Abstract
Chronic wounds are a challenging medical entity for patients, medical professionals and healthcare systems. Frequently, patients present themselves to wound specialists after months or even years of unsuccessful treatment. Recent developments have resulted in a multitude of different advanced wound dressings created to treat complex, chronic wounds, one of which is the polylactide dressing Suprathel. This study aimed at investigating the healing potential of Suprathel in chronic wounds and differentiating between old and “young”, diabetic and non‐diabetic chronic wounds. A prospective, multicentric, non‐controlled intervention study was conducted, treating patients with chronic lower leg ulcers (>3 months) with Suprathel and assessing them weekly. Afterwards, a retrospective analysis was performed analysing the wound size initially, after 4 and after 8 weeks of treatment. Furthermore, a differentiation between diabetic and non‐diabetic, and chronic wounds older and younger than 12 months, was assessed. A significant reduction in wound size was observed in the study population after 8 weeks of treatment. The effect size in the diabetic wound and the old chronic wound group even reached more than one, with the other groups still showing a large effect of the intervention. This study shows that Suprathel is a valuable tool in the armamentarium of a wound specialist. Not only could we show a positive effect on chronic wounds, we could even demonstrate a significant wound size reduction in chronic wounds of old and young, as well as diabetic wounds, with the treatment of older chronic and diabetic wounds yielding an even larger effect size. Further randomised, controlled studies are necessary to show the full potential of advanced wound dressing materials in large patient cohorts.
Keywords: bandages, diabetes mellitus, re‐epithelialisation, skin ulcer, wound healing
1. INTRODUCTION
Wound care is a highly relevant medical field. Besides acute wounds in general need of being treated by surgery, chronic wounds resulting from diabetic or vascular preconditions can occur from trivial trauma that can lead to complex wounds often requiring wound management by specialists. 1 , 2 , 3 While the primary goal of wound care is quick and efficient wound closure, accomplishing this goal can be tedious and challenging. Usually, chronic wounds are found in the senescent population, resulting from comorbidities such as diabetes, vascular or other morbidities. 4 The ongoing trend towards an older and ageing society makes 'chronic wounds' an essential topic of interest and will be an even more present problem in the future. Chronic wounds can drastically impair a patient's quality of life and have an effect on caretakers and families of those affected, as well. In the end, chronic wounds are a huge burden for the healthcare system and lastly to society. 3
Plastic surgeons or other departments specialising in wound care are consulted after months or even years of unsuccessful wound treatment with “every dressing and ointment there is.”. The wounds presented and the underlying cause(s) are usually treated with the respective department's favoured standard of care – ideally adapted to the patient's individual needs. Another challenge in the treatment of chronic wounds is to start treatment as early as possible. A ‘young’ chronic wound might still show signs of possible healing like formation of granulation tissue or bleeding, while ‘older’ chronic wounds appear inert with no sign of healing whatsoever.
In most countries, the current market and the reimbursement system allow hospitals to use more elaborate, hence, more expensive wound dressings than general practitioners in their offices. Several ‘advanced’ wound dressings have been developed, including foams, hydrogels, hydrocolloids, or different polymers – more than 3000 in 2015 and rising. 5 However, the ideal wound dressing remains to be developed. 6
One of these wound dressings is Suprathel (PolyMedics Innovations GmbH, Denkendorf, Germany), initially created to improve burn care. Suprathel is a porous synthetic copolymer of DL‐lactide. The polylactide degrades to lactic acids and its salts 7 , 8 after using up physiological buffers, ultimately resulting in a signalling of hypoxic conditions in normoxic surroundings, whereby cytokines and growth factors are released influencing the wound healing cascade. 9 , 10 , 11 Given the fact that complicated and chronic wounds often show an increased pH being the foundation for infections and other complications, 12 , 13 the upregulated lactate levels, 14 which are further supported by Suprathel, provide metabolisms to support healing, suggesting Suprathel as potent dressing for the treatment of chronic wounds.
This is the first study investigating the effect of Suprathel in chronic wounds. We retrospectively analysed prospectively collected data. The primary outcome was the wound size after treatment with Suprathel. The secondary outcome was whether differences in the treatment outcome of ‘old’ or ‘young’, diabetic or non‐diabetic chronic wounds exist.
2. MATERIALS AND METHODS
The initial study was designed as a prospective, multicentric, non‐controlled intervention study. The ethics committee of the Eberhard‐Karls‐University, Tübingen, Germany, approved the study for applying the resorbable wound dressing Suprathel in chronic wounds (No. 239/2009MPG2). Preliminary data were used for the doctoral dissertation of Shubitidze, D. 15
2.1. Summary of the preliminary prospective study
The preliminary study was conducted in six hospitals in a 25‐month period. 15 In total, there were 22 participants, of whom 11 participants’ wounds (50%) had healed during the study. Only one participant's wound had not healed during the study, which was limited to 6 months per participant. Ten participants had dropped out (infection = 2, wound progress/stagnation = 5, wrong inclusion [carcinoma] = 1, amputation after trauma = 1, vascular surgical intervention = 1). Because of the high number of dropouts, the retrospective analysis was limited to an eight‐week interval.
2.2. Study design
A retrospective analysis of 22 chronic leg ulcers that were prospectively enrolled and treated with Suprathel was performed in this investigation. The wound size in cm2 after 8 weeks of treatment was defined as the primary endpoint. Initial (T0) wound size, after 4 weeks (T1) and after 8 weeks (T2) were measured. If the wound had healed, wound size was indicated as 0. Dressing changes occurred weekly.
To assess efficacy in different subgroups, wound size in wounds of less than 12 months (further referred to as ‘young’) was compared to those 12 months or older (further referred to as ‘old’) and wound size in diabetic and non‐diabetic wounds at those time points.
Inclusion criteria were a chronic wound (more than 3 months) located at the lower leg of a patient (18 years or older) of no more than 25 cm2.
2.3. Statistical analysis
Statistical analysis was performed using Prism 9 (GraphPad Software, San Diego, CA, USA). Data were analysed using means, median, standard deviation (in the following indicated as ‘±’) and other variables of descriptive statistics. To describe inferential statistics, one‐way analysis of variance (ANOVA) with repeated measures was used to analyse wound size. Tukey's multiple comparisons test was used to further investigate significance. Mann–Whitney U‐test was used for the analysis of the different subgroups at the respectively indicated timepoints. Significance was set to P < .05. Given that statistical significance can only be reached in groups with a large enough sample size, and this study was of exploratory character, P values have to be interpreted in a descriptive, non‐confirmatory sense. In addition to statistical significance, the effect size was calculated using Cohen's d, allowing an estimation of the actual effect also for small sample size groups. 16
3. RESULTS
3.1. Study population
Nineteen patients completed the study, while three were lost to follow‐up in the prospective intervention study (infection: n = 1, wound size progression: n = 1, patient's wish to terminate the study: n = 1).
The mean wound age of the patients included was 13.26 months (range: 3‐36), while the patients' age ranged from 30 to 87 years with a mean age of 69.21 years. Thirteen patients were male (68.42%), and six female (31.58%). Four of the patients suffered from diabetes mellitus (21.05%). No adverse event associated to the intervention has occurred in the study period.
Results are summarised in Table 1.
TABLE 1.
Summary of study collective and results
| Wound age (mo) | Patient age (y) | Gender (F/M) | Diabetes mellitus (Y/N) | Wound Size T0 (cm2) | Wound Size T1 (cm2) | Wound Size T2 (cm2) |
|---|---|---|---|---|---|---|
| 3 | 81 | F | N | 4 | 1 | 0 |
| 4 | 83 | F | N | 9 | 6 | 2,5 |
| 5 | 86 | F | N | 24,25 | 18 | 15 |
| 24 | 85 | F | Y | 2,8 | 2,6 | 1,2 |
| 7 | 49 | M | N | 6,25 | 12 | 5,1 |
| 4 | 71 | M | N | 25 | 6 | 3 |
| 6 | 87 | M | N | 3 | 1,4 | 1,4 |
| 18 | 53 | M | Y | 11,4 | 6,7 | 5 |
| 6 | 72 | M | N | 5,7 | 4,8 | 5,5 |
| 12 | 82 | M | N | 3,7 | 2,2 | 2,6 |
| 5 | 30 | M | N | 4 | 3,3 | 1,8 |
| 6 | 67 | M | N | 3,9 | 3,3 | 3,6 |
| 10 | 73 | M | N | 10 | 11,5 | 3,6 |
| 36 | 75 | F | N | 6,25 | 3 | 2,7 |
| 24 | 43 | F | N | 3,4 | 0 | 0 |
| 23 | 73 | M | N | 2,81 | 0,42 | 1,9 |
| 10 | 75 | M | Y | 7,4 | 6,8 | 4,3 |
| 36 | 59 | M | Y | 4,1 | 0,2 | 0 |
| 13 | 71 | M | N | 4,5 | 3,75 | 3,75 |
Note: T0 is the day of inclusion; T1 is after 4 weeks of treatment; T2 is after 8 weeks of treatment.
Abbreviations: F, female; M, male; Y, yes; N, no.
3.2. Wound healing
The average wound size at T0 was 7.45 cm2 (±6.54 cm2), at T1 4.89 cm2 (±4.66 cm2) and at T2 3.32 cm2 (±3.29 cm2). The ANOVA yielded a significant difference (P < .001). Figure 1 shows the overall wound size over time.
FIGURE 1.
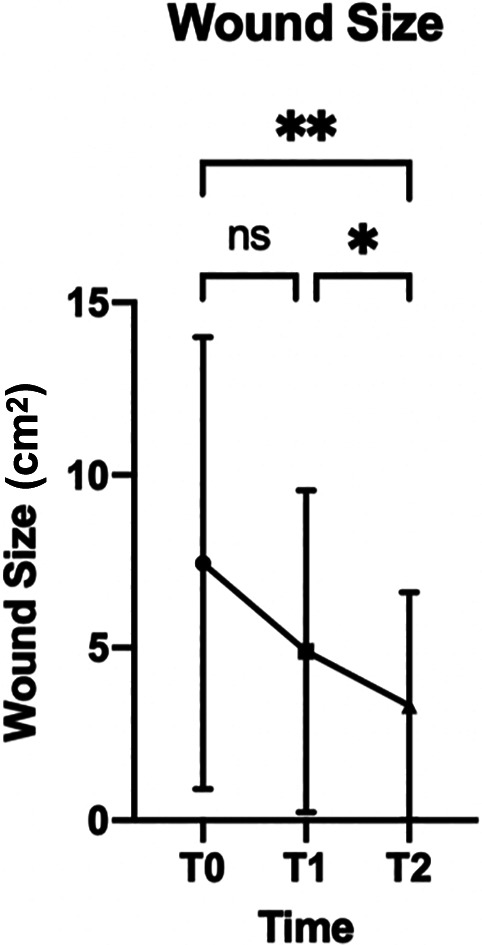
Wound size over time indicated as mean and standard deviation. T0 is the day of inclusion, T1 is after 4 weeks, and T2 is after 8 weeks. ns, not significant, * P < .05, **P < .01
While no significant difference was found between T0 and T1 (P = .074), the wound size differed significantly between T1 and T2 (P = .031). The wound size between T0 and T2 also decreased significantly (P = .006).
One of the 19 included wounds had healed at T1 already (5.3%) and two more at T2 (15.79%).
3.3. Old vs. young chronic wound
There were 8 old and 11 young wounds. The wound size at T0 did not differ significantly between these two groups (P = .113), neither did the patients' age (P = .614), the gender ratio (P > .999) or the occurrence of diabetes mellitus (P = .262). Figure 2 shows the wound healing over time of old vs. young chronic wounds.
FIGURE 2.
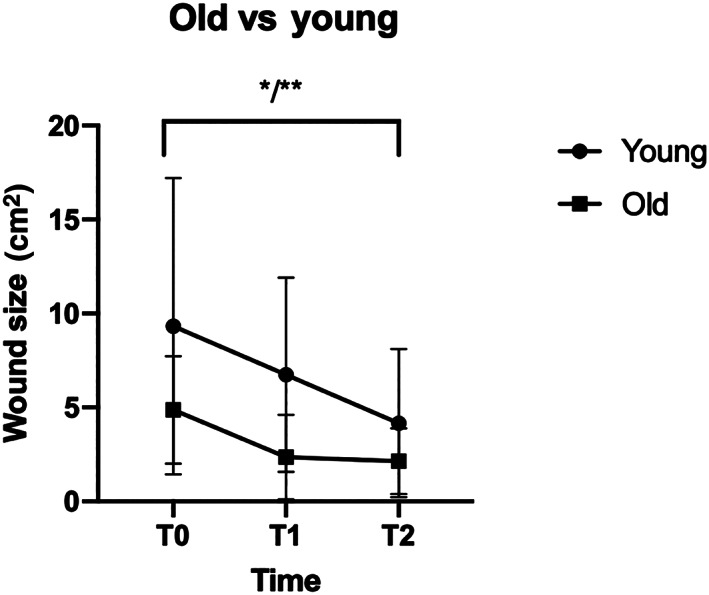
Comparison of the wound size in old vs young wounds indicated as mean and standard deviation. T0 is the day of inclusion, T1 is after 4 weeks and T2 is after 8 weeks. ns, not significant
The overall wound size showed a significant reduction in the ANOVA of old and young wounds (P = 0.002 and 0.03, respectively). In old wounds, a reduction from a mean of 4.87 cm2 (±2.86 cm2; T0) to 2.36 cm2 (±2.44 cm2; T1) and 2.14 cm2 (±1.75 cm2; T2) was observable. The overall reduction reached significance (P = .015). In young wounds, a reduction from a mean of 9.32 cm2 (±7.88 cm2; T0) to 6.74 cm2 (±5.17 cm2; T1) and 4.16 cm2 (±3.94 cm2; T2) could be seen. The reduction reached significance (P = .03).
The mean wound size reduction in old wounds during the whole study period (T0‐T2) was 5.15 cm2 (±5.99 cm2) and 2.73 cm2 (±1.86 cm2) in young wounds. The difference was not significant (P = .531).
3.4. Diabetic vs. non‐diabetic chronic wound
The average wound sizes between diabetic and non‐diabetic wounds did not differ significantly at the time of study inclusion (T0) (P = .944), the wound age differed significantly with 22 (range: 10‐36) months on average in the diabetes group and 10.93 (range: 3‐36) months in the non‐diabetes group (P = .049); the patients' age did not differ significantly (P = .899). Figure 3 shows the wound size over time in diabetic vs. non‐diabetic chronic wounds.
FIGURE 3.
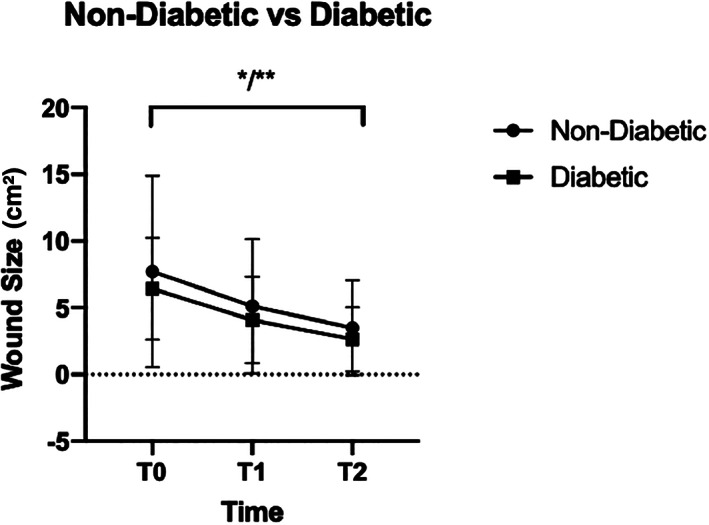
Comparison of the wound size in non‐diabetic vs diabetic wounds indicated as mean and standard deviation. T0 is the day of inclusion, T1 is after 4 weeks and T2 is after 8 weeks, ns, not significant
The overall wound size showed a significant reduction in the ANOVA of diabetic and non‐diabetic wounds (P = .005 and .015, respectively). In diabetic wounds, a reduction from a mean of 6.43 cm2 (±3.84 cm2; T0) to 4.08 cm2 (±3.24 cm2; T1) and 2.63 cm2 (±2.41 cm2; T2) was observable. The overall reduction was significant (P = .014). In non‐diabetic wounds, a reduction from a mean of 7.72 cm2 (±7.18 cm2; T0) to 5.11 cm2 (±5.04 cm2; T1) and 3.50 cm2 (±3.55 cm2; T2) could be seen. The reduction reached significance (P = .028).
The mean wound size reduction in diabetic wounds during the whole study period (T0‐T2) was 3.80 cm2 (±2.02 cm2) and 4.22 cm2 (±5.59 cm2) in non‐diabetic wounds. The difference was not significant (P = .514).
3.5. Effect size
Since the case number in the groups was relatively small, the effect size was calculated additionally. Overall, the effect size between T0 and T1 was 0.449. The effect size between T1 and T2 was 0.391, and the effect size between T0 and T2 was 0.798.
The overall effect size (T0 vs T2) of the influence of the intervention on wound size in the group with the young chronic wounds (less than 12 months) was 0.827, while the effect size (T0 vs T2) in the group with the old chronic wounds was 1.15.
The overall effect size (T0 vs T2) in the non‐diabetic group was 0.746, while the effect size (T0 vs T2) in the diabetic group was 1.183.
4. DISCUSSION
In this retrospective analysis of prospectively collected data, the healing effect of Suprathel on chronic lower leg wounds was evaluated. A significant reduction in wound size was seen after treatment for 8 weeks with high effect sizes on wound size reduction in wounds older or younger than 12 months, diabetic or non‐diabetic wounds.
The polylactide wound dressing Suprathel was initially designed to treat burn wounds. 7 Consequently, several studies have investigated its effectiveness on burn wounds of different degrees with promising results. 17 , 18 Its use as an epidermal skin substitute with no need for frequent dressing changes makes it an effective wound dressing for split‐thickness skin donor sites. 8 , 19 Furthermore, it was used successfully in toxic epidermal necrolysis cases in infants. 20
Given that burn wounds can take several months to heal and are therefore usually classified as complex wounds, 21 the promising results of the use of Suprathel in the indications mentioned above implied the use in another group of complex wounds: the chronic wound. This is the first report of the use of Suprathel in chronic wounds to the authors' knowledge. Our study population included a valid and representative cohort of elderly patients in terms of assessed parameters, typically suffering from chronic lower leg ulcers. 4 , 22
We observed no significant reduction in wound size after the initial 4 weeks of treatment, with the ‘healing effect’ becoming apparent after another 4 weeks (8 weeks of treatment); however, given the small sample size, we could see an effect on wound size reduction of d = 0.449. Many chronic wounds are inert, and the wound healing cascade appears to have stopped before properly entering the proliferation phase. 23 These chronic wounds have a higher pH in their ‘resting state’, which favours bacterial growth, closing the vicious circle and showing colonisation with a multitude of different stems of bacteria, further inhibiting wound healing. 22 , 24 With advanced wound healing, a wound's pH decreases towards more acidic, and the typical pH values of the surface of healed skin of 4 to 6. 13 , 25 , 26 , 27 This release of lactate anions, which is the working principle of Suprathel, 7 might cause a marked reduction of bacterial load. 28 Furthermore, the postulated increase of lactate as energy provider for wound healing and inductor of cytokines ultimately catalyses the resumption of the wound healing cascade. Given the inactive and often desolate status of chronic wounds, a delayed effect on wound size reduction could be explained that shows already a high effect of d = 0.449 and even reaches significance not after four but after 8 weeks of treatment.
Since we intended to investigate whether ‘old’ chronic wounds (12 months or older) can be treated the same way as ‘younger’ chronic wounds (between 3 and 12 months), we compared two groups in which the wounds were classified according to their age. Comparing wound size, gender ratio, patients' age and occurrence of diabetes as co‐morbidity at T0 showed no significant differences between the two groups, yet due to the small sample size, (non‐)significance cannot be seen as confirmatory. A significant wound size reduction in both groups (P = .002 and .03, respectively) and high effect sizes (d = 1.15 and 0.87) on wound size could be seen, therefore suggesting the conclusion that ‘old’ and ‘young’ chronic wounds can be effectively treated with Suprathel. While significance has to be seen in a descriptive manner due to the low sample size, the high effect sizes indicate an effective treatment. It is assumable that once a wound has become chronic, it becomes self‐sustaining with insignificant alterations in its healing potential. The higher effect size, observed in the group with ‘older’ chronic wounds (1.15 vs 0.87), however, indicates differently: despite the very large effect size in both groups (<0.5 is considered as large theoretically, 16 empirically values higher than 0.3 ought to show a large effect 29 ), the use of Suprathel appears to have a larger effect on ‘older’ chronic wounds. Since we could not retrieve a single study from the available online literature investigating the healing potential of ‘old’ vs ‘young’ chronic wounds, no temporal comparison with other studies is possible. Further studies are necessary to properly evaluate treatment, metabolism and the local differences in differently aged chronic wounds.
In addition to wound age, we tried to further differentiate between diabetic and non‐diabetic wounds. A significantly higher wound age was seen prior to the treatment in the diabetes group, emphasising once more the diabetic preconditions as a risk factor for (highly) prolonged wound healing. 22 When comparing the diabetic and non‐diabetic groups, a significant reduction in both groups (diabetic: P = .005 and non‐diabetic: P = .015) could be seen, while the effect size showed a larger effect in the diabetic than in the non‐diabetic group (1.186 vs 0.798). This difference in effect size could however be seen due to different base value from the beginning (not significant at T0, but possible camouflage thereof due to the low sample size). An investigation analysing pH and surface temperature in diabetic vs. non‐diabetic chronic foot ulcers showed no significant differences of those biomarkers between the groups. 30 Consequently, similar conclusions are therefore to be drawn regarding wound aetiology: diabetic and non‐diabetic chronic wounds can effectively be treated with Suprathel. However, this statement needs to be put in parentheses as the case number in the diabetic group was very low.
4.1. Limitations and outlook
The case number was limited, which resulted in the additional calculation of the effect size as a parameter, further allowing the interpretation of our results. This limited case number primarily affects diabetic vs. non‐diabetic wounds: There were only four cases with diabetic wounds included in the analysis. Another reason for the low number of diabetic wounds is that diabetic chronic wounds were more likely to be lost during the initial prospective study course, only allowing the retrospective evaluation until after 8 weeks. During the prospective study, diabetic wounds developed complications (e.g., infections) more often, which resulted in premature termination of the intervention study, hence not allowing a proper analysis. The time interval analysed in this investigation (8 weeks) was also heavily affected by the high number of dropouts after 8 weeks (data not shown), which would have resulted in a distortion further yielding no usable statistical analysis. The dropouts, however, were not associated with adverse events associated to the intervention. Finally, further differentiation in the aetiology of the chronic wounds (venous, pressure ulcers, etc.) was not assessed. While the wounds could be considered as their own control group (not having shown signs of healing for 12 weeks), the lack of a proper control group and, therefore, a possible bias by wounds that would have healed without intervention, needs to be listed as limitation as well. Future studies with large sample sizes should be performed to further evaluate the true effect of Suprathel on different kinds of chronic wounds; this study was able to show a large effect size in young, old, diabetic and non‐diabetic wounds in a small sample for the first time. Follow‐up studies are important to gain more insight in possible effective therapies of long‐term unhealed wounds, whose implications have a major impact on health services and the health of those who suffer from such wounds.
In conclusion, this study shows that Suprathel is both safe and efficacious for treating chronic wounds. Hence, it is a valuable tool in the armamentarium of a wound care specialist. A significant wound size reduction could be shown in our cohort consisting of chronic wounds of old and young age as well as diabetic and non‐diabetic wounds. Differences in effect sizes suggest that future studies with larger cohort sizes that assess aetiology in addition to the wound age should be performed, ideally in a prospective, controlled and randomised manner.
CONFLICT OF INTEREST
Herbert L. Haller is a medical consultant for training and teaching for Polymedics Innovations GmbH. Other than that, there is no conflict of interest to be reported in association with this study.
Nischwitz SP, Popp D, Shubitidze D, et al. The successful use of polylactide wound dressings for chronic lower leg wounds: A retrospective analysis. Int Wound J. 2022;19(5):1180-1187. doi: 10.1111/iwj.13713
Funding informationPMI funded the conduction of the prospective intervention study. The company did not take any influence on the patient selection or the results of the study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Jones RE, Foster DS, Longaker MT. Management of Chronic Wounds‐2018. JAMA. 2018;320:1481‐1482. doi: 10.1001/jama.2018.12426 [DOI] [PubMed] [Google Scholar]
- 2. Atkin L. Chronic wounds: the challenges of appropriate management. Br J Community Nurs. 2019;24:S26‐S32. doi: 10.12968/bjcn.2019.24.Sup9.S26 [DOI] [PubMed] [Google Scholar]
- 3. Olsson M, Järbrink K, Divakar U, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 2019;27:114‐125. doi: 10.1111/wrr.12683 [DOI] [PubMed] [Google Scholar]
- 4. Mustoe T. Understanding chronic wounds: a unifying hypothesis on their pathogenesis and implications for therapy. Am J Surg. 2004;187:S65‐S70. doi: 10.1016/S0002-9610(03)00306-4 [DOI] [PubMed] [Google Scholar]
- 5. Dhivya S, Padma VV, Santhini E. Wound dressings‐a review. BioMed. 2015;5:24‐28. doi: 10.7603/s40681-015-0022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Popp D, Tapking C, Branski LK. Skin substitutes for burn wounds. Regenerative Medicine and Plastic Surgery. Cham: Springer International Publishing; 2019:137‐146. doi: 10.1007/978-3-030-19962-3_10 [DOI] [Google Scholar]
- 7. Haller HL, Rapp M, Popp D, Nischwitz SP, Kamolz LP. Made in Germany: a quality indicator not only in the automobile industry but also when it comes to skin replacement: how an automobile textile research institute developed a new skin substitute. Medicina. 2021;57:1‐16. doi: 10.3390/medicina57020143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schwarze H, Küntscher M, Uhlig C, et al. Suprathel®, a new skin substitute, in the management of donor sites of split‐thickness skin grafts: results of a clinical study. Burns. 2007;33:850‐854. doi: 10.1016/j.burns.2006.10.393 [DOI] [PubMed] [Google Scholar]
- 9. Philp A, Macdonald AL, Watt PW. Lactate‐a signal coordinating cell and systemic function. J Exp Biol. 2005;208:4561‐4575. doi: 10.1242/jeb.01961 [DOI] [PubMed] [Google Scholar]
- 10. Constant JS, Feng JJ, Zabel DD, et al. Lactate elicits vascular endothelial growth factor from macrophages: a possible alternative to hypoxia. Wound Repair Regen. 2000;8:353‐360. doi: 10.1111/j.1524-475x.2000.00353.x [DOI] [PubMed] [Google Scholar]
- 11. Trabold O, Wagner S, Wicke C, et al. Lactate and oxygen constitute a fundamental regulatory mechanism in wound healing. Wound Repair Regen. 2003;11:504‐509. doi: 10.1046/j.1524-475X.2003.11621.x [DOI] [PubMed] [Google Scholar]
- 12. Nischwitz SP, Bernardelli de Mattos I, Hofmann E, et al. Continuous pH monitoring in wounds using a composite indicator dressing—a feasibility study. Burns. 2019;45:1336‐1341. doi: 10.1016/j.burns.2019.02.021 [DOI] [PubMed] [Google Scholar]
- 13. Power G, Moore Z, O'Connor T. Measurement of pH, exudate composition and temperature in wound healing: a systematic review. J Wound Care. 2017;26:381‐397. doi: 10.12968/jowc.2017.26.7.381 [DOI] [PubMed] [Google Scholar]
- 14. Dalton SJ, Whiting CV, Bailey JR, Mitchell DC, Tarlton JF. Mechanisms of chronic skin ulceration linking lactate, transforming growth factor‐β, vascular endothelial growth factor, collagen remodeling, collagen stability, and defective angiogenesis. J Invest Dermatol. 2007;127:958‐968. doi: 10.1038/sj.jid.5700651 [DOI] [PubMed] [Google Scholar]
- 15. Shubitidze DK. Prospektive Multicenterstudie für eine neue Lokaltherapie des Ulcus cruris mit einer resorbierbaren Wundabdeckung (Suprathel); 2016.
- 16. Cohen J. A power primer. Psychol Bull. 1992;112:155‐159. doi: 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- 17. Hundeshagen G, Collins VN, Wurzer P, et al. A prospective, randomized, controlled trial comparing the outpatient treatment of pediatric and adult partial‐thickness burns with suprathel or Mepilex Ag. J Burn Care Res. 2018;39:261‐267. doi: 10.1097/BCR.0000000000000584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keck M, Selig HF, Lumenta DB, Kamolz LP, Mittlböck M, Frey M. The use of Suprathel® in deep dermal burns: first results of a prospective study. Burns. 2012;38:388‐395. doi: 10.1016/j.burns.2011.09.026 [DOI] [PubMed] [Google Scholar]
- 19. Kaartinen IS, Kuokkanen HO. Suprathel® causes less bleeding and scarring than Mepilex® transfer in the treatment of donor sites of split‐thickness skin grafts. J Plast Surg Hand Surg. 2011;45:200‐203. doi: 10.3109/2000656X.2011.583515 [DOI] [PubMed] [Google Scholar]
- 20. Pfurtscheller K, Zobel G, Roedl S, Trop M. Use of Suprathel® dressing in a young infant with TEN. Pediatr Dermatol. 2008;25:541‐543. doi: 10.1111/j.1525-1470.2008.00766.x [DOI] [PubMed] [Google Scholar]
- 21. Hall C, Hardin C, Corkins CJ, et al. Pathophysiologic mechanisms and current treatments for cutaneous sequelae of burn wounds. Compr Physiol. 2018;8:371‐405. doi: 10.1002/cphy.c170016 [DOI] [PubMed] [Google Scholar]
- 22. Mustoe TA, O'Shaughnessy K, Kloeters O. Chronic wound pathogenesis and current treatment strategies: a unifying hypothesis. Plast Reconstr Surg. 2006;117:35S‐41S. doi: 10.1097/01.prs.0000225431.63010.1b [DOI] [PubMed] [Google Scholar]
- 23. Inoue Y, Hasegawa M, Maekawa T, et al. The wound/burn guidelines‐1: wounds in general. J Dermatol. 2016;43:357‐375. doi: 10.1111/1346-8138.13276 [DOI] [PubMed] [Google Scholar]
- 24. Halbert AR, Stacey MC, Rohr JB, Jopp‐Mckay A. The effect of bacterial colonization on venous ulcer healing. Australas J Dermatol. 1992;33:75‐80. doi: 10.1111/j.1440-0960.1992.tb00083.x [DOI] [PubMed] [Google Scholar]
- 25. Schneider LA, Korber A, Grabbe S, Dissemond J. Influence of pH on wound‐healing: a new perspective for wound‐therapy? Arch Dermatol Res. 2007;298:413‐420. doi: 10.1007/s00403-006-0713-x [DOI] [PubMed] [Google Scholar]
- 26. Shukla VK, Shukla D, Tiwary SK, Agrawal S, Rastogi A. Evaluation of pH measurement as a method of wound assessment. J Wound Care. 2007;16:291‐294. doi: 10.12968/jowc.2007.16.7.27062 [DOI] [PubMed] [Google Scholar]
- 27. Sharpe JR, Booth S, Jubin K, Jordan NR, Lawrence‐Watt DJ, Dheansa BS. Progression of wound pH during the course of healing in burns. J Burn Care Res. 2013;34:e201‐e208. doi: 10.1097/BCR.0b013e31825d5569\ [DOI] [PubMed] [Google Scholar]
- 28. Kurabayashi H, Tamura K, Machida I, Kubota K. Inhibiting bacteria and skin pH in hemiplegia: effects of washing hands with acidic mineral water. Am J Phys Med Rehabil. 2002;81:40‐46. doi: 10.1097/00002060-200201000-00007 [DOI] [PubMed] [Google Scholar]
- 29. Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Personal Individ Differ. 2016;102:74‐78. doi: 10.1016/j.paid.2016.06.069 [DOI] [Google Scholar]
- 30. Gethin G, O'Connor GM, Abedin J, et al. Monitoring of pH and temperature of neuropathic diabetic and nondiabetic foot ulcers for 12 weeks: an observational study. Wound Repair Regen. 2018;26:251‐256. doi: 10.1111/wrr.12628 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


