Abstract
Chronic wounds commonly decrease patients' quality of life. Understanding how chronic wounds impact a patient's health‐related quality of life (HRQoL) is important for healthcare service delivery and treatment management. This study explored HRQoL among patients suffering from chronic wounds and investigated associations with patients' socio‐demographics and wound characteristics. Two hundred and thirty‐three patients across six primary care clinics were assessed and responded to a survey that collected information on socio‐demographic, wound characteristics, and HRQoL using the EQ‐5D‐5L instrument. Data were analysed by descriptive statistics and generalised linear models. The mean age of patients was 61.2 (SD: 14.6) years; 68.2% were males; and 61.8% were of Chinese origin. Arterial ulcers had the greatest negative impact on HRQoL related to mobility, self‐care, pain/discomfort and anxiety/depression, and the lowest VAS mean score 62.31 (SD: 28.3; range: 0‐100) indicating the worst health. HRQoL related to mobility was significantly associated with age (β = 0.008, P < .001), non‐Chinese ethnicity (β = 0.25, P = .001), mixed ulcers (β = −0.41, P = .022), atypical hard‐to‐heal wounds (β = −0.38, P = .021), wounds with low (β = 0.24, P = .044) to moderate (β = 0.29, P = .018) exudate level, and a wound duration ≥6 months (β = 0.19, P = .033). The findings can be used to improve healthcare delivery for patients with chronic wound to optimise their HRQoL.
Keywords: chronic wound, health‐related quality of life, primary care, Singapore, socio‐demographics
1. INTRODUCTION
Chronic or hard‐to‐heal wounds are commonly defined as wounds that have not reduced in size by more than 40% to 50% 1 or healed within 1 month. 2 , 3 The global prevalence of chronic wounds is estimated at 1.51 to 2.21 per 1000 population, 4 and the incidence is expected to rise with ageing populations worldwide. 5 Chronic wounds may have different aetiologies and are commonly classified in the categories of diabetic foot ulcers (DFUs), wounds related to peripheral arterial disease, venous leg ulcers, pressure injuries (PIs), 6 and atypical hard‐to‐heal wounds (AHHW). 7 , 8 Healing of chronic wounds depends on several complex biological factors and wound care regimens. 9 , 10 However, even after a chronic wound heals up to 40% of DFUs 11 and 69% of venous leg ulcers 12 may recur within 1 year.
Chronic wounds are associated with significant physical, emotional, and economic burdens, 13 both at an individual 14 , 15 and societal level. 16 , 17 , 18 Heath‐related quality of life (HRQoL) is a patient‐reported outcome that presents the patient's own perception of well‐being 19 and reflects the total impact of health and illness on the individual. 20 HRQoL is decreased in chronic wound patients since wounds often cause physical problems, impaired mobility, social distress, pain, depression, and restricted lifestyle. 13 , 15 , 21 , 22 , 23 , 24 , 25 Understanding the factors that contribute to HRQoL in patients with chronic wounds can guide the identification of patients in whom further support may improve their quality of life outcomes. 15 , 21 Assessing HRQoL in patients with chronic conditions is increasingly important as it provides valuable knowledge that can be used to highlight and develop interventions to assist patients to achieve the best possible patient outcomes and HRQoL. 21
HRQoL is a complex multidimensional concept related to physical function, psychological state, psychosocial life and physical symptoms, which enables an understanding of the general health and health status. 26 Instruments developed to collect data on HRQoL can either be disease specific or generic. There are several disease‐specific instruments developed for wound patients, 27 such as the Cardiff Wound Impact Schedule, Würzburg Wound Score and Freiburg Life Quality Assessment. 28 , 29 , 30 Generic HRQoL instruments collect data that is not specific to a disease or condition and can be applied to any population, 19 , 31 which have the advantage that HRQoL can be compared across different disease groups. 32
In Singapore, the incidence of chronic wound has increased exponentially over the past two decades and is expected to raise further due to a rapidly ageing population and growing prevalence of chronic conditions, such as diabetes. 5 The increased prevalence of chronic wounds in Singapore has generated a significant clinical and economic burden related to extended wound care services and healthcare costs at both a hospital and primary care level. 33 There is limited knowledge about the factors associated with HRQoL for patients with chronic wound treated in primary care. This study therefore aimed at exploring HRQoL and associations with patients' socio‐demographic and wound characteristics in a multi‐ethnic primary care population.
2. MATERIALS AND METHODS
2.1. Study design and participants
This population‐based cross‐sectional study explored associations between HRQoL, clinical wound characteristics and socio‐demographic in patients with chronic wounds that were treated in primary care in Singapore. Patients were recruited between March and April 2018 from six general primary care clinics. Included patients had to receive wound care at the primary care clinic for a wound that was chronic (not healed within 1 month), be 21 years of age or older or have a Legally Authorised Representative that could give consent for their participation in the study. Patients with malignant and surgical wounds that were healing by primary intention were excluded. All patients with chronic wounds who visited the participating primary care clinics for wound care during the recruitment period were assessed by their attending nurses for eligibility on their treatment day. Eligible patients were invited to participate in the study and introduced to research assistants who provided information about the study.
2.2. Instruments and outcome measures
A pre‐developed Wound Care Inventory Questionnaire including wound management, healthcare service utilisation and the instrument was used to obtain data on patient socio‐demographic, specific clinical wound information, healthcare service use, medical history and patient‐reported HRQoL. The questionnaire was inspired by the Client Socio‐Demographic and Service Receipt Inventory 34 and developed in close collaboration with wound care experts and clinicians to collect data relevant for patients receiving wound care in Singapore. Patients were administered the survey to fill in the non‐clinical sections (eg, socio‐demographic data and the HRQoL instrument) after they had received their wound care at the clinics. The survey was either self‐administered or filled in with the aid of the research assistants. Patients were offered to sit in a designated area at the clinics that offered more privacy while filling in the survey.
2.2.1. Health‐related quality of life
The generic and validated instrument EQ‐5D‐5L 35 is self‐reported by patients and consists of two parts: a descriptive system and a visual analogue scale (VAS). The descriptive system contains questions relating to five domains of health, namely, mobility, self‐care, usual activities, pain/discomfort and anxiety/depression. There are five levels to each question ranging from ‘no problems’, ‘slight problems’, ‘moderate problems’, ‘severe problems’ to ‘extreme problems’ or ‘unable to’. The VAS is a 20 cm long vertical line that ranges from ‘worst imaginative health state’ set at 0 to ‘best imaginable health state’ set at 100, where respondents rate their current health status. EQ‐5D‐5L was available in all language versions for which the instrument is validated in Singapore (English, Mandarin, Malay and Tamil).
2.2.2. Wound characteristics
Wound characteristics and other medical data were extracted from the patients' medical record at the primary care clinics. Wounds were classified as venous ulcers, arterial ulcers, mixed (arterial and venous) ulcers, DFUs and atypical hard‐to‐heal wounds, which were those chronic wounds that presented atypical clinical features and did not fall into a typical wound category, that is, venous, arterial, mixed, pressure injury or DFU 1 , 7 , 8 and failed to heal following a normal healing trajectory. Pressure injuries, sinus wounds and wounds with unclear aetiology were categorised as ‘others’ due to the small number of patients that suffered from those wound types. For patients with more than one wound, only the wound assessed as the most severe, was described.
Trained registered nurses ascertained wound characteristics in accordance with medical records and institutional wound management guidelines. This included wound aetiology, wound size, wound exudate level, wound bed appearance and wound infection. Wound size was recorded in square centimetres (cm2). Appearance of wound bed referred to the percentage of wound bed tissue including necrotic, granulating, sloughy and epithelialising. Wound exudate level was assessed based on wound exudate score and reported as ‘none’, ‘low’, ‘moderate’ and ‘heavy’. 36 Wound infection referred to wounds that were treated with oral antibiotics. Other wound variables included wound duration, number of wounds, wound location and dressing frequency.
2.3. Ethical considerations
The study was approved by the Institutional Review Board of Nanyang Technological University (IRB‐2017‐05‐020‐02) and the National Healthcare Group Domain Specific Review Board (2017/01159). Written and verbal information about the study was provided to participants, and they were informed that participation was voluntary. Signed informed consent from participants was obtained prior to participation in the survey.
2.4. Data analysis
Descriptive statistics are reported with mean and standard deviation (SD) for continuous variables, and categorical variables are reported with frequencies with proportions. Kolmogorov–Smirnov and Shapiro–Wilk tests were used to assess the normality of continuous variables. Furthermore, as HRQoL variables were measured on nonlinear, ordinary linear regression with log‐transformation is not appropriate due to the ‘retransformation bias’. 37 Therefore, generalised linear model (GLM) with gamma family log link function was used to explore association between socio‐demographic and wound‐related factors with HRQoL outcome variables. The modified Park test was used to select the appropriate family within the GLM approach using the most likely appropriate variance function. The estimated coefficient (λ) from the modified Park test indicated that a gamma family was appropriate (λ value close to 2 indicates Gamma family). 37 Regression coefficients with corresponding standard errors (SE) are reported. A range of goodness‐of‐fit measures was used to assess the fitting of the model such as deviance distribution, correlation between observed and predicted outcome, and link test for model adequacy. Co‐linearity and interactions between predictors and outcomes were controlled for when necessary. All statistical analyses were performed by using Stata software version 16.1 (StataCorp, College Station, Texas). A two‐tailed P‐value <.05 was considered statistically significant for the analysis.
3. RESULTS
3.1. Demographic and clinical characteristics of patients with chronic wounds
A total of 233 patients participated in the study (Table 1). The mean age of patients was 61.2 ± 14.6 years and 68.2% of the sample were males. Chinese (61.8%) was the most common ethnicity, and almost half of the study population were either full‐time, part‐time or self‐employed. Most patients lived in 4 to 5 room (58.5%) and 1 to 3 room (33.5%) HDB (public housing) flats. In the sample, 43.8% had 1 to 2 comorbidities and 39.9% had more than two comorbidities. The majority of patients (61.3%) were diagnosed with diabetes. A little less than half of the sample suffered from hypertension. Almost one‐third of participants had kidney disease.
TABLE 1.
Socio‐demographic and clinical characteristics of study participants
| Patient characteristics | n (%) / mean (SD) (n = 233) |
|---|---|
| Age (years) (mean (SD)) | 61.2 (14.6) |
| Gender | |
| Female | 74 (31.8) |
| Male | 159 (68.2) |
| Ethnicity | |
| Chinese | 144 (61.8) |
| Malay | 34 (14.6) |
| Indian | 51 (21.9) |
| Others | 4 (1.7) |
| Employment status | |
| Employed full‐time/part‐time/ self‐employed | 109 (46.8) |
| Retired | 77 (33.1) |
| Unemployed/ students/ housewife | 47 (20.17) |
| Accommodation | |
| 1‐3 room public housing flats | 78 (33.5) |
| 4‐5 room public housing flats | 137 (58.8) |
| Others | 18 (7.7) |
| Number of comorbidities | |
| 0 | 38 (16.3) |
| 1‐2 | 102 (43.8) |
| ≥3 | 93 (39.9) |
| Comorbidities | |
| Autoimmune disease | 1 (0.4) |
| Cerebro‐vascular accident | 15 (6.4) |
| COPD | 1 (0.4) |
| Deep venous thrombosis | 3 (1.3) |
| Diabetes mellitus | 143 (61.4) |
| Gout | 13 (5.6) |
| Heart disease | 50 (21.5) |
| Hypertension | 106 (45.5) |
| Kidney disease | 69 (29.6) |
| Osteoarthritis | 18 (7.7) |
| Peripheral vascular disease | 59 (24.9) |
| Rheumatoid arthritis | 2 (0.9) |
Abbreviations: COPD, chronic obstructive pulmonary disease; SD, standard deviation.
3.2. Wound aetiology and characteristics of chronic wounds
Patients with AHHW (34.3%) and DFU (33.5%) made up two‐thirds of the study population. Most patients (70.4%) had only one wound. The majority of the wounds were located to the foot (40.3%) or lower leg (33.0%). Nearly half of the wounds (46.4%) were small (<2 cm2). The main bulk of wounds (87.6%) appeared granulating and approximately one‐third had medium (32.2%) or high (2.6%) exudate levels. More than half of the wounds had a duration shorter than 6 months. Less than every fifth wound (18.5%) was a recurrent wound. Nearly half (48.1%) of the wounds were infected. Chronic wound aetiologies and characteristics are presented in Table 2.
TABLE 2.
Wound aetiology and characteristics of chronic wounds
| Wound aetiology characteristics (n = 233) | n (%) |
|---|---|
| Wound aetiology | |
| Venous ulcer | 24 (10.3) |
| Arterial ulcer | 13 (5.6) |
| Mixed ulcer | 18 (7.7) |
| DFU | 78 (33.5) |
| AHHW | 80 (34.3) |
| Othersa | 20 (8.6) |
| No of wound(s) | |
| 1 | 164 (70.4) |
| 2 | 55 (23.6) |
| ≥3 | 14 (6.0) |
| Location of most serious wound | |
| Head or neck | 9 (3.9) |
| Arms | 2 (0.9) |
| Chest | |
| Abdomen | 14 (6.0) |
| Back | 14 (6.0) |
| Sacrum | 3 (1.3) |
| Hip | 1 (0.4) |
| Upper leg/groin | 8 (3.4) |
| Lower leg/ankle | 77 (33.1) |
| Foot | 94 (40.3) |
| Others | 11 (4.7) |
| Wound size (cm2) | |
| <2 | 108 (46.4) |
| 2‐5 | 57 (24.5) |
| 6‐10 | 33 (14.2) |
| 11‐25 | 19 (8.2) |
| >25 | 8 (3.4) |
| Not applicable | 8 (3.4) |
| Appearance of wound bed | |
| Necrotic | 8 (3.4) |
| Granulating | 204 (87.6) |
| Sloughy | 85 (36.5) |
| Epithelialising | 58 (24.9) |
| Fungating | 1 (0.4) |
| Exudate level | |
| Low | 132 (56.7) |
| Medium | 75 (32.2) |
| High | 6 (2.6) |
| Wound duration | |
| 4‐6 weeks | 65 (27.9) |
| 6 weeks to <3 months | 57 (24.5) |
| 3 months to <6 months | 46 (19.7) |
| 6 months to 1 year | 29 (12.5) |
| 1‐5 years | 29 (12.5) |
| >5 years | 7 (3.0) |
| Recurrent wound | 43 (18.5) |
| Infected wound | 112 (48.1) |
Abbreviations: AHHW, atypical hard‐to‐heal wounds; DFU, diabetic foot ulcers.
Others refer to pressure injuries, sinus wounds and wounds with unclear aetiology.
3.3. EQ‐5D‐5L distribution across genders, frequencies and proportions reported by domains and level of problems
There was no difference in the overall response pattern of HRQoL outcomes between male and female participants (Figure 1). More than half of the patients reported ‘no problems’ across all five domains. Most patients perceived ‘slight/moderate/severe/extreme problems’ for HRQoL related to the domains mobility and pain/discomfort compared to the other three domains (Table 3).
FIGURE 1.
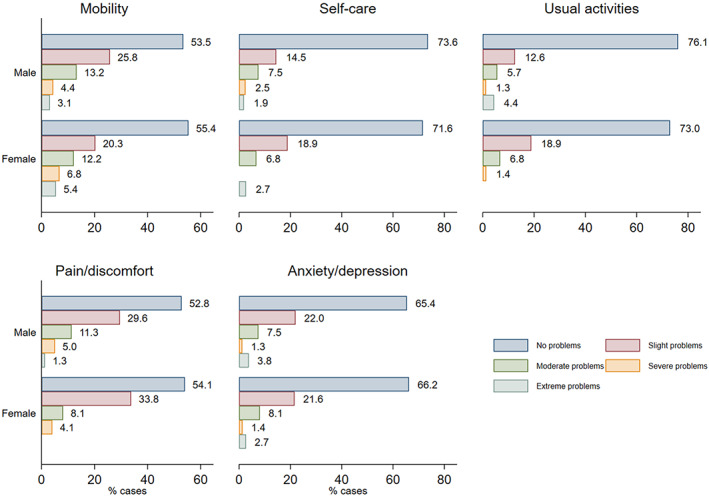
Distribution of health‐related quality of life responses across genders assessed with EQ‐5D‐5L questionnaire
TABLE 3.
EQ‐5D‐5L frequencies and proportions reported by domain and level of problem (n = 233)
| Mobility n (%) | Self‐care n (%) | Usual activities n (%) | Pain/discomfort n (%) | Anxiety/depression n (%) | |
|---|---|---|---|---|---|
| No problems | 127 (54.4) | 169 (72.6) | 174 (74.6) | 125 (53.5) | 153 (65.8) |
| Any problems (slight, moderate, severe and extreme problems) | 106 (45.6) | 64 (27.4) | 60 (25.6) | 109 (46.5) | 80 (34.2) |
| Total | 233 (100) | 233 (100) | 233 (100) | 233 (100) | 233 (100) |
3.4. HRQoL scores according to wound aetiology, wound exudate level and wound duration
Table 4 shows HRQoL EQ‐5D‐5L and VAS mean scores according to wound aetiology, wound exudate level and wound duration in which the domain mobility had the lowest overall mean score 1.81 (SD: 1.09; range: 0‐5) across all domains indicating the greatest impact. There was a variation between different wound aetiologies in which arterial ulcers had the highest mean scores for HRQoL related to mobility 2.23 (SD:1.17; range: 0‐5), self‐care 1.92 (SD: 1.38; range: 0‐5), pain/discomfort 2.00 (SD: 1.22; range: 0‐5) and anxiety/depression 1.69 (SD: 0.95; range: 0‐5), and the lowest VAS mean score 62.31 (SD: 28.3; range: 0‐100), indicating the greatest negative impact on HRQoL compared to other wound aetiologies. Mean HRQoL scores also varied between different exudate levels in which patients with medium to high levels of wound exudate had greater mean scores with mobility and self‐care and having lower mean VAS score compared to a low level of wound exudate. A variation between different wound durations and HRQoL was also found in which the lowest mean score of HRQoL related to mobility 2.24 (SD: 1.46; range: 0‐5) and pain/discomfort 2.07 (SD: 0.84; range: 0‐5) and indicated the lowest perceived HRQoL among patients with a wound duration between 6 months to 1‐year, while the lowest VAS mean score 67.81 (SD: 23.04; range: 0‐100) was for wound durations of 6 weeks to 3 months, which also was the duration displaying the greatest negative impact on HRQoL.
TABLE 4.
HRQoL EQ‐5D‐5L scores and VAS scores according to wound aetiology, wound exudate level and wound duration (n = 233)
| HRQoL EQ‐5D and VAS | ||||||
|---|---|---|---|---|---|---|
| Mobility | Self‐care | Usual activities | Pain/discomfort | Anxiety/depression | VAS score | |
| Parameters | Mean (SD) | |||||
| Wound aetiology | ||||||
| Venous ulcer (n = 24) | 1.79 (1.14) | 1.33 (0.70) | 1.25 (0.53) | 1.96 (1.00) | 1.54 (1.02) | 73.96 (20.54) |
| Arterial ulcer (n = 13) | 2.23 (1.17) | 1.92 (1.38) | 1.46 (0.97) | 2.00 (1.22) | 1.69 (0.95) | 62.31 (28.33) |
| Mixed ulcer (n = 18) | 1.61 (0.85) | 1.44 (0.98) | 1.33 (0.69) | 1.67 (0.91) | 1.33 (0.97) | 77.50 (11.91) |
| DFU (n = 78) | 2.00 (1.14) | 1.50 (0.99) | 1.50s (1.03) | 1.56 (0.77) | 1.60 (0.90) | 74.38 (16.93) |
| AHHW (n = 80) | 1.51 (0.83) | 1.35 (0.64) | 1.40 (0.85) | 1.68 (0.92) | 1.55 (1.02) | 74.60 (18.83) |
| Others (n = 20) | 2.15 (1.60) | 1.40 (0.82) | 1.50 (1.05) | 1.75 (0.91) | 1.45 (0.76) | 72.00 (13.51) |
| Wound exudate level | ||||||
| Low (n = 132) | 1.78 (1.11) | 1.44 (0.92) | 1.44 (0.95) | 1.72 (0.86) | 1.52 (0.93) | 74.66 (19.05) |
| Medium (n = 75) | 1.93 (1.03) | 1.48 (0.83) | 1.40 (0.84) | 1.71 (0.93) | 1.63 (0.98) | 73.40 (18.45) |
| High (n = 6) | 1.83 (0.75) | 1.67 (1.03) | 1.33 (0.82) | 1.67 (0.82) | 1.50 (0.84) | 68.33 (17.22) |
| Wound duration | ||||||
| 4‐6 weeks (n = 65) | 1.62 (0.90) | 1.54 (0.95) | 1.51 (1.00) | 1.60 (0.81) | 1.48 (0.75) | 75.77 (13.47) |
| 6 weeks to <3 months (n = 57) | 1.82 (1.10) | 1.35 (0.79) | 1.42 (1.02) | 1.68 (1.07) | 1.54 (0.98) | 67.81 (23.04) |
| 3 months to <6 months (n = 46) | 1.74 (1.00) | 1.48 (0.89) | 1.46 (0.94) | 1.70 (0.87) | 1.43 (0.86) | 75.87 (18.11) |
| 6 months to 1 year (n = 29) | 2.24 (1.46) | 1.45 (0.91) | 1.31 (0.60) | 2.07 (0.84) | 1.62 (1.08) | 73.62 (17.82) |
| 1‐5 years (n = 29) | 1.90 (1.05) | 1.41 (0.87) | 1.31 (0.60) | 1.55 (0.74) | 1.62 (0.94) | 77.93 (13.98) |
| Any others (n = 7) | 1.71 (1.50) | 1.14 (0.38) | 1.43 (0.79) | 1.57 (1.13) | 2.43 (1.81) | 73.57 (25.61) |
| Overall | 1.81 (1.09) | 1.44 (0.87) | 1.42 (0.90) | 1.69 (0.90) | 1.55 (0.95) | 73.78 (18.27) |
Note: HRQoL was assessed with EQ‐5D‐5L, higher scores indicate greater impact; VAS: lower scores indicate greater impact.
Abbreviations: AHHW, atypical hard‐to‐heal wounds; DFU, diabetic foot ulcers; HRQoL EQ‐5D, health‐related quality of life 5 domains; SD, standard deviation; VAS, visual analogue scale.
3.5. Factors associated with HRQoL outcomes
Factors associated with HRQoL by EQ‐5D‐5L domain and VAS‐score are presented in Table 5 as regression coefficients with 95% CIs. The coefficients quantify the size and the direction of the impact when other variables included in the model are controlled for. Age had a positive impact on HRQoL related to mobility (β = 0.008, P = .001), but a negative impact in relation to usual activities (β = −0.009, P = .001). Non‐Chinese ethnicity implied a negative impact on HRQoL in the domains of mobility (β = 0.25, P = .001), self‐care (β = 0.15, P = .046) and anxiety/depression (β = 0.18, P = .025) when other factors were controlled for. Mixed ulcers and AHHWs were the aetiologies that impacted HRQoL related to mobility the least, β = −0.41, P = .022 and β = −0.38, P = .021, respectively. A wound duration over 6 months had the greatest negative impact on HRQoL related to mobility (β = 0.19, P = .033), while a duration of 6 weeks to 3 months was most negatively impacted according to the VAS score (β = −0.105, P = .031). Wound size was shown to be non‐significant related to HRQoL independently of domain and VAS scores. Wound exudate, particularly low (β = 0.24, P = .044) to medium (β = 0.29, 0.018) levels, had a clear negative impact on HRQoL related to mobility.
TABLE 5.
Generalised linear regression analysis to explore factors associated with HRQoL (n = 233)
| Variables | Mobility | Self‐care | Usual activities | Pain/discomfort | Anxiety/depression | VAS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. (95%CI) | P‐value | Coef. (95%CI) | P‐value | Coef. (95%CI) | P‐value | Coef. (95%CI) | P‐value | Coef. (95%CI) | P‐value | Coef. (95%CI) | P‐value | |
| Age (years) | 0.008 (0.004, 0.012) | P < .001 | 0.002 (−0.003, 0.007) | .416 | −0.009 (−0.014, −0.004) | .001 | −0.002 (−0.006, 0.003) | .474 | −0.001 (−0.006, 0.004) | .604 | −0.002 (−0.004, <0.001) | .081 |
| Female (reference = male) | 0.07 (−0.08, 0.21) | .361 | −0.03 (−0.181, 0.12) | .694 | −0.09 (−0.235, 0.064) | .260 | −0.12 (−0.246, 0.016) | .086 | −0.002 (−0.151, 0.148) | .982 | 0.005 (−0.013, 0.123) | .110 |
| Other ethnic group (reference = Chinese) | 0.25 (0.11, 0.391) | .001 | 0.15 (0.03, 0.297) | .046 | −0.002 (−0.151, 0.147) | .979 | 0.08 (−0.05, 0.216) | .221 | 0.18 (0.023, 0.337) | .025 | −0.007 (−0.082, 0.067) | .847 |
| Wound aetiology (reference = others) | ||||||||||||
| Venous ulcer (n = 24) | −0.35 (−0.73, 0.04) | .077 | −0.17 (−0.516, 0.17) | .323 | −0.16 (−0.538, 0.211) | .393 | 0.01 (−0.288, 0.316) | .929 | −0.09 (−0.445, 0.266) | .623 | 0.03 (−0.118, 0.167) | .732 |
| Arterial ulcer (n = 13) | −0.17 (−0.57, 0.25) | .431 | 0.26 (−0.223, 0.714) | .304 | 0.12 (−0.383, 0.616) | .648 | 0.15 (−0.275, 0.581) | .484 | 0.10 (−0.317, 0.526) | .628 | −0.12 (−0.39, 0.143) | .363 |
| Mixed ulcer (n = 18) | −0.41 (−0.76, −0.06) | .022 | −0.08 (−0.46, 0.293) | .662 | −0.05 (−0.442, 0.345) | .811 | −0.13 (−0.442, 0.189) | .432 | −0.21 (−0.525, 0.096) | .175 | 0.05 (−0.058, 0.166) | .348 |
| DFU (n = 78) | −0.12 (−0.44, 0.21) | .480 | 0.004 (−0.304, 0.311) | .982 | −0.69 (−0.421, 0.283) | .700 | −0.20 (−0.445, 0.467) | .112 | 0.001 (−0.272, 0.274) | .994 | 0.04 (−0.056, 0.144) | .384 |
| AHHW (n = 80) | −0.38 (−0.69, −0.06) | .021 | −0.11 (−0.402, 0.182) | .459 | −0.17 (−0.516, 0.167) | .317 | −0.12 (−0.379, 0.132) | .344 | −0.03 (−0.310, 0.258) | .857 | 0.04 (−0.061, 0.140) | .441 |
| Wound duration (reference = 4‐6 weeks) | ||||||||||||
| 6 weeks to <3 months (n = 57) | 0.15 (−0.02, 0.33) | .085 | −0.16 (−0.362, 0.457) | .128 | −0.87 (−0.302, 0.129) | .430 | 0.02 (−0.174, 0.208) | .859 | −0.002 (0.206, 0.182) | .906 | −0.11 (−0.201, −0.009) | .031 |
| 3 months to <6 months (n = 46) | 0.05 (−0.13, 0.23) | .605 | −0.87 (−0.307, 0.133) | .438 | −0.05 (−0.281, 0.178) | .661 | −0.005 (−0.197, 0.186) | .958 | −0.07 (−0.280, 0.137) | .503 | 0.02 (−0.062, 0.101) | .643 |
| ≥6 months (n = 58) | 0.19 (0.02, 0.37) | .033 | −0.14 (−0.334, 0.503) | .148 | −0.15 (−0.337, 0.043) | .130 | 0.07 (−0.104, 0.234) | .453 | 0.11 (−0.070, 0.298) | .224 | 0.004 (−0.735, 0.082) | .913 |
| Wound size (reference = <2 sq.cm) | ||||||||||||
| 2‐5 sq.cm (n = 57) | 0.03 (−0.14, 0.20) | .711 | −0.004 (−0.188, 0.179) | .964 | −0.06 (−0.268, 0.143) | .549 | −0.09 (−0.257, 0.085) | .323 | 0.05 (−0.139, 0.247) | .583 | −0.007 (−0.115, 0.100) | .892 |
| 6‐10 sq.cm (n = 33) | 0.12 (−0.08, 0.32) | .247 | 0.06 (−0.191, 0.309) | .641 | 0.03 (−0.198, 0.261) | .787 | −0.10 (−0.295, 0.105) | .351 | −0.18 (−0.396, 0.041) | .111 | −0.05 (−0.116, 0.084) | .751 |
| >10 sq.cm (n = 27) | 0.03 (−0.18, 0.24) | .779 | 0.09 (−0.11, 0.282) | .388 | −0.09 (−0.309, 0.134) | .440 | 0.03 (−0.204, 0.259) | .815 | −0.02 (−0.258, 0.210) | .842 | 0.02 (−0.074, 0.120) | .642 |
| Wound exudate level (reference = none) | ||||||||||||
| Low (n = 123) | 0.24 (0.01, 0.47) | .044 | 0.17 (−0.033, 0.366) | .101 | −0.04 (−0.292, 0.207) | .737 | 0.22 (−0.067, 0.503) | .135 | 0.02 (−0.291, 0.336) | .886 | 0.03 (−0.067, 0.133) | .515 |
| Medium (n = 75) | 0.29 (0.05, 0.53) | .018 | 0.20 (−0.012, 0.419) | .065 | <0.001 (−0.263, 0.263) | .999 | 0.23 (−0.073, 0.529) | .137 | 0.13 (−0.191, 0.453) | .424 | 0.02 (−0.091, 0.130) | .728 |
| Heavy (n = 6) | 0.28 (−0.18, 0.73) | .235 | 0.29 (−0.222, 0.795) | .269 | −0.03 (−0.337, 0.434) | .895 | 0.13 (−0.334, 0.599) | .577 | 0.07 (−0.445, 0.590) | .784 | ‐0.05 (−0.253, 0.154) | .634 |
Abbreviations: AHHW, atypical hard‐to‐heal wounds; CI, Confidence interval; DFU, diabetic foot ulcers; HRQoL, health‐related quality of life; VAS, visual analogue scale.
4. DISCUSSION
The mean age 61.2 (SD: 4.6) of the patients with chronic wound in this study is similar to previous studies from Germany (65.3 years, SD: 14.8) 38 and Brazil (average 61.0 years). 39 However, it is lower than the reported age in an earlier study conducted in Singapore (median 74, IQR 63‐84), which obtained data from a nationwide administrative claims database including admissions from all levels of care to public and private acute care hospitals. 5 The lower age of the participants in our study compared to in the above‐mentioned Singaporean study may be because our study only recruited patients in primary care. Hence, participants in our study may be in better health states compared to patients with chronic wounds in hospitals and nursing homes.
Age was negatively associated with HRQoL related to usual activities (β = −0.009, P = .001). This finding is in alignment with a hospital setting study from Saudi Arabia, which reported that age affected HRQoL, particularly for physical functions in patients with DFUs. 40 The finding is also supported by a recent German study of chronic wound patients from three university hospitals and one foot care centre, which found a significant negative correlation between the total Wound‐QoL score and age in patients with arterial leg ulcers. 41 However, findings from a Swedish study from a specialist wound centre on patients with venous leg ulcers did not find a correlation between age and HRQoL 42 and neither did a mixed aetiologies chronic wound study from three outpatient settings and one hospital setting in Brazil. 39 A possible explanation for this could be attributed to variations in patients' mean age between the studies, where the present study has a relatively low mean age that possibly affected HRQoL less compared to a sample with a high mean age over 70 years, as HRQoL generally declines by age. The differences between the findings from the present study and the other studies may also be related to the use of various HRQoL instruments.
We also found that most participants in the present study were employed either full‐time, part‐time or self‐employed. This is rather unusual as patients with chronic wounds most frequently reported lower HRQoL in the domains related to physical functioning 13 and most patients with chronic wounds are retired. 44 , 45 This may indicate that chronic wound patients treated in primary care are younger compared to those in hospitals in Singapore. 5 , 33
The most common wound aetiologies in the present study were atypical hard‐to‐heal wounds and DFUs. This differs to other chronic wound studies from Singapore 5 , 33 and China, 45 which showed that pressure injuries were most prevalent. A plausible explanation for this could be that those studies reported the prevalence of wounds from inpatient settings, where patients may be bed bound to a higher extent, whereas this primary care setting study included patients that are ambulant and more independent. 5 , 33 , 45
Our results showed that the overall response pattern of HRQoL outcomes was similar across male and female participants. This finding is different from a recent study, which assessed HRQoL for patients with chronic wounds with Wound‐QoL tool and found that the overall QoL scores for male were higher than female. 41 However, the finding is in accordance with a study from China, which assessed HRQoL with SF‐36 tool and reported no difference in the overall responses to HRQoL outcomes between male and female participants. 44 This could possibly be attributed to cultural norms and beliefs which may contribute to differences in self‐reported health status, particularly in patients with chronic wound conditions. For the present study, response patterns for women and men were similar to the findings in the Chinese sample 44 but different from the German sample. 41 Further studies in a Singaporean context are needed to explore relatable aspects more comprehensively.
Arterial ulcers had the greatest impact on HRQoL related to four of five dimensions of health compared to other wound aetiologies. Furthermore, arterial ulcer also had the lowest VAS mean score 62.31 (SD: 28.3; range: 0‐100) indicating the greatest negative impact on HRQoL among all wound categories. This finding is consistent with another study where patients with arterial ulcers had the lowest quality of life when compared to other types of leg ulcers. 46 A study from Poland reported that patients with arterial ulcers had increased risk of sleep disturbances and pain. 47 A systematic review on quality of life in patients with arterial ulcers and DFU also concluded that patients with arterial ulcers suffered more from pain and restrictions related to their physical and social life compared to other chronic wounds. 48
The present study did not find that wound size was associated with HRQoL in any domain nor for the VAS score, even though wound size has been associated with HRQoL in previous studies for patients with venous leg ulcers 43 and other chronic wound aetiologies. 49 This could potentially be explained by the fact that most participants in the current study presented with rather small wound sizes (<2 cm2) compared to wounds in other studies. 43 , 49 The finding in the current study is consistent with other studies from Sweden 42 and Spain 50 including patients with large wound sizes that did not find any association between ulcer size and HRQoL.
This study found that a low to moderate level of wound exudate was negatively associated with HRQoL related to mobility, but not associated with any other domain or the VAS score. A previous study found that the quality (ie, characteristics and odour) of exudate rather than quantity (ie, amount) of exudate was associated with HRQoL in patients with chronic wounds. 49 A systematic review from year 2018 also reported that odour and exudate characteristics affected HRQoL negatively in patients with venous leg ulcers related to sleep, mobility and mood. 51
A wound duration longer than 6 months was negatively associated with HRQoL for the domain mobility, and the lowest VAS score was associated with a wound duration between 6 weeks and 3 months in the current study. These findings are different from a small Swedish study (n = 50), which did not find any associations between HRQoL and wound duration for primary care patients with venous leg ulcer. 42 However, wound duration has been associated with HRQoL in other primary care studies that assessed patients with chronic wounds in Brazil (n = 170) 49 and patients with venous leg ulcer in Canada (n = 424). 43 Given that the findings of the large studies 43 , 49 show that longer duration yielded lower HRQoL, a possible plausible explanation for the negative association between wound duration and HRQoL in the current study could be attributed to a positively overrated HRQoL by patients with chronic wounds longer than 6 months.
HRQoL related to mobility was impacted for patients with mixed ulcers and atypical hard‐to‐heal wounds. The findings from recent studies from primary care in Brazil 49 and a Spanish study found that the ‘physical symptoms and daily living’ and ‘domestic activities’ domain were the least affected domains in patients with chronic wound and venous leg ulcer. 50 A 2019 systematic review found that patients with chronic wounds most frequently reported lower HRQoL in the domains related to physical functioning. 13
Limitations for this study include that patients were recruited from non‐specialised wound clinics. Hence, some patients with wounds that may be less severe are more likely to be treated there rather than in specialised wound clinics, where more complicated wound patients may be treated. This could possibly reduce the generalisability of our findings. The study findings also showed that the majority of the patients with chronic wound reported ‘no problems’ indicating a better health state. A positively overrated HRQoL with more ‘no problem’ could be due to ceiling effects of the EQ‐5D‐5L instrument. This may influence the precision of calculating the true health state. Also, a generic and wound‐specific instrument could have been used for better sensitivity, but that would have disabled us to compare the findings to other patient groups.
This study assessed HRQoL and characteristics of chronic wounds in primary care patients in Singapore. The findings revealed that HRQoL was most impacted for patients suffering from arterial ulcers compared to other wound aetiologies. Patients with non‐Chinese ethnicity perceived greater impact on HRQoL compared to other ethnicities. The duration of the chronic wound and the level of exudate impact HRQoL related to mobility. The findings can be used to improve health care delivery for patients with chronic wound to optimise their HRQoL. This could, for example, be done by targeting areas in which patients experience the lowest HRQoL and provide treatments to alleviate problems related to that specific domain of health.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors contributed to and approved the final manuscript.
ACKNOWLEDGEMENTS
The authors would like to thank Lee Kong Chian School of Medicine, Nanyang Technological University Singapore and the A*STAR BMRC Strategic Positioning Fund for Skin Biology awarded to the Institute of Medical Biology for the research funding. The authors wish to express their gratitude to National Healthcare Group Polyclinic Nursing Services, Clinical Research Unit, and Heads and Nurse Managers of six clinics for their support. The authors wish to thank National Healthcare Group Polyclinic Wound Care Nurses for their assistance in wound data entry. The authors' heartfelt appreciation to all patients who participated in the survey and Dr Edward Tan who was the Project Manager at Centre for Population Health Sciences, Lee Kong Chian School of Medicine, and Nanyang Technological University Singapore for his support. The research is supported by the MOE Start‐Up Grant on Health Services Outcome Research awarded by the Lee Kong Chian School of Medicine, Nanyang Technological University, and the A*STAR BMRC Strategic Positioning Fund for Skin Biology awarded to the Institute of Medical Biology.
Zhu X, Olsson MM, Bajpai R, Järbrink K, Tang WE, Car J. Health‐related quality of life and chronic wound characteristics among patients with chronic wounds treated in primary care: A cross‐sectional study in Singapore. Int Wound J. 2022;19(5):1121-1132. doi: 10.1111/iwj.13708
Funding information The research is supported by the MOE Start‐Up Grant on Health Services Outcome Research awarded by the Lee Kong Chian School of Medicine, Nanyang Technological University and the A*STAR BMRC Strategic Positioning Fund for Skin Biology awarded to the Institute of Medical Biology; Institute of Medical Biology, Grant/Award Number: A*STAR BMRC Strategic Positioning Fund for Skin Biology; Lee Kong Chian School of Medicine, Nanyang Technological University, Grant/Award Number: MOE Start‐Up Grant on Health Services Outcome Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Atkin L, Bućko Z, Montero EC, et al. Implementing TIMERS: the race against hard‐to‐heal wounds. J Wound Care. 2019;23:S1‐S52. [DOI] [PubMed] [Google Scholar]
- 2. Kyaw B, Järbrink K, Martinengo L, Car J, Harding K, Schmidtchen A. Need for improved definition of “chronic wounds” in clinical studies. Acta Derm Venereol. 2018;98(1):157‐158. doi: 10.2340/00015555-2786 [DOI] [PubMed] [Google Scholar]
- 3. Sen CK, Roy S, Gordillo GM. Wound Healing (Neligan Plastic Surgery: Volume One). Amsterdam, The Netherlands: Elsevier; 2017. [Google Scholar]
- 4. Martinengo L, Olsson M, Bajpai R, et al. Prevalence of chronic wounds in the general population: systematic review and meta‐analysis of observational studies. Ann Epidemiol. 2019;29:8‐15. [DOI] [PubMed] [Google Scholar]
- 5. Goh OQ, Ganesan G, Graves N, Ng YZ, Harding K, Tan KB. Incidence of chronic wounds in Singapore, a multiethnic Asian country, between 2000 and 2017: a retrospective cohort study using a nationwide claims database. BMJ Open. 2020;10(9):e039411. doi: 10.1136/bmjopen-2020-039411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dissemond J, Bültemann A, Gerber V, Jäger B, Kröger K, Münter C. Diagnosis and treatment of chronic wounds: current standards of Germany's initiative for chronic wounds e. V. J Wound Care. 2017;26(12):727‐732. doi: 10.12968/jowc.2017.26.12.727 [DOI] [PubMed] [Google Scholar]
- 7. Janowska A, Dini V, Oranges T, Iannone M, Loggini B, Romanelli M. Atypical ulcers: diagnosis and management. Clin Interv Aging. 2019;14:2137‐2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Isoherranen K, O'Brien JJ, Barker J, et al. EWMA document: atypical wounds. Best clinical practice and challenges. J Wound Care. 2019;28(6):S1‐S92. [DOI] [PubMed] [Google Scholar]
- 9. Eming SA, Martin P, Tomic‐Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6:265sr6‐265sr6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lim HW, Collins SAB, Resneck JS, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76(5):958‐972.e2. [DOI] [PubMed] [Google Scholar]
- 11. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367‐2375. [DOI] [PubMed] [Google Scholar]
- 12. Nelson EA. Venous leg ulcers. BMJ Clin Evid. 2011;12:1‐73. [PMC free article] [PubMed] [Google Scholar]
- 13. Olsson M, Järbrink K, Divakar U, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 2019;27:114‐125. [DOI] [PubMed] [Google Scholar]
- 14. Torres SM d SS d O, Araújo R d O e, IKF C, et al. Health‐related quality of life in patients with venous leg ulcer treated in primary care in Brazil and Portugal. PLoS One. 2018;13(4):e0195990. doi: 10.1371/journal.pone.0195990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Finlayson K, Miaskowski C, Alexander K, et al. Distinct wound healing and quality‐of‐life outcomes in subgroups of patients with venous leg ulcers with different symptom cluster experiences. J Pain Symptom Manag. 2017;53:871‐879. doi: 10.1016/j.jpainsymman.2016.12.336 [DOI] [PubMed] [Google Scholar]
- 16. Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care. 2015;4(9):560‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Phillips CJ, Humphreys I, Fletcher J, Harding K, Chamberlain G, Macey S. Estimating the costs associated with the management of patients with chronic wounds using linked routine data. Int Wound J. 2016;13(6):1193‐1197. doi: 10.1111/iwj.12443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kerr M, Barron E, Chadwick P, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995‐1002. doi: 10.1111/dme.13973 [DOI] [PubMed] [Google Scholar]
- 19. Rabin R, De Charro F. EQ‐5D: a measure of health status from the EuroQol group. Ann Med. 2001;33:337‐343. doi: 10.3109/07853890109002087 [DOI] [PubMed] [Google Scholar]
- 20. Price PE, Krasner DL. Health‐related quality of life and chronic wounds: evidence and implications for practice. In: Price PE, Krasner DL, eds. Chronic Wound Care: A Clinical Source Book for Healthcare Professionals. 5th ed. Malvern, PA: HMP Communications; 2012. https://www.researchgate.net/publication/230560341_Health‐Related_Quality_of_Life_and_Chronic_Wounds_Evidence_and_Implications_for_Practice [Google Scholar]
- 21. Wukich DK, Raspovic KM. Assessing health‐related quality of life in patients with diabetic foot disease: why is it important and how can we improve? The 2017 Roger E Pecoraro award lecture. Diabetes Care. 2017;41:397. doi: 10.2337/dci17-0029 [DOI] [PubMed] [Google Scholar]
- 22. Rutherford C, Brown JM, Smith I, et al. A patient‐reported pressure ulcer health‐related quality of life instrument for use in prevention trials (PU‐QOL‐P): psychometric evaluation. Health Qual Life Outcomes. 2018;16(1):1‐11. doi: 10.1186/s12955-018-1049-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Erfurt‐Berge C, Renner R. Quality of life in patients with chronic wounds. Dermatologist. 2020;71:863‐869. [DOI] [PubMed] [Google Scholar]
- 24. Higginson IJ, Carr AJ. Measuring quality of life using quality of life measures in the clinical setting. BMJ. 2001;322:1297‐1300. doi: 10.1136/bmj.322.7297.1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Renner R, Erfurt‐Berge C. Depression and quality of life in patients with chronic wounds: ways to measure their influence and their effect on daily life. Chronic Wound Care Manag Res. 2017;4:143‐151. doi: 10.2147/CWCMR.S124917 [DOI] [Google Scholar]
- 26. Guyatt GH, Feeny DH, Patrick DL. Measuring health‐related quality of life. Ann Intern Med. 1993;118:622‐629. [DOI] [PubMed] [Google Scholar]
- 27. Hogg FRA, Peach G, Price P, Thompson MM, Hinchliffe RJ. Measures of health‐related quality of life in diabetes‐related foot disease: a systematic review. Diabetologia. 2012;55:552‐565. doi: 10.1007/s00125-011-2372-5 [DOI] [PubMed] [Google Scholar]
- 28. Price P, Harding K. Cardiff wound impact schedule: the development of a condition‐specific questionnaire to assess health‐related quality of life in patients with chronic wounds of the lower limb. Int Wound J. 2004;1(1):10‐17. doi: 10.1111/j.1742-481x.2004.00007.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Spech E Lebensqualität bei Patienten mit chronisch venösen und arteriellen Ulcera cruris [dissertation]. Würzburg. 2003. https://d-nb.info/969451946/34
- 30. Augustin M, Herberger K, Rustenbach SJ, Schäfer I, Zschocke I, Blome C. Quality of life evaluation in wounds: validation of the Freiburg life quality assessment‐wound module, a disease‐specific instrument. Int Wound J. 2010;7(6):493‐501. doi: 10.1111/j.1742-481X.2010.00732.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mo F, Choi BCK, Li FCK, Merrick J. Using health utility index (HUI) for measuring the impact on health‐related quality of life (HRQL) among individuals with chronic diseases. Sci World J. 2004;4:746‐757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen TH, Li L, Kochen MM. A systematic review: how to choose appropriate health‐related quality of life (HRQOL) measures in routine general practice? J Zhejiang Univ Sci B. 2005;6:936‐940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lo ZJ, Lim X, Eng D, et al. Clinical and economic burden of wound care in the tropics: a 5‐year institutional population health review. Int Wound J. 2020;17(3):790‐803. doi: 10.1111/iwj.13333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chisholm D, Knapp MRJ, Knudsen HC, Amaddeo A, Gaite L, Van Wijngaarden B. Client socio‐demographic and service receipt inventory ‐ European version: development of an instrument for international research. EPSILON study 5. Br J Psychiatry. 2000;177(SUPPL. 39):s28‐s33. doi: 10.1192/bjp.177.39.s28 [DOI] [PubMed] [Google Scholar]
- 35. EuroQol Research Foundation . EQ‐5D User Guides – EQ‐5D. 2020. https://euroqol.org/publications/user-guides/
- 36. Falanga V. Classifications for wound bed preparation and stimulation of chronic wounds. Wound Repair Regen. 2000;8(5):347‐352. doi: 10.1111/j.1524-475X.2000.00347.x [DOI] [PubMed] [Google Scholar]
- 37. Hardin JW, Hilbe JW. Generalized linear models and extensions. 3rd ed. StataCorp LP: Stata Press Books; 2012. https://ideas.repec.org/b/tsj/spbook/glmext.html [Google Scholar]
- 38. Blome C, Baade K, Sebastian Debus E, Price P, Augustin M. The “wound‐QoL”: a short questionnaire measuring quality of life in patients with chronic wounds based on three established disease‐specific instruments. Wound Repair Regen. 2014;22(4):504‐514. doi: 10.1111/wrr.12193 [DOI] [PubMed] [Google Scholar]
- 39. Naiara Vogt T, Koller FJ, Dias Santos PN, et al. Quality of life assessment in chronic wound patients using the wound‐QoL and FLQA‐Wk instruments. Investig Educ Enferm. 2020;38(3):1‐12. doi: 10.17533/UDEA.IEE.V38N3E11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Al Ayed M, Ababneh M, Alwin Robert A, et al. Factors associated with health‐related quality of life in patients with diabetic foot ulcer: a cross‐sectional study from Saudi Arabia. Cureus. 2020;12(6):1‐14. doi: 10.7759/cureus.8658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reinboldt‐Jockenhöfer F, Babadagi Z, Hoppe H, et al. Association of wound genesis on varying aspects of health‐related quality of life in patients with different types of chronic wounds: results of a cross‐sectional multicentre study. Int Wound J. 2021;18:432‐439. doi: 10.1111/iwj.13543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Öien RF, Åkesson N, Forssell H. Assessing quality of life in patients with hard‐to‐heal ulcers using the EQ‐5D questionnaire. J Wound Care. 2013;22(8):442‐447. doi: 10.12968/jowc.2013.22.8.442 [DOI] [PubMed] [Google Scholar]
- 43. Hopman WM, Vandenkerkhof EG, Carley ME, Kuhnke JL, Harrison MB. Factors associated with health‐related quality of life in chronic leg ulceration. Qual Life Res. 2014;23(6):1833‐1840. doi: 10.1007/s11136-014-0626-7 [DOI] [PubMed] [Google Scholar]
- 44. Yan R, Yu F, Strandlund K, Han J, Lei N, Song Y. Analyzing factors affecting quality of life in patients hospitalized with chronic wound. Wound Repair Regen. 2020;29(1):70‐78. doi: 10.1111/wrr.12870 [DOI] [PubMed] [Google Scholar]
- 45. Jiang Q, Dumville JC, Cullum N, Pan J, Liu Z. Epidemiology and disease burden of complex wounds for inpatients in China: an observational study from Sichuan province. BMJ Open. 2020;10:e039894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Szewczyk MT, Mos¨cicka P, Jawień A, et al. Quality of life in patients with leg ulcers or skin lesions ‐ a pilot study. Postep Dermatologii i Alergol. 2015;32(6):465‐469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hellström A, Nilsson C, Nilsson A, et al. Leg ulcers in older people: a national study addressing variation in diagnosis, pain and sleep disturbance. BMC Geriatr. 2016;16(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Herber OR, Schnepp W, Rieger MA, et al. A systematic review on the impact of leg ulceration on patients' quality of life. Health Qual Life Outcomes. 2007;5(1):44. doi: 10.1186/1477-7525-5-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. De Oliveira AC, De Macêdo RD, Bezerra SMG, Andrade EMLR, Dos Santos AMR, Nogueira LT. Quality of life of people with chronic wounds. ACTA Paul Enferm. 2019;32(2):194‐201. doi: 10.1590/1982-0194201900027 [DOI] [Google Scholar]
- 50. González de la Torre H, Quintana‐Lorenzo ML, Perdomo‐Pérez E, Verdú J. Correlation between health‐related quality of life and venous leg ulcer's severity and characteristics: a cross‐sectional study. Int Wound J. 2017;14(2):360‐368. doi: 10.1111/iwj.12610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Phillips P, Lumley E, Duncan R, et al. A systematic review of qualitative research into people's experiences of living with venous leg ulcers. J Adv Nurs. 2018;74:550‐563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


