoxaemia compared with other antidiabetic drugs124. In a prospective study involving 3,781 patients with type 1 diabetes, the number of antibiotic purchases, a surrogate of bacterial infection, as well as high LPS activity were independently associated with incident cardiovascular events during a follow-up of 15 years125.
Metabolic endotoxaemia can also have a negative effect on liver cells, in which LPS can localize and elicit liver damage. Higher serum LPS levels and LPS hepatocyte localization have been detected in patients with NAFLD or NASH and in mouse models of these conditions compared with the levels in controls31. Immunohistochemistry analysis revealed a potential causal interplay between the liver steatosis and fibrosis and the TLR4 overexpression in macrophages and platelets31. Of note, a significant association was observed between platelet TLR4 levels and circulating LPS levels, suggesting a role for LPS in increasing platelet activation. This finding might provide insights on the role of platelets in liver inflammation as well as in cardiovascular events in patients with liver disease129,130.
Atrial fibrillation is another clinical setting in which the role of LPS as a trigger of arrhythmia or cardiovascular events has been explored. In patients with atrial fibrillation, a progressive increase in circulating LPS levels has been observed with increasing age, with high LPS levels found in middle-aged and older patients with atrial fibrillation127. A potential cause–effect relationship between endotoxaemia and atrial fibrillation was investigated in experimental models of atrial fibrillation, which demonstrated a role for gut dysbiosis in promoting atrial fibrillation in old rats and a reduction in atrial fibrillation susceptibility in old rats that received faecal transplantation from young animals127. Overexpression of TLR4 and activation of the NLRP3 inflammasome in the atria were key factors driving atrial fibrosis and increased susceptibility to atrial fibrillation127. The pro-inflammatory activity of LPS might also be relevant for the clinical outcomes of atrial fibrillation, as evidenced by a higher incidence of major adverse cardiovascular events during a follow-up of 3 years in patients with blood LPS levels >100 pg/ml than in patients with LPS <100 pg/ml126.
Low-grade endotoxaemia has also been detected in the acute phase of infection in patients with community-acquired pneumonia or with coronavirus disease 2019 (COVID-19), even in the absence of overt sepsis19,66. Of note, both community-acquired pneumonia and COVID-19 can be complicated by venous and/or arterial thrombosis during the hospital stay, with patients with COVID-19 having an incidence double than that seen in patients with community-acquired pneumonia128. In patients with COVID-19, circulating LPS levels correlated with serum zonulin levels and independently predicted the risk of venous and arterial thrombosis19.
Box 2 Metabolic profile of endotoxaemia.
Endotoxaemia is associated with alterations in the metabolic profile in humans, as indicated by changes in the plasma levels of major metabolites, including lipoproteins, amino acids and glucose163. The available data on plasma metabolite changes during endotoxaemia come from metabolomics studies in inflammatory diseases or in experimental models of endotoxaemia, in which healthy volunteers received intravenous administration of endotoxin.
In the largest cohort study of metabolic changes in endotoxaemia, the presence of endotoxaemia in individuals who smoked or in patients with high BMI and metabolic syndrome was positively and strongly associated with the concentrations of lipoproteins in the serum, including VLDL, intermediate-density lipoproteins and LDL164. Endotoxaemia was also associated with large VLDL particle diameters and small LDL and HDL particle diameters, and with high serum concentrations of monounsaturated fatty acids, saturated fatty acids, branched-chain amino acids, glucose, lactate, pyruvate and glycerol. Conversely, the serum levels of large HDL particles and polyunsaturated fatty acids were inversely associated with endotoxemia164. In studies in healthy volunteers, an endotoxin bolus injection induced progressive hyperglycaemia within 2–6 h after the endotoxin challenge, as well as a significant increase in lipid levels, including fatty acid levels in arterial tissue165 and plasma levels of monounsaturated and polyunsaturated fatty acids163, but decreased amino acid levels in the plasma163.
The observed changes in lipoprotein composition and plasma lipid levels associated with endotoxaemia might be explained by lipopolysaccharide (LPS)-induced adipose tissue lipolysis, together with increased lipid biosynthesis and decreased lipid oxidation in the liver163,164. The increased clearance of amino acids from plasma in endotoxaemia is likely to be due to increased LPS-induced synthesis of acute-phase proteins in the liver and the use of amino acids in energy production163.
Therapeutic implications
Potential therapeutic approaches to improving gut permeability and low-grade endotoxaemia have been proposed, but the clinical relevance of these options needs to be determined (Fig. 5). The Mediterranean diet, which is rich in fibre, is likely to be one of the best approaches to improving gut permeability and eventually eliminating low-grade endotoxaemia. Indeed, high adherence to the Mediterranean diet has been associated with beneficial microbiome-related metabolomic profiles, an increase in plasma SCFA levels and a reduction in circulating LPS levels compared with low adherence to the Mediterranean diet126,131,132. Administration of extra virgin olive oil, a key component of the Mediterranean diet, reduced endotoxaemia and serum zonulin levels and improved the metabolic profile of healthy individuals and patients with impaired fasting glucose133. These findings have been corroborated by an interventional study that found decreased circulating levels of LPS in patients with metabolic syndrome who received a fibre-rich diet for 75 days134.
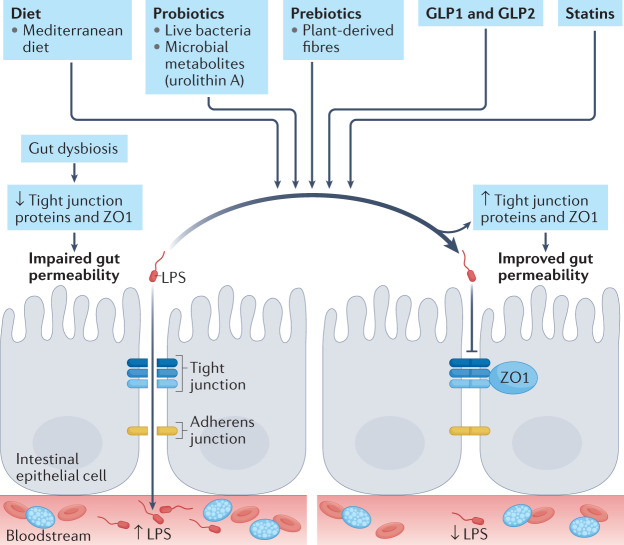
Fig. 5. Potential therapeutic strategies to reduce low-grade endotoxaemia.
Gut dysbiosis downregulates junction proteins, which leads to increased gut permeability and increased translocation of lipopolysaccharide (LPS) into the systemic circulation. Dietary and pharmacological interventions might improve gut barrier dysfunction by upregulating the levels of tight junction proteins and the zonula occludens protein ZO1 and thereby lower circulating LPS levels. Potential interventions include a Mediterranean diet, probiotics (live bacteria or microbial metabolites such as urolithin A), prebiotics (fermentable fibres), interventions that increase glucagon-like peptide 1 (GLP1) and GLP2 levels, and statins.
Prebiotics, which are plant-derived fibres with beneficial effects on gut microbiota, gut permeability and low-grade endotoxaemia, is another potential strategy to reduce low-grade endotoxaemia. Indeed, mice fed a diet supplemented with a fermentable fibre (oligofructose) showed improved gut barrier function and reduced circulating LPS levels compared with control mice135. Specific mechanisms that might account for the improved gut permeability included upregulation of ZO1 and occludin. An increase in glucagon-like peptide 1 (GLP1) and GLP2 levels is another intriguing and potential beneficial effect mediated by prebiotics. Indeed, mice fed a prebiotic-rich diet had an upregulation of GLP1 and GLP2 in the portal circulation compared with control mice, with a significant correlation between high GLP2 levels in the portal blood and improved gut barrier function135. This finding was recapitulated in another study in mice showing that GLP2 administration improved gut permeability, upregulated ZO1 and occludin levels in epithelial cells, lowered circulating LPS levels and reduced liver steatosis135. All these changes were associated with a reduction in systemic inflammation and oxidative stress135. However, the effect of these molecules on atherothrombosis remains to be established. Of note, administration of inulin, a prebiotic polysaccharide, in Apoe−/− mice slowed atherosclerosis progression and reduced liver steatosis136.
Another potential nutrition-related strategy to improve gut barrier permeability is the high intake of fish oils to increase the ratio of n-3 polyunsaturated fatty acids (n-3 PUFAs) to n-6 PUFAs137. However, the role of n-3 PUFAs in the modulation of gut permeability needs to be further clarified.
Other approaches to improving gut permeability include the use of probiotics, which are live bacteria, such as Lactobacillus plantarum or Akkermansia muciniphila, or microbial metabolites such as urolithin A or oxyberberine40. For example, urolithin A administration in mice improved gut barrier function via upregulation of claudin 4, occludin and ZO1 levels in intestinal epithelial cells, whereas oxyberberine administration downregulated the expression of Tlr4 and the production of pro-inflammatory cytokines such as Il-1β, IL-6 and TNF in colonic tissue40. Similar protective effects on barrier function have been achieved in vitro by incubation of epithelial cells with SCFAs, such as propionate, butyrate and acetate, that stem from dietary fibre and indigestible carbohydrate fermentation by commensal microbiota such as Bifidobacterium, Bacteroides, Enterobacter, Faecalibacterium and Roseburia40. In addition, administration of a diet rich in SCFAs to patients with metabolic syndrome resulted in upregulation of epithelial adhesion proteins40,138. However, the implementation of these strategies is so far limited to patients with inflammatory bowel disease40. Therefore, further studies are needed to assess the effect on gut permeability and low-grade endotoxaemia in patients at risk of or with cardiovascular disease.
Statins are lipid-lowering drugs that effectively reduce atherosclerosis and its complications139. Evidence indicates that statins have beneficial effects on gut barrier function by modulating gut dysbiosis or upregulating the levels of intestinal adhesion proteins140,141. Furthermore, in vitro experiments have shown that atorvastatin inhibits the pro-inflammatory effects caused by low-grade endotoxemia93. However, whether statins can counteract the effects of low-grade endotoxaemia in humans and the potential implication of these effects on the development of cardiovascular disease remain to be established.
Conclusions
Experimental data support the association between low-grade endotoxaemia, atherosclerosis and thrombosis, and indicate that gut dysbiosis-induced changes in intestinal permeability are a key step for LPS translocation into the systemic circulation. So far, different experimental assays for measuring LPS activity or concentration have been used for clinical purposes (Box 3), but no consensus exists about the methodology that better reflects LPS biological activity in humans142,143. Therefore, an internationally validated methodology for measuring blood LPS is mandatory to confirm and substantiate the relationship between low-grade endotoxaemia and cardiovascular events. In addition, targeting dysbiosis-induced gut barrier dysfunction to lower LPS translocation into the systemic circulation or impair LPS pro-inflammatory activity should be an important objective to establish whether a cause–effect relationship between low-grade endotoxaemia and cardiovascular events does exist.
In conclusion, the coexistence of low-grade endotoxaemia and atherosclerotic cardiovascular disease in patients provides further insight into the inflammatory processes underlying atherosclerosis. Gut permeability-related low-grade endotoxaemia might represent a novel tool to explore further the role of inflammation in the pathogenesis of atherothrombosis.
Box 3 Methods of LPS detection.
Rabbit pyrogen test
The rabbit pyrogen test is the first method to be developed for detecting lipopolysaccharide (LPS) and was approved by the FDA in 1942. This test is based on measuring the increase in body temperature in rabbits after intravenous injection of endotoxin. The detection limit is >5 endotoxin units (EU) per millilitre per kilogram of body weight, whereby EU refers to a measure of LPS activity rather than of mass, and 1 EU is equal to approximately 0.1 ng of LPS.
Limulus amoebocyte lysate assay
The limulus amoebocyte lysate (LAL) assay is the gold-standard method for the detection of lipid A in LPS. The LAL assay is based on the discovery by Bang in 1956 that blood cells (amoebocytes) from horseshoe crabs (Limulus polyphemus) agglomerate after reacting with endotoxin166. The test is based on the coagulation cascade of horseshoe crab blood triggered by endotoxins, which involves several serine proteases and is initiated by the combination of LPS with zymogen factor C167. The detection limit is 0.06 EU/ml. However, improved methods, such as the chromogenic and turbidimetric methodologies, increase the LAL test sensitivity to 0.015 EU/ml and 0.005 EU/ml, respectively168.
ELISA
The enzyme-linked immunosorbent assay (ELISA), a technique developed in 1971, can be used to detect either the LPS antigen or LPS antibody titres. The ELISA detects LPS by primary capture antibody. To overcome the problems related to cross-reactivity or false positive results due to the heterogeneity of LPS, a microplate assay EndoLISA was developed in 2011, which directly detects endotoxin by using the target analyte (LPS) selectively bound to the surface of the precoated plate followed by detection with factor C169. However, the assay cannot differentiate between bacterial serotypes. To date, specific immunological assays have been developed by using LPS preparations purified from different serotypes, which primarily differ in the chemical nature of the LPS O-antigen, or antibodies targeted against the hypervariable O-antigen region to ensure discriminatory detection of the assays.
Mass spectrometry-based methods
Gas chromatography (GC) mass spectrometry (MS) provides a direct measure of LPS mass by enabling the quantification of 3-hydroxytetradecanoic acid, the most abundant hydroxylated fatty acid of the lipid A moiety of most LPS molecules170. However, only small amounts of lipid-rich samples can be loaded onto GC columns. High-performance liquid chromatography (HPLC) tandem MS (MS/MS) methods overcome the technical issues of GC–MS or GC–MS/MS, providing a sensitive, accurate and direct quantification of total amounts of LPS in the plasma171. The HPLC–MS/MS method has high specificity and a low limit of detection and quantification, allowing the detection of the low concentrations of LPS found in the context of low-grade endotoxaemia.
Biosensors
In the past 10 years, biosensing techniques with high specificity, low cost and easy-to-operate and fast methods have been developed. Biosensors detect the presence of a specific analyte by using a biological recognition element on their surface, and can be monitored by the optical, electronic, mass or magnetic signal variation induced by the interaction with the analyte of interest172. Different types of biosensors to detect LPS have been developed, including biosensors based on proteins, peptides, aptamers and antibodies. In particular, aptamers, single-stranded oligonucleotides that bind to specific targets with high affinity and specificity, are an emerging molecular recognition tool for biosensing LPS173.
Glossary
- Gut dysbiosis
Any change in the number or diversity of resident commensal gut microbiota relative to the community present in healthy individuals.
- Trimethylamine-N-oxide
(TMAO). A small organic compound formed from trimethylamine, which is generated by metabolism of dietary choline and phosphatidylcholine by flavin monooxygenases from gut microbiota.
- Endotoxaemia
The presence in the blood of endotoxins, such as lipopolysaccharide (LPS), which is a component of the outer membrane of Gram-negative bacteria.
- Non-alcoholic fatty liver disease
(NAFLD). A condition caused by ectopic fat accumulation in the liver in the absence of excessive alcohol intake.
- Non-alcoholic steatohepatitis
(NASH). A severe form of non-alcoholic fatty liver disease that is characterized by liver inflammation and that can progress to cirrhosis.
- Intestinal adhesion proteins
The scaffold of the epithelial cell barrier that protects from the translocation of microorganisms or microbial products into the systemic circulation.
- Increased gut permeability
Impaired function of epithelial cell adhesion proteins and loss of epithelial cell barrier integrity, with translocation of microorganisms and toxins into the bloodstream.
- NADPH oxidase
A ubiquitous, multisubunit cellular enzyme that is a major producer of reactive oxygen species.
- Neutrophil extracellular traps
(NETs). Extracellular net-like structures composed of DNA, histones and cytoplasmic granule proteins released by neutrophils after activation.
- Prebiotics
Non-digestible food ingredients (fibres) that promote a shift to a healthier gut microbiota profile.
- Probiotics
Live microorganisms that confer a health benefit in the host when administered in adequate amounts.
Author contributions
F.V. developed the concept and design of the review and wrote the manuscript. All the authors contributed to the discussion of content and reviewed and edited the manuscript before submission.
Peer review
Peer review information
Nature Reviews Cardiology thanks Christoph Reinhardt; Christoph Thiemermann, who co-reviewed with Shireen Mohammad; Pirkko Pussinen; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Roberto Carnevale and Cristina Nocella.
References
- 1.Ross R. Inflammation or atherogenesis. N. Engl. J. Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 2.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 3.Shibata N, Glass CK. Regulation of macrophage function in inflammation and atherosclerosis. J. Lipid Res. 2009;50:S277–S281. doi: 10.1194/jlr.R800063-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Violi F, Loffredo L, Carnevale R, Pignatelli P, Pastori D. Atherothrombosis and oxidative stress: mechanisms and management in elderly. Antioxid. Redox Signal. 2017;27:1083–1124. doi: 10.1089/ars.2016.6963. [DOI] [PubMed] [Google Scholar]
- 5.Tabas I. 2016 Russell Ross Memorial Lecture in Vascular Biology: Molecular–Cellular Mechanisms in the Progression of Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2017;37:183–189. doi: 10.1161/ATVBAHA.116.308036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ridker PM, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N. Engl. J. Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 7.Nidorf SM, et al. Colchicine in patients with chronic coronary disease. N. Engl. J. Med. 2020;383:1838–1847. doi: 10.1056/NEJMoa2021372. [DOI] [PubMed] [Google Scholar]
- 8.Wang B, Yao M, Lv L, Ling Z, Li L. The human microbiota in health and disease. Engineering. 2017;3:71–82. doi: 10.1016/J.ENG.2017.01.008. [DOI] [Google Scholar]
- 9.O’Toole PW, Jeffery IB. Gut microbiota and aging. Science. 2015;350:1214–1215. doi: 10.1126/science.aac8469. [DOI] [PubMed] [Google Scholar]
- 10.Ascher S, Reinhardt C. The gut microbiota: an emerging risk factor for cardiovascular and cerebrovascular disease. Eur. J. Immunol. 2018;48:564–575. doi: 10.1002/eji.201646879. [DOI] [PubMed] [Google Scholar]
- 11.Caesar R, Fåk F, Bäckhed F. Effects of gut microbiota on obesity and atherosclerosis via modulation of inflammation and lipid metabolism: review. J. Intern. Med. 2010;268:320–328. doi: 10.1111/j.1365-2796.2010.02270.x. [DOI] [PubMed] [Google Scholar]
- 12.Moreira APB, Texeira TFS, Ferreira AB, Do Carmo Gouveia Peluzio M, De Cássia Gonçalves Alfenas R. Influence of a high-fat diet on gut microbiota, intestinal permeability and metabolic endotoxaemia. Br. J. Nutr. 2012;108:801–809. doi: 10.1017/S0007114512001213. [DOI] [PubMed] [Google Scholar]
- 13.Cani PD, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–1772. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 14.den Dekker WK, Cheng C, Pasterkamp G, Duckers HJ. Toll like receptor 4 in atherosclerosis and plaque destabilization. Atherosclerosis. 2010;209:314–320. doi: 10.1016/j.atherosclerosis.2009.09.075. [DOI] [PubMed] [Google Scholar]
- 15.Carnevale R, et al. Low-grade endotoxaemia enhances artery thrombus growth via toll-like receptor 4: implication for myocardial infarction. Eur. Heart J. 2020;41:3156–3165. doi: 10.1093/eurheartj/ehz893. [DOI] [PubMed] [Google Scholar]
- 16.Koupenova M, Clancy L, Corkrey HA, Freedman JE. Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ. Res. 2018;122:337–351. doi: 10.1161/CIRCRESAHA.117.310795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koupenova M, Freedman JE. Platelets and COVID-19: inflammation, hyperactivation and additional questions. Circ. Res. 2020;127:1419–1421. doi: 10.1161/CIRCRESAHA.120.318218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiedermann CJ, et al. Association of endotoxemia with carotid atherosclerosis and cardiovascular disease: prospective results from the Bruneck study. J. Am. Coll. Cardiol. 1999;34:1975–1981. doi: 10.1016/S0735-1097(99)00448-9. [DOI] [PubMed] [Google Scholar]
- 19.Oliva A, et al. Low-grade endotoxemia and thrombosis in COVID-19. Clin. Transl. Gastroenterol. 2021;12:e00348. doi: 10.14309/ctg.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cani PD, et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 21.Guerville M, et al. Western-diet consumption induces alteration of barrier function mechanisms in the ileum that correlates with metabolic endotoxemia in rats. Am. J. Physiol. Endocrinol. Metab. 2017;313:E107–E120. doi: 10.1152/ajpendo.00372.2016. [DOI] [PubMed] [Google Scholar]
- 22.Carnevale R, et al. Gut-derived lipopolysaccharides increase post-prandial oxidative stress via Nox2 activation in patients with impaired fasting glucose tolerance: effect of extra-virgin olive oil. Eur. J. Nutr. 2019;58:843–851. doi: 10.1007/s00394-018-1718-x. [DOI] [PubMed] [Google Scholar]
- 23.Ghoshal S, Witta J, Zhong J, de Villiers W, Eckhardt E. Chylomicrons promote intestinal absorption of lipopolysaccharides. J. Lipid Res. 2009;50:90–97. doi: 10.1194/jlr.M800156-JLR200. [DOI] [PubMed] [Google Scholar]
- 24.Manco M, Putignani L, Bottazzo GF. Gut microbiota, lipopolysaccharides, and innate immunity in the pathogenesis of obesity and cardiovascular risk. Endocr. Rev. 2010;31:817–844. doi: 10.1210/er.2009-0030. [DOI] [PubMed] [Google Scholar]
- 25.Stoll LL, Denning GM, Weintraub NL. Potential role of endotoxin as a proinflammatory mediator of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2004;24:2227–2236. doi: 10.1161/01.ATV.0000147534.69062.dc. [DOI] [PubMed] [Google Scholar]
- 26.Levels JHM, et al. Lipopolysaccharide is transferred from high-density to low-density lipoproteins by lipopolysaccharide-binding protein and phospholipid transfer protein. Infect. Immun. 2005;73:2321–2326. doi: 10.1128/IAI.73.4.2321-2326.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flegel WA, Wolpl A, Mannel DN, Northoff H. Inhibition of endotoxin-induced activation of human monocytes by human lipoproteins. Infect. Immun. 1989;57:2237–2245. doi: 10.1128/iai.57.7.2237-2245.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levine DM, Parker TS, Donnelly TM, Walsh A, Rubin AL. In vivo protection against endotoxin by plasma high density lipoprotein. Proc. Natl Acad. Sci. USA. 1993;90:12040–12044. doi: 10.1073/pnas.90.24.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parker TS, et al. Reconstituted high-density lipoprotein neutralizes gram-negative bacterial lipopolysaccharides in human whole blood. Infect. Immun. 1995;63:253–258. doi: 10.1128/iai.63.1.253-258.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guerville M, Boudry G. Gastrointestinal and hepatic mechanisms limiting entry and dissemination of lipopolysaccharide into the systemic circulation. Am. J. Physiol. Liver Physiol. 2016;311:G1–G15. doi: 10.1152/ajpgi.00098.2016. [DOI] [PubMed] [Google Scholar]
- 31.Carpino G, et al. Increased liver localization of lipopolysaccharides in human and experimental NAFLD. Hepatology. 2020;72:470–485. doi: 10.1002/hep.31056. [DOI] [PubMed] [Google Scholar]
- 32.Poltorak A, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 33.Park BS, Lee JO. Recognition of lipopolysaccharide pattern by TLR4 complexes. Exp. Mol. Med. 2013;45:e66. doi: 10.1038/emm.2013.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pålsson-McDermott EM, O’Neill LAJ. Signal transduction by the lipopolysaccharide receptor, Toll-like receptor-4. Immunology. 2004;113:153–162. doi: 10.1111/j.1365-2567.2004.01976.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu T, Zhang L, Joo D, Sun SC. NF-κB signaling in inflammation. Sig. Transduct. Target. Ther. 2017;2:17023. doi: 10.1038/sigtrans.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buckley A, Turner JR. Cell biology of tight junction barrier regulation and mucosal disease. Cold Spring Harb. Perspect. Biol. 2018;10:a029314. doi: 10.1101/cshperspect.a029314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johansson MEV, Sjövall H, Hansson GC. The gastrointestinal mucus system in health and disease. Nat. Rev. Gastroenterol. Hepatol. 2013;10:352–361. doi: 10.1038/nrgastro.2013.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sturgeon C, Fasano A. Zonulin, a regulator of epithelial and endothelial barrier functions, and its involvement in chronic inflammatory diseases. Tissue Barriers. 2016;4:e1251384. doi: 10.1080/21688370.2016.1251384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farquhar MG, Palade GE. Junctional complexes in various epithelia. J. Cell Biol. 1963;17:375–412. doi: 10.1083/jcb.17.2.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ghosh S, Whitley CS, Haribabu B, Jala VR. Regulation of intestinal barrier function by microbial metabolites. Cell Mol. Gastroenterol. Hepatol. 2021;11:1463–1482. doi: 10.1016/j.jcmgh.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matsuda M, Kubo A, Furuse M, Tsukita S. A peculiar internalization of claudins, tight junction-specific adhesion molecules, during the intercellular movement of epithelial cells. J. Cell Sci. 2004;117:1247–1257. doi: 10.1242/jcs.00972. [DOI] [PubMed] [Google Scholar]
- 42.Spadoni I, et al. A gut-vascular barrier controls the systemic dissemination of bacteria. Science. 2015;350:830–834. doi: 10.1126/science.aad0135. [DOI] [PubMed] [Google Scholar]
- 43.Mouries J, et al. Microbiota-driven gut vascular barrier disruption is a prerequisite for non-alcoholic steatohepatitis development. J. Hepatol. 2019;71:1216–1228. doi: 10.1016/j.jhep.2019.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paradis T, Bègue H, Basmaciyan L, Dalle F, Bon F. Tight junctions as a key for pathogens invasion in intestinal epithelial cells. Int. J. Mol. Sci. 2021;22:2506. doi: 10.3390/ijms22052506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen LJ, et al. Commensal bacteria make GPCR ligands that mimic human signalling molecules. Nature. 2017;549:48–53. doi: 10.1038/nature23874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mydel P, et al. Roles of the host oxidative immune response and bacterial antioxidant rubrerythrin during porphyromonas gingivalis infection. PLoS Pathog. 2006;2:e76. doi: 10.1371/journal.ppat.0020076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hiippala K, et al. The potential of gut commensals in reinforcing intestinal barrier function and alleviating inflammation. Nutrients. 2018;10:988. doi: 10.3390/nu10080988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Franceschi C, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000;908:244–254. doi: 10.1111/j.1749-6632.2000.tb06651.x. [DOI] [PubMed] [Google Scholar]
- 49.Nagpal R, et al. Gut microbiome and aging: physiological and mechanistic insights. Nutr. Healthy Aging. 2018;4:267–285. doi: 10.3233/NHA-170030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Odamaki T, et al. Age-related changes in gut microbiota composition from newborn to centenarian: a cross-sectional study. BMC Microbiol. 2016;16:90. doi: 10.1186/s12866-016-0708-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thevaranjan N, et al. Age-associated microbial dysbiosis promotes intestinal permeability, systemic inflammation, and macrophage dysfunction. Cell Host Microbe. 2017;21:455–466.e4. doi: 10.1016/j.chom.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fort MM, et al. A synthetic TLR4 antagonist has anti-inflammatory effects in two murine models of inflammatory bowel disease. J. Immunol. 2005;174:6416–6423. doi: 10.4049/jimmunol.174.10.6416. [DOI] [PubMed] [Google Scholar]
- 53.Wang W, Xia T, Yu X. Wogonin suppresses inflammatory response and maintains intestinal barrier function via TLR4-MyD88-TAK1-mediated NF-κB pathway in vitro. Inflamm. Res. 2015;64:423–431. doi: 10.1007/s00011-015-0822-0. [DOI] [PubMed] [Google Scholar]
- 54.Ungaro R, et al. A novel Toll-like receptor 4 antagonist antibody ameliorates inflammation but impairs mucosal healing in murine colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;296:G1167–G1179. doi: 10.1152/ajpgi.90496.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peterson CY, et al. Toll-like receptor-4 mediates intestinal barrier breakdown after thermal injury. Surg. Infect. 2010;11:137–144. doi: 10.1089/sur.2009.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bentala H, et al. Removal of phosphate from lipid a as a strategy to detoxify lipopolysaccharide. Shock. 2002;18:561–566. doi: 10.1097/00024382-200212000-00013. [DOI] [PubMed] [Google Scholar]
- 57.Ghosh SS, et al. Over-expression of intestinal alkaline phosphatase attenuates atherosclerosis. Circ. Res. 2021;128:1646–1659. doi: 10.1161/CIRCRESAHA.120.317144. [DOI] [PubMed] [Google Scholar]
- 58.Han YH, et al. Enterically derived high-density lipoprotein restrains liver injury through the portal vein. Science. 2021;373:eabe6729. doi: 10.1126/science.abe6729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kriegel MA, et al. Naturally transmitted segmented filamentous bacteria segregate with diabetes protection in nonobese diabetic mice. Proc. Natl Acad. Sci. USA. 2011;108:11548–11553. doi: 10.1073/pnas.1108924108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bäckhed F, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl Acad. Sci. USA. 2004;101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wood Heickman LK, DeBoer MD, Fasano A. Zonulin as a potential putative biomarker of risk for shared type 1 diabetes and celiac disease autoimmunity. Diabetes Metab. Res. Rev. 2020;36:e3309. doi: 10.1002/dmrr.3309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fasano A. Intestinal permeability and its regulation by zonulin: diagnostic and therapeutic implications. Clin. Gastroenterol. Hepatol. 2012;10:1096–1100. doi: 10.1016/j.cgh.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li X, Atkinson MA. The role for gut permeability in the pathogenesis of type 1 diabetes–a solid or leaky concept? Pediatr. Diabetes. 2015;16:485–492. doi: 10.1111/pedi.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jayashree B, et al. Increased circulatory levels of lipopolysaccharide (LPS) and zonulin signify novel biomarkers of proinflammation in patients with type 2 diabetes. Mol. Cell. Biochem. 2014;388:203–210. doi: 10.1007/s11010-013-1911-4. [DOI] [PubMed] [Google Scholar]
- 65.Aasbrenn M, Lydersen S, Farup PG. Changes in serum zonulin in individuals with morbid obesity after weight-loss interventions: a prospective cohort study. BMC Endocr. Disord. 2020;20:108. doi: 10.1186/s12902-020-00594-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cangemi R, et al. Low-grade endotoxemia, gut permeability and platelet activation in community-acquired pneumonia. J. Infect. 2016;73:107–114. doi: 10.1016/j.jinf.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 67.Hanada S, Pirzadeh M, Carver KY, Deng JC. Respiratory viral infection-induced microbiome alterations and secondary bacterial pneumonia. Front. Immunol. 2018;9:2640. doi: 10.3389/fimmu.2018.02640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhou X, et al. Gut-dependent microbial translocation induces inflammation and cardiovascular events after ST-elevation myocardial infarction. Microbiome. 2018;6:66. doi: 10.1186/s40168-018-0441-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith SM, Eng RHK, Campos JM, Chmel H. D-Lactic acid measurements in the diagnosis of bacterial infections. J. Clin. Microbiol. 1989;27:385–388. doi: 10.1128/jcm.27.3.385-388.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sun XQ, et al. Relationship between plasma D(-)-lactate and intestinal damage after severe injuries in rats. World J. Gastroenterol. 2001;7:555–558. doi: 10.3748/wjg.v7.i4.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fukui H. Gut-liver axis in liver cirrhosis: how to manage leaky gut and endotoxemia. World J. Hepatol. 2015;7:425–442. doi: 10.4254/wjh.v7.i3.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sequeira IR, Lentle RG, Kruger MC, Hurst RD. Standardising the lactulose mannitol test of gut permeability to minimise error and promote comparability. PLoS ONE. 2014;9:e99256. doi: 10.1371/journal.pone.0099256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mundi S, et al. Endothelial permeability, LDL deposition, and cardiovascular risk factors–a review. Cardiovasc. Res. 2018;114:35–52. doi: 10.1093/cvr/cvx226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wu MY, Li CJ, Hou MF, Chu PY. New insights into the role of inflammation in the pathogenesis of atherosclerosis. Int. J. Mol. Sci. 2017;18:2034. doi: 10.3390/ijms18102034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Iuliano L, Mauriello A, Sbarigia E, Spagnoli LG, Violi F. Radiolabeled native low-density lipoprotein injected into patients with carotid stenosis accumulates in macrophages of atherosclerotic plaque. Circulation. 2000;101:1249–1254. doi: 10.1161/01.CIR.101.11.1249. [DOI] [PubMed] [Google Scholar]
- 76.Jonsson AL, Bäckhed F. Role of gut microbiota in atherosclerosis. Nat. Rev. Cardiol. 2017;14:79–87. doi: 10.1038/nrcardio.2016.183. [DOI] [PubMed] [Google Scholar]
- 77.Karlsson FH, et al. Symptomatic atherosclerosis is associated with an altered gut metagenome. Nat. Commun. 2012;3:1245. doi: 10.1038/ncomms2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Emoto T, et al. Characterization of gut microbiota profiles in coronary artery disease patients using data mining analysis of terminal restriction fragment length polymorphism: gut microbiota could be a diagnostic marker of coronary artery disease. Heart Vessel. 2017;32:39–46. doi: 10.1007/s00380-016-0841-y. [DOI] [PubMed] [Google Scholar]
- 79.Kiouptsi K, et al. The microbiota promotes arterial thrombosis in low-density lipoprotein receptor-deficient mice. MBio. 2019;10:e02298-19. doi: 10.1128/mBio.02298-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Violi F, Carnevale R, Loffredo L, Pignatelli P, Gallin JI. NADPH oxidase-2 and atherothrombosis: insight from chronic granulomatous disease. Arterioscler. Thromb. Vasc. Biol. 2017;37:218–225. doi: 10.1161/ATVBAHA.116.308351. [DOI] [PubMed] [Google Scholar]
- 81.Nocella C, et al. Lipopolysaccharide as trigger of platelet aggregation via eicosanoid over-production. Thromb. Haemost. 2017;117:1558–1570. doi: 10.1160/TH16-11-0857. [DOI] [PubMed] [Google Scholar]
- 82.Carnevale R, et al. LDL are oxidatively modified by platelets via GP91(phox) and accumulate in human monocytes. FASEB J. 2007;21:927–934. doi: 10.1096/fj.06-6908com. [DOI] [PubMed] [Google Scholar]
- 83.Carnevale R, et al. LDL oxidation by platelets propagates platelet activation via an oxidative stress-mediated mechanism. Atherosclerosis. 2014;237:108–116. doi: 10.1016/j.atherosclerosis.2014.08.041. [DOI] [PubMed] [Google Scholar]
- 84.Carnevale R, et al. Low-grade endotoxemia, gut permeability and platelet activation in patients with impaired fasting glucose. Nutr. Metab. Cardiovasc. Dis. 2017;27:890–895. doi: 10.1016/j.numecd.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 85.Carnevale R, et al. Localization of lipopolysaccharide from Escherichia coli into human atherosclerotic plaque. Sci. Rep. 2018;8:3598. doi: 10.1038/s41598-018-22076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Levels JHM, Abraham PR, Van Barreveld EP, Meijers JCM, Van Deventer SJH. Distribution and kinetics of lipoprotein-bound lipoteichoic acid. Infect. Immun. 2003;71:3280–3284. doi: 10.1128/IAI.71.6.3280-3284.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hersoug LG, Møller P, Loft S. Role of microbiota-derived lipopolysaccharide in adipose tissue inflammation, adipocyte size and pyroptosis during obesity. Nutr. Res. Rev. 2018;31:153–163. doi: 10.1017/S0954422417000269. [DOI] [PubMed] [Google Scholar]
- 88.Rehues P, et al. Characterization of the LPS and 3OHFA contents in the lipoprotein fractions and lipoprotein particles of healthy men. Biomolecules. 2021;12:47. doi: 10.3390/biom12010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Memon RA, et al. Infection and inflammation induce LDL oxidation in vivo. Arterioscler. Thromb. Vasc. Biol. 2000;20:1536–1542. doi: 10.1161/01.ATV.20.6.1536. [DOI] [PubMed] [Google Scholar]
- 90.Fuijkschot WW, et al. LPS-induced systemic inflammation does not alter atherosclerotic plaque area or inflammation in ApoE3*Leiden mice in the early phase up to 15 days. Shock. 2018;50:360–365. doi: 10.1097/SHK.0000000000001026. [DOI] [PubMed] [Google Scholar]
- 91.Lehr HA, et al. Immunopathogenesis of atherosclerosis: endotoxin accelerates atherosclerosis in rabbits on hypercholesterolemic diet. Circulation. 2001;104:914–920. doi: 10.1161/hc3401.093153. [DOI] [PubMed] [Google Scholar]
- 92.Ostos MA, Recalde D, Zakin MM, Scott-Algara D. Implication of natural killer T cells in atherosclerosis development during a LPS-induced chronic inflammation. FEBS Lett. 2002;519:23–29. doi: 10.1016/S0014-5793(02)02692-3. [DOI] [PubMed] [Google Scholar]
- 93.Rice JB, et al. Low-level endotoxin induces potent inflammatory activation of human blood vessels: inhibition by statins. Arterioscler. Thromb. Vasc. Biol. 2003;23:1576–1582. doi: 10.1161/01.ATV.0000081741.38087.F9. [DOI] [PubMed] [Google Scholar]
- 94.Violi F, Calvieri C, Ferro D, Pignatelli P. Statins as antithrombotic drugs. Circulation. 2013;127:251–257. doi: 10.1161/CIRCULATIONAHA.112.145334. [DOI] [PubMed] [Google Scholar]
- 95.Michelsen KS, et al. Lack of Toll-like receptor 4 or myeloid differentiation factor 88 reduces atherosclerosis and alters plaque phenotype in mice deficient in apolipoprotein E. Proc. Natl Acad. Sci. USA. 2004;101:10679–10684. doi: 10.1073/pnas.0403249101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vink A, et al. In vivo evidence for a role of toll-like receptor 4 in the development of intimal lesions. Circulation. 2002;106:1985–1990. doi: 10.1161/01.CIR.0000032146.75113.EE. [DOI] [PubMed] [Google Scholar]
- 97.Ding Y, et al. Toll-like receptor 4 deficiency decreases atherosclerosis but does not protect against inflammation in obese low-density lipoprotein receptor-deficient mice. Arterioscler. Thromb. Vasc. Biol. 2012;32:1596–1604. doi: 10.1161/ATVBAHA.112.249847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Koupenova M, Livada AC, Morrell CN. Platelet and megakaryocyte roles in innate and adaptive immunity. Circ. Res. 2022;130:288–308. doi: 10.1161/CIRCRESAHA.121.319821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jaw JE, et al. Lung exposure to lipopolysaccharide causes atherosclerotic plaque destabilisation. Eur. Respir. J. 2016;48:205–215. doi: 10.1183/13993003.00972-2015. [DOI] [PubMed] [Google Scholar]
- 100.Schumski A, et al. Endotoxinemia accelerates atherosclerosis through electrostatic charge-mediated monocyte adhesion. Circulation. 2021;143:254–266. doi: 10.1161/CIRCULATIONAHA.120.046677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mawhin M-A, et al. Neutrophils recruited by leukotriene B4 induce features of plaque destabilization during endotoxaemia. Cardiovasc. Res. 2018;114:1656–1666. doi: 10.1093/cvr/cvy130. [DOI] [PubMed] [Google Scholar]
- 102.Zhu W, et al. Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell. 2016;165:111–124. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Violi F, et al. Bleeding time in patients with cirrhosis: relation with degree of liver failure and clotting abnormalities. J. Hepatol. 1994;20:531–536. doi: 10.1016/S0168-8278(05)80501-X. [DOI] [PubMed] [Google Scholar]
- 104.Violi F, et al. Association between low-grade disseminated intravascular coagulation and endotoxemia in patients with liver cirrhosis. Gastroenterology. 1995;109:531–539. doi: 10.1016/0016-5085(95)90342-9. [DOI] [PubMed] [Google Scholar]
- 105.Fimognari FL, Violi F. Portal vein thrombosis in liver cirrhosis. Intern. Emerg. Med. 2008;3:213–218. doi: 10.1007/s11739-008-0128-0. [DOI] [PubMed] [Google Scholar]
- 106.Saliola M, et al. Enhanced expression of monocyte tissue factor in patients with liver cirrhosis. Gut. 1998;43:428–432. doi: 10.1136/gut.43.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Camerer E, Huang W, Coughlin SR. Tissue factor- and factor X-dependent activation of protease-activated receptor 2 by factor VIIa. Proc. Natl Acad. Sci. USA. 2000;97:5255–5260. doi: 10.1073/pnas.97.10.5255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ferro D, et al. Vitamin E reduces monocyte tissue factor expression in cirrhotic patients. Blood. 1999;93:2945–2950. doi: 10.1182/blood.V93.9.2945.409k29_2945_2950. [DOI] [PubMed] [Google Scholar]
- 109.Zhang WJ, Wojta J, Binder BR. Notoginsenoside R1 counteracts endotoxin-induced activation of endothelial cells in vitro and endotoxin-induced lethality in mice in vivo. Arterioscler. Thromb. Vasc. Biol. 1997;17:465–474. doi: 10.1161/01.ATV.17.3.465. [DOI] [PubMed] [Google Scholar]
- 110.Ruan Q, Deng Z, Song J. Ligustrazini inhibits endotoxin induced PAI-1 expression in human umbilical vein endothelial cells. J. Tongji Med. Univ. 2001;21:6–7. doi: 10.1007/BF02888023. [DOI] [PubMed] [Google Scholar]
- 111.Ren M, et al. Endothelial cells but not platelets are the major source of Toll-like receptor 4 in the arterial thrombosis and tissue factor expression in mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2014;307:R901–R907. doi: 10.1152/ajpregu.00324.2014. [DOI] [PubMed] [Google Scholar]
- 112.Carnevale R, et al. Gut-derived endotoxin stimulates factor VIII secretion from endothelial cells. Implications for hypercoagulability in cirrhosis. J. Hepatol. 2017;67:950–956. doi: 10.1016/j.jhep.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 113.Sambrano GR, et al. Cathepsin G activates protease-activated receptor-4 in human platelets. J. Biol. Chem. 2000;275:6819–6823. doi: 10.1074/jbc.275.10.6819. [DOI] [PubMed] [Google Scholar]
- 114.Nadir Y, et al. Heparanase enhances the generation of activated factor X in the presence of tissue factor and activated factor VII. Haematologica. 2010;95:1927–1934. doi: 10.3324/haematol.2010.023713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Brinkmann V, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 116.Li P, et al. PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J. Exp. Med. 2010;207:1853–1862. doi: 10.1084/jem.20100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yao W, et al. ONO-5046 suppresses reactive oxidative species-associated formation of neutrophil extracellular traps. Life Sci. 2018;210:243–250. doi: 10.1016/j.lfs.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 118.Khan MA, et al. JNK activation turns on LPS- and gram-negative bacteria-induced NADPH oxidase-dependent suicidal NETosis. Sci. Rep. 2017;7:3409. doi: 10.1038/s41598-017-03257-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Barillà F, et al. Toll-like receptor 4 activation in platelets from myocardial infarction patients. Thromb. Res. 2022;209:33–40. doi: 10.1016/j.thromres.2021.11.019. [DOI] [PubMed] [Google Scholar]
- 120.Jäckel S, et al. Gut microbiota regulate hepatic von Willebrand factor synthesis and arterial thrombus formation via Toll-like receptor-2. Blood. 2017;130:542–553. doi: 10.1182/blood-2016-11-754416. [DOI] [PubMed] [Google Scholar]
- 121.Asada M, et al. Serum lipopolysaccharide-binding protein levels and the incidence of cardiovascular disease in a general Japanese population: the Hisayama study. J. Am. Heart Assoc. 2019;8:e013628. doi: 10.1161/JAHA.119.013628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Leskelä J, et al. Genetic profile of endotoxemia reveals an association with thromboembolism and stroke. J. Am. Heart Assoc. 2021;10:e022482. doi: 10.1161/JAHA.121.022482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pussinen PJ, et al. Endotoxemia, immune response to periodontal pathogens, and systemic inflammation associate with incident cardiovascular disease events. Arterioscler. Thromb. Vasc. Biol. 2007;27:1433–1439. doi: 10.1161/ATVBAHA.106.138743. [DOI] [PubMed] [Google Scholar]
- 124.Gomes JMG, de Costa JA, de Alfenas RCG. Metabolic endotoxemia and diabetes mellitus: a systematic review. Metabolism. 2017;68:133–144. doi: 10.1016/j.metabol.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 125.Simonsen JR, et al. The association between bacterial infections and the risk of coronary heart disease in type 1 diabetes. J. Intern. Med. 2020;288:711–724. doi: 10.1111/joim.13138. [DOI] [PubMed] [Google Scholar]
- 126.Pastori D, et al. Gut-derived serum lipopolysaccharide is associated with enhanced risk of major adverse cardiovascular events in atrial fibrillation: effect of adherence to Mediterranean diet. J. Am. Heart Assoc. 2017;6:e005784. doi: 10.1161/JAHA.117.005784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zhang Y, et al. Gut microbiota dysbiosis promotes age-related atrial fibrillation by lipopolysaccharide and glucose-induced activation of NLRP3-inflammasome. Cardiovasc. Res. 2021;118:785–797. doi: 10.1093/cvr/cvab114. [DOI] [PubMed] [Google Scholar]
- 128.Cangemi R, et al. Comparison of thrombotic events and mortality in patients with community-acquired pneumonia and COVID-19: a multicenter observational study. Thromb. Haemost. 2021;122:257–266. doi: 10.1055/a-1692-9939. [DOI] [PubMed] [Google Scholar]
- 129.Malehmir M, et al. Platelet GPIbα is a mediator and potential interventional target for NASH and subsequent liver cancer. Nat. Med. 2019;25:641–655. doi: 10.1038/s41591-019-0379-5. [DOI] [PubMed] [Google Scholar]
- 130.Baratta F, et al. Nonalcoholic fatty liver disease and fibrosis associated with increased risk of cardiovascular events in a prospective study. Clin. Gastroenterol. Hepatol. 2020;18:2324–2331.e4. doi: 10.1016/j.cgh.2019.12.026. [DOI] [PubMed] [Google Scholar]
- 131.Amar J. Microbiota-host crosstalk: a bridge between cardiovascular risk factors, diet, and cardiovascular disease. Am. J. Hypertens. 2018;31:941–944. doi: 10.1093/ajh/hpy067. [DOI] [PubMed] [Google Scholar]
- 132.De Filippis F, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65:1812–1821. doi: 10.1136/gutjnl-2015-309957. [DOI] [PubMed] [Google Scholar]
- 133.Bartimoccia S, et al. Extra virgin olive oil reduces gut permeability and metabolic endotoxemia in diabetic patients. Nutrients. 2022;14:2153. doi: 10.3390/nu14102153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Guevara‐Cruz M, et al. Improvement of lipoprotein profile and metabolic endotoxemia by a lifestyle intervention that modifies the gut microbiota in subjects with metabolic syndrome. J. Am. Heart Assoc. 2019;8:e012401. doi: 10.1161/JAHA.119.012401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cani PD, et al. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut. 2009;58:1091–1103. doi: 10.1136/gut.2008.165886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rault-Nania MH, et al. Inulin attenuates atherosclerosis in apolipoprotein E-deficient mice. Br. J. Nutr. 2006;96:840–844. doi: 10.1017/BJN20061913. [DOI] [PubMed] [Google Scholar]
- 137.Dourado E, Ferro M, Guerreiro CS, Fonseca JE. Diet as a modulator of intestinal microbiota in rheumatoid arthritis. Nutrients. 2020;12:3504. doi: 10.3390/nu12113504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Knudsen KEB, et al. Impact of diet-modulated butyrate production on intestinal barrier function and inflammation. Nutrients. 2018;10:1499. doi: 10.3390/nu10101499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rosenson RS. Statins in atherosclerosis: lipid-lowering agents with antioxidant capabilities. Atherosclerosis. 2004;173:1–12. doi: 10.1016/S0021-9150(03)00239-9. [DOI] [PubMed] [Google Scholar]
- 140.Zhang S, et al. Atorvastatin attenuates cold-induced hypertension by preventing gut barrier injury. J. Cardiovasc. Pharmacol. 2019;74:143–151. doi: 10.1097/FJC.0000000000000690. [DOI] [PubMed] [Google Scholar]
- 141.Vieira-Silva S, et al. Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature. 2020;581:310–315. doi: 10.1038/s41586-020-2269-x. [DOI] [PubMed] [Google Scholar]
- 142.Fukui H. Leaky gut and gut-liver axis in liver cirrhosis: clinical studies update. Gut Liver. 2021;15:666–676. doi: 10.5009/gnl20032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Munford RS. Endotoxemia–menace, marker, or mistake? J. Leukoc. Biol. 2016;100:687–698. doi: 10.1189/jlb.3RU0316-151R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rinninella E, et al. What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms. 2019;7:14. doi: 10.3390/microorganisms7010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Thursby E, Juge N. Introduction to the human gut microbiota. Biochem. J. 2017;474:1823–1836. doi: 10.1042/BCJ20160510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Berg RD. The indigenous gastrointestinal microflora. Trends Microbiol. 1996;4:430–435. doi: 10.1016/0966-842X(96)10057-3. [DOI] [PubMed] [Google Scholar]
- 147.Cani PD. Human gut microbiome: hopes, threats and promises. Gut. 2018;67:1716–1725. doi: 10.1136/gutjnl-2018-316723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dieterich W, Schink M, Zopf Y. Microbiota in the gastrointestinal tract. Med. Sci. 2018;6:116. doi: 10.3390/medsci6040116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Shin NR, Whon TW, Bae JW. Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trends Biotechnol. 2015;33:496–503. doi: 10.1016/j.tibtech.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 150.Stojanov S, Berlec A, Štrukelj B. The influence of probiotics on the Firmicutes/Bacteroidetes ratio in the treatment of obesity and inflammatory bowel disease. Microorganisms. 2020;8:1715. doi: 10.3390/microorganisms8111715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Deo PN, Deshmukh R. Oral microbiome: unveiling the fundamentals. J. Oral. Maxillofac. Pathol. 2019;23:122–128. doi: 10.4103/jomfp.JOMFP_304_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chen C, et al. Oral microbiota of periodontal health and disease and their changes after nonsurgical periodontal therapy. ISME J. 2018;12:1210–1224. doi: 10.1038/s41396-017-0037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat. Rev. Microbiol. 2018;16:745–759. doi: 10.1038/s41579-018-0089-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Del Giudice C, et al. Infective endocarditis: a focus on oral microbiota. Microorganisms. 2021;9:1218. doi: 10.3390/microorganisms9061218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Koren O, et al. Human oral, gut, and plaque microbiota in patients with atherosclerosis. Proc. Natl Acad. Sci. USA. 2011;108:4592–4598. doi: 10.1073/pnas.1011383107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bensel T, et al. Periodontal pockets as potential sources of cystic fibrosis lung infection. J. Cyst. Fibros. 2010;9:S38. doi: 10.1016/S1569-1993(10)60147-6. [DOI] [Google Scholar]
- 157.Tan L, Wang H, Li C, Pan Y. 16S rDNA-based metagenomic analysis of dental plaque and lung bacteria in patients with severe acute exacerbations of chronic obstructive pulmonary disease. J. Periodontal Res. 2014;49:760–769. doi: 10.1111/jre.12159. [DOI] [PubMed] [Google Scholar]
- 158.Prescott SL, et al. The skin microbiome: impact of modern environments on skin ecology, barrier integrity, and systemic immune programming. World Allergy Organ. J. 2017;10:29. doi: 10.1186/s40413-017-0160-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sanford JA, Gallo RL. Functions of the skin microbiota in health and disease. Semin. Immunol. 2013;25:370–377. doi: 10.1016/j.smim.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Morand A, et al. Human bacterial repertoire of the urinary tract: a potential paradigm shift. J. Clin. Microbiol. 2019;57:e00675-18. doi: 10.1128/JCM.00675-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Nielubowicz GR, Mobley HLT. Host-pathogen interactions in urinary tract infection. Nat. Rev. Urol. 2010;7:430–441. doi: 10.1038/nrurol.2010.101. [DOI] [PubMed] [Google Scholar]
- 162.Ulett GC, et al. Uropathogenic Escherichia coli virulence and innate immune responses during urinary tract infection. Curr. Opin. Microbiol. 2013;16:100–107. doi: 10.1016/j.mib.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 163.Kamisoglu K, et al. Temporal metabolic profiling of plasma during endotoxemia in humans. Shock. 2013;40:519–526. doi: 10.1097/SHK.0000000000000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Määttä AM, et al. Endotoxemia is associated with an adverse metabolic profile. Innate Immun. 2021;27:3–14. doi: 10.1177/1753425920971702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Fong Y, et al. The acute splanchnic and peripheral tissue metabolic response to endotoxin in humans. J. Clin. Invest. 1990;85:1896–1904. doi: 10.1172/JCI114651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bang FB. A bacterial disease of Limulus polyphemus. Bull. Johns. Hopkins Hosp. 1956;98:325–351. [PubMed] [Google Scholar]
- 167.Levin J, Bang FB. The role of endotoxin in the extracellular coagulation of limulus blood. Bull. Johns. Hopkins Hosp. 1964;115:265–274. [PubMed] [Google Scholar]
- 168.Sondhi P, Maruf MHU, Stine KJ. Nanomaterials for biosensing lipopolysaccharide. Biosensors. 2020;10:2. doi: 10.3390/bios10010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Grallert H, Leopoldseder S, Schuett M, Kurze P, Buchberger B. EndoLISA®: a novel and reliable method for endotoxin detection. Nat. Methods. 2011;8:iii–v. doi: 10.1038/nmeth.f.350. [DOI] [Google Scholar]
- 170.Maitra SK, Schotz MC, Yoshikawa TT, Guze LB. Determination of lipid A and endotoxin in serum by mass spectroscopy. Proc. Natl Acad. Sci. USA. 1978;75:3993–3997. doi: 10.1073/pnas.75.8.3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.De Barros JPP, et al. Quantitative lipopolysaccharide analysis using HPLC/MS/MS and its combination with the Limulus amebocyte lysate assay. J. Lipid Res. 2015;56:1363–1369. doi: 10.1194/jlr.D059725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ding X, Su W, Ding X. Methods of endotoxin detection. J. Lab. Autom. 2015;20:354–364. doi: 10.1177/2211068215572136. [DOI] [PubMed] [Google Scholar]
- 173.Xie P, et al. Highly sensitive detection of lipopolysaccharides using an aptasensor based on hybridization chain reaction. Sci. Rep. 2016;6:29524. doi: 10.1038/srep29524. [DOI] [PMC free article] [PubMed] [Google Scholar]