Abstract
Background
In Benin, access to water, sanitation and hygiene (WASH) remains an issue. This study aims to provide an overview of household access to basic WASH services based on nationally representative data.
Method
Secondary analyses were run using the ‘HOUSEHOLD’ dataset of the fifth Demographic and Health Survey 2017–2018. The dependent variables were household access to individual and combined basic WASH services. The characteristics of the household head and those related to the composition, wealth and environment of the household were independent variables. After a descriptive analysis of all study variables, multivariate logistic regression was performed to identify predictors of outcome variables.
Results
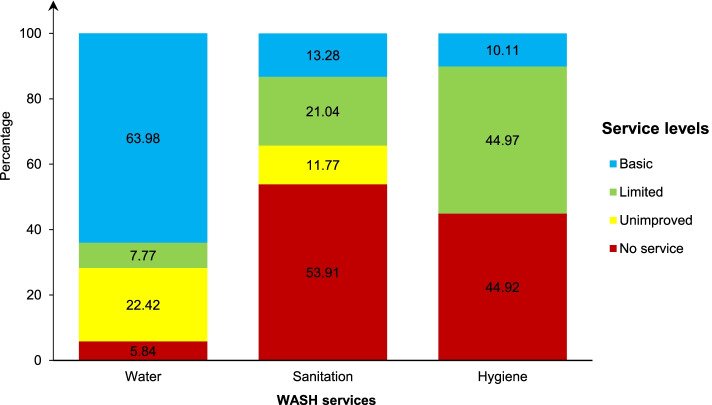
The study included 14,156 households. Of these, 63.98% (95% CI = 61.63–66.26), 13.28% (95% CI = 12.10–14.57) and 10.11% (95% CI = 9.19–11.11) had access to individual basic water, sanitation and hygiene facilities, respectively. Also, 3% (95% CI = 2.53–3.56) of households had access to combined basic WASH services. Overall, the richest households and few, and those headed by people aged 30 and over, female and with higher levels of education, were the most likely to have access to individual and combined basic WASH services. In addition, disparities based on the department of residence were observed.
Conclusion
The authors suggest a multifactorial approach that addresses the identified determinants.
Keywords: Determinant, Logistic regression, Household, Access, Water, Sanitation, Hygiene, Map, National data, Benin
Background
In 2010, the United Nations General Assembly (UNGA) recognised the right to drinking water and sanitation as a human right and called on states to intensify efforts to provide safe, clean, accessible and affordable drinking water and sanitation for all [1]. Also, in 2015, the Member States of the United Nations adopted the 2030 Agenda for Sustainable Development, Goal 6 of which aims to “ensure availability and sustainable management of water and sanitation for all” [2].
In 2020, 489 million people worldwide still lacked access to improved drinking water facilities—water points that can deliver safe water because of their design and construction—including 122 million people using surface water (river, dam, lake, pond, stream, canal or irrigation canal) for drinking water [3, 4]. People's access to improved sanitation facilities—facilities designed to hygienically separate excreta from human contact—increased over 2000–2020 [3, 4]. However, in 2020, 494 million people were still practising open defecation [3]. In addition, 670 million people do not have handwashing facilities with soap and water [3]. Evidence shows that contaminated water and poor sanitation are associated with the transmission of diseases and other symptoms such as cholera, bacillary diarrhoea, viral hepatitis A, typhoid, polio and acute respiratory infections, etc. [5–11]. According to the World Health Organization (WHO), inadequate access to Water, Sanitation and Hygiene (WASH) services is responsible for nearly 2 million deaths annually worldwide, most of them children [11]. Sub-Saharan Africa still has the largest burden of morbidity and mortality due to inadequate WASH facilities (60% and 53% of all DALYs and deaths attributable to inadequate WASH facilities, respectively) [11].
In Benin, access to appropriate WASH facilities remains an issue. In its Health Development Plan (PNDS, Plan National de Développement Sanitaire in French) 2018–2022, Benin defined the promotion of hygiene and basic sanitation as a key action to prevent and fight diseases [12]. Therefore, Objective 6 of the National Development Plan (PND) 2018–2025, which guides the government's actions, aims “to guarantee access for all to water supply and sanitation services” [13]. In addition, in 2018, Benin adopted the National Strategy for the Promotion of Hygiene and Basic Sanitation (SNPHAB, Stratégie Nationale de Promotion de l’Hygiène et de l’Assainissement de Base in French) in rural areas [14]. This 12-year strategy (2018–2030) aims to “ensure equitable access to adequate sanitation and hygiene services for the rural population of Benin” [14]. Furthermore, like several other low-income countries, Benin benefits from the technical and financial assistance of several partners to improve people's access to WASH services. In particular, the United Nations International Children's Fund (UNICEF) is implementing the Community-Led Total Sanitation (CLTS) approach, which aims to support and encourage communities to take collective action to improve their hygiene and sanitation practices [15–17]. However, the high morbidity and mortality indicators for waterborne diseases show that there are still significant gaps in people's access to appropriate WASH services. In Benin, 13,390 (14%) deaths and 1,028,459 (15%) DALYs are attributable to inadequate WASH facilities in 2016 [18]. Also, ten children continue to die every day, 90% of these deaths being because of the ingestion of contaminated water and the lack of community sanitation facilities [16]. Specifically, the prevalence of diarrhoeal diseases was 11%, with a case fatality rate of 16 deaths per 10,000 children [19, 20].
Consequently, efforts to improve access to appropriate WASH services are required. For these interventions to be successful, the surveillance of progress in coverage of WASH services needs to be enhanced, and the inequalities that determine household access to these facilities need to be better understood. According to studies in Africa and Asia, the factors associated with household access to improved or basic WASH services were the characteristics of the household head and the composition, wealth and environment of the household [21–31]. So far, in Benin, there is scarce information on disparities in people's access to WASH facilities. One relevant study highlighted socio-demographic and environmental factors but was limited to a specific geographical area (the commune of Lalo) [32]. However, the national coverage of WASH services is regularly monitored every five years through the Demographic and Health Surveys (DHS). To date, Benin has conducted five DHS. The results of the Fourth Demographic and Health Survey (DHS-IV) showed that despite progress in terms of household access to improved drinking water sources, the use of water from unprotected wells is still widespread (15%), with 3.6% of households using surface water for drinking water [33]. In addition, nearly two-thirds of households (66.4%) had access to unimproved toilets, and 54.2% did not have any sanitation facilities [33]. Also, 43% of households did not have a handwashing facility [33].
In 2017–2018, the Fifth Demographic and Health Survey (DHS-V) took place and provided data on the coverage of households with WASH facilities. Thus, the present work aims to study household access to WASH facilities based on nationally representative data of the Beninese population collected during the DHS-V.
Methods
Study area
Benin is a West African state covering an area of 114,763 km2 with an urbanization rate of 44% [34]. The Fourth General Census of Population and Housing (Recensement Général de la Population et de l'Habitation in French, RGPH-IV) in 2013 counted 10,008,749 inhabitants, 51.2% of whom were women [35]. According to estimates, the population growth is about + 2.7% per year [34]. The 2019 projections put the population in Benin at 11,884,127 (5,846,550 men and 6,037,577 women) [34]. Administratively, Benin has 12 departments divided into 77 communes.
Study design and data source
This study used a cross-sectional design and consisted of a secondary analysis of data obtained from the DHS-V. The DHS surveys are a standard series of surveys (DHS-I in 1996, DHS-II in 2001, DHS-III in 2006, DHS-IV in 2011–2012 and DHS-V in 2017–2018) at the national level that provide up-to-date estimates of basic demographic and health indicators. The DHS-V was conducted by the National Institute of Statistics and Demography (INStaD, Institut National de la Statistique et de la Démographie in French) in collaboration with the Ministry of Health and with technical support from ICF through the DHS Program of the United States Agency for International Development (USAID). Details on the DHS Program are described elsewhere [36]. In this study, the unit of analysis was households. Following a request sent via the DHS Program website—https://dhsprogram.com/—DHS-V ‘HOUSEHOLD’ dataset (BJHR71DT) was downloaded.
Sampling procedure and sample size
The DHS-V employed a nationally representative sample of the Beninese population using a two-stage stratified sampling procedure. The twelve departments were stratified into urban and rural areas, except for Littoral, an entirely urban stratum. This stratification resulted in 23 strata. In each stratum, a specific number of Primary Sample Units (PSUs) were systematically selected (in the first stage) with Probability Proportional to the Size (PPS). The list of Enumeration Areas (EAs) established during the RGPH-IV served as the sampling frame for this selection. After listing the households within the selected EAs, a systematic sample of 26 households was drawn from each PSU (in the second stage). Details on the survey sampling procedure and data collection methods are described elsewhere [37]. Of the 14,435 households selected, 14,293 were identified during the survey [37]. Of these, 14,156 (response rate = 99%) were successfully surveyed [37].
Study variables
Dependent variables
The dependent variables were household access to basic WASH services. By the WHO/UNICEF Joint Monitoring Programme (JMP) guidelines, household access to a source of drinking water, sanitation, and hygiene could be grouped according to the level of service provided: “basic”, “limited”, “unimproved” and “no service” (Tables 1 and 2) [4]. A dichotomisation was performed to obtain the dependent variables: yes = 1 when the service level was basic, and no = 0 otherwise (individual basic WASH services). Finally, a last binary dependent variable was generated for the households that combined all three basic facilities (combined basic WASH services).
Table 1.
WHO/UNICEF Joint Monitoring Programme (JMP) ladder for water, sanitation and hygiene (WASH) services
| Service level | Water | Sanitation | Hygiene |
|---|---|---|---|
| Basic | Drinking water from an improved source, provided collection time is not more than 30 min for a round trip, including queuing | Use of improved facilities that are not shared with other households | Availability of a handwashing facility on premises with soap and water |
| Limited | Drinking water from an improved source for which collection time exceeds 30 min for a round trip, including queuing | Use of improved facilities shared between two or more households | Availability of a handwashing facility on premises without soap and water |
| Unimproved | Drinking water from an unprotected dug well or unprotected spring | Use of pit latrines without a slab or platform, hanging latrines or bucket latrines | Not applicable |
| No service | Surface water | Open defecation | No handwashing facility on premises |
Source Adapted from WHO; UNICEF. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines; WHO: Geneva, 2017; ISBN 978–92-4–151,289-3. [4]
Table 2.
JMP classification of improved/unimproved water and sanitation facility types
| Facility types | Water | Sanitation |
|---|---|---|
| Improved facilities |
Piped supplies • Tap water in the dwelling, yard or plot • Public standposts Non-piped supplies • Boreholes/tubewells • Protected wells and springs • Rainwater • Packaged water, including bottled water and sachet water • Delivered water, including tanker trucks and small carts |
Networked sanitation • Flush and pour flush toilets connected to sewers On-site sanitation • Flush and pour flush toilets or latrines connected to septic tanks or pits • Ventilated improved pit latrines • Pit latrines with slabs • Composting toilets, including twin pit latrines and container-based systems |
| Unimproved facilities |
Non-piped supplies • Unprotected wells and springs |
On-site sanitation • Pit latrines without slabs • Hanging latrines • Bucket latrines |
Source Adapted from WHO; UNICEF. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines; WHO: Geneva, 2017; ISBN 978–92-4–151,289-3. [4]
Covariates
The independent variables were:
the variables related to the household head: age (< 30, 30–39, 40–49, 50–59, ≥ 60), sex (male, female), level of education (no formal education, primary, secondary, higher) and marital status (single, in couple);
the variables related to household's composition and wealth: household size (≤ 5, > 5), children aged five and under in the household (yes, no) and wealth index (poorest, poorer, middle, richer, richest);
the variables related to the household's environment of residence: area (urban, rural) and department (Alibori, Atacora, Atlantic, Borgou, Collines, Couffo, Donga, Littoral, Mono, Ouémé, Plateau and Zou).
These variables were chosen from a literature review [22, 23, 25, 27, 28, 30].
Data analysis
All analyses included the sample weight. The independent and dependent variables were described by calculating the numbers and percentages of their categories. Also, the spatial distribution of household access to individual and combined basic WASH facilities was described using QGIS 2.18. Chi-square tests were performed to determine the association between the independent and dependent variables. Multivariate logistic regressions were performed to identify predictors of access to individual and combined basic WASH facilities. Potential factors were selected at p < 0.20 using simple logistic regression [38]. They were then entered into a multivariate logistic regression using a backward stepwise strategy to obtain adjusted estimates. For each regression, the indicators used to measure the association between the dependent and independent variables were the odds ratio (OR) and the 95% CI. The significance level was 5%. All statistical analyses were conducted in Stata 15 (StataCorp, College Station, TX, USA).
Ethical approval
All methods were performed by the principles of the Declaration of Helsinki. Firstly, the launch of the DHS-V data collection was conditional on the authorisation of the National Statistical Council (Conseil National de la Statistique in French, CNS) to obtain the statistical visa of opportunity and conformity, and on the approval of the National Committee on Health Research Ethics (Comité National d’Ethique pour la Recherche en Santé in French, CNERS) to get the binding scientific and ethical opinion of the survey [37]. These two institutions reviewed and approved the methodological and financial documents and the collection tools [37]. Then, during data collection, the informed consent of eligible respondents was sought before starting the interviews. Finally, the dataset used for the secondary analyses in this study was fully anonymised so that the individuals surveyed could not be identified in any way [37].
Results
Basic characteristics of households
The study included 14,156 households. Table 3 presents the basic characteristics of the surveyed households. The majority of household heads were 30–39 years old (26.91%), male (75.12%), and in a couple (77.62%). More than half (53,35%) of the household heads had no formal education. The poorest wealth quintile comprises about 17.67% of the sample compared to 22.82% for the richest quintile. In addition, 61.66% of households had five or fewer members. Children aged five and under were present in 60.45% of households. About 57% of the households lived in rural areas. As regards department of residence, households in Atlantique (13.91%), Ouémé (11.53%) and Borgou (10.58%) were the most represented.
Table 3.
Basic characteristics of the households in Benin, 2017–2018
| Variables | n | % |
|---|---|---|
| Age (years) | ||
| < 30 | 2,454 | 17.34 |
| 30–39 | 3,810 | 26.91 |
| 40–49 | 2,970 | 20.98 |
| 50–59 | 2,146 | 15.16 |
| ≥ 60 | 2,775 | 19.60 |
| Sex | ||
| Male | 10,634 | 75.12 |
| Female | 3,522 | 24.88 |
| Level of education | ||
| No formal education | 7,553 | 53.35 |
| Primary | 3,232 | 22.83 |
| Secondary | 2,593 | 18.32 |
| Higher | 778 | 5.50 |
| Marital status | ||
| Single | 3,169 | 22.38 |
| In couple | 10,987 | 77.62 |
| Wealth index | ||
| Poorest | 2,501 | 17.67 |
| Poorer | 2,675 | 18.89 |
| Middle | 2,798 | 19.77 |
| Richer | 2,951 | 20.85 |
| Richest | 3,231 | 22.82 |
| Household size | ||
| ≤ 5 | 8,728 | 61.66 |
| > 5 | 5,428 | 38.34 |
| Children aged 5 and under in the household | ||
| No | 5,598 | 39.55 |
| Yes | 8,558 | 60.45 |
| Area | ||
| Urban | 6,104 | 43.12 |
| Rural | 8,052 | 56.88 |
| Department | ||
| Alibori | 1,192 | 8.42 |
| Atacora | 923 | 6.52 |
| Atlantique | 1,969 | 13.91 |
| Borgou | 1,498 | 10.58 |
| Collines | 981 | 6.93 |
| Couffo | 1,108 | 7.83 |
| Donga | 740 | 5.23 |
| Littoral | 852 | 6.02 |
| Mono | 879 | 6.21 |
| Ouémé | 1,633 | 11.53 |
| Plateau | 984 | 6.95 |
| Zou | 1,399 | 9.88 |
Household access to WASH services
Figure 1 shows the level of household access to WASH services.
Fig. 1.
Level of household access to water, sanitation and hygiene (WASH) services in Benin, 2017–2018
Water
About 64% (95% CI = 61.63–66.26) of households had access to basic drinking water services versus 5.84% (95% CI = 4.70–7.23) using surface water for drinking.
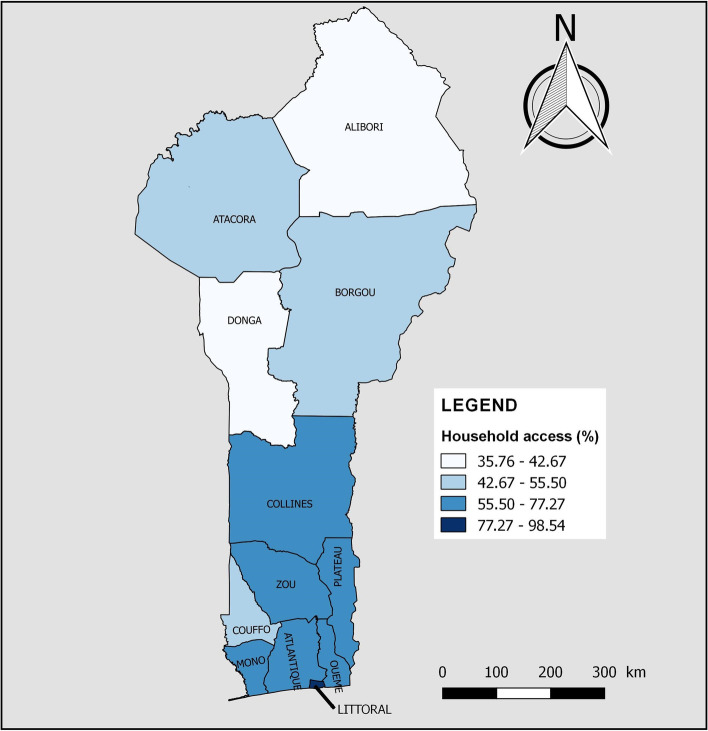
Table 4 analyses the association between independent variables and household access to individual and combined basic WASH services. Household access to basic drinking water services varied significantly with the age of the household head (p = 0.002). It increased significantly with the level of education of the household head (p < 0.001) and with the wealth index (p < 0.001). Furthermore, it was significantly higher in households where the head was female (68.22% vs 62.57%, p < 0.001) or single (66.20% vs 63.34%, p = 0.018). The pattern was similar for households with five or fewer people (67.78% vs 57.86%, p < 0.001) or without children aged 5 and under (67.62% vs 61.60%, p < 0.001). On the other hand, the proportion of households using basic drinking water services was significantly lower in rural areas than in urban areas (73.30% vs 56.91%, p < 0.001). Figure 2 shows household access to basic drinking water services by department of residence. There was a decrease in household coverage of basic drinking water services moving towards the northern departments. Littoral (98.54%), Ouémé (77.27%), Zou (72.14%), Atlantique (70.36%) and Plateau (70.11%) had the highest coverage compared to Atacora (50.78%), Donga (42.67%) and Alibori (35.76%) which had the lowest.
Table 4.
Association between independent variables and household access to individual and combined basic WASH services in Benin, 2017–2018
| Variables | Water | Sanitation | Hygiene | Combined WASH | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | Yes | No | p | Yes | No | p | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |||||
| Age (years) | 0.002 | < 0.001 | 0.225 | 0.001 | ||||||||||||||||
| < 30 | 1,562 | 63.63 | 893 | 36.37 | 220 | 8.95 | 2,235 | 91.05 | 238 | 9.72 | 2,216 | 90.28 | 44 | 1.78 | 2,411 | 98.22 | ||||
| 30–39 | 2,507 | 65.80 | 1,303 | 34.20 | 462 | 12.12 | 3,348 | 87.88 | 380 | 9.98 | 3,430 | 90.02 | 101 | 2.65 | 3,709 | 97.35 | ||||
| 40–49 | 1,924 | 64.79 | 1,046 | 35.21 | 451 | 15.19 | 2,519 | 84.81 | 324 | 10.92 | 2,645 | 89.08 | 107 | 3.59 | 2,863 | 96.41 | ||||
| 50–59 | 1,389 | 64.70 | 758 | 35.30 | 356 | 16.60 | 1,790 | 83.40 | 234 | 10.92 | 1,912 | 89.08 | 86 | 4.03 | 2,060 | 95.97 | ||||
| ≥ 60 | 1,675 | 60.36 | 1,100 | 39.64 | 392 | 14.11 | 2,384 | 85.89 | 254 | 9.14 | 2,522 | 90.86 | 87 | 3.14 | 2,688 | 96.86 | ||||
| Sex | < 0.001 | 0.135 | 0.555 | 0.081 | ||||||||||||||||
| Male | 6,654 | 62.57 | 3,980 | 37.43 | 1,383 | 13.01 | 9,251 | 86.99 | 1,085 | 10.21 | 9,548 | 89.79 | 336 | 3.16 | 10,298 | 96.84 | ||||
| Female | 2,403 | 68.22 | 1,119 | 31.78 | 497 | 14.12 | 3,025 | 85.88 | 346 | 9.81 | 3,177 | 90.19 | 89 | 2.51 | 3,434 | 97.49 | ||||
| Level of education | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||||
| No formal education | 4,319 | 57.18 | 3,234 | 42.82 | 492 | 6.52 | 7,060 | 93.48 | 469 | 6.21 | 7,084 | 93.79 | 43 | 0.57 | 7,510 | 99.43 | ||||
| Primary | 2,164 | 66.97 | 1,067 | 33.03 | 427 | 13.21 | 2,805 | 86.79 | 303 | 9.39 | 2,929 | 90.61 | 55 | 1.71 | 3,177 | 98.29 | ||||
| Secondary | 1,899 | 73.23 | 694 | 26.77 | 587 | 22.64 | 2,006 | 77.36 | 401 | 15.44 | 2,193 | 84.56 | 145 | 5.57 | 2,449 | 94.43 | ||||
| Higher | 674 | 86.68 | 104 | 13.32 | 374 | 48.09 | 404 | 51.91 | 258 | 33.18 | 520 | 66.82 | 182 | 23.36 | 596 | 76.64 | ||||
| Marital status | 0.018 | 0.784 | 0.550 | 0.948 | ||||||||||||||||
| Single | 2,098 | 66.20 | 1,071 | 33.80 | 426 | 13.45 | 2,743 | 86.55 | 330 | 10.40 | 2,839 | 89.60 | 94 | 2.98 | 3,074 | 97.02 | ||||
| In couple | 6,959 | 63.34 | 4,028 | 36.66 | 1,454 | 13.23 | 9,533 | 86.77 | 1,101 | 10.02 | 9,886 | 89.98 | 330 | 3.01 | 10,657 | 96.99 | ||||
| Wealth index | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||||
| Poorest | 1,034 | 41.32 | 1,468 | 58.68 | 3 | 0.10 | 2,499 | 99.90 | 96 | 3.82 | 2,406 | 96.18 | 0 | 0.00 | 2,501 | 100.00 | ||||
| Poorer | 1,412 | 52.78 | 1,263 | 47.22 | 23 | 0.85 | 2,652 | 99.15 | 146 | 5.47 | 2,528 | 94.53 | 1 | 0.02 | 2,674 | 99.98 | ||||
| Middle | 1,653 | 59.06 | 1,145 | 40.94 | 72 | 2.57 | 2,726 | 97.43 | 179 | 6.41 | 2,619 | 93.59 | 0 | 0.00 | 2,798 | 100.00 | ||||
| Richer | 2,086 | 70.68 | 865 | 29.32 | 412 | 13.96 | 2,539 | 86.04 | 255 | 8.63 | 2,696 | 91.37 | 18 | 0.60 | 2,933 | 99.40 | ||||
| Richest | 2,873 | 88.93 | 358 | 11.07 | 1,371 | 42.43 | 1,860 | 57.57 | 755 | 23.37 | 2,476 | 76.63 | 406 | 12.58 | 2,825 | 87.42 | ||||
| Household size | < 0.001 | 0.330 | 0.033 | 0.003 | ||||||||||||||||
| ≤ 5 | 5,916 | 67.78 | 2,812 | 32.22 | 1,184 | 13.56 | 7,544 | 86.44 | 923 | 10.58 | 7,805 | 89.42 | 297 | 3.40 | 8,431 | 96.60 | ||||
| > 5 | 3,141 | 57.86 | 2,287 | 42.14 | 697 | 12.83 | 4,731 | 87.17 | 508 | 9.36 | 4,920 | 90.64 | 128 | 2.36 | 5,300 | 97.64 | ||||
| Children aged 5 and under in the household | < 0.001 | < 0.001 | 0.008 | < 0.001 | ||||||||||||||||
| No | 3,785 | 67.62 | 1,813 | 32.38 | 894 | 15.97 | 4,704 | 84.03 | 624 | 11.14 | 4,975 | 88.86 | 220 | 3.94 | 5,378 | 96.06 | ||||
| Yes | 5,271 | 61.60 | 3,286 | 38.40 | 986 | 11.53 | 7,571 | 88.47 | 807 | 9.44 | 7,750 | 90.56 | 204 | 2.39 | 8,353 | 97.61 | ||||
| Area | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||||
| Urban | 4,474 | 73.30 | 1,630 | 26.70 | 1,365 | 22.36 | 4,739 | 77.64 | 841 | 13.78 | 5,262 | 86.22 | 369 | 6.04 | 5,735 | 93.96 | ||||
| Rural | 4,583 | 56.91 | 3,470 | 43.09 | 515 | 6.40 | 7,537 | 93.60 | 590 | 7.32 | 7,463 | 92.68 | 56 | 0.69 | 7,996 | 99.31 | ||||
| Department | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||||
| Alibori | 426 | 35.76 | 765 | 64.24 | 47 | 3.97 | 1,144 | 96.03 | 98 | 8.25 | 1,093 | 91.75 | 6 | 0.53 | 1,185 | 99.47 | ||||
| Atacora | 469 | 50.78 | 455 | 49.22 | 39 | 4.20 | 885 | 95.80 | 38 | 4.11 | 885 | 95.89 | 11 | 1.17 | 913 | 98.83 | ||||
| Atlantique | 1,385 | 70.36 | 584 | 29.64 | 355 | 18.02 | 1,614 | 81.98 | 359 | 18.24 | 1,610 | 81.76 | 126 | 6.38 | 1,843 | 93.62 | ||||
| Borgou | 788 | 52.63 | 709 | 47.37 | 131 | 8.72 | 1,367 | 91.28 | 178 | 11.90 | 1,319 | 88.10 | 30 | 2.03 | 1,467 | 97.97 | ||||
| Collines | 652 | 66.44 | 329 | 33.56 | 51 | 5.19 | 930 | 94.81 | 135 | 13.75 | 846 | 86.25 | 11 | 1.13 | 970 | 98.87 | ||||
| Couffo | 615 | 55.50 | 493 | 44.50 | 62 | 5.62 | 1,046 | 94.38 | 108 | 9.76 | 1,000 | 90.24 | 9 | 0.80 | 1,099 | 99.20 | ||||
| Donga | 316 | 42.67 | 424 | 57.33 | 40 | 5.35 | 701 | 94.65 | 41 | 5.52 | 700 | 94.48 | 2 | 0.26 | 739 | 99.74 | ||||
| Littoral | 839 | 98.54 | 12 | 1.46 | 293 | 34.35 | 559 | 65.65 | 246 | 28.83 | 606 | 71.17 | 135 | 15.90 | 716 | 84.10 | ||||
| Mono | 606 | 69.00 | 272 | 31.00 | 92 | 10.48 | 787 | 89.52 | 38 | 4.33 | 841 | 95.67 | 6 | 0.64 | 873 | 99.36 | ||||
| Ouémé | 1,261 | 77.27 | 371 | 22.73 | 328 | 20.07 | 1,305 | 79.93 | 121 | 7.44 | 1,511 | 92.56 | 60 | 3.65 | 1,573 | 96.35 | ||||
| Plateau | 690 | 70.11 | 294 | 29.89 | 125 | 12.68 | 859 | 87.32 | 15 | 1.50 | 969 | 98.50 | 5 | 0.56 | 979 | 99.44 | ||||
| Zou | 1,009 | 72.14 | 390 | 27.86 | 319 | 22.81 | 1,079 | 77.19 | 54 | 3.85 | 1,345 | 96.15 | 24 | 1.69 | 1,375 | 98.31 | ||||
Fig. 2.
Household access to basic drinking water services by department of residence in Benin, 2017–2018
Sanitation
In 53.91% (95% CI = 51.35–56.44) of the households, members practiced open defecation. Basic sanitation services were reported in 13.28% (95% CI = 12.10–14.57) of households, respectively.
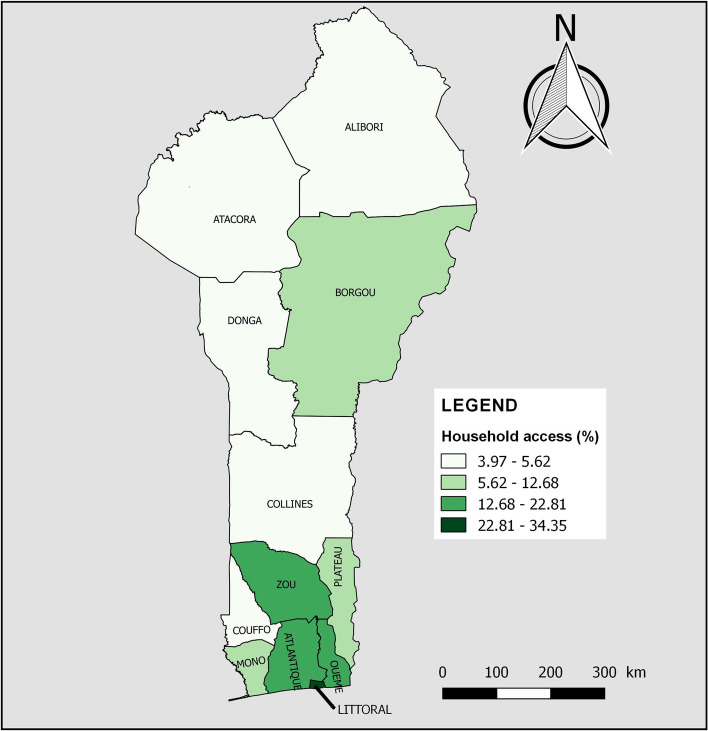
According to Table 4, household coverage of basic sanitation services showed significant differences by age (p < 0.001) and level of education (p < 0.001) of the household head, and by wealth index (p < 0.001). Also, household access to improved non-shared (basic) sanitation facilities was significantly higher in urban areas (22.36% vs 6.40%, p < 0.001) and in households without children aged 5 and under (15.97% vs 11.53%, p < 0.001). Figure 3 shows household access to basic sanitation services by department of residence. The departments in the South and Centre, notably Littoral (34.35%), Zou (22.81%), Ouémé (20.07%) and Atlantique (18.02%), had the highest coverage, unlike Atacora (4.20%) and Alibori (3.97%) in the North (Fig. 3).
Fig. 3.
Household access to basic sanitation services by department of residence in Benin, 2017–2018
Hygiene
Basic handwashing facilities were in 10.11% (95% CI = 9.19–11.11) of households. In contrast, 44.92% (95% CI = 42.72–47.14) had no handwashing facilities.
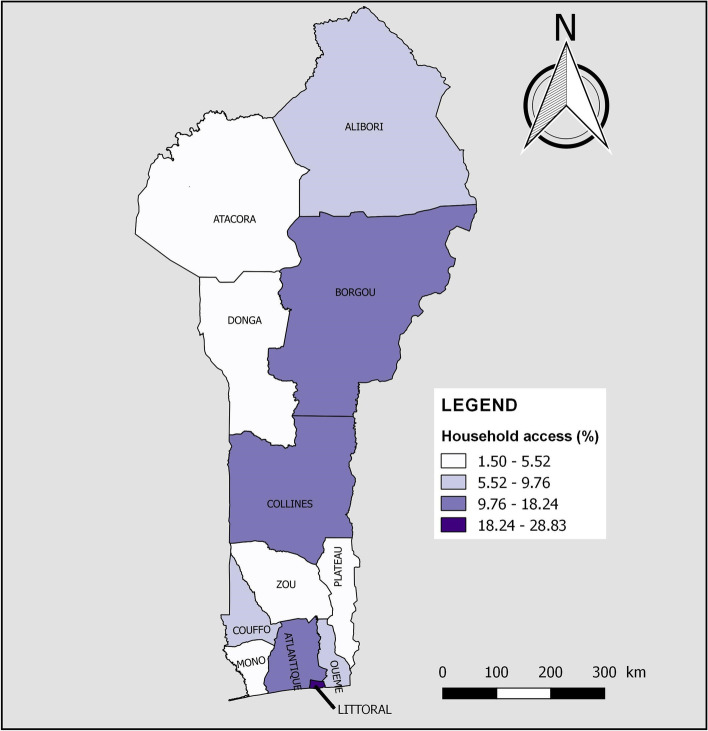
According to Table 4, the availability of handwashing facilities with soap and water increased significantly with the level of education of the household head (p < 0.001). About 24% of the richest households had access to basic handwashing facilities, whereas fewer than 10% of households in the other four wealth quintiles had access to such facilities (p < 0.001). The availability of basic handwashing facilities was significantly higher in households with five or fewer people (10.58% vs 9.36%, p = 0.033), with no children aged 5 and under (11.14% vs 9.44%, p = 0.008) and living in urban areas (13.78% vs 7.32%, p < 0.001). Figure 4 shows household access to basic hygiene services by department of residence. Household access to basic handwashing facilities was highest in Littoral (28.83%), Atlantique (18.24%), Collines (13.75%) and Borgou (11.90%). In the other departments, less than one household in ten had such facilities.
Fig. 4.
Household access to basic hygiene services by department of residence in Benin, 2017–2018
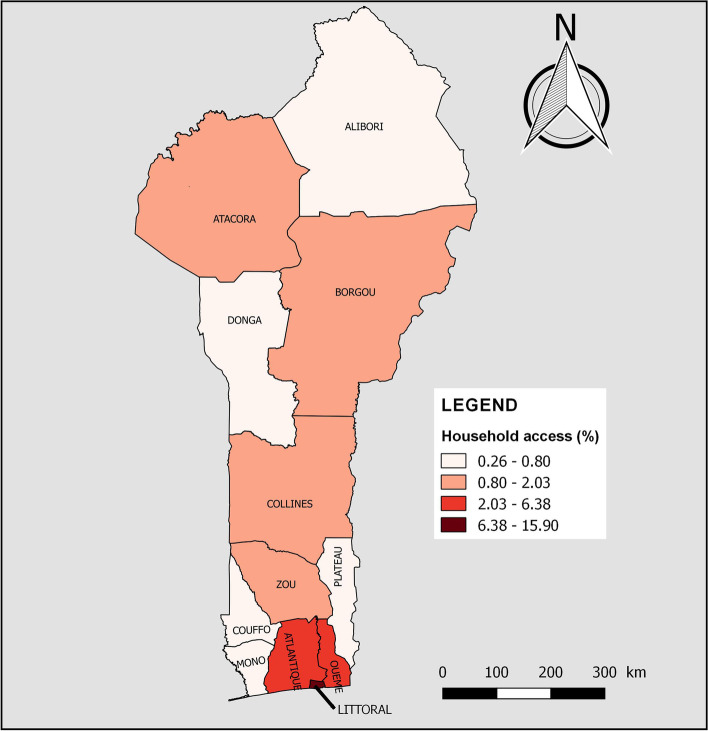
Combined WASH
About 3% (95% CI = 2,53–3,56) of households had access to combined basic WASH services. According to Table 4, household access to combined basic WASH services varied significantly by age (p < 0.001) and level of education of the household head (p < 0.001). It was also higher in households with five or fewer people (3.40% vs 2.36%, p = 0.003), without children aged 5 and under (3.94% vs 2.39%, p < 0.001) and those living in urban areas (6.04% vs 0.69%, p < 0.001). No poorest or middle households had access. However, 12.58%, 0.60% and 0.02% of the poorer, richer and richest household had access to combined basic WASH services, respectively (p < 0.001). Figure 5 shows household access to combined basic WASH services by department of residence. In Couffo (0.80%), Mono (0.64%), Plateau (0.56%), Alibori (0.53%) and Donga (0.26%), less than one in 100 households had access to combined basic WASH facilities.
Fig. 5.
Household access to combined basic WASH services by department of residence in Benin, 2017–2018
Factors associated with WASH services
Table 5 presents the results of the multivariate analysis and highlights the factors associated with household access to individual and combined basic WASH services.
Table 5.
Factors associated with household access to individual and combined basic WASH services, 2017–2018
| Variables | Water | Sanitation | Hygiene | Combined WASH | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | p | aOR | 95% CI | p | aOR | 95% CI | p | aOR | 95% CI | p | |
| Age (years) | ||||||||||||
| < 30 | Ref | Ref | Ref | Ref | ||||||||
| 30–39 | 1.20 | 1.05–1.38 | 0.008 | 1.71 | 1.37–2.13 | < 0.001 | 1.16 | 0.94–1.43 | 0.155 | 1.88 | 1.2–2.94 | 0.006 |
| 40–49 | 1.19 | 1.04–1.38 | 0.014 | 3.33 | 2.68–4.13 | < 0.001 | 1.49 | 1.22–1.83 | < 0.001 | 4.15 | 2.77–6.21 | < 0.001 |
| 50–59 | 1.17 | 1.01–1.35 | 0.035 | 3.78 | 2.94–4.84 | < 0.001 | 1.51 | 1.22–1.87 | < 0.001 | 4.26 | 2.9–6.26 | < 0.001 |
| ≥ 60 | 1.06 | 0.92–1.22 | 0.431 | 4.80 | 3.76–6.12 | < 0.001 | 1.65 | 1.32–2.06 | < 0.001 | 6.02 | 3.95–9.18 | < 0.001 |
| Sex | ||||||||||||
| Male | Ref | Ref | ||||||||||
| Female | 1.13 | 1.01–1.25 | 0.031 | 1.32 | 1.14–1.53 | < 0.001 | ||||||
| Level of education | ||||||||||||
| No formal education | Ref | Ref | Ref | |||||||||
| Primary | 1.09 | 0.91–1.30 | 0.336 | 1.22 | 1.01–1.46 | 0.040 | 1.23 | 0.81–1.87 | 0.329 | |||
| Secondary | 1.65 | 1.37–1.98 | < 0.001 | 1.71 | 1.42–2.05 | < 0.001 | 2.92 | 1.99–4.27 | < 0.001 | |||
| Higher | 3.54 | 2.73–4.59 | < 0.001 | 3.18 | 2.50–4.04 | < 0.001 | 9.84 | 6.55–14.77 | < 0.001 | |||
| Wealth index | ||||||||||||
| Poorest | Ref | Ref | Ref | Ref | ||||||||
| Poorer | 1.48 | 1.26–1.74 | < 0.001 | 7.61 | 1.48–39.28 | 0.015 | 1.40 | 1.02–1.93 | 0.038 | |||
| Middle | 1.85 | 1.54–2.22 | < 0.001 | 22.13 | 4.55–107.55 | < 0.001 | 1.61 | 1.19–2.19 | 0.002 | |||
| Richer | 2.80 | 2.27–3.45 | < 0.001 | 143.28 | 29.90–686.56 | < 0.001 | 2.18 | 1.58–3.01 | < 0.001 | 19.27 | 2.63–141.13 | 0.004 |
| Richest | 7.06 | 5.38–9.27 | < 0.001 | 651.82 | 136.20–3,119.53 | < 0.001 | 4.93 | 3.54–6.88 | < 0.001 | 380.23 | 55.99–2,581.98 | < 0.001 |
| Household size | ||||||||||||
| ≤ 5 | 1.15 | 1.04–1.28 | 0.007 | |||||||||
| > 5 | Ref | |||||||||||
| Department | ||||||||||||
| Alibori | Ref | 1.86 | 1.12–3.10 | 0.017 | 8.34 | 4.19–16.60 | < 0.001 | 5.27 | 1.10–25.16 | 0.037 | ||
| Atacora | 2.04 | 1.34–3.12 | 0.001 | 1.51 | 0.82–2.78 | 0.181 | 3.45 | 1.60–7.43 | 0.002 | 6.89 | 1.58–29.96 | 0.010 |
| Atlantique | 2.51 | 1.54–4.09 | < 0.001 | 2.13 | 1.43–3.18 | < 0.001 | 10.10 | 5.06–20.15 | < 0.001 | 12.25 | 2.91–51.64 | 0.001 |
| Borgou | 1.74 | 1.16–2.61 | 0.007 | 1.81 | 1.10–2.97 | 0.019 | 9.04 | 4.73–17.28 | < 0.001 | 6.43 | 1.57–26.30 | 0.010 |
| Collines | 2.82 | 1.76–4.51 | < 0.001 | Ref | 10.67 | 5.50–20.69 | < 0.001 | 4.46 | 0.83–24.12 | 0.082 | ||
| Couffo | 1.92 | 1.15–3.22 | 0.013 | 1.65 | 1.00–2.75 | 0.052 | 7.96 | 4.00–15.85 | < 0.001 | 4.20 | 0.83–21.22 | 0.082 |
| Donga | 1.01 | 0.63–1.64 | 0.956 | 1.04 | 0.56–1.93 | 0.912 | 3.72 | 1.64–8.44 | 0.002 | Ref | ||
| Littoral | 32.13 | 14.23–72.56 | < 0.001 | 1.49 | 0.99–2.23 | 0.054 | 9.10 | 4.62–17.92 | < 0.001 | 10.77 | 2.66–43.62 | 0.001 |
| Mono | 3.12 | 1.79–5.43 | < 0.001 | 1.92 | 1.22–3.02 | 0.005 | 2.50 | 1.02–6.11 | 0.044 | 1.65 | 0.29–9.28 | 0.568 |
| Ouémé | 3.28 | 2.05–5.24 | < 0.001 | 2.05 | 1.35–3.11 | 0.001 | 3.20 | 1.60–6.38 | 0.001 | 5.73 | 1.41–23.29 | 0.015 |
| Plateau | 3.48 | 2.17–5.58 | < 0.001 | 3.60 | 2.23–5.81 | < 0.001 | Ref | 2.57 | 0.41–16.05 | 0.311 | ||
| Zou | 3.27 | 2.02–5.27 | < 0.001 | 6.44 | 4.04–10.29 | < 0.001 | 2.19 | 1.08–4.42 | 0.029 | 4.81 | 1.15–20.20 | 0.032 |
aOR Adjusted Odd Ratio, Ref Reference category
For identifying predictors of combined basic WASH services, the categories 'Poorest' and ' Poorer' of the 'Wealth Index' were put together, as well as 'Middle' and 'Richer'
Water
Factors associated with household access to basic water facilities were age and sex of the household head, and size, wealth index and department of the household. The odds of having access to basic water facilities was significantly higher in households whose heads were aged 30–39 (aOR = 1.20, 95% CI = 1.05–1.38), compared to those whose heads were under 30. Compared to male-headed households, female-headed households were 1.13 times (aOR = 1.13, 95% CI = 1.01–1.25) more likely to have access to basic drinking water services. Also, the odds of having access to basic drinking water services increased significantly with the wealth index. Compared to the poorest households, the richest households were 7.06 times (aOR = 7.06, 95% CI = 5.38–9.27) more likely to have access. Households with five or fewer people were 1.15 times (aOR = 1.15, 95% CI = 1.04–1.28) more likely to have access to basic water facilities compared to households with more than five people. Compared to households in Alibori, those in Littoral (aOR = 32.13, 95% CI = 14.23—72.56) had much higher odds of basic water service coverage.
Sanitation
Factors associated with household access to basic sanitation facilities were age, sex and level of education of the household head, and wealth index and department of the household. The likelihood of a household with a head aged 60 and over having access to basic sanitation facilities was multiplied by 4.80 (aOR = 4.80, 95% CI = 3.76–6.12) compared to a household headed by a person under 30 years old. Female-headed households (aOR = 1.32, 95% CI = 1.14–1.53) were more likely to have access to basic sanitation facilities. Households with higher educated heads were 3.54 times (aOR = 3.54, 95% CI = 2.73–4.59) more likely to have access to basic sanitation facilities compared to households with heads who had no formal education. The richest households (aOR = 651.82, 95% CI = 136.20–3,119.53) were more likely to have access to basic sanitation facilities than the poorest households. Furthermore, compared to Collines, Zou (aOR = 6.44, 95% CI = 4.04–10.29) were associated with significantly higher odds of access to basic sanitation services.
Hygiene
Factors associated with household access to basic handwashing facilities were age and level of education of the household head, and wealth index and department of the household. Thus, households with a head aged 60 years and over were 1.65 times (aOR = 1.65, 95% CI = 1.32–2.06) more likely to have handwashing facilities with soap and water compared to households with heads under 30 years old. Households whose heads had a higher level of education were 3.18 times (aOR = 3.18, 95% CI = 2.50–4.04) more likely to have access to basic hygiene services than households headed by people with no formal education. The richest households were 4.93 times (aOR = 4.93, 95% CI = 3.54–6.88) more likely to have basic handwashing facilities than the poorest households. Compared to Plateau, the other departments were associated with significantly higher odds of access to basic hygiene services (p < 0.05). Households in the Atlantique, Collines and Littoral were 10.10 (aOR = 10.10, 95% CI = 5.06–20.15), 10.67 (aOR = 10.67, 95% CI = 5.50–20.69) and 9.10 (aOR = 9.10, 95% CI = 4.62–17.92) times more likely to have access to basic handwashing facilities, respectively.
Combined WASH
Factors associated with combined basic WASH services were age and level of education of the household head, and wealth index and department of residence of the household. Households with heads aged 60 years and above and with higher education levels were 6.02 (aOR = 6.02, 95% CI = 3.95–9.18) and 9.84 (aOR = 9.84, 95% CI = 6.55–14.77) times more likely to have access to combined basic WASH services, respectively. Also, the richest households (aOR = 380.23, 95% CI = 55.99–2,581.98) were more likely to have access to combined basic WASH services than the poorest/poorer. The odds of a household having access to combined basic WASH services were significantly higher in Atlantique (aOR = 12.25, 95% CI = 2.91–51.64) and Littoral (aOR = 10.77, 95% CI = 2.66–43.62), compared to Donga.
Discussion
This study aimed to provide an overview of household access to WASH facilities using nationally representative data. The study estimated the proportion of households using basic WASH services and identified predictors of access to these facilities. The use of nationally representative data, which can improve the generalisation of results, is one of the strengths of this study.
About 6% of households used water from rivers, dams, lakes, ponds, streams, canals or irrigation canals. Based on the results of previous DHS, there is a downward trend in the proportion of households using surface water for drinking (12.1% in 2001, 9.9% in 2006, 3.6% in 2011–2012 and 5.84% in 2017–2018) [33, 39, 40]. According to the results of this study, 63.98% and 7.77% of households used basic and limited drinking water facilities, respectively. It indicates that 71.75% of households use improved drinking water facilities. Hence, the proportion of households using such facilities increased by 4% between 2001 and 2017–2018, from 66.50% to 71.75% [33, 39, 40]. By comparison, the proportion of households with access to improved drinking water sources found in other African countries and Asia was higher than that noted here. Indeed, a percentage ranging from 68.5% to 97.6% of households using water from an improved source was recorded in Ethiopia [21, 22], Ghana [23], Malaysia [24], Eswatini [27] and Vietnam [30]. Regarding household access to basic drinking water services, a study in Bangladesh in 2021 reported a proportion of 99.5% compared to 63.98% in this study [25]. This proportion is still higher than that estimated for sub-Saharan Africa (53.6%) in 2017 [41].
More than half of the households had no access to sanitation facilities or toilets and practised open defecation. There is evidence of a gradual decrease in the proportion of households practising open defecation: from 67% in 2001 to 61.7% in 2006, then 54.2% in 2011–2012 and finally 53.91% in 2017–2018 [33, 39, 40]. This decrease can be attributed to various interventions in Benin to reduce the prevalence of open defecation [14–17]. Between 2014 and 2017, the CTPS approach resulted in 2,724 localities achieving open defecation free status [16]. Nevertheless, there is a need to strengthen initiatives to combat open defecation. In sub-Saharan Africa, the overall prevalence of open defecation (53.91%) is about half that observed in this study [41]. It ranged from 12.02% in East Africa to 31.10% in West Africa [41]. Furthermore, 21.04% and 13.28% of the surveyed households used limited and basic sanitation services, respectively. Thus, 34.32% had access to improved sanitation facilities. Studies in Ethiopia, Ghana, Vietnam and Afghanistan found percentages ranging from 12 to 85.7% [22, 23, 28–30]. The results of a study in Malaysia indicated that this country has almost achieved universal coverage of improved sanitation facilities [24]. The present study found that only 13.28% of households use improved non-shared (basic) sanitation facilities. However, this proportion has increased significantly from 2001 to 2017–2018 (3% in 2001, 7% in 2006, 15.2% in 2011–2012, and 13.28% in 2017–2018) [33, 39, 40]. In Bangladesh, the proportion of households using basic sanitation services is more than four times higher than the proportion we found [25].
The proportion of households without handwashing facilities has decreased substantially over the past two decades (96.1% in 2001, 94.1% in 2006, 68.9% in 2011–2012 and 44.92% in 2017–2018) [33, 39, 40]. However, only 10.11% of households had basic handwashing facilities. A study in 2021 reported a proportion of 56.3% [25].
Approximately 3% of households had access to combined basic WASH services, compared to 40.2% in Bangladesh in 2021 [25]. In sub-Saharan Africa, household-level access to combined basic WASH services ranges from 0.8% in Liberia to 22.6% in Namibia, with a regional average of only 4.2% [41].
The results of this study suggest that households with heads aged 30 and over were more likely to have access to individual and combined basic WASH services. The older the age of the household head, the more likely households were to have access to these services. One possible explanation is that individuals aged 30 and over, in the majority of cases, are in the active economic group and are more likely to install basic WASH facilities, especially when they own their homes [28]. Also, the low level of financial resources available to some young people, especially those under 30, may lead them to opt for cheap homes (especially rented ones), which may not have basic WASH facilities. Also, some authors suggest that as people age, they make choices or adopt behaviours that improve their quality of life [23]. The findings of some studies in Ethiopia and Ghana are consistent with the current one [21, 23, 28]. They indicated that households headed by older people were more likely to have access to improved water and sanitation facilities [21, 23, 28]. In contrast, in Eswatini, the age of the household head was negatively associated with the use of water from an improved source [27]. The older the household head, the less likely the household was to have access to improved water sources. According to the authors, the majority of older subjects (i.e. 35 years and older) in their sample came from poor households and mainly from rural areas and therefore could not afford improved drinking water sources [27].
The odds for access to basic water and sanitation facilities were significantly higher among female-headed households. Some studies reported similar results [22, 23]. Some authors suggest that, compared to men, most women in sub-Saharan Africa have greater responsibilities within the household, associated with high water use [23]. To reduce the burden of fetching water in remote locations, women heads of household ensure that their families have good access to water and sanitation facilities [23]. Findings in the opposite direction were found by other studies; i.e. male-headed households were more likely to have access to improved drinking water and sanitation facilities [27, 28]. Concerning access to water, one of the reasons given was that households with low coverage of improved water sources are located in rural areas, where most female-headed households are found [27].
A positive relationship was found between the level of education of the household head and access to basic sanitation and hygiene services. The higher the education level of the household head, the more likely the household was to be covered by these services. The same relation is noted for access to combined basic WASH services. These results are consistent with findings from other studies [22, 23, 25, 28, 30]. The level of education is an essential social determinant of health that influences, most notably, the ability to make better decisions about the health of household members [42]. In the present study, the more educated household heads would be more aware of the benefits of improved and basic WASH conditions. Since it is not possible to improve the level of education of household heads at a late point in their lives, some authors have suggested an approach based on large-scale promotional campaigns focusing on people's access to WASH services [25]. Some studies have shown the beneficial effects of mass awareness and promotion interventions on increasing access to WASH facilities [43, 44].
The findings of this study suggest that the better the wealth status of households, the more likely they are to be covered by individual and combined basic WASH services. Indeed, access to these facilities increased significantly from the second wealth quintile (poorer) onwards, reaching its highest level in the last quintile (richest). Other studies supported these results [22–25, 27, 28, 30]. The richest households can afford the costs associated with connection to the National Water Company (SONEB, Société Nationale des Eaux du Benin in French), and the installation of improved private toilets and functional handwashing facilities in the home. These expenditures may seem high for the poorest households who face other constraints and daily expenses. Specifically for this study, there appears to be a disproportionate difference in the odds of access to individual and combined basic WASH facilities between the richest and poorest households. In recent years, interventions to improve access to WASH have focused on the poorest people [14]. The results of this study show the relevance of this strategy but indicate that much more needs to be done. Providing financial assistance to the poorest populations to enable them to acquire adequate WASH equipment is an option that should be explored. In this perspective, the path of microfinance, which has the potential to offer more flexibility to the poorest, deserves to be taken. Microfinance has evolved considerably over the past decades, from micro-credit for the poorest to a wide range of financial and non-financial services and products targeted to the needs of poor men and women [45]. Integrating population-based WASH products with microfinance has been tested in some settings, with interesting results [46–48].
This study found a negative association between an increase in the number of members in the household and access to basic drinking water services. This result is in line with the findings of a study in Eswatini in 2020 in which the authors advocated for enhanced promotion of family planning products [27]. In contrast, a positive association between household size and access to basic WASH facilities was found in Bangladesh in 2021 [25]. According to the authors, regardless of their economic status, larger families may spend more on basic WASH facilities [25]. In the Beninese context, where some studies show a positive relationship between poverty and household size [49, 50], a high number of people in the household is associated with high expenditure on water consumption. This could explain why some households choose to use unimproved facilities to limit the costs of using basic water facilities.
We found that the proportion of households with access to individual and combined basic WASH services was higher in urban than in rural areas. However, all other things being equal, area of residence was not a factor associated with household access to WASH services.
Compared to basic sanitation and hygiene facilities, basic drinking water services were the most available at the household level, with the Littoral reaching universal coverage. Interventions need to be strengthened so that everyone has effective access. As regards basic sanitation and hygiene services, the coverage observed remains relatively low, even in the Littoral, although it has the highest level of access. Specifically for the country, this study found that all other things being equal, households in Alibori, Collines, Plateau and Donga were the least likely to have access to individual and combined basic WASH services. They should therefore be the focus of special attention.
The main limitation of this study is that it is a cross-sectional study, which does not allow a causal relationship to be established with certainty between the identified predictors and the outcomes.
Conclusion
In 24, despite the progress made, there is still a lack of coverage of households with basic WASH facilities. Only 3% of households in Benin had the three main components of WASH facilities at a basic level. The study also identified predictors of household access to individual and combined basic WASH. Overall, the richest households and few, and those headed by people over 30 years old, female and with higher levels of education, were the most likely to have access to individual and combined basic WASH. In addition, disparities based on the department of residence were observed. This reflects the multifactorial reality of the issue of people's access to appropriate WASH services. Consequently, isolated or single-factor interventions can only lead to limited results. This will require better integration of the various interventions carried out as well as better concertation and coordination between the actors. The CLTS approach developed by UNICEF, which aims to end open defecation, is a good example. On the basis of the results, the following suggestions were made: implement large-scale promotion campaigns focusing on people's access to WASH services, strengthen poverty fighting at national and local levels and provide financial support to the poorest people, promote family planning and take into account regional disparities. Future studies can examine the impact of additional factors on household access to WASH services that have not been studied here.
Acknowledgements
We would like to thank the DHS program for authorising us to use the data used in this study.
Abbreviations
- aOR
Adjusted Odd Ratio
- CI
Confidence Interval
- CNERS
National Committee on Health Research Ethics (Comité National d’Ethique pour la Recherche en Santé)
- CNS
National Statistical Council (Conseil National de la Statistique)
- cOR
Crude Odd Ratio
- DALYs
Disability-Adjusted Life Years
- CLTS
Community-Led Total Sanitation
- DHS
Demographic and Health Survey
- EA
Enumeration Area
- INStaD
National Institute of Statistics and Demography (Institut National de la Statistique et de la Démographie)
- JMP
WHO/UNICEF Joint Monitoring Programme
- PND
National Development Plan (Plan National de Développement)
- PNDS
Health Development Plan (Plan National de Développement Sanitaire)
- PPS
Probability Proportional to the Size
- PSU
Primary Sample Units
- RGPH
General Census of Population and Housing (Recensement Général de la Population et de l'Habitation)
- SDG
Sustainable Development Goals
- SNPHAB
National Strategy for the Promotion of Hygiene and Basic Sanitation (Stratégie Nationale de Promotion de l’Hygiène et de l’Assainissement de Base)
- SONEB
Benin National Water Company (Société Nationale des Eaux du Benin)
- UNGA
United Nations General Assembly
- UNICEF
United Nations International Children's Fund
- USAID
United States Agency for International Development
- WASH
Water, Sanitation and Hygiene
- WHO
World Health Organization
Authors’ contributions
N.G. contributed to conceptualisation, methodology, data curation, formal analysis, visualisation, validation, preparation, revision and editing of the original draft. A.K. and C.D. participated in conceptualisation, methodology, validation, revision of the original draft and supervision. Y.G.A. was engaged in conceptualisation, methodology, revision of the original draft and supervision. R.G.K. and R.S. helped with the conceptualisation, revision of the original draft and administration of the project. All authors have read and approved this version of the manuscript.
Funding
This research received no external funding.
Availability of data and materials
The data used in this study can be obtained by sending a request via the DHS Program website to https://dhsprogram.com/data/dataset/Benin_Standard-DHS_2017.cfm?flag=0
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical principles stated in the Helsinki Declaration. The launch of the DHS-V data collection was conditional on the authorisation of the National Statistical Council and the approval of the National Committee on Health Research Ethics. During data collection, the informed consent of eligible respondents was sought before starting the interviews. The dataset used was fully anonymised.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UN General Assembly. The human right to water and sanitation : resolution / adopted by the General Assembly. 2010.
- 2.United Nations. The 17 Goals | Sustainable Development. https://sdgs.un.org/goals. Accessed 19 Dec 2021.
- 3.World Health Organization, United Nations Children’s Fund (UNICEF). Progress on household drinking water, sanitation and hygiene 2000–2020: five years into the SDGs. Geneva: WHO; 2021.
- 4.World Health Organization, United Nations Children’s Fund (UNICEF) Progress on drinking water, sanitation and hygiene 2017 update and SDG baselines. Geneva: WHO; 2017. [Google Scholar]
- 5.Wolf J, Hunter PR, Freeman MC, Cumming O, Clasen T, Bartram J, et al. Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: updated meta-analysis and meta-regression. Trop Med Int Health. 2018;23:508–525. doi: 10.1111/tmi.13051. [DOI] [PubMed] [Google Scholar]
- 6.Luby SP, Rahman M, Arnold BF, Unicomb L, Ashraf S, Winch PJ, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Glob Health. 2018;6:e302–e315. doi: 10.1016/S2214-109X(17)30490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobsen K, Koopman J. The effects of socioeconomic development on worldwide hepatitis A virus seroprevalence patterns. Int J Epidemiol. 2005;34:600–609. doi: 10.1093/ije/dyi062. [DOI] [PubMed] [Google Scholar]
- 8.Im J, Islam MT, Ahmmed F, Kim DR, Islam Khan A, Zaman K, et al. Can Existing Improvements of Water, Sanitation, and Hygiene (WASH) in Urban Slums Reduce the Burden of Typhoid Fever in These Settings? Clin Infect Dis. 2021;72:e720–e726. doi: 10.1093/cid/ciaa1429. [DOI] [PubMed] [Google Scholar]
- 9.Mehndiratta MM, Mehndiratta P, Pande R. Poliomyelitis Neurohospitalist. 2014;4:223–229. doi: 10.1177/1941874414533352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashraf S, Islam M, Unicomb L, Rahman M, Winch PJ, Arnold BF, et al. Effect of Improved Water Quality, Sanitation, Hygiene and Nutrition Interventions on Respiratory Illness in Young Children in Rural Bangladesh: A Multi-Arm Cluster-Randomized Controlled Trial. Am J Trop Med Hyg. 2020;102:1124–1130. doi: 10.4269/ajtmh.19-0769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . Safer water, better health. Geneva: World Health Organization; 2019. [Google Scholar]
- 12.Ministère de la Santé. Plan National de Développement Sanitaire 2018-2022. Cotonou, Bénin: Ministère de la Santé; 2018
- 13.Ministère du Plan et du Dévloppement. Plan de National de Développement 2018-2025. 2018
- 14.Houngnihin R, Fousseni P, Agossou E, Amoussou A. Stratégie nationale de promotion de l’hygiène et de l’assainissement de base (SNPHAB) en milieu rural au Bénin (2018-2030). Cotonou: GIZ & DNSP; 2018
- 15.SNV Netherlands Development Organisation. Hygiene and sanitation with Community Led Total Sanitation. 2021. https://snv.org/project/hygiene-and-sanitation-community-led-total-sanitation. Accessed 15 Dec 2021.
- 16.UNICEF Bénin. Survie UNICEF Bénin : Eau, Hygiène, Assainissement. 2020. https://www.unicef.org/benin/recits/eau-hygi%C3%A8ne-assainissement. Accessed 10 Nov 2021.
- 17.Hoteyi S, Agbodande M, Gnimadi C, Oussou R, Padonou U, Comlanvi F, et al. Équilibre d’un écosystème par l’Assainissement Total Piloté par la Communauté (ATPC) au Bénin. BRAB. 2018;:1–15.
- 18.Prüss-Ustün A, Wolf J, Bartram J, Clasen T, Cumming O, Freeman MC, et al. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low- and middle-income countries. Int J Hyg Environ Health. 2019;222:765–777. doi: 10.1016/j.ijheh.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reiner RC, Graetz N, Casey DC, Troeger C, Garcia GM, Mosser JF, et al. Variation in Childhood Diarrheal Morbidity and Mortality in Africa, 2000–2015. N Engl J Med. 2018;379:1128–1138. doi: 10.1056/NEJMoa1716766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simen-Kapeu A, Bogler L, Weber A-C, Ntambi J, Zagre NM, Vollmer S, et al. Prevalence of diarrhoea, acute respiratory infections, and malaria over time (1995–2017): A regional analysis of 23 countries in West and Central Africa. J Glob Health. 2021;11:13008. doi: 10.7189/jogh.11.13008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gebremichael SG, Yismaw E, Tsegaw BD, Shibeshi AD. Determinants of water source use, quality of water, sanitation and hygiene perceptions among urban households in North-West Ethiopia: A cross-sectional study. PLoS One. 2021;16:e0239502. doi: 10.1371/journal.pone.0239502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andualem Z, Dagne H, Azene ZN, Taddese AA, Dagnew B, Fisseha R, et al. Households access to improved drinking water sources and toilet facilities in Ethiopia: a multilevel analysis based on 2016 Ethiopian Demographic and Health Survey. BMJ Open. 2021;11:e042071. doi: 10.1136/bmjopen-2020-042071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agbadi P, Darkwah E, Kenney PL. A Multilevel Analysis of Regressors of Access to Improved Drinking Water and Sanitation Facilities in Ghana. J Environ Public Health. 2019;2019:e3983869. doi: 10.1155/2019/3983869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kong Y-L, Anis-Syakira J, Fun WH, Balqis-Ali NZ, Shakirah MS, Sararaks S. Socio-Economic Factors Related to Drinking Water Source and Sanitation in Malaysia. Int J Environ Res Public Health. 2020;17:E7933. doi: 10.3390/ijerph17217933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmed MS, Islam MI, Das MC, Khan A, Yunus FM. Mapping and situation analysis of basic WASH facilities at households in Bangladesh: Evidence from a nationally representative survey. PLoS ONE. 2021;16:e0259635. doi: 10.1371/journal.pone.0259635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anthonj C, Githinji S, Kistemann T. The impact of water on health and ill-health in a sub-Saharan African wetland: Exploring both sides of the coin. Sci Total Environ. 2018;624:1411–1420. doi: 10.1016/j.scitotenv.2017.12.232. [DOI] [PubMed] [Google Scholar]
- 27.Simelane MS, Shongwe MC, Vermaak K, Zwane E. Determinants of Households’ Access to Improved Drinking Water Sources: A Secondary Analysis of Eswatini 2010 and 2014 Multiple Indicator Cluster Surveys. Adv Public Health. 2020;2020:e6758513. doi: 10.1155/2020/6758513. [DOI] [Google Scholar]
- 28.Akpakli DE, Manyeh AK, Akpakli JK, Kukula V, Gyapong M. Determinants of access to improved sanitation facilities in rural districts of southern Ghana: evidence from Dodowa Health and Demographic Surveillance Site. BMC Res Notes. 2018;11:473. doi: 10.1186/s13104-018-3572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muslim EU, Stanikzai MH, Wasiq AW, Khan A, Sayam H. The Availability of Improved Sanitation Facilities and Its Associated Factors in the 12th District of Kandahar City. Afghanistan J Environ Public Health. 2021;2021:e5569582. doi: 10.1155/2021/5569582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tuyet-Hanh TT, Lee J-K, Oh J, Van Minh H, Ou Lee C, Hoan LT, et al. Household trends in access to improved water sources and sanitation facilities in Vietnam and associated factors: findings from the Multiple Indicator Cluster Surveys, 2000–2011. Glob Health Action. 2016;9:29434. doi: 10.3402/gha.v9.29434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Admasie A, Debebe A. Estimating Access to Drinking Water Supply, Sanitation, and Hygiene Facilities in Wolaita Sodo Town, Southern Ethiopia, in Reference to National Coverage. J Environ Public Health. 2016;2016:1–9. doi: 10.1155/2016/8141658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson RC, Boni G, Barogui Y, Sopoh GE, Houndonougbo M, Anagonou E, et al. Assessment of water, sanitation, and hygiene practices and associated factors in a Buruli ulcer endemic district in Benin (West Africa) BMC Public Health. 2015;15:801. doi: 10.1186/s12889-015-2154-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institut National de la Statistique et de l’Analyse Economique, ICF. Enquête Démographique et de Santé 2011-2012. Cotonou, Bénin & Calverton, Maryland, USA: INSAE & Calverton; 2013
- 34.Institut National de la Statistique et de l’Analyse Economique. Fiche de données sur la population au Bénin. 2018. https://www.insae-bj.org/statistiques/indicateurs-recents/43-population. Accessed 12 Dec 2019.
- 35.Institut National de la Statistique et de l’Analyse Économique. Recensement Général de la Population et de l’Habitation IV : Cahier des villages et quartiers de ville Littoral. 2016.
- 36.Croft, Trevor N, Aileen M. J. M, Courtney K. A. Guide to DHS Statistics. Rockville, Maryland, USA: ICF; 2018.
- 37.Institut National de la Statistique et de l’Analyse Economique, ICF. Enquête Démographique et de Santé 2017–2018. Cotonou, Bénin & Rockville, Maryland, USA: INSAE & ICF; 2019.
- 38.El Sanharawi M, Naudet F. Comprendre la régression logistique. J Fr Ophtalmol. 2013;36:710–715. doi: 10.1016/j.jfo.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 39.Institut National de la Statistique et de l’Analyse Economique, ORC Macro. Enquête Démographique et de Santé 2001. Cotonou, Bénin & Calverton, Maryland, USA: INSAE & ORC Macro; 2001
- 40.Institut National de la Statistique et de l’Analyse Economique, Macro International Inc. Enquête Démographique et de Santé 2006. Cotonou, Bénin & Calverton, Maryland, USA: INSAE & Macro International Inc.; 2007
- 41.Belay DG, Asratie MH, Aragaw FM, Tsega NT, Endalew M, Gashaw M. Open defecation practice and its determinants among households in sub-Saharan Africa: pooled prevalence and multilevel analysis of 33 sub-Saharan Africa countries demographic and health survey. Trop Med Health. 2022;50:28. doi: 10.1186/s41182-022-00416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anctil H, Jobin L, Pigeon M, Emond A, Quebec (Province), Ministère de la santé et des services sociaux, et al. La santé et ses déterminants mieux comprendre pour mieux agir. Québec: Ministère de la santé et des services sociaux, Direction des communications; 2012.
- 43.Gizaw Z, Addisu A, Dagne H. Effects of water, sanitation and hygiene (WASH) education on childhood intestinal parasitic infections in rural Dembiya, northwest Ethiopia: an uncontrolled before-and-after intervention study. Environ Health Prev Med. 2019;24:16. doi: 10.1186/s12199-019-0774-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gizaw Z, Addisu A. Evidence of Households’ Water, Sanitation, and Hygiene (WASH) Performance Improvement Following a WASH Education Program in Rural Dembiya. Northwest Ethiopia Environ Health Insights. 2020;14:1178630220903100. doi: 10.1177/1178630220903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sainz-Fernandez I, Torre-Olmo B, López-Gutiérrez C, Sanfilippo-Azofra S. Development of the Financial Sector and Growth of Microfinance Institutions: The Moderating Effect of Economic Growth. Sustainability. 2018;10:3930. doi: 10.3390/su10113930. [DOI] [Google Scholar]
- 46.Davis J, White G, Damodaron S, Thorsten R. Improving access to water supply and sanitation in urban India: microfinance for water and sanitation infrastructure development. Water Sci Technol J Int Assoc Water Pollut Res. 2008;58:887–891. doi: 10.2166/wst.2008.671. [DOI] [PubMed] [Google Scholar]
- 47.Geissler KH, Goldberg J, Leatherman S. Using microfinance to facilitate household investment in sanitation in rural Cambodia. Health Policy Plan. 2016;31:1193–1199. doi: 10.1093/heapol/czw051. [DOI] [PubMed] [Google Scholar]
- 48.Dhungana BR, Singh JK, Acharya D, Gautam S, Paudyal P. Perceived Usefulness of a Microfinance Intervention on Health Awareness and Practices in Nepal. Front Public Health. 2016;3:289. doi: 10.3389/fpubh.2015.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Attanasso M-O. Analyse des déterminants de la pauvreté monétaire des femmes chefs de ménage au Bénin. Mondes En Dev. 2004;128:41–63. [Google Scholar]
- 50.Alexandre B, Damien M, Djabar A, Elise A, Mouchitaba L, Raïmi E. Note sur la pauvreté au Bénin en 2015. Cotonou: INSAE; 2015
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study can be obtained by sending a request via the DHS Program website to https://dhsprogram.com/data/dataset/Benin_Standard-DHS_2017.cfm?flag=0